Abstract
Public health crises palpably demonstrate how social determinants of health have led to disparate health outcomes. The staggering mortality rates among African Americans, Native Americans, and Latinx Americans during the COVID-19 pandemic have revealed how recalcitrant structural inequities can exacerbate disparities and render not just individuals but whole communities acutely vulnerable. While medical curricula that educate students about disparities are vital in rousing awareness, it is experience that is most likely to instill passion for change. The authors first consider the roots of health care disparities in relation to the current pandemic. Then, they examine the importance of salient learning experiences that may inspire a commitment to championing social justice. Experiences in diverse communities can imbue medical students with a desire for lifelong learning and advocacy. The authors introduce a 3-pillar framework that consists of trust building, structural competency, and cultural humility. They discuss how these pillars should underpin educational efforts to improve social determinants of health. Effecting systemic change requires passion and resolve; therefore, perseverance in such efforts is predicated on learners caring about the structural inequities in housing, education, economic stability, and neighborhoods—all of which influence the health of individuals and communities.
The COVID-19 pandemic has amplified disquieting health care disparities and inequities in the United States. Statistics have demonstrated the skewed impact, including greater mortality, that COVID-19 has had on minority communities across the country. In Michigan, 21% of the deaths from COVID-19 (by April 2021) were among African Americans, who account for only 14% of the state’s residents. 1 In Louisiana, 38% of all coronavirus-related deaths (again by April 2021) occurred among African Americans, who account for just 32% of the population. 2 In New York City, Latinx residents had 1.4 times the mortality rate of Whites as of April 9, 2021. 3 Early statistics were worse: coronavirus was twice as deadly for Latinx residents in New York City as of April 21, 2020, and Massachusetts General Hospital reported a 400% increase in Latinx hospital admissions relative to baseline by early April 2020. 4 Data collected from February to July 2020 demonstrate Latinx Americans, African Americans, and American Indians/Alaska natives accounted for approximately 75% of COVID-19 deaths in persons aged less than 21, even though these groups represent only 41% of the U.S. population. 5
Deeply rooted structural inequities are responsible for the disproportionate harm to vulnerable individuals and communities. 6 Social determinants of health (SDOH), such as higher poverty rates, limited transportation, crowded living conditions, and insufficient workplace protections, preclude social distancing. 7 Furthermore, systemic racism and mistrust of health care systems have rendered minority communities acutely vulnerable to harm. 7,8 An old saying in some African American communities is that “When White folks catch a cold, Black folks get pneumonia.” This maxim captures the stark economic disparities among Americans. An economic downturn that yields hardships for White Americans can be catastrophic for even middle- and upper-class Black Americans who have fewer financial buffers. 9 This axiom can be applied to the unequal—and unconscionable—death toll from COVID-19 in minority communities.
Structural barriers in the health system, as well as disparities in the quality of health care delivered, adversely affect racial/ethnic minority groups. 10 Elevated blood pressure, diabetes, heart disease, renal disease, and asthma are linked to severe illness and mortality with COVID-19. 11 All of these predisposing conditions are more common among racial/ethnic minorities, owing to adverse SDOH and unequal care within health systems. 10,11 Members of racial and ethnic minority groups have less access to care, receive lower quality of care, and experience worse health care outcomes. 10,12 Health providers perpetuate these disparities when they are unaware of, fail to respond to, or lack the skill to understand the circumstances of at-risk patients. 13 The COVID-19 pandemic highlights the imperative for physicians to take action within communities and health systems by advocating policies and effecting positive changes in SDOH to improve health care delivery and achieve greater equity.
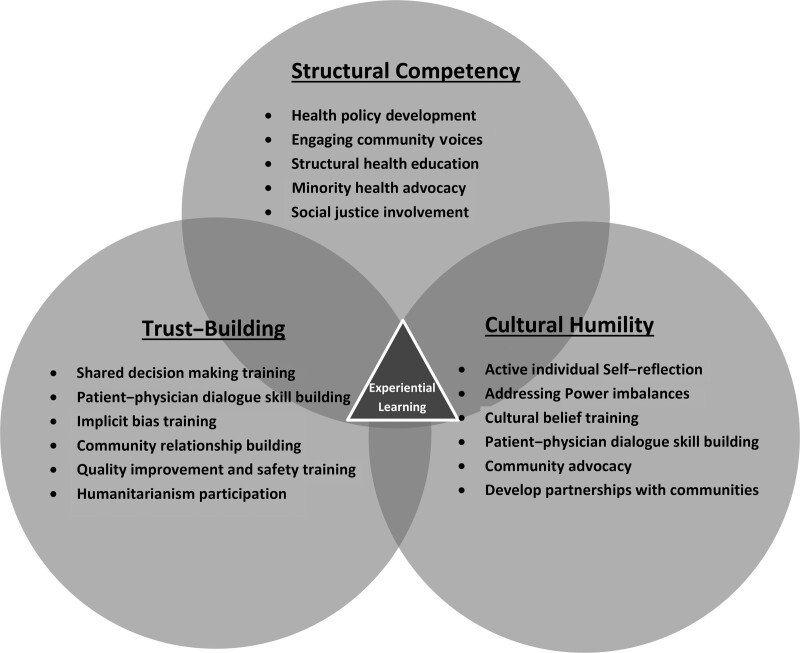
Eradicating health disparities requires an approach to medical education that meets community needs, comprehensively addresses health inequities, and is accountable to all members of communities, especially the most vulnerable. 14 Experiential learning is critical to achieve this goal. 15,16 Formative experiences in underserved communities afford a breadth of understanding of the culture, needs, and challenges of marginalized groups. Those experiences instill a passion for change, encourage advocacy, and teach physicians the skills to address negative health outcomes imposed by poverty, inequality, and discrimination. 17 In this article, we describe a new framework for improving medical education that combines the 3 pillars of trust building, structural competency, and cultural humility (Figure 1).
Figure 1.
A 3-pillar medical education model for mitigating social determinants of health. Trust building curricula promote awareness of mistrust and develop the skills to build relationships with individuals and communities. Structural competency emphasizes systemic inequities that students can address through advocacy and engagement. Cultural humility cultivates self-awareness, self-reflection, and a lifelong commitment to alleviating disparities. Experiential learning binds together the tripartite framework.
Trust Building
Trust is an underused lever for improving health outcomes, and overcoming pervasive mistrust requires caring and open communication in medical education. Patients’ trust in physicians influences their self-efficacy, their adherence to therapeutic regimes, and their health outcomes. 18 At its core, medicine is about caring for people who are suffering; it is a moral enterprise grounded in a covenant of trust. 19 Yet, Gallup poll surveys document a decline from 80% of Americans who trust health care in 1975 to just 37% in 2017—a more rapid fall than any experienced in other industries measured over 50 years. 20 This erosion of trust may be particularly severe among those who have been disenfranchised or exploited. 21
The United States has a troubling history of racial injustices that engender mistrust, and medical students need to understand this history. In the 1918 flu pandemic, Jim Crow policies led to inferior care for Black patients, if any care at all, 22 and in the Tuskegee Study of Untreated Syphilis in the Negro Male, hundreds of Black men remained untreated for syphilis despite penicillin’s wide availability. Penicillin had become the standard of care for treating infection in 1947, yet the Tuskegee study continued until 1972. 23 Further, the immortalized HeLa cell line was developed and used for research without consent from Henrietta Lacks, a young Black woman with cervical carcinoma. 24 Most recently, the Flint water crisis became another bellwether for the lack of preparedness of public institutions to swiftly address the needs of the poor; the crisis further eroded public trust and has weighed on the psyches of individuals and communities. 25
Patient trust is associated with more beneficial health behaviors, higher quality of life, and greater satisfaction with treatment. 18 Trust thus plays a particularly critical role in public health crises, when adherence to medical advice and government ordinances relies heavily on citizens’ confidence in the information provided. In the context of COVID-19, patients’ trust may influence receptiveness to lifesaving care, including ventilator care, hospital isolation, “do not resuscitate” orders, safety measures (e.g., mask wearing), and procedures such as tracheostomy. Medical students and physicians must understand that patients should not be faulted for mistrust, which is rooted in a history of exploitation, inequalities, and unconscionable research practices.
Restoring trust is a moral imperative that requires humility, respect, and solicitude. Little time is devoted in medical education to the teaching of trust, despite its centrality to the patient–physician relationship. The prevailing practices assume that medical trainees will learn how to build trust with patients on their own through trial and error and limited experience. While some trainees succeed, others can become demoralized or experience burnout when they fail. 26 Medical education should imbue students with a deep sense of deference to patients—to their life experiences, to their beliefs and values, and to their rights.
Trust is not inherent in patient–physician interactions but can be built through meaningful dialogue that shifts the power dynamic from one of hierarchy wherein the physician has the most control to a more collaborative relationship. 27 Physicians who have learned shared-decision-making skills can build greater respect and engagement with patients, which in turn increases dialogue and engenders mutual satisfaction and trust. 21 While experience is likely the best teacher, standardized patient simulations can provide trainees with the opportunity to develop necessary skills for building strong rapport with their patients. 28 Furthermore, research indicates that patient trust is built by physicians who maintain a high standard of quality and safety in the care they provide. 29 Patient safety and quality improvement training may therefore have a role in improving trust with patients.
Importantly, trust is influenced by stereotypes, racial profiling, and implicit bias. Through implicit bias training, learners can learn to recognize and mitigate the biases that influence how they care for patients. 30 Some institutions have found that education on racial profiling and historical mistreatment can explain reasons for patient mistrust and that case-based learning can help students to understand how trust between patients and the medical team improves outcomes and quality care. 21 Engagement within underserved communities is one of the most effective ways to cultivate altruism and trust building skills. 26 Forging partnerships between medical schools and communities that are often marginalized can facilitate advocacy, promote parity, and mitigate disparities. 15,17 In addition, developing curricula that foster cultural humility and awareness of structural inequities is a preliminary step in diminishing the role mistrust plays in health disparities. 18,21
Structural Competency
Medical educators, social scientists, and ethicists have increasingly recognized the importance of structural competency for understanding the social and economic forces influencing health outcomes. 31 Whereas cultural competency emphasizes physicians’ awareness of multiple cultures, preparedness to care for diverse patients, and communication skills, structural competency addresses larger questions of systemic bias and health equity. Structural factors encompass the historical, socioeconomic, and political factors that affect the health of populations and their living conditions, food supply, infrastructure, sanitation, and life circumstances. Studies consistently show low levels of physician recognition of the ways health systems contribute to health disparities. 32 Even among physicians who identify racial, ethnic, and socioeconomic disparities in the U.S. health system, only a minority recognize the health system disparities affecting their own patients. 33 Structural competency provides a framework for understanding and addressing health-related aspects of social justice.
Cultivating structural competency in medical students is an important step in increasing the ranks of policy leaders who can identify and address institutionalized racial bias. For example, many policy makers were slow to recognize the latent threat to racial/ethnic minorities posed by the COVID-19–triggered Crisis Standards of Care (CSC), which codified altered health care operations during the pandemic. CSC may preferentially triage ventilators, intensive care unit beds, and other lifesaving resources for patients based on their likelihood of survival, with the utilitarian goal of directing scarce resources to patients thought most likely to benefit. The problem that arises for minorities is that when comorbidities are used in prioritization schemes, minority patients—already at increased risk of dying during the pandemic because of comorbidities linked to SDOH—may experience the double jeopardy arising from decreased access to care. 4 A structurally competent solution might include, in recognition of the reality that SDOH differ among patients, provisions for patients of a racial minority or for patients who reside in impoverished neighborhoods.
Structural competency can also help in managing public health crises by identifying barriers to care. 33 One study showed that documenting patient housing needs in electronic health records was associated with more consistent social interventions in patient treatment plans. 34 Structural competency can be implemented through immersion experiences with public health experts (e.g., workshops, internships, community improvement projects) and through partnerships between medical school and public health faculty. Schulz and colleagues’ recent public health perspective 35 suggests strategic actions that health practitioners can take to effect changes within occupational settings (e.g., promoting policies that increase access to protective equipment, paid sick leave), housing (e.g., supporting efforts to extend moratoriums on evictions and to increase access to rental assistance), and the built environment (e.g., taking actions to ensure access to clean water and air). These actions will not only relieve some of the immediate effects of the pandemic but also enhance long-term health equity.
Through public health and experiential learning, students discover the importance of authentic and humble engagement with community members, of advocacy to effect policy change, and of the application of scientific evidence and rigorous evaluation to influence policy. 35 This cross-pollination (among public health, medical education, and experiential learning) may change how medical education is experienced and how students care for their patients and communities once they become practicing physicians. While relatively few curricula emphasizing structural factors have been implemented, 31 such approaches hold promise for improving the care of patients and communities experiencing disparities. Recent publications 36,37 have demonstrated the need for further implementation and evaluation of such curricula. A nuanced understanding of structural inequality can empower leaders in health care to create changes in systems, 38 and such change is most likely to be successful if interventions reflect the lens of cultural humility.
Cultural Humility
Education in patients’ cultures improves objective health outcomes, perceived quality of health care, satisfaction with health care, and adherence to treatment and advice. 39 Most educational efforts focus on cultural competency and on combinations of several defining attributes such as knowledge, skills, awareness, understanding, and sensitivity. “Cultural competency” remains the most widely used term, and efforts in this arena are laudable, yet recognizing the pitfall of cultural competence is important. Cultural competence suggests there is an achievable mastery of a finite body of knowledge. 40 Whereas cultural competence implies an endpoint, 41 cultural humility is an ongoing process of introspection and reflection, continually being aware of how social inequities present barriers to care and of the need to strive for parity in the physician–patient relationship. 40
Cultural competency and humility are promising approaches to illuminating the underlying challenges affecting members of racial and ethnic minority groups and to working toward the ultimate goal of alleviating these racial and ethnic disparities. 42 The Accreditation Council for Graduate Medical Education and the Liaison Committee on Medical Education endorse curricula in cultural competency and humility to increase awareness; reduce bias; and provide safe, high-quality care to diverse patients. The attributes and skills of cultural competency and humility are urgently needed to understand the needs of and care for the populations at risk from public health crises, such as COVID-19. 42
Approaches to clinical training in cultural competency and humility vary in content, pedagogy, timing, and methods of learner assessment and program evaluation. 40,43–45 Studies suggest that medical students are inadequately prepared for delivering culturally effective care. 46,47 Among Harvard medical students, for example, fewer than half the students in their final year felt sufficiently prepared on 8 out of 11 preparedness items (e.g., caring for patients with health beliefs at odds with Western medicine, patients with religious beliefs that might affect treatment, patients who use alternative or complementary medicines). 46 Likewise, fewer than half of these students felt sufficiently skilled on 5 out of 10 skillfulness items (e.g., assessing English proficiency, identifying relevant cultural and religious beliefs, counseling patients about their use of complementary medicine). 46 Lack of experience caring for diverse patients was cited as the greatest barrier, 46 a finding that underscores the importance of first-hand experience in caring for patients in diverse communities. Such experiences help learners grasp SDOH and understand the pervasiveness of racial inequality.
Cultural humility is likely a better goal than cultural competency; it focuses on experiential learning to help reduce hierarchical relationships, promote understanding, and improve health outcomes. While an increase in cultural knowledge of health beliefs is critical, an isolated increase in knowledge without a consequent change in attitudes and behavior is of little value. Training in cultural humility avoids conferring a sense of cultural expertise or completion. 40 Cultural humility training can help trainees learn to identify and mitigate the effects of their personal biases, and it cultivates awareness of the perspectives of others. 48,49 A few pedagogical approaches have met with success: small-group discussions, personal journals, meeting with positive professional role models from cultural groups, and videotaping interactions and receiving feedback. 40
A key component of cultural training includes learning cross-cultural skills related to patient–physician dialogue. 46 Cultural humility creates an atmosphere that actively invites the patient’s contributions and that values the patient’s experience and perspective jointly with physician expertise. 50 Humility in dialogue allows for collaborative physician–patient decision making during times of crisis since it diminishes power differentials and builds trust. Educators can teach communication skills that embrace humility through small groups, videos, and work with standardized patients. 13 Experiences in the community and with community members also lead to effective lessons on cultural humility and on advocating for changes to mitigate health disparities. 15,17 Cultural humility and experiential learning improve medical students’ awareness of health inequity and may instill within them a passion to become leaders who respond to health care disparities, mistrust, and structural injustices throughout their future careers.
Conclusion
Medical schools should embody the ideals of the medical profession, and they provide the setting where many physicians’ attitudes and beliefs form and mature. The 3 pillars of trust building, structural competency, and cultural humility form the foundation for addressing health care disparities arising from poverty, structural racism, and other social injustices. Understanding the history of racism and mistrust is necessary to contextualize the formidable challenges of the present and to prevent future injustice. Training learners to address implicit bias and build respectful relationships with patients is a preliminary step in assuaging the deep ambivalence and mistrust many patients and members of marginalized communities feel. Structural competency, which is critical for identifying and rectifying systemic inequities, can be achieved through strategic partnerships involving medical schools, public health faculty, and communities. Cultural humility, given its emphasis on lifelong learning and continuous self-reflection, promotes understanding and agency in mitigating SDOH.
Experiential learning and active engagement with diverse communities are the cornerstones of rectifying disparities. It is only through first-hand experiences that learners can maximally broaden their perspective and share in the lives of patients. These powerful experiences can inspire students to learn more, to understand more, and to do more as they rise to meet the challenge of countering injustice. All physicians see their patients through the lens of their own biases, and perhaps the hard lessons of the COVID-19 pandemic will inspire each of us to address these personal prejudices, to build trusting partnerships with patients, and to strive for true parity in care. As we work in the years to come to clear the rubble of the COVID-19 pandemic, we will look back on this time as a defining moment of moral reckoning. How we respond to the pandemic and to the inequalities that it has uncovered will say much about who we are and what we stand for as educators.
Footnotes
Funding/Support: Cherie-Ann Nathan is supported by the National Institutes of Health (NIH; grant 5R01CA217180-03). John M. Carethers is supported by the United States Public Health Service (NIH grant CA206010) and by the A. Alfred Taubman Medical Research Institute of the University of Michigan. Rajesh S. Mangrulkar is supported by an American Medical Association (AMA) Accelerating Change in Education grant. Michael J. Brenner is supported by the Vice Provost for Global Engagement Research on Teaching & Learning Grant (University of Michigan).
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Contributor Information
Andrew D.P. Prince, Email: adprince@med.umich.edu.
Alexander R. Green, Email: ARGREEN@mgh.harvard.edu.
David J. Brown, Email: davidjb@med.umich.edu.
Dana M. Thompson, Email: dmthompson@luriechildrens.org.
Enrique W. Neblett, Jr, Email: eneblett@umich.edu.
Cherie-Ann Nathan, Email: CNatha@lsuhsc.edu.
John M. Carethers, Email: jcarethe@med.umich.edu.
Rebekah E. Gee, Email: rgee@lsuhsc.edu.
Larry D. Gruppen, Email: lgruppen@med.umich.edu.
Rajesh S. Mangrulkar, Email: rajm@med.umich.edu.
References
- 1.State of Michigan. Coronavirus: Michigan data. 2021. Demographics. Deaths by Race. https://www.michigan.gov/coronavirus/0,9753,7-406-98163_98173---,00.html. Accessed April 21, 2021
- 2.Louisiana Department of Health. Louisiana Coronavirus COVID-19. Additional Data on COVID-19 Deaths in Louisiana. https://ldh.la.gov/index.cfm/page/4065. Accessed April 21, 2021
- 3.City of New York. COVID-19: Data. 2021. Totals. Case, Hospitalization and Death Rates. https://www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-19-deaths-race-ethnicity-04082020-1.pdf. Accessed April 22, 2021.
- 4.Tartak JC, Khidir H. Opinion: U.S. must avoid building racial bias into COVID-19 emergency guidance. NPR. https://www.npr.org/sections/health-shots/2020/04/21/838763690/opinion-u-s-must-avoid-building-racial-bias-into-covid-19-emergency-guidance. Published April 21, 2020. Accessed April 9, 2021
- 5.Bixler D, Miller AD, Mattison CP, et al. SARS-CoV-2–Associated deaths among persons aged <21 years—United States, February 12–July 31, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:1324–1329. 10.15585/mmwr.mm6937e4. Accessed April 9, 2021 [DOI] [PubMed] [Google Scholar]
- 6.Webb Hooper M, Napoles AM, Perez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020; 323:2466–2467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yancy CW. COVID-19 and African Americans. JAMA. 2020; 323:1891–1892 [DOI] [PubMed] [Google Scholar]
- 8.Laurencin CT, McClinton A. The COVID-19 pandemic: A call to action to identify and address racial and ethnic disparities. J Rac Ethn Health Disparities. 2020; 7:398–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siegel J, Coleman DL, James T. Integrating social determinants of health into graduate medical education: A call for action. Acad Med. 2018; 93:159–162 [DOI] [PubMed] [Google Scholar]
- 10.Blumenthal D, Fowler EJ, Abrams M, Collins SR. Covid-19—Implications for the health care system. N Engl J Med. 2020; 383:1483–1488 [DOI] [PubMed] [Google Scholar]
- 11.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382:1708–1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003 [PubMed] [Google Scholar]
- 13.Brottman MR, Char DM, Hattori RA, Heeb R, Taff SD. Toward cultural competency in health care: A scoping review of the diversity and inclusion education literature. Acad Med. 2020; 95:803–813 [DOI] [PubMed] [Google Scholar]
- 14.Mullan F. Social mission in health professions education: Beyond Flexner. JAMA. 2017; 318:122–123 [DOI] [PubMed] [Google Scholar]
- 15.Strasser R, Worley P, Cristobal F, et al. Putting communities in the driver’s seat: The realities of community-engaged medical education. Acad Med. 2015; 90:1466–1470 [DOI] [PubMed] [Google Scholar]
- 16.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet. 2010; 376:1923–1958 [DOI] [PubMed] [Google Scholar]
- 17.O’Mara-Eves A, Brunton G, Oliver S, Kavanagh J, Jamal F, Thomas J. The effectiveness of community engagement in public health interventions for disadvantaged groups: A meta-analysis. BMC Public Health. 2015; 15:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Birkhauer J, Gaab J, Kossowsky J, et al. Trust in the health care professional and health outcome: A meta-analysis. PLoS One. 2017; 12:e0170988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crawshaw R, Rogers DE, Pellegrino ED, et al. Patient-physician covenant. JAMA. 1995; 273:1553. [PubMed] [Google Scholar]
- 20.Knight Commission on Trust, Media, and Democracy. Draft Chapter 1: The necessity for trust. https://medium.com/trust-media-and-democracy/renewing-americans-trust-b16a63eb5e63. Published March 21, 2018. Accessed April 9, 2021
- 21.Gupta N, Thiele CM, Daum JI, et al. Building patient-physician trust: A medical student perspective. Acad Med. 2020; 95:980–983 [DOI] [PubMed] [Google Scholar]
- 22.Gamble VN. “There wasn’t a lot of comforts in those days”: African Americans, public health, and the 1918 influenza epidemic. Public Health Rep. 2010; 125suppl 3114–122 [PMC free article] [PubMed] [Google Scholar]
- 23.Frieden TR, Collins FS. Intentional infection of vulnerable populations in 1946-1948: Another tragic history lesson. JAMA. 2010; 304:2063–2064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang S. The surgeon who experimented on slaves. The Atlantic. https://www.theatlantic.com/health/archive/2018/04/j-marion-sims/558248. Published April 18, 2018. Accessed April 9, 2021 [Google Scholar]
- 25.Cuthbertson CA, Newkirk C, Ilardo J, Loveridge S, Skidmore M. Angry, scared, and unsure: Mental health consequences of contaminated water in Flint, Michigan. J Urban Health. 2016; 93:899–908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hendren EM, Kumagai AK. A matter of trust. Acad Med. 2019; 94:1270–1272 [DOI] [PubMed] [Google Scholar]
- 27.Kumagai AK, Naidu T. Reflection, dialogue, and the possibilities of space. Acad Med. 2015; 90:283–288 [DOI] [PubMed] [Google Scholar]
- 28.Hoffmann T, Glasziou P. Bringing shared decision making and evidence-based practice together. Elwyn G, Edwards A, Thompson R, eds. In: Shared Decision Making in Health Care: Achieving Evidence-Based Patient Choice. Oxford, UK: Oxford University Press; 2016 [Google Scholar]
- 29.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013; 3:e001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sukhera J, Watling C. A framework for integrating implicit bias recognition into health professions education. Acad Med. 2018; 93:35–40 [DOI] [PubMed] [Google Scholar]
- 31.Metzl JM, Petty J. Integrating and assessing structural competency in an innovative prehealth curriculum at Vanderbilt University. Acad Med. 2017; 92:354–359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Britton BV, Nagarajan N, Zogg CK, et al. Awareness of racial/ethnic disparities in surgical outcomes and care: Factors affecting acknowledgment and action. Am J Surg. 2016; 212:102–108 [DOI] [PubMed] [Google Scholar]
- 33.Metzl JM, Petty J, Olowojoba OV. Using a structural competency framework to teach structural racism in pre-health education. Soc Sci Med. 2018; 199:189–201 [DOI] [PubMed] [Google Scholar]
- 34.Garg A, Butz AM, Dworkin PH, Lewis RA, Serwint JR. Screening for basic social needs at a medical home for low-income children. Clin Pediatr (Phila). 2009; 48:32–36 [DOI] [PubMed] [Google Scholar]
- 35.Schulz AJ, Mehdipanah R, Chatters LM, Reyes AG, Neblett EW, Jr, Israel BA. Moving health education and behavior upstream: Lessons from COVID-19 for addressing structural drivers of health inequities. Health Educ Behav. 2020; 47:519–524 [DOI] [PubMed] [Google Scholar]
- 36.Neff J, Holmes SM, Knight KR, et al. Structural competency: Curriculum for medical students, residents, and interprofessional teams on the structural factors that produce health disparities. MedEdPORTAL. 2020; 16:10888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bourgois P, Holmes SM, Sue K, Quesada J. Structural vulnerability: Operationalizing the concept to address health disparities in clinical care. Acad Med. 2017; 92:299–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.American Medical Association. Declaration of Professional Responsibility Medicine’s Social Contract with Humanity. https://www.ama-assn.org/system/files/2020-03/declaration-professional-responsibility-english.pdf. Published December 4, 2001. Accessed April 9, 2021 [PubMed]
- 39.Henderson S, Horne M, Hills R, Kendall E. Cultural competence in healthcare in the community: A concept analysis. Health Soc Care Community. 2018; 26:590–603 [DOI] [PubMed] [Google Scholar]
- 40.Tervalon M, Murray-Garcia J. Cultural humility versus cultural competence: A critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved. 1998; 9:117–125 [DOI] [PubMed] [Google Scholar]
- 41.Engebretson J, Mahoney J, Carlson ED. Cultural competence in the era of evidence-based practice. J Prof Nurs. 2008; 24:172–178 [DOI] [PubMed] [Google Scholar]
- 42.Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O, II. Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003; 118:293–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rapp DE. Integrating cultural competency into the undergraduate medical curriculum. Med Educ. 2006; 40:704–710 [DOI] [PubMed] [Google Scholar]
- 44.Loudon RF, Anderson PM, Gill PS, Greenfield SM. Educating medical students for work in culturally diverse societies. JAMA. 1999; 282:875–880 [DOI] [PubMed] [Google Scholar]
- 45.Flores G, Gee D, Kastner B. The teaching of cultural issues in U.S. and Canadian medical schools. Acad Med. 2000; 75:451–455 [DOI] [PubMed] [Google Scholar]
- 46.Green AR, Chun MBJ, Cervantes MC, et al. Measuring medical students’ preparedness and skills to provide cross-cultural care. Health Equity. 2017; 1:15–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Weissman JS, Betancourt J, Campbell EG, et al. Resident physicians’ preparedness to provide cross-cultural care. JAMA. 2005; 294:1058–1067 [DOI] [PubMed] [Google Scholar]
- 48.Smith RC, Hoppe RB. The patient’s story: Integrating the patient- and physician-centered approaches to interviewing. Ann Intern Med. 1991; 115:470–477 [DOI] [PubMed] [Google Scholar]
- 49.Weiss T, Swede MJ. Transforming preprofessional health education through relationship-centered care and narrative medicine. Teach Learn Med. 2019; 31:222–233 [DOI] [PubMed] [Google Scholar]
- 50.Berlin EA, Fowkes WC, Jr. A teaching framework for cross-cultural health care. Application in family practice. West J Med. 1983; 139:934–938 [PMC free article] [PubMed] [Google Scholar]