Abstract
Tick-borne pathogens cause infectious diseases that inflict much societal and financial hardship worldwide. Blacklegged ticks, Ixodes scapularis, are primary vectors of several epizootic and zoonotic pathogens. The aim was to find varius pathogens of I. scapularis and to determine their prevalence. In Ontario and Quebec, 113 I. scapularis ticks were collected from songbirds, mammals, including humans, and by flagging. PCR and DNA sequencing detected five different microorganisms: Anaplasma phagocytophilum, 1 (0.9%); Babesia odocoilei, 17 (15.3%); Babesia microti-like sp., 1 (0.9%); Borrelia burgdorferi sensu lato (Bbsl), 29 (26.1%); and Hepatozoon canis, 1 (0.9%). Five coinfections of Bbsl and Babesia odocoilei occurred. Notably, H. canis was documented for the first time in Canada and, at the same time, demonstrates the first transstadial passage of H. canis in I. scapularis. Transstadial passage of Bbsl and B. odocoilei was also witnessed. A novel undescribed piroplasm (Babesia microti-like) was detected. An established population of I. scapularis ticks was detected at Ste-Anne-de-Bellevue, Quebec. Because songbirds widely disperse I. scapularis larvae and nymphs, exposure in an endemic area is not required to contract tick-borne zoonoses. Based on the diversity of zoonotic pathogens in I. scapularis ticks, clinicians need to be aware that people who are bitten by I. scapularis ticks may require select antimicrobial regimens.
Keywords: tick-borne pathogens, Anaplasma phagocytophilum, Borrelia burgdorferi sensu lato, Babesia odocoilei, Babesia sp., Hepatozoon canis, blacklegged tick, Ixodes scapularis, Ontario, Quebec
1. Introduction
Tick-borne zoonotic diseases cause unrelenting woe and hardship worldwide. Polymicrobial infections typically complicate diagnosis and augment disease severity, which result in more disabling sequelae of illness. Tick-borne polymicrobial infections are relatively common in patients, but infrequently reported [1,2,3]. These zoonoses range from subclinical to fatal infections with a disproportionate incidence in children and the elderly.
In North America, Lyme disease caused by Borrelia burgdorferi sensu lato (Bbsl) is the most commonly reported tick-borne disease. Several other tick-related diseases include human anaplasmosis, human babesiosis, and human bartonellosis. When ticks are laden with multiple pathogens, they have the potential for simultaneous transmission of two or more pathogenic microorganisms to a host [4,5]. Notably, four different tick-borne zoonotic pathogens in a single blacklegged tick, Ixodes scapularis (Acari: Ixodidae), have been reported [6].
In North America, I. scapularis can harbor any combination of at least nine different pathogens [7,8]. This tick species is widely distributed east of the Rocky Mountains, and is dispersed by migratory songbirds (Order: Passeriformes) as far west and north as northwestern Alberta, and as far east and north as the southern part of Newfoundland and Labrador [9]. Passerine migrants play a key role in the wide dispersal of I. scapularis larvae and nymphs especially during northward spring migration [8,9,10,11,12,13,14]. In eastern and central Canada, songbird-transported I. scapularis ticks may be infected with a plethora of tick-borne pathogens, especially Bbsl and Babesia odocoilei (Apicomplexa: Piroplasmida: Babesiidae). Of note, a triple co-infection of Bbsl, Babesia microti, and A. phagocytophilum has been documented in a blacklegged tick nymph parasitizing a Veery [15].
Recently, molecular and biomedical researchers revealed that human babesiosis caused by B. odocoilei is pathogenic [16]. Not only does this tick-borne zoonotic pathogen infect humans, this Babesia sp. infects a wide range of cervid and bovid hosts. The biographical distribution of B. odocoilei coincides with I. scapularis, which are indigenous east of the Rocky Mountains [17,18,19], and in far-western North America, the western blacklegged tick, Ixodes pacificus [20], is indigenous. Pertinent to I. scapularis ticks, B. odocoilei has transovarial transmission (female to eggs to larvae) [19,21] and, similarly, transstadial passage (larva to nymph or nymph to adult) [8,14,19,21]. The present epidemiological study, which is centered directly in the territorial heartland of I. scapularis and white-tailed deer, Odocoileus virginianus, was conducted in the Great Lakes basin [22,23,24].
The aim of this tick study was to (1) assess the geographic distribution of tick-borne pathogens in eastern Canada, (2) ascertain the presence of zoonotic pathogens in field-collected ticks, and (3) determine the prevalence of select pathogens in I. scapularis. This newfound study elucidates the first report of B. odocoilei in eastern Ontario and the Hepatozoon canis piroplasm in Canada.
2. Results
2.1. Tick Collection
A total of 113 I. scapularis ticks were collected from 69 vertebrate hosts (songbirds, mammals including humans) and by flagging (Table 1, Figure 1). These collections comprised of 23 songbirds (n = 29 ticks), 46 mammals (n = 59 ticks), and flagging (n = 25 ticks) (Table 1). Two ticks collected from songbirds were lost during field operations, and 111 ticks were tested for tick-borne zoonotic pathogens.
Table 1.
Detection of tick-borne pathogens in Ixodes scapularis ticks collected from vertebrates and by flagging, Ontario and Quebec, 2020.
| Source | No. of Hosts | No. Ticks Collected | Ixodes scapularis | Ticks Tested | Pathogens | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| L | N | M | F | Bbsl | Bab | Aph | Hcn | ||||
| Songbirds | |||||||||||
| Lincoln’s Sparrow, Melospiza lincolnii |
1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Indigo Bunting, Passerina cyanea |
1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| House Wren, Troglodytes aedon |
4 | 5 | 0 | 5 | 0 | 0 | 5 | 1 | 0 | 0 | 1 |
| Common Yellowthroat, Geothlypis trichas |
5 | 5 | 3 | 2 | 0 | 0 | 5 | 0 | 3 | 0 | 0 |
| Veery, Catharus fuscescens |
3 | 3 | 0 | 3 | 0 | 0 | 3 | 0 | 0 | 0 | 0 |
| Baltimore Oriole, Icterus galbula |
2 | 2 | 0 | 2 | 0 | 0 | 2 | 0 | 1 | 0 | 0 |
| American Robin, Turdus migratorius |
1 | 3 | 1 | 1 | 0 | 0 | 2 | 1 | 0 | 0 | 0 |
| Song Sparrow, Melospiza melodia |
2 | 4 | 0 | 3 | 0 | 0 | 3 | 1 | 1 | 0 | 0 |
| Black-capped Chickadee Poecile atricapillus |
1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Eastern Towhee, Pipilo erythrophthalmus |
1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 |
| Ovenbird, Seiurus aurocapilla |
1 | 2 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 |
| Northern Waterthrush, Parkesia noveboracensis |
1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 |
| Mammals | |||||||||||
| Dog, Canis familiaris |
32 | 39 | 0 | 0 | 4 | 35 | 39 | 5 | 3 | 0 | 0 |
| Cat, Felis catus |
9 | 11 | 0 | 0 | 2 | 9 | 11 | 1 | 3 | 1 | 0 |
| North American porcupine, Erethizon dorsatum |
1 | 5 | 0 | 0 | 0 | 5 | 5 | 3 | 1 | 0 | 0 |
| Human, Homo sapiens |
4 | 4 | 0 | 0 | 0 | 4 | 4 | 2 | 0 | 0 | 0 |
| Flagging | |||||||||||
| Vegetation | 0 | 25 | 0 | 0 | 8 | 17 | 25 | 14 | 5 | 0 | 0 |
| Total | 69 | 113 | 7 | 20 | 14 | 70 | 111 | 29 | 18 | 1 | 1 |
L, larva(e); N, nymph(s); M, male(s); F, female(s). Bbsl, Borrelia burgdorferi sensu lato; Bab, Babesia spp.; Aph, Anaplasma phagocytophilum; Hcn, Hepatozoon canis.
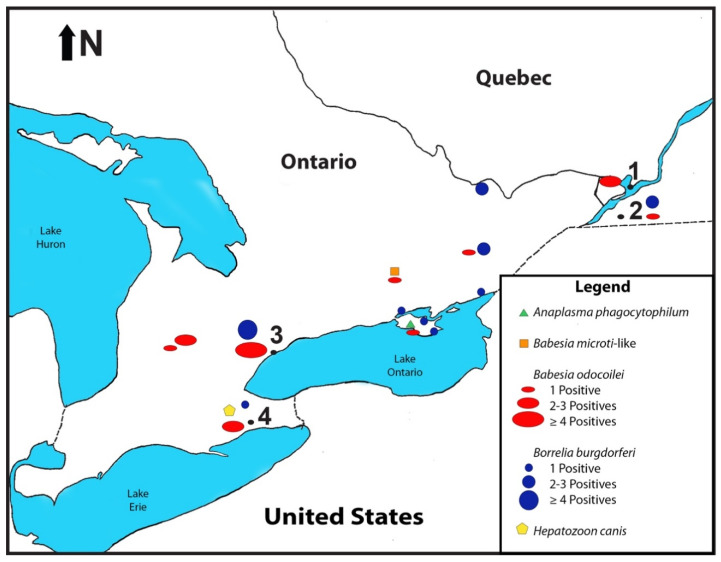
Figure 1.
Map showing core geographic locations of Ixodes scapularis collected. (1) McGill Bird Observatory, Ste-Anne-de-Bellevue, Quebec: 45.43 N, 73.94 W. (2) Montée Biggar, Quebec; 45.09 N, 74.22 W. (3) Rouge National Urban Park, Toronto, Ontario; 43.82 N, 79.17 W. (4) Ruthven Park National Historic Site Banding Station, Haldimand Bird Observatory, Cayuga, Ontario; 42.97 N, 79.87 W.
2.2. Pathogen Detection
Overall, PCR and DNA sequencing found pathogen targets in 49/111 (44.1%) of I. scapularis ticks tested. Based on the five microbial targets, 1/111 (0.9%) I. scapularis tested positive for A. phagocytophilium; 1/111 (0.9%) positive for B. microti-like sp.; 17/111 (15.3%) were positive for B. odocoilei; 29/111 (26.1%) positive for Bbsl; and 1/111 (0.9%) positive for H. canis (Table 2).
Table 2.
Dataset denoting representative apicomplexan microorganisms detected in Ixodes scapularis collected from vertebrates in Ontario and Quebec, 2020. L, larva(e); N, nymph(s); M, male(s); F, female(s).
| Geographic Location. | Source | Life Stage | Pathogen | GenBank Accession Number |
|---|---|---|---|---|
| Cayuga, ON | Common Yellowthroat | N | B. odocoilei | MZ841618 |
| Belwood, ON | Cat, domestic | F | B. odocoilei | MZ841619 |
| Montée Biggar, QC | Song Sparrow | N | B. odocoilei | OK041475 |
| Ste-Anne-de-Belleville, QC | Common Yellowthroat | L | B. odocoilei | MZ841620 |
| Toronto, ON | Vegetation | M | B. odocoilei | MZ841621 |
| Fergus, ON | Dog, domestic | F | B. odocoilei | MZ841622 |
| Westport, ON | Porcupine | F | B. odocoilei | MZ841623 |
| Bloomfield, ON | Dog, domestic | F | B. odocoilei | MZ841624 |
| Tweed, ON | Cat, domestic | F | B. microti-like | MZ841625 |
| Tweed, ON | Dog, domestic | F | B. odocoilei | OK041476 |
| Cayuga, ON | House Wren | N | H. canis | MZ841626 |
Fourteen (56%) of 25 I. scapularis adults collected by flagging were positive for Bbsl. Five (20%) of these 25 I. scapularis adults were infected with B. odocoilei. Four of these females were co-infected with Bbsl and B. odocoilei. All ticks in this study were negative for B. microti.
Of special enzootic note, a fully engorged I. scapularis nymph was collected from a House Wren on 19 May 2020 at Ruthven Park, Cayuga, Ontario. The nymph underwent transstadial passage, and molted to a male in 42 days (Table 1). By using PCR testing, DNA sequencing, and Basic Local Alignment Search Tool (BLAST) analysis, Hepatozoon canis was detected. This detection is the first report of H. canis in an I. scapularis tick, and constitutes the first detection of H. canis in Canada.
An engorged I. scapularis female was collected from a cat in Picton, Ontario, on 16 October 2020, and this partially fed female tested positive for A. phagocytophilum. This is the first detection in Canada of A. phagocytophilum-infected I. scapularis tick parasitizing a domestic cat.
Five I. scapularis females were collected from a North American porcupine, Erethizon dorsatum, hit by a moving vehicle at Westboro, Ontario, on 17 October 2020. Three females were infected with Bbsl, and one female was infected with B. odocoilei. One of these females was co-infected with Bbsl and B. odocoilei.
Six (30%) of 20 I. scapularis nymphs collected from passerine birds were positive for B. odocoilei.
3. Discussion
Our findings reveal a quaint observation about the incidence of tick-borne pathogens in eastern Canada. Based on our results, babesial infections are more common on songbird-transported I. scapularis ticks than the Lyme disease bacterium. Although emergency departments and medical clinics are targeting tick bites with short-term antibiotic treatments for Lyme disease, they are missing the fact that anti-Babesia therapy may be required. Other tick-borne pathogens, such A. phagocytophilum and H. canis, are also entering the pathogenic picture.
3.1. Pathogen-Positive I. scapularis
When we consider all mobile life stages (larvae, nymphs, adults) of 111 I. scapularis ticks tested, we obtained pathogen-positive ticks comprising Bbsl, 29 (26.1%); B. odocoilei, 17 (15.3%); B. microti-like sp., 1 (0.9%); A. phagocytophilum, 1 (0.9%); and H. canis, 1 (0.9%). Tick researchers in the Great Lakes basin have likewise detected Bbsl, Babesia spp., and A. phagocytophilum in I. scapularis ticks [22,23,24]. Within the the same basin, a research team found an infection prevalence of 71% for B. odocoilei detected in I. scapularis females collected from cats and dogs in west-central Ontario [25]. Even though the Bbsl infection prevalence for I. scapularis was lower than B. odocoilei for songbird-derived ticks (Figure 2), we found that it was highest overall for I. scapularis parasitizing avifauna(Table 1). Notably, five (4.5%) of 111 I. scapularis adults in this study were co-infected with Bbsl and B. odocoilei. Whenever people are bitten by a I. scapularis tick, clinicians must realize that patients may require a combination of antimicrobials to match the pathogen load.
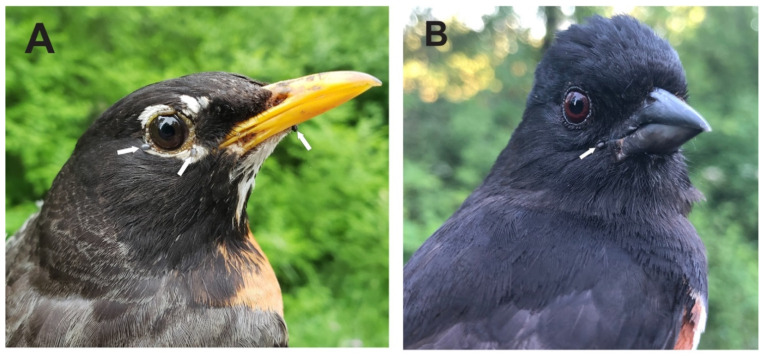
Figure 2.
Ground-frequenting songbirds parasitized by Borrelia burgdorferi sensu lato-positive larval and nymphal blacklegged ticks: (A) American Robin, adult breeding male, and (B) Eastern Towhee, second year male. These songbird-derived ticks were collected during the nesting season. Photo credits: Ana Morales.
3.2. Distribution of B. odocoilei
Both I. scapularis ticks and white-tailed deer have a wide distribution east of the Rocky Mountains, and play a key role in the enzootic transmission cycle for B. odocoilei. Continent-wide, B. odocoilei has been documented in several provinces and states including Texas [19,26], California [20], Oklahoma [26], Virginia [27], Pennsylvania [13,24,27,28], New York state [29], Michigan [22], Wisconsin [23], Indiana [23], Maine [30], Ontario [8,25], Quebec [8], and Saskatchewan [31]. Consistent with these research findings, we also located a new population of I. scapularis ticks in a western suburb of Montreal, Quebec.
3.3. Comparative Relationship between Babesia Spp.
Many people in the medical field contend that B. duncani and B. microti are unequivocally the main cause of human babesiosis in North America [32,33]. However, neither B. duncani nor B. microti were detected during the present study. Instead, B. odocoilei was the focal Babesia species. Of medical significance, B. odocoilei causes human babesiosis and is pathogenic to humans [16]. Throughout the present study, there was only one B. microti-like piroplasm; it was detected in an I. scapularis female removed from a cat. In the Great Lakes basin, white-tailed deer are the reservoir of B. odocoilei, and I. scapularis is the vector [25]. Both are indigenous throughout the Great Lakes region, and perpetuate an enzootic transmission cycle of B. odocoilei.
3.4. Source of B. odocoilei-Infected Ticks
The source of I. scapularis parasitizing songbirds varies depending on the time of year. Throughout the temperate months, 50% of the B. odocoilei-infected I. scapularis were collected during northward spring migration, whereas 17% were obtained during the nesting and fledgling period at Montée Biggar, Quebec, in juxtaposition to the nesting spot (Figure 3). Of significance, 33% of the B. odocoilei-infected I. scapularis were attained during fall migration. Ticks acquired during nesting will account for the locally acquired ticks [34], whereas infestations on neotropical passerines, which are heading to the boreal forest to breed and rear their young [13], will represent a large portion of the ticks occurring from long-distant dispersal.
Figure 3.
Song Sparrow, hatch year, parasitized by two Ixodes scapularis nymphs of which one was positive for Babesia odocoilei. These ticks were collected during the nesting period. Photo credits: Ana Morales.
3.5. Pathways of B. odocoilei
The origin of B. odocoilei detected in the I. scapularis larva, which was collected from a Common Yellowthroat, is uncertain. The larva may have become infected via transovarial transmission or, alternatively, from the host bird. To date, there is no conclusive evidence to show that songbirds are reservoir-competent hosts of B. odocoilei.
It is noteworthy that transovarial transmission of B. odocoilei has been documented in I. scapularis [19,21,26]. Because the I. scapularis larva, which was collected from the Common Yellowthroat, successfully molted to a nymph in 29 days, we affirm that transstadial passage of B. odocoilei occurs in I. scapularis. Transstadial passage of B. odocoilei in collections in 2018 and 2019 from larva to nymph [8,14,34], and also from nymph to adult, revealed transstadial passage [8,14,34]. Since transovarial transmission and transstadial passage occur in I. scapularis [19,26], these pathways provide a continuous cycle of B. odocoilei infection. Notably, southeast Texas (the original site of B. odocoilei study) and southwest Quebec are 15 latitudes apart.
Tick researchers recently reported the coexistence of Bbsl and B. odocoilei in an I. scapularis nymph collected in 2018 from a Veery in Canada [13]. In the present study, co-infection of Bbsl and B. odocoilei has also been documented in I. scapularis collected from avian and mammalian hosts and, likewise, by flagging.
3.6. Phylogeny of B. microti-Like Piroplasm
The phylogeny of a B. microti-like piroplasm detected in an I. scapularis female is currently an undescribed species. Based on BLAST analysis, supported with 99% coverage, the Babesia variant has a sequence divergence of 95.7% relative to the type strain of B. microti. The host cat may have been infected with this variant at the time of tick bite and passed the infection during the blood meal. Alternatively, because the I. scapularis female had imbibed two previous blood meals prior to the blood meal from a suitable host, this tick may have become infected during the larval-nymphal blood meal or the nymphal-adult blood meal. This Babesia sp. variant could be a newly discovered species that is yet to be identified. All the other babesial infections in this pathogen study were B. odocoilei. Of note, B. microti was not detected in any of the I. scapularis ticks collected during this study.
3.7. Ixodes scapularis Parasitize Mammalian Hosts
In the present study, a North American porcupine was infested with five I. scapularis ticks. Three of these females were infected with Bbsl, and one of these partially engorged females was infected with B. odocoilei. Previously, B. odocoilei was detected in I. scapularis adults collected from canids and felids in the Huronia area of southern Ontario [25] and, in this sylvan environment, this tick species exhibited a significantly higher prevalence (71%) of B. odocoilei [25]. This infestation signifies the first documentation of a mammalian parasitism in Canada where the I. scapularis was co-infected with Bbsl and B. odocoilei. North American porcupines are denizens of arboreal habitats, and help to propel the enzootic transmission cycle of Bbsl and B. odocoilei. Whenever patients are bitten by I. scapularis ticks, each one needs to be tested for tick-borne pathogens, especially Bbsl and B. odocoilei. For efficacious treatment, an anti-babesial regimen should be considered for this type of polymicrobial infection.
3.8. Novel Discovery of H. canis in Canada
The detection of H. canis in a tick in Canada is a newfound discovery. Moreover, this is the first time that H. canis has been detected in an I. scapularis tick. Neotropical songbirds transport ticks into Canada from as far south as the northern part of South America [8,9,10,11,12,13,14], and would most likely acquire this H. canis-infected nymph in neotropical regions or the southern United States. House Wrens, Troglodytes aedon, have southern breeding grounds in Central America and South America, as far south as Argentina, and commonly have hemisphere-spanning migration. The House Wren likely made a migratory stopover in the southern United States, and transported the H. canis-infected I. scapularis nymph firsthand via cross-border flight to Ontario. By allowing this fully engorged nymph to molt to an adult (male), we were able to show that H. canis successfully undergoes transstadial passage. Therefore, this alveolate can successfully pass from larva to nymph and, likewise, from nymph to adult.
More than 300 species of Hepatozoon, which belong to the family Hepatozoidae, are known to infect animals [35]. Hepatozoon canis is typically found in the brown dog tick, Rhipicephalus sanguineus, which has wide distribution, including southern Europe, Africa, and Asia.
Members of the genus Hepatozoon are well known in veterinary circles for causing tick-borne diseases, namely hepatozoonosis in certain mammals. Hepatozoon canis, a one-celled, intraerythrocytic parasite infects members of the family Canidae (e.g., dog, coyotes, and foxes) [35]. Biogeographically, H. canis has been reported in several states across the southern United States [36]. It is noteworthy that H. canis is epizootic in dogs, and clinical manifestations include lethargy, fever, weight loss, decreased appetite, muscle pain/weakness, reluctance to move, and discharge from eyes and nose and, in severe cases, it can cause death [36].
In the United States, American canine hepatozoonosis is also caused by Hepatozoon americanum, and is delineated from H. canis by molecular identification. When dogs are bitten by or ingest Gulf Coast ticks, Amblyomma maculatum, which is the source of infective oocysts of H. americanum, the host canid normally becomes infected [35].
3.9. American Robins Are Competent Reservoirs of B. burgdorferi Sensu Lato
In the present study, two I. scapularis larvae and one I. scapularis nymph were collected from an American Robin, and a single larva molted to a nymph in 27 d; it was positive for Bbsl (Figure 1). This event shows transstadial passage of Bbsl in I. scapularis. Both Bbsl and B. odocoilei are maintained in the tick midgut during the molt [37], and both of these pathogenic microorganisms successfully retain their viability to pursue host-seeking activities.
Since the larva had not had a previous blood meal prior to feeding on the American Robin, we re-iterate the fact that American Robins are reservoir-competent hosts. Using spirochete-free, xenodiagnostic larvae, researchers reported that the American Robin is a reservoir host of Bbsl [38]. Because transovarial transmission of Bbsl is not present in I. scapularis, we confirm that the American Robin is a reservoir-competent host of Bbsl.
3.10. Human Babesiosis as a Tick-Borne Zoonosis
Human babesiosis has received considerable attention as a tick-borne zoonosis worldwide. Historically, this single-celled intraerythrocytic piroplasmid was initially discovered in 1888 by Victor Babes, a Romanian pathologist [39]. Five years later, American researchers found that ticks are the primary vector that transmit Babesia spp. to terrestrial vertebrate [40]. The first documentation of a human case of babesiosis was described in a splenectomized Croatian cattle farmer in 1956 [41], and the red blood cell parasite was later named Babesia divergens. Clinical manifestations relating to human babesiosis vary from asymptomatic to life-threatening. Symptoms are wide-ranging, including profound fatigue, flushing, sweats (especially night sweats), chills, muscle aches, increased thirst, headaches, sleep disturbance, fever, and anxiety.
Human babesiosis caused by B. odocoilei is a recalcitrant infection [16]. Human subjects often have low parasitemia [16] but are symptomatic. When B. odocoilei-infected red blood cells adhere to fibrin, which line the endothelial cells of capillaries and venules, cytoadherence (binding to endothelial cells) and sequestration result. This fibrin-bonding mechanism is similar to the sequestration discerned with B. canis in dogs [42]. Cytoadherence and sequestration develop as the microvasculature of capillaries and venules fill up with infected erythrocytes. Longstanding infections of B. odocoilei can induce clinical symptoms involving ischemia, profound fatigue, severe hemolysis, thrombocytopenia, dysautonomia, hemodynamic instability, sustained inflammation, and multi-organ dysfunction and, eventually, may lead to death [32,33,43]. A fibrin-dissolving enzyme, such as lumbrokinase, is required to slowly loosen the infected piroplasmids. The procedure is a gradual, long-term anti-babesial therapy. Based on fibrin-bonding sequestration, B. odocoilei ranks as the most pronounced chronic human babesiosis in North America.
A wide diversity of Babesia species that cause human babesiosis globally include B. crassa, B. divergens, B. duncani (WA1), B. microti, B. odocoilei, B. venatorum, Babesia sp. variants CA1, CA3, and CA4, Babesia sp. CN1, Babesia divergens-like MO1, and Babesia sp. TW1 [16,44,45,46,47,48,49,50,51,52].
Not only are babesial piroplasmids transmitted by ticks, they are transmitted by blood transfusion [53], organ transplantation [54], and maternal–fetal transmission [55,56,57,58]. Similarly, Lyme disease spirochetes can be transmitted by maternal–fetal transmission [59,60,61,62,63]. Throughout a person’s life, these two pathogens can be an insidious life-altering disease. In reality, co-infection of B. odocoilei and Bbsl can potentially occur in the neonate if a pregnant person is bitten by an I. scapularis tick that is coinfected with these two tick-borne, zoonotic microorganisms.
3.11. Endemic Area Not Required to Contract Tick-Borne Diseases
Even though people are bitten in endemic areas, our results show that people can be bitten anywhere that ticks drop from songbirds and mammals. Passerine migrants are directly involved in the wide dispersal of pathogen-positive I. scapularis ticks [8,9,10,11,12,13,14]. These epizootic and zoonotic pathogens can be carried hundreds of kilometers and dispersed across the landscape [8,9,10,11,12,13,14]. Based on our findings at Montée Biggar, Quebec (Table 1, Figure 1), we re-affirm that this nesting site is an endemic area for I. scapularis [34]. Both I. scapularis larvae and nymphs were collected from nesting songbirds, which constitutes an established population [34,64]. In addition, white-tailed deer are prominent in this locale, and support the reproduction and propagation of I. scapularis, especially adults. Outdoor people can be bitten whenever they venture into grassy and woodland areas. At the time of fall migration, songbirds fly southward from this nesting and fledgling site, and widely disperse larval and nymphal I. scapularis while en route to their southern breeding grounds. Since songbirds widely disperse songbird-transported ticks during bi-directional flight, people do not have to reside in an endemic area to acquire tick-borne zoonotic diseases.
In 2020, six (86%) of seven songbird-transported I. scapularis, which were held to molt, successfully developed to the next developmental life stage. These ecological findings help to substantiate that an established population of I. scapularis is located at Ste-Anne-de-Bellevue, Quebec. This western Montréal suburb at the junction of the Ottawa River and the St. Lawrence River fulfil the criteria (two life stages in a collection period) for an established population of I. scapularis ticks [34,64]. Based on these tick collections, this campus woods represents an established population of I. scapularis [34,64] and, additionally, has an enzootic transmission cycle for both Bbsl and B. odocoilei.
3.12. Diversity of Pathogens in I. scapularis
When bitten by a questing I. scapularis tick, people can contract any one of at least nine different tick-borne zoonotic pathogens [7,16,25]. We detected Bbsl (the causal organism of Lyme disease) and B. odocoilei (the causal organism of human babesiosis) in both larval and nymphal I. scapularis.
When it comes to tick bites, the present mindset focuses on Lyme disease. In the present study, 16.2% of the I. scapularis ticks tested were infected with Babesia spp. Since Babesia spp. require a different treatment protocol than other pathogenic microorganisms, healthcare providers need to be aware that people bitten by an I. scapularis tick may be infected with B. odocoilei. Medically, B. odocoilei causes human babesiosis and is pathogenic to humans [16]. Since cross-reactivity is an ongoing issue with Babesia spp., other modes of testing, such as molecular identification (e.g., PCR, DNA sequencing), are needed to firmly delineate Babesia species [65]. When it comes to I. scapularis tick bites, clinicians must consider a wide spectrum of pathogens and include them in the differential diagnosis. Consideration of Babesia piroplasmids is vitally important in administering an efficacious approach to treatment.
4. Materials and Methods
4.1. Tick Collection
Ticks were collected from songbirds by bird banders using super-fine point stainless steel forceps. These ticks were put into 8.5 mL, polypropylene, round-bottom tubes, 75 × 15 mm containing a slightly moistened paper towel. After inserting ticks, the mouth of the tube was covered with a piece of tulle netting, and a push-cap with a 7 mm hole was placed into the mouth of the tube to prevent live ticks from escaping. The collection tube was put into a self-sealing plastic bag with a slightly moistened paper towel. An attached label for the background information of each bird was completed. Live ticks were sent directly to the lab (J.D.S.) for identification. Partially and fully engorged larvae and nymphs were held to molt to the next developmental life stage using a photoperiod of 16:8 h (Light: Dark) with ambient temperature and 90–95% humidity. As the daylength shortened, a 12W, full-spectrum LED daylight bulb (LifeEnergy Systems, Canada) was used, and plugged into an electrical timer. Complete tick records (i.e., geographic location, collecting date, tick species, developmental life stage, and bird species) were logged for each tick collection.
Ticks from humans were self-collected, put in a tightly sealed vial containing 99% isopropyl alcohol, and promptly submitted to the laboratory (J.D.S.) for identification. These vials were then sent to the laboratory (R.R.P.) by courier for pathogen testing.
Ticks parasitizing mammals were collected by veterinarians and veterinarian technicians using fine-pointed stainless steel forceps, and then placed directly in 2 mL micro tubes containing 94% ethyl alcohol. At the end of the collection period for I. scapularis adults, all ticks were sent to the lab (J.D.S.) for identification. All collected ticks were identified morphologically to species, life stage, and gender (if adult) by using a stereoscopic microscope and taxonomic keys [66,67,68].
A flannel-back vinyl cloth measuring 59 cm × 71 cm attached to an aluminum telescopic window washer’s pole, 197 cm in length, was used to flag for questing I. scapularis adults. Flannel-back vinyl cloth was used because it does not blow around in the wind. In addition, it withstands thorny stems of brambles, a cane-like, prickly shrub. When low-lying vegetation is dry to the touch, flagging is conducted between 1000 hrs. and 1600 hrs. during cloudy or partly cloudy days. Flagging was done in grassy areas and, similarly, along trails and pathways.
4.2. Pathogen Detection
Ethanol storage medium was allowed to evaporate before proceeding with tick DNA extraction. Clean razor blades were used to bisect each tick (anteriorly to posteriorly through the capitulum) to isolate a 5–10 mg fragment [69]. DNA was extracted using the Purelink Genomic DNA Mini Kit (Invitrogen, Waltham, MA, USA), following manufacturer’s instructions, and eluted in 80 µL Genomic Elution Buffer. The quantity and quality of DNA was assessed using the Nanodrop One spectrophotometer (Thermo Scientific, Waltham, MA, USA).
Real-time PCR amplification was performed in duplicate aliquots using 2 µL of extracted DNA in a 20 µL reaction of Taqman Fast Advanced Master Mix (Applied Biosystems, Waltham, MA, USA). As well, the published primers and probes for the 16S gene of Bbsl [70] and msp2 gene of A. phagocytophilum [71] were employed. The B. burgdorferi s.l. probe specifically excluded Borrelia miyamotoi [70]. A sample was considered positive when the cycle threshold (CT) was less than 40 with a characteristic curve. Conventional PCR amplification for the 18S gene of Babesia spp. was performed in duplicate and visualized on a 1% gel using methods and reagents as previously described [8]. Samples were considered positive when amplicons of 400–500 base pairs (bp) were observed. All PCR reactions included molecular-grade water and, also, synthetic gBlock gene fragments (Integrated DNA Technologies, Coralville, IA, USA) of B. burgdorferi (MH781147.1), A. phagocytophilum (AY151054.1), and B. microti (MT974173.1) as controls. When tick species was uncertain, based on morphology alone, the 16S and 12S genes were amplified using 2 µL of extracted DNA in a 25 µL conventional PCR reaction of GoTaqGreen Master Mix (Promega, Madison, WI, USA) with earlier established primers [72,73], followed by sequencing.
PCR products were prepared for sequencing using either ExoSAP-IT (Applied Biosystems) or PureLink Quick Gel Extraction Kit (Invitrogen, Waltham, MA, USA). All sequencing was performed at the Genomics Shared Resource laboratory at the Comprehensive Cancer Center within the Ohio State University using forward and reverse primers. Manual edits and alignments were performed in the program CLC Main Workbench v.21.0.3 (www.qiagenbioinformatics.com/, accessed on 27 August 2021) followed by BLAST in GenBank (NCBI; http://blast.ncbi.nlm.nih.gov/Blast.cgi, accessed on 27 August 2021).
5. Conclusions
In this tick-host-pathogen study, we crossed a new threshold with the novel discovery of H. canis in Canada. Moreover, we have disclosed the premiere detection of H. canis in an I. scapularis tick. Since this I. scapularis nymph was collected during peak spring migration, this bird parasitism by a neotropical songbird documents cross-border flight into Canada. We provide the first authentic documentation of an I. scapularis tick infected with A. phagocytophilum parasitizing a feline host in Canada. Based on DNA sequencing and BLAST analysis, we document the first B. microti-like pathogen in Canada and, upon further multi-locus analysis, could potentially be a new Babesia sp. Overall, 15.3% of I. scapularis were infected with B. odocoilei in eastern Canada, and similarly, 30% of the songbird-transported I. scapularis nymphs were positive for B. odocoilei. Each of these babesial infection groupings present a significant health risk. Because migratory songbirds widely disperse I. scapularis ticks, people do not have to frequent an endemic area to contract tick-borne zoonoses. When treating I. scapularis tick bites, clinicians at medical clinics and emergency departments need to be aware that there is a subtle difference between antimicrobial therapies for B. odocoilei and Bbsl.
Acknowledgments
We thank bird banders, wildlife rehabilitators, veterinarians, and veterinary technicians for collecting ticks. We are grateful to Amanda Green for computer graphics.
Author Contributions
Conceptualization, J.D.S.; methodology, J.D.S. and R.R.P.; software, R.R.P.; validation, J.D.S. and R.R.P.; formal analysis, J.D.S. and R.R.P.; investigation, J.D.S. and R.R.P.; resources, J.D.S. and R.R.P.; data curation, J.D.S. and R.R.P.; writing—original draft preparation, J.D.S. and R.R.P.; writing—review and editing, J.D.S. and R.R.P.; supervision, R.R.P.; project administration, J.D.S. and R.R.P.; funding acquisition, J.D.S. and R.R.P. All authors have read and agreed to the published version of the manuscript.
Funding
Funding for this tick-borne zoonotic study was provided in part by the Mary Alice Holmes Memorial Foundation and, likewise, by a philanthropic donor Diane Kindree. We are most grateful to Lyme Ontario for helping to fund this project. Research reported in this publication was supported through Shared Resources of The Ohio State University Comprehensive Cancer Center and the National Institutes of Health under grant number P30 CAO16058.
Data Availability Statement
All data are reported in the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Magnarelli L.A., Dumler J.S., Anderson J.F., Johnson R.C., Fikrig E. Coexistence of antibodies to tick-borne pathogens of babesiosis, ehrlichiosis, and Lyme borreliosis in human sera. J. Clin. Microbiol. 1995;33:3054–3057. doi: 10.1128/jcm.33.11.3054-3057.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mitchell P.D., Reed K.D., Hofkes J.M. Immunoserologic evidence of coinfection with Borrelia burgdorferi, Babesia microti, and human granulocytic Ehrlichia species in residents of Wisconsin and Minnesota. J. Clin. Microbiol. 1996;34:724–727. doi: 10.1128/jcm.34.3.724-727.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stricker R.B. Lyme disease: A potential polymicrobial infection. ASM News. 2003;69:265. [Google Scholar]
- 4.Benach J.L., Coleman J.L., Habicht G.S., MacDonald A., Grunwaldt E., Giron J.A. Serological evidence for simultaneous occurrences of Lyme disease and babesiosis. J. Infect. Dis. 1985;152:473–477. doi: 10.1093/infdis/152.3.473. [DOI] [PubMed] [Google Scholar]
- 5.Anderson J.F., Mintz E.D., Gadbaw J.J., Magnarelli L.A. Babesia microti, human babesiosis, and Borrelia burgdorferi in Connecticut. J. Clin. Microbiol. 1991;29:2779–2783. doi: 10.1128/jcm.29.12.2779-2783.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanchez-Vicente S., Tagliafierro T., Coleman J.L., Benach J.L., Tokarz R. Polymicrobial nature of tick-borne diseases. mBio. 2019;10:e02055-19. doi: 10.1128/mBio.02055-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nicholson W.A., Sonenshine D.E., Noden B.H. Ticks (Ixodida) In: Mullen G.R., Durden L.A., editors. Medical and Veterinary Entomology. 3rd ed. Academic Press; London, UK: 2019. pp. 603–672. [Google Scholar]
- 8.Scott J.D., Pascoe E.L., Sajid M.S., Foley J.E. Detection of Babesia odocoilei in Ixodes scapularis ticks collected from songbirds in Ontario and Quebec, Canada. Pathogens. 2020;9:781. doi: 10.3390/pathogens9100781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scott J.D., Clark K.L., Foley J.E., Bierman B.C., Durden L.A. Far-reaching dispersal of Borrelia burgdorferi sensu lato-infected blacklegged ticks by migratory songbirds in Canada. Healthcare. 2018;6:89. doi: 10.3390/healthcare6030089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morshed M.G., Scott J.D., Fernando K., Beati L., Mazerolle D.F., Geddes G., Durden L.A. Migratory songbirds disperse ticks across Canada, and first isolation of the Lyme disease spirochete, Borrelia burgdorferi, from the avian tick, Ixodes auritulus. J. Parasitol. 2005;91:780–790. doi: 10.1645/GE-3437.1. [DOI] [PubMed] [Google Scholar]
- 11.Scott J.D., Clark K.L., Foley J.E., Anderson J.F., Bierman B.C., Durden L.A. Extensive distribution of the Lyme disease bacterium, Borrelia burgdorferi sensu lato, in multiple tick species parasitizing avian and mammalian hosts across Canada. Healthcare. 2018;6:131. doi: 10.3390/healthcare6040131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reed K.D., Meece J.K., Henkel J.S., Shukla S.K. Birds, migration and emerging zoonoses: West Nile virus, Lyme disease, Influenza A and enteropathogens. Clin. Med. Res. 2002;1:5–12. doi: 10.3121/cmr.1.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scott J.D., Clark K.L., Coble N.M., Ballantyne T.R. Presence of Babesia odocoilei and Borrelia burgdorferi sensu stricto in a tick and dual parasitism of Amblyomma inornatum and Ixodes scapularis on a bird in Canada. Healthcare. 2019;7:46. doi: 10.3390/healthcare7010046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scott J.D., Clark K.L., Coble N.M., Ballantyne T.R. Detection and transstadial passage of Babesia species and Borrelia burgdorferi sensu lato in ticks collected from avian and mammalian hosts in Canada. Healthcare. 2019;7:155. doi: 10.3390/healthcare7040155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hersh M.H., Ostfeld R.S., McHenry D.J., Tibbetts M., Brunner J.L., Killilea M.E., LoGiudice K., Schmidt K.A., Kessing F. Co-infection of blacklegged ticks with Babesia microti and Borrelia burgdorferi is higher than expected and acquired from small mammal hosts. PLoS ONE. 2014;9:e99348. doi: 10.1371/journal.pone.0099348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scott J.D., Sajid M.S., Pascoe E.L., Foley J.E. Detection of Babesia odocoilei in humans with babesiosis symptoms. Diagnostics. 2021;11:947. doi: 10.3390/diagnostics11060947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Emerson H.R., Wright W.T. The isolation of a Babesia in white-tailed deer. Bull. Wildl. Dis. Assoc. 1968;4:142–143. doi: 10.7589/0090-3558-4.4.142. [DOI] [PubMed] [Google Scholar]
- 18.Emerson H.R., Wright W.T. Correction. J. Wildl. Dis. 1970;6:519. doi: 10.2307/495851. [DOI] [Google Scholar]
- 19.Holman P.J., Madeley J., Craig T.M., Allsopp B.A., Allsopp M.T., Petrini K.R., Waghela S.D., Wagner G.G. Antigenic, phenotypic and molecular characterization confirms Babesia odocoilei isolated from three cervids. J. Wildl. Dis. 2000;36:518–530. doi: 10.7589/0090-3558-36.3.518. [DOI] [PubMed] [Google Scholar]
- 20.Eshoo M.W., Carolan H.E., Massire C., Chou D.M., Crowder C.D., Rounds M.A., Phillipson C.A., Schutzer S.E., Ecker D.J. Survey of Ixodes pacificus ticks in California reveals a diversity of microorganisms and a novel and widespread Anaplasmataceae species. PLoS ONE. 2015;10:e0135828. doi: 10.1371/journal.pone.0135828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waldrup K.A., Kocan A.A., Barker R.W., Wagner G.G. Transmission of Babesia odocoilei in white-tailed deer (Odocoileus virginianus) by Ixodes scapularis (Acari: Ixodidae) J. Wildl. Dis. 1990;26:390–391. doi: 10.7589/0090-3558-26.3.390. [DOI] [PubMed] [Google Scholar]
- 22.Hamer S.A., Roy P.L., Hickling G.J., Walker E.D., Foster E.S. Zoonotic pathogens in Ixodes scapularis, Michigan. Emerg. Infect. Dis. 2007;13:1131–1133. doi: 10.3201/eid1307.070046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steiner F.E., Pinger R.R., Vann C.N., Grindle N., Civitello D., Clay K., Fuqua C. Infection and co-infection rates of Anaplasma phagocytophilum variants, Babesia spp., Borrelia burgdorferi, and the rickettsial endosymbiont in Ixodes scapularis (Acari: Ixodidae) from sites in Indiana, Maine, Pennsylvania, and Wisconsin. J. Med. Entomol. 2008;45:289–297. doi: 10.1093/jmedent/45.2.289. [DOI] [PubMed] [Google Scholar]
- 24.Livengood J., Hutchinson M.L., Thirumalapura N., Tewari D. Detection of Babesia, Borrelia, Anaplasma, and Rickettsia spp. in adult black-legged ticks (Ixodes scapularis) from Pennsylvania, United States, with Luminex Multiplex Bead Assay. Vector Borne Zoonotic Dis. 2020;20:406–411. doi: 10.1089/vbz.2019.2551. [DOI] [PubMed] [Google Scholar]
- 25.Scott J.D., Pascoe E.L., Sajid M.S., Foley J.E. Detection of Babesia odocoilei in Ixodes scapularis ticks collected in southern Ontario, Canada. Pathogens. 2021;10:327. doi: 10.3390/pathogens10030327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Waldrup K.A., Kocan A.A., Qureshi T., Davis D.S., Baggett D., Wagner G.G. Serological prevalence and isolation of Babesia odocoilei among white-tailed deer (Odocoileus virginianus) in Texas and Oklahoma. J. Wildl. Dis. 1989;25:194–201. doi: 10.7589/0090-3558-25.2.194. [DOI] [PubMed] [Google Scholar]
- 27.Perry B.D., Nichols D.K., Cullom E.S. Babesia odocoilei Emerson and Wright, 1970 in white-tailed deer, Odocoileus virginianus (Zimmermann), in Virginia. J. Wildl. Dis. 1985;21:149–152. doi: 10.7589/0090-3558-21.2.149. [DOI] [PubMed] [Google Scholar]
- 28.Shock B.C., Moncayo A., Cohen S., Mitchell E.A., Williamson P.C., Lopez G., Garrison L.E., Yabsley M.J. Diversity of piroplasms detected in blood-fed and questing ticks from several states in the United States. Ticks Tick Borne Dis. 2014;5:373–380. doi: 10.1016/j.ttbdis.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 29.Schoelkopf L., Hutchinson C.E., Bendele K.G., Goff W.L., Willette M., Rasmussen J.M., Holman P.J. New ruminant hosts and wider geographic range identified for Babesia odocoilei (Emerson and Wright 1970) J. Wildl. Dis. 2005;41:683–690. doi: 10.7589/0090-3558-41.4.683. [DOI] [PubMed] [Google Scholar]
- 30.Smith R.P., Jr., Elias S.P., Borelli T.J., Missaghi B., York B.J., Kessler R.A., Lubelczyk C.B., Lacombe E.H., Hayes C.M., Coulter M.S., et al. Human babesiosis, Maine, USA, 1995–2011. Emerg. Infect. Dis. 2014;20:1727–1730. doi: 10.3201/eid2010.130938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pattullo K.M., Wobeser G., Lockerbie B.P., Burgess H.J. Babesia odocoilei infection in a Saskatchewan elk (Cervus elaphus canadensis) herd. J. Vet. Diagn. Investig. 2013;25:535–540. doi: 10.1177/1040638713491746. [DOI] [PubMed] [Google Scholar]
- 32.Horowitz R.I. Why Can’t I Get Better? St. Martin’s Press; New York, NY, USA: 2013. Lyme and Other Co-infections: Parasitic, Viral, and Fungal Infectivity; pp. 134–162. [Google Scholar]
- 33.Kinderlehrer D.A. Recovery from Lyme disease: The Integrative Medicine Guide to Diagnosing and Treating Tick-Bore Illness. Skyhorse Publishing; New York, NY, USA: 2021. Babesia; pp. 93–101. [Google Scholar]
- 34.Scott J.D., Pascoe E.L., Sajid M.S., Foley J.E. Monitoring of nesting songbirds detects established population of blacklegged ticks and associated Lyme disease endemic area in Canada. Healthcare. 2020;8:59. doi: 10.3390/healthcare8010059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baneth G., Mathew J.S., Shkap V., Macintire D.K., Barta J.R., Ewing S.A. Canine hepatozoonosis: Two disease syndromes caused by separate Hepatozoon spp. Trends Parasitol. 2003;19:27–31. doi: 10.1016/S1471-4922(02)00016-8. [DOI] [PubMed] [Google Scholar]
- 36.Macintire D.K., Vincent-Johnson N., Dillon A.R., Blagburn B., Lindsay D., Whitley E.M., Banfield C. Hepatozoonosis in dogs: 22 cases (1989–1994) J. Am. Vet. Med. Assoc. 1997;210:916–922. [PubMed] [Google Scholar]
- 37.Kaufman R.W. Integument and ecdysis. In: Sonenshine E.E., Roe R.M., editors. Biology of Ticks. 2nd ed. Volume 1. Oxford University Press; Oxford, UK: 2013. pp. 99–196. [Google Scholar]
- 38.Richter D., Spielman A., Momar N., Matuschka F.-R. Competence of American Robins as reservoir hosts for Lyme disease spirochetes. Emerg. Infect. Dis. 2000;6:133–138. doi: 10.3201/eid0602.000205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Babes V. Sur l’hémoglobinurie bactérienne du boeuf. C. R. Acad. Sci. 1888;107:692–694. [Google Scholar]
- 40.Smith T., Kilborne F.L. Investigation into the Nature, Causation, and Prevention of Southern Cattle Fever. 1st ed. United States Government Printing Office; Washington, DC, USA: 1983. pp. 85–116. [Google Scholar]
- 41.Škrabalo Z., Deanović Z. Piroplasmosis in man: Report on a case. Doc. Med. Geogr. Trop. 1957;9:11–16. [PubMed] [Google Scholar]
- 42.Schetters T. Mechanisms involved in the persistence of Babesia canis infection in dogs. Pathogens. 2019;8:94. doi: 10.3390/pathogens8030094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gray J., Zintl A., Hildebrandt A., Hunfeld K.-P., Weiss L. Zoonotic babesiosis: Overview of the disease and novel aspects of pathogen identity. Ticks Tick Borne Dis. 2010;1:3–10. doi: 10.1016/j.ttbdis.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 44.Scholtens R.G., Braff E.H., Healy R.R., Gleason N. A case of babesiosis in man in the United States. Am. J. Trop. Med. Hyg. 1968;17:810–813. doi: 10.4269/ajtmh.1968.17.810. [DOI] [PubMed] [Google Scholar]
- 45.Western K.A., Benson G.D., Gleason N.N., Healy G.R., Schultz M.G. Babesiosis in a Massachusetts resident. N. Engl. J. Med. 1970;283:854–856. doi: 10.1056/NEJM197010152831607. [DOI] [PubMed] [Google Scholar]
- 46.Herwaldt B.L., Caccio S., Gherlinzoni F., Aspöck H., Siemenda S.B., Piccaluga P., Martinelli G., Edelhofer R., Hollenstain U., Poletti G., et al. Molecular characterization of a non-Babesia divergens organism causing zoonotic babesiosis in Europe. Emerg. Infect. Dis. 2003;9:942–948. doi: 10.3201/eid0908.020748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shih C.M., Liu L.P., Chung W.C., Ong S.J., Wang C.C. Human babesiosis in Taiwan: Asymptomatic infection with a Babesia microti-like organism in Taiwanese woman. J. Clin. Microbiol. 1997;35:450–454. doi: 10.1128/jcm.35.2.450-454.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kjemtrup A.M., Conrad P.A. Human babesiosis: An emerging tick-borne disease. Int. J. Parasitol. 2000;30:1323–1337. doi: 10.1016/S0020-7519(00)00137-5. [DOI] [PubMed] [Google Scholar]
- 49.Herwaldt B.L., Persing D.H., Precigout E.A., Goff W.L., Mathiesen D.A., Taylor P.W., Eberhard M.L., Gorenflot A.F. A fatal case of babesiosis in Missouri: Identification of another piroplasm that infects humans. Ann. Intern. Med. 1996;124:643–650. doi: 10.7326/0003-4819-124-7-199604010-00004. [DOI] [PubMed] [Google Scholar]
- 50.Ord R.L., Lobo C.A. Human babesiosis: Pathogens, prevalence, diagnosis, and treatment. Cur. Clin Microbiol. Rep. 2015;2:173–181. doi: 10.1007/s40588-015-0025-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim J.-Y., Cho S.-H., Joo H.-N., Tsuji M., Cho S.-R., Park I.-J., Chung G.-T., Ju J.-W., Cheun H.-I., Lee H.-W., et al. First case of human babesiosis in Korea: Detection and characterization of a novel type of Babesia sp. (KO1) similar to ovine Babesia. J. Clin. Microbiol. 2007;45:2084–2087. doi: 10.1128/JCM.01334-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zintl A., Mulcahy G., Skerrett H.E., Taylor S.M., Gray J.S. Babesia divergens, bovine blood parasite of veterinary and zoonotic importance. Clin. Microbiol. Rev. 2003;16:622–636. doi: 10.1128/CMR.16.4.622-636.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tonnetti L., Young C., Kessler D.A., Williamson P.C., Reik R., Proctor M.C., Brès V., Deisting B., Bakkour S., Schneider W. Transcription-mediated amplification blood donation screening for Babesia. Transfusion. 2020;60:317–325. doi: 10.1111/trf.15630. [DOI] [PubMed] [Google Scholar]
- 54.Brennan M.B., Herwaldt B.L., Kazmierczak J.J., Weiss J.W., Klein C.L., Leith C.P., He R., Oberley M.J., Tonnetti. L., Wilkins P.P., et al. Transmission of Babesia microti parasites by solid organ transplantation. Emerg. Infect. Dis. 2016;22:1869–1876. doi: 10.3201/eid2211.151028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.New D.L., Quinn J.B., Qureshi M.Z., Sigler S.J. Vertically transmitted babesiosis. J. Pediatr. 1997;131:163–164. doi: 10.1016/S0022-3476(97)70143-4. [DOI] [PubMed] [Google Scholar]
- 56.Fox L.M., Winger S., Ahmed A., Arnold A., Chou J., Rhein L., Levy O. Neonatal babesiosis: Case report and review of the literature. Pediatr. Infect. Dis. J. 2006;25:169–173. doi: 10.1097/01.inf.0000195438.09628.b0. [DOI] [PubMed] [Google Scholar]
- 57.Cornett J.K., Malhotra A., Hart D. Vertical transmission of babesiosis from a pregnant, splenectomized mother to her neonate. Infect. Dis. Clin. Pract. 2012;20:408–410. doi: 10.1097/IPC.0b013e31825b20c1. [DOI] [Google Scholar]
- 58.Iyer S., Goodman K. Congenital babesiosis from maternal exposure: A case report. J. Emerg. Med. 2019;56:E39–E41. doi: 10.1016/j.jemermed.2018.12.044. [DOI] [PubMed] [Google Scholar]
- 59.Lavoie P.E., Lattner B.P., Duray P.H., Barbour A.G., Johnson P.C. Culture positive seronegative transplacental Lyme borreliosis infect morality. Arthritis Rheum. 1987;30:50. [Google Scholar]
- 60.MacDonald A.B. Human fetal borreliosis, toxemia of pregnancy, and fetal death. Zentralbl. Bakteriol. Mikrobiol. Hyg. A. 1986;263:189. doi: 10.1016/S0176-6724(86)80122-5. [DOI] [PubMed] [Google Scholar]
- 61.Trevisan G., Stinco G., Cinco M. Neonatal skin lesions due to spirochetal infection; A case of congenital Lyme borreliosis? Int. J. Dermatol. 1997;36:677–680. doi: 10.1046/j.1365-4362.1997.00217.x. [DOI] [PubMed] [Google Scholar]
- 62.Horowitz R.I. Lyme disease and pregnancy: Implication of chronic infection, PCR testing, and prenatal treatment; In Proceeding of the 16th International Scientific Conference on Lyme Disease & Other Tick-Borne Disorders; Hartford, CT, USA. 7–8 June 2003. [Google Scholar]
- 63.Gardner T. Lyme disease. In: Remington J.S., Klein J.O., editors. Infectious Diseases of the Fetus and Newborn Infant. 5th ed. W.B. Sanders Company; Philadelphia, PA, USA: 2001. pp. 519–641. Chapter 11. [Google Scholar]
- 64.Eisen R.J., Eisen L., Beard C.B. Country-scale distribution of Ixodes scapularis and Ixodes pacificus (Acari: Ixodidae) in the continental United States. J. Med. Entomol. 2016;53:349–386. doi: 10.1093/jme/tjv237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Penzhorn B.L., Oosthuizen M.C. Babesia species of domestic cats: Molecular characterization has opened Pandora’s box. Front. Vet. Sci. 2020;7:134. doi: 10.3389/fvets.2020.00134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Keirans J.E., Clifford C.M. The genus Ixodes in the United States: A scanning electron microscope study and key to the adults. J. Med. Entomol. 1978;15:1–38. doi: 10.1093/jmedent/15.suppl2.1. [DOI] [PubMed] [Google Scholar]
- 67.Keirans J.E., Hutcheson H.J., Durden L.A., Klompen J.S.H. Ixodes (Ixodes) scapularis (Acari: Ixodidae): Redescription of all active stages, distribution, hosts, geographical variation, and medical and veterinary importance. J. Med. Entomol. 1996;33:297–318. doi: 10.1093/jmedent/33.3.297. [DOI] [PubMed] [Google Scholar]
- 68.Durden L.A., Keirans J.E. Nymphs of the Genus Ixodes (Acari: Ixodidae) of the United States: Taxonomy, Identification Key, Distribution, Hosts, and Medical Veterinary Importance, Monographs. Thomas Say Publications in Entomology, Entomological Society of America; Lanham, MD, USA: 1996. p. 95. [Google Scholar]
- 69.Foley J., Tinoco-Gracia L., Rodriguez-Lomelf M., Estrada-Guzmán J., Fierro M., Mattar-Lopez E., Peterson A., Pascoe E., Gonzalez Y., Hori-Oshima S., et al. Unbiased assessment of abundance of Rhipicephalus sanguineus sensu lato ticks, canine exposure to spotted fever group Rickettsia, risk factor in Mexicali, México. Am. J. Trop. Med. Hyg. 2019;101:22–32. doi: 10.4269/ajtmh.18-0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Barbour A.G., Bunikis J., Tranvinsky B., Hoen A.B., Diuk-Wasser M.A., Fish D., Tsao J.I. Niche partitioning of Borrelia burgdorferi and Borrelia miyamotoi in the same tick vector and mammalian reservoir species. Am. J. Trop. Med. Hyg. 2009;8:1120–1131. doi: 10.4269/ajtmh.2009.09-0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Drazenovich N., Foley J., Brown R.N. Use of real-time quantitative PCR targeting the msp2 protein gene to identify cryptic Anaplasma phagocytophilum infections in wildlife and domestic animals. Vector Borne Zoonotic Dis. 2006;6:83–90. doi: 10.1089/vbz.2006.6.83. [DOI] [PubMed] [Google Scholar]
- 72.Black W.C., 4th, Piesman J. Phylogeny of hard- and soft-tick taxa (Acari: Ixodidae) based on mitochondrial 16S rDNA sequences. Proc. Natl. Acad. Sci. USA. 1994;91:10034–10038. doi: 10.1073/pnas.91.21.10034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Beati L., Keirans J.E. Analysis of the systematic relationships among ticks of the genera Rhipicephalus and Boophilus (Acari: Ixodidae) based on mitochondrial 12 ribosomal DNA gene sequences and morphological characters. J. Parasitol. 2001;87:32–48. doi: 10.1645/0022-3395(2001)087[0032:AOTSRA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are reported in the manuscript.