Abstract
Context:
Supervised injection facilities are harm reduction interventions that allow people who inject drugs to use previously obtained substances under the supervision of health professionals. Though currently considered illegal under U.S. federal law, several U.S. cities are considering implementing supervised injection facilities anyway as a response to the escalating overdose crisis. The objective of this review is to determine the effectiveness of supervised injection facilities, compared with control conditions, for harm reduction and community outcomes.
Methods:
Studies were identified from 2 sources: a high-quality, broader review examining supervised injection facility–induced benefits and harms (database inception to January 2014), and an updated search using the same search strategy (January 2014–September 2019). Systematic review methods developed by the Guide to Community Preventive Services were used (screening and analysis, September 2019–December 2020).
Results:
Twenty-two studies were included in the current review—16 focused on 1 supervised injection facility in Vancouver, Canada. Quantitative synthesis was not conducted given inconsistent outcome measurement across studies. Supervised injection facilities in included studies (n = number of studies per outcome category) were mostly associated with significant reductions in opioid overdose morbidity and mortality (n=5), significant improvements in injection behaviors and harm reduction (n=7), significant improvements in access to addiction treatment programs (n=7), and no increase or reductions in crime and public nuisance (n=7).
Conclusions:
For people who inject drugs, supervised injection facilities may reduce risk of overdose morbidity and mortality and improve access to care, while not increasing crime or public nuisance to the surrounding community.
INTRODUCTION
Roughly 450,000 people have died from opioid-involved overdose in the U.S. since 2000, with a rapid escalation in deaths in the past decade due to the rise of exposure to illicit fentanyl and related analogs.1 Roughly 2 million people in the U.S. had an opioid use disorder in 2018.2 However, it is estimated that only one third of individuals with opioid use disorder have received any treatment,3 despite the availability of effective, evidence-based medications to treat opioid use disorder long term (e.g., buprenorphine, methadone).4 An emerging wave of stimulant injection behavior and overdoses in recent years has compounded the crisis.5 Making matters worse, the U.S. Centers for Disease Control and Prevention warns that the social and economic disruption of the coronavirus disease 2019 (COVID-19) pandemic may exacerbate substance use disorder (SUD) morbidity and mortality and worsen barriers to treatment and preventive services.6
Faced with such crises, local governments across the U.S. have considered implementing supervised injection facilities (SIFs),7–9 a harm reduction intervention common in other Western democracies but currently considered illegal under U.S. federal law.10–12 SIFs are facilities that allow people who inject drugs (PWID) to use previously obtained substances under the supervision of healthcare professionals.13 SIFs emerged in Europe in the 1990s out of a harm reduction model, which seeks to meet people with SUD “where they are” without imposing behavior change requirements.13,14 SIFs—or more broadly, overdose prevention centers or supervised consumption facilities (SCFs)—are a form of tertiary prevention, aimed at reducing health-related risks from injecting (e.g., shared syringes and equipment, rushed and public injections).15 As such, they hold great promise in preventing infectious disease acquisition (e.g., HIV) and potentially reducing the occurrence of non-fatal and fatal overdose among PWID. SIFs can also be co-located with or offer referrals to SUD treatment, facilitating access to such services.16 Most legally sanctioned SIFs are located in Europe, followed by Canada and Australia12; however, unsanctioned SIFs exist in other countries, including the U.S.9
Despite decades of research, SIFs remain politically controversial in some countries, including the U.S. Critics of SIFs claim that such interventions “subsidize drug use,” enabling people to use drugs without consequence and contributing to addiction.17 Others fear secondary impacts SIFs might have on their communities. Such “not in my backyard” perspectives often focus on how SIFs might increase local crime, intensify drug use—related public nuisance (e.g., improperly discarding needles, injecting in public areas), and negatively impact property values.18
The evidence base supporting the effectiveness of SIFs is steadily growing, and multiple systematic reviews capture the developments of this fast-moving field.19–22 Kennedy et al.21 examined quantitative studies of SCFs (a broader intervention than SIFs, including non-injected drugs) and found associated favorable health and public order outcomes, including reduced overdose risk and no increase in crime. Caulkins and colleagues20 looked at “higher-quality” literature (i.e., quasi-experiments, modeling studies) of SCFs, framing conclusions in the perspective of various decision makers (e.g., politicians, academics).
The present study builds on these reviews by narrowing focus exclusively to quantitative effectiveness studies of existing SIFs (not modeling studies, not SCFs broadly). The original analysis plan for this review included quantitative synthesis methods, which benefit from a narrower, more-homogenous scope. One well-conducted review by Potier et al.22 examined SIF literature (database inception–January 2014). The present study uses the Potier and colleagues review as a basis given it was the most-cited review on SIFs at the time of writing and because its end search date is now >7 years old.
In an effort to inform local and national debates about SIFs and their effectiveness in preventing the health harms associated with injection drug use using the most current evidence, the present systematic review was conducted. This review focuses exclusively on studies with quantitative results that compared SIFs (as an intervention) with control conditions. It also focuses specifically on SIFs (rather than the broader category of SCFs) because SIFs are the current focus of U.S. debate. This is the first review, to review authors’ knowledge, that utilizes the Community Guide systematic review methods,23,24 which form the basis for findings of the U.S. Community Preventive Services Task Force. These methods are optimized to assess and synthesize a variety of study designs focused on population-level public health interventions such as SIFs.10,11
The research questions for this review are as follows. How effective are SIFs at the community level, compared with defined control conditions (e.g., areas without a SIF, before versus after SIF implementation), in improving outcomes in the domains of: (1) overdose-induced mortality and morbidity, (2) injection behaviors and harm reduction, (3) access to addiction treatment programs, and (4) crime and public nuisance related to drug use? How effective is SIF use at the individual level compared with defined control conditions (e.g., PWID who do not use SIFs, more frequent versus less frequent utilization of SIF among PWID [dose response]) in improving outcomes in these 4 domains?
Evidence Acquisition
A team of specialists in systematic review methods and subject matter experts in research, policy, and practice related to SUD and harm reduction interventions including SIFs conducted a systematic search for relevant articles and present it herein according to PRISMA guidelines.25
Review authors used standard systematic review methods outlined by the Community Guide.23,24 This systematic review was not registered and the protocol was not previously published.
Search for Evidence
This review used the strategy of Potier et al.(22)(Appendix). Authors conducted a bridge to conduct a bridge search from their original search period (database inception to January 26, 2014) to updated search dates (January 26, 2014 to September 23, 2019).
Screening and Inclusion Criteria
Two review authors (TL and GY) independently screened all bridge search results using uniform inclusion criteria, and the authors discussed and reconciled any disagreements on studies that should be included. For consistency, review authors screened all studies using Potier and colleagues’22 inclusion criteria: title and abstract screen (“written in English”; “related to SI[F]s”) and full-text screen (“(1) peer-reviewed articles that (2) contained original data on SI[F] assessment”). To answer the research questions on SIF effectiveness, review authors then screened studies using additional full-text screening criteria, including: (3) quantitatively measured outcomes, (4) outcomes within stated domains of interest, and (5) effectiveness studies (i.e., SIF versus control condition). This review defined effectiveness studies in the following ways: At the community level, it included studies comparing areas with and without an SIF, before and after SIF implementation, or both. It also included studies comparing outcomes when SIFs were open versus closed. At the individual level, this review considered studies comparing PWID who use SIFs to PWID who do not or studies comparing frequent SIF users to infrequent users (control). For completeness, review authors also extracted and screened the references of the studies included after the first round of screening (“snowball screen”). Finally, review authors considered all included studies from the Potier et al.22 review for a second round of full-text screening using additional criteria.
Assessing and Summarizing the Body of Evidence on Effectiveness
Using Community Guide methods,23,24 review authors assessed each study for threats to internal and external validity and suitability of study design. Threats included inadequate description of intervention or control condition, population, or sampling frame; inadequate measurement of exposure or outcome; inadequate description or inappropriate use of analytic methods; high attrition; or failure to control for confounding or biasing factors. Each threat was assigned 1 limitation. Review authors categorized studies’ quality of execution as good (0–1 limitation), fair (2–4 limitations), or limited (>4 limitations). Studies with limited quality of execution were excluded. Review authors categorized each study by its suitability of study design (greatest, moderate, least) using standard Community Guide methods.23
This review determined papers to be “linked” if multiple papers investigated the same underlying cohort of individuals in an overlapping study period and measured the same or similar outcomes. An example of a “linked” study would be papers from the same authors—a paper reporting the initial outcomes of the study, and a second paper reporting the same outcomes measured in the same way several years later. In the case of “linked” papers, review authors used the most recent results.
Two review authors (combinations of TL, GY, MD, SO) independently abstracted each study using a standardized data collection form that was designed and approved by all authors. Authors collected data on study design; location; urbanicity; whether the SIF was legally sanctioned; whether possession of injectable drugs is illegal, legal, or decriminalized; study duration; intervention/SIF program details; statistical analysis; sample size; demographic information; outcomes; and conclusions. Authors discussed and reconciled any disagreements in weekly meetings.
Given the heterogeneity of outcome measurements from included studies, this review did not attempt quantitative synthesis and did not calculate summary measures. Instead, it provided a narrative synthesis and summary tables of study results, organized by outcome domains. Review authors stratified results by suitability of study design, highlighting studies with greatest suitability. Because authors did not conduct a meta-analysis, they were unable to assess publication bias using standard methods.26
Evidence Synthesis
Search Yield
This review identified 732 unique records from the bridge search. After title and abstract screening, review authors identified 95 studies potentially related to SIF effectiveness (Figure 1). They then screened using the Potier and colleagues22 criteria and added in records identified from references (“snowball screen”) and from the Potier et al. review. After screening using this review’s additional inclusion criteria, authors identified 29 effectiveness papers.27–55 They removed 3 papers27,30,32 with limited quality of execution and consolidated 7 papers37–39,47,50,52,54 into 3 linked studies39,47,54 (removing 4 records37,38,50,52). The final yield included 22 effectiveness studies (Figure 1).
Figure 1.
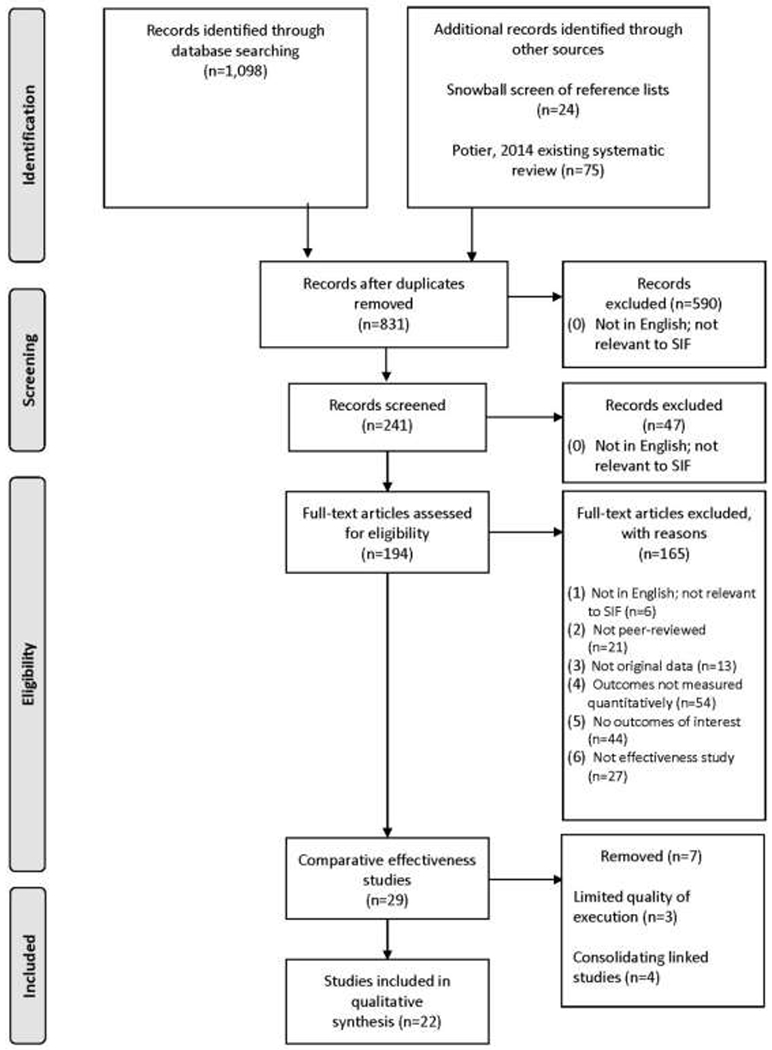
PRISMA flow diagram of search and screening process.
SIF, supervised injection facilities.
Quality of Execution Assessment
Of the 22 included studies.28,29,31,33–36,39–49,51,53–55 8 studies39–41,46,48,49,51,54 had good quality of execution (1 or no limitation); the other 14 had fair quality of execution (2–4 limitations). Of the 14 studies with fair quality of execution, 6 studies29,35,43,44,47,52 received 2 limitations and 8 studies28,31,33,34,36,42,45,53 received 3 limitations. The most common limitation was related to poor description of methods or poor reporting of demographic data among 10 of the 22 studies29,31,33,36,40,42–45,53 (Appendix).
Study Characteristics
Table 1 synthesizes demographic characteristics from included studies with individual-level data. As with previous reviews, most included studies came from Vancouver, Canada (16 studies33–35,41,43–45,49,51–54) or Australia (3 studies36,47,48), though a few studies came from locations in Europe that were not included in the Potier and colleagues review22 (3 studies 28,31,40). On average, two thirds of clients of the SIFs in included studies were men; a quarter of clients were experiencing homelessness. History of incarceration was common in the study populations of included studies, as were HIV and hepatitis C virus infection and poor mental health indicators. Most clients of SIFs injected heroin, followed by stimulants. Finally, study participants (SIF clients and non-clients) reported high levels of syringe sharing behavior and history of overdose, regardless of SIF use.
Table 1.
Synthesized Demographic Characteristics
| Characteristics | Number of studies,a n | Median (if n ≥3) | IQR (n≥5) | Unique measures / details (if n <3) |
|---|---|---|---|---|
| Location | ||||
| Canada | 16 | – | – | Vancouver, British Columbia (n=16) |
| Australia | 3 | – | – | Sydney, New South Wales (n=3) |
| Europe | 3 | – | – | • Catalonia, Spain • Barcelona and Madrid, Spain • Oslo, Norway |
| Standard demographics | ||||
| Sample size, n | 8 | 707 | (499–1,146.5) | – |
| Age, years | 5 | 38 | (35.7–39) | Age >30 years: 48.8% Age (all under 30) ≤25: 59(23.7%) >25: 190(76.3) |
| Sex, % male | 8 | 71 | (66–74.9) | |
| SES | ||||
| Income | 0 | – | – | – |
| Education (primary or lower), % | 2 | – | – | 53.5; 29.7 |
| Homelessness or unstable housing, % | 5 | 19 | (11.1–26.5) | – |
| Employment | 3 | (1) 14.7 employed; (2) 57.7 social security income; (3) marginal/illegal source of income (47.4%) | ||
| Insurance, % insured | 7 | 100 | (100–100) | – |
| Race/Ethnicity | ||||
| White, % | 2 | – | – | 59, 80.1 |
| Non-White, % | 2 | – | – | 41, 19.9 |
| Native American/Indigenous/Aboriginal, % | 3 | 21 | – | – |
| Marginalized identity | ||||
| Prison, % | 5 | (1) Ever in prison: 73.9; (2) ever in prison 13.7; (3) incarceration: 34.3; (4) recent prison 25.2; (5) recently incarcerated 29.6 | ||
| Sex work, % | 4 | 12.5 | – | Traded sex for drugs: 18.5 |
| HIV positive, % | 4 | 29.0 | – | – |
| HCV positive, % | 4 | 75.1 | – | – |
| Mental health, % | 2 | – | – | Previous psychiatric illness/self-harm: 19.8; 89.4 |
| Drug use behaviors | ||||
| Drug of use | 2 | – | – | • Cocaine injection; greater than once daily: 24.6% • Heroin injection; greater than once daily: 50.3% • Crack use; greater than once daily: 6.6% Drug most frequently injected: • Speedball: 108 (43.4%) • Heroin or cocaine separately: 141 (56.6%) |
| Years of injection drug use | 1 | – | – | 15.8 years (SD=9.8) |
| Frequency of use, % weekly or more | 2 | – | – | 87.4; 58.2 |
| Syringe sharing, % lending or borrowing | 4 | 8.2 | – | – |
| Equipment sharing | 2 | – | – | (1) Shared injecting equipment indirectly: 69 (27.7%) (69 of 216): (broken down further into subcategories listed below. Subcategories are not mutually exclusive, percentage out of total sample (n=216) • 18.1% (33 of 216) for diluting drug in some else’s used cookers • 13.3% (45 of 203) for diluting drug in someone else’s used syringes (back/front loading) • 9.3% (23 of 225) for using filters used by someone else • 7.6% (19 of 230) for rinsing syringes with used liquid • 1.2% (3 of 246) for cleaning cleaned oneself with borrowed used cotton (2) Borrowed needles: 6.1% Lent needles: 7.6 |
| Past overdose, % | 2 | – | – | 19.8%; 11% |
| Current or recent treatment, % | 3 | 31 | – | – |
Number of studies with individual level outcomes, for all rows except location.
Outcomes
Table 2 provides a summary overview of the outcomes reported by each study. Across all included studies, SIFs were associated with significantly favorable differences or changes in all 4 outcome domains, with some studies reporting null associations. No studies reported significantly unfavorable associations. Specifically, there was no demonstrated increase in crime or drug use–related public nuisance, which commonly concern opponents of SIFs.17
Table 2.
Summary Overview of Outcomes
| Author, year | Country | Suitability of study design – Quality of execution | Overdose-induced mortality and morbidity | Injection behaviors and harm reduction | Access to addiction treatment programs | Crime and public nuisance |
|---|---|---|---|---|---|---|
| Marshall, 2011 | Canada | Greatest-Good | ++ | |||
| Salmon, 2010 | Australia | Greatest-Good | ++ | |||
| Linked study: | Canada | Greatest-Fair | + | ++ | ||
| Lloyd-Smith, 2010 | ||||||
| Lloyd-Smith, 2009 | ||||||
| Lloyd-Smith, 2008 | ||||||
| DeBeck, 2011 | Canada | Greatest-Fair | ++ | |||
| Kimber, 2008b | Australia | Greatest-Fair | ++ | |||
| Linked study: | Canada | Greatest-Good | ++ | |||
| Wood, 2007 | ||||||
| Wood, 2006d | ||||||
| Myer, 2017 | Canada | Greatest-Good | ++ | |||
| Linked study: | Australia | Moderate-Fair | ++ | |||
| Salmon, 2007 | ||||||
| Thein, 2005 | ||||||
| Folch, 2018 | Spain | Least-Fair | + | ++ | ++ | ++ |
| Milloy, 2008a | Canada | Least-Fair | ∅ | |||
| Madah-Amiri, 2019 | Norway | Least-Good | ++ | |||
| Kerr, 2005c | Canada | Least-Fair | ++ | |||
| Kerr, 2006a | Canada | Least-Fair | ∅ | |||
| Bravo, 2008 | Spain | Least-Fair | ++ | |||
| Wood, 2005b | Canada | Least-Fair | ++ | |||
| Stoltz, 2007b | Canada | Least-Good | ++ | |||
| Gaddis, 2017 | Canada | Least-Fair | ++ | |||
| Milloy, 2010 | Canada | Least-Fair | ∅ | |||
| McKnight, 2007 | Canada | Least-Fair | ++ | |||
| Milloy, 2009 | Canada | Least-Fair | ∅ | |||
| Wood, 2006a | Canada | Least-Fair | ∅ | |||
| Wood, 2004 | Canada | Least-Good | ++ |
++ favorable and significant (p<0.05); + favorable but not significant (p≥0.05); ∅ not meaningfully different from null; – unfavorable but not significant (p≥0.05) (none); – – unfavorable and significant (p<0.05) (none).
For “Overdose-induced mortality and morbidity”, “Injection behaviors and harm reduction”, and “Crime and public nuisance” a decrease or lower value is favorable; for “Access to addiction treatment programs” an increase or higher value is favorable.
Table 2 shows summary results for the studies assigned “greatest” suitability of study design. There were significantly favorable results reported by this subset of studies across all outcome domains except “injection behaviors and harm reduction,” which had 1 study39 reporting non-significant, but favorable changes. The study with the greatest suitability of study design that examined crime as an outcome observed a sustained decrease in crime following the opening of a SIF; the reduction was only observed in the vicinity of the SIF and was not observed in the rest of the city.
Overdose-Induced Mortality and Morbidity
Five studies31,40,41,43,48 reported outcomes relevant to overdose-induced mortality and morbidity. Two studies with the greatest suitability of design and good quality of execution (Marshall et al.41 and Salmon and colleagues48) found that illicit drug overdose deaths and opioid-involved overdoses, respectively, declined at a greater magnitude in the vicinity of an SIF than in the rest of the city/region. Marshall et al.41 found 26% net reduction in overdose deaths in the area immediately surrounding an SIF in Vancouver, Canada after its establishment as compared with the rest of the city. Salmon and colleagues48 described a greater decline in opioid-related overdoses seen by ambulances in the vicinity of an SIF in Sydney, Australia after it opened compared with the rest of the state where it was located.
Review authors deemed the other 3 studies (Milloy et al.,43 Folch and colleagues,31 and Madah-Amiri et al.40) to be of least suitable study design and fair quality of execution. Milloy and colleagues43 (a prospective cohort study analyzed in a cross-sectional manner) and Folch et al.31 (a cross-sectional study) both assessed the association between frequency of SIF use and prevalence of overdoses among SIF clients. Each study found null or non-significant favorable association (respectively) between frequency and overdose prevalence. Finally, Madah-Amiri and colleagues40 examined a cross-section of ambulance data (like Salmon et al.48) from Oslo, Norway, identifying >1,000 opioid-related overdoses in the study period. Patients were more likely to require ambulance transport for overdose when the SIF was closed for the day. Emergency medical service patients from the SIF displayed more severe initial clinical overdose symptoms than patients experiencing overdose at other locations, though they were less likely to require transport to the hospital (indicating emergency medicine services assessed them as stable, presumably from SIF-administered interventions).
Injection Behaviors and Harm Reduction
Seven studies28,31,34,35,39,49,53 reported outcomes relevant to injection behaviors and harm reduction. One prospective cohort study with greatest suitability of design and fair quality of execution (Lloyd-Smith and colleagues39), found a non-statistically significant, 49% lower odds of developing an injection-related skin infection among “always” attenders of the Vancouver SIF (100% of injections conducted at SIF) versus clients who attended less frequently.
Review authors deemed the other 6 studies to be of least suitability of study design, with 1 study rated “good” quality of execution (Stoltz et al.49) and the rest rated as “fair” (Folch and colleagues,31 Kerr et al.,35 Kerr and colleagues,34 Bravo et al.,28 and Wood and colleagues53). Stoltz et al.,49 Folch and colleagues,31 and Wood et al.53 all examined the association between sharing syringes or equipment and frequency of SIF use (albeit at different thresholds), finding a significantly favorable, lower prevalence of multiple sharing behaviors among “consistent” (≥25% of injections), “frequent” (attending SIF every day when injecting drugs), and “exclusive” SIF users (100% of injection), respectively. Stoltz and colleagues49 and Wood et al.53 were both prospective cohort studies analyzed in a cross-sectional manner, and Folch and colleagues31 was a cross-sectional study. Two other cross-sectional studies— Kerr et al.35 (in Vancouver, Canada) and Bravo and colleagues28 (in Barcelona and Madrid, Spain) —compared SIF users with nonusers more-broadly, both finding significantly lower odds of sharing used syringes associated with SIF use. Finally, Kerr et al.34 using a before–after study design (rather than cross-sectional), identified a null change in community injection drug use and binge drug use in the year before and after the opening of the Vancouver SIF.
Access to Addiction Treatment Programs
Seven studies29,31,33,36,39,44,54 reported outcomes relevant to access to addiction treatment programs. Review authors deemed four studies to be of greatest suitability of study design, with one of these studies (Wood and colleagues54) rated good quality of execution and the rest (Lloyd-Smith et al.,39 DeBeck and colleagues,29 and Kimber et al.36) rated fair. Wood and colleagues,54 DeBeck et al.,29 and Kimber and colleagues36 each calculated hazard ratios for the association between frequency of SIF attendance and access to addiction treatment or detoxification services. They found that frequent SIF use increased the rate of accessing treatment significantly in the study period by anywhere from 1.4 to 1.7 times, as compared with less frequent or nonusers. Lloyd-Smith et al.39 found that, among SIF users hospitalized for injection-related skin infection, about a fifth had received care for their infection by a nurse at the SIF, and those who had been referred to the hospital by a SIF nurse had significantly shorter lengths of stay in the hospital than those who had not been referred.
Review authors categorized the 3 other studies (Folch and colleagues,31 Gaddis et al.,33 and Milloy and colleagues44) as least suitable study design and fair quality of execution. Both Gaddis et al.33 and Milloy and colleagues44 assessed the association between frequent use of the Vancouver SIF and access to care, finding a significant and favorable association with on-site detoxification services and null association with reporting being “unable” to access addiction treatment services, respectively. Folch et al.31 found frequent SIF users in Spain had around twice the odds of accessing addiction treatment services in the previous 6 months as compared with less frequent SIF attendees.
Crime and Drug Use-Related Public Nuisance
Seven studies31,42,45–47,51,52 reported outcomes relevant to crime and drug use–related public nuisance. Review authors determined one study (Myer and colleagues46) to be of greatest suitability and good quality, and another study (Salmon et al.47) to be of moderate suitability and fair quality. The 2017 study of Myer and colleagues46 examined crime in Vancouver, Canada using a quasi-experimental design (interrupted time series with comparison) following the opening of an SIF. The study authors found that crime did not meaningfully change in most of the city, except in the district where the SIF is located, which observed an abrupt, persistent decrease in crime following the SIF’s opening. Salmon et al. took multiple snapshots of resident and business owner reports of crime and drug use–related nuisance indicators before and after an SIF opened in Sydney. Over 5 years, the study authors witnessed a significant decrease in the proportion of residents and business owners reporting witnessing public injecting or observing publicly discarded syringes. Over the same time period, there was no change in proportion of residents or business operators who had been offered drugs for purchase.
Review authors deemed the 5 remaining studies (Folch and colleagues,31 McKnight et al.,42 Wood and colleagues,51 Milloy et al.,45 and Wood and colleagues52) to be of least suitable study design and fair quality (with the exception of Wood et al.,51 which was deemed good quality). Wood and colleagues51 in 2004 examined drug use–related public nuisance measures in the weeks before and after the Vancouver SIF opened, finding significant reductions in public injection, publicly discarded syringes, and injection-related litter after the SIF opened. In 2006, Wood et al.52 examined Vancouver crime records in the year before and after the Vancouver SIF opened. The study authors found no meaningful or significant changes in drug trafficking and assaults/robbery, but observed significant declines in vehicle break-ins/theft. Milloy and colleagues45 (a prospective cohort study analyzed in a cross-sectional manner) found no association between frequent SIF use and recent incarceration. McKnight et al.42 (a cross-sectional study) found that public injecting was significantly less likely when the SIF did not have a wait time (i.e., the SIF was readily available). Folch and colleagues31 (a cross-sectional study in 2018) found that frequent SIF attendees were significantly less likely to inject in public and significantly more likely to dispose of used syringes safely.
DISCUSSION
Implications for Research
This review highlights several evidence gaps warranting further investigation. First, SIFs are increasingly common, yet scientific evaluation has only occurred in a limited number of international settings. Most effectiveness studies originate in Vancouver, Canada or Sydney, Australia. Research is needed in a broader range of settings, including resource-poor and politically diverse settings, to enhance the generalizability and utility of findings within this literature. Drug use behaviors differ between settings, as do structural factors such as the legality of substances, law enforcement practices, and cultural stigma. However, more studies are being published in an increasing number of settings. One study by Kral et al.56 published after the search period ended examined an unsanctioned SIF at an undisclosed U.S. location. The authors found that after 5 years of observation and >10,000 injection events, there was not a single overdose death that occurred at the site. This finding is consistent with the included studies, none of which observed any fatal overdoses at their respective SIFs.
Review authors also found that most effectiveness studies had the “least” suitable quality of design (e.g., they were cross-sectional studies, before–after studies, or were prospective cohort studies analyzed in a cross-sectional manner). This likely reflects a historical, systemic withholding of funding and limited governmental support for harm reduction interventions.57,58 It also reflects the reality that SIFs are first and foremost community responses to crises; structuring ideal research conditions is, rightly, not their priority. Evaluators should advocate for more empirically rigorous study designs whenever possible. Potential low-resource, high-rigor studies that would inform implementation, if not effectiveness, would be testing, observing, and evaluating the effectiveness of distinct components of the SIF intervention (e.g., staffing, hours of operation, policy changes). Third, the inconsistent measurement of outcomes, heterogeneous control groups, and high number of linked studies in the existing literature make quantitative synthesis difficult. Efforts to standardize outcome measures across sites and studies are needed. Finally, no effectiveness studies in the bridge search assessed how SIFs are responding to emerging trends in the opioid overdose epidemic. Future work should explicitly consider the changing patterns of drug-related overdose and other health harms experienced in diverse populations of PWID.
This systematic review has similar conclusions to other well-conducted systematic reviews20,21 The present review’s use of Community Guide methods frames the findings in the language of U.S. decision makers. The goal with this systematic review is to inform debates between local municipalities considering implementing SIFs7–9 and the U.S. federal government, which as of this writing, still considers such harm reduction interventions illegal under federal law.10,11
Implications for Practice
For policymakers, this review relays evidence from a growing body of literature demonstrating the effectiveness of SIFs in reducing overdose mortality and frequency, as well as improving access to addiction treatment. These outcomes were observed with no increase in crime and drug use–related public nuisance. In fact, several included studies in this review documented decreases in crime following the opening of SIFs. Given the narrow focus in the literature on the SIFs in Vancouver and Sydney, decision makers should assess whether there is a potential benefit for their local populations struggling with SUDs. There is a broader literature on SIFs that does not focus on effectiveness specifically and includes research from a number of sites beyond those featured here. The review authors plan to qualitatively synthesize implementation strategies used to establish and operate SCFs in a forthcoming systematic review.
Overall, the studies included in this systematic review suggest SIFs are associated with reduced rates of overdose morbidity and mortality, increased access to addiction treatment, and minimal change or even reductions in crime and drug use–related public nuisance.
As the debate over SIFs in the U.S. and in other countries progresses, and as the overdose epidemic evolves, there is only so much systematic reviews will ever be able to demonstrate to stay current. In addition to scientific evidence, other considerations for decision makers include ethics, funding, and most importantly, the right to appropriate and quality health care for all groups of people, regardless of any stigmatized behaviors or qualities.
Limitations
This review also has limitations. First, given the pronounced focus of research on SIFs in Vancouver and Sydney, the generalizability of findings to other locations is uncertain. However, this review includes more sites than the previous review of Potier and colleagues,22 suggesting that research may be expanding to include additional locations. Another limitation is publication bias, in which favorable results are published and null or unfavorable results may be less likely to be published. Third, the heterogeneity of comparisons (SIF versus various controls) in these studies (Appendix) and outcome measures makes synthesis difficult. Finally, to avoid further heterogeneity, the review authors did not include overdose prevention sites; future work should consider these related harm reduction interventions.
CONCLUSIONS
This systematic review of 22 effectiveness studies relayed evidence of the public health benefits of supervised injection facilities for SIF clients as well as surrounding communities. The strongest evidence suggests that SIFs may help reduce overdose morbidity and mortality and improve access to addiction treatment. An increase in crime, an often-cited concern of SIF opponents, was not observed to be associated with SIFs in most included studies, and crime was actually found to decrease in 2 studies (1 greatest and 1 least suitability of design).
Supplementary Material
ACKNOWLEDGMENTS
The research presented in this paper is that of the authors and does not reflect the official policy of NIH. The findings and conclusions in this study have not been formally determined by the Community Preventive Services Task Force or disseminated by the Centers for Disease Control and Prevention and should not be construed to represent any Community Preventive Services Task Force or agency determination or policy. Dr. Brandon Marshall provided subject matter expert feedback at end of the review process—he had no involvement with screening or quality assessment of his own (or others’) included studies.
Timothy W. Levengood, Grace H. Yoon, Melissa J. Davoust, and Shannon N. Ogden were supported by the National Institute on Drug Abuse of the National Institutes of Health under award number T32DA04189803. Brandon D.L. Marshall was supported by the National Institute on Drug Abuse (R01-DA046620) and the National Institute of General Medical Sciences (P20-GM125507) during the conduct of this study. Sean R. Cahill was supported by the Fenway Institute general funds. Angela R. Bazzi was supported by NIH under award numbers K01DA043412, R01DA051849, and P30AI042853, and the Boston University Peter Paul Professorship. The study sponsors had no role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Timothy W. Levengood was involved in all aspects of the systematic review and publication. He led the conception and design of the study, data acquisition, abstraction of all articles, data analysis and interpretation; wrote the article and revised the article for important intellectual content; and read and approved the final version of the submitted manuscript. Grace H. Yoon was involved in all aspects of the systematic review and publication. She made a substantial contribution to the conception and design of the study, data acquisition, abstraction of articles, data analysis and interpretation; revised the article for important intellectual content; and read and approved the final version of the submitted manuscript. Melissa J. Davoust was involved in most aspects of the systematic review and publication. She made a substantial contribution to data acquisition, abstraction of articles, data analysis and interpretation; revised the article for important intellectual content; and read and approved the final version of the submitted manuscript. Shannon N. Ogden was involved in most aspects of the systematic review and publication. She made a substantial contribution to data acquisition, abstraction of articles, data analysis and interpretation; revised the article for important intellectual content; and read and approved the final version of the submitted manuscript. Brandon D.L. Marshall made a substantial contribution to the conception of the study and to data interpretation; revised the article for important intellectual content; and read and approved the final version of the submitted manuscript. Sean R. Cahill made a substantial contribution to the conception of the study and design of the study and to data interpretation; revised the article for important intellectual content; and read and approved the final version of the submitted manuscript. Angela R. Bazzi made a substantial contribution to the conception of the study and design of the study and to data interpretation; revised the article for important intellectual content; and read and approved the final version of the submitted manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The near-final results of this study were presented at the annual meeting of the American Public Health Association on October 27, 2020.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Understanding the Epidemic. Opioid Overdose. Centers for Disease Control and Prevention, https://www.cdc.gov/drugoverdose/epidemic/index.html. Published 2020. Accessed October 19, 2020. [Google Scholar]
- 2.What is the U.S. Opioid Epidemic? HHS. https://www.hhs.gov/opioids/about-the-epidemic/index.html. Published 2020. Accessed October 19, 2020.
- 3.Jones CM, McCance-Katz EF. Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug Alcohol Depend. 2019;197:78–82. 10.1016/j.drugalcdep.2018.12.030. [DOI] [PubMed] [Google Scholar]
- 4.Medications to Treat Opioid Use Disorder Research Report How effective are medications to treat opioid use disorder. National Institute on Drug Abuse, HHS. https://www.drugabuse.gov/publications/research-reports/medications-to-treat-opioid-addiction/efficacy-medications-opioid-use-disorder. Published 2020. Accessed October 8, 2020. [Google Scholar]
- 5.Jones CM, Bekheet F, Park JN, Alexander GC. The evolving overdose epidemic: synthetic opioids and rising stimulant-related harms. Epidemiol Rev. 2020;42(1):154–166. 10.1093/epirev/mxaa011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alcohol and Substance Use. Centers for Disease Control and Prevention, HHS. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/stress-coping/alcohol-use.html. Published 2020. Accessed October 19, 2020. [Google Scholar]
- 7.Buell S In Opening a Safe Injection Site, Somerville Would Call Feds’Bluff. Boston Magazine. August 14, 2019. [Google Scholar]
- 8.Allyn B Philadelphia Nonprofit Opening Nation’s 1st Supervised Injection Site Next Week. National Public Radio. February 26, 2020. [Google Scholar]
- 9.Kornfield M, Wan W. America needs to reduce soaring overdoses. A secret supervised injection site may show us how. The Washington Post. July 10, 2020. [Google Scholar]
- 10.Crack House Statute, 21 USCA §856(2006).
- 11.Beletsky L, Davis CS, Anderson E, Burris S. The law (and politics) of safe injection facilities in the United States. Am J Public Health. 2008;98(2):231–237. 10.2105/ajph.2006.103747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.International Network of Drug Consumption Rooms. Drug Consumption Rooms (DCRs) in the world. http://www.drugconsumptionroom-international.org/index.php#. Published 2020. Accessed October 19, 2020.
- 13.European Monitoring Centre for Drugs and Drug Addiction. Drug consumption rooms: an overview of provision and evidence. Lisbon, Portugal: European Monitoring Centre for Drugs and Drug Addiction; 2018. https://www.emcdda.europa.eu/topics/pods/drug-consumption-rooms_en. Accessed May 10, 2021. [Google Scholar]
- 14.Marlatt GA, Tapert SF. Harm reduction: reducing the risks of addictive behaviors. In: Addictive behaviors across the life span: Prevention, treatment, and policy issues. Thousand Oaks, CA: Sage Publications, Inc; 1993:243–273. [Google Scholar]
- 15.Prevention. Centers for Disease Control and Prevention, HHS, Picture of America. https://www.cdc.gov/pictureofamerica/pdfs/picture_of_america_prevention.pdf. Published 2017. Accessed October 19, 2020.
- 16.Supervised Consumption Sites. Vancouver Coastal Health, http://www.vch.ca/public-health/harm-reduction/supervised-consumption-sites. Published 2020. Accessed October 19, 2020.
- 17.Rosenstein RJ. Fight Drug Abuse, Don’t Subsidize It. The New York Times. August 27, 2018; Opinion. [Google Scholar]
- 18.Supervised Injection Services Community Consultations Report. Windsor-Essex County Health Unit, https://www.wechu.org/reports/supervised-injection-services-community-consultations-report. Published 2019. Accessed May 10, 2021.
- 19.Belackova V, Salmon AM, Day CA, et al. Drug consumption rooms: a systematic review of evaluation methodologies. Drug Alcohol Rev. 2019;38(4):406–422. 10.1111/dar.12919. [DOI] [PubMed] [Google Scholar]
- 20.Caulkins JP, Pardo B, Kilmer B. Supervised consumption sites: a nuanced assessment of the causal evidence. Addiction. 2019;114(12):2109–2115. 10.1111/add.14747. [DOI] [PubMed] [Google Scholar]
- 21.Kennedy MC, Karamouzian M, Kerr T. Public health and public order outcomes associated with supervised drug consumption facilities: a systematic review. Curr HIV/AIDS Rep. 2017;14(5):161–183. 10.1007/s11904-017-0363-y. [DOI] [PubMed] [Google Scholar]
- 22.Potier C, Laprévote V, Dubois-Arber F, Cottencin O, Rolland B. Supervised injection services: what has been demonstrated? A systematic literature review. Drug Alcohol Depend. 2014;145:48–68. 10.1016/j.drugalcdep.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 23.Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based Guide to Community Preventive Services--methods. The Task Force on Community Preventive Services. Am J Prev Med. 2000;18(1 suppl):35–43. 10.1016/s0749-3797(99)00119-1. [DOI] [PubMed] [Google Scholar]
- 24.Zaza S, Wright-De Agüero LK, Briss PA, et al. Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Task Force on Community Preventive Services. Am J Prev Med. 2000;18(1 suppl 1):44–74. 10.1016/s0749-3797(99)00122-1. [DOI] [PubMed] [Google Scholar]
- 25.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahmed I, Sutton AJ, Riley RD. Assessment of publication bias, selection bias, and unavailable data in meta-analyses using individual participant data: a database survey. BMJ. 2012;344:d7762. 10.1136/bmj.d7762. [DOI] [PubMed] [Google Scholar]
- 27.Belackova V, Silins E, Salmon AM, Jauncey M, Day CA. “Beyond safer injecting” - health and social needs and acceptance of support among clients of a supervised injecting facility. Int J Environ Res Public Health. 2019;16(11):2032. 10.3390/ijerph16112032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bravo MJ, Royuela L, De la Fuente L, et al. Use of supervised injection facilities and injection risk behaviours among young drug injectors. Addiction. 2009;104(4):614–619. 10.1111/j.1360-0443.2008.02474.x. [DOI] [PubMed] [Google Scholar]
- 29.DeBeck K, Kerr T, Bird L, et al. Injection drug use cessation and use of North America’s first medically supervised safer injecting facility. Drug Alcohol Depend. 2011;113(2–3):172–176. 10.1016/j.drugalcdep.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fitzgerald J, Burgess M, Snowball L. Trends in property and illicit drug crime around the medically supervised injecting centre in Kings Cross: an update. Crime and Justice Statistics. 2010;51. https://apo.org.au/sites/default/files/resource-files/2010-10/apo-nid22857.pdf. Accessed May 10, 2021. [Google Scholar]
- 31.Folch C, Lorente N, Majó X, et al. Drug consumption rooms in Catalonia: a comprehensive evaluation of social, health and harm reduction benefits. Int J Drug Policy. 2018;62:24–29. 10.1016/j.drugpo.2018.09.008. [DOI] [PubMed] [Google Scholar]
- 32.Freeman K, Jones CG, Weatherburn DJ, Rutter S, Spooner CJ, Donnelly N. The impact of the Sydney Medically Supervised Injecting Centre (MSIC) on crime. Drug Alcohol Rev. 2005;24(2):173–184. 10.1080/09595230500167460. [DOI] [PubMed] [Google Scholar]
- 33.Gaddis A, Kennedy MC, Nosova E, et al. Use of on-site detoxification services co-located with a supervised injection facility. J Subst Abuse Treat. 2017;82:1–6. 10.1016/j.jsat.2017.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kerr T, Stoltz J-A, Tyndall M, et al. Impact of a medically supervised safer injection facility on community drug use patterns: a before and after study. BMJ. 2006;332(7535):220. 10.1136/bmj.332.7535.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kerr T, Tyndall M, Li K, Montaner J, Wood E. Safer injection facility use and syringe sharing in injection drug users. Lancet. 2005;366(9482):316–318. 10.1016/s0140-6736(05)66475-6. [DOI] [PubMed] [Google Scholar]
- 36.Kimber J, Mattick RP, Kaldor J, van Beek I, Gilmour S, Ranee JA. Process and predictors of drug treatment referral and referral uptake at the Sydney Medically Supervised Injecting Centre. Drug Alcohol Rev. 2008;27(6):602–612. 10.1080/09595230801995668. [DOI] [PubMed] [Google Scholar]
- 37.Lloyd-Smith E, Wood E, Zhang R, Tyndall MW, Montaner JS, Kerr T. Determinants of cutaneous injection-related infection care at a supervised injecting facility. Ann Epidemiol. 2009;19(6):404–409. 10.1016/j.annepidem.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 38.Lloyd-Smith E, Wood E, Zhang R, Tyndall MW, Montaner JSG, Kerr T. Risk factors for developing a cutaneous injection-related infection among injection drug users: a cohort study. BMC Public Health. 2008;8:405. 10.1186/1471-2458-8-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lloyd-Smith E, Wood E, Zhang R, et al. Determinants of hospitalization for a cutaneous injection-related infection among injection drug users: a cohort study. BMC Public Health. 2010;10:327. 10.1186/1471-2458-10-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Madah-Amiri D, Skulberg AK, Braarud AC, et al. Ambulance-attended opioid overdoses: An examination into overdose locations and the role of a safe injection facility. Subst Abus. 2019;40(3):383–388. 10.1080/08897077.2018.1485130. [DOI] [PubMed] [Google Scholar]
- 41.Marshall BD, Milloy MJ, Wood E, Montaner JS, Kerr T. Reduction in overdose mortality after the opening of North America’s first medically supervised safer injecting facility: a retrospective population-based study. Lancet. 2011;377(9775):1429–1437. 10.1016/s0140-6736(10)62353-7. [DOI] [PubMed] [Google Scholar]
- 42.McKnight I, Maas B, Wood E, et al. Factors associated with public injecting among users of Vancouver’s supervised injection facility. Am J Drug Alcohol Abuse. 2007;33(2):319–325. 10.1080/00952990601175102. [DOI] [PubMed] [Google Scholar]
- 43.Milloy MJ, Kerr T, Mathias R, et al. Non-fatal overdose among a cohort of active injection drug users recruited from a supervised injection facility. Am J Drug Alcohol Abuse. 2008;34(4):499–509. 10.1080/00952990802122457. [DOI] [PubMed] [Google Scholar]
- 44.Milloy MJ, Kerr T, Zhang R, Tyndall M, Montaner J, Wood E. Inability to access addiction treatment and risk of HIV infection among injection drug users recruited from a supervised injection facility. J Public Health (Oxf). 2010;32(3):342–349. 10.1093/pubmed/fdp089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Milloy MJ, Wood E, Tyndall M, Lai C, Montaner J, Kerr T. Recent incarceration and use of a supervised injection facility in Vancouver, Canada. Addict Res Theory. 2009;17(5):538–545. 10.1080/16066350802023065. [DOI] [Google Scholar]
- 46.Myer AJ, Belisle L. Highs and lows: an interrupted time-series evaluation of the impact of North America’s only supervised injection facility on crime. J Drug Issues. 2017;48(1):36–49. 10.1177/0022042617727513. [DOI] [Google Scholar]
- 47.Salmon AM, Thein HH, Kimber J, Kaldor JM, Maher L. Five years on: what are the community perceptions of drug-related public amenity following the establishment of the Sydney Medically Supervised Injecting Centre? Int J Drug Policy. 2007;18(1):46–53. 10.1016/j.drugpo.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 48.Salmon AM, van Beek I, Amin J, Kaldor J, Maher L. The impact of a supervised injecting facility on ambulance call-outs in Sydney, Australia. Addiction. 2010;105(4):676–683. 10.1111/j.1360-0443.2009.02837.x. [DOI] [PubMed] [Google Scholar]
- 49.Stoltz JA, Wood E, Small W, et al. Changes in injecting practices associated with the use of a medically supervised safer injection facility. J Public Health (Oxf). 2007;29(1):35–39. 10.1093/pubmed/fdl090. [DOI] [PubMed] [Google Scholar]
- 50.Thein H-H, Kimber J, Maher L, MacDonald M, Kaldor JM. Public opinion towards supervised injecting centres and the Sydney Medically Supervised Injecting Centre. Int J Dnig Policy. 2005;16(4):275–280. 10.1016/j.drugpo.2005.03.003. [DOI] [Google Scholar]
- 51.Wood E, Kerr T, Small W, et al. Changes in public order after the opening of a medically supervised safer injecting facility for illicit injection drug users. CMAJ. 2004;171(7):731–734. 10.1503/cmaj.1040774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wood E, Tyndall MW, Lai C, Montaner JSG, Kerr T. Impact of a medically supervised safer injecting facility on drug dealing and other drug-related crime. Subst Abuse Treat Prev Policy. 2006;1:13. 10.1186/1747-597x-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wood E, Tyndall MW, Stoltz J-A, et al. Factors associated with syringe sharing among users of a medically supervised safer injecting facility. Am J Infect Dis. 2005;1(1):50–54. [Google Scholar]
- 54.Wood E, Tyndall MW, Zhang R, Montaner JSG, Kerr T. Rate of detoxification service use and its impact among a cohort of supervised injecting facility users. Addiction. 2007;102(6):916–919. 10.1111/j.1360-0443.2007.01818.x. [DOI] [PubMed] [Google Scholar]
- 55.Wood E, Tyndall MW, Zhang R, et al. Attendance at supervised injecting facilities and use of detoxification services. N Engl J Med. 2006;354(23):2512–2514. 10.1056/nejmc052939. [DOI] [PubMed] [Google Scholar]
- 56.Kral AH, Lambdin BH, Wenger LD, Davidson PJ. Evaluation of an unsanctioned safe consumption site in the United States. N Engl J Med. 2020;383(6):589–590. 10.1056/nejmc2015435. [DOI] [PubMed] [Google Scholar]
- 57.Hyshka E, Anderson-Baron J, Karekezi K, et al. Harm reduction in name, but not substance: a comparative analysis of current Canadian provincial and territorial policy frameworks. Harm Reduct J. 2017;14:50. 10.1186/s12954-017-0177-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Showalter D Federal funding for syringe exchange in the US: explaining a long-term policy failure. Int J Drug Policy. 2018;55:95–104. 10.1016/j.drugpo.2018.02.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


