Abstract
Background:
Unilateral cleft palates have a large spectrum of variability. Key morphologic factors such as cleft width and palatal length are not represented in current classification systems. Palate length and velopharyngeal port size are clinically linked to speech outcomes, as the soft palate must close the posterior pharynx for proper phonation. This study investigates the relationship between objective preoperative measures and postoperative velopharyngeal port size, to define a reproducible severity scale.
Methods:
Surgical data were prospectively collected from unilateral cleft palate patients in Morocco, Bolivia, Vietnam, and Madagascar. Key measurements were cleft width and palate width at the hard–soft palate junction, alveolar cleft width, vertical alveolar discrepancy, velopharyngeal port size. Cleft width ratio (CWR) was defined as the width of the cleft at the hard–soft junction, divided by the palate width.
Results:
Seventy-six patients were evaluated. Thirty-one had complete clefts and average age at surgical repair was 2.9 years. Mean CWR was 0.50 ± 0.12. Palate length was increased by an average of 2.2 mm (11%) after palatoplasty. Multivariate analysis determined greater CWR and larger preoperative velopharyngeal ports were significantly correlated with a smaller percent change in palate length after palatoplasty (P < 0.01).
Conclusions:
A wider palatal cleft decreases the surgeon’s ability to decrease velopharyngeal port size through palatoplasty. Given the ease of measurement even in low-resource settings, CWR may be a valuable tool for setting expectations for speech results, modifying surgical technique, and correlating future speech outcomes in evidence-based cleft care.
INTRODUCTION
Unilateral cleft palates have a wide range of morphologic variability. Classification systems created in the last century capture location of the cleft but do not address disease severity or likelihood of a successful surgical outcome. Consequently, there is no universally used method to categorize preoperative severity of a cleft palate. Communication among surgeons and data standardization remains a challenge.
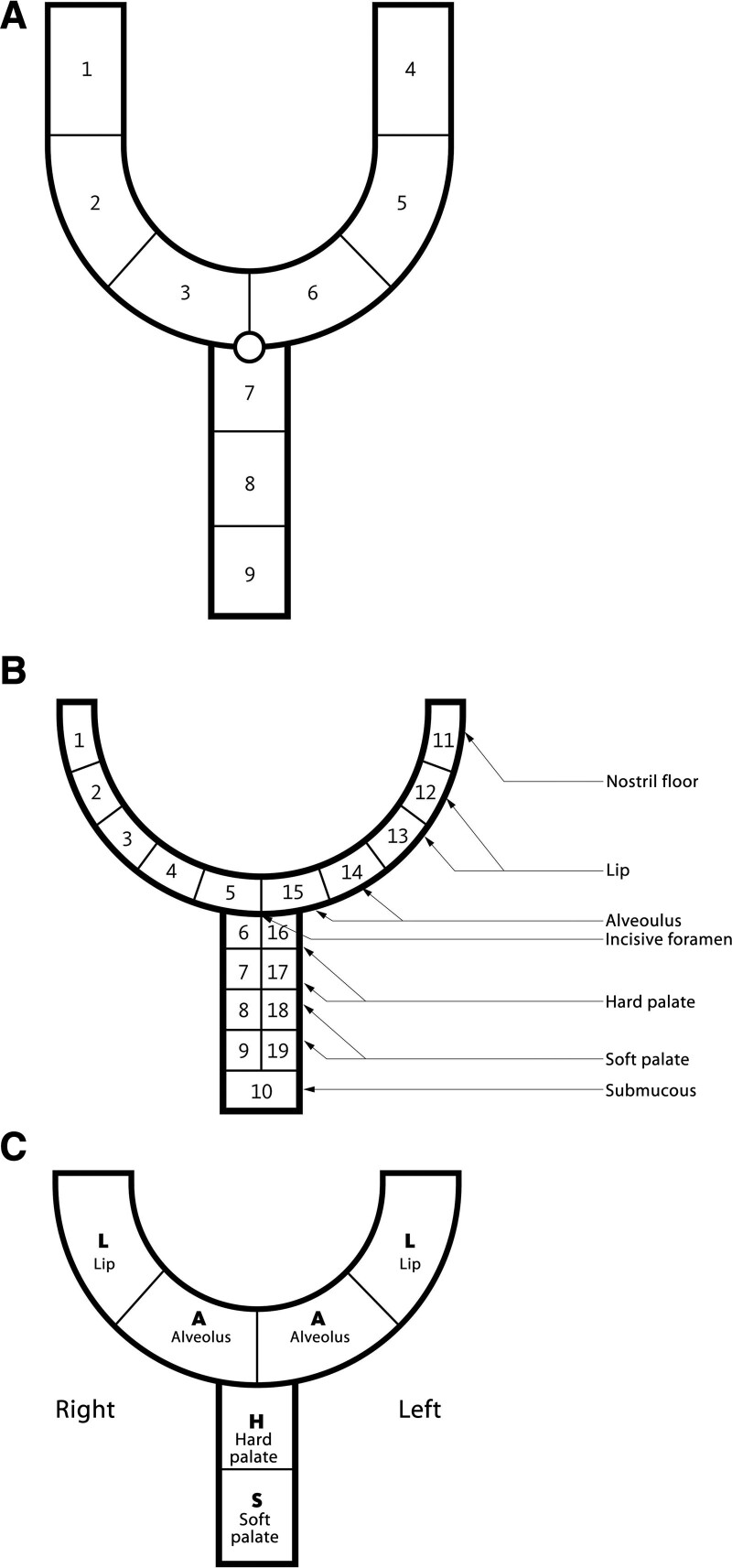
In 1931, Veau1 focused on the anterior-posterior extent of the cleft palate and created four cleft groups based on laterality and extent of hard palate and alveolar involvement: soft palate only, soft palate extending into the hard palate, complete unilateral, and complete bilateral. Forty years later, Kernahan (1971) introduced modifications to the Veau system.2 In their Y-shaped classification, the upper limbs represent the left and right sides of the primary palate and the lower limb represents the hard and soft palate (Fig. 1A). Noordoff3 modified the Kernahan and Stark Y classification to accommodate laterality (Fig. 1B). Kriens4 introduced a palindromic classification with the acronym “LAHSHAL,” describing the bilateral anatomy of the lip (L), alveolus (A), hard (H), and soft (S) palates from right to left. LAHSHAL is used in the outcomes registry for the American Cleft Palate and Craniofacial Association (Fig. 1C).
FIG. 1.
A, The “striped-Y” classification system developed by Kernahan that divides the primary and secondary palate by the incisive foramen. B, Noordhoff’s double-Y number classification, allowing more precision for laterality. C, Kriens’ LAHSHAL pictographic palindrome of anatomic structures involved in a cleft.
The systems above describe the location of a cleft but fail to address two aspects of disease morphology that have important implications for surgical success and future speech outcomes: cleft width and palate length. Bardach defined a “wide” cleft palate as a palatal gap greater than 1.5 cm,5 whereas others describe an “extremely wide” cleft as a defect larger than the width of both palatal shelves.6 Multiple studies have correlated wider clefts with increased rates of postpalatoplasty fistula and velopharyngeal insufficiency.7–10 Lengthening the soft palate through palatoplasty decreases the velopharyngeal port size, and is critical for allowing closure of the posterior pharynx and normal phonation. Randall et al11 demonstrated that patients with longer palates (smaller velopharyngeal ports) postoperatively had better speech outcomes.
The low incidence of cleft disease, variable treatment algorithms, and barriers to long-term follow-up make large-scale studies difficult. Recording objective phenotypic data before and after surgery is challenging, given the lack of a standardized severity scale.12 Consistent and easy to record measurements would mitigate obstacles for analytic research in cleft palate. Our previous work (“The Smile Index” Part 1 and Part 2) identified universal and reproducible measurements for unilateral cleft lip that correlated with clinical outcomes.13,14 We aim to similarly guide surgical expectations and surgical technique selection in unilateral cleft palate by recommending objective measures that represent disease severity.
METHODS
This prospective study includes all children with unilateral cleft through the hard and soft palate (with or without cleft lip) who received a primary palatoplasty at Operation Smile surgical mission sites in Hanoi, Vietnam (November 2014), Santa Cruz, Bolivia (March 2015), Dakhla, Morocco (April 2015), and Antananarivo, Madagascar (April 2015). Locations were chosen based on geographic and ethnic diversity. Operation Smile is an international not-for-profit organization that offers free surgical treatment for cleft lip and palate. This study was approved by the institutional review board of the University of Southern California and Operation Smile International.
Demographic, photographic, physical examination, and surgical data were recorded using an encrypted iPhone application designed for this study. (See figure, Supplemental Digital Content 1, which displays the screenshots from the iPhone application developed for this study, used to collect measurements for (a) palate width and cleft width ratio (CWR), and (b) velopharyngeal port size. http://links.lww.com/PRSGO/B806.)
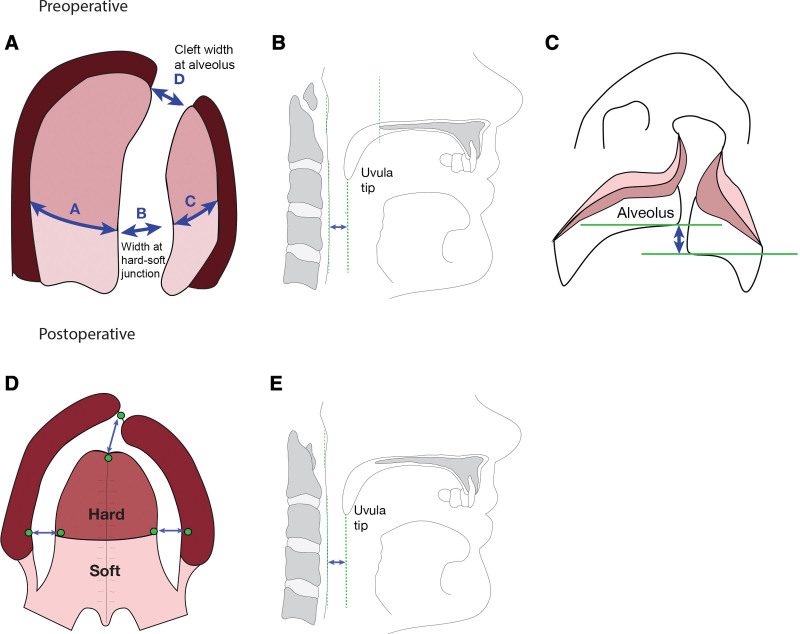
Figure 2 details the landmarks, measurements, and ratios documented for each patient preoperatively and postoperatively. Metrics were chosen from the related literature by Noordhoff,3 Bardach,5 Landheer et al,7 Rossel-Perry et al,8 and Phua and de Chalain.9 Linear distances were measured by the first author, a pediatric plastic surgeon specializing in cleft surgery, using a caliper to the nearest 0.5 mm. CWR was defined as the width of the cleft at the hard–soft junction, divided by the full palate width (Fig. 2A). Alveolar discrepancy was the vertical distance between the inferior-most aspect of the greater and lesser segment (Fig. 2C). Velopharyngeal port size was defined as the distance from the tip of uvula to the posterior pharynx (Fig. 2B and E); this was measured using a depth gauge with the patient supine and a Dingman retractor in place. Velopharyngeal port size was used to infer palate length. Figure 2D demonstrates how the size of anterolateral mucosal gaps was measured.
FIG. 2.
Measurement definitions: (A) Palate measurements: CWR (at the hard–soft junction) = B/A+C; Alveolar CWR = D/A+C. B, Preoperative velopharyngeal port size (distance from tip of uvula to posterior pharynx). C, Alveolar height difference. D, Width of raw surfaces resulting from relaxing incisions or palatal flap pushback. E, Postoperative velopharyngeal port size (palate length proxy).
RESULTS
We examined 76 patients with unilateral cleft palate from four countries: Bolivia (n = 15), Vietnam (n = 35), Morocco (n = 8), and Madagascar (n = 28). Fifty-four cleft palates were left-sided and 31 were complete. The majority had cleft lip and palate (n = 57), whereas 19 patients had isolated cleft palate. Average age at palatoplasty was 2.9 years (range 10 months–11 years) with an average weight of 12.0 kg. Cleft palate repairs were done by 13 different surgeons, who all used variations of a two-flap palatoplasty technique with islandization. In this approach, mucoperiosteal flaps are raised based on the greater palatine neurovascular bundles, elevating the flaps from the hard palate and the muscle attached to the posterior edge of it, providing significant mobilization toward midline. The two flaps are then pushed back, leaving a raw area anteriorly and laterally. Surgeon experience ranged from 1 to 25 years of posttraining practice, with a mean of 12 years of experience.
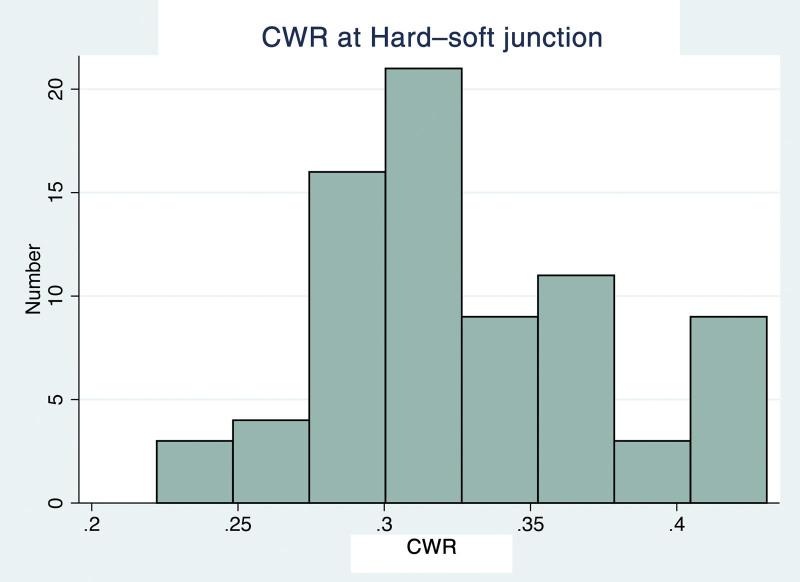
Mean and median CWR were 0.50 ± 0.12 and 0.48, respectively. The distribution of CWR was skewed to the right (Fig. 3). Velopharygeal port size (distance from the tip of uvula to the posterior pharynx) had a preoperative mean of 14.4 mm ± 4.0 mm and a postoperative mean of 12.2 mm ± 3.6 mm (P < 0.01, paired t-test), representing an average palatal length increase of 2.2 mm (11%, range −4 to 12 mm). The palate was lengthened in 57 cases (75%). Mean CWR at the alveolus (width of the alveolar cleft divided by the width of the palate) was 0.07 ± 0.06.
FIG. 3.
Histogram of CWR, demonstrating a rightward skew.
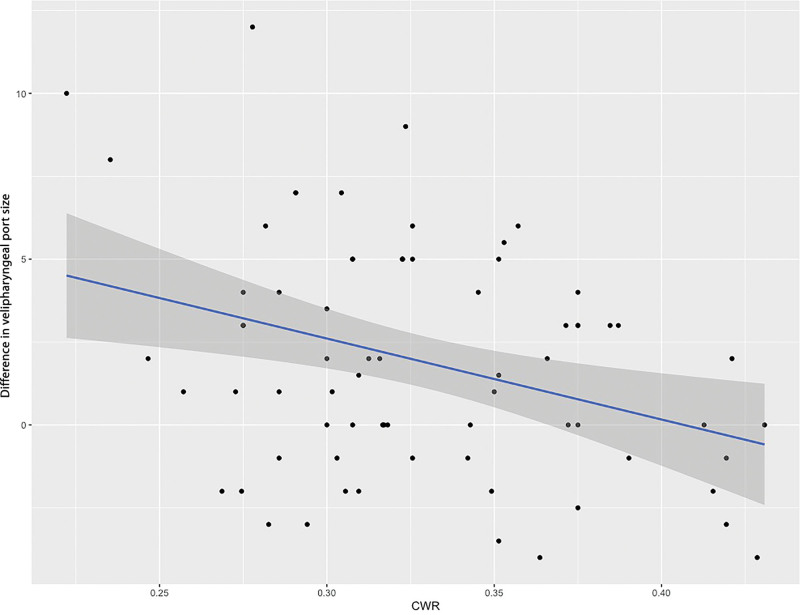
Univariate analysis showed no significant correlation between the change in velopharyngeal port size and the following variables: patient weight, surgeon experience, cleft laterality, alveolar cleft width, and postoperative anterolateral mucosal gap (Table 1). Preoperative velopharyngeal port size and postoperative mucosal gap (cumulative) were not significantly correlated (R-squared = 0.2, P = 0.21). Smaller velopharyngeal port size (longer palate) after surgery significantly correlated with smaller CWR (P < 0.01, Fig. 4), smalle. preoperative velopharyngeal port size (P < 0.01, Fig. 5), and less alveolar height discrepancy (P < 0.01).
TABLE 1.
Univariate Analysis of Patient and Cleft Characteristics Associated with Decreased Postoperative Velopharyngeal Port Size
| Characteristic | Coefficient | Univariate Analysis | ||
|---|---|---|---|---|
| 95% CI | P | |||
| Weight (kg) | 0.016 | −0.19 | 0.23 | 0.88 |
| Surgeon experience | 0.94 | −3.48 | 2.68 | 0.29 |
| Cleft laterality (right) | 0.012 | −1.83 | 1.86 | 0.99 |
| CWR | −24.42 | −40.58 | −8.26 | 0.004 |
| Alveolar height discrepancy | 2.00 | 3.21 | 0.79 | <0.01 |
| Preoperative velopharyngeal port size | 0.47 | 0.29 | 0.64 | <0.01 |
| Postoperative mucosal gap | 0.096 | −0.041 | 0.23 | 0.17 |
Bold values indicate variables that were significant (p < 0.05).
FIG. 4.
Greater reduction in velopharyngeal port size after cleft palate repair was significantly correlated with lower CWR.
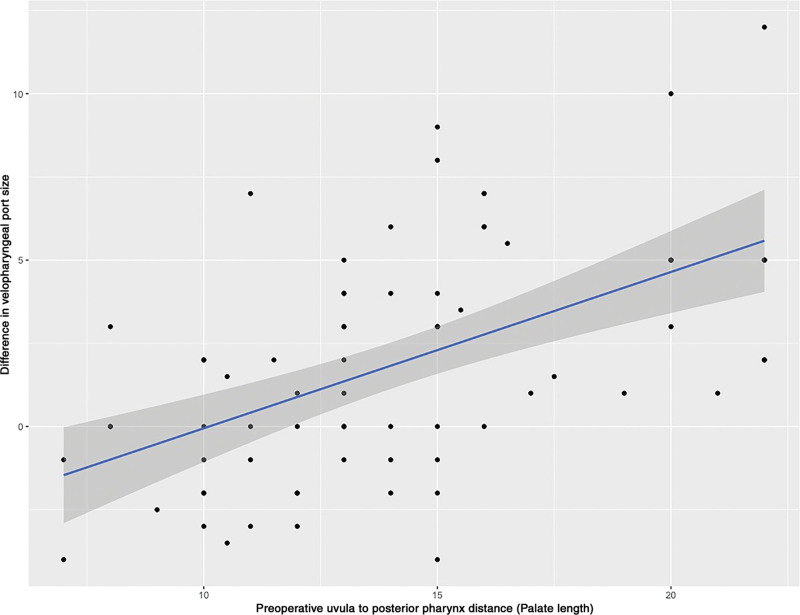
FIG. 5.
Reduction in velopharyngeal port size after cleft palate repair was significantly correlated with smaller preoperative velopharyngeal port (longer palate length).
There was a strong correlation between complete cleft palate and greater CWR (B = −15.6, P ≤ 0.01, logistic). Preoperative velopharyngeal port size was not significantly associated with CWR (B = −16.9, B = 0.07) or complete cleft palate (B = 0.13, P = 0.07).
Stepwise multivariate regression examined which of the following variables were most predictive of increasing palate length: CWR, preoperative velopharyngeal port size, preoperative alveolar discrepancy, cleft completeness, cleft laterality, child weight, country of origin, and surgeon experience (sle = sls = 0.15). CWR (P = 0.07) and velopharyngeal port size (a proxy for palate length, P < 0.01) were the only significant predictors of postoperative velopharyngeal port size.
DISCUSSION
Surgeons intuitively know that initial cleft characteristics play an important role in case planning, technical challenges, and surgical results. Existing literature confirms that wider clefts present greater operative difficulty and are associated with more postoperative velopharyngeal insufficiency.10,15–19 We found that simple preoperative metrics may be used to anticipate palatoplasty outcomes. Initial size of the cleft was the most intuitive, easy to measure and influential characteristic associated with ability to decrease the size of the velopharyngeal port. Preoperative velopharyngeal port size was also a strong predictor, but this variable is harder to visualize and impossible to measure in an awake patient.
Wider clefts were significantly more likely to be a complete cleft, but complete cleft was not an important predictor for postoperative velopharyngeal port size. Although repair of complete cleft palates is often regarded as more technically difficult, our model shows that cleft width may be the most important consideration. Complete cleft palate and vertical alveolar discrepancy were strong predictors in univariate regression, but not significant in multivariate stepwise regression. Shorter palates (large velopharyngeal ports) preoperatively achieved the most lengthening through palatoplasty, with diminishing returns as preoperative length increased. Our results showed a decreased ability to surgically lengthen the palate in wider clefts. There may be a relatively static upper limit for the length a palate can gain from palatoplasty.
Data have repeatedly shown an association between wider clefts and postpalatoplasty fistula. Rossell-Perry et al7 proposed a “palatal index” severity scale to quantify tissue deficiency in a cleft palate. Specialized computer software was used to analyze intraoperative photographs and calculate the surface area of missing tissue relative to intact palate. Their retrospective analysis of 152 unilateral cleft patients from a single-surgeon found a strong association between palatal index and fistula at 1- to 5-year follow-up.7 Landheer et al’s series of 121 patients demonstrated that cleft width greater than 13 mm was associated with postoperative fistula.8 Despite an emerging emphasis on palate width, there have been few translations to clinical use. The index presented in this study can be measured easily during patient examination and does not require sophisticated software.
The effect of palatal lengthening on velopharyngeal port size was chosen as the outcome of interest based on multiple studies demonstrating an association between palatal length and rates of fistula and velopharyngeal insufficiency. Short palate length after palatoplasty has been linked to poor speech outcomes, as the soft palate must reach the posterior pharynx for proper phonation and correction of hypernasal speech.11,16–19 As early as the 19th century, surgeons believed a “nasal quality in speech was due to shortening of the palate.”20,21 Interestingly, in this study, ability to lengthen the palate did not come through direct posterior transposition of palatal tissue. We hypothesized larger mucosal gaps would occur after palatoplasty with wider clefts, as surgeons would need more palatal flap pushback for more severe disease morphology. This was not the case. As all surgeons used variations of the two-flap technique, it is possible that palatal lengthening was primarily achieved through soft-tissue movement via surgical dissection, and not direct posterior transposition of palatal tissue.
Given our multiethnic cohort from four countries and inclusion of 13 surgeons with different levels of experience, results from this report are more generalizable than typical single-surgeon cleft studies. A larger study population from a greater number of countries would ensure widely generalizable results. Although hand measurements have an element of error, our measurements were more consistent because they were taken by the same surgeon. Most surgeons make personal modifications to the two-flap technique, making surgical technique consistency a limitation. Our results may not be applicable to palatoplasty techniques other than the two-flap, such as Furlow. Additionally, surgeons may have different anatomical goals of palatoplasty; although some prioritize lengthening the palate for speech improvement, others prioritize minimal dissection to prevent scarring. Lack of longitudinal follow-up made it impossible to track fistula rates, speech development, or other complications. Without long-term speech data, we could not validate velopharyngeal port size as our outcome of interest. International cohorts from surgical missions are inherently limited in longitudinal follow-up due to a lack of resources. Extending this study to children’s hospitals in the United States could determine whether immediate postoperative velopharyngeal port size is related to long-term speech outcomes.
CONCLUSIONS
CWR is a scale for cleft palate disease severity that is easily measured and affects the ability to lengthen the palate through surgery. Although other factors such as preoperative velopharyngeal port size, completeness of cleft, and alveolar height discrepancy are also associated with palate lengthening through palatoplasty, these variables tell an incomplete story. Current classification systems describe basic cleft anatomy, but do not account for aspects of disease severity that surgeons intuitively identify. CWR captures important prognostic aspects of morphology and offers a simple metric that may be used in future evidence-based studies of cleft palate.
Supplementary Material
Footnotes
Published online 22 October 2021.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Veau V. Division Palatine. Paris: Masson; 1931. [Google Scholar]
- 2.Kernahan DA. The striped Y–a symbolic classification for cleft lip and palate. Plast Reconstr Surg. 1971;47:469–470. [DOI] [PubMed] [Google Scholar]
- 3.Noordhoff MS, Wu J. Multidisciplinary management of cleft lip and palate in Taiwan. In: Bardach J, ed. Multidisciplinary Management of Cleft Lip and Palate. Philadelphia: WB Saunders; 1990:18–26. [Google Scholar]
- 4.Kriens O. Anatomy of the velopharyngeal area in cleft palate. Clin Plast Surg. 1975;2:261–288. [PubMed] [Google Scholar]
- 5.Bardach J, ed. Atlas of Craniofacial and Cleft Surgery. Vol 2. Philadelphia: Lippincott Raven; 1999. [Google Scholar]
- 6.Bumsted RM. A new method for achieving complete two-layer closure of a massive palatal cleft. Arch Otolaryngol. 1982;108:147–150. [DOI] [PubMed] [Google Scholar]
- 7.Rossell-Perry P, Caceres Nano E, Gavino-Gutierrez AM. Association between palatal index and cleft palate repair outcomes in patients with complete unilateral cleft lip and palate. JAMA Facial Plast Surg. 2014;16:206–210. [DOI] [PubMed] [Google Scholar]
- 8.Landheer JA, Breugem CC, van der Molen AB. Fistula incidence and predictors of fistula occurrence after cleft palate repair: two-stage closure versus one-stage closure. Cleft Palate Craniofac J. 2010;47:623–630. [DOI] [PubMed] [Google Scholar]
- 9.Phua YS, de Chalain T. Incidence of oronasal fistulae and velopharyngeal insufficiency after cleft palate repair: an audit of 211 children born between 1990 and 2004. Cleft Palate Craniofac J. 2008;45:172–178. [DOI] [PubMed] [Google Scholar]
- 10.Lam DJ, Chiu LL, Sie KC, et al. Impact of cleft width in clefts of secondary palate on the risk of velopharyngeal insufficiency. Arch Facial Plast Surg. 2012;14:360–364. [DOI] [PubMed] [Google Scholar]
- 11.Randall P, LaRossa D, McWilliams BJ, et al. Palatal length in cleft palate as a predictor of speech outcome. Plast Reconstr Surg. 2000;106:1254–1259. [DOI] [PubMed] [Google Scholar]
- 12.Sivertsen Å, Wilcox A, Johnson GE, et al. Prevalence of major anatomic variations in oral clefts. Plast Reconstr Surg. 2008;121:587–595. [DOI] [PubMed] [Google Scholar]
- 13.Yao CA, Imahiyerobo T, Swanson J, et al. The smile index: part 1. A large-scale study of phenotypic norms for preoperative and postoperative unilateral cleft lip. Plast Reconstr Surg. 2018;141:137–146. [DOI] [PubMed] [Google Scholar]
- 14.Yao CA, McCullough M, Auslander A, et al. The smile index: part 2. A simple, prognostic severity scale for unilateral cleft lip. Plast Reconstr Surg. 2019;143:790e–797e. [DOI] [PubMed] [Google Scholar]
- 15.Wu R, Cheraghlou S, Parsaei Y, et al. Does cleft palate width correlate with Veau classification and outcome? J Craniofac Surg. 2017;28:1369–1374. [DOI] [PubMed] [Google Scholar]
- 16.Fisher DM, Sommerlad BC. Cleft lip, cleft palate, and velopharyngeal insufficiency. Plast Reconstr Surg. 2011;128:342e–360e. [DOI] [PubMed] [Google Scholar]
- 17.Morris HL. Velopharyngeal competence and primary cleft palate surgery, 1960-1971: a critical review. Cleft Palate J. 1973;10:62–71. [PubMed] [Google Scholar]
- 18.Conley SF, Gosain AK, Marks SM, et al. Identification and assessment of velopharyngeal inadequacy. Am J Otolaryngol. 1997;18:38–46. [DOI] [PubMed] [Google Scholar]
- 19.Chen PK, Wu JT, Chen YR, et al. Correction of secondary velopharyngeal insufficiency in cleft palate patients with the Furlow palatoplasty. Plast Reconstr Surg. 1994;94:933–941. [PubMed] [Google Scholar]
- 20.Millard DR. Cleft Craft: The Evolution of its Surgery. Vol. 3. Boston: Little, Brown; 1980. [Google Scholar]
- 21.Passavant G. Ueber die verbesserung der sprache nach der uranoplastik. Arch Klin Chir. 1879;23:771–780. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.