Escalation of support
Central Message.
Acute respiratory distress syndrome after cardiopulmonary bypass can be managed with veno-venous extracorporeal membrane oxygenation.
Acute respiratory distress syndrome (ARDS) encountered during the course of cardiothoracic (CT) surgery is a rare (1.1% incidence) unfortunate event increasing both morbidity and mortality.1,2 Cardiogenic shock occurring during CT surgery can contribute to lung dysfunction, which may compound or overlap pure respiratory pathophysiology. Supportive care strategies are numerous and varied but, with the exception of low tidal-volume ventilation, lack clear evidence demonstrating a survival benefit in randomized controlled trials.
Overview
The CT surgery patient presents a unique set of challenges not encountered in the nonsurgical ARDS population. Many of the supportive therapies may already have been applied, would have minimal benefit, or are impractical. When ARDS occurs in the CT surgery patient, standard approaches to ARDS are challenging. The ability to tolerate lung protective ventilation with permissive hypercapnia if right ventricular function is poor and the ability to prone due to fresh sternotomy are 2 key components of ARDS management that pose unique challenges in critical CT surgery patients. Inhaled nitric oxide or prostacyclin may improve oxygenation to some degree but may increase the risk of renal dysfunction.3 Transfusions to increase oxygen-carrying capacity are reasonable but must be weighed against the benefits of a fluid-restrictive strategy. Although transfusion and restrictive fluid strategies are not necessarily mutually exclusive, this strategy can pose a challenge. Any transfusion is associated with infectious and immunologic risk as well as with worsening ARDS (ie, transfusion-related acute lung injury and transfusion-associated circulatory overload). Pharmacologic decongestive strategies, such as diuretics, risk causing increased serum creatinine and acute kidney injury, leading to the need for extracorporeal treatments such as hemodialysis or continuous veno-venous (VV) hemofiltration. Low tidal volume ventilation does provide a survival benefit; however, the resultant effect on blood gases might not be sustainable in patients with severe hypoxemia.
Extracorporeal membrane oxygenation (ECMO) is an invasive rescue option that can be deployed in the operating room, catheterization laboratory, or intensive care unit (Figure 1). Although both studies have limitations, the CESAR4 and the EOLIA5 trials have suggested patient benefits from the use of ECMO for severe ARDS.
Figure 1.
Escalation of rescue therapies for acute respiratory distress syndrome. ARDS, Acute respiratory distress syndrome; VV, veno-venous; ECMO, extracorporeal membrane oxygenation; RV, right ventricle; VA, veno-arterial.
Pathophysiology of Postcardiotomy ARDS
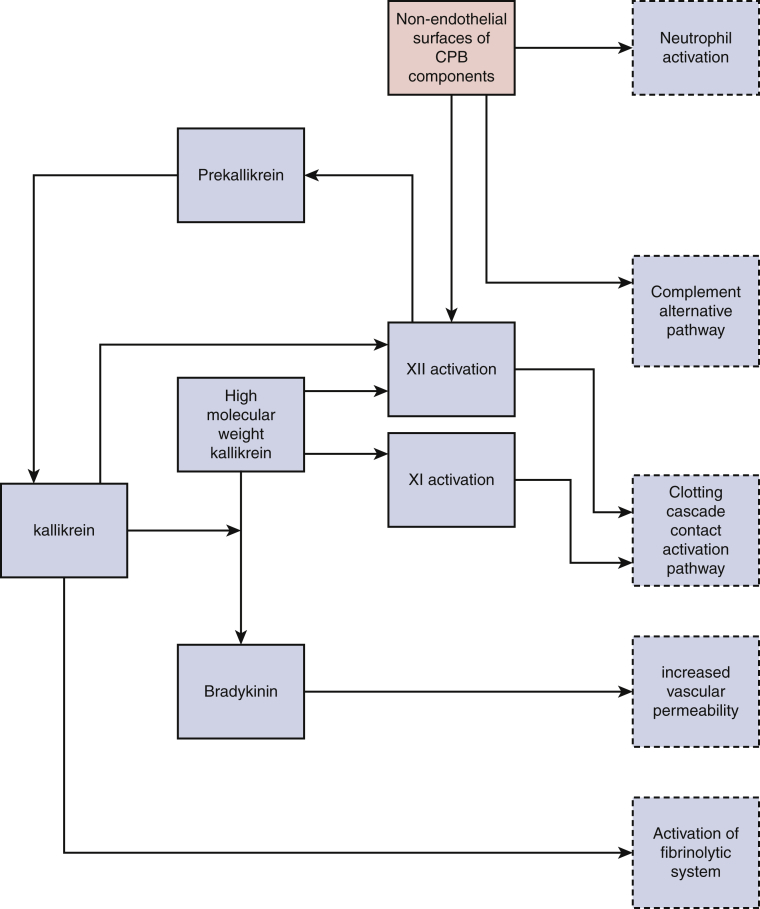
Given the proper circumstances, numerous pathways can lead to lung injury in the CT surgery patient (Figure 2). Cardiopulmonary bypass (CPB) can be a potent contributor to inflammation (Table 1). Nonendothelial negatively charged surfaces that blood encounters extracorporeally activate factor XII and complement protein C3b, which up-regulates multiple humoral pathways. During CPB, both right atrial and left atrial neutrophil levels increase. After aortic cross-clamp removal, right atrial neutrophil levels continue to increase, but left atrial levels decrease (ie, lung trapping). Thiobarbituric acid (indicative of lipid peroxidation oxygen free radical production) shows the same phenomenon.6
Figure 2.
Inflammatory pathways of cardiopulmonary bypass (CPB). Nonendothelial surfaces of CPB components activate multiple inflammatory pathways.
Table 1.
CPB-related and non–CPB-related risk factors for lung injury
| CPB-related | Non–CPB-related |
|---|---|
|
|
CPB, Cardiopulmonary bypass; FEV1, reduced forced expiration in 1 second; DLCO, diffusion capacity of the lung for carbon monoxide; ROS, reactive oxygen species; TRALI, transfusion-related acute lung injury.
Elimination of CPB does not remove all potential stimuli of lung injury. Numerous risk factors are intrinsic to any CT operation, and some may preexist in the patient before surgery (Table 1).
Preventive Strategies
Preservation of pleural integrity and off-pump coronary artery bypass grafting are surgical alternatives that may reduce the risk of lung complications. Institutional efforts to decrease blood transfusion during cardiac surgery have been successful.7 Techniques to reduce the time on CPB may be of use.
Indications for ECMO and Risk Assessment
Application of ECMO postcardiotomy for ARDS should incorporate risk assessment and appropriate indications. However, when using ECMO in a postcardiotomy ARDS setting, appropriate use will depend largely on institutional standards that have been established preoperatively. The most important indication for ECMO especially in the postoperative CT patient is reversibility of disease. Understanding that successful lung recovery after VV ECMO for CPB is dependent on reasonable lung function before cardiac surgery, as ideally determined by pulmonary lung function studies. The lung injury is likely secondary to the prolonged CPB and/or ischemic time in addition to other confounding factors, such as numerous blood product transfusions. Contraindications to ECMO generally pertain to futility of support (Table 2). Relative contraindications should be evaluated on a case-by-case basis.
Table 2.
Contraindications to ECMO support8
| Absolute contraindication | Relative contraindication |
|---|---|
| ICH/irreversible brain injury | ESRD, emphysema, cirrhosis |
| Refusal of blood products | Advanced age |
| Untreatable metastatic cancer | MV longer than 7 d pre-ECMO |
| Unrecoverable organ dysfunction coupled with noncandidacy for transplant or MCS | Severe aortic insufficiency |
| Lactate >20 mmol/L or suggestion of unrecoverable pre-ECMO injury |
ECMO, Extracorporeal membrane oxygenation; ICH, intracranial hemorrhage; ESRD, end-stage renal disease; MV, mechanical ventilation; MCS, mechanical circulatory support.
Mechanical ventilation is the standard of care for the hypoxemic patient. In severe lung injury, mechanical ventilation might not be sufficient to improve hypoxia and/or hypercapnia. Extended periods of mechanical ventilation can potentially injure the lungs, worsening the clinical situation.
VV ECMO improves oxygenation and helps prevent end-organ dysfunction.9 The 2 most recent randomized clinical trials of ECMO for ARDS suggested a survival benefit.6,7 Indications for ECMO include (1) refractory hypoxia and/or hypercapnia on maximal ventilatory settings, and (2) liberation from detrimental ventilatory settings. ECMO should be considered in a patient with a mortality risk >50%, Murray score ≥2.5, or P/F ratio (ie, arterial oxygen partial pressure to fractional inspired oxygen) <100.10 Patients have the best chance for a successful outcome with VV ECMO when it is instituted early in the course of ARDS, ideally within the first 24 to 48 hours.
Rescue Measures: A Practical Approach
“Exclusion and escalation” is the best approach to the CT surgery patient in respiratory distress. Therapy should be the least invasive necessary to obtain the desired results (Figure 3). The lowest level of exclusion eliminates such problems as mucous plugging by suction or bronchoscopy and checking for migration or torsion of the endotracheal tube. Second, albuterol, gentle recruitment maneuvers, and changes to ventilator mode and pressure/volume settings should be considered. Third, inhaled nitric oxide or epoprostenol are reasonable early interventions. If respiratory failure is noted intraoperatively, there is also utility in transitioning from an anesthesia machine ventilator to a more advanced ventilator from the intensive care unit. CPB can be used as a temporary rescue measure to avoid hypoxia while determining the best course of action, but it also can be the culprit and perpetuate the problem.
Figure 3.
Decision making flowchart for postcardiotomy acute respiratory distress syndrome (ARDS). VV, Veno-venous; VA, veno-arterial; ECMO, extracorporeal membrane oxygenation; RIJ, right internal jugular vein; LIJ, left internal jugular vein; fem, femoral; PCC, prothrombin complex concentrate; IV, intravenous; Qb, blood flow; ASA, aspirin; PTT, partial thromboplastin time.
After initiation of mechanical ventilation, inhaled nitric oxide or epoprostenol, and other interventions, if there remains only minimal improvement in oxygenation, consideration and institution ECMO is reasonable and prudent. The threshold, or level of hypoxia–hypercapnia, that a medical ARDS patient can tolerate most often will be higher than that of the surgical CT patient. The merits of avoiding ECMO must be weighed against the very real danger of hypoxia leading to cardiac, renal, gastrointestinal, and neurologic complications postoperatively.
Cannulation Strategies and Initial Management
After exclusion of non-ARDS factors and stepwise escalation of therapy, some patients will require ECMO (Figure 3). For this group, our preferred means of support is VV ECMO. This configuration is usually achieved with right internal jugular dual-lumen cannula; however, some patients will have ARDS in the setting of right heart failure and will require veno-arterial (VA) ECMO, which can be accomplished centrally or peripherally. A potential alternative to VA ECMO for right ventricular support is a right ventricular assist device with an oxygenator (oxy-RVAD) introduced either surgically via the femoral vein to the pulmonary artery or percutaneously with a ProtekDuo cannula (LivaNova, London, United Kingdom). Ideally, closure of the patient's chest is the best scenario to prevent sternal wound infection, mediastinitis, wean the ventilator, and ambulate while on VV ECMO and/or oxy-RVAD.
A dual-site cannulation involving the right internal jugular vein and the right femoral vein can be used in situations with limited imaging. When it is not expedient to access the neck, a return cannula may be placed alternatively in the contralateral femoral vein.
Ventilator pressures and volumes would transition to “rest settings”: low tidal volume, low airway pressure, low ventilator fraction of inspired oxygen (FiO2), and low respiratory rate. We recommend adding a daily low-dose aspirin (81 mg). For VV ECMO, we recommend no anticoagulation.8
The barotraumatic mechanics of cyclical expansion and deflation of the lungs at high pressure and volume are most deleterious. Time acts as an amplifier. As such, tidal volume and peak pressures should be minimized. When doing so, protective and ultraprotective volumes should be deployed, ranging between 4 and 6 mL/kg and between 2 and 4 mL/kg, respectively. To this end, we endorse a simple strategy of decreasing FiO2 to 30% with a pressure support of 10 cmH2O and a positive end-expiratory pressure of 10 cmH2O.
Special Considerations
Lung transplantation
Lung transplantation remains the best strategy for treating patients with end-stage lung disease when no other medical or surgical therapeutic options are available. Although most transplantations are performed in patients with gradually progressive pulmonary disease, an increasing number of patients are either presenting with severe or rapidly progressive disease or deteriorating while on the waitlist. Bridging strategies incorporating ECMO are valuable in providing an approach to get these patients to transplantation.11, 12, 13, 14 Although early studies reflect that the use of ECMO pretransplantation was associated with greater perioperative risk and worse outcomes, more recent work has shown that advances in ECMO technology, patient selection, and management have led to improved outcomes in these patients.15,16
The ideal ECMO modality is considered after establishing that the patient is deemed an appropriate lung transplantation candidate and is suitable for an ECMO bridge-to-transplantation (BTT) procedure. The approach will depend on the underlying disease, patient characteristics, and, as importantly, the multidisciplinary ECMO and transplantation team's experience. As a BTT, the chosen method should allow for the patient to be mobilized and ambulated.17
VV ECMO is the most common modality for candidates with hypercapnic, hypoxemic, or combined respiratory failure without significant right heart dysfunction.18,19 In patients with respiratory failure along with significant right heart strain or dysfunction from pulmonary hypertension, VV ECMO often cannot provide adequate support. For this cohort of patients, an oxy-RVAD, VA ECMO, or a pulmonary artery–to–left atrium circuit may be used.20
A crucial component for ECMO as a BTT is an aggressive and intensified physical therapy program. Patients who are immobile and require sedation and mechanical ventilation while on ECMO are at increased risk for delirium and critical care neuropathy and myopathy and have a high post-transplantation mortality rate.21, 22, 23 Most large ECMO centers have multidisciplinary teams that have developed successful awake and ambulatory programs.
ECMO as a BTT plays a vital role in providing transplantation to critically ill patients with end-stage lung disease. Priorities for successful outcomes post-transplantation include careful patient selection, adequate clinical infrastructure with an experienced multidisciplinary team, and the ability for ambulation.
ECMO has proven essential in the perioperative and postoperative management of selected patients after lung transplantation. In some cohorts, ECMO has been shown to improve overall outcomes.
ECMO is implemented primarily for 2 different purposes. It serves as a rescue therapy to salvage grafts in those patients who develop severe early graft dysfunction, either very early with the development of primary graft dysfunction (PGD) or later due to acute rejection or pneumonia, and in patients with severe PGD when lung protective strategies cannot fully support ventilatory and oxygen requirements. VA ECMO is initiated when there is hemodynamic instability (ie, severe post-transplantation pulmonary hypertension). In such cases, VA ECMO can be used to protect against hyperperfusion of the graft.24,25
The second major use of ECMO post-transplantation is in patients requiring continuation of intraoperative ECMO into the postoperative period. This use should be considered pretransplantation in, for example, patients deemed at particularly high risk of developing PGD, such as those with pulmonary arterial hypertension. In patients with pulmonary arterial hypertension, intraoperative ECMO that continues through the postoperative period may allow for the left ventricle to adapt to the new hemodynamic conditions post-transplantation.26
Determination of the optimal type of platform, patient selection, timing of implementation of ECMO perioperatively and postoperatively, and weaning strategies continue to evolve as our experience increases with this therapy.
Anticoagulation management
Providers managing patients undergoing ECMO must face the formidable challenge of balancing bleeding and thrombosis. Anticoagulation can limit thrombus formation but, due to the altered physiological effects of ECMO, may lead to unintentional bleeding, especially in patients who underwent recent cardiac surgery including CPB. Commonly encountered bleeding catalysts include clotting factor deficiency, acquired von Willebrand syndrome,27 and thrombocytopenia.
Historically, unfractionated heparin has been the most commonly used anticoagulant in ECMO patients, and activated clotting time has been the most common test used to measure effect. Other frequently used tests include activated partial thromboplastin time (aPTT), anti-Xa level, and viscoelastic assays. Although heparin has been used extensively to provide anticoagulation to patients on ECMO, we have transitioned to direct thrombin inhibitors (DTIs) when anticoagulation is required, because of lower rates of transfusion and thrombotic events.28
DTIs, such as argatroban and bivalirudin, bind to the catalytic site and to the anion-binding exosite of circulating and clot-bound thrombin.29,30 DTIs may provide a better risk profile for bleeding than heparin.31 We feel that aPTT-guided bivalirudin dosing to 40 to 50 seconds coupled with daily aspirin represents the best compromise to avoid both bleeding and thrombotic events. We also would advocate for maintaining platelet counts >75 K/μL and fibrinogen >200 mg/dL in all VV ECMO patients regardless of anticoagulation regimen.
Alternatively, it is possible to forgo systemic anticoagulation in VV ECMO patients.32, 33, 34 Centers contemplating eliminating systemic anticoagulation should first clarify (1) surface coatings of ECMO components currently in use, (2) an acceptable minimum blood flow rate, and (3) adjunctive anticoagulants in use. Our preference for VV ECMO is ECMO components with biocompatibility surface coatings, minimal blood flow >3 LPM (preferably 4 LPM), 81 mg aspirin once daily, and no systemic anticoagulation. For VA ECMO when bleeding has decreased to <200 mL/hour per chest tube for 6 hours, we recommend starting bivalirudin to achieve an aPTT of 40 to 60 seconds.
Weaning off ECMO is initiated when arterial blood gas results improve at rest settings. FiO2 and sweep gas of the oxygenator are reduced while ventilator FiO2 remains ≤60% with a tidal volume ≥4 mL/kg and peak inspiratory pressure ≤35 mL H2O. Following a 24-hour period of zero gas flow to the oxygenator with partial pressure of CO2 ≤50 and arterial O2 saturation ≥90%, when a patient can demonstrate the ability to be off VV ECMO, the patient is then decannulated.
Conclusions
VV ECMO is an important tool in the armamentarium of the CT physician, providing rescue therapy for CT surgery patients burdened with ARDS. When used in conjunction with a lung-protective ventilation strategy, it can be beneficial for the CT surgery patient who is also affected by ARDS, refractory pneumonia, or severe refractory acute lung injury and/or as a bridge to lung transplantation. Postoperative CT surgery patients can be supported well and extubated, and they may be able to ambulate as they recover or await lung transplantation.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
References
- 1.Weissman C. Pulmonary complications after cardiac surgery. Semin Cardiothorac Vasc Anesth. 2004;8:185–211. doi: 10.1177/108925320400800303. [DOI] [PubMed] [Google Scholar]
- 2.Kogan A., Segel M.J., Ram E., Raanani E., Peled-Potashnik Y., Levin S., et al. Acute respiratory distress syndrome following cardiac surgery: comparison of the American-European consensus conference definition versus the Berlin definition. Respiration. 2019;97:518–524. doi: 10.1159/000495511. [DOI] [PubMed] [Google Scholar]
- 3.Munshi L., Adhikari N.K.J. Inhaled nitric oxide and acute kidney injury: new insights from observational data. Crit Care. 2017;21:83. doi: 10.1186/s13054-017-1651-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peek G.J., Mugford M., Tiruvoipati R., Wilson A., Allen E., Thalanany M.M., et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374:1351–1363. doi: 10.1016/S0140-6736(09)61069-2. [DOI] [PubMed] [Google Scholar]
- 5.Combes A., Hajage D., Capellier G., Demoule A., Lavoué S., Guervilly C., et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378:1965–1975. doi: 10.1056/NEJMoa1800385. [DOI] [PubMed] [Google Scholar]
- 6.Sladen R.N., Berkowitz D.E. In: Cardiopulmonary Bypass Principles and Practice. Gravlee G.P., Davis R.F., Utley J.R., editors. Williams & Wilkins; Baltimore: 1993. Cardiopulmonary bypass and the lung; pp. 468–487. [Google Scholar]
- 7.Brevig J., McDonald J., Zelinka E.S., Gallagher T., Jin R., Grunkemeier G.L. Blood transfusion reduction in cardiac surgery: multidisciplinary approach at a community hospital. Ann Thorac Surg. 2009;87:532–539. doi: 10.1016/j.athoracsur.2008.10.044. [DOI] [PubMed] [Google Scholar]
- 8.New York Presbyterian Contraindications to ECMO. https://www.nyp.org/ecmo-program/for-physicians-carf/contraindications-to-ecmo Accessed February 5, 2021. Available at:
- 9.Durinka J.B., Bogar L.J., Hirose H., Brehm C., Koerner M.M., Pae W.E., et al. End-organ recovery is key to success for extracorporeal membrane oxygenation as a bridge to implantable left ventricular assist device. ASAIO J. 2014;60:189–192. doi: 10.1097/MAT.0000000000000043. [DOI] [PubMed] [Google Scholar]
- 10.Del Sorbo L., Fan E. In: Extracorporeal Life Support: The ELSO Red Book. 5th ed. Brogan T., Lequier L., Lorusso R., MacLaren G., Peek G., editors. Extracorporeal Life Support Organization; Ann Arbor, MI: 2017. Chapter 37 Indications and contraindications for ECLS in adults with respiratory failure; pp. 415–427. [Google Scholar]
- 11.Hakim A.H., Ahmad U.A., McCurry K.R., Johnston D.R., Pettersson G.B., Budev M., et al. Contemporary outcomes of extracorporeal membrane oxygenation used as bridge to lung transplantation. Ann Thorac Surg. 2018;106:192–198. doi: 10.1016/j.athoracsur.2018.02.036. [DOI] [PubMed] [Google Scholar]
- 12.Biscotti M., Sonett J., Bacchetta M. ECMO as bridge to transplant. Thorac Surg Clin. 2015;25:17–25. doi: 10.1016/j.thorsurg.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 13.Hayanga A.J., Hayanga H.K., Holmes S.D., Ren Y., Shigemura N., Badhwar V., et al. Mechanical ventilation and extracorporeal membrane oxygenation as a bridge to lung transplantation: closing the gap. J Heart Lung Transplant. 2019;38:1104–1111. doi: 10.1016/j.healun.2019.06.026. [DOI] [PubMed] [Google Scholar]
- 14.Ius F., Tudorache I., Warnecke G. Extracorporeal support, during and after lung transplantation: the history of an idea. J Thorac Dis. 2018;10:5131–5148. doi: 10.21037/jtd.2018.07.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoopes C.W., Kukreja J., Golden J., Davenport D.L., Diaz-Guzman E., Zwischenberger J.B. Extracorporeal membrane oxygenation as a bridge to pulmonary transplantation. J Thorac Cardiovasc Surg. 2013;145:862–867. doi: 10.1016/j.jtcvs.2012.12.022. discussion 867-8. [DOI] [PubMed] [Google Scholar]
- 16.Hayanga A.J., Du A.L., Joubert K., Tuft M., Baird R., Pilewski J., et al. Mechanical ventilation and extracorporeal membrane oxygenation as a bridging strategy to lung transplantation: significant gains in survival. Am J Transplant. 2018;18:125–135. doi: 10.1111/ajt.14422. [DOI] [PubMed] [Google Scholar]
- 17.Hämmäinen P., Schersten H., Lemström K., Riise G.C., Kukkonen S., Swärd K., et al. Usefulness of extracorporeal membrane oxygenation as a bridge to lung transplantation: a descriptive study. J Heart Lung Transplant. 2011;30:103–107. doi: 10.1016/j.healun.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 18.Abrams D., Brodie D., Arcasoy S.M. Extracorporeal life support in lung transplantation. Clin Chest Med. 2017;38:655–666. doi: 10.1016/j.ccm.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 19.Hayanga A.J., Aboagye J., Esper S., Shigemura N., Bermudez C.A., D'Cunha J., et al. Extracorporeal membrane oxygenation as a bridge to lung transplantation in the United States: an evolving strategy in the management of rapidly advancing pulmonary disease. J Thorac Cardiovasc Surg. 2015;149:291–296. doi: 10.1016/j.jtcvs.2014.08.072. [DOI] [PubMed] [Google Scholar]
- 20.Downey P., Ragalie W., Gudzenko V., Ardehali A. Ambulatory central veno-arterial extracorporeal membrane oxygenation in lung transplant candidates. J Heart Lung Transplant. 2019;38:1317–1319. doi: 10.1016/j.healun.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Fuehner T., Kuehn C., Hadem J., Wiesner O., Gottlieb J., Tudorache I., et al. Extracorporeal membrane oxygenation in awake patients as bridge to lung transplantation. Am J Respir Crit Care Med. 2012;185:763–768. doi: 10.1164/rccm.201109-1599OC. [DOI] [PubMed] [Google Scholar]
- 22.Rehder K.J., Turner D.A., Hartwig M.G., Williford W.L., Bonadonna D., Walczak R.J., Jr., et al. Active rehabilitation during extracorporeal membrane oxygenation as a bridge to lung transplantation. Respir Care. 2013;58:1291–1298. doi: 10.4187/respcare.02155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Polastri M., Loforte A., Dell'Amore A., Nava S. Physiotherapy for patients on awake extracorporeal membrane oxygenation: a systemic review. Physiother Res Int. 2016;21:203–209. doi: 10.1002/pri.1644. [DOI] [PubMed] [Google Scholar]
- 24.Bermudez C.A., Adusumilli P.S., McCurry K.R., Zaldonis D., Crespo M.M., Pilewski J.M., et al. Extracorporeal membrane oxygenation for primary graft dysfunction after lung transplantation: long-term survival. Ann Thorac Surg. 2009;87:854–860. doi: 10.1016/j.athoracsur.2008.11.036. [DOI] [PubMed] [Google Scholar]
- 25.Hartwig M.G., Walczak R., Lin S.S., Davis R.D. Improved survival but marginal allograft function in patients treated with extracorporeal membrane oxygenation after lung transplantation. Ann Thorac Surg. 2012;93:366–371. doi: 10.1016/j.athoracsur.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 26.Moser B., Jaksch P., Taghavi S., Muraközy G., Lang G., Hager H., et al. Lung transplantation for idiopathic pulmonary arterial hypertension on intraoperative and post operatively prolonged extracorporeal membrane oxygenation provides optimally controlled reperfusion and excellent outcome. Eur J Cardiothorac Surg. 2018;53:178–185. doi: 10.1093/ejcts/ezx212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kalbhenn J., Schlagenhauf A., Rosenfelder S., Schmutz A., Zieger B. Acquired von Willebrand syndrome and impaired platelet function during venovenous extracorporeal membrane oxygenation: rapid onset and fast recovery. J Heart Lung Transplant. 2018;37:985–991. doi: 10.1016/j.healun.2018.03.013. [DOI] [PubMed] [Google Scholar]
- 28.Rivosecchi R.M., Arakelians A., Ryan J., Murray H., Ramanan R., Gomez H., et al. Comparison of anticoagulation strategies in patients requiring venovenous extracorporeal membrane oxygenation: heparin versus bivalirudin. Crit Care Med. 2021;49:1129–1136. doi: 10.1097/CCM.0000000000004944. [DOI] [PubMed] [Google Scholar]
- 29.Sandoz Canada Inc Argatroban prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/022485lbl.pdf Accessed November 22, 2020. Available at:
- 30.The Medicines Company Angiomax prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/020873s036lbl.pdf Accessed November 22, 2020. Available at:
- 31.Ranucci M., Ballotta A., Kandil H., Isgrò G., Carlucci C., Baryshnikova E., et al. Bivalirudin-based versus conventional heparin anticoagulation for postcardiotomy extracorporeal membrane oxygenation. Crit Care. 2011;15:R275. doi: 10.1186/cc10556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kurihara C., Walter J.M., Karim A., Thakkar S., Saine M., Odell D.D., et al. Feasibility of venovenous extracorporeal membrane oxygenation without systemic anticoagulation. Ann Thorac Surg. 2020;110:1209–1215. doi: 10.1016/j.athoracsur.2020.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fina D., Matteucci M., Jiritano F., Meani P., Kowalewski M., Ballotta A., et al. Extracorporeal membrane oxygenation without systemic anticoagulation: a case-series in challenging conditions. J Thorac Dis. 2020;12:2113–2119. doi: 10.21037/jtd.2020.04.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carter K.T., Kutcher M.E., Shake J.G., Panos A.L., Cochran R.P., Creswell L.L., et al. Heparin-sparing anticoagulation strategies are viable options for patients on veno-venous ECMO. J Surg Res. 2019;243:399–409. doi: 10.1016/j.jss.2019.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]