Abstract
Background
The aim of this study was to adapt and modify the HIV/AIDS Stigma Instrument-Patient to develop the COVID-19 Stigma Instrument-Patient (CSI-P) and validate its psychometric characteristics, as well as explore how affected individuals in China experienced COVID-related stigma and its associated variables, including depressive symptomology and quality of life (QOL).
Methods
From September to October 2020, 151 COVID-19 survivors recruited in Shanghai, China, completed a set of measures of demographic characteristics, depression, stigma, and QOL.
Results
The 15-item CSI-P-2 achieved a Cronbach's α of 0.67 to 0.91. The six-factor structure was obtained by exploratory factor analysis. The mean score for the CSI-P-2 in Chinese COVID survivors was 8.14 ± 9.98. Regression analysis showed that survivors' age, comorbid diseases, education levels, and loneliness level were the factors influencing their COVID-19 stigma, explaining 37.80% of the total variance (F = 19.25, p < 0.001). Also, stigma's effect on QOL was significant in direct and indirect paths mediated by depressive symptomology.
Limitations
First, this sample might limit the generalization of the findings to other Chinese-speaking regions. Second, future longitudinal or experimental studies are warranted for checking and further refinement of the scale. Finally, future studies are needed on the changing dynamics of stigma in different stages of the pandemic.
Conclusions
The 29-item CSI-P-2 with six domains is an instrument with sound psychometric properties that can be used to measure COVID-19 stigma during the COVID-19 outbreak and, later, for COVID-19 survivors. Future studies should explore how to integrate the significant demographic and psychological characteristics influencing the experience of stigma work on this study into the development of stigma-reducing interventions.
Keywords: COVID-19, Stigma, Survivors, Psychometrics, Survey, Influencing factors
1. Introduction
As the number of affected people and deaths due to the novel coronavirus 2019 (COVID-19) has risen, the stigma associated with having COVID-19 has been identified as a significant barrier to controlling its transmission (Imran et al., 2020). Longstanding research on infectious diseases, such as HIV, tuberculosis, and severe acute respiratory syndrome (SARS), indicates that stigma is experienced by those affected by infectious diseases both directly and indirectly, such as survivors, family members, and healthcare providers (Roelen et al., 2020). Indeed, stigmatization is mounting against those infected with or having survived COVID, as well as those in proximity to people with COVID, e.g., health workers and family members (Imran et al., 2020; Muhidin, et al., 2020). For example, Cassiani-Miranda et al. (2020) found that 42.3% of the general Colombian population stigmatize COVID-19 patients and 35.4% view COVID health care providers as “not clean.” Dar et al. (2020) found that 98% of COVID-19 survivors in India reported that they experienced stigma, mainly enacted and perceived externalized stigma (Dar et al., 2020). Although some empirical evidence on COVID-associated stigma of survivors indicated that stigma is a prominent issue among patients with COVID-19 (Cassiani-Miranda et al., 2020; Dar et al., 2020; Duan et al., 2020), most existing instruments currently being used to measure COVID stigma were self-made questionnaires or adapted measures from existing stigma questionnaires of infectious diseases (e.g., HIV, tuberculosis, Ebola) and lack reports of important psychometric indexes (Cassiani-Miranda et al., 2020; Dar et al., 2020; Duan et al., 2020). To our best knowledge, there is currently no validated instrument used to measure COVID-associated stigma experienced by COVID-19 patients. Consequently, efforts to explore how affected individuals experience COVID-19 stigma and associated variables will be limited (Peprah and Gyasi, 2020; Ransing et al., 2020).
As described by the Health Stigma and Discrimination Framework (HSDF), the unaddressed stigma may cause severe consequences both for individuals and society (Stangl et al., 2019). It is well documented that being stigmatized is very likely to impede individuals' health-seeking behavior and access to healthcare and social services, undermine their treatment adherence, and lead to social exclusion, mental distress, violence (in some cases), and decreased quality of life (QOL; Roelen et al., 2020; Stangl et al., 2019). Previous HIV studies confirmed that stigma is associated with mental health (e.g., depressive symptoms) and QOL (Chan et al., 2020; Charles et al., 2012; Rao et al., 2012); however, there is still a lack of understanding as to how stigma, depression, and QOL interact among COVID-19 patients. For affected areas and countries, the stigma can cause economic loss, regional discrimination, and racism (Duan et al., 2020), and also hamper the effects of disease containment strategies, leading to elevated risks for community transmission, excessive safety hazards for healthcare workers, and overwhelmed local healthcare systems (Jenkins et al., 2020). Such an unsupportive environment could further fuel harmful stereotypes and undermine social cohesion (Abdelhafiz and Alorabi, 2020). Therefore, considering the screening of stigma among COVID-19 survivors, exploring the pathway between stigma, depression, and QOL, and later, designing interventions to overcome this crisis is essential (Muhidin et al., 2020).
To reduce COVID-19-associated stigma and its potential consequences, a reliable and valid measure to measure COVID-19-associated stigma is urgently needed. Considering that similar stigma conditions have been experienced by individuals with other infectious diseases (Logie, 2020), in this paper, we aim to: (1) adapt and modify the HIV/AIDS Stigma Instrument-Patient (HASI-P) to develop the COVID-19 Stigma Instrument-Patient (CSI-P) and validate its psychometric characteristics, (2) describe the COVID-19-associated stigma experienced by COVID survivors and its influencing factors in Shanghai, China, and (3) explore the pathway between stigma, depressive symptoms, and QOL, for which we hypothesize that depressive symptoms mediate the relationship between stigma and QOL.
2. Methods
2.1. Study design
This cross-sectional, descriptive study was conducted in Shanghai, China, from September to October 2020. The study was conducted in two phases. In Phase I, we adapted and modified the HASI-P (Holzemer et al., 2007) into the CSI-P and examined the psychometric properties of the CSI-P in ways adherent to the COnsensus-based Standards for the selection of health status Measurement INstruments (COSMIN) checklist (Mokkink et al., 2010a, 2010b). In Phase II, we conducted a cross-sectional survey to describe the current status of the COVID-19 stigma perpetrated and experienced by COVID-19 patients to identify the factors associated with the stigma and the pathway between stigma, depressive symptoms, and QOL. The survey and analysis were conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (von Elm E et al., 2014).
3. Participants
A list of 890 eligible patients was obtained from the discharged COVID-19 patients records of the treating hospital. By using a computer-generated random number, we contacted the person with that number on the discharge list. This process was repeated until the target number of participants was achieved, at which point, we stopped the recruitment. When the research staff contacted these potential participants, we screened them for the inclusion criteria, which were: (a) oral confirmation that the person on the phone or texting was a COVID-19 patient on the institution's list; (b) recovered from COVID-19 and returned home at least 14 days previously, (c) willing to participate in the survey, and (d) at least 18 years old. Patients were excluded from the study if they were unable to complete the Chinese questionnaire or had severe impairment in their physical or mental functions. If they agreed to participate and were able to provide informed consent, an individualized survey link was sent to them via WeChat (A free cell phone application similar to text messaging). After completing the survey, participants were reimbursed for their participation and time.
4. Data collection
Phase I: Instrument Adaptation, Modification, and Validation
The HASI-P has 33 items and six factors, including verbal abuse, negative self-perception, healthcare neglect, social isolation, fear of contagion, and workplace stigma. Items were rated on a 4-point Likert scale ranging from 0 (never) to 3 (most of the time). Higher scores indicate greater stigmatization experienced by patients. The HASI-P presented with good reliability, and its overall Cronbach's alpha reliability was 0.94. A significant negative correlation between stigma, quality of life, and life satisfaction was further supported by the concurrent validity of the HASI-N (Holzemer et al., 2007).
We adapted and modified the HASI-P into the CSI-P in the following steps:
Step 1-Modification: We replaced “HIV/AIDS” with “COVID-19” on the scale.
Step 2-Translation: We applied Brislin's translation model to the cross-cultural translation, including translation, back-translation, comparison, and linguistic adaption (Brislin, 1970; Jones et al., 2001). First, a bilingual nurse who provided infectious disease care in China independently translated the 33-item HASI-P from English into Chinese. Then, a bilingual researcher back-translated the Chinese version into English. Later, a third member of the research team compared the back-translated English version with the original English scale. One item change was made to ensure that the back-translated English version did not differ from the original instrument. That is, the Chinese phrase" 有人试图把我解雇" ("Someone tried to fire me") in item 20 was replaced with" 有人试图让我没工作". This process yielded Chinese Version 1 of the CSI-P (CSI-P-1).
Step 3-Pilot test: An individual phone-based cognitive interview was conducted with 15 of the eligible Chinese COVID-19 patients to explore their thoughts on items of the fluency, readability, and comprehensibility of the CSI-P-Version 1. None of the participants reported confusion or incomprehension regarding the items of the scale.
Step 4-Psychometric test: We examined the psychometric properties of the scale by CTT analysis according to the recommendations in the COSMIN checklist (Terwee et al., 2012). After item analysis, we removed four items (I-12, I-13, I-28, and I-29) and generated the final 29 items of CSI-P-2 (see Appendix A).
Phase II: Cross-sectional survey
For this anonymous cross-sectional survey, we invited 450 COVID-19 patients to participant in the survey, and 151 patients (33.56%) agreed and completed the questionnaires on the popular Chinese online survey platform, Wenjuanxing (aka Questionnaire Star (QS), which is similar to Survey Monkey). We shared the QS code or the URL of the CSI-P-1 by WeChat (https://www.wenjuan.in/s/aiuaMfj/). Eligible patients independently completed the 20-minute online survey that consisted of standardized measures to assess demographics, the CSI-P-2, the Veterans Short Form (VR-12; Chen, et al., 2013), the depression subscale of the Hospital Anxiety and Depression scale (HADS; Ye and Xu, 1993), and the 10-item UCLA-Loneliness Scale (LS; in this study, the overall Cronbach's α in this sample was 0.89; Knight et al., 1988).
The HADS contains 14 items for anxiety and depression. In this study, the depression subscale was used, which is scored from 0 to 21, with higher scores indicating more severe depression symptoms. The Chinese version of HADS has been validated (Ye and Xu, 1993). In this study, the Cronbach's α coefficients for the overall scale was 0.895. The VR-12 (Chen et al., 2013), a 12-item health survey, was used to describe physical and mental health-related quality of life. Scores on the Physical Component Summary (PCS) and Mental Component Summary (MCS) of the VR-12 are standardized with a mean of 50 and a standard deviation of 10; scores range from 0 to 100, with higher scores denoting better physical health and mental health, respectively. In this study, the overall Cronbach's α in this sample was 0.76. The sociodemographic variables included participants’ age, gender, marital status, working status, educational levels, whether they had health insurance, and comorbid diseases.
5. Ethical considerations
This research was approved by the relevant institutional review boards (IRB#20–000832 and YZ-2020-S037–01).
6. Statistical analyses
Data analyses were conducted using SPSS 23.0 (IBM, Chicago, IL, USA) and AMOS 23.0 (IBM, Chicago, IL), with p < 0.05 considered as significant. We replaced missing data using full information maximum likelihood.
6.1. Statistical analysis of Phase I
A). Item analysis: We deleted the item if it met the following criteria of CTT analysis: (1) cross-loading or factor loading < 0.4, and (2) the alpha coefficient for the overall scale was increased after item deletion (Johnson et al., 2011).
After item analysis, we analyzed the reliability and validity of the CSI-P-2, as follows.
B). Structural validity: We used the exploratory factor analysis (EFA) to assess the structural validity of the scale. Principal component analysis (PCA) and Promax oblique rotation were used. The number of factors was determined by parallel analysis (Johnson et al., 2011).
C). Construct validity: We estimated the convergent validity of the CSI-P-2 by calculating Pearson's correlations among the CSI-P-2, the depression subscale of the HADS, the LS, and the VR-12.
D). Reliability was estimated by Cronbach's α and composite reliability (Johnson et al., 2011).
6.2. Statistical analysis of Phase II
The data met the assumptions of normality, as one-sample Kolmogorov-Smirnov tests were not statistically significant. Continuous variables were expressed as means and standard deviations (SDs), and categorical variables were expressed as proportions or percentages. We performed independent t-tests and one-way analyses of variance (ANOVAs) to identify differences in the COVID-19 stigma score among patients. In additon, we conducted Pearson's correlation analyses to examine the relationships among age, the depression subscale score of the HADS, the VR-12 score, the LS score, and the COVID-19 stigma score. Then, we conducted multiple linear stepwise regression to determine the influencing factors associated with COVID-19 stigma for the patients. Multicollinearity was assessed with the variance inflation factor. Categorical variables (e.g., marital status, working status) were recoded into dummy variables for the multiple linear regression analysis. Lastly, we applied the bootstrap method (repeated 1000 times) to obtain stable and valid standard errors of the estimates of the direct and indirect effects of these factors in relationships among stigma, depressive symptoms, and QOL. Standardized regression coefficient (β) and p values for β of direct, indirect, and total effects were identified and reported by path analysis.
7. Results
7.1. Sample characteristics
A total of 151 patients responded to the survey, 56.30% (85/151) of whom were male. The mean age of patients was 34.26 years (SD = 13.60), and 70.9% (107/151) of them had health insurance. Only four patients (2.6%) were still taking hormones, and only one patient (0.7%) was still taking antibiotics. Twenty-nine (19.21%) patients experienced some kind of COVID-related symptom (e.g., snivels, stuffiness, cough, dyspnea, diarrhea, loss of taste, weakness of limbs, fatigue). The other socio-demographic characteristics of the patients are presented in Table 1 .
Table 1.
Sociodemographic characteristics of the COVID-19 patients (N = 151).
| Variables | N (%) | Total scores | t /F value | P value |
|---|---|---|---|---|
| Gender | ||||
| Male | 85 (56.30%) | 8.16 ± 10.47 | 0.04 | 0.97 |
| Female | 66 (43.70%) | 8.11 ± 9.40 | ||
| Marital status | ||||
| Single | 68 (45.00%) | 5.49 ± 7.44 | 3.41 | 0.02 |
| Married | 75(49.70%) | 10.31 ± 11.57 | ||
| Divorced | 5 (3.30%) | 7.60 ± 5.18 | ||
| Widowed | 3 (2.0%) | 15.00 ± 11.27 | ||
| Educational level | ||||
| Middle school degree | 26 (17.20%) | 14.19 ± 14.78 | 4.88 | 0.003 |
| High school or associate's degree | 39 (25.80%) | 8.38 ± 8.47 | ||
| Bachelor's degree | 63 (41.70%) | 6.76 ± 8.62 | ||
| Master's or doctoral degree | 23 (15.30%) | 4.65 ± 6.06 | ||
| Working status | ||||
| Full time | 75 (49.70%) | 6.12 ± 7.76 | 3.23 | 0.04 |
| Part time | 9 (6.00%) | 6.11 ± 7.98 | ||
| No | 67 (44.40%) | 10.19 ± 11.54 | ||
| Health insurance | ||||
| No | 107 (70.90%) | 10.43 ± 11.11 | 1.82 | 0.07 |
| Yes | 44 (29.10%) | 7.20 ± 9.38 | ||
| Comorbid diseases | ||||
| No | 120 (79.5%) | 15.55 ± 12.90 | 3.83 | 0.00 |
| Yes | 31 (20.5%) | 6.23 ± 8.11 |
7.2. Psychometric properties of the CSI-P-2
7.2.1. Item retention
According to the criteria for item retention, four items (I-12, I-13, I-28, and I29) were removed for cross-loading.
7.2.2. Structural validity
The Bartlett test of sphericity indicated that the sample was adequate for factor analysis (χ2 = 2659.75, df = 406, p < 0.001; Kaiser-Meyer-Olkin = 0.812). Six factors were extracted with an eigenvalue of 1.14 to 9.13, together explaining 66.15% of the overall variance. Factor loadings for all items were between 0.40 and 0.89 (see Table 2 ). According to the original structure of the HASI-P, the six factors of CSI-P were labeled (a) verbal abuse, (b) negative self-perception, (c) healthcare neglect, (d) social isolation, (e) fear of contagion, and (f) workplace stigma. The comparison of item distribution between the HASI-P and CSI-P are shown in Appendix A.
Table 2.
Factor structure of the CSI-P scale.
| Items | Factors |
|||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| I-17 People cut down visiting me. | 0.87 | |||||
| I-16 People avoided me. | 0.79 | |||||
| I-18 People ended their relationships with me. | 0.74 | |||||
| I-8 A friend would not chat with me. | 0.69 | |||||
| I-7 Someone stopped being my friend. | 0.52 | |||||
| I-26 At the hospital/clinic, I was made to wait until last. | 0.89 | |||||
| I-24 I was discharged from the hospital while still needing care |
0.81 | |||||
| I-27 At the hospital, I was left in a soiled bed. | 0.81 | |||||
| I-25 I was shuttled around instead of being helped by a nurse. |
0.66 | |||||
| I-23 I was refused treatment because I was told I was going to die anyway. |
0.64 | |||||
| I-22 I was denied health care. | 0.51 | |||||
| I-33 I felt that I am no longer a person. | 0.74 | |||||
| I-31 I felt completely worthless. | 0.70 | |||||
| I-30 I felt ashamed of having this disease. | 0.59 | |||||
| I-32 I felt that I brought a lot of trouble to my family. | 0.52 | |||||
| I-1 I was told to use my own eating utensils. | 0.82 | |||||
| I-6 I was asked to leave because I was coughing. | 0.71 | |||||
| I-3 I was made to drink last from the cup. | 0.57 | |||||
| I-4 Someone mocked me when I passed by. | 0.52 | |||||
| I-14 I was made to eat alone. | 0.49 | |||||
| I-5 I stopped eating with other people. | 0.40 | |||||
| I-21 My employer denied me opportunities. | 0.81 | |||||
| I-20 Someone tried to get me fired from my job. | 0.80 | |||||
| I-11 I was told that I have no future. | 0.65 | |||||
| I-9 I was called bad names. | 0.77 | |||||
| I-10 People sang offensive songs when I passed by. | 0.66 | |||||
| I-15 Someone insulted me. | 0.52 | |||||
| I-19 I was blamed for my COVID status. | 0.47 | |||||
| Eigenvalue | 9.13 | 3.10 | 2.30 | 2.10 | 1.41 | 1.14 |
| Cumulative percentages | 31.48 | 42.18 | 50.12 | 57.34 | 62.21 | 66.15 |
7.2.3. Convergent validity
Pearson's correlation analysis showed that the total CSI-P-2 score was significantly negatively correlated with the physical domain of the VR-12 (r = -0.23, p < 0.01) and positively correlated with the anxiety, depressive symptoms, and loneliness levels (r = 0.46, 0.42, &0.37, p < 0.01).
7.2.4. Reliability
The CSI-P-2 achieved a Cronbach's α of 0.91 (each subscale: 0.67–0.88) and a composite reliability of 0.96 (each subscale: 0.70–0.87).
7.3. COVID-19 stigma scores of the participants
The total mean scores for the CSI-P-2 among the Chinese COVID-19 survivors was 8.14 ± 9.98 (range 0–52) overall. As for domains, the highest three scores were fear of contagion (2.99 ± 4.21, range 0–19), social isolation (2.05 ± 3.10, range 0–14), and negative self-perception (1.32 ± 1.87, range 0–9). The lowest three scores were healthcare neglect (0.42 ± 1.53, range 0–12), workplace stigma (0.46 ± 1.16, range 0–6), and verbal abuse (0.9 ± 1.66, range 0–9). The mean score for each item is shown in Appendix 1.
7.4. Factors associated with COVID-19 stigma of the patients
Pearson's analysis results showed that age is significantly correlated with the COVID-19 stigma score (r = 0.25, p < 0.05). As shown in Table 1, participants’ marital status, working status, educational levels, and comorbid diseases were significantly associated with the total stigma score (p < 0.05), while other socio-demographic variables showed no statistical significance (p > 0.05).
Thus, in the regression analysis, the COVID-19 stigma score was the dependent variable and the statistical significance of participants’ age, marital status, working status, educational levels, comorbid diseases, anxiety, depressive symptoms, and loneliness scores were selected as independent variables (p < 0.05). Stepwise regression analysis showed that participants' age, comorbid diseases, education levels, anxiety, and loneliness levels were the factors influencing survivors' COVID-19 stigma, explaining 37.80% of the total variance (F = 19.25, p < 0.001; see Table 3 ). The variance inflation factor for all factors was below the value of 2.1.
Table 3.
Multivariable linear regression analysis results for total score.
| Independent variables in the model | Adjusted regression coefficient (β) | Standard error | t | P value | 95% confidence interval |
||
|---|---|---|---|---|---|---|---|
| Lower limit | Upper limit | ||||||
| Constant | 4.14 | .03 | .98 | -8.06 | 8.30 | ||
| Anxiety score | 0.31 | 0.21 | 4.17 | .00 | 0.46 | 1.28 | |
| Comorbid diseases | No | Ref | |||||
| Yes | 0.24 | 1.72 | 3.43 | .00 | 2.50 | 9.29 | |
| Age | 0.22 | 0.05 | 3.15 | .00 | 0.06 | 0.27 | |
| Loneliness score | 0.20 | 0.12 | 2.75 | .00 | 0.09 | 0.57 | |
| Education level | -0.14 | 0.47 | 2.15 | .03 | -1.96 | -0.08 | |
Adjusted R2 = 37.80%, F = 19.25, p < 0.001.
7.4.1. Mediating effect analysis
The results suggest that stigma, depressive symptoms, and QOL are significantly correlated with each other. That is, the total CSI-P-2 score was significantly negatively correlated with the VR-12 score (r = -0.45, p < 0.01) and positively correlated with participants’ level of depression (r = 0.42, p < 0.01). Depression level was negatively correlated with the VR-12 score (r = -0.61, p < 0.01)
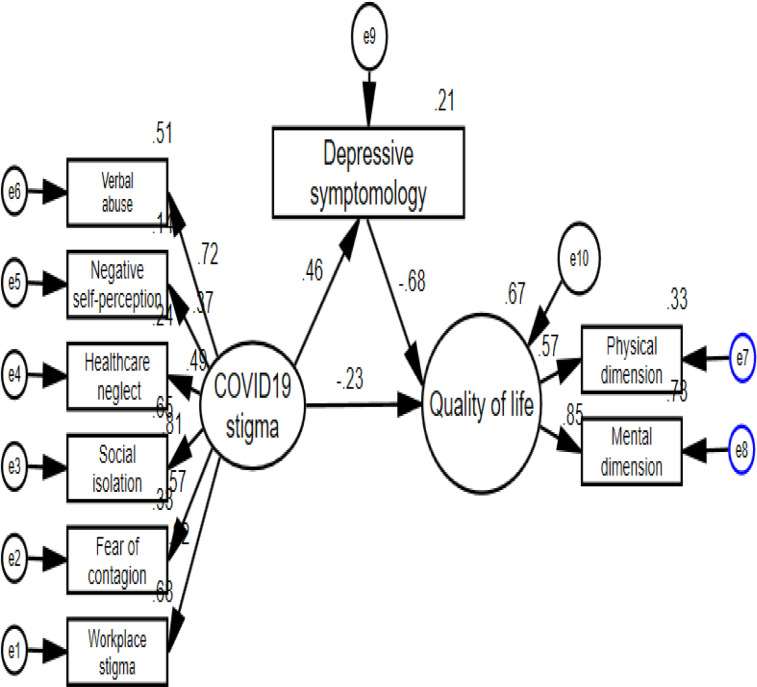
After controlling for the participants' demographic and disease characteristics, we found that the hypothesized relationships were significant and supported by the data; the final pathway fit well to the data (χ2(25) = 2.105, p = 0.001, RMSEA = 0.08, CFI = 0.94 & TLI = 0.91), as shown in Fig. 1 . The standardized direct, indirect, and total estimates of the final model's paths are shown in Appendix 2.
Fig. 1.
The final Pathway.
8. Discussion
This is the first study to adapt, modify, and validate the CSI-P-2 through a rigorous, multiphase process. The psychometric evaluation showed that the 29-item CSI-P-2 with a six-factor structure is a reliable and valid self-report measure for assessing COVID-19 stigma for survivors. On the whole, the factor analytic strategies of CSI-P-2 shared the same factor structure model with the original scale, the HSI-P (Holzemer et al., 2007), that is, the CSI-P-2 can adequately measure verbal abuse, negative self-perception, healthcare neglect, social isolation, fear of contagion, and workplace stigma experienced by COVID-19 survivors in China. The deletions and adjustment of some of the items of the HSI-P in developing the CSI-P-2 may be explained by the different cultures and beliefs between western countries and China. For example, the deletion of Item 13 (I was told that God is punishing me) coincided with the Chinese government policy of promoting atheism (Tang and Chen, 2018). Item 11 (I was told that I have no future), which was moved to the workplace stigma domain, indicates that most COVID-19 survivors thought that their COVID diagnosis might influence their work and even their future.
The convergent validity of the scale was also supported, considering the significant negative correlation found with the physical domain of quality of life and the positive correlations with anxiety, depressive symptoms, and loneliness levels. Similar to previous studies, our findings showed that the COVID stigma associated with survivors' physical and mental health may lead to “double stigma,” or stigma associated with mental illness and the stigma now shown towards certain COVID-positive patients, and increased morbidity (Duan et al., 2020; Kaufman et al., 2020; Liu et al., 2020). In addition, the Cronbach's α and composite reliability of more than 0.6 indicated that the CSI-P-2 had satisfactory internal consistency and reliability (Johnson et al., 2011).
Also in concordance with previous studies (Brooks et al., 2020, Dar et al., 2020), our study further reveals the experience of stigma by COVID-19 survivors in China, with our participants scoring high on fear of contagion, social isolation, and negative self-perception. The participants reported various forms of being insulted, shunned, marginalized, and rejected in various aspects of their lives, including familial relationships and social activities, even after their recovery. The possible explanation is the uncertain character and unpredictable course of COVID-19, the perceived risk of acquiring the infection and the non-availability of effective treatment, the unpredictable outcomes of the disease, its high fatality rate, and the novelty of the infection (Dar et al., 2020).
On the other hand, survivors also reported internalized stigma (e.g., worthlessness, guilt, shame, and self-blame), which was similar to findings regarding other infectious pandemics (Mo and Ng, 2017), but contradict the findings of COVID-19 survivors in India (Dar et al., 2020). For example, most survivors endorsed the “I felt that I brought a lot of trouble to my family” item. This indicates that family responsibility is a key element in Chinese culture and that survivors' failure to fulfill family responsibilities results in higher levels of self-stigma (Sun et al., 2020).
Our study findings reveal that COVID-19 survivors with comorbid diseases, who were elderly, or who had a lower educational level experienced significantly greater stigma. Consistent with previous studies (Roelen et al., 2020; Sun et al., 2020), the elderly and those with comorbid diseases were particularly vulnerable to worse outcomes from COVID-19 and, thus, considerable fear regarding the disease is raised by their outcomes (Li et al., 2020). Also, older survivors who might have cognitive decline have shown greater mood fluctuations and more anxiety and pessimism about the disease (Sun et al., 2020). Interestingly, contrary to previous studies related to COVID (Dar et al., 2020; Duan et al., 2020), we found highly educated survivors presented with lower stigma. The possible reasons for this could be that higher education is associated with more knowledge about this emerging infectious disease and the ability to recognize the authenticity of information provided by the various media or other people regarding the disease. Therefore, with the overabundance of news, rumors, and fake news regarding COVID, these highly educated COVID-19 survivors can separate fact from fiction (Naeem and Bhatti, 2020) and possibly better deal with any social stigma they may face.
In addition to these demographic characteristics, we also found that individuals with higher anxiety and loneliness were more likely to report stigma. These findings corresponded with HSDF points, that is, social-psychological and cognitive factors are risk factors for stigma (Stangl et al., 2019). In this study, people with higher anxiety and loneliness, either from required quarantining or lack of family support, might have experienced an enhanced feeling of stigma because of COVID-19. Furthermore, consistent with previous findings on HIV (Chan et al., 2020; Charles et al., 2012; Rao et al., 2012), we found that COVID-19 survivors who felt more stigma suffered from greater depressive symptoms and presented with less QOL. In addition, depressive symptoms mediated the association between COVID stigma and QOL. In this study, higher stigma was associated with higher depressive symptoms. Also, higher depressive symptoms were significantly related to lower QOL. Likewise, studies on people living with HIV have proven that stigma is associated with their depressive symptoms and QOL (Rao et al., 2012). Future studies should explore the role of family support and other protective factors to decrease stigma and depressive symptoms in order to provide people with COVID a better quality of life.
This study has several limitations. First, this sample came from one of the premier health institutions in Shanghai, China; therefore, it might limit the generalization of the findings to other Chinese-speaking regions. Second, the relatively small sample size limited our ability to use more powerful statistical techniques, such as structural equation modeling. Third, some psychometric characteristics of the CSI-P-2 should be assessed further, such as test-retest reliability, responsibility, sensitivity, and the cut-value of the scale. Therefore, future longitudinal or experimental studies are warranted, as is further refinement of the scale. Item-response analysis can be used with a larger representative sample and can produce stable parameter estimates and robust results. Fourth, the survey relied on the self-reported online survey. Due to the time of data collection, the participants who were diagnosed early in the pandemic were being asked to recall a period that occurred months earlier. Therefore, their recollections might not be accurate. In addition, at that time, the general public was still in shock due to this new infectious disease, and, therefore, study participants might have felt more stigmatized during the first wave of the COVID epidemic. Finally, this is a cross-sectional study and follow-up data were not employed. Future studies are needed on the changing dynamics of stigma in different stages of the pandemic.
9. Relevance for clinical practice
Screening of COVID-19 stigma in COVID-19 survivors and coordinated specific stigma-reducing interventions are increasingly needed to improve mental health during the COVID-19 pandemic (World Health Organization, 2020). This study shines a light on new research directions. There are several implications of this study.
First, the CSI-P-2 can accurately measure COVID-19-associated stigma among COVID-19 survivors. This study should be replicated in different countries to build up culturally tailored stigma-reduction interventions for COVID-19 survivors.
Second, our findings indicated that the stigma associated with COVID-19 should not be neglected, especially fear of contagion, social isolation, and negative self-identity. Therefore, culturally sensitive evidence-based stigma-reducing interventions should be integrated into public health protocols and healthcare measures to cope with the pandemic. Specifically, people affected by COVID-19 could be involved in the development and implementation of stigma reduction interventions (Peprah and Gyasi, 2020).
Third, addressing stigma toward individuals affected by COVID-19 and individual groups at higher risk (e.g., healthcare providers, flight attendants) should be a societal priority, especially, for COVID-19 survivors with comorbid diseases, the elderly, those with a lower educational level, and those with poor mental health. Family support should also be included in the stigma-reduction interventions, especially when vaccine and personal protection equipment are available and fully utilized.
Fourth, depressive symptoms should be considered when developing stigma-reducing interventions for COVID-19 survivors. To improve the QOL of COVID survivors, the accessibility of depressive symptoms management must be considered to reduce COVID-related stigma.
10. Conclusions
The psychometric properties of the 29-item CSI-P-2 in this study support the use of the scale as a measure of COVID-19 stigma among COVID-19 survivors. This study can facilitate the future development of tailored stigma-reduction interventions. Fear of contagion, social isolation, and negative self-perceptions were found among COVID-19 survivors. Aging, comorbid diseases, lower educational level, higher anxiety, and loneliness levels were predictors of higher COVID-19 stigma. Future studies should focus on developing culturally sensitive stigma-reduction interventions and considering the significant mediating effect of depressive symptoms on the experience of stigma.
CRediT authorship contribution statement
Feifei Huang: Formal analysis, Writing – original draft, Writing – review & editing. Wenxiu Sun: Data curation, Formal analysis, Funding acquisition, Investigation, Project administration, Validation, Visualization, Writing – review & editing. Lin Zhang: Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing. Hongzhou Lu: Funding acquisition, Investigation, Methodology, Resources, Supervision, Writing – review & editing. Wei-Ti Chen: Conceptualization, Formal analysis, Funding acquisition, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
All authors are no conflict of interest exists in carrying out this study and writing this manuscript.
Acknowledgments
Acknowledgements
We gratefully acknowledge all the study participants, without them, it is not possible to complete these projects.
Funding sources
This publication is a result, in part, from research supported by Fudan University Science Establishment (IDF162005), Novel coronavirus “2019-NCOV” research project of Shanghai Public Health Clinical Center (No. 2020YJKY01), UCLA CTSI/SON Intramural fund March 2020, NIMH (P30MH058107; R25MH087217).
Ethical Conduct of Research
This research was approved by the relevant institutional review boards of UCLA (IRB#20–000832) and Shanghai public health clinical center (YZ-2020-S037–01). Research was conducted in accordance with the Helsinki Declaration as revised 1989.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.10.043.
Appendix. Supplementary materials
References
- Abdelhafiz A.S., Alorabi M. Social stigma: the hidden threat of COVID-19. Front. Public Health. 2020;8:429. doi: 10.3389/fpubh.2020.00429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brislin R.W. Back-translation for cross-cultural research. J. Cross- Cultural Psychol. 1970;1(3):187–216. [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet North Am. Ed. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassiani-Miranda C.A., Campo-Arias A., Tirado-Otálvaro A.F., Botero-Tobón L.A., Upegui-Arango L.D., Rodríguez-Verdugo M.S., Scoppetta O. Stigmatisation associated with COVID-19 in the general Colombian population. Int. J. Soc. Psychiatry. 2020 doi: 10.1177/0020764020972445. 0020764020972445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan R.C., Mak W.W., Ma G.Y., Cheung M. Interpersonal and intrapersonal manifestations of HIV stigma and their impacts on psychological distress and life satisfaction among people living with HIV: Toward a dual-process model. Qual. Life Res. 2020:1–12. doi: 10.1007/s11136-020-02618-y. [DOI] [PubMed] [Google Scholar]
- Charles B., Jeyaseelan L., Pandian A.K., Sam A.E., Thenmozhi M., Jayaseelan V. Association between stigma, depression and quality of life of people living with HIV/AIDS (PLHA) in South India–a community based cross sectional study. BMC Public Health. 2012;12(1):1–11. doi: 10.1186/1471-2458-12-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W.T., Wantland D., Reid P., Corless I.B., Eller L.S., Iipinge S., Webel A.R. Engagement with health care providers affects self-efficacy, self-esteem, medication adherence and quality of life in people living with HIV. J. AIDS & Clin. Res. 2013;4(11):256. doi: 10.4172/2155-6113.1000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dar S.A., Khurshid S.Q., Wani Z.A., Khanam A., Haq I., Shah N.N., Mustafa H. Stigma in coronavirus disease-19 survivors in Kashmir, India: a cross-sectional exploratory study. PLoS One. 2020;15(11) doi: 10.1371/journal.pone.0240152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan W., Bu H., Chen Z. COVID-19-related stigma profiles and risk factors among people who are at high risk of contagion. Soc. Sci. Med. 2020;266 doi: 10.1016/j.socscimed.2020.113425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzemer W.L., Uys L.R., Chirwa M.L., Greeff M., Makoae L.N., Kohi T.W., Durrheim K. Validation of the HIV/AIDS Stigma Instrument—PLWA (HASI-P) AIDS Care. 2007;19(8):1002–1012. doi: 10.1080/09540120701245999. [DOI] [PubMed] [Google Scholar]
- Imran N., Afzal H., Aamer I., Hashmi A., Shabbir B., Asif A., Farooq S. Scarlett Letter: a study based on experience of stigma by COVID-19 patients in quarantine. Pak. J. Med. Sci. 2020;36(7):1471. doi: 10.12669/pjms.36.7.3606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins W.D., Bolinski R., Bresett J., Van Ham B., Fletcher S., Walters S., Ouellet L. COVID-19 during the opioid epidemic-exacerbation of stigma and vulnerabilities. J. Rural Health. 2020 doi: 10.1111/jrh.12442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson C., Aaronson N., Blazeby J.M., Bottomley A., Fayers P., Koller M., Kuliś D., Ramage J., Sprangers M., Velikova G., Young T. 4rd ed. EORTC: On behalf of the Quality of Life Group; Brussels: 2011. Guidelines For Developing Questionnaire Modules. [Google Scholar]
- Jones P.S., Lee J.W., Phillips L.R., Zhang X.E., Jaceldo K.B. An adaptation of Brislin's translation model for cross-cultural research. Nurs. Res. 2001;50:300–304. doi: 10.1097/00006199-200109000-00008. [DOI] [PubMed] [Google Scholar]
- Kaufman K.R., Petkova E., Bhui K.S., Schulze T.G. A global needs assessment in times of a global crisis: world psychiatry response to the COVID-19 pandemic. BJPsych. Open. 2020;6(3):e48. doi: 10.1192/bjo.2020.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight R.G., Chisholm B.J., Marsh N.V., Godfrey H.P. Some normative, reliability, and factor analytic data for the revised UCLA Loneliness Scale. J. Clin. Psychol. 1988;44(2):203–206. doi: 10.1002/1097-4679(198803)44:2<203::aid-jclp2270440218>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020;382 doi: 10.1056/NEJMoa2001316. 1199e207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D., Baumeister R.F., Veilleux J.C., Chen C., Liu W., Yue Y., Zhang S. Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie C.H. Lessons learned from HIV can inform our approach to COVID-19 stigma. J. Int. AIDS Soc. 2020;23(5):e25504. doi: 10.1002/jia2.25504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo P.K., Ng C.T. Stigmatization among people living with HIV in Hong Kong: a qualitative study. Health Expect. 2017;20(5):943–951. doi: 10.1111/hex.12535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokkink L.B., Terwee C.B., Patrick D.L., Alonso J., Stratford P.W., Knol D.L., De Vet H.C. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual. Life Res. 2010;19(4):539–549. doi: 10.1007/s11136-010-9606-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokkink L.B., Terwee C.B., Patrick D.L., Alonso J., Stratford P.W., Knol D.L., de Vet H.C. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J. Clin. Epidemiol. 2010;63(7):737–745. doi: 10.1016/j.jclinepi.2010.02.006. [DOI] [PubMed] [Google Scholar]
- Muhidin S., Vizheh M., Moghadam Z.B. Anticipating COVID-19-related stigma in survivors and health-care workers: Lessons from previous infectious diseases outbreaks–An integrative literature review. Psychiatry Clin. Neurosci. 2020;74(11):617–618. doi: 10.1111/pcn.13140. [DOI] [PubMed] [Google Scholar]
- Naeem S.B., Bhatti R. The Covid-19 ‘infodemic’: a new front for information professionals. Health Inf. Libr. J. 2020;37(3):233–239. doi: 10.1111/hir.12311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peprah P., Gyasi R.M. Stigma and COVID-19 crisis: a wake-up call. Int. J. Health Plann. Manage. 2020 doi: 10.1002/hpm.3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransing R., Ramalho R., de Filippis R., Ojeahere M.I., Karaliuniene R., Orsolini L., Fa F.A. Infectious disease outbreak related stigma and discrimination during the COVID-19 pandemic: drivers, facilitators, manifestations, and outcomes across the world. Brain Behav. Immun. 2020;89:555–558. doi: 10.1016/j.bbi.2020.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao D., Chen W.T., Pearson C.R., Simoni J.M., Fredriksen-Goldsen K., Nelson K., Zhang F. Social support mediates the relationship between HIV stigma and depression/quality of life among people living with HIV in Beijing, China. Int. J. STD AIDS. 2012;23(7):481–484. doi: 10.1258/ijsa.2009.009428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roelen K., Ackley C., Boyce P., Farina N., Ripoll S. COVID-19 in LMICs: The need to place stigma front and centre to its response. Eur. J. Dev. Res. 2020;32(5):1592–1612. doi: 10.1057/s41287-020-00316-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stangl A.L., Earnshaw V.A., Logie C.H., van Brakel W., Simbayi L.C., Barré I., Dovidio J.F. The health stigma and discrimination framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17(1):1–13. doi: 10.1186/s12916-019-1271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang K., Chen W.T. HIV and religion in HIV-infected Asians and their families: a qualitative study. Appl. Nurs. Res. 2018;44:18–24. doi: 10.1016/j.apnr.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terwee C.B., Mokkink L.B., Knol D.L., Ostelo R.W., Bouter L.M., de Vet H.C. Rating the methodological quality in systematic reviews of studies on measurement properties: a scoring system for the COSMIN checklist. Qual. Life Res. 2012;21(4):651–657. doi: 10.1007/s11136-011-9960-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak. https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf; 2020 (accessed on 1st April, 2020).
- Ye W.F., Xu J.M. Application and evaluation of the Hospital Anxiety and Depression Scale in patients of general hospital. Chin. J. Behav. Med. Sci. 1993;2(3):17–19. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.