Abstract
Background:
Many childhood cancer survivors experience at least one late effect of treatment, and both late effects and persistent cancer-related worry can negatively impact quality of life in survivorship. Little is known about the prevalence or impact of parental worry about late effects early in treatment. This study evaluated parental perceived likelihood, impact, and worry about late effects of childhood cancer.
Procedure:
We surveyed 96 parents of pediatric cancer patients at Dana Farber/Boston Children’s Cancer and Blood Disorders Center within a year of diagnosis. Parents were asked about their experiences with late effects communication, general worry about late effects, and specific late effect worries.
Results:
Most (96%) parents valued information about late effects, and 93% considered late effects in their treatment decision-making. Yet, 24% could not recall receiving any information about late effects, and only 51% felt well prepared for potential late effects. Though only 20% of parents considered their child at high risk of experiencing late effects, 61% were extremely/very worried about late effects. Those who felt their child was at high risk of experiencing late effects were more likely to worry (OR=4.7, p=0.02).
Conclusions:
Many parents feel inadequately informed about late effects of cancer treatment, and only one-fifth of parents consider late effects to be likely for their child. However, a majority of parents worry about late effects, including ones they think their child is unlikely to experience. While some worry is anticipated, disproportionate worry may be mitigated by addressing both educational shortfalls and emotional concerns.
Keywords: Pediatrics, Late effects, Health-care communication, Cancer worry, Quality of Life
Introduction:
When a child is diagnosed with cancer and begins cancer treatment, the child’s parents often have a multitude of questions about the diagnosis, prognosis, acute toxicities of treatment, life disruptions for the child and family, and the child’s life after cancer treatment.1 While early care discussions aim to address these concerns,2 many parents find these conversations overwhelming and distressing.3 Perhaps as a result, parents often have persistent information needs about these topics,4 may have ongoing worries about their child’s health and quality of life (QOL) throughout treatment, and some may suffer from persistent stress and anxiety.5,6 Many parents have lingering concerns about their child’s health and potential late effects of therapy in survivorship.7–9
These uncertainties are not unfounded. While pediatric cancer mortality has continued to improve, with relative survival rates of 85% in the most recent treatment era,10 many childhood cancer survivors have substantial morbidity from treatment. A majority of survivors experience at least one long-term health condition, or late effect, as a result of cancer treatment.11 Despite parental desire for early information about late effects of treatment,1,12–14 potential late effects do not usually take center stage in early treatment discussions.15 As a result many parents feel they lack the information they need to participate in care decisions,13 and many feel sub-optimally prepared for their child’s cancer survivorship.16
Worry about late effects is prevalent during survivorship for both parents and patients alike,17–19 and has been described during treatment for adolescents and young adults with cancer.20 Some degree of worry is expected. However, persistent or disproportionate levels of other types of cancer-related worries, such as fear of cancer recurrence, have been shown to negatively impact QOL, relationships, and psychological outcomes in survivors of both pediatric and adult cancer.19,21 The prevalence and impact of early parental worry about late effects is poorly understood, yet the disjunct between parental desire for information about late effects starting from the time of diagnosis14 and parental feelings of inadequate preparation, suggests that parental late effects worry may begin early. In this study, we aimed to elucidate the intersection between parental worry about late effects, understanding of risk of late effects, and the role late effect worries play in treatment decision-making. We hypothesized that many parents would be worried about late effects early in treatment and that those parents who felt their children were most likely to experience late effects may be most worried.
Methods:
We surveyed parents of children with cancer at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center about their late effects communication experiences from November 2016 to June 2018.22 Permission to approach was obtained from the child’s primary oncologist; parents were approached to participate within a year of their child’s oncologic diagnosis. One parent per child completed the survey. Eligibility criteria included child ≤18 years of age, parent able to read English, and ongoing receipt of initial cancer directed therapy. See Supplemental Table 1 for additional details on patient eligibility and screening. All parents who participated in this study had received and signed an informed consent document which listed potential acute and long-term effects of their child’s chemotherapy per our institutional standard. Parents of children whose oncologist determined they had incurable disease were ineligible as this study focused on long-term outcomes. Eligible parents were approached in-person in the outpatient clinic or inpatient hospital with a letter describing participation. Parent surveys were administered electronically on tablet computers. As a token of appreciation, participants received a $20 gift card. The institutional review board of the Dana-Farber Cancer Institute approved this study; documentation of informed consent was waived per the IRB’s recommendation.
Data Collection:
Parents completed a 39-item survey that included previously utilized items or adapted items drawn from established questionnaires.16,22–26 Limited novel items were developed after literature review, employing general principles of survey design.27 The survey was pilot tested with 12 parents to assess face and content validity and took approximately 15–20 minutes to complete.
Surveys focused on parents’ experiences with cancer-related communication and decision-making about potential late effects. Receipt of late effects information was evaluated by asking parents if they were ever told that their child “may have a risk of having future health problems after treatment is finished” (yes/no).28 We also assessed parental experience of early communication about late effects with the following established items and scales, all with response options extremely, very, somewhat, a little, not at all:
Preparedness for late effects was assessed by asking how well information from their child’s oncologist prepared them for the possibility of “health problems after treatment is finished”.16
Importance of late effects information was evaluated by asking, “how important is it to you to receive information about the possibility that your child could have health problems after treatment is finished”.16
Influences on treatment decision-making was assessed by asking “when making decisions about treatment” how important was “having as few long-term health effects from treatment after treatment is finished,” “offering the best chance of cure,” and “minimizing acute effects of treatment”.29
The primary outcome for this analysis was parental worry about late effects which was assessed by asking how worried parents were that their child “could experience health problems after treatment is finished.”9,26 The secondary outcome was parental perception of their child’s risk of experiencing late effects, which was evaluated by asking how likely it is that their child would “develop health problems after treatment is finished.”16 Both items had response categories of extremely, very, somewhat, a little, and not at all.
We also evaluated parental worry, perceived risk, and perceived impact on QOL for 5 specific late effects: neurocognitive impairment, infertility, cardiac toxicity, second malignancies, and impaired growth and development.28 These late effects, which were defined using language targeted towards an 8th grade reading level, were chosen as some of the most common late effects experienced across pediatric cancer survivors, and ones about which parents have questions.30–34 For each late effect we asked parents if they were ever told their child was at risk for the specified late effect (yes/no/I don’t remember). Those parents who responded that they had been told their child was at risk were asked if they received “as much information as you wanted” with answers “Yes, definitely,” “yes, somewhat,” and “No.” Parents were also asked their perception of their child’s likelihood of experiencing each late effect, their degree of worry, and how impactful it would be to their child’s QOL should their child experience each late effect, all with response options extremely, very, somewhat, a little, not at all.
The survey also assessed the following potential explanatory factors we hypothesized may be associated with parent late effect worries:
Perceived prognosis: Parents were asked the child’s likelihood of cure.16,25 Prognosis estimations were dichotomized as “favorable” (>75% chance of cure), or “less favorable” (<75% chance of cure) to approximate median survival estimates for all children with cancer.
Dispositional Optimism was evaluated using the Life Orientation Test-Revised scale.35
Parent/child attributes: Parent sex, age, educational level, and race/ethnicity were obtained by questionnaire. Child’s sex, diagnosis, date of diagnosis, and date of birth were obtained by medical record review.
Statistical Methods:
Parent and patient characteristics and responses to items about late effect information preferences were summarized descriptively. Parental worry about late effects was dichotomized as extremely/very vs. somewhat/a little/not at all. Perceived risk of late effects was similarly dichotomized as high (extremely/very likely) vs. low (moderately/somewhat/unlikely). Univariable logistic regression was used to evaluate factors associated with heightened late effect worries. Explanatory factors were dichotomized consistent with prior work, with pre-specified cutoffs as shown in the tables and text.29
For each of the 5 specific late effects assessed, Fisher’s Exact Test was used to evaluate the association between parental worry about that late effect and perceived risk of experiencing the late effect, and between worry and perceived impact on QOL. Two-sided p-values <0.05 were considered statistically significant. Statistical analyses were conducted using SAS version 9.4 (SAS Institute, Inc, Cary, NC).
Results:
Characteristics of participating parents and their children are described in Table 1. Eighty-two percent (96/117) of eligible parents who were approached completed the questionnaire. Parents who declined participation (n=21) had children with similar ages and diagnoses as participating parents. Participating parents were largely female (74%), white (85%), and college educated (76%). A majority of their children had a hematologic malignancy (55%).
TABLE 1.
Characteristics of Participating Parents and their Children (N=96)
| Parent Characteristics | N (%) |
|---|---|
| Gender | |
| Female | 71/96 (74) |
| Race | |
| White | 80/94 (85) |
| Black | 3/94 (3) |
| Asian/Pacific Islander | 8/94 (9) |
| Other | 3/94 (3) |
| Ethnicity | |
| Hispanic | 9/95 (9) |
| Education | |
| <College graduate | 23/96 (24) |
| College graduate | 45/96 (47) |
| Graduate/professional school | 28/96 (29) |
| Child Characteristics | N (%) |
| Child age at diagnosis in years | |
| 0–2 | 17/96 (18) |
| 3–6 | 37/96 (39) |
| 7–12 | 23/96 (24) |
| 13–18 | 19/96 (20) |
| Gender | |
| Female | 43/96 (45) |
| Child Diagnosis | |
| Hematologic malignancy | 53/96 (55) |
| Extracranial Solid tumor | 32/96 (33) |
| Brain tumor | 11/96 (11) |
| Parent Perception of Prognosis | |
| Favorable (≥75% chance of cure) | 82/94 (87) |
| Treatment Receiveda | |
| Chemotherapy | 96/96 (100) |
| Radiation | 22/96 (23) |
| Surgery | 40/96 (42) |
| Stem cell transplant | 5/96 (5) |
| Days from diagnosis to survey, median (range) | 139 (29–365) |
Data were missing for race (n = 2), ethnicity (n=1), and parent perception of prognosis (n=2)
Categories are not mutually exclusive.
Nearly all parents considered receiving information about late effects of treatment to be extremely or very important (96%, 92/96, Table 2). However, 24% (23/96) did not recall receiving any information about their child’s risk of late effects. Only half (51%, 48/95) felt their child’s oncologist prepared them extremely or very well for potential late effects of cancer or its treatment. When asked to identify their treatment decision-making priorities, all parents considered offering the best chance of cure to be extremely or very important (100%, 96/96). Many valued minimizing acute effects of treatment (73%, 70/96) and most prioritized minimizing late effects (93%, 89/96).
TABLE 2.
Parent late effects communication experiences and preferences (N=96)
| Information Preferences | N (%) |
|---|---|
| Extremely/very important to know late effects information | 92/96 (96) |
| Extremely/very important consideration in treatment decision-makinga | |
| Best chance of cure | 96/96 (100) |
| Minimizing acute effects of treatment | 70/96 (73) |
| Minimizing late effects of treatment | 89/96 (93) |
| Communication Experiences | |
| Received information about late effects | 73/96 (76) |
| Extremely/very well prepared for late effects | 48/95 (51) |
| Parent Late Effect Perceived Likelihood & Worries | |
| Extremely/very likely for child to develop late effects | 19/94 (20) |
| Extremely/very worried about late effects | 58/96 (60) |
Data were missing for late effects preparation (n = 1) and likelihood of late effects (n=2)
Categories are not mutually exclusive.
Twenty percent of parents (19/94) believed that that their child was extremely or very likely to experience late effects of treatment. A majority of parents reported that they were extremely or very worried about late effects (60%, 58/96). Univariate analyses of factors associated with increased worry about late effects are shown in Table 3. Parents were more likely to worry about late effects if they felt their child was at high risk of experiencing late effects (odds ratio [OR]=4.7, 95% confidence interval [CI]=1.3–17.4, p=0.02). Parents with higher dispositional optimism scores were less likely to worry about late effects (OR=0.4, 95%CI=0.2–0.9, p=0.03). There was no statistically significant relationship between worry about late effects and understanding of prognosis, feeling prepared for late effects, receipt of late effects information, child diagnosis, race/ethnicity, or parent education.
TABLE 3.
Univariate logistic regression analysis of parent and child characteristics with being extremely/very worried about late effects (N=96)
| Participants (n)a | N (%) with heightened worry | ORb (95% CI) | P | |
|---|---|---|---|---|
| Overall | 96 | 58 (60) | ||
| Perceived Prognosis | ||||
| Less favorable | 12 | 8 (67) | 1.4 (0.4–5.1) | 0.6 |
| Favorable (>75% chance of cure) | 82 | 48 (59) | Ref | |
| Perceived Likelihood of Late Effects | ||||
| Extremely/very | 19 | 16 (84) | 4.7 (1.3–17.4) | 0.02 |
| Moderately/somewhat/unlikely | 75 | 40 (53) | Ref | |
| Received Late Effect Information | ||||
| Yes | 73 | 46 (63) | 1.6 (0.6–4) | 0.4 |
| No | 23 | 12 (52) | Ref | |
| Preparation for Late Effects | ||||
| Extremely/very | 48 | 28 (58) | 0.8 (0.3–1.8) | 0.6 |
| Somewhat/a little/not at all | 47 | 30 (64) | Ref | |
| Child Age at Diagnosis (years) | ||||
| <10 | 68 | 39 (57) | 0.6 (0.3–1.6) | 0.3 |
| ≥10 | 28 | 19 (68) | Ref | |
| Child Sex | ||||
| Female | 43 | 28 (65) | 1.4 (0.6–3.3) | 0.4 |
| Male | 53 | 30 (57) | Ref | |
| Cancer Diagnosis | Global p=0.2 | |||
| Solid tumor | 32 | 23 (72) | 2.3 (0.9–5.8) | 0.09 |
| Brain tumor | 11 | 7 (64) | 1.6 (0.4–6) | 0.5 |
| Hematologic malignancy | 53 | 28 (53) | Ref | |
| Race/Ethnicity | ||||
| Non-white or Hispanic | 21 | 13 (62) | 1.1 (0.4–3.1) | 0.8 |
| White | 73 | 43 (59) | Ref | |
| Parent Sex | ||||
| Female | 71 | 46 (65) | 2 (0.8–5) | 0.14 |
| Male | 25 | 12 (48) | Ref | |
| Parent Education | ||||
| ≤Some college | 23 | 14 (61) | 1 (0.4–2.7) | 0.96 |
| ≥College graduate | 73 | 44 (60) | Ref | |
| Optimism | ||||
| Optimistic | 49 | 24 (49) | 0.4 (0.2–0.9) | 0.03 |
| Less optimistic | 46 | 33 (72) | Ref |
Due to some missing values, not all samples total 96
Odds Ratios (OR) >1 represent a greater likelihood of heightened worry
Ninety-five percent Confidence Interval (95% CI)
Similar to their general late effect concerns, parents tended to be more worried about those specific late effects they thought their child was at risk of experiencing. There was a statistically significant relationship between perceived likelihood and worry for impaired growth (p=0.004), cardiac toxicity (p=0.016), infertility (p<0.0001), and neurocognitive impairment (p<0.0001), and trend towards a relationship for second malignancies (Table 4). There was also a significant association between recollection of being told a child was at risk for a specific late effect and parental worry for impaired growth (p=0.01), infertility (p=0.003), and neurocognitive impairment (p=0.009).
TABLE 4.
Association between parental worry and parental perception of likelihood, and parent recall of being told their child was at risk for individual late effects, N=96
| Parental Worry by Specific Late Effect | Parental perception of likelihood | Parent ever told child at risk | ||||
|---|---|---|---|---|---|---|
| Extremely/very likely | Not at all, a little or somewhat likely | p-value | Yes | No | p-value | |
| Growth Impairment | 0.004 | 0.01 | ||||
| Extremely/very worried | 6/7(86%) | 24/86(28%) | 14/25(56%) | 14/56(25%) | ||
| Not at all, a little, somewhat worried | 1/7(14%) | 62/86(72%) | 11/25(44%) | 42/56 (75%) | ||
| Cardiac Toxicity | 0.016 | 0.13 | ||||
| Extremely/very worried | 5/6(83%) | 26/85(31%) | 16/37(43%) | 8/33(24%) | ||
| Not at all, a little, somewhat worried | 1/6(17%) | 59/85(69%) | 21/37(57%) | 25/33(76%) | ||
| Infertility | <0.0001 | 0.003 | ||||
| Extremely/very worried | 17/19(89%) | 21/73(29%) | 29/51(57%) | 9/37(24%) | ||
| Not at all, a little, somewhat worried | 2/19(11%) | 52/73(71%) | 22/51(43%) | 28/37(76%) | ||
| Secondary Cancers | 0.06 | 0.13 | ||||
| Extremely/very worried | 5/5(100%) | 46/90(51%) | 29/48(60%) | 16/38(42%) | ||
| Not at all, a little, somewhat worried | 0/5(0%) | 44/90(49%) | 19/48(40%) | 22/38(58%) | ||
| Neurocognitive Impairment | <0.0001 | 0.009 | ||||
| Extremely/very worried | 10/10(100%) | 26/84(31%) | 17/28(61%) | 16/54(30%) | ||
| Not at all, a little, somewhat worried | 0/10(0%) | 58/84(69%) | 11/28(39%) | 38/54(70%) | ||
Due to some missing values, not all samples total 96
However, relatively few parents felt their child was likely to experience each of the five specific late effects evaluated. For example, 21% (19/93) of parents considered it extremely/very likely that their child would experience infertility as a result of treatment, and only 5% (5/95) of parents felt their child was extremely/very likely to experience a second malignancy. Even parents who did not consider late effects likely reported that they worried about these late effects, with 32–54% of parents identifying as extremely or very worried about each specific late effect (Figure 1). In addition, many parents (48–91%) felt that individual late effects would have an extremely or very negative impact on their child’s QOL if they were to occur.
Figure 1:
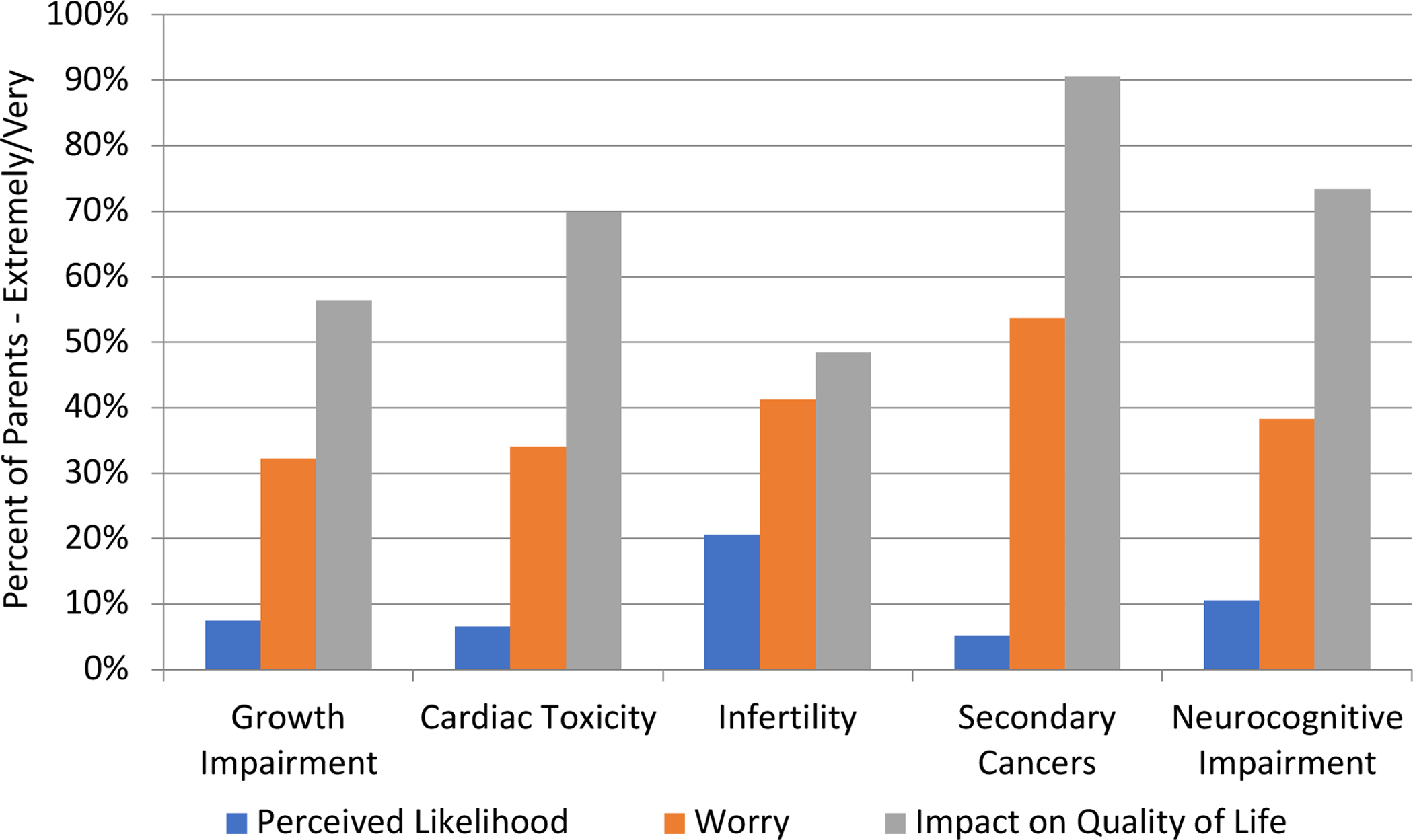
Parental Perceived Likelihood, Worry, & Impact on Quality of Life by Late Effect
Discussion
Although the rate of childhood cancer survival continues to improve, most survivors experience at least one late effect of treatment, often impacting QOL after cure.11,36 In this study, we found that even early in treatment, parents want information about late effects and consider this information influential to their treatment decision-making, though many feel underinformed. Parents in our study had considerable worries about late effects in general, as well as worries about specific late effects such as secondary malignancies and infertility. Though parents who felt their child to be at high risk of late effects were more likely to worry, there was also a substantial subset of parents who did not perceive late effects to be highly likely, but who worried about them nonetheless. While some degree of worry about late effects is expected, disproportionate or excessive worry may be detrimental to parental coping and well-being, which may negatively influence their children’s anxiety and QOL.
It is understandable that parents would worry about the potential long-term implications of their child’s treatment, particularly if their child has a high likelihood of developing late effects. While we did not assess individual children’s actual risks of late effects in this study, we found that parents who believed there was a higher likelihood of their child experiencing late effects were more worried. Yet, many parents were worried even when they perceived their child’s risk of late effect risk to be low. Despite the lack of focus on late effects information early on, the mere mention of the possibility of late effects may contribute to parental worry.13 Though the actual risks of some of the late effects we studied are quite low, such as the risk of chemotherapy-associated second malignancies, parents in our study felt that their children’s QOL would be significantly negatively impacted if they were to experience late effects. This is consistent with prior literature that shows that QOL in survivorship is decreased for those who experience more late effects.36 Therefore, parents may worry not only about the likelihood of late effects, but also the impact of late effects on their children’s wellbeing. Further, as their children have already experienced the very rare occurrence of a childhood malignancy, their perception of the likelihood of rare events may be understandably skewed. The degree of worry had no relation to the type of cancer, perception of prognosis, perceived effectiveness of preparation for late effects by the oncologist, or recall of information received, reflecting pervasive parental concern.
The discrepancy between perceived low likelihood of late effects and considerable worry is likely compounded by parents feeling simultaneously underinformed and overwhelmed. Most parents in our study wanted information about late effects and valued this information in their treatment decision-making. Concerningly, nearly one quarter of parents did not recall receiving any information about late effects, and half felt that communication about late effects had been inadequate. Though we did not find an association between receipt of information and worry, we may have been underpowered to detect such a difference, or parents may have felt they received information, but not in a way they could fully comprehend. As this study did not observe or record discussions between providers and parents, we do not know how late effects information was conveyed. Similarly, providers were not queried about their typical information provision practices or their perceptions of a child’s risks of specific late effects, as we relied on parent report to understand their communication experiences. Informed consent documents at our institution include tables of the anticipated acute and long-term effects of each chemotherapeutic agent, and many providers use these documents as the basis of their discussions. Yet, early discussions about diagnosis and treatment are often emotionally charged and include a large amount of information that must be communicated to families.3 Furthermore, the urgency of initiating treatment and the necessity of therapy makes it challenging to think about future health considerations such as the potential development of late effects. For these reasons, late effects are often not a primary focus of conversations and parents may be unable to process or fully integrate information about this topic.16 Though parent recollection may not reflect all that was discussed in a communication encounter, it does capture what parents took away from a conversation.
Our finding of near universal parental desire for information yet only half of parents feeling well prepared for potential late effects suggests a need for improvement in early communication about risks of late effects. This requires attention to both information needs and the emotional experience. While receipt of late effects information was not associated with decreased parental worry, importantly providing information did not increase parental worry. Education on late effects should begin early, as parents feel this information informs treatment decision-making, and as it may impact the ability to use mitigating measures such as fertility preservation prior to treatment initiation. As many parents could not recall having received any information about late effects, and given the overwhelming amount of information provided at diagnosis, most families would likely benefit from hearing this information again during treatment and at treatment completion.
Information alone is insufficient; attending to parental worry is equally important. Ongoing parental worry about late effects is associated with decreased peace of mind in parents of survivors of childhood cancer,9 suggesting that it may interfere with coping and well-being. Further, parental stress and distress may contribute to increased child distress and anxiety in pediatric oncology.37 Previous studies suggest that the emotional impact of cancer therapy is an unmet need for many patients and parents, therefore proactively addressing this concern may be beneficial.4 Cancer survivors with greater cancer-related worries may be the most likely to benefit from interventions to improve QOL in survivorship.38 Effective interventions in adult oncology, such as ConquerFear, that pair education with concrete strategies focused on controlling and modifying worry could be adapted and tested with families in pediatric oncology.39 It was also notable that optimism had a protective effect in our study - parents with higher dispositional optimism scores were less likely to worry, much as prior studies have shown a protective effect of dispositional optimism for cancer-related worries among adult cancer survivors.21 While optimism may be difficult to intervene upon, it is related to resilience, which may help counteract distress.40 Formalized resilience interventions that impart skills in stress management and reframing have been used with success with both parents and patients in pediatric oncology.41,42 Future researchers could continue to expand and explore the impact of these types of interventions on late effect worries during and after childhood cancer treatment.
This study has several limitations. It was conducted at a single large academic site with limited racial, ethnic, and educational diversity among enrolled study participants. The generalizability of our findings could be confirmed with future multi-site studies with more diverse participants. Similarly, the communication and information needs of non-English speakers and those with limited health literacy warrant further exploration as these groups may be more vulnerable to communication gaps or may have unique needs and preferences. We surveyed parents, as the primary decision-makers for their children, in the first year of their child’s treatment. As some time had elapsed between early treatment conversations and survey administration, and as we did not record or observe the conversations themselves, it is possible that these topics were discussed in depth but were not recalled by parents. However, our findings of pervasive worry and the level of import parents place on these topics demonstrate the salience of late effect concerns. Additionally, if the information we provide is not memorable, this suggests that we need to find new ways to convey it. We did not explore the accuracy of parent perceptions of their child’s risks of late effects in this analysis. Future studies may help us better understand the role of specific late effect worries in real-time treatment decision-making, and qualitative investigations may be utilized to better understand how these concerns evolve at completion of treatment and in survivorship. Our moderate sample size may have limited the power to detect differences between subgroups. Finally, the perspective, knowledge, and preferences of the patients themselves were not elicited in this study and bear further exploration.
As the number of pediatric cancer survivors continues to increase, the impact of late effects of childhood cancer on the health and well-being of survivors is ever more important. This study improves our understanding of parental worries about late effects of childhood cancer, and highlights the interplay between worry, perceived risk, and treatment decision-making. Parents disproportionately worry about late effects and see them as impactful to their child’s future QOL. As such, parental education about late effects at the time of diagnosis and throughout treatment, combined with interventions that focus on the emotional significance of late effects, may be jointly harnessed to improve parental awareness of risk while mitigating worry.
Supplementary Material
Funding:
This work was supported by Agency for Healthcare Research and Quality K12 HS022986 (KAG); and National Cancer Institute K08 CA245036 (KAG)
Abbreviations:
- QOL
quality of life
Footnotes
Conflicts of Interest: The authors have no relevant financial or non-financial interests to disclose.
Data Availability:
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
- 1.Kessel RM, Roth M, Moody K, Levy A. Day One Talk: parent preferences when learning that their child has cancer. Support Care Cancer. November 2013;21(11):2977–82. doi: 10.1007/s00520-013-1874-8 [DOI] [PubMed] [Google Scholar]
- 2.Mack JW, Grier HE. The Day One Talk. J Clin Oncol. February 1 2004;22(3):563–6. doi: 10.1200/JCO.2004.04.078 [DOI] [PubMed] [Google Scholar]
- 3.Levi RB, Marsick R, Drotar D, Kodish ED. Diagnosis, disclosure, and informed consent: learning from parents of children with cancer. J Pediatr Hematol Oncol. Jan-Feb 2000;22(1):3–12. [DOI] [PubMed] [Google Scholar]
- 4.Levine DR, Liederbach E, Johnson LM, et al. Are we meeting the informational needs of cancer patients and families? Perception of physician communication in pediatric oncology. Cancer. May 1 2019;125(9):1518–1526. doi: 10.1002/cncr.31937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Santacroce S, Uncertainty, anxiety, and symptoms of posttraumatic stress in parents of children recently diagnosed with cancer. J Pediatr Oncol Nurs. May-Jun 2002;19(3):104–11. doi: 10.1177/104345420201900305 [DOI] [PubMed] [Google Scholar]
- 6.Katz LF, Fladeboe K, King K, et al. Trajectories of child and caregiver psychological adjustment in families of children with cancer. Health Psychol. August 2018;37(8):725–735. doi: 10.1037/hea0000619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ljungman L, Cernvall M, Gronqvist H, Ljotsson B, Ljungman G, von Essen L. Long-term positive and negative psychological late effects for parents of childhood cancer survivors: a systematic review. PLoS One. 2014;9(7):e103340. doi: 10.1371/journal.pone.0103340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leventhal-Belfer L, Bakker AM, Russo CL. Parents of Childhood Cancer Survivors. Journal of Psychosocial Oncology. 1993/November/17 1993;11(2):19–41. doi: 10.1300/J077V11N02_02 [DOI] [Google Scholar]
- 9.Sisk BA, Weng S, Mack JW. Persistently low peace of mind in parents of cancer patients: A five-year follow-up study. Pediatr Blood Cancer. May 2019;66(5):e27609. doi: 10.1002/pbc.27609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siegel DA, Richardson LC, Henley SJ, et al. Pediatric cancer mortality and survival in the United States, 2001–2016. Cancer. July 29 2020;doi: 10.1002/cncr.33080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phillips SM, Padgett LS, Leisenring WM, et al. Survivors of childhood cancer in the United States: prevalence and burden of morbidity. Cancer Epidemiol Biomarkers Prev. April 2015;24(4):653–63. doi: 10.1158/1055-9965.EPI-14-1418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greenzang KA, Cronin AM, Kang TI, Mack JW. Parental distress and desire for information regarding long-term implications of pediatric cancer treatment. Cancer. December 1 2018;124(23):4529–4537. doi: 10.1002/cncr.31772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greenzang KA, Dauti A, Mack JW. Parent perspectives on information about late effects of childhood cancer treatment and their role in initial treatment decision making. Pediatr Blood Cancer. June 2018;65(6):e26978. doi: 10.1002/pbc.26978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sisk BA, Greenzang KA, Kang TI, Mack JW. Longitudinal parental preferences for late effects communication during cancer treatment. Pediatr Blood Cancer. January 2018;65(1)doi: 10.1002/pbc.26760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramirez LY, Huestis SE, Yap TY, Zyzanski S, Drotar D, Kodish E. Potential chemotherapy side effects: what do oncologists tell parents? Pediatr Blood Cancer. April 2009;52(4):497–502. doi: 10.1002/pbc.21835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greenzang KA, Cronin AM, Mack JW. Parental preparedness for late effects and long-term quality of life in survivors of childhood cancer. Cancer. August 15 2016;122(16):2587–94. doi: 10.1002/cncr.30092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Michel G, Brinkman TM, Wakefield CE, Grootenhuis M. Psychological Outcomes, Health-Related Quality of Life, and Neurocognitive Functioning in Survivors of Childhood Cancer and Their Parents. Pediatr Clin North Am. December 2020;67(6):1103–1134. doi: 10.1016/j.pcl.2020.07.005 [DOI] [PubMed] [Google Scholar]
- 18.Wang R, Syed IA, Nathan PC, Barr RD, Rosenberg-Yunger ZR, Klassen AF. Exploring Cancer Worry in Adolescent and Young Adult Survivors of Childhood Cancers. J Adolesc Young Adult Oncol. December 2015;4(4):192–9. doi: 10.1089/jayao.2015.0029 [DOI] [PubMed] [Google Scholar]
- 19.Yang Y, Li W, Wen Y, et al. Fear of cancer recurrence in adolescent and young adult cancer survivors: A systematic review of the literature. Psychooncology. April 2019;28(4):675–686. doi: 10.1002/pon.5013 [DOI] [PubMed] [Google Scholar]
- 20.Bult MK, van Bindsbergen KLA, Schepers SA, et al. Health-Related Quality of Life of Adolescents with Cancer During the First Year of Treatment. J Adolesc Young Adult Oncol. October 2019;8(5):616–622. doi: 10.1089/jayao.2019.0017 [DOI] [PubMed] [Google Scholar]
- 21.Deimling GT, Bowman KF, Sterns S, Wagner LJ, Kahana B. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology. April 2006;15(4):306–20. doi: 10.1002/pon.955 [DOI] [PubMed] [Google Scholar]
- 22.Greenzang KA, Al-Sayegh H, Ma C, Najafzadeh M, Wittenberg E, Mack JW. Parental Considerations Regarding Cure and Late Effects for Children With Cancer. Pediatrics. May 2020;145(5)doi: 10.1542/peds.2019-3552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mack JW, Wolfe J, Grier HE, Cleary PD, Weeks JC. Communication about prognosis between parents and physicians of children with cancer: parent preferences and the impact of prognostic information. J Clin Oncol. November 20 2006;24(33):5265–70. [DOI] [PubMed] [Google Scholar]
- 24.Mack JW, Cronin AM, Kang TI. Decisional Regret Among Parents of Children With Cancer. J Clin Oncol. September 12 2016;34(33):4023–4029. doi: 10.1200/JCO.2016.69.1634 [DOI] [PubMed] [Google Scholar]
- 25.Mack JW, Cook EF, Wolfe J, Grier HE, Cleary PD, Weeks JC. Understanding of prognosis among parents of children with cancer: parental optimism and the parent-physician interaction. J Clin Oncol. April 10 2007;25(11):1357–62. [DOI] [PubMed] [Google Scholar]
- 26.Mack JW, Wolfe J, Cook EF, Grier HE, Cleary PD, Weeks JC. Hope and prognostic disclosure. J Clin Oncol. December 10 2007;25(35):5636–42. doi: 10.1200/JCO.2007.12.6110 [DOI] [PubMed] [Google Scholar]
- 27.Fowler FJ. Survey research methods. Fifth edition. ed. Applied social research methods series. SAGE; 2014:xi, 171 pages. [Google Scholar]
- 28.Lindell RB, Koh SJ, Alvarez JM, et al. Knowledge of diagnosis, treatment history, and risk of late effects among childhood cancer survivors and parents: The impact of a survivorship clinic. Pediatr Blood Cancer. August 2015;62(8):1444–51. doi: 10.1002/pbc.25509 [DOI] [PubMed] [Google Scholar]
- 29.Greenzang KA, Fasciano KM, Block SD, Mack JW. Early information needs of adolescents and young adults about late effects of cancer treatment. Cancer. July 15 2020;126(14):3281–3288. doi: 10.1002/cncr.32932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oeffinger KC, Mertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. October 12 2006;355(15):1572–82. doi: 10.1056/NEJMsa060185 [DOI] [PubMed] [Google Scholar]
- 31.Oeffinger KC, Nathan PC, Kremer LC. Challenges after curative treatment for childhood cancer and long-term follow up of survivors. Hematol Oncol Clin North Am. February 2010;24(1):129–49. doi: 10.1016/j.hoc.2009.11.013 [DOI] [PubMed] [Google Scholar]
- 32.Diller L, Chow EJ, Gurney JG, et al. Chronic disease in the Childhood Cancer Survivor Study cohort: a review of published findings. J Clin Oncol. May 10 2009;27(14):2339–55. doi: 10.1200/JCO.2008.21.1953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Langeveld NE, Grootenhuis MA, Voute PA, de Haan RJ, van den Bos C. Quality of life, self-esteem and worries in young adult survivors of childhood cancer. Psychooncology. December 2004;13(12):867–81. doi: 10.1002/pon.800 [DOI] [PubMed] [Google Scholar]
- 34.Lehmann V, Gronqvist H, Engvall G, et al. Negative and positive consequences of adolescent cancer 10 years after diagnosis: an interview-based longitudinal study in Sweden. Psychooncology. November 2014;23(11):1229–35. doi: 10.1002/pon.3549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. December 1994;67(6):1063–78. [DOI] [PubMed] [Google Scholar]
- 36.Yeh JM, Hanmer J, Ward ZJ, et al. Chronic Conditions and Utility-Based Health-Related Quality of Life in Adult Childhood Cancer Survivors. J Natl Cancer Inst. September 2016;108(9)doi: 10.1093/jnci/djw046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bakula DM, Sharkey CM, Perez MN, et al. Featured Article: The Relationship Between Parent and Child Distress in Pediatric Cancer: A Meta-Analysis. J Pediatr Psychol. November 1 2019;44(10):1121–1136. doi: 10.1093/jpepsy/jsz051 [DOI] [PubMed] [Google Scholar]
- 38.Parker PA, Banerjee SC, Matasar MJ, et al. Cancer worry and empathy moderate the effect of a survivorship-focused intervention on quality of life. Psychooncology. June 2020;29(6):1012–1018. doi: 10.1002/pon.5371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Butow PN, Turner J, Gilchrist J, et al. Randomized Trial of ConquerFear: A Novel, Theoretically Based Psychosocial Intervention for Fear of Cancer Recurrence. J Clin Oncol. December 20 2017;35(36):4066–4077. doi: 10.1200/JCO.2017.73.1257 [DOI] [PubMed] [Google Scholar]
- 40.Rosenberg AR, Bradford MC, Bona K, et al. Hope, distress, and later quality of life among adolescent and young adults with cancer. J Psychosoc Oncol. Mar-Apr 2018;36(2):137–144. doi: 10.1080/07347332.2017.1382646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rosenberg AR, Bradford MC, Junkins CC, et al. Effect of the Promoting Resilience in Stress Management Intervention for Parents of Children With Cancer (PRISM-P): A Randomized Clinical Trial. JAMA Netw Open. September 4 2019;2(9):e1911578. doi: 10.1001/jamanetworkopen.2019.11578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rosenberg AR, Bradford MC, McCauley E, et al. Promoting resilience in adolescents and young adults with cancer: Results from the PRISM randomized controlled trial. Cancer. October 1 2018;124(19):3909–3917. doi: 10.1002/cncr.31666 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


