Abstract
Background
Various stressors during childhood and adulthood, such as experiencing poor parenting, abuse, and harassment, have long-lasting effects on depression. The long-term effects of childhood stressors, such as childhood abuse and inappropriate parenting experiences, on adult depression are mediated by personality traits. In the present study, we hypothesized that parental bonding in childhood influences adulthood depression, and that this association is mediated by childhood victimization experiences and negative life event evaluations in adulthood. To test this hypothesis, multiple regression analysis and structural equation modeling were performed.
Methods
A questionnaire survey, including Patient Health Questionnaire-9, victimization scale in childhood, Parental Bonding Instrument (PBI), and Life Experiences Survey was administered to 449 general adult volunteers (age: 41.1 ± 11.7 years; 196 men and 253 women). Multiple variables were analyzed by multiple regression analysis and structural equation modeling.
Results
Multiple regression analysis demonstrated that victimization experiences in childhood affect adulthood depression independently of several other factors. Structural equation modeling showed that the “parental care” subscale of the PBI decreased adulthood depression directly, as well as indirectly through its effects on victimization experiences in childhood and negative life events. On the other hand, the “parental overprotection” subscale of the PBI increased adulthood depression directly, as well as indirectly through its effects on the experience of victimization in childhood and negative life events.
Conclusion
The present study indicates that the experience of victimization in childhood is a risk factor of adulthood depression. Furthermore, we found that parenting quality experienced in childhood influences adulthood depression, and that these effects are mediated by the experiences of victimization in childhood and negative life events in adulthood.
Keywords: victimization, parental bonding, negative life event appraisal, depression, structural equation modeling
Introduction
Various stressors during childhood influence depressive symptoms and the development of major depression in adulthood.1–7 A retrospective study showed that childhood adversities, including serious family drinking problems, family mental illness, family violence, parental marital problems, and parental divorce increases the incidence and prevalence of major depression.1 Childhood abuse, including sexual abuse, punishment, and neglect are associated with depression in adulthood and its severity and consequences.3,4,6,7 Furthermore, a parenting style characterized by a lack of warmth and caring and by negative psychological control, ie, overprotection or affectionless control, has also been suggested to influence adulthood depression; ie, inadequate nurturing is partly analogous to neglect and is considered a form of childhood abuse.4,6 Because these previous studies had a cross-sectional design, and hence retrospectively evaluated childhood experiences, there is a possibility that the assessment of childhood abuse and parenting was confounded by the subject’s subsequent experiences and uncertain memory. However, long-term prospective studies have confirmed the long-term influence of adverse childhood experiences on depression.2,4–6
Stressful life events in adulthood trigger the onset of depression more quickly than childhood stress.8,9 Various types of stressors have been indicated as risk factors for depression, such as experiencing assault, financial problems, serious housing problems, serious illness or injury, legal problems, loss of confidant, serious marital problems, being robbed, and the death or serious illness of someone in the subject’s social network, etc.8 A prospective study showed that more severe stressful life events are more likely to cause major depression.10 More recently, large scale prospective studies reported that stressful life events in workplaces cause depression.11,12
The clinical question remains as to how childhood abuse and inappropriate parenting experiences influence, over long periods of time, the onset of depression in adulthood. Cross-sectional studies have suggested that the long-term effects of childhood stress, such as childhood abuse and inappropriate parenting experiences, on adult depression are mediated by various personality traits (eg, affective temperament, neuroticism, interpersonal sensitivity, self-esteem, and trait anxiety), which may answer this clinical question.13–20 Among these mediators of personality traits, prospective studies have demonstrated that neuroticism interacts with stressful life events in adulthood, and induces the onset of depression.9,10,21,22
Childhood maltreatment has also been reported to increase stress sensitivity in adulthood, both psychologically and biologically.23–25 As mentioned above, part of this effect is through personality traits, such as neuroticism.15,16 The negative appraisal of adult life events is associated with the development of depression.8–10,14,15 In addition, workplace harassment, one of the most common form of negative life events, has recently become a major social issue, and prospective research has demonstrated that workplace harassment is a risk factor for depression and a factor to change neuroticism in adulthood.11,12,26 Accordingly, some studies have demonstrated that adverse childhood experiences increase stress sensitivity by affecting personality traits, and in turn, adult stressors induce depression in combination with increased stress sensitivity.15,16,23–25,27
In addition to childhood maltreatment and parenting experiences, childhood bullying victimization in schools and communities is associated with depression, suicidality, and self-harm, according to a large prospective study.28–30 Interestingly, Lereya et al reported that children who are maltreated in childhood are more likely to be victimized by their peers, suggesting that there are common personal and family factors between maltreatment and bullying victimization.30 Although there have been some reports on the association between depression and victimization, few studies have analyzed the factors that mediate this association. Tachi et al focused on mediating factors, and found that victimization experiences in childhood affect the onset of depression in adulthood and the severity of depression in depressed and healthy individuals through their effects on neuroticism.31 In other words, the mediation of depressogenic effects by neuroticism is common in subjects who experienced victimization and maltreatment.16,31 It is also known that parenting quality affects victimization.32,33 Parenting quality influences personality development, as well as the negative evaluation of life events and adulthood depression.20,27 Therefore, the association between parenting quality, adult stress, and depression may be mediated by the childhood experience of victimization. However, it has not been reported as to how parenting quality experienced in childhood influences adulthood depression via victimization in childhood and life event appraisal in adulthood.
Several lines of evidence, as introduced above, have suggested the possible associations among childhood abuse and inappropriate parenting, bullying victimization in schools and communities, stressful life events in adulthood, and depression. However, these associations have not been fully clarified, and the previous studies were performed in different sociocultural contexts and with different study designs. Therefore, the associations among the above 4 factors should be studied simultaneously in the same context. In the present study, we hypothesized that parenting quality experienced in childhood influences adulthood depression, and that victimization in childhood and negative life event appraisal in adulthood mediates this effect. To confirm this hypothesis, we conducted a questionnaire survey on adult volunteers regarding their parenting experiences by the Parental Bonding Instrument (PBI), victimization during childhood by the assessment scale that we previously developed, negative life event appraisal by the Life Experiences Survey (LES), and depression by Patient Health Questionnaire-9 (PHQ-9). The associations among these 4 factors were analyzed by structural equation modeling.
Subjects and Methods
Subjects
Between April 2017 and April 2018, questionnaires and instructions of this study were distributed to 1237 adults by convenience sampling through our acquaintances at Tokyo Medical University. A total of 597 (48.3%) adult volunteers participated in this study. All participants provided informed consent to participate. The study was conducted by a paper-based survey. A total of 449 subjects (196 men and 253 women, mean age: 41.1 ± 11.7 years), excluding those with missing data, were analyzed. The inclusion criteria were (a) being 20 years or older, and (b) being capable of agreeing to study participation. The exclusion criteria were (a) having any severe physical illness, and (b) having any organic brain illness. The participants were informed that (a) participation in this study was voluntary, (b) no disadvantage would be caused to those who did not consent, (c) the data would be strictly controlled, and (d) personal information would be adequately managed. This study was part of a larger study, which analyzed the results of several questionnaires.34 The study was performed based on the Declaration of Helsinki (amended in Fortaleza in 2013) and was approved by the Institutional Review Board of Tokyo Medical University (study approval number: SH3502).
Questionnaires
This study was conducted using the participants’ answers to mainly 4 questionnaires, as well as demographic and clinical information, ie, age, sex, marital status, past history of psychiatric disease, current psychiatric treatment, living alone or not status, years of education, and employment status, as shown in Table 1.
Table 1.
Demographic Characteristics and PHQ-9, PBI, LES, and Other Data of 449 General Adult Volunteers and Their Effects on PHQ-9 Score
| Characteristic or Measure | Value (Mean ± SD or Number [%] of Subjects) | Effect on PHQ-9 Score (Mean ± SD, t-test) or Correlation with PHQ-9 Score (r) | |
|---|---|---|---|
| Age (years) | 41.1 ± 11.7 | r = 0.011, p = 0.812 | |
| Sex (male: female) | 196 (43.7%): 253 (56.3%) | Male: 3.4 ± 4.0 vs female: 4.7 ± 4.5, p = 0.03 (t-test) | |
| Marital status (married: single) | 305 (67.9%): 144 (32.0%) | Married: 3.6 ± 4.0 vs single: 5.2 ± 4.7, p = 0.561 (t-test) | |
| Past history of psychiatric disease (yes: no) | 46 (10.2%): 403 (89.8%) | Yes: 7.5 ± 5.7 vs no: 3.7 ± 3.9, p < 0.001 (t-test) | |
| Current psychiatric treatment (yes: no) | 16 (3.6%): 433 (96.4%) | Yes: 8.3 ± 5.6 vs no: 4.0 ± 4.2, p < 0.001 (t-test) | |
| Living alone (yes: no) | 93 (20.7%): 356 (79.3%) | Yes: 5.2 ± 4.9 vs no: 3.9 ± 4.1, p = 0.02 (t-test) | |
| Years of education | 14.7 ± 1.8 | r = –0.120, p = 0.011 | |
| Employment (yes: no) | 441 (98.2%): 8 (1.8%) | Yes: 4.1 ± 4.3 vs no: 3.3 ± 5.5, p = 0.56 (t-test) | |
| PHQ-9 score | 4.12 ± 4.29 | ||
| Victimization scale score | 2.31 ± 3.07 | r = 0.287, p < 0.001 | |
| LES (change score) | |||
| Negative | 1.83 ± 3.29 | r = 0.339, p < 0.001 | |
| Positive | 1.53 ± 2.58 | r = –0.11, p = 0.020 | |
| PBI score | |||
| Paternal care | 23.5 ± 8.5 | r = –0.189, p < 0.001 | |
| Paternal overprotection | 9.8 ± 7.0 | r = 0.220, p < 0.001 | |
| Maternal care | 28.0 ± 7.2 | r = –0.033, p < 0.001 | |
| Maternal overprotection | 9.7 ± 7.0 | r = 0.253, p < 0.001 | |
| Subjective social status score (1: lowest; 10: highest) | 5.1 ± 1.6 | r = –0.293, p < 0.001 | |
Notes: Values represent the number or mean ± standard deviation (SD). r = Pearson correlation coefficient.
Abbreviations: SD, standard deviation; PHQ-9, Patient Health Questionnaire-9; PBI, Parental Bonding Instrument; LES, Life Experiences Survey.
Patient Health Questionnaire-9 (PHQ-9)
The PHQ-9 is a self-report rating scale of 9 depression symptoms.35 The Japanese version was developed and validated by Muramatsu et al.36 The PHQ-9 is a questionnaire that evaluates the severity of depression experienced in the past 2 weeks, using the 4-point Likert scale. The total score was used in the present analysis.
Assessment Scale of Victimization in Childhood
The revised victimization scale of the National Institute for Educational Policy Research in Japan was used, as described in our previous study.31,37 In our previous study, the score of the victimization scale significantly correlated with neuroticism, having depression, and the severity of depressive symptoms.31 This scale is a self-report questionnaire that asks the frequency and degree of victimization of an individual in the community and school during childhood, using a 5-point Likert scale (0 to 4 points). The total score of the 5 items was regarded as the victimization score. A high score indicates a high degree of victimization. In the present study, Cronbach’s α coefficient calculated for this scale was 0.862, indicating very high internal consistency.
Parental Bonding Instrument (PBI)
The PBI is a self-rating scale of parenting quality, which assesses parental nurturing attitudes that a subject experienced during childhood.38 A Japanese version of the PBI was developed and validated by Kitamura and Suzuki.39 The PBI is divided into the “care” and “overprotection” subscales. The higher the score for “care”, the more appropriately a subject was nurtured by the parents (less indifference and rejection), and the higher the score for “overprotection” the more overprotective a subject’s parents were (less encouragement of independence). In the present study, the total score of each subscale for the fathers and mothers were summed, and the scores of the four items were used for analysis.
Life Experiences Survey (LES)
The LES is a scale that subjectively assesses a subject’s experiences in the previous year of 57 life events and their psychological impact (positive or negative).40 Rating is performed on a 7-point scale ranging from extremely negative (–3) to extremely positive (+3). Summing the impact ratings of the events designated as positive by the subject provides a positive change score. A negative change score is derived by summing the impact ratings of the events designated as negative by the subject. The Japanese version was developed and validated by Nakai et al.15 Positive and negative change scores were used in the analysis.
Data Analysis
The associations of demographic and questionnaire data with depression (PHQ-9) were determined by the Pearson correlation coefficient or Student’s t-test using SPSS Statistics 26.0J software (IBM, Armonk, NY, USA). In addition, multiple regression analysis was conducted using the forced entry method, with the PHQ-9 score as the dependent variable and the following 16 variables as independent variables: age, sex, education years, marital status, past history of psychiatric disease, current psychiatric treatment, living alone, employment status, subjective social status score (1: lowest; 10: highest), victimization score in childhood, negative and positive change scores of LES, PBI care scores of the fathers and mothers, and PBI overprotection scores of the fathers and mothers.
Based on the hypothesis presented in the Introduction section, the 2 structural equation models described below were created using PBI care or overprotection, victimization score in childhood, negative change score of LES, and PHQ-9 score. The dependent variable was the severity of depression assessed by the PHQ-9. Two latent variables, ie, “parental care” and “parental overprotection”, were created from the observed variables of the PBI subscales of care and overprotection received from the father and the mother.
Model 1: Childhood “care” influences the experience of victimization in childhood, which in turn influences adulthood depression directly and indirectly through negative evaluations of life events.
Model 2: Childhood “overprotection” influences the experience of victimization in childhood, which in turn influences adulthood depression directly and indirectly through negative evaluations of life events.
The Mplus 8.4 software (Muthén & Muthén, Los Angeles, CA, USA) was used for statistical analysis of the structural equation modeling, and covariance structure analysis with the robust maximum likelihood estimation method was performed. Two goodness-of-fit indices, namely, the Comparative Fit Index (CFI) and Root Mean Square Error Approximation (RMSEA), were used as goodness-of-fit indices for comprehensive judgment. If the CFI was greater than 0.95 and the RMSEA was lower than 0.08, the model was considered to be acceptable, and if the CFI was greater than 0.97 and the RMSEA was lower than 0.05, the model fit was considered to be a good fit.41
Results
Associations of Demographic Information and Questionnaire Data with Depression Scores
Table 1 shows the results of the associations between demographic and questionnaire data and PHQ-9 scores in 449 adult volunteers of the entire study population. Women, living alone, current psychiatric treatment, and past history of psychiatric diseases showed a significant association with high scores on PHQ-9. The victimization score in childhood and the negative change sore (LES) positively correlated with PHQ-9 scores, and the positive change score (LES) and years of education correlated negatively with PHQ-9 scores. Higher PBI care scores of the father and mother demonstrated an association with lower PHQ-9 scores. Higher PBI overprotection scores of the father and mother demonstrated an association with higher PHQ-9 scores. Higher subjective social status demonstrated an association with lower PHQ-9 scores.
Multiple Regression Analysis Using the Forced Entry Method with PHQ-9 as the Dependent Variable
Table 2 shows the results of multiple regression analysis using the forced entry method for total PHQ-9 score. PHQ-9 score was found to significantly correlate with LES negative change score (standardized partial regression coefficient β: 0.231), subjective social status (β: –0.167), maternal care (β: –0.156), victimization in childhood (β: 0.148), and past history of psychiatric disease (β: 0.132). The other 11 independent variables showed no statistically significant correlation. Multicollinearity was denied. This regression model explained 27.9% of the variability in PHQ-9 scores.
Table 2.
Results of Multiple Regression Analysis with PHQ-9 as the Dependent Variable (Forced Entry Method)
| Independent Variable | β | p-value | VIF |
|---|---|---|---|
| LES negative change score | 0.231 | 0.000 | 1.095 |
| Subjective social status score | –0.167 | 0.000 | 1.368 |
| Maternal care (PBI) | –0.156 | 0.014 | 2.503 |
| Victimization in childhood | 0.148 | 0.001 | 1.206 |
| Past history of psychiatry disease (yes: no) | 0.132 | 0.006 | 1.435 |
| Living alone (yes: no) | 0.098 | 0.064 | 1.737 |
| Current psychiatric treatment (yes: no) | 0.081 | 0.087 | 1.392 |
| Sex (male: female) | 0.079 | 0.069 | 1.159 |
| LES positive change score | –0.062 | 0.153 | 1.178 |
| Paternal care (PBI) | 0.051 | 0.374 | 2.017 |
| Paternal overprotection (PBI) | 0.038 | 0.528 | 2.231 |
| Maternal overprotection (PBI) | 0.027 | 0.666 | 2.457 |
| Age | –0.023 | 0.651 | 1.606 |
| Employment (yes: no) | 0.017 | 0.681 | 1.038 |
| Marital status (yes: no) | –0.014 | 0.797 | 1.682 |
| Years of education | 0.000 | 0.994 | 1.602 |
Notes: Adjusted R2 = 0.279. β, standardized partial regression coefficient. yes: 2, no: 1. Male: 1, female: 2.
Abbreviation: VIF, variance inflation factor.
Structural Equation Modeling
According to the results of univariable analyses and multiple regression analysis, PBI scores, LES negative change score, and victimization in childhood were significantly associated with adulthood depression. Furthermore, we analyzed the association between these 4 factors by structural equation modeling using the following 2 models described in the Methods section.
Model 1
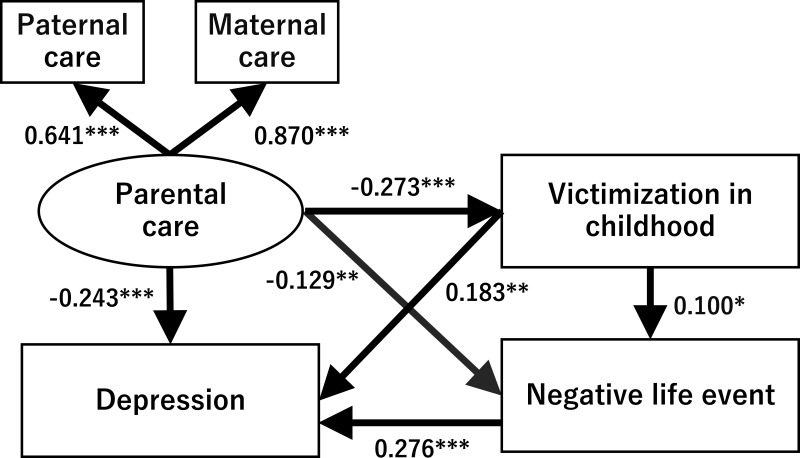
In Model 1, the PBI subscales of paternal care and maternal care as observed variables composed the latent variable of “parental care”. We analyzed a structural equation model using the robust maximum likelihood method, with “parental care”, victimization score in childhood, negative life events expressed as the LES negative change score, and depression expressed as the PHQ-9 score as variables (Figure 1). The goodness-of-fit of Model 1 was CFI = 0.998 and RMSEA = 0.023, which indicates a good fit. The standardized coefficient of “parental care” to “maternal care” was 0.870, which was greater than that from “parental care” to “paternal care”, which was 0.641.
Figure 1.
Results of the structural equation model with “parental care” as the latent variable. A structural equation model was created with the “parental care” subscale of the Parental Bonding Instrument, victimization in childhood, negative life events evaluated by the negative change score on the Life Experiences Survey, and depression evaluated by the Patient Health Questionnaire-9 score. The oval shows the latent variable, and rectangles show the observed variables. Solid arrows indicate statistically significant pathways. The numbers show the standardized path coefficients (–1 ≤ β ≤ 1). *p< 0.05, **p < 0.01, ***p< 0.001.
“Parental care” in childhood showed a significant negative effect on victimization in childhood, negative life events in adulthood, and adulthood depression (Figure 1, Table 3). In addition, victimization in childhood showed a significant positive effect on negative life events and depression. Negative life events also had a significant positive effect on depression.
Table 3.
Standardized Path Coefficients Between Each Variable and 95% Confidence Intervals in Model 1 of Parental Care
| Direct Effect on | |||
|---|---|---|---|
| From | Victimization | Negative Life Events | Depression |
| Parental care | −0.273*** (–0.415, –0.130) | −0.129** (–0.221, –0.036) | −0.243*** (–0.344, –0.142) |
| Victimization | 0.100* (0.020, 0.180) | 0.183** (0.070, 0.297) | |
| Negative life events | 0.276*** (0.176, 0.376) | ||
| Indirect Effect on | |||
| Via | Negative Life Events | Depression | |
| Parental care | Victimization | −0.027* (–0.053, –0.002) | −0.050** (–0.086, –0.014) |
| Negative life events | −0.035* (–0.063, –0.008) | ||
| Victimization + negative life events | −0.008 (–0.015, 0.000) | ||
| Victimization | Negative life events | 0.028* (0.003, 0.052) | |
Notes: *p < 0.05, **p < 0.01, ***p < 0.001. Numbers in parentheses indicate lower limits and upper limits of 95% confidence intervals.
Regarding indirect effects (Table 3), the indirect effect of “parental care” on negative life events via victimization in childhood was statistically significant (standardized path coefficient β = –0.027, p = 0.035). Furthermore, the indirect effect of “parental care” on depression via negative life events (β = –0.035, p = 0.012), that of “parental care” on depression through victimization in childhood (β = –0.050, p = 0.007), and that of victimization in childhood via negative life events on depression (β = 0.028, p = 0.027) were all statistically significant. On the other hand, the indirect effect of “parental care” on depression via victimization in childhood and negative life events was not statistically significant (β = –0.008, p = 0.053). The coefficient of determination of depression was 0.228, ie, this model accounts for 22.8% of the variability of depression.
Thus, these results demonstrate that “parental care” has a direct negative effect on adulthood depression, and also has an indirect negative effect on adulthood depression through victimization in childhood and negative life events.
Model 2
In Model 2, the PBI subscales of paternal overprotection and maternal overprotection as observed variables composed the latent variable of “parental overprotection”. We analyzed a structural equation model using the robust maximum likelihood method with “parental overprotection”, victimization in childhood, negative life events expressed by the LES negative change score, and depression expressed by the PHQ-9 score as variables (Figure 2). The goodness-of-fit of Model 2 was CFI = 1.000 and RMSEA = 0.000, indicating a good fit. The standardized coefficient of “parental overprotection” to “maternal overprotection” was 0.848, which was greater than that from “parental overprotection” to “paternal overprotection”, which was 0.698.
Figure 2.
Results of the structural equation model with “parental overprotection” as the latent variable. A structural equation model was created with the “parental overprotection” subscale of the Parental Bonding Instrument, victimization in childhood, negative life events evaluated by the negative change score on the Life Experiences Survey, and depression evaluated by the Patient Health Questionnaire-9 score. The oval shows the latent variable, and rectangles show the observed variables. Solid arrows indicate statistically significant pathways. Broken Arrows indicate statistically nonsignificant pathways. The numbers show the standardized path coefficients (–1 ≤ β ≤ 1). **p < 0.01, ***p < 0.001.
“Parental overprotection” showed a significant positive effect on victimization in childhood and adulthood depression, but the direct effect on negative life events in adulthood was not statistically significant (Figure 2, Table 4). In addition, victimization in childhood showed a significant positive effect on negative life events and depression. Negative life events also had a significant positive effect on depression.
Table 4.
Standardized Path Coefficients Between Each Variable and 95% Confidence Intervals in Model 2 of Parental Overprotection
| Direct Effect on | |||
|---|---|---|---|
| From | Victimization | Negative Life Events | Depression |
| Parental overprotection | 0.308*** (0.188, 0.427) | 0.091 (–0.004, 0.185) | 0.211*** (0.101, 0.320) |
| Victimization | 0.107** (0.027, 0.187) | 0.183** (0.065, 0.301) | |
| Negative life events | 0.288*** (0.189, 0.387) | ||
| Indirect Effect on | |||
| Via | Negative Life Events | Depression | |
| Parental overprotection | Victimization | 0.033* (0.005, 0.060) | 0.056** (0.018, 0.094) |
| Negative life events | 0.026 (–0.002, 0.054) | ||
| Victimization + negative life events | 0.009* (0.001, 0.018) | ||
| Victimization | Negative life events | 0.031* (0.005, 0.057) | |
Notes: *p < 0.05, **p < 0.01, ***p < 0.001. Numbers in parentheses indicate lower limits and upper limits of 95% confidence intervals.
Next, regarding indirect effects (Table 4), the indirect effect of “parental overprotection” on negative life events via victimization in childhood was statistically significant (standardized coefficient: β = 0.033, p = 0.019). Furthermore, the indirect effect of “parental overprotection” on depression via victimization in childhood (β = 0.056, p = 0.004), that of victimization in childhood on depression through negative life events (β = 0.031, p = 0.019), and that of “parental overprotection” on depression via victimization in childhood and negative life events (β = 0.009, p = 0.032) were all statistically significant. However, the indirect effect of “parental overprotection” on depression via negative life events was not statistically significant (β = 0.026, p = 0.067). The coefficient of determination of depression was 0.214, ie, this model accounts for 21.4% of the variability of depression.
Thus, these results demonstrate that “parental overprotection” has a direct positive effect on adulthood depression, and also has an indirect positive effect on adulthood depression through victimization in childhood and negative life events.
Discussion
In this study, multiple regression analysis showed that victimization in childhood, the quality of parenting experienced, negative life event appraisal in the previous year in adulthood, subjective social status, and past history of psychiatric disease were significantly associated with the severity of adulthood depression, independent of several factors. This suggests that victimization experiences in childhood directly increase adulthood depression independently of the influence of several possible confounders. The structural equation model demonstrated a chain reaction, in which the quality of parenting influenced victimization experiences in childhood, which in turn influenced adulthood depression through its impact on negative life event appraisal in adulthood. To the best of our knowledge, the present study reports for the first time that the experience of victimization in childhood is a mediating factor in the influence of parental nurturing experiences in childhood on adulthood depression.
First of all, in the present study, inadequate parenting increased the experience of victimization in childhood, which was consistent with the results of previous reports.32,33 A previous study reported that parenting is a significant predictor of victimization, and the effect of parenting style on victimization is mediated by peer attachment.33 Hence, the influence of parenting on peer attachment may account for increased victimization from peers. Furthermore, in the present study, inadequate parenting increased the appraisal of negative life events both directly and indirectly through victimization in childhood. Consistent with this finding, experiences of victimization and neglect have been reported to lead to negative life event appraisal in adulthood, which mediates the effects on functional impairment, generalized fear, and global distress.42 However, mediation by victimization has not been reported to date, and hence this study clarified for the first time the mediating associations among parenting, victimization, and negative life events in adulthood.
Earlier studies have reported that parenting quality and victimization in childhood play substantial roles in causing depression.4,20,27–30,43 Negative life event appraisal in adulthood may lead to the onset of depression and the worsening of depression.8,14,27 Consistent with these previous studies, the present study showed that 3 factors, ie, parenting quality, victimization in childhood, and negative life event appraisal in adulthood are all associated with depression in adult volunteers. Although the mediating effects of victimization in childhood, and negative life event appraisal in adulthood between parenting and depression have not been reported, negative life event appraisal in adulthood has been reported to mediate the effects of victimization on functional impairment, generalized fear, and global distress, indicating a similar type of mediating effect to that clarified in our present study.42
As discussed above, although there have been studies on the relationship between 2 of the above 4 factors (parenting quality experienced, victimization in childhood, negative life event appraisal, and depression), no studies have reported the association between the 4 factors in terms of their mediating effects. The present results suggest that the cascading and multifactorial effects of negative stress factors, such as parenting quality experienced, victimization in childhood, and subjective negative life events in adulthood, cause the onset of depression. As we described in the Introduction section, increased neuroticism as a common basis of these stress factors may link the 4 above factors, and may account for the mechanism of this chain reaction.16,26,27,31 Bondy et al suggested that neuroticism may promote vulnerability to stress-associated depression, and that sensitivity to stress-associated ventral striatum dysfunction may be a potential neural mechanism underlying vulnerability to stress-associated clinically significant depression.9 Future studies are needed to analyze the involvement of ventral striatum reward and neuroticism in this chain reaction.
The clinical implications of our findings are a warning for clinicians: clinicians should be aware that depression in individual patients are often associated with their experiences of poor parenting in childhood, victimization in childhood, and negative life events. Parker reported that parental bonding is associated with the pathogenesis of neurotic depression, in which psychological factors are considered to be primary factors in the induction of depression.43 In other words, in clinical practice, it is important to consider not only current stressors, but also the possibility that the experiences of poor parenting and victimization in childhood may have created vulnerable personality traits in a patient that amplify the effects of stress in adulthood. In fact, patients with depression often report experiences of inappropriate parenting, childhood abuse, childhood victimization, and stressful life events. Each of these factors should hence be identified before psychotherapeutic or psychiatric interventions are implemented.
One limitation of this study is that because it is a cross-sectional study, it is not possible to conclude the exact causal associations between the factors. In addition, because self-administered questionnaires asking the subject to recall childhood experiences were used, the effect of recall bias should be considered. In the future, a large-scale prospective study should be performed to analyze whether the effects of parenting experiences on adulthood depression are mediated by the experiences of victimization in childhood or negative life event evaluations. The number of women and men in this study were different, indicating another limitation that may have affected the results. It will also be necessary to analyze the mediating effects of neuroticism and other personality traits. These future studies will enable further elucidation of the mechanisms by which victimization causes depression.
Conclusions
In this study, we showed that the experience of victimization in childhood had an exacerbating effect on the depression of adult volunteers of a wide age range, independently of several demographic factors. Furthermore, we found that parenting quality experienced by subjects in childhood influenced their adulthood depression, and that these effects were mediated by experiences of victimization in childhood and negative life event appraisal in adulthood. A good parent-child bond is expected to reduce the likelihood of experiencing victimization in childhood, improve personality development, and reduce negative life event appraisal and stress perceptions, and thereby reduce adulthood depression.
Acknowledgments
We thank Dr. Nobutada Takahashi of Fuji Psychosomatic Rehabilitation Institute Hospital, Dr. Hiroshi Matsuda of Kashiwazaki Kosei Hospital, Dr. Yasuhiko Takita (deceased) of Maruyamasou Hospital, and Dr. Yoshihide Takaesu of Izumi Hospital for their collection of subject data. We thank Dr. Helena Popiel of the Department of International Medical Communications, Tokyo Medical University, for editorial review of the manuscript.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by Takeshi Inoue, without undue reservation.
Author Contributions
Conceptualization: Yoshitaka Ishii, Chihiro Morishita, Motoki Higashiyama, Takeshi Inoue.
Data curation: Yoshitaka Ishii, Chihiro Morishita, Motoki Higashiyama, Takeshi Inoue.
Formal analysis: Yoshitaka Ishii, Takeshi Inoue.
Investigation: Yoshitaka Ishii, Takeshi Inoue, Jiro Masuya.
Methodology: Yoshitaka Ishii, Takeshi Inoue.
Project administration: Yoshitaka Ishii, Jiro Masuya, Masahiko Ichiki, Takeshi Inoue.
Supervision: Jiro Masuya, Masahiko Ichiki, Motoki Higashiyama, Takeshi Inoue.
Validation: Yoshitaka Ishii, Chihiro Morishita, Jiro Masuya, Masahiko Ichiki, Motoki Higashiyama, Takeshi Inoue.
Writing – original draft: Yoshitaka Ishii, Chihiro Morishita, Jiro Masuya, Masahiko Ichiki, Motoki Higashiyama, Takeshi Inoue.
Writing – review & editing: Yoshitaka Ishii, Chihiro Morishita, Jiro Masuya, Masahiko Ichiki, Motoki Higashiyama, Takeshi Inoue.
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Jiro Masuya has received personal compensation from Otsuka Pharmaceutical, Eli Lilly, Astellas, and Meiji Yasuda Mental Health Foundation, and grants from Pfizer. Takeshi Inoue has received personal fees from Mochida Pharmaceutical, Takeda Pharmaceutical, Eli Lilly, Janssen Pharmaceutical, MSD, Taisho Toyama Pharmaceutical, Yoshitomiyakuhin, and Daiichi Sankyo; grants from Shionogi, Astellas, Tsumura, and Eisai; and grants and personal fees from Otsuka Pharmaceutical, Dainippon Sumitomo Pharma, Mitsubishi Tanabe Pharma, Kyowa Pharmaceutical Industry, Pfizer, Novartis Pharma, and Meiji Seika Pharma; and is a member of the advisory boards of Pfizer, Novartis Pharma, and Mitsubishi Tanabe Pharma. Masahiko Ichiki has received personal compensation from Otsuka Pharmaceutical, Pfizer, Eli Lilly, Mitsubishi Tanabe Pharma, Mochida Pharmaceutical, Meiji Seika Pharma, Janssen Pharmaceutical, Takeda Pharmaceutical Company, MSD, Dainippon Sumitomo Pharma, and Eisai; grants from Otsuka Pharmaceutical, Eli Lilly, Eisai, Shionogi, Takeda Pharmaceutical, MSD, and Pfizer; and is a member of the advisory board of Meiji Seika Pharma. The other authors declare that they have no actual or potential conflicts of interest associated with this study.
References
- 1.Kessler RC, Magee WJ. Childhood adversities and adult depression: basic patterns of association in a US national survey. Psychol Med. 1993;23:679–690. doi: 10.1017/S0033291700025460 [DOI] [PubMed] [Google Scholar]
- 2.Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386–389. doi: 10.1126/science.1083968 [DOI] [PubMed] [Google Scholar]
- 3.Chapman DP, Whitfield CL, Felitti VJ, et al. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82(2):217–225. doi: 10.1016/j.jad.2003.12.013 [DOI] [PubMed] [Google Scholar]
- 4.Alloy LB, Abramson LY, Smith JM, Gibb BE, Neeren AM. Role of parenting and maltreatment histories in unipolar and bipolar mood disorders: mediation by cognitive vulnerability to depression. Clin Child Fam Psychol Rev. 2006;9:23–64. doi: 10.1007/s10567-006-0002-4 [DOI] [PubMed] [Google Scholar]
- 5.Li M, D’Arcy C, Meng X. Maltreatment in childhood substantially increases the risk of adult depression and anxiety in prospective cohort studies: systematic review, meta-analysis, and proportional attributable fractions. Psychol Med. 2016;46:717–730. doi: 10.1017/S0033291715002743 [DOI] [PubMed] [Google Scholar]
- 6.Nemeroff CB. Paradise lost: the neurobiological and clinical consequences of child abuse and neglect. Neuron. 2016;89:892–909. doi: 10.1016/j.neuron.2016.01.019 [DOI] [PubMed] [Google Scholar]
- 7.Ng QX, Yong BZJ, Ho CYX, Lim DY, Yeo WS. Early life sexual abuse is associated with increased suicide attempts: an update meta-analysis. J Psychiatr Res. 2018;99:129–141. doi: 10.1016/j.jpsychires.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 8.Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry. 1999;156(6):837–841. doi: 10.1176/ajp.156.6.837 [DOI] [PubMed] [Google Scholar]
- 9.Bondy E, Baranger DAA, Balbona J, et al. Neuroticism and reward-related ventral striatum activity: probing vulnerability to stress-related depression. J Abnorm Psychol. 2021;130:223–235. doi: 10.1037/abn0000618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am J Psychiatry. 2004;161(4):631–636. doi: 10.1176/appi.ajp.161.4.631 [DOI] [PubMed] [Google Scholar]
- 11.Lange S, Burr H, Rose U, et al. Workplace bullying and depressive symptoms among employees in Germany: prospective associations regarding severity and the role of the perpetrator. Int Arch Occup Environ Health. 2020;93(4):433443. doi: 10.1007/s00420-019-01492-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rugulies R, Sørensen K, Aldrich PT, et al. Onset of workplace sexual harassment and subsequent depressive symptoms and incident depressive disorder in the Danish workforce. J Affect Disord. 2020;277:21–29. doi: 10.1016/j.jad.2020.06.058 [DOI] [PubMed] [Google Scholar]
- 13.Kanai Y, Takaesu Y, Nakai Y, et al. The influence of childhood abuse, adult life events, and affective temperaments on the well-being of the general, nonclinical adult population. Neuropsychiatr Dis Treat. 2016;12:823–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Toda H, Inoue T, Tsunoda T, et al. Affective temperaments play an important role in the relationship between childhood abuse and depressive symptoms in major depressive disorder. Psychiatry Res. 2016;236:142–147. doi: 10.1016/j.psychres.2015.12.016 [DOI] [PubMed] [Google Scholar]
- 15.Nakai Y, Inoue T, Toda H, et al. The influence of childhood abuse, adult stressful life events and temperaments on depressive symptoms in the nonclinical general adult population. J Affect Disord. 2014;158:101–107. doi: 10.1016/j.jad.2014.02.004 [DOI] [PubMed] [Google Scholar]
- 16.Ono K, Takaesu Y, Nakai Y, et al. Associations among depressive symptoms, childhood abuse, neuroticism, and adult stressful life events in the general adult population. Neuropsychiatr Dis Treat. 2017;13:477–482. doi: 10.2147/NDT.S128557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hayashi Y, Okamoto Y, Takagaki K, et al. Direct and indirect influences of childhood abuse on depression symptoms in patients with major depressive disorder. BMC Psychiatry. 2015;15:244. doi: 10.1186/s12888-015-0636-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uchida Y, Takahashi T, Katayama S, et al. Influence of trait anxiety, child maltreatment, and adulthood life events on depressive symptoms. Neuropsychiatr Dis Treat. 2018;14:3279–3287. doi: 10.2147/NDT.S182783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higashiyama M, Hayashida T, Sakuta K, et al. Complex effects of childhood abuse, affective temperament, and subjective social status on depressive symptoms of adult volunteers from the community. Neuropsychiatr Dis Treat. 2019;15:2477–2485. doi: 10.2147/NDT.S209100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hayashida T, Higashiyama M, Sakuta K, et al. Subjective social status via mediation of childhood parenting is associated with adulthood depression in non-clinical adult volunteers. Psychiatry Res. 2019;274:352–357. doi: 10.1016/j.psychres.2019.02.061 [DOI] [PubMed] [Google Scholar]
- 21.Kendler KS, Gardner CO. A longitudinal etiologic model for symptoms of anxiety and depression in women. Psychol Med. 2011;41(10):2035–2045. doi: 10.1017/S0033291711000225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kendler KS, Gardner CO. Sex differences in the pathways to major depression: a study of opposite-sex twin pairs. Am J Psychiatry. 2014;171(4):426–435. doi: 10.1176/appi.ajp.2013.13101375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Betz LT, Penzel N, Rosen M, et al. Relationships between childhood trauma and perceived stress in the general population: a network perspective. Psychol Med. 2020. doi: 10.1017/S003329172000135X [DOI] [PubMed] [Google Scholar]
- 24.Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol Psychiatry. 2001;49(12):1023–1039. doi: 10.1016/S0006-3223(01)01157-X [DOI] [PubMed] [Google Scholar]
- 25.LoPilato AM, Zhang Y, Pike M, et al. Associations between childhood adversity, cognitive schemas and attenuated psychotic symptoms. Early Interv Psychiatry. 2021;15(4):818–827. [DOI] [PubMed] [Google Scholar]
- 26.Persson R, Høgh A, Grynderup MB, et al. Relationship between changes in workplace bullying status and the reporting of personality characteristics. J Occup Environ Med. 2016;58(9):902–910. doi: 10.1097/JOM.0000000000000822 [DOI] [PubMed] [Google Scholar]
- 27.Ono Y, Takaesu Y, Nakai Y, et al. The influence of parental care and overprotection, neuroticism and adult stressful life events on depressive symptoms in the general adult population. J Affect Disord. 2017;217:66–72. doi: 10.1016/j.jad.2017.03.058 [DOI] [PubMed] [Google Scholar]
- 28.Takizawa R, Maughan B, Arseneault L. Adult health outcomes of childhood bullying victimization: evidence from a five-decade longitudinal British birth cohort. Am J Psychiatry. 2014;171(7):777–784. doi: 10.1176/appi.ajp.2014.13101401 [DOI] [PubMed] [Google Scholar]
- 29.Bowes L, Joinson C, Wolke D, et al. Peer victimisation during adolescence and its impact on depression in early adulthood: prospective cohort study in the United Kingdom. BMJ. 2015;350:h2469. doi: 10.1136/bmj.h2469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lereya ST, Copeland WE, Costello EJ, et al. Adult mental health consequences of peer bullying and maltreatment in childhood: two cohorts in two countries. Lancet Psychiatry. 2015;2(6):524–531. doi: 10.1016/S2215-0366(15)00165-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tachi S, Asamizu M, Uchida Y, et al. Victimization in childhood affects depression in adulthood via neuroticism: a path analysis study. Neuropsychiatr Dis Treat. 2019;15:2835–2841. doi: 10.2147/NDT.S220349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van der Watt R. Attachment, parenting styles and bullying during pubertal years. J Child Adolesc Ment Health. 2014;26(3):251–261. doi: 10.2989/17280583.2014.947966 [DOI] [PubMed] [Google Scholar]
- 33.Charalampous K, Demetriou C, Tricha L, et al. The effect of parental style on bullying and cyber bullying behaviors and the mediating role of peer attachment relationships: a longitudinal study. J Adolesc. 2018;64:109–123. doi: 10.1016/j.adolescence.2018.02.003 [DOI] [PubMed] [Google Scholar]
- 34.Seki T, Shimura A, Miyama H, et al. Influence of parenting quality and neuroticism on perceived job stressors and psychological and physical stress response in adult workers from the community. Neuropsych Dis Treat. 2020;16:2007–2015. doi: 10.2147/NDT.S260624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737 [DOI] [PubMed] [Google Scholar]
- 36.Muramatsu K, Miyaoka H, Kamijima K, et al. The patient health questionnaire, Japanese version: validity according to the mini-international neuropsychiatric interview-plus. Psychol Rep. 2007;101(3 Pt 1):952–960. [DOI] [PubMed] [Google Scholar]
- 37.National Institute for Educational Policy Research in Japan. Ijime follow-up research 2010-2012. Tokyo: National Institute for Educational Policy Research in Japan; 2013. Available from: https://www.nier.go.jp/shido/centerhp/2507sien/ijime_research-2010-2012.pdf. Accessed October 4, 2021. [Google Scholar]
- 38.Parker G, Tupling H, Brown LB. A parental bonding instrument. Br J Med. 1979;52:1–10. [Google Scholar]
- 39.Kitamura T, Suzuki T. A validation study of the parental bonding instrument in a Japanese population. Jpn J Psychiatry Neurol. 1993;47(1):29–36. [DOI] [PubMed] [Google Scholar]
- 40.Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the life experiences survey. J Consult Clin Psychol. 1978;46(5):932–946. doi: 10.1037/0022-006X.46.5.932 [DOI] [PubMed] [Google Scholar]
- 41.Schermelleh-Engel K, Moosbrugger H. Evaluating the fit of structural equation model: tests of significance and descriptive goodness-of-fit measures. MPR Online. 2003;8:23–74. [Google Scholar]
- 42.Sweeting JA, Garfin DR, Holman EA, et al. Associations between exposure to childhood bullying and abuse and adulthood outcomes in a representative national U.S. sample. Child Abuse Negl. 2020;101:104048. doi: 10.1016/j.chiabu.2019.104048 [DOI] [PubMed] [Google Scholar]
- 43.Parker G. Parental ‘affectionless control’ as an antecedent to adult depression. A risk factor delineated. Arch Gen Psychiatry. 1983;40(9):956–960. doi: 10.1001/archpsyc.1983.01790080038005 [DOI] [PubMed] [Google Scholar]