Summary:
Total breast reconstruction with a fat-augmented latissimus dorsi flap (F-LDF) is a breakthrough approach that surmounts the shortcomings of the latissimus dorsi flap (LDF), such as volume insufficiency. Unlike the abdominal flap, the LDF can be harvested as a sole muscle flap without a skin paddle. This makes it possible to perform breast reconstruction with no donor-site scar when breast skin replacement is not required (eg, nipple-sparing mastectomy, two-stage reconstruction using a tissue expander). Here we describe a new approach for total breast reconstruction, namely scarless F-LDF reconstruction. First, the dorsal and ventral planes of the LDF are widely dissected through an inferolateral incision with monopolar electrocautery. The origin of the muscle is then separated using an energy-based device inserted through a stab incision, and immediate fat grafting is performed concurrently to the LDF and pectoralis major muscle. This new method was used in five cases, with a mean specimen weight of 285 g (range, 181–420), mean flap weight of 174 g (125–230), mean total fat graft volume of 214 ml (126–335), and mean duration of reconstruction surgery of 213 minutes (161–260). In all cases, sufficient volume was obtained postoperatively with satisfactory esthetic results. In addition to avoiding a donor-site scar, this method could reduce postoperative pain and donor-site seroma. The scarless F-LDF can be used for total breast reconstruction in certain populations, especially in cases requiring no skin replacement and for small- to medium-sized breasts.
Takeaways
Question: Autologous breast reconstruction leaves a conspicuous donor-site scar, and fat grafting requires multiple surgeries, which are drawbacks that need to be addressed.
Findings: Total breast reconstruction was successfully performed with a fat-augmented latissimus dorsi flap harvested with an energy-based device and augmented by immediate fat grafting, thereby achieving acceptable results while minimizing visible scarring without requiring any donor-site skin incision.
Meaning: This method can be a preferable option for total breast reconstruction in cases where skin replacement is not required and for small- to medium-sized breasts.
INTRODUCTION
Autologous breast reconstruction allows for restoration of natural breasts. Although large-volume tissue transfer is possible at the time of flap reconstruction, this leaves conspicuous donor-site scars. Autologous fat grafting achieves scarless reconstruction but requires more than three follow-up surgeries for total breast reconstruction.1 The fat-augmented latissimus dorsi flap (F-LDF) was first reported by Santanelli et al in 2014 as an innovative approach to compensate for volume insufficiency.2 Unlike the abdominal flap, the LDF can be harvested without a skin paddle; so, breast reconstruction without a donor-site scar is feasible if replacement of breast skin is not required (eg, nipple-sparing mastectomy, two-stage reconstruction using a tissue expander). Here, we describe a novel approach for scarless total breast reconstruction in which an LDF is harvested with an energy-based device and augmented by immediate concurrent fat grafting.
PROCEDURE
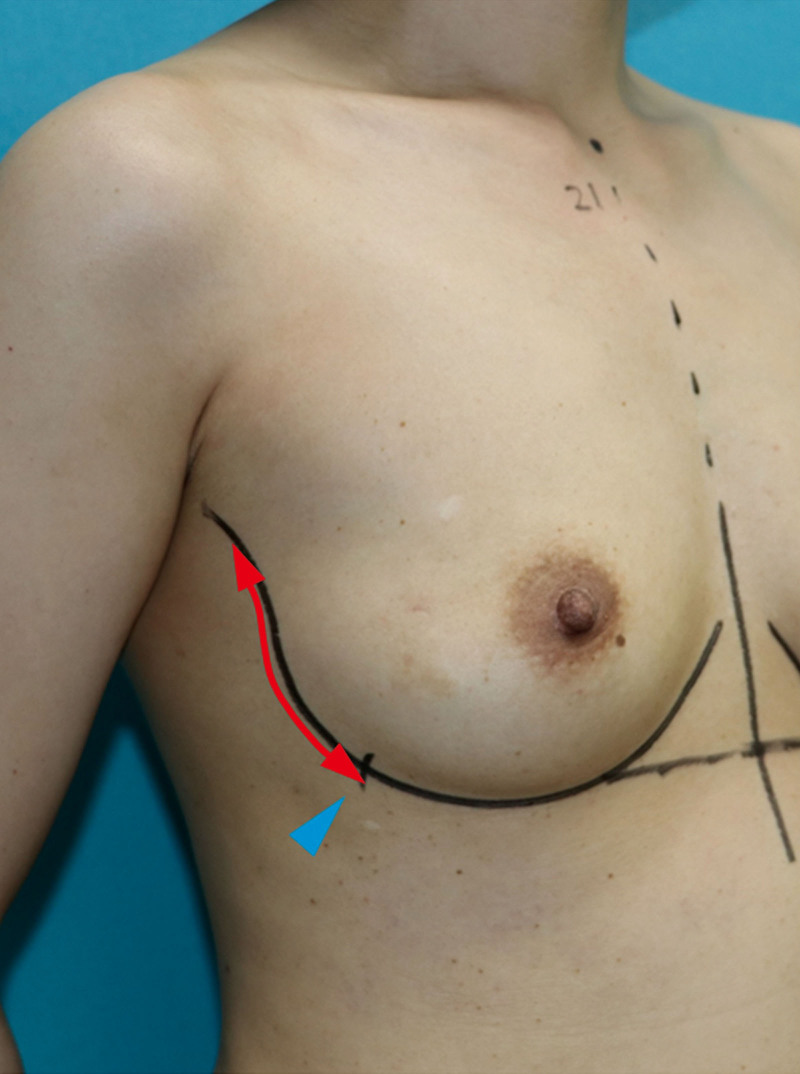
This study was approved by the review board of our institution. Informed consent was obtained from all patients. Our method is applicable in cases where an inferolateral incision has been made for mastectomy (Fig. 1, red arrow). If the mastectomy was performed at another facility, the incision is occasionally extended caudally so that the end of the incision is as low as the inframammary fold (Fig. 1, blue arrowhead), allowing direct visualization of the latissimus dorsi muscle (LDM). For two-stage reconstruction, the patient is placed in the lateral decubitus position, and for immediate reconstruction after mastectomy, the patient is moved from the supine to lateral decubitus position. The range of the LDM is marked on the skin of the back to the caudal lateral end, along with a marking for a stab incision through which an energy-based device is inserted. (See figure 1, Supplemental Digital Content 1, which displays the range of the LDM harvested and a marking for a stab incision through which an energy-based device is inserted. http://links.lww.com/PRSGO/B817.)
Fig. 1.
Our method is applicable only in cases where an inferolateral incision has been made for mastectomy (red arrow), and the end of the incision is as low as the inframammary fold (blue arrowhead).
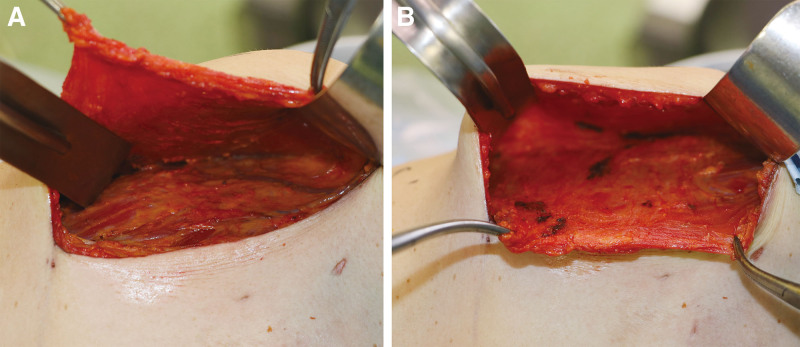
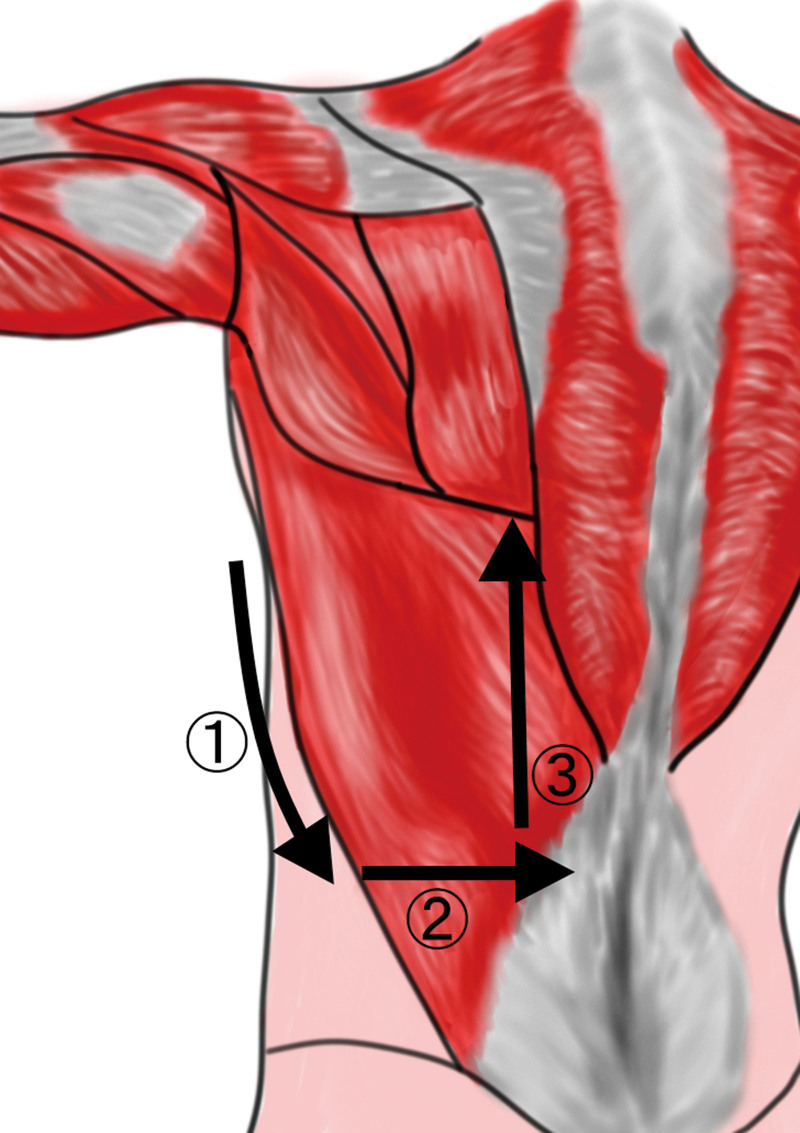
We use the LigaSure Maryland Jaw Open Sealer/Divider (23 cm, LF1923, Covidien) or ENSEAL X1 Tissue Sealer, Curved Jaw (25 cm, NSLX125C, Ethicon) to divide the origin of LDM. The muscle flap is elevated through the inferolateral incision, and after identifying the lateral border of the LDM, the ventral and dorsal planes of the muscle are widely dissected with monopolar electrocautery and a lighted retractor (Fig. 2). Great attention is paid while dissecting the medial and caudal areas of the muscle, as damaging the intercostal perforators coming through the chest wall can result in severe bleeding. Except around the insertion of the muscle, fat tissue below the superficial fascia is included in the flap to augment flap volume (Fig. 2B). After the two sides of the LDM are dissected, the lateral border is separated with monopolar electrocautery (Fig. 3, arrow 1), and further dissection from the caudal border to the medial border is made using an energy-based device inserted through the stab incision (Fig. 3, arrows 2 and 3). (See Video [online], which displays the actual operative technique.) At this stage, a penrose drain is inserted between the teres major muscle and LDM. By towing both ends of the drain together in the lateral direction, visualization near the midline is improved. Following this, the muscle is lifted outward to provide greater visualization and facilitate the identification of the thoracodorsal vessels and nerve. The insertion of the muscle is divided, paying attention to the pedicles, and the muscle paddle is freed completely. With the patient in the supine position, fat tissue is harvested from the bilateral thighs or abdomen and injected into the muscle paddle and pectoralis major muscle (PMM) using a 17-gauge epidural needle (length 12 cm; Hakko Medical Products, Tokyo, Japan), as previously described.3 We use a sharp needle instead of a blunt needle to inject microribbons of fat carefully in separate planes,1 especially when injecting into the muscle. The F-LDF is used to reconstruct the lower pole of the breast, whereas the upper pole is reconstructed by fat grafting to the PMM.
Fig. 2.
Dissection of the LDM. From the inferolateral incision, the ventral plane of the LDM is first dissected with monopolar electrocautery (A). Next, while pulling the lateral edge of the LDM with forceps, the dorsal plane of the LDM (just below the superficial fascia) is dissected (B).
Fig. 3.
Division of the origin of the LDM. First, the lateral edge of the LDM is divided with monopolar cautery (arrow 1), and further division proceeds from the caudal border (arrow 2) to the medial boarder (arrow 3) of the LDM using an energy-based device inserted through a stab incision at the lateral chest.
Video 1. this video displays the actual operative technique using an energy-based device.
RESULTS
Between December 2020 and April 2021, five patients with unilateral breast cancer underwent scarless F-LDF reconstruction (immediate reconstruction, 3; two-stage reconstruction, 2) at Osaka University Medical Hospital. Demographics, operative data, and complications are summarized in Table 1. Mean age was 45 years (range, 39–52), mean body mass index was 22.7 (18.1–26.6), mastectomy-specimen weight was 285 g (181–420), operative time (excluding mastectomy) was 213 minutes (161–260), flap weight was 174 g (125–230), and injected fat volumes were 138 ml (71–230) and 76 ml (55–105) for the flap and PMM, respectively. No major perioperative complication was noted, and donor-site seroma (if any) was resolved within 1 month after drain removal. Postoperative cosmetic outcomes were evaluated by three plastic surgeons using the Harvard scale4 (excellent, 3; good, 2; Table 1) (See figure 2, Supplemental Digital Content 2, which displays preoperative and postoperative views, respectively, of patient 2 at 6 months after right breast reconstruction. http://links.lww.com/PRSGO/B818.) (See figure 3, Supplemental Digital Content 3, which displays preoperative and postoperative views, respectively, of patient 3 at 7 months after left breast reconstruction. http://links.lww.com/PRSGO/B819.)
Table 1.
Patient Characteristics
| Patient | Age (y) | BMI (kg/m2) | Mastectomy Subtype | Timing of Reconstruction | Mastectomy Weight (g) | Flap Weight (g) | Volume of Fat Graft to Flap (ml) | Volume of Fat Graft to PMM (ml) | Operative Time (min) | Complications | Esthetic Outcome | Follow-up Period (mo) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 45 | 18.1 | NSM | Immediate | 181 | 125 | 71 | 55 | 161 | — | Good | 7 |
| 2 | 40 | 21.7 | NSM | Immediate | 208 | 180 | 153 | 59 | 189 | — | Good | 6 |
| 3 | 52 | 26.5 | NSM | Two-stage immediate | 420 | 230 | 230 | 105 | 245 | — | Excellent | 5 |
| 4 | 49 | 24.6 | NSM | Two-stage immediate | 286 | 140 | 142 | 69 | 212 | — | Excellent | 5 |
| 5 | 39 | 22.7 | SSM | Immediate | 330 | 195 | 94 | 91 | 260 | — | Excellent | 4 |
BMI, body mass index, NSM, nipple-sparing mastectomy, SSM, skin-sparing mastectomy.
DISCUSSION
The scarless LDF was originally developed as an autologous alternative to acellular dermal matrix.5 It leaves no donor-site scar, and skin-color mismatching at the recipient site is not a concern. Moreover, in addition to a reduced operative time and length of hospital stay, the occurrence of complications is reduced by 25% compared with traditional LDF reconstruction due to reduced seroma formation.6 Elevating the scarless LDF with an energy-based device further reduces seroma formation7 by enabling reliable division of the origin of the LDM, even without sufficient visibility. Although we did not quantitatively evaluate postoperative pain in this study, our method might also mitigate postoperative pain and the feeling of tightness at the donor site. Ioannidis et al reported that the systemic inflammatory response induced by skin-only surgical trauma is directly proportional to the length of skin incision in rodent models.8 Because scarless LDF reconstruction requires no skin incision at the donor site, postoperative pain can be significantly reduced.
Autologous breast reconstruction is associated with higher patient satisfaction psychosocially and sexually compared with implant-based reconstruction.9,10 The abdominal flap has been the gold standard in autologous reconstruction, whereas the LDF is often used as an ancillary flap in prosthesis-based reconstruction. Although the LDF may lack the tissue volume required for total breast reconstruction, fat grafting in F-LDF reconstruction ensures that acceptable results can be obtained especially for small- to medium-sized breasts.2,3
CONCLUSIONS
Although the number of cases is small, this study demonstrates that scarless F-LDF reconstruction provides acceptable results while minimizing visible scarring, as it requires no donor-site skin incision. This method might be a preferable option for total breast reconstruction when skin replacement is not required and for small- to medium-sized breasts.
Supplementary Material
Footnotes
Published online 22 October 2021.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Khouri RK, Rigotti G, Khouri RK, Jr, et al. Tissue-engineered breast reconstruction with Brava-assisted fat grafting: a 7-year, 488-patient, multicenter experience. Plast Reconstr Surg. 2015;135:643–658. [DOI] [PubMed] [Google Scholar]
- 2.Santanelli di Pompeo F, Laporta R, Sorotos M, et al. Latissimus dorsi flap for total autologous immediate breast reconstruction without implants. Plast Reconstr Surg. 2014;134:871e–879e. [DOI] [PubMed] [Google Scholar]
- 3.Taminato M, Tomita K, Nomori M, et al. Fat-augmented latissimus dorsi myocutaneous flap for total breast reconstruction: a report of 54 consecutive Asian cases. J Plast Reconstr Aesthet Surg. 2021;74:1213–1222. [DOI] [PubMed] [Google Scholar]
- 4.Harris JR, Levene MB, Svensson G, et al. Analysis of cosmetic results following primary radiation therapy for stages I and II carcinoma of the breast. Int J Radiat Oncol Biol Phys. 1979;5:257–261. [DOI] [PubMed] [Google Scholar]
- 5.Elliott LF, Ghazi BH, Otterburn DM. The scarless latissimus dorsi flap for full muscle coverage in device-based immediate breast reconstruction: an autologous alternative to acellular dermal matrix. Plast Reconstr Surg. 2011;128:71–79. [DOI] [PubMed] [Google Scholar]
- 6.Lee MA, Miteff KG. The scarless latissimus dorsi flap provides effective lower pole prosthetic coverage in breast reconstruction. Plast Reconstr Surg Glob Open. 2014;2:e147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee JS, Kim DG, Lee JW, et al. Usefulness of the LigaSure small jaw sealing device for breast reconstruction with a latissimus dorsi flap. J Plast Surg Hand Surg. 2019;53:295–300. [DOI] [PubMed] [Google Scholar]
- 8.Ioannidis A, Arvanitidis K, Filidou E, et al. The length of surgical skin incision in postoperative inflammatory reaction. JSLS. 2018;22:e2018.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fracon S, Renzi N, Manara M, et al. Patient satisfaction after breast reconstruction: implants vs. autologous tissues. Acta Chir Plast. 2018;59:120–128. [PubMed] [Google Scholar]
- 10.Santosa KB, Qi J, Kim HM, et al. Long-term patient-reported outcomes in postmastectomy breast reconstruction. JAMA Surg. 2018;153:891–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.