Abstract
Objectives
Women may differ by whether they rely on health providers and/or social ties for seeking information and advice about family planning. It is unknown whether these differences matter for contraceptive outcomes. This study assessed the association between women’s family planning (FP) network (social and/or provider ties) and contraceptive use.
Study Design
This cross-sectional, egocentric network study was conducted among reproductive-age women (n=193) in rural Madagascar. Data included socio-demographics and contraceptive use. Respondents listed who they relied on for contraceptive information, advice or guidance and provided ties’ gender, age, relationship, and perceived support of contraceptive use. The primary outcome was current contraceptive use. Predictors included having a FP network (0/1) and FP network composition (no network, social ties only, provider ties only, both provider and social ties), respectively. Analyses were conducted using a generalized linear model specifying a Poisson distribution, with covariate adjustment and cluster robust standard errors.
Results
Having a network of individuals to turn to for contraceptive information compared to having no FP network was positively associated with contraceptive use (adjusted relative risk [aRR] 4.4, 95% confidence interval [CI] 2.00-9.87). Having a social network, a provider network, or a combination of social and provider network were all positively associated with contraceptive use (aRR 4.30 [CI 1.92-9.66], aRR 4.46 [CI 2.04-9.75], aRR 4.72 [CI 1.93-11.50], respectively), compared to having no FP network.
Conclusions
Contraceptive use was higher among women who relied on social ties, provider ties or both for contraceptive information and advice, compared to women with no FP network. These findings suggest that FP interventions should use a multi-component approach taking into account both social and provider networks.
Implications:
It is unknown whether differences in whether women rely on social ties (friends, partner, family members) versus providers for contraceptive information and advice affect contraceptive outcomes. Women are just as likely to use contraception whether they rely on social ties, provider ties, or both for contraceptive information and advice.
Keywords: social networks, contraceptives, family planning, community health workers, Madagascar, sub-Saharan Africa
1. Introduction
Contraceptive use remains low in sub-Saharan Africa, including in Madagascar where 36% of women are using modern contraception and one quarter of women (24%) have an unmet need for contraception [1,2]. Reducing unmet need for contraception can significantly reduce the persistently high rates of maternal mortality including in Madagascar [3,4]. Ensuring that women have universal access to family planning (FP) services is recognized as a priority in the 2030 Sustainable Development Goals [5]. Removing barriers to access, providing information and support for seeking reproductive health services, and offering respectful care will allow women to use contraception when desired and exercise their reproductive autonomy [6].
Social networks, or the relations that women have with their partners, family members, and friends [7,8], may be an influential factor in women’s use of contraceptive services. Researchers across disciplines are increasingly drawing on social network theory and analysis to explore how women’s reproductive health decisions are tied to others in their networks [9–11]. Several studies, including a systematic review, have shown that contraceptive use within women’s social networks may influence women’s fertility-related behaviors [12–21]. Most studies have found a positive relationship between women’s contraceptive use and contraceptive-related attitudes and behaviors among women’s social relations [12–21]. For example, Valente et al. (1997) demonstrated that women in Cameroon were more likely to use contraception if their network approved of contraception, used it and encouraged them to use it [15]. In a longitudinal study adjusting for unmeasured confounding and homophily, women in Kenya with network members who used contraception had twice the odds of using contraception [16]. Other research highlights that the network composition influences contraceptive use: in Mali, contraceptive use was lower when women’s networks included conjugal kin compared to when they included individuals from outside the village [22]. In Niger, women’s use of contraception was associated with ties’ contraceptive use only if ties were sisters but not friends [23].
Women may differ in the types of individuals (i.e. ties) they rely on for seeking information, advice and guidance about contraception. Some women may rely on social ties, including friends, partners and family members. Other women may rely on health provider ties (e.g. community health workers [CHWs], doctors, nurses, or mid-wives). Women may also rely on a combination of both types of ties, or no one at all. Trusted information sources about contraception can include health providers, peers, family members, and the media, but women will vary in the extent to which they rely on or trust these different sources [24–26]. A systematic review of contraceptive knowledge among adolescents in low-and middle-income countries found that, while health workers were a trusted source of contraceptive information, adolescent girls tended to receive most information from peers and family members [25].
Very few studies have examined whether the type of tie women rely on for contraceptive information and advice affects contraceptive outcomes. Most network research on contraceptive use has looked at social ties, with few studies comparing the influence of social versus provider ties. In Kenya, having a provider network for contraceptive information was not associated with current use of contraception but was associated with ever use of contraception [18]. In Tanzania, contraceptive use was associated with relying on interpersonal ties for contraceptive information but not with relying on health providers [27]. In our study among men in partnership in Madagascar, couples’ contraceptive use just as high whether men relied on social ties versus provider ties for contraceptive information [28].
While women may vary by who they rely on for contraceptive information and advice, there is limited evidence on whether the composition of women’s FP networks, be it social ties and/or provider ties, is differentially associated with contraceptive use. Ties to providers offer learning opportunities about contraception especially if providers are perceived as trusted information sources offering patient-centered care [29,30]. Social ties not only offer learning opportunities but can also affect decisions through social influence, which may accelerate contraceptive adoption [31]. Alternatively, social ties may constrain reproductive health behaviors to align with other network members, depending on the social norms and types of network ties [22,32]. Understanding whether differences in the composition of women’s FP networks is associated with contraceptive use will help inform the design of better strategies to ensure access to and use of contraception for all women who desire them.
In this egocentric study, we collected FP network data from reproductive-age women in Madagascar to assess the associations between contraceptive use and: 1) having a FP network, 2) the composition of that FP network, and 3) knowing other contraceptive users.
2. Material and methods
2.1. Respondents
We recruited the study sample from 27 villages randomly selected from the 80 villages within a five kilometer radius of the semi-urban town of Ambalavao in Fianarantsoa Province, in southern Madagascar. Data collectors enumerated all households by village and then used random number draws to identify households for study participation. The total sample size chosen from each village was proportionate to the number of households in the village, with a minimum of five households per village. Inclusion criteria included women aged 18 to 45 willing to answer FP questions. In each selected household, data collectors enumerated all eligible women and randomly selected one. Female data collectors conducted the surveys in Malagasy to facilitate study recruitment and elicit candid answers about reproductive health topics. Prior to administering the survey, the data collectors obtained respondents’ informed consent, either written or orally if respondents were illiterate. All women who were randomly chosen consented, yielding a study sample of 213 women. Respondents received a lamba, a cloth used locally for multiple purposes, for their participation in the study. We removed 20 pregnant women from the analytical sample. The final analytical sample consisted of 193 respondents. The University of California San Francisco Institutional Review Board and the National Ethics Committee in Madagascar both approved this study.
2.2. Data collection
From June to July 2019, we asked respondents if they were currently using modern contraceptive methods including the implant, intra-uterine device (IUD), oral contraceptives, injectables, the external/male condom, and female or male sterilization. We also asked respondents if they knew of any person who was using these methods, whether or not the person was in the woman’s FP network to capture women’s awareness of contraceptive use in their community. We also collected data on respondents’ age, parity, marital status (married/living with partner, partnered but living apart, divorced, widowed, or no partner), household size, school attendance, highest grade attained, occupation, household earnings in past month, and whether the household had electricity. We also asked respondents if they had a menstrual period in the last four weeks and, if not, why (with “currently pregnant” as an answer category). Among those not pregnant, we asked if, in the last 4 weeks, they had wanted to become pregnant (with answer categories for wanted to become pregnant, did not want to, and was not certain). We also gathered data about who, within the couple, made decisions about contraceptive use (respondent, her partner, or together as a couple) and about the respondent’s partner including occupation. Twenty-four respondents (12% of sample) have missing values for some of these data.
To collect network data, we adapted questions from Brunson (2013) [33] and asked study respondents (known as egos in social network studies) to list the individuals (known as alters which can include friends, family members or other types of social ties) from whom they obtain information, advice, and/or guidance about contraceptive methods. Interviewers then prompted respondents to review if they had forgotten any individuals and asking them to consider their partner(s), siblings, parents, CHWs, and other health providers to ensure completeness. We defined respondents who listed one or more alters who they relied on for contraceptive information and advice as having a FP network, while we defined those with no alters as having no FP network. While respondents could list up to 20 alters, the maximum number of alters was seven with some women listing no alters. The interviewers then asked respondents to select the top five alters who they relied on most for contraceptive information and advice and provide those alters’ age, gender, nature of the relationship, and alters’ perceived support of contraceptive use (supportive of modern contraceptive use vs. not supportive).
2.3. Measures
The primary outcome was a binary measure of whether the participant was currently using modern contraception. We defined modern contraception as injectables, the pill, implant, IUD and external condom, but excluded male and female sterilization because respondents misunderstood the question. For reference, four percent of women in Madagascar report using female sterilization and 0.3% report that men were sterilized.2 We generated the following network measures as predictors in separate analyses. The first predictor variable was a dichotomous variable for whether a woman reported having no FP network (i.e., she named no alters) or if she had a FP network (i.e., she named one or more alters in her FP network). The second was a dichotomous variable for whether the FP network was composed of social relations (referred to as social network), including partner, other family members, and/or friends. The variable took on a value of 1 if her FP network included social relations and 0 if her FP network did not include social relations or if she had no FP network. Similarly, the third dichotomous variable measured whether the FP network was composed of health providers (referred to as provider network), including CHWs, health educators, nurses, mid-wives or doctors. The variable equaled 1 if her FP network included providers and 0 if her FP network had no health providers or she had no FP network. The next predictor variable was a mutually exclusive categorical variable for the network’s composition: 1) no FP network, 2) social network only; 3) provider network only; and 4) social and provider network, composed of both social and provider ties. Network size was defined as: 1) a categorical variable for no FP network, one alter, or ≥ two alters and 2) a continuous variable. A dichotomous variable was created to identify women who knew someone else using modern contraception (whether or not that person was in their FP network). The last set of analyses at the ego-level included all three network variables together (FP network composition, size of network (continuous), and whether women knew someone using contraception to compare the relative importance of these different correlates of contraceptive use (results available upon request). There were no differences in contraceptive use or network composition by missingness of baseline covariates.
2.4. Analytical approach
We fitted a generalized linear model specifying a Poisson distribution with robust standard errors, interpreting the estimated incidence rate ratios as relative risk ratios (RR) [34]. In all analyses, we adjusted for individual-level characteristics including age, parity, marital status, primary school completion, and household earnings. We included fixed effects by sub-district (the Malagasy fokontany, which represents groups of villages). We conducted these analyses at the ego-level using cluster-correlated robust standard errors at the sub-district level. We then conducted alter-level analyses among the women with a FP network to examine the association between alter characteristics (alter gender, alter age, perceived support from the alter for contraceptive use, and alter’s relationship with the ego [e.g. CHW]) and women’s use of contraception, also with robust standard errors clustered by sub-district. Sensitivity analyses included: adjusting for 1) household size and occupation as farmer, 2) pregnancy desires, 3) couples’ contraceptive decision-making, 4) restricting the sample to women who were sexually active in the last 4 weeks, and 5) restricting the sample to women who were married or in partnership.
3. Results
3.1. Descriptive statistics of sample
Table 1 provides summary statistics of the study sample. Ambivalence about becoming pregnant was common with 123 (75%) women saying they were uncertain about whether they wanted to become pregnant. Two-thirds of the women reported currently using a modern contraceptive method (131 [69%]) (Table 2). The most common modern contraceptive methods were injectables (75 [39%]), the implant (30 [16%]), and the pill (27 [14%]). Three-quarters of the women knew someone else using modern contraception.
TABLE 1.
Percentage distribution of women aged 15-49 in Madagascar who participated in a survey about who they relied on for contraceptive information and advice, by selected characteristics (n=193)
| n | % | |
|---|---|---|
| Demographics | ||
| Mean age (SD) | 31 | (8.4) |
| Parity | ||
| 0 | 24 | 12 |
| 1 | 50 | 6 |
| 2 | 46 | 24 |
| 3 | 31 | 16 |
| 4 | 23 | 12 |
| 5+ | 19 | 10 |
| Marital status | ||
| Married or living with partner | 143 | 79 |
| Has partner but not living together | 12 | 07 |
| Divorced | 16 | 09 |
| Widow | 2 | 01 |
| No partner | 9 | 05 |
| Attended school | 187 | 97 |
| Completed primary education | 126 | 66 |
| Mean grade attained (SD) | 5.8 | (3.0) |
| Mean household size (SD) | 4.9 | (1.9) |
| Socioeconomics | ||
| Occupation farmer | 184 | 96 |
| Home has electricity | 9 | 05 |
| Mean household earnings (US dollars) last month (SD) | 30.8 | (82.4) |
| Pregnancy desires | ||
| Wants to become pregnant | 8 | 5 |
| Does not want to become pregnant | 33 | 20 |
| Is not certain | 123 | 75 |
| Partner Relationship (n=155) | ||
| Partner’s occupation as farmer | 106 | 94 |
| Ever hidden contraceptive use from partner | 17 | 18 |
| Decision-making about contraceptive use with partner | ||
| Woman decides | 6 | 6 |
| Partner decides | 29 | 28 |
| Couple decides together | 68 | 66 |
TABLE 2.
Percentage distribution of women aged 15-49 in Madagascar who participated in a survey about whom they relied on for contraceptive information and advice, by contraceptive and family planning network indicators (n=193)
| Outcomes | n | % |
|---|---|---|
| Contraceptive use (current) | ||
| Any modern method | 131 | 69 |
| Injectable | 75 | 39 |
| Pill | 27 | 14 |
| Implant | 30 | 16 |
| Intra-uterine device | 1 | 1 |
| External/male condom | 0 | 0 |
| No modern method | 59 | 31 |
| Network predictors | ||
| Has a FP network | 152 | 79 |
| ------ that includes friends, family and/or partner (social network) | 81 | 42 |
| ------ that includes health providers (provider network) | 91 | 47 |
| Composition of FP network | ||
| Social network only | 61 | 32 |
| Provider network only | 71 | 37 |
| Social and provider network | 20 | 10 |
| No FP network | 41 | 21 |
| Mean size of FP network (SD) | 1.1 | (0.9) |
| Number of alters in FP network | ||
| Zero alters | 41 | 21 |
| One alter | 112 | 58 |
| Two alters | 24 | 12 |
| Three alters | 11 | 6 |
| Four alters | 3 | 2 |
| Five or more alters | 2 | 1 |
| Knows someone using: | ||
| Modern contraceptive method | 136 | 76 |
| Injectable | 107 | 59 |
| Pill | 96 | 53 |
| Implant | 98 | 54 |
| Intra-uterine device | 16 | 9 |
| External/male condom | 5 | 3 |
| Alter characteristics (reported by ego) (n=214) | ||
| Mean age (SD) | 39 | (11.8) |
| Female | 171 | 88 |
| Supportive of contraceptive use | 200 | 96 |
| Relationship to ego | ||
| Community health worker | 46 | 22 |
| Health educator | 27 | 13 |
| Health provider (mid-wife, nurse, doctor) | 37 | 17 |
| Friend | 46 | 22 |
| Partner | 20 | 9 |
| Sibling | 13 | 6 |
| Mother | 14 | 7 |
| Aunt | 4 | 2 |
| Other | 7 | 3 |
Notes: “Alter” refers to any individual that study respondents identified as being someone upon whom they relied on for contraceptive information and advice.
Most women reported having a FP network (152 [79%]) meaning they listed one or more alters that they turned to for contraceptive information and advice. Among women with a FP network, most relied only on one alter, while only one-fifth of the women relied on two or more alters. The composition of the FP network varied among the sample, with one-third of women relying only on social ties (61 [32%]), another third relying only on providers ties (71 [37%]) and ten percent (20) relying on both social and provider ties for contraceptive information and advice.
Among the 214 nominated alters, most of them were women (171 [88%]), and almost all were perceived to be supportive of contraceptive use (200 [96%]). The most common types of relationships/roles included in these women’s FP networks were friends (22%), CHWs (22%), health educators (13%), and other health providers (nurses, mid-wives and doctors) (17%). Only 9% of alters were partners, while family members who were nominated included mothers (7%), siblings (6%), and aunts (2%).
3.2. Association between composition of FP network and use of contraception
Contraceptive use varied by the type of FP networks (p ≤ 0.001, Figure 1). Regression analyses showed that having a network of individuals to turn to for contraceptive information and advice was positively associated with contraceptive use (adjusted Relative Risk [aRR] 4.44; 95% confidence interval [CI] 2.00-9.87; p=0.000) (Table 3). Compared with having no FP network, having a social network only, having a provider network only, and having both a social and a provider network were all positively associated with contraceptive use ([aRR] 4.30 [CI 1.92-9.66]; aRR 4.46 [CI 2.04-9.75]; aRR 4.72 [CI 1.93-11.50], respectively). Tests of equality of the coefficients across women with different types of FP networks found no differences (social only vs. provider only network [p=0.61], social only vs. social and provider network [p=0.22], provider only vs. social and provider network [p=0.68]). Compared with having no FP network, having one alter (aRR 4.35; CI 1.95-9.70) and having two or more alters (aRR 4.68; CI 2.04-10.76) were both positively associated with contraceptive use.
Figure 1.
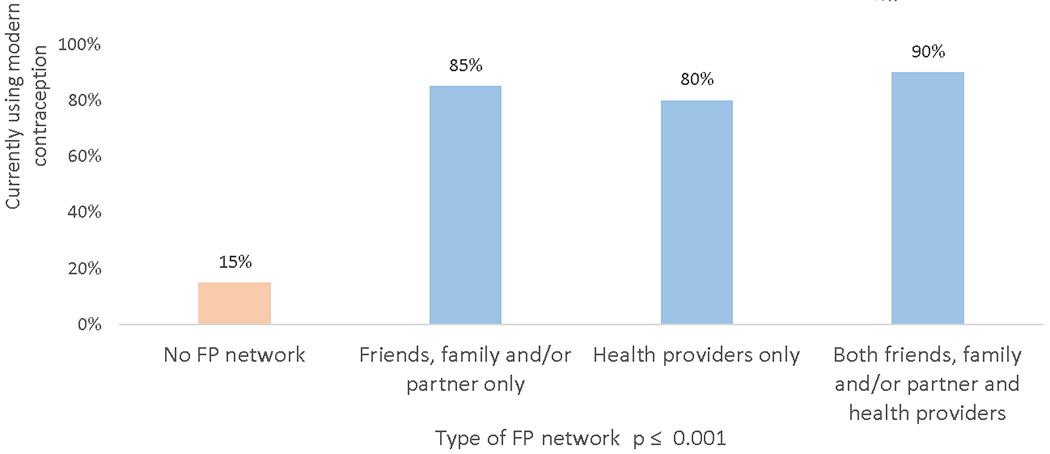
Contraceptive use by whether women rely on family/friends, health providers or both for contraceptive information and advice
Note: FP network can be composed of social relations only (friends, family and/or partner), health providers, or a combination of both social and provider relations. FP network is defined as those individuals women rely on for contraceptive information and advice
Table 3.
Associations between current contraceptive use, family planning network size, and composition of family planning network (N=193 women)
| Currently using modern contraception* | ||
|---|---|---|
| Independent variables | aRR | 95% CI |
| Has a FP network | 4.44 | (2.00 – 9.87) |
| FP network includes friends, family and/or partner (social network) | 1.37 | (1.04 – 1.80) |
| FP network includes health providers (provider network) | 1.49 | (1.34 – 1.66) |
| Composition of FP network~ | ||
| No FP network (reference group) | -- | |
| Social network only | 4.30 | (1.92 – 9.66) |
| Provider network only | 4.46 | (2.04 – 9.75) |
| Social and provider network | 4.72 | (1.93 – 11.50) |
| Size of FP network~ | ||
| No FP network (reference group) | -- | |
| One alter in FP network | 4.35 | (1.95 – 9.70) |
| Two or more alters in FP network | 4.68 | (2.04 – 10.76) |
| Number of alters in network (continuous) | 1.26 | (1.04 – 1.51) |
| Knows someone using modern contraceptive method | 2.04 | (1.08 – 3.85) |
Each estimate corresponds to the results of a single multivariable Poisson regression model. Contraceptive use is the dependent variable and the row variable is the primary explanatory variable of interest. All models adjust for respondent’s age, parity, marital status, primary school completion, and household earnings and sub-district fixed effects. We excluded women who were currently pregnant and used cluster-correlated robust standard errors at the sub-district level.
Both composition of FP network and size of FP networks are categorical variables. In both cases, the estimates for each category within those variables are from one multivariable model.
Notes: aRR = adjusted risk ratio; FP = family planning.
When we mutually adjusted for the different network measures, the composition of the FP network was the most important correlate for contraceptive use. Having a social network only, having a provider network only, and having both a social and a provider network, compared with having no FP network, were all positively associated with contraceptive use (p≤0.01). The adjusted risk ratios on network size and knowing someone using modern contraception became smaller in magnitude and were no longer statistically significant (results available upon request).
Among women with a FP network (N=152 women; n=214 alters), alter age was negatively associated with contraceptive use while alter supportiveness of contraceptive use was positively associated with use (Table 4). Contraceptive use was higher among women who relied on CHWs in their FP network (aRR 1.19 [CI 1.06-1.35]) and among women who relied on their partner (aRR 1.14 [CI 1.02-1.28]), compared with women who relied on doctors, nurses, and mid-wives (reference group). Tests of equality of the coefficients found no differences in contraceptive use between women who relied on friends vs. women who relied on mothers/aunts (P=0.98), women who relied on friends vs. women who relied on siblings (P=0.96), and women who relied on siblings vs. women who relied on mothers/aunts (P=1.00).
Table 4.
Associations between current contraceptive use and alter characteristics, among women with a family planning network (N=152 women; n=214 alters)
| Currently using modern contraception* | ||
|---|---|---|
| Alter characteristics | aRR | 95% CI |
| Female | 0.90 | (0.80 – 1.02) |
| Age (years) | 0.99 | (0.99 – 0.996) |
| Supportive of contraceptive use | 7.58 | (1.18 – 48.64) |
| Type of relation with respondent ~ | ||
| Provider (nurse, mid-wife, doctor) (reference group) | -- | |
| Community health worker | 1.19 | (1.06 – 1.35) |
| Health educator | 0.94 | (0.72 – 1.23) |
| Friend | 1.01 | (0.83 – 1.23) |
| Partner | 1.14 | (1.02 – 1.28) |
| Mother or aunt | 1.01 | (0.78 – 1.29) |
| Sibling | 1.01 | (0.80 – 1.27) |
| Other | 1.19 | (1.05 – 1.35) |
Each estimate corresponds to the results of a single multivariable Poisson regression model. Contraceptive use is the dependent variable and the row variable is the primary explanatory variable of interest. All models adjust for respondent’s age, parity, marital status, primary school completion, and household earnings and sub-district fixed effects. We restricted these analyses to the 152 women who reported having a family planning network and excluded women who were currently pregnant, and used cluster-correlated robust standard errors at the sub-district level.
Type of relation with respondent is a categorical variables. The estimates for each category within that variable are from one multivariable model. Notes: aRR = adjusted risk ratio; FP = family planning. “Alter” refers to any individual that study respondents identified as being someone upon whom they relied for contraceptive information and advice.
3.3. Association between knowing other contraceptive users and own contraceptive use
Contraceptive use among women who knew someone else using contraception was higher (76%) compared to contraceptive use (43%) among women who did not know other contraceptive users (p ≤ 0.001; Figure 2). Regression analyses confirmed that knowing someone else using contraception was positively associated with women’s own use of contraception (aRR 2.04; CI 1.08-3.85) (Table 3). We conducted similar analyses by method type, focusing on the most common methods (injectables [39% ], the pill [14%] and implant [16%]) and found that knowing someone else using an injectable, the pill, or the implant was positively associated with use of that method (Appendix A).
Figure 2.
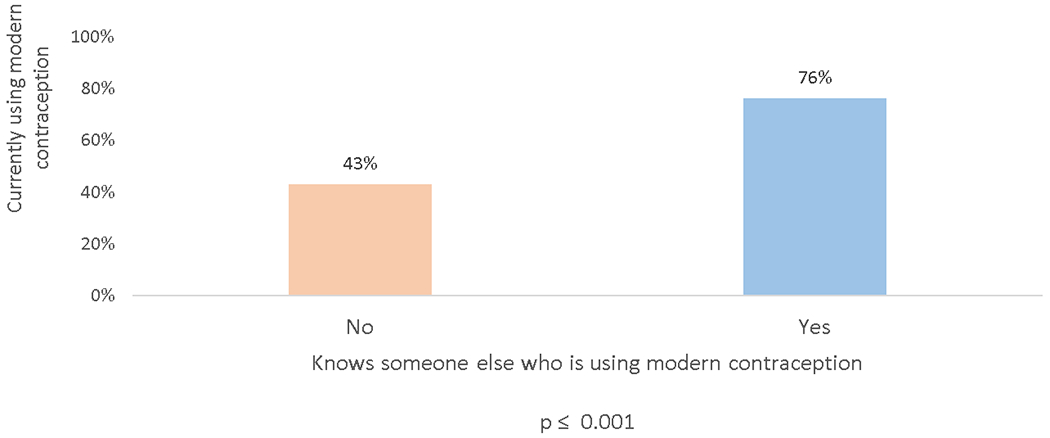
Contraceptive use by whether women know someone else who is also using contraception
3.4. Sensitivity analyses
The results were consistent after adjusting for additional covariates, including 1) household size and occupation, 2) pregnancy desires, and 3) couples’ decision-making power about contraceptive use. Results were consistent when regressions were adjusted for household size and occupation (results not shown). Wanting to avoid pregnancy was positively associated with contraceptive use (aRR 1.49; CI 1.31-1.71), whereas being uncertain about wanting to become pregnant was not associated with contraceptive use (Appendix B). When covariates for couples’ decision-making power about contraception were included, only having a provider network was positively associated with contraceptive use (Appendix B). There was no statistically significant association between contraceptive use and decision-making power. The main results were consistent when the sample was restricted to women who were sexually active in the last 4 weeks (n=145 [94%]) and women who were in partnership/married (n=155 [85%]) (results not shown).
4. Discussion
In this novel egocentric network study among women in rural Madagascar, we found that having a FP network was positively associated with contraceptive use. One-third of women rely on social ties only, one-third rely on provider ties only, and 10% rely on both social and provider ties, yet all of these women had higher contraceptive use compared to women who reported relying on no one for information and advice about contraception. Having a FP network was more important than the specific composition of that network including its size. Together, these findings suggest that FP interventions should use a multi-component approach taking into account both social and provider networks, not exclusively one or the other.
This study builds on the current literature by examining the composition of FP networks. Since very few studies have examined whether women tend to rely on social ties, provider ties or both for contraceptive information and advice, it is unknown whether these different types of FP networks are similarly associated with contraceptive use. Indeed, our findings showed that, while women differed in the type of FP network they had, having a FP network (whether it included social ties and/or provider ties) was similarly associated with higher contraceptive use compared to women with no FP network.
Our findings provide further evidence that women who rely on health providers as sources of information and advice about contraception are more likely to use contraception. These results are consistent with findings from men in couple in Madagascar [28], yet differ from studies among women in Kenya and Tanzania [18,27]. The positive association between relying on social ties and contraceptive use is consistent with many network studies [12–21]. While other network studies have found that the type of social tie may differentially matter for contraceptive use [22,23], our results only showed differential associations among women who relied on their partner and on CHWs as compared to those who relied on doctors, nurses and midwives. There were no differences in contraceptive use between women who relied on friends versus sisters versus aunts/mothers. Furthermore, while network size is a predictor of whether women use contraception, the more important network predictor of contraceptive use relates to whether women have a FP network and the composition of that network. In this particular study context, most women (64%) only had one alter in their FP network and other country contexts where women have larger networks may show different results.
The higher use of contraceptives among women who relied on CHWs compared to other health providers confirms the important role CHWs play in Madagascar for education about and provision of contraceptive methods [35,36]. These findings further confirm that interventions engaging CHWs are a promising avenue for improving contraceptive access. The higher use of contraceptives among women who report relying on their male partner for contraceptive information and advice suggests that these male partners are supportive of their partner’s contraceptive use. Yet, only 9% of alters were partners and up to one-fifth of study respondents reported having hidden contraceptive use from their partner. Future work should explore how partner engagement in contraceptive decision-making can facilitate women’s use of contraception, if desired.
As shown in other studies [15–17], women were more likely to use contraception if they knew someone else using contraception. Yet the coefficient was no longer statistically significant when measures of network composition were added. These findings imply that the most important network predictor related to contraceptive use is the composition of the FP network and whether women have a FP network at all. These FP networks can offer opportunities not only to learn about contraceptives but also receive support for contraceptive use from social and provider ties. Having a supportive FP network (whether the network members are contraceptive users or not) seems to be of particular importance in predicting contraceptive use, as shown here and elsewhere [13,15,18,19]. For example, Valente et al. (1997) found that perceptions of ties’ approval of contraceptive use was more important than whether ties were using contraception themselves [15]. Social influence, including social norms, may also be at play. Indeed, network research on contraceptive use has shown that the density of a woman’s social network and having ties to other contraceptive users affects contraceptive use through social influence including social norms [17]. Research on social norms in sub-Saharan Africa has found that perceptions about whether friends or most people within a local reference group engage in a health-related behavior are potentially more important than peers’ actual behaviors in relation to individuals’ own behaviors [15,20,37,38]. While the data did not allow for a distinction between alters’ active use versus ego’s perception of their use, future research should explore the role of both actual and perceived contraceptive use by alters on contraceptive use.
There are several study limitations. First, the cross-sectional nature of the network data limited our ability to establish causal relationships as it is not possible to rule out the role of homophily, or the influence of shared environmental factors that may affect contraceptive use. A woman using contraceptives could be more likely to know other contraceptive users not because she was influenced by these users but because she met those users while seeking contraceptive services, for example. Second, the data did not include alter-level contraceptive use for comparison to egos’ perceptions. Third, the sample may not be representative of rural populations in Madagascar since the villages were within a five kilometer radius of a well-resourced semi-urban town. Contraceptive use in the sample (69%) was higher than reported contraceptive use (36%) in Madagascar as a whole [2], potentially due to ease of access to providers in the study region.
This study on the role of social and provider networks for FP shows that having a network of individuals to turn to for information and advice about contraception was critical for the uptake of contraception among women in rural Madagascar. Women varied in whether they relied on providers, social relations, or a combination of both, yet all these women had higher contraceptive use compared to those with a FP network. Developing interventions to ensure that women have information about and access to contraception needs to be a multi-component strategy that integrates providers, including CHWs, as well as women’s social networks.
Acknowledgements:
This study was funded by Opportunity Solutions International (http:\www.opportunitysolutions.org), a 501(c)3 non-profit organization focused on health innovation and research in resource-limited settings. Funding for Dr. Comfort was also supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development through the Social Network and Health Fellowship (1R25HD079352). Funding for Dr. Krezanoski was also supported by the National Institutes of Health National Institute of Allergy and Infectious Disease via a Career Mentored Award (K23AI139364). We are grateful to the research team at Opportunity Solutions International who led the data collection in the field. We would like to thank all study respondents for sharing this valuable information about contraceptive decision-making. We would also like to acknowledge the helpful guidance and comments provided by Dilys Walker, Craig Cohen, Alison El Ayadi, Patience Afulani and other members of the Bixby Early Career Investigators Works in Progress seminar participants at UCSF.
Role of funding source:
This study was funded by Opportunity Solutions International (http:\\www.opportunitysolutions.org), a 501(c)3 non-profit organization focused on health innovation and research in resource-limited settings. Dr. Comfort and Dr. Krezanoski are co-Founders of Opportunity Solutions International. They receive no salary support from the organization. Funding for Dr. Comfort was also supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development through the Social Network and Health Fellowship (1R25HD079352). Funding for Dr. Krezanoski was also supported by the National Institutes of Health National Institute of Allergy and Infectious Disease via a Career Mentored Award (K23AI139364).
APPENDIX A.
Associations between current contraceptive use and composition of family planning network, stratified by type of contraception (N=162 women)
| Currently using modern contraception* | ||||||
|---|---|---|---|---|---|---|
| Injectables | Pill^ | Implant | ||||
| Independent variables | aRR | 95% CI | aRR | 95% CI | aRR | 95% CI |
| Has a FP network | 3.16 | (1.39 – 7.17) | 1.72e+07 | (5.64e+06 – 5.22e+07) | 5.56 | (2.51 – 12.33) |
| Composition of FP network~ | ||||||
| No FP network (reference group) | -- | -- | -- | |||
| Social network only | 2.89 | (1.32 – 6.32) | 1.94e+07 | (6.90e+06 – 5.46e+07) | 6.23 | (2.78 – 13.94) |
| Provider network only | 3.11 | (1.22 – 7.97) | 1.51e+07 | (4.36e+06 – 5.23e+07) | 6.34 | (3.34 – 12.02) |
| Social and provider network | 4.21 | (1.94 – 9.12) | 1.42e+07 | (1.51e+06 – 1.34e+08) | 3.53 | (1.37 – 9.10) |
| Knows someone using that same method | 2.28 | (1.62 – 3.20) | 17.48 | (1.77 – 172.75) | 6.30 | (3.36 – 11.80) |
Each estimate corresponds to the results of a single multivariable Poisson regression model. Contraceptive use is the dependent variable and the row variable is the primary explanatory variable of interest. All models adjust for respondent’s age, parity, marital status, primary school completion, and household earnings and sub-district fixed effects.
We excluded women who were currently pregnant and used cluster-correlated robust standard errors at the sub-district level.
The estimates for pill use are large because, among pill users, all women had a FP network and almost all women knew someone else using the pill.
Composition of FP network is a categorical variable. The estimates for each category within that variable are from one multivariable model.
Notes: aRR = adjusted risk ratio; FP = family planning
Appendix B.
Associations between current contraceptive use and composition of family planning network, adjusting for pregnancy desires and contraceptive decision-making (N=111 women)
| Currently using modern contraception± | ||||
|---|---|---|---|---|
| Independent variables | aRR | 95% CI | aRR | 95% CI |
| Composition of FP network | ||||
| No FP network (Reference group) | -- | -- | ||
| Social network only | 3.27 | (1.75 – 6.11) | 2.27 | (0.89 – 5.80) |
| Provider network only | 3.20 | (1.72 – 5.97) | 2.44 | (1.04 – 5.70) |
| Social and provider network | 3.57 | (1.90 – 6.68) | 2.04 | (0.69 – 6.05) |
| Pregnancy desires | ||||
| Wants to become pregnant (Reference group) | -- | -- | ||
| Does not want to become pregnant | 1.49 | (1.31 – 1.71) | ||
| Is not certain | 1.24 | (0.91 – 1.69) | ||
| Decision-making about contraceptive use with partner | ||||
| Woman decides (Reference group) | -- | |||
| Partner decides | 1.08 | (0.83 – 1.40) | ||
| Couple decides together | 1.24 | (0.90 – 1.70) | ||
Each column corresponds to the results of a single multivariable Poisson regression model. Contraceptive use is the dependent variable and composition of the FP network and either pregnancy desires or decision-making about contraceptive use are specified as the explanatory variables of interest. These variables are mutually adjusted for each other and adjusted for respondent’s age, parity, marital status, primary school completion, and household earnings and sub-district fixed effects. We excluded women who were currently pregnant and used cluster-correlated robust standard errors at the sub-district level.
Notes: aRR = adjusted risk ratios; FP = family planning
Contributor Information
Alison B. Comfort, University of California San Francisco, Opportunity Solutions International, 3333 California Street, San Francisco, CA 94143, United States
Cynthia C. Harper, University of California San Francisco, 3333 California Street, San Francisco, CA 94143, United States
Alexander C. Tsai, Center for Global Health and Mongan Institute, Massachusetts General Hospital, Harvard Medical School, 125 Nashua Street, Suite 722, Boston, MA 02114
James Moody, Duke University, 268 Soc/Psych Building, Duke University, Durham NC 27708-0088
Jessica M. Perkins, Peabody College of Education and Human Development, Vanderbilt University, PMB 90, 230 Appleton Place, Nashville, Tennessee 37203-5721
Justin Ranjalahy Rasolofomana, Institut National de Santé Publique et Communautaire, Ex-Ecole de Médecine de Befelatanana, BP 176, Antananarivo, Madagascar
Cora Alperin, University of Chicago, 5438 S Woodlawn Avenue, Chicago, IL 60615.
Anja Noeliarivelo Ranjalahy, TANDEM SARL, Lot H 107, Merimanjaka, 102, Antananarivo Madagascar.
Ravo Heriniaina, Opportunity Solutions International, Lot III G17, Ambalavao, Madagascar.
Paul J. Krezanoski, University of California San Francisco, Zuckerberg San Francisco General Hospital, Opportunity Solutions International, 1001 Potrero Ave, San Francisco, CA 94110
REFERENCES
- [1].United Nations, Department of Economic and Social Affairs, Population Division. Estimates and Projections of Family Planning Indicators. New York: United Nations, 2019. [Google Scholar]
- [2].FP2020. FP2020 Women at the Center 2018-2019. Washington DC: United Nations Foundation, 2019. [Google Scholar]
- [3].Global Burden of Disease Maternal Mortality Collaborators. Global, regional, and national levels of maternal mortality, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388(10053): 1775–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Guttamcher Institute. Adding It Up: Investing in Contraception and Maternal and Newborn Health, 2017. https://www.guttmacher.org/fact-sheet/adding-it-up-contraception-mnh-2017 (accessed April 17, 2020).
- [5].United Nations. Goal 3: Ensure healthy lives and promote well-being for all at all ages. 2020. https://www.un.org/sustainabledevelopment/health/ (accessed April 17, 2020).
- [6].Holt K, Reed R, Crear-Perry J, Scott C, Wulf S, Dehlendorf C. Beyond same-day long-acting reversible contraceptive access: a person-centered framework for advancing high-quality, equitable contraceptive care. Am J Obstet Gynecol 2020; 222(4s): S878.e1–S.e6. [DOI] [PubMed] [Google Scholar]
- [7].Tsai AC, Papachristos AV. From social networks to health: Durkheim after the turn of the millennium. Introduction. Soc Sci Med 2015; 125: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Jackson MO. Social and Economic Networks. Princeton, New Jersey: Princeton University Press; 2008. [Google Scholar]
- [9].Bernardi L, Klarner A. Social networks and fertility. Demog Res 2014; 30(2): 641–670. [Google Scholar]
- [10].Sandberg J Infant Mortality, Social Networks, and Subsequent Fertility. Am Sociol Rev 2006; 71(2): 288–309. [Google Scholar]
- [11].Bongaarts J, Watkins SC. Social interactions and contemporary fertility transitions. Popul Dev Rev 1996; 22(4): 639–82. [Google Scholar]
- [12].Lowe SMP, Moore S. Social networks and female reproductive choices in the developing world: a systematized review. Reprod Health 2014; 11: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Gayen K, Raeside R. Social networks and contraception practice of women in rural Bangladesh. Soc Sci Med 2010; 71(9): 1584–92. [DOI] [PubMed] [Google Scholar]
- [14].Mosha IH, Ruben R. Communication, knowledge, social network and family planning utilization among couples in Mwanza, Tanzania. Afr J Reprod Health 2013; 17(3): 57–69. [PubMed] [Google Scholar]
- [15].Valente TW, Watkins SC, Jato MN, van der Straten A, Tsitsol LP. Social network associations with contraceptive use among Cameroonian women in voluntary associations. Soc Sci Med 1997; 45(5): 677–87. [DOI] [PubMed] [Google Scholar]
- [16].Behrman JR, Kohler HP, Watkins SC. Social networks and changes in contraceptive use over time: evidence from a longitudinal study in rural Kenya. Demography 2002; 39(4): 713–38. [DOI] [PubMed] [Google Scholar]
- [17].Kohler H-P, Behrman JR, Watkins SC. The density of social networks and fertility decisions: evidence from South Nyanza District, Kenya. Demography 2001; 38(1): 43–58. [DOI] [PubMed] [Google Scholar]
- [18].Musalia JM. Gender, social networks, and contraceptive use in Kenya. Sex Roles 2005; 53(11): 835–46. [Google Scholar]
- [19].Boulay M, Valente T. The relationship of social affiliation and interpersonal discussion to family planning knowledge, attitudes and practice. Int Fam Plann Perspect 1999; 25: 112–38. [Google Scholar]
- [20].Dynes M, Stephenson R, Rubardt M, Bartel D. The influence of perceptions of community norms on current contraceptive use among men and women in Ethiopia and Kenya. Health Place 2012; 18(4): 766–73. [DOI] [PubMed] [Google Scholar]
- [21].Islam S Social networks and their effects on the choice of contraceptive use and method in Bangladesh. Int J Hum Rights Healthc 2019: 13(1). [Google Scholar]
- [22].Madhavan S, Adams A. Women’s networks and the social world of fertility behavior. Int Fam Plan Perspect 2003; 29(2): 58–68. [DOI] [PubMed] [Google Scholar]
- [23].Shakya HB, Challa S, Nouhou AM, Vera-Monroy R, Carter N, Silverman J. Social network and social normative characteristics of married female adolescents in Dosso, Niger: Associations with modern contraceptive use. Glob Public Health 2020: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Alege SG, Matovu JK, Ssensalire S, Nabiwemba E. Knowledge, sources and use of family planning methods among women aged 15-49 years in Uganda: a cross-sectional study. Pan Afr Med J 2016; 24: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Munakampe MN, Zulu JM, Michelo C. Contraception and abortion knowledge, attitudes and practices among adolescents from low and middle-income countries: a systematic review. BMC Health Serv Res 2018; 18(1): 909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Ajong AB, Njotang PN, Kenfack B, Yakum MN, Mbu ER. Knowledge of women in family planning and future desire to use contraception: a cross sectional survey in Urban Cameroon. BMC Res Notes 2016; 9: 347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Nsanya MK, Atchison CJ, Bottomley C, Doyle AM, Kapiga SH. Modern contraceptive use among sexually active women aged 15-19 years in North-Western Tanzania: results from the Adolescent 360 (A360) baseline survey. BMJ Open 2019; 9(8): e030485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Comfort AB, Harper C, Tsai A, Perkins JM, Moody J, Rasolofomanana JR, Alperin C, Schultz M, Ranjalahy AN, Heriniaina R, Krezanoski PJ. The association between men’s family planning networks and contraceptive use among their female partners: an egocentric network study in Madagascar. BMC Public Health 2021; 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Wekesa E, Coast E. Contraceptive need and use among individuals with HIV/AIDS living in the slums of Nairobi, Kenya. Int J Gynaecol Obstet 2015; 130 Suppl 3(Suppl 3): E31–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Sundstrom B, Szabo C, Dempsey A. “My Body. My Choice”: A qualitative study of the influence of trust and locus of control on postpartum contraceptive choice. J Health Commun 2018; 23(2): 162–9. [DOI] [PubMed] [Google Scholar]
- [31].Montgomery MR, Casterline JB. Social Learning, Social Influence, and New Models of Fertility. Population and Development Review 1996; 22(Supplement: Fertility in the United States: New Patterns, New Theories): 151–75. [Google Scholar]
- [32].Kincaid DL. Social networks, ideation, and contraceptive behavior in Bangladesh: a longitudinal analysis. Soc Sci Med 2000; 50(2): 215–31. [DOI] [PubMed] [Google Scholar]
- [33].Brunson EK. The impact of social networks on parents’ vaccination decisions. Pediatrics 2013; 131(5): e1397–e404. [DOI] [PubMed] [Google Scholar]
- [34].Zou G A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004; 159(7): 702–6. [DOI] [PubMed] [Google Scholar]
- [35].Comfort AB, Chankova S, Juras R, Hsi CN, Peterson LA, Hathi P. Providing free pregnancy test kits to community health workers increases distribution of contraceptives: results from an impact evaluation in Madagascar. Contraception 2016; 93(1): 44–51. [DOI] [PubMed] [Google Scholar]
- [36].Comfort AB, Juras RC, Bradley SEK, Ranjalahy Rasolofomanana J, Noeliarivelo Ranjalahy A, Harper CC. Do home pregnancy tests bring women to community health workers for antenatal care counselling? A randomized controlled trial in Madagascar. Health Policy Plann 2019; 34(8): 566–73. [DOI] [PubMed] [Google Scholar]
- [37].Perkins JM, Krezanoski P, Takada S, Kakuhikire B, Batwala V, Tsai AC, et al. Social norms, misperceptions, and mosquito net use: a population-based, cross-sectional study in rural Uganda. Malar J 2019; 18(1): 189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Perkins JM, Nyakato VN, Kakuhikire B, Mbabazi PK, Perkins HW, Tsai AC et al. Actual versus perceived HIV testing norms, and personal HIV testing uptake: a cross-sectional, population-based study in rural Uganda. AIDS Behav 2018; 22(2): 616–28. [DOI] [PMC free article] [PubMed] [Google Scholar]


