Abstract
Diabetes self-management education and support enhance self-efficacy and promote self-management behaviors essential for diabetes management. We investigated the mediating effect of self-efficacy on the association between diabetes education or care coordination and self-care activities.
We surveyed a population-based sample of adults with type 2 diabetes (19 – 64 years of age) covered by Alabama Medicaid. We examined whether receipt of diabetes education or care coordination were associated with improvements in diabetes self-care activities. We then examined if improvements were mediated by self-efficacy. Models were adjusted for age, gender, race, education, insulin use, diabetes duration and depressive symptoms.
Results.
A total of 1,318 participants were included in the study (Mean Age: 52.9, SD 9.6 72.5% Female, 56.4% Black, 3.1% Hispanic). Diabetes education was associated with increases in self-care activity scores related to general diet, physical activity, glucose self-monitoring and foot care; care coordination was associated with glucose self-monitoring. In addition, mediation analysis models confirmed that improvements in self-efficacy led to improved self-care activities scores, mediating the association of diabetes education and self-care activities.
Conclusions.
Diabetes education and self-efficacy were associated with better self-care. Receiving diabetes education led to a higher likelihood of engaging in self-care activities, driven in part by increases in self-efficacy. Future interventions that aim to improve diabetes self-management behaviors can benefit from targeting self-efficacy constructs and from the integration of diabetes education in the care coordination structure.
Keywords: Diabetes education, self-efficacy, self-care management, mediation analysis
Introduction
Type 2 diabetes is a chronic condition that affects more than 31 million Americans (Control & Prevention, 2020). The demands that diabetes imposes on individuals are complex and costly. The American Diabetes Association (ADA) recommends that self-management education and support (DSMES) be given at four critical times: at diagnosis; annually or when not meeting treatment targets; when complications develop, and when transitions in life and care occur (American Diabetes Association, 2020; Powers et al., 2020). DSMES is intended to address clinical, educational and behavioral aspects of diabetes daily self-care by giving individuals with diabetes the knowledge, skills and confidence needed to self-manage their care. Self-care is critical in preventing acute complications and encompasses most of a person’s diabetes care.
Certified diabetes educators and care coordinators can enhance diabetes self-management by teaching individuals how to initiate and maintain self-care activities and how to function in the health care environment effectively. In acquiring this knowledge and skills, an individual becomes health literate. In diabetes, health literacy is closely related to diabetes education, self-efficacy skills and self-management activities. The association between low health literacy with poorer health outcomes and lower use of health care services has been established for a number of conditions (Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011). However, there is limited evidence of the association between health literacy and processes or outcomes related to diabetes care (Al Sayah, Majumdar, Williams, Robertson, & Johnson, 2013). On the other hand, self-efficacy is a well-studied construct that influences diabetes self-management (Sarkar, Fisher, & Schillinger, 2006). Patients with diabetes are expected to perform daily self-care activities and self-efficacy is a potential mechanism that can increase consistency in performing these activities. Defined as one’s perceived capability to carry out a target behavior (Bandura, 1977), self-efficacy is theorized to enhance task motivation and intention to complete targeted behaviors (Bandura, Reese, & Adams, 1982; Maddux, Sherer, & Rogers, 1982).
A growing body of research has confirmed the role of self-efficacy in predicting behavior in patients with diabetes as well as the need for diabetes education to include more practical and interactive exercises to develop specific skills (Cox, Carpenter, Bruce, Poole, & Gaylord, 2004; Krichbaum, Aarestad, & Buethe, 2003; Sarkar et al., 2006; Wallston, Rothman, & Cherrington, 2007). Lower self-efficacy and its reflection on poorer self-management of chronic conditions such as diabetes has also been linked to minority and disadvantaged populations (Hankonen, Absetz, Haukkala, & Uutela, 2009). In Hispanic populations, studies found a positive association between self-efficacy and self-management behaviors (Lorig, Ritter, & Jacquez, 2005; Peña-Purcell, Boggess, & Jimenez, 2011; Rosal et al., 2011; Valen, Narayan, & Wedeking, 2012). However, tests of the association between higher self-efficacy and better self-management in racially mixed populations have been inconclusive (Hawthorne, Robles, Cannings-John, & Edwards, 2008). Little is known about the mediating effect of self-efficacy in the association between diabetes education and self-care behaviors in low-income, racially diverse populations where diabetes and low health literacy are prevalent.
In order for healthcare professionals to be able to develop and implement theory-based needed interventions in these vulnerable populations, it is necessary to confirm the mediating role of self-efficacy. Self-efficacy focused education has been more effective than traditional diabetes education programs in improving diabetes health outcomes, regulating self-management behaviors and increasing patients’ overall quality of life (Jiang, Wang, Lu, Jiang, & Li, 2019). In particular, interventions based on cognitive reframing techniques to motivate individuals as well as those involving peer educators produced better results in minority populations (Ricci-Cabello et al., 2014).
In this study we sought to estimate the prevalence of diabetes education and care coordination in a diverse low-income population of diabetes patients enrolled in Medicaid; to determine whether diabetes education or care coordination had a positive association with self-care behaviors, and to assess whether this association was mediated by self-efficacy. We hypothesized that the prevalence of diabetes education and care coordination would be low and that participants who reported having had diabetes education or care coordination would show higher self-efficacy and higher self-care management scores.
Methods
Study design and population
We conducted a cross-sectional, population-based survey within the Alabama Care Plan study. This study enrolled adults with type 2 diabetes between the ages of 19 and 64 years, who were covered by Alabama Medicaid for the prior 12 months. In Alabama, the Medicaid program covers one in eight adults (Brooks, Roygardner, & Artiga, 2019). Medicaid eligibility for adults in Alabama includes parents of minor children with incomes at or below 18% of Federal Poverty Level (FPL) and adults with disability eligible for the Supplemental Security Income (SSI) program. Diabetes was ascertained if participants had at least one inpatient or two outpatient diabetes codes according to the International Classification of Diseases (ICD-9 or ICD-10) in the preceding two years. Participants were excluded if they were non-English speaking, were mentally or physically incapable of completing the survey per caregiver report, or had type 1 diabetes. Approval for this study was obtained from the institutional review board of the University of Alabama at Birmingham (UAB).
Data collection
From Alabama Medicaid enrollment and claims data files, we generated a list of potential participants who met the age, Medicaid enrollment, and diabetes diagnosis inclusion criteria. The UAB Recruitment and Retention Shared Facility (RRSF) contacted potential participants by letter. This letter provided information about the study and an option to decline participation by contacting a toll-free number or by mail. Subsequently, RRSF interviewers contacted potential participants who did not decline by phone to invite them to participate and schedule a time to complete the survey. Using a protocol similar to that used by the Centers for Disease Control Behavioral Risk Factor Surveillance System, RRSF interviewers called participants multiple times at different times and days, including evenings and weekends, with a maximum of 15 call attempts. For eligible participants who agreed to participate, informed consent was obtained by phone. RRSF interviewers used a computer-assisted telephone interview system to complete a 125-item survey which included measures detailed below.
Measures
Outcome of interest
Self-care diabetes activities were assessed by the Summary of Diabetes Self-Care Activities (SDSCA) (Toobert, Hampson, & Glasgow, 2000). We used the following domains of self-management activities from the SDSCA: General Diet; Specific Diet; Physical Activity; Self-Monitoring of Blood Glucose; and Foot Care. Participants were asked how often they completed the activity in the past seven days (0–7 days). Scores for each activity were based on the average of two related questions for each domain. If one item was missing the score was the answer to the non-missing item, if both items were missing the score was set to missing.
Predictors of interest
Diabetes education: participants responded to the question Have you ever taken a course or class in how to manage your diabetes yourself?
Care coordination: participants responded to Has a care coordinator, healthcare outreach worker, or other health care professional from your health plan or Medicaid contacted you to talk about your health, diabetes care, or other related issue?
In addition, participants responded to care coordination questions such as How did the care coordinator first contact you? How many times were you contacted by this person? and About how long ago was your last contact with the care coordinator, healthcare outreach worker or other health care professional? Answers to these questions were summarized only because they did not modify the dichotomous outcome variable.
Mediator
Diabetes self-efficacy was measured using the 8-item Perceived Diabetes Self-Management Scale (PDSMS) (Wallston et al., 2007). The responses for the PDSMS items ranged from 1 = “Strongly Disagree” to 5 = “Strongly Agree.” Four of the items (#s 1, 2, 6, & 7) that were worded such that high agreement signifies low self- efficacy or perceived competence were reverse-scored prior to being added to the other four items so that higher scores indicated more confidence in diabetes self-management. If only one item was missing, the score was the sum of the non-missing seven items. The total PDSMS score ranged from 8 to 40.
Covariates
Participants reported age, sex, race, ethnicity, education level, marital status, and disease severity (self-reported duration of diabetes and insulin use). Participants’ geographic status – rural or urban – was determined using a crosswalk of ZIP code and census tract data; participant ZIP codes were categorized as rural if more than 50% of residents live in a designated non-metropolitan area based on census tract (Ratcliffe, Burd, Holder, & Fields, 2016). We collected information on annual household income. The majority of participants (70%) reported income below $15K, while 22% refused or did not know the answer. We did not collect data on household size.
We included the 8-item Patient Health Questionnaire (PHQ-8) (Kroenke et al., 2009) as a covariate because depression has been associated with negative assessments of individual capabilities and self-efficacy in patients with diabetes (Schoenthaler, Ogedegbe, & Allegrante, 2009), as well as with treatment non-adherence (Gonzalez et al., 2008). The PHQ-8 assesses frequency of depressive symptoms, including somatic and cognitive-affective symptoms, experienced during the preceding two weeks with responses ranging from “not at all” (0) to “nearly every day” (3). A higher score indicates greater depressive symptoms. If only one item was missing, the score was the sum of the non-missing seven items. If two or more items were missing, PHQ-8 was set to missing.
Statistical Analysis
Descriptive statistics were computed to summarize demographic and diabetes-related characteristics in the sample. Bivariate associations between demographic and clinical characteristics (e.g., age, sex, race, ethnicity, education level, marital status, self-reported duration of diabetes, insulin use and depression) and diabetes education, care coordination, self-efficacy, and diabetes care behaviors were assessed using Mantel-Haenszel Chi-squared tests for categorical variables. For continuous variables, independent t-tests tests were conducted. We evaluated bivariate associations between diabetes education, care coordination, self-efficacy and self-management behaviors using Pearson’s correlation coefficients.
To assess whether self-efficacy mediated the association between diabetes education or care coordination and self-care activities scores, we conducted mediation models using the SAS macro PROCESS (Hayes, 2017) to assess the direct effect of diabetes education or care coordination as antecedent variables on self-care activities score (c) and the indirect effect of the influence of each antecedent variable on self-efficacy (a), and the influence of self-efficacy on self-activities scores (b) (Mackinnon & Dwyer, 1993; Mackinnon, Warsi, & Dwyer, 1995; Preacher & Hayes, 2004). Figure 1. The PROCESS macro computes 95% bias-corrected bootstrapped asymmetrical confidence intervals for the indirect effect. The bootstrap procedure is based on 10,000 samples that generate the sampling distribution of the indirect effect. Significant mediation was established if the intervals did not contain zero. The proportion of the effect from either diabetes education or care coordination that was attributed to self-efficacy was computed by dividing the indirect effect (pathway ab) by the total effect (pathway c + pathway ab). Single mediator models were computed for each self-care activity, adjusting for age, sex, race, ethnicity, education level, marital status, self-reported duration of diabetes, insulin use and depression. Interaction terms with race and age were tested.
Figure 1.
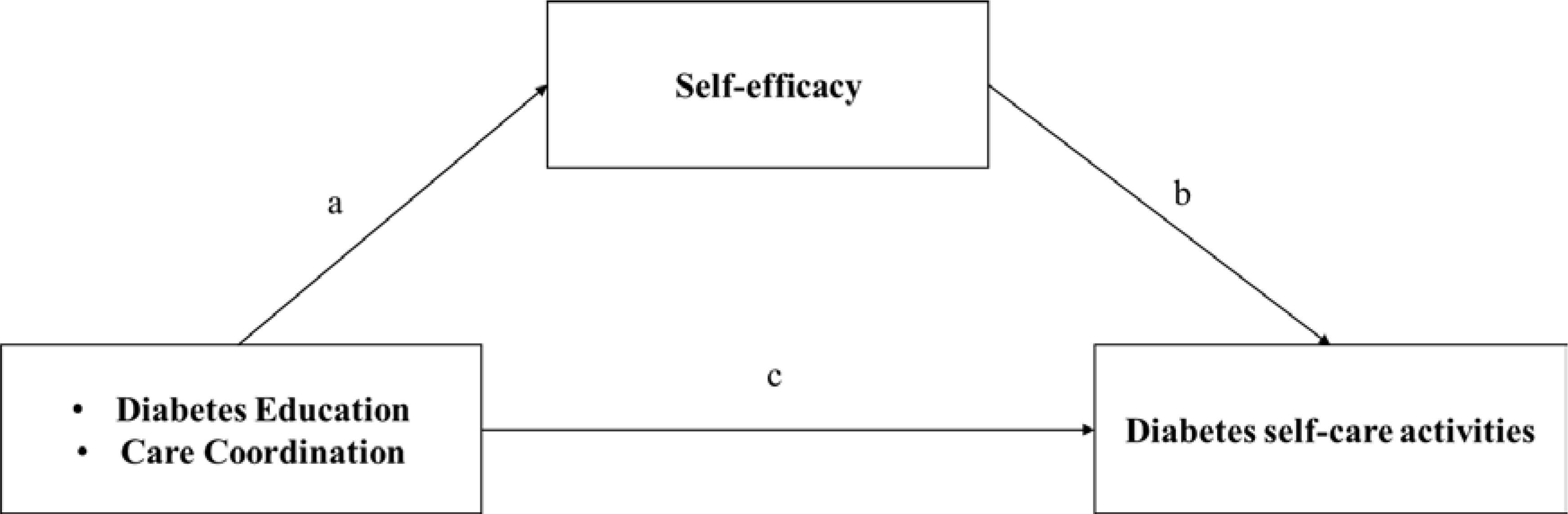
Conceptual model
Missing data
From 1344 participants who were eligible for the study, 26 were excluded because they had missing answers to diabetes education or care coordination. Of the remaining 1318, 172 (13.1%) had missing data. There were no significant differences between participants with complete and incomplete data. Since the proportion of participants with missing data was above 10%, multiple imputation was performed. We used chained equations methods in SAS to impute missing data. Results from analysis using complete and incomplete data did not yield significant differences (data not shown). All analyses were performed in SAS version 9.4
Results
The study population included 1,318 individuals. Figure 2 presents a STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) diagram of the study sample. Characteristics of the original study population including the number of missing cases for each variable are presented in Table 1. The sample was predominantly female (73%), racially diverse (56% Blacks and 3% Hispanics), of low socioeconomic status (36% had less than high school education, 70% reported annual household income below $15K) and 39% lived in rural areas. The mean age of the participants was 52.9 years old, they had been diagnosed with diabetes an average of 12.1 years and 41% were on insulin. Diabetes education and care coordination rates were 40 and 23%, respectively. Care coordination contacts were mostly done via phone (72%); more than half (57%) had at least three contacts with a care coordinator, and about half (53%) of those having at least one contact, had this contact within one month on the survey. In the majority of cases (71%), the care coordinator discussed obstacles or worrisome matters regarding their diabetes care and gave reminders to keep a healthy diet, being physically active, keeping up with their diabetes medications and explained how to use of a glucometer.
Figure 2.
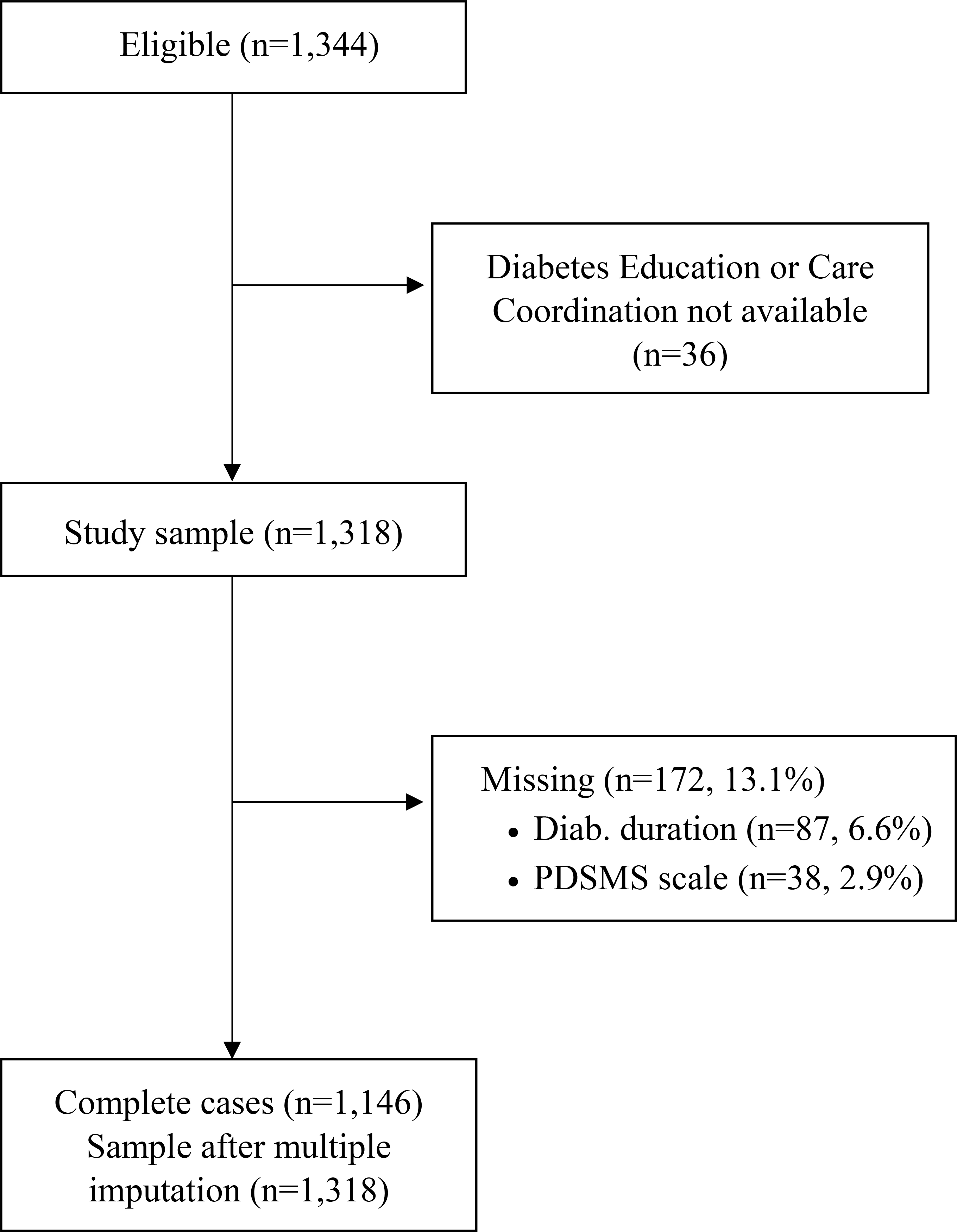
STROBE diagram of study population
Table 1.
Characteristics of the sample (n=1,318)
| Characteristic | % or mean (SD) | No. of missing |
|---|---|---|
|
| ||
| Demographic | ||
| Age (range 19–64) | 52.9 (9.6) | 0 |
| Female | 72.5 | 0 |
| Black | 56.4 | 11 |
| Hispanic | 3.1 | 8 |
| Education: Less than High School | 36.2 | 6 |
| Married | 20.3 | 15 |
| Rural residence | 39.2 | 0 |
| Severity of disease | ||
| Diabetes duration (range 0–59 years) | 12.1 (11.2) | 87 |
| Insulin Use | 41.1 | 2 |
| Diabetes education | 40.0 | 0 |
| Care coordination | 22.8 | 0 |
| Scales | ||
| PHQ (range 0–24) | 7.4 (5.9) | 20 |
| PDSMS (range 10–40) | 27.3 (4.8) | 38 |
| SDSCA Diet (range 0–7 days) | 4.0 (2.4) | 18 |
| SDSCA Special Diet (range 0–7 days) | 4.3 (1.8) | 11 |
| SDSCA Physical Activity (range 0–7 days) | 2.8 (2.6) | 4 |
| SDSCA Glucose Testing (range 0–7 days) | 4.5 (2.9) | 12 |
| SDSCA Foot Care (range 0–7 days) | 4.6 (2.6) | 8 |
PHQ - Patient Health Questionnaire
PDSMS - Perceived Diabetes Self-Management Scale
SDSCA - Self-care diabetes activities were assessed by the Summary of Diabetes Self-Care Activities
The average score for the depression scale of the Patient Health Questionnaire (PHQ-8) was 7.4, indicating mild depressive symptoms. The average self-efficacy score was 27.3 and the self-care activities ranged between 2.8 and 4.6 days. The correlation coefficients between self-efficacy and each of the self-care behaviors were significant, except for glucose self-monitoring (Table 2).
Table 2.
Unadjusted bivariate correlations between Self-Efficacy (PDSMS) and Self-Care Behaviors
| Self-efficacy | General Diet | Special diet | Physical Activity | Glucose Monitoring | Foot Care | |
|---|---|---|---|---|---|---|
|
| ||||||
| Self-efficacy | 1.00 | |||||
| General Diet | 0.25 (<.0001) | 1.00 | ||||
| Special diet | 0.22 (<.0001) | 0.42 (<.0001) | 1.00 | |||
| Physical Activity | 0.20 (<.0001) | 0.16 (<.0001) | 0.11 (<.0001) | 1.00 | ||
| Glucose Monitoring | 0.05 (0.0880) | 0.16 (<.0001) | 0.11 (<.0001) | 0.06 (0.0419) | 1.00 | |
| Foot Care | 0.13 (<.0001) | 0.18 (<.0001) | 0.18 (<.0001) | 0.17 (<.0001) | 0.14 (<.0001) | 1.00 |
Table 3 presents the results from the multivariate linear regressions used to test the association of diabetes education and care coordination with self-care activities as well as the potential mediating effect of self-efficacy on self-care activities.
Table 3.
Results from mediation analysis: effects and 95% Confidence Intervals
| Self-Care Activity | ||||||||
|---|---|---|---|---|---|---|---|---|
| Diet | Physical Activity | Glucose Testing | Foot care | |||||
|
| ||||||||
| Total effect of diabetes education | 0.58 (0.30–0.85) | * | 0.30 (0.00–0.59) | * | 0.42 (0.11–0.11) | * | 0.57 (0.28–0.86) | * |
| Direct effect of diabetes education | 0.49 (0.22–0.76) | * | 0.22 (−0.08–0.51) | 0.37 (0.06–0.06) | * | 0.51 (0.23–0.80) | * | |
| Effect of diabetes education mediated by self-efficacy | 0.09 (0.04–0.16) | * | 0.08 (0.03–0.14) | * | 0.05 (0.02–0.02) | * | 0.06 (0.02–0.12) | * |
| Proportion explained by self-efficacy (%) | 15.5 | 11.9 | 10.5 | |||||
| Total effect of Care Coordination | 0.52 (0.17–0.87) | * | ||||||
| Direct effect of Care Coordination | 0.51 (0.16–0.86) | * | ||||||
| Effect of Care Coordination mediated by self-efficacy | 0.01 (−0.02–0.05) | |||||||
| Proportion explained by self-efficacy (%) | Not Significant | |||||||
Statistically significant at 0.05 level
Diabetes Education
Diabetes education was a significant predictor of self-efficacy and of four of the five self-care activities: general diet, physical activity, glucose self-monitoring and foot care. In addition, self-efficacy mediated the effect of diabetes education on these four self-care activities. The models for special diet did not yield any significant associations with diabetes education.
The total effect of diabetes education was highest for general diet, 0.58 (0.30–0.85). That is, for those who reported diabetes education and who scored a unit more in the self-efficacy scale, their general diet score would be 0.58 days higher on average. The indirect effect, 0.09 (0.04–0.16) indicates that the amount of the total effect mediated through self-efficacy on general diet was 15.5%. Total effects for foot care and glucose self-monitoring were 0.57 (0.28–0.86) and 0.42 (0.11–0.11) and their corresponding indirect effects were 0.05 (0.02–0.02) and 0.06 (0.02–0.12) respectively. The total effect for physical activity was 0.30 and the effect of education was fully mediated by self-efficacy. That is, for physical activity, education has a significant positive effect on physical activity score through its effect on self-efficacy.
Care Coordination
Care coordination was not a significant predictor of self-efficacy, general diet, special diet, physical activity or foot care. However, the direct effect of care coordination on glucose self-monitoring (0.51) was higher than the total effect of diabetes education on the same activity.
Discussion
Consistent with our hypotheses, we found that in this low-income, diverse population, the prevalence of diabetes education and care coordination support was below national standards, 40% and 23%, respectively. The association between diabetes education and self-management behaviors was positive and significant for general diet, physical activity, glucose self-monitoring and foot care, and self-efficacy mediated these associations. In addition, for physical activity, self-efficacy fully mediated the association between diabetes education and activity score. The effect of care coordination was limited to glucose self-monitoring. Self-efficacy was not found to be a significant mediating factor in the relationship between care coordination and self-management behaviors.
A major contribution of this study is that it highlights the urgent need to increase DSMES in disadvantaged populations where individuals need to overcome multiple personal and societal barriers to initiate and maintain self-care behaviors. The gap between the diabetes education prevalence in our sample compared to the national average is sizable. The estimated national average of people with diabetes who ever had diabetes education based on data from the 2017 Behavioral Risk Factor Surveillance System (BRFSS) was 51.7%. The current goal of Healthy People 2030 is to increase this percentage to 55.2% (Healthy People 2030, 2020 ). The estimates from our sample fall short and justify the need for intervention to increase DSMES to reach the Healthy People 2030 national goal.
Our results not only confirm the well-studied association between self-efficacy and self-care behaviors, they show that self-efficacy mediates the effect of diabetes education of self-care management in a disadvantaged population. From a cognitive-behavioral standpoint, this finding suggests that self-efficacy can be modified to promote self-management behaviors. In practice, healthcare providers can target self-efficacy to help people with diabetes to perform self-management activities. This study shows that ever having diabetes education increases an individual’s perceived self-efficacy and the frequency of their self-care activities. This is in agreement with social cognitive theory which proposes that in order to change behavior, an individual needs to increase their capabilities, self-confidence, determination and self-efficacy (Bandura, 1998). Importantly, this study shows that it is the combined effect of diabetes education and self-efficacy that has the potential to increase self-care activity scores.
The models used in this analysis show different contributions of self-efficacy on the total effect of diabetes education for each type of activity. Notably, the effect of diabetes education on physical activity was fully mediated by self-efficacy; the effect of self-efficacy was higher for general diet activities than for glucose self-monitoring and foot-care. Health professionals developing intervention programs in this population should ensure that participants demonstrate self-efficacy related to physical activities in particular. Although the effect of care coordination on self-management behaviors was not confirmed in this study, care coordination had a higher effect than diabetes education on glucose self-monitoring, suggesting that care coordination may be more beneficial on more complex self-care activities. Studies show that interventions that use self-efficacy focused education based on goal setting, practicing and recording self-management skills as well as persuasion techniques and peer models help reduce blood sugar levels, boost self-efficacy, encourage self-management behaviors, increase health literacy and improve overall quality of life of participants (Jiang et al., 2019).
Limitations of this study included the use of self-reported data. Social desirability and recalling issues may have biased the true prevalence of diabetes education and care coordination. Since diabetes education and care coordination were assessed with dichotomous, closed questions, we were not able to assess specific details on the mode, frequency and delivery of either one nor were we able to measure health literacy. The study design was cross-sectional, thus our findings cannot address causation of the associations. This was a population-based sample of individuals with type 2 diabetes covered by Medicaid and generalizability to other populations will be limited.
In conclusion, diabetes education and self-efficacy are positively associated with frequency of self-care behaviors. These findings can assist development of educational interventions for individuals with diabetes in disadvantaged populations. Future studies should investigate how self-efficacy based education can assist primary care givers, health educators and care coordinators to promote sustained positive behavior change. Educational interventions that improve self-efficacy can be used in combination with care coordinators’ and health providers’ efforts to initiate and maintain self-management activities.
Acknowledgments:
Funding: The project described was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (R18DK109501, Cherrington). Support was also provided by UAB Diabetes Research Center (P30 DK079626, Cherrington). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, the Agency for Healthcare Research and Quality, or the Alabama Medicaid Agency. Representatives for the Alabama Medicaid Agency were provided an opportunity to review and provide comments on the manuscript prior to submission. This manuscript was not prepared in collaboration with the Alabama Medicaid Agency and does not necessarily reflect the opinions or represent the official views of the Alabama Medicaid Agency.
References
- Al Sayah F, Majumdar SR, Williams B, Robertson S, & Johnson JA (2013). Health literacy and health outcomes in diabetes: a systematic review. Journal of general internal medicine, 28(3), 444–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Diabetes Association. (2020). Standards of Medical Care in Diabetes 2020. Diabetes Care, 43, S1–S224. [DOI] [PubMed] [Google Scholar]
- Bandura A (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2), 191–215. doi: 10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]
- Bandura A (1998). Health promotion from the perspective of social cognitive theory. Psychology and health, 13(4), 623–649. [Google Scholar]
- Bandura A, Reese L, & Adams NE (1982). Microanalysis of action and fear arousal as a function of differential levels of perceived self-efficacy. J Pers Soc Psychol, 43(1), 5–21. doi: 10.1037//0022-3514.43.1.5 [DOI] [PubMed] [Google Scholar]
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, & Crotty K (2011). Low health literacy and health outcomes: an updated systematic review. Ann Intern Med, 155(2), 97–107. doi: 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- Brooks T, Roygardner L, & Artiga S (2019). Medicaid and CHIP eligibility, enrollment, and cost sharing policies as of January 2019: Findings from a 50-state survey. Georgetown University Center for Children and Families, available at https://www.kff.org/medicaid/report/medicaid-and-chip-eligibility-enrollment-and-cost-sharing-policies-asof-january-2019-findings-from-a-50-state-survey. [Google Scholar]
- Control, C. f. D., & Prevention. (2020). National diabetes statistics report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services. [Google Scholar]
- Cox RH, Carpenter JP, Bruce FA, Poole KP, & Gaylord CK (2004). Characteristics of Low-Income African-American and Caucasian Adults That Are Important in Self-Management of Type 2 Diabetes. Journal of Community Health, 29(2), 155–170. doi: 10.1023/B:JOHE.0000016719.89848.b1 [DOI] [PubMed] [Google Scholar]
- Gonzalez JS, Peyrot M, McCarl LA, Collins EM, Serpa L, Mimiaga MJ, & Safren SA (2008). Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care, 31(12), 2398–2403. doi: 10.2337/dc08-1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankonen N, Absetz P, Haukkala A, & Uutela A (2009). Socioeconomic status and psychosocial mechanisms of lifestyle change in a type 2 diabetes prevention trial. Ann Behav Med, 38(2), 160–165. doi: 10.1007/s12160-009-9144-1 [DOI] [PubMed] [Google Scholar]
- Hawthorne K, Robles Y, Cannings-John R, & Edwards AG (2008). Culturally appropriate health education for type 2 diabetes mellitus in ethnic minority groups. Cochrane Database Syst Rev(3), Cd006424. doi: 10.1002/14651858.CD006424.pub2 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach: Guilford publications. [Google Scholar]
- Healthy People 2030. (2020. ). Increase the proportion of people with diabetes who get formal diabetes education — D‑06. Retrieved August 28, 2020, from https://health.gov/healthypeople/objectives-and-data/browse-objectives/diabetes/increase-proportion-people-diabetes-who-get-formal-diabetes-education-d-06
- Jiang X, Wang J, Lu Y, Jiang H, & Li M (2019). Self-efficacy-focused education in persons with diabetes: a systematic review and meta-analysis. Psychology research and behavior management, 12, 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krichbaum K, Aarestad V, & Buethe M (2003). Exploring the connection between self-efficacy and effective diabetes self-management. Diabetes Educ, 29(4), 653–662. doi: 10.1177/014572170302900411 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, & Mokdad AH (2009). The PHQ-8 as a measure of current depression in the general population. J Affect Disord, 114(1–3), 163–173. doi: 10.1016/j.jad.2008.06.026 [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter PL, & Jacquez A (2005). Outcomes of Border Health Spanish/English Chronic Disease Self-management Programs. The diabetes educator, 31(3), 401–409. doi: 10.1177/0145721705276574 [DOI] [PubMed] [Google Scholar]
- Mackinnon DP, & Dwyer JH (1993). Estimating Mediated Effects in Prevention Studies. Evaluation Review, 17(2), 144–158. doi: 10.1177/0193841x9301700202 [DOI] [Google Scholar]
- Mackinnon DP, Warsi G, & Dwyer JH (1995). A Simulation Study of Mediated Effect Measures. Multivariate Behav Res, 30(1), 41. doi: 10.1207/s15327906mbr3001_3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddux JE, Sherer M, & Rogers RW (1982). Self-efficacy expectancy and outcome expectancy: Their relationship and their effects on behavioral intentions. Cognitive Therapy and Research, 6(2), 207–211. [Google Scholar]
- Peña-Purcell NC, Boggess MM, & Jimenez N (2011). An empowerment-based diabetes self-management education program for Hispanic/Latinos: a quasi-experimental pilot study. Diabetes Educ, 37(6), 770–779. doi: 10.1177/0145721711423319 [DOI] [PubMed] [Google Scholar]
- Powers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, Hess-Fischl A, … Uelmen S (2020). Diabetes Self-management Education and Support in Adults With Type 2 Diabetes: A Consensus Report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care, 43(7), 1636–1649. doi: 10.2337/dci20-0023 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36(4), 717–731. doi: 10.3758/BF03206553 [DOI] [PubMed] [Google Scholar]
- Ratcliffe M, Burd C, Holder K, & Fields A (2016). Defining rural at the US Census Bureau. American community survey and geography brief, 1(8). [Google Scholar]
- Ricci-Cabello I, Ruiz-Pérez I, Rojas-García A, Pastor G, Rodríguez-Barranco M, & Gonçalves DC (2014). Characteristics and effectiveness of diabetes self-management educational programs targeted to racial/ethnic minority groups: a systematic review, meta-analysis and meta-regression. BMC Endocr Disord, 14, 60. doi: 10.1186/1472-6823-14-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosal MC, Ockene IS, Restrepo A, White MJ, Borg A, Olendzki B, … Reed G (2011). Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income latinos: latinos en control. Diabetes Care, 34(4), 838–844. doi: 10.2337/dc10-1981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar U, Fisher L, & Schillinger D (2006). Is Self-Efficacy Associated With Diabetes Self-Management Across Race/Ethnicity and Health Literacy? Diabetes Care, 29(4), 823–829. doi: 10.2337/diacare.29.04.06.dc05-1615 [DOI] [PubMed] [Google Scholar]
- Schoenthaler A, Ogedegbe G, & Allegrante JP (2009). Self-Efficacy Mediates the Relationship Between Depressive Symptoms and Medication Adherence Among Hypertensive African Americans. Health Education & Behavior, 36(1), 127–137. doi: 10.1177/1090198107309459 [DOI] [PubMed] [Google Scholar]
- Toobert DJ, Hampson SE, & Glasgow RE (2000). The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care, 23(7), 943–950. doi: 10.2337/diacare.23.7.943 [DOI] [PubMed] [Google Scholar]
- Valen MS, Narayan S, & Wedeking L (2012). An innovative approach to diabetes education for a Hispanic population utilizing community health workers. J Cult Divers, 19(1), 10–17. [PubMed] [Google Scholar]
- Wallston KA, Rothman RL, & Cherrington A (2007). Psychometric properties of the Perceived Diabetes Self-Management Scale (PDSMS). J Behav Med, 30(5), 395–401. doi: 10.1007/s10865-007-9110-y [DOI] [PubMed] [Google Scholar]


