Abstract
Background
Although the association between malaria and anaemia is widely studied in patient cohorts, the population-representative causal effects of malaria on anaemia remain unknown. This study estimated the malaria-induced decrease in haemoglobin levels among young children in malaria-endemic Burkina Faso.
Methods
The study was based on pooled individual-level nationally representative health survey data (2010–2011, 2014, 2017–2018) from 17 599 children under 5 years of age. This data was used to estimate the effects of malaria on haemoglobin concentration, controlling for household fixed-effects, age, and sex in a series of regression analyses. The fixed-effects controlled for observed and unobserved confounding on the household level and allowed to determine the impact of malaria infection status on haemoglobin levels and anaemia prevalence. Furthermore, the diagnostic results from microscopy and rapid diagnostic tests were leveraged to provide a quasi-longitudinal perspective of acute and prolonged effects after malaria infection.
Results
The prevalence of both malaria (survey prevalence ranging from 17.4% to 65.2%) and anaemia (survey prevalence ranging from 74% to 88.2%) was very high in the included surveys. Malaria was estimated to significantly reduce haemoglobin levels, with an overall effect of − 7.5 g/dL (95% CI − 8.5, − 6.5). Acute malaria resulted in a − 7.7 g/dL (95% CI − 8.8, − 6.6) decrease in haemoglobin levels. Recent malaria without current parasitaemia decreased haemoglobin concentration by − 7.1 g/dL (95% CI − 8.3, − 5.9). The in-sample predicted prevalence of severe anaemia was 9.4% among malaria positives, but only 2.2% among children without malaria.
Conclusion
Malaria infection has a strong detrimental effect on haemoglobin levels among young children in Burkina Faso. This effect seems to carry over even after acute infection, indicating prolonged haemoglobin reductions even after successful parasite-elimination. The quasi-experimental fixed-effect approach adds a population level perspective to existing clinical evidence.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12936-021-03948-z.
Keywords: Malaria, Anaemia, Haemoglobin, Household fixed-effects, Burkina Faso, Rapid diagnostic tests, Microscopy
Background
Burkina Faso has, according to World Health Organization (WHO) data, by far the highest prevalence of anaemia worldwide among young children (86% in 2016) [1]. It is also among the countries in sub-Saharan Africa that are burdened the most by malaria [2]. A large portion (43.8%) of Burkinabe people live in conditions marked by extreme poverty (less than 1.90 USD a day) and they and their children are thus particularly vulnerable to anaemia, malaria, and the associated, serious long term health consequences [3, 4]. However, Burkina Faso was also the setting of a recent, highly promising malaria-vaccine trial [5].
Malaria is a disease, caused by the Plasmodium spp. parasites that replicate in the human liver and erythrocytes [6]. In 2019, malaria accounted for the deaths of 384,000 children younger than 5 years in sub-Saharan Africa, 4% of which occurred in Burkina Faso [2]. This high death toll is partially a consequence of acute anaemia, one of malaria’s most prominent complications. However, malarial anaemia can also become chronic through pathways of persistent inflammation and bone marrow suppression leading to reduced production of erythrocytes [7–9]. Since anaemic children have lower oxygen-capacity, they are more susceptible to opportunistic infections, more tired, and less resilient than healthy children [10]. These symptoms ultimately add up to a higher risk of cognitive and physical development deficits in anaemic young children [3, 10–14].
Anaemia is screened for by measuring blood haemoglobin (Hb [g/L]), the erythrocytic protein that binds oxygen. Although the effect of malaria on haemoglobin has been the subject of extensive clinical research, epidemiological investigations on the population impact are severely lacking. The difficulty with determining the malaria attributable effect to population-wide haemoglobin reductions lies in the complex aetiology of anaemia. Aside from malaria, anaemia in children can be caused by genetic predisposition, other infectious diseases and wider socio-economic factors, especially nutritional deficits [10]. These contributors to anaemia are difficult to measure and may vary substantially between and even within given countries, thus making it hard to causally determine the impact of any one particular contributor to anaemia on the population level.
Most epidemiologic studies that try to causally link malaria to population haemoglobin are conducted within relatively small local communities within highly endemic areas [9, 15–18]. They consistently report a detrimental effect over time of acute and repeated malaria infections on haemoglobin levels among children and adults [19–21]. While this important research confirms the causal effect of malaria on anaemia, external validity of these studies is often low due to regional restrictions and comparatively small or non-representative study populations. This study aims to build on this base by using an econometric modelling approach, fixed-effect analysis, that makes it possible to approximate causal effects by implicitly controlling for known and unknown confounders at the household level [22–25]. The household fixed-effect analysis is an extension on the analytic concept of repeated measures data, where every individual within a household is considered a measurement of the same entity, i.e., the household. This study applies the fixed-effect approach to a large cross-sectional and nationally representative dataset of young children in Burkina Faso, a country burdened by extreme prevalence of malaria and anaemia alike. Burkina Faso is therefore a highly relevant target in the effort to combat both (Fig. 1).
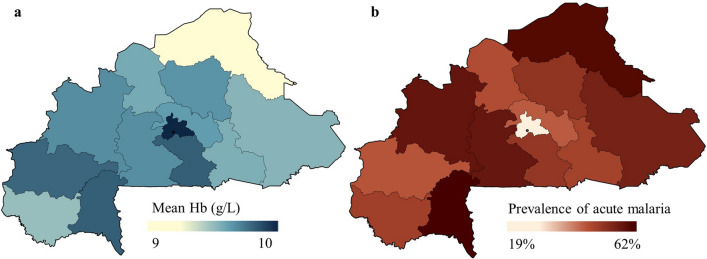
Fig. 1.
Map of the mean regional haemoglobin (a) and prevalence of malaria (b) in Burkina Faso. Panel a indicates the pooled mean regional haemoglobin values across all three surveys. Lighter colours represent lower average haemoglobin values and thus higher prevalence of anaemia. Panel b indicates the pooled mean regional prevalence of acute malaria as diagnosed by thick smear microscopy. Darker colours represent higher prevalence of anaemia. Demographic and Health Survey (DHS) and Malaria Indicator Survey (MIS) data obtained through https://dhsprogram.com/
This study aims to contribute to the fight against the harmful effects of anaemia in Burkina Faso by providing a better understanding of the contribution of malaria to the burden of anaemia. The quasi-experimental study design makes it possible to estimate the population-wide effect of malaria infection on haemoglobin levels in children, while avoiding ethically questionable randomized controlled study designs. This will also underline the importance of eliminating malaria and illustrates the potential gains from the recent vaccine candidate in Burkina Faso [5].
Methods
Data
The analysis is based on pooled data from the 2010 Demographic and Health Survey (DHS) and 2014 and 2017–18 Malaria Indicator Surveys (MISs) from Burkina Faso. The DHSs and MISs are nationally representative household surveys that include demographic, health, and nutrition data, including recognized malaria indicators. The combined datasets contained data from 17,599 children from 11,886 households divided over 572 sample clusters. Field operators collected the survey data from May 2010 to January 2011 (DHS 2010–2011), from September to October 2014 (MIS 2014) and from November 2017 to March 2018 (MIS 2017–2018). Malaria transmission in Burkina Faso is highest from July to November, therefore the pooled surveys reflect the annual average alongside changes between years, e.g., successful implementation of malaria programmes [26–28]. New households were selected for each survey; therefore, this study does not offer a longitudinal perspective on the individual households. During the surveys, field workers gathered data for two parallel methods of malaria diagnostics: rapid diagnostic antigen tests (RDT) for immediate screening results and thick smear microscopy (henceforth referred to as microscopy) to be analysed later in central laboratories. The RDT model for MIS 2014 and 2017–2018 was “SD Bioline Pan/Pf” (manufacturer: Standard Diagnostics, Inc.), a combined HRP-2/pLDH-test. The MIS 2010 final report did not specify the RDT model or type. Haemoglobin concentrations (g/L, Hb) were collected with the survey and measured by HemoCue test (manufacturer: HemoCue). More information on the data and collection process can be found at www.dhsprogram.com.
The following variables were extracted from the surveys for analysis: RDT results, microscopy test result, haemoglobin blood levels, age in months, sex, and household identifier. The severity of anaemia was categorized according to the WHO cut-off values for anaemia among children 59 and younger: any haemoglobin concentrations of less than 110 g/L were considered anaemia, further classified as mild (90–109 g/L), moderate (70–89 g/L) or severe anaemia (< 70 g/L) [29]. Age in months was converted to age groups by completed years (6–12; 13–24; 25–36; 37–48; 49–59 months).
The presence of Plasmodium spp. in the bloodstream was detected via thick smear microscopy, the current gold standard. Formally, ruling out malaria with microscopy requires three consecutive negative samples. Therefore, since survey samples were only collected once, DHS microscopy results are at risk of false negatives. Rapid diagnostic tests detect Plasmodium antigens in the blood stream for the diagnosis of malaria infections. These antigens have been reported to remain positive for up to 30 days after an acute is treated or controlled [30–32]. This results in a time window, where positive microscopy represents acute cases and positive RDTs with negative microscopy indicate post-infection status [33]. This time-lage was exploited to create a quasi-longitudinal perspective in the cross-sectional data to illustrate acute and prolonged effects of malaria on haemoglobin. Malaria status was further stratified into three separate groups for analysis, firstly “overall malaria” including all cases with any positive malaria test (RDT or microscopy), secondly “acute malaria” which included all cases that tested positive in microscopy screening and thirdly “sub-microscopic malaria” which included only those cases, that tested positive by RDT but negative by microscopy. A sub-microscopic infection refers to a time window either before or after the acute infection crosses the microscopy detection threshold and in addition to the time window when remaining circulating antigens cause the RDT to be positive after the acute infection has been cleared. Within this period, the patient is usually asymptomatic, but can be symptomatic in rare cases.
Statistical methods
The primary analysis estimated the population-level effect of malaria on haemoglobin concentrations (g/L) in a series of nested linear regression models. The first model, the overall malaria model, used any positive malaria-test result (RDT or microscopy) as indicator of malaria infection. The second, the stratified model, used the two malaria measurements, microscopy and RDT, to create three malaria-status groups: malaria negative (if microscopy and RDT negative), acute malaria (if microscopy positive), sub-microscopic malaria (if microscopy negative, but RDT positive). The (econometric) household fixed-effects were included in all primary analyses to control for observed and unobserved confounders that are shared between all children within one given household [22, 23]. These confounders include known factors such as socioeconomic, temporal, and spatial differences that vary between households but not within. Unknown factors could, amongst others, include nutritional or socio-economic traits which are likely shared between family members within one household but not across households [10].
The final model was stratified for malaria status, age, sex and household fixed-effect. For the mathematical formula of the final model please refer to Additional file 1: S29. Survey weights were not applied because the within-survey weights are not representative for multiple-survey analyses.
To provide a more tangible perspective on the malaria-attributable effect on anaemia prevalence in the observed population, in-sample predictions were generated to illustrate the possible changes in anaemia prevalence by eliminating malaria. The predictions were calculated based on the indidividual haemoglobin estimates from each child in the overall malaria and stratified models. For the predictions, anaemia was stratified into three clinically relevant severity groups (any anaemia if Hb < 110 g/L; moderate or worse anaemia if Hb < 90 g/L; severe anaemia if Hb < 70 g/L) to assess the influence of malaria on anaemia prevalence by severity.
Finally, an additional series of sensitivity analyses on the stratified model were performed to further validate the modelling approach. Firstly, the nested series was repeated to check for possible interaction between malaria, age, and sex, respectively and combined. Secondly, subgroup analyses were added based on sex, survey, and malaria season. An additional nested series with household modelled as random rather than fixed effect concluded the sensitivity analyses. The random-effects modelwas expected to show larger effects than the corresponding fixed-effects model.
All analyses were done in R version 4.0.2 or higher (“plm” package version 2.2-5, “fixest” package version 0.8.2). Maps were generated with ArcGIS Pro version 2.3.
Results
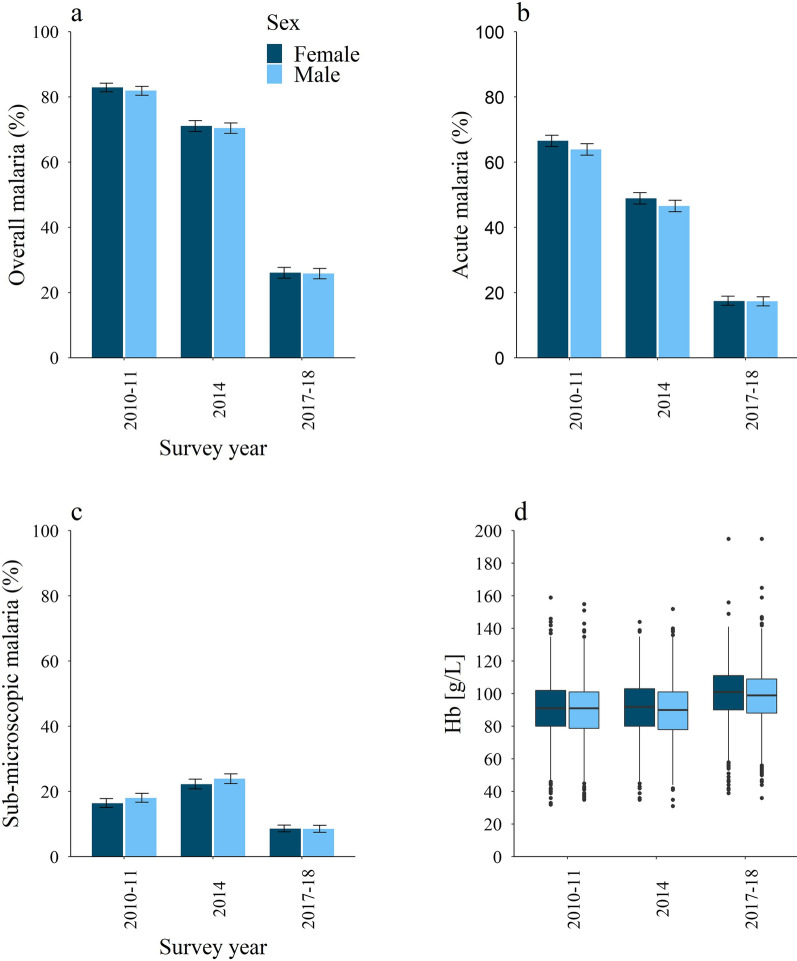
A summary of the population and survey characteristics is provided in Table 1. The final sample included 17 599 children from 11 816 households in Burkina Faso, aged 6 months to 5 years. Figure 2 and Table 1 present a more detailed description of malaria and anaemia in the study populations by survey. The prevalence of malaria varied between the consecutive surveys and averaged 44% for the pooled data (17.4–65.2%, Table 1). Anaemia (haemoglobin < 110 g/L) prevalence showed less variation between surveys but also declined over the years. The overall anaemia prevalence for the pooled data was 83.2%, 31.1% for moderate anaemia and 9.2% for severe anaemia. Regional distributions of malaria prevalence and average haemoglobin levels across the pooled surveys are shown in Fig. 1. An additional plot of the haemoglobin levels by malaria status, age, and sex was added to the Additional file 1: S30. The differences in mean haemoglobin for the subgroups of negative malaria and acute malaria [p < 0.001], negative malaria and sub-microscopic malaria [p < 0.001] and acute and sub-microscopic malaria [p < 0.001] were statistically significant in unpaired T-tests.
Table 1.
Characteristics of study population and subgroups
| Overall (pooled data sample) | Stratified by survey | Stratified by sex | ||||
|---|---|---|---|---|---|---|
| 2010–2011 May–Jana |
2014 Sept–Deca |
2017–2018 Dec–March |
Males | Females | ||
| Sample size | 17,599 | 5926 | 6110 | 5563 | 8962 | 8637 |
| Sex (%) | ||||||
| Female | 8637 (49.1) | 2882 (48.6) | 3003 (49.1) | 2752 (49.5) | – | – |
| Male | 8962 (50.9) | 3044 (51.4) | 3107 (50.9) | 2811 (50.5) | – | – |
| Age [months] (%) | ||||||
| 6–12 | 1918 (10.9) | 651 (11) | 657 (10.8) | 610 (11) | 984 (11) | 934 (10.8) |
| 13–24 | 3750 (21.3) | 1301 (22) | 1297 (21.2) | 1152 (20.7) | 1945 (21.7) | 1805 (20.9) |
| 25–36 | 3942 (22.4) | 1328 (22.4) | 1404 (23) | 1210 (21.8) | 2032 (22.7) | 1910 (22.1) |
| 37–48 | 4091 (23.2) | 1363 (23) | 1402 (22.9) | 1326 (23.8) | 2020 (22.5) | 2071 (24) |
| 49–59 | 3898 (22.1) | 1283 (21.7) | 1350 (22.1) | 1265 (22.7) | 1981 (22.1) | 1917 (22.2) |
| Malaria status (%) | ||||||
| Negative | 6954 (39.5) | 1045 (17.6) | 1787 (29.2) | 4122 (74.1) | 3558 (39.7) | 3396 (39.3) |
| Acute | 7740 (44) | 3861 (65.2) | 2913 (47.7) | 966 (17.4) | 3876 (43.2) | 3864 (44.7) |
| Sub-microscopic | 2905 (16.5) | 1020 (17.2) | 1410 (23.1) | 475 (8.5) | 1528 (17) | 1377 (15.9) |
| Anaemia | ||||||
| Mean Hb (g/L) (SD) | 93 (17) | 90 (17) | 90 (17) | 99 (17) | 92 (17) | 94 (17) |
| Anaemic | 14 639 (83.2) | 5229 (88.2) | 5291 (86.6) | 4119 (74) | 7576 (84.5) | 7063 (81.8) |
| Not anaemic | 2960 (16.8) | 697 (11.8) | 819 (13.4) | 1444 (26) | 1386 (15.2) | 1574 (18.2) |
| Mild | 7535 (42.8) | 2464 (41.6) | 2382 (39) | 2689 (48.3) | 3802 (42.4) | 3733 (43.2) |
| Moderate | 5482 (31.1) | 2135 (36) | 2112 (34.6) | 1235 (22.2) | 2856 (31.9) | 2626 (30,4) |
| Severe | 1622 (9.2) | 630 (10.6) | 797 (13.0) | 195 (3.5) | 918 (10.2) | 704 (8.2) |
Anaemia categories: Not anaemic (Hb ≥ 110 g/L); Mild anaemia (Hb < 110 g/L); Moderate anaemia (Hb < 90 g/L); Severe anaemia (Hb < 70 g/L) [29]. Due to rounding the percent might not add up to 100
Hb haemoglobin, SD standard deviation, TSM thick smear microscopy, RDT rapid diagnostic test
aTime frames covering malaria peak season in Burkina Faso from July to November
Fig. 2.
Prevalence of overall (a), acute (b) and sub-microscopic malaria (c); Haemoglobin concentrations [g/L] (d). The plots demonstrate the change in the study populations from the successive surveys based on sex. The error bars mark the 95% confidence intervals in panels a, b and c. Dark blue (dark grey, left column) represents females, light blue (grey, right column) represents males. Demographic and Health Survey (DHS) and Malaria Indicator Survey (MIS) data obtained through https://dhsprogram.com/
The outcomes of the overall malaria and stratified models and the respective reductions in haemoglobin are summarised in Table 2. In the overall model, a positive malaria test (RDT or microscopy) reduced haemoglobin by − 7.5 g/L [95% CI − 8.5; − 6.5]. In the stratified model (by malaria infection duration), acute malaria resulted in a − 7.7 g/L [95% CI − 8.8; − 6.6] decrease in haemoglobin concentration after controlling for age and sex. The prolonged effect after a cleared malaria infection was − 7.1 g/L [95% CI − 8.3; − 5.9] (Additional file 1: S30). Older age had an increasingly beneficial effect on haemoglobin levels, except for the 12–24 months age-group, that conversely had reduced haemoglobin levels of − 2 g/L [95% CI − 3.3; − 0.7]. Female sex had a protective effect of 2 g/L [95% CI 1.3; 2.7]. The results for the remaining models of the nested series were appended to the Additional file 1: S1–S8.
Table 2.
Main household fixed-effect regression models of malaria status adjusted for sex and age
| Coefficients | Overall malaria modela | Stratified modelb | |
|---|---|---|---|
| Malaria effect on haemoglobin | |||
| Overall malaria status | |||
| Reference: negative | |||
| Malaria | Estimate | − 7.5 | |
| p-value | < 0.001 | ||
| CI 95 | (− 8.5; − 6.5) | ||
| Stratified malaria status | |||
| Reference: negative | |||
| Acute | − 7.7 | ||
| < 0.001 | |||
| (− 8.8; − 6.6) | |||
| Sub-microscopic | − 7.1 | ||
| < 0.001 | |||
| (− 8.3; − 5.9) | |||
| Age group | |||
| Reference:6–12 months | |||
| 13–24 months | − 2 | − 2 | |
| 0.002 | 0.002 | ||
| (− 3.3; − 0.7) | (− 3.3; − 0.7) | ||
| 25–36 months | 2.8 | 2.8 | |
| < 0.001 | < 0.001 | ||
| (1.5; 4.1) | (1.5; 4.1) | ||
| 37–48 months | 8.3 | 8.3 | |
| < 0.001 | < 0.001 | ||
| (7.1; 9.4) | (7.1; 9.4) | ||
| 49–50 months | 13.2 | 13.3 | |
| < 0.001 | < 0.001 | ||
| (12.1; 14.4) | (12.1; 14.5) | ||
| Sex | |||
| Reference: male | |||
| Female | 0.2 | 0.2 | |
| < 0.001 | < 0.001 | ||
| (0.13; 0.27) | (0.13; 0.27) | ||
CI confidence interval
aLinear regression of all malaria positive cases on haemoglobin
bLinear regression of acute and sub-microscopic malaria cases on haemoglobin
The overall effect of all positive malaria tests is − 7.5 g/L (overall malaria model). Children with acute malaria have − 7.7 g/L less haemoglobin when compared to the healthy population. The prolonged effect after infection is − 7.1 g/L when compared to the healthy population (stratified model)
The in-sample predictions from the overall malaria model indicate a 92.5% prevalence of anaemia among malaria positive children, compared to 77.9% among malaria negative children. The absolute difference was largest for moderate or severe anaemia (Hb < 90 g/L; malaria positives: 51.5%, malaria negatives: 24.6%) and the relative difference was largest for severe anaemia (Hb < 70 g/L; malaria positives: 9.4%, malaria negatives: 2.2%). The results from the predictions are illustrated in Fig. 3.
Fig. 3.
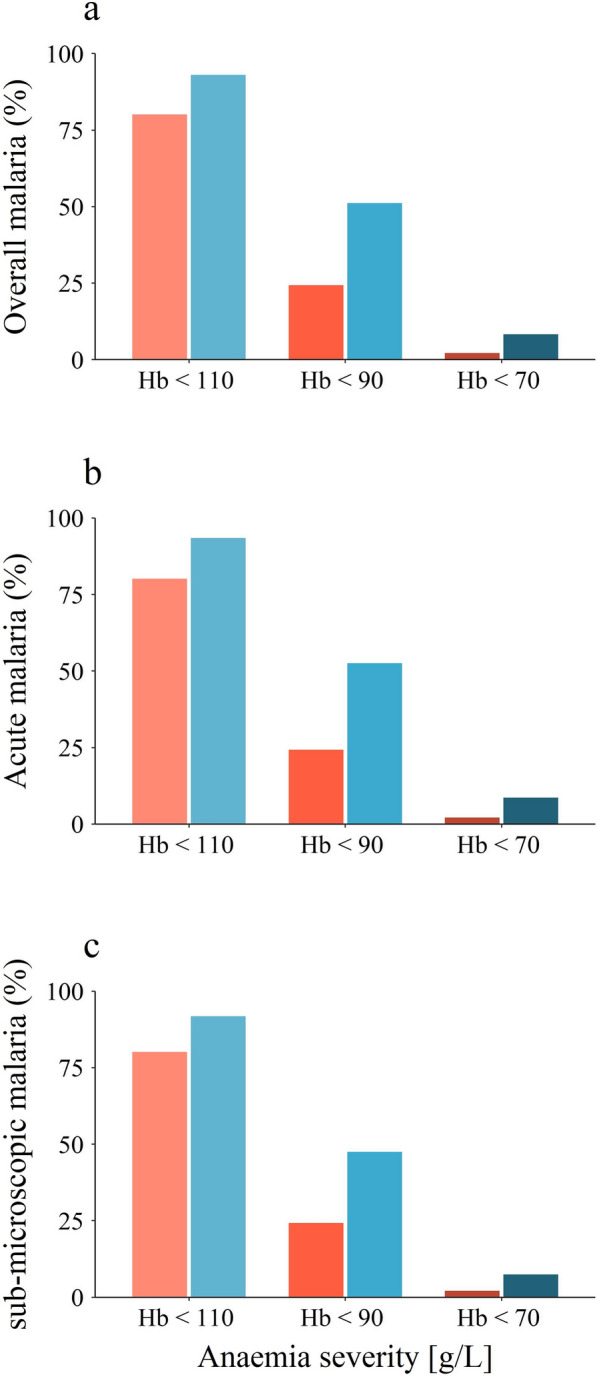
Predicted prevalence of any, moderate or worse and severe anaemia by malaria status. In-sample predicted prevalence of any anaemia (Hb < 110 g/L), moderate or worse anaemia (Hb < 90 g/L) and severe anaemia (Hb < 70 g/L) by malaria status for all malaria positive cases (a), acute cases (b) and sub-microscopic cases (c). Eliminating malaria from the study population would substantially reduce the total prevalence of malaria, moderate anaemia and almost eliminate severe anaemia. The stratification by malaria status affected the results only marginally. Red shades (lighter colours, left bars) indicate malaria negative cases and blue shades (darker colours, right bars) malaria positive cases
The random effects models showed generally larger effects for the acute and prolonged effects (Additional file 1: S9–S15) but remained consistent with the results of the main fixed-effect models. The larger effects are attributable to the reduced control for confounding on the household level due to the random effect assumption and are thus likely the result of bias, which is eliminated in the household fixed-effect analysis. Similarly, the subset analysis for male participants (Additional file 1: S16–S18) and female participants (Additional file 1: S19–S21), seasonality (Additional file 1: S22, S23) and survey (Additional file 1: S24–S26) remained consistent with the main outcomes.
Discussion
Both malaria prevalence (44% in the pooled data) and anaemia prevalence (83% in the pooled data) were high among young children in Burkina Faso between 2010 and 2018. This study estimated a malaria-attributable haemoglobin decrease of − 7.7 g/L during acute infection and of − 7.1 g/L in the time post-infection. Older children had higher haemoglobin levels than younger children and female sex improved haemoglobin levels by 2 g/L.
The malaria-induced haemoglobin changes can have large clinical implications. For instance, it has been shown that an increase of 10 g/L haemoglobin is associated with a 0.78 relative risk of mental retardation in young children [34]. This implies that a malaria-attributable haemoglobin reduction as shown in the data might pose substantial threat of cognitive development disorders in affected children. Especially the predictions of anaemia prevalence illustrate the severity of the burden of malarial anaemia in Burkina Faso and the analyses indicate that most cases of severe anaemia and a sizeable portion of moderate anaemia could be avoided if malaria were successfully eliminated.
Several studies have previously reported on the malaria-associated decrease in haemoglobin concentrations in clinical and national settings using different analytic methods [35–37]. The age group and sex dependent variation in haemoglobin values, as observed in this study, have been described previously in a similar fashion but especially the differences by sex might warrant further research [38].
This study is unique in that it could quantify the strong association between malaria and anaemia at the population-level, using a household fixed-effect approach controlling for all confounding that is constant within a given household. Furthermore, it is representative not only in its sampling design, but also in its seasonal composition, given that surveys were conducted on- and off malaria season. Finally, this study is based on a very large and nationally representative sample of 17,599 children and thus offers enough power to inspire confidence in its results as they are consistent even in the reduced subset analyses.
This study is influenced by several limitations. Firstly, a large number of children had a positive rapid test, but no corresponding positive microscopy test result. Thick smear microscopy is considered the gold standard but has varying sensitivity (from 55 to 98%) and specificity (from 81% to > 98%), depending on the experience of the diagnostician and the slide quality [39–41]. To rule out malaria it is required to repeat the microscopy test over the course of several days, which has not been done in the surveys and thus likely results in an underestimation of the malaria prevalence in this study [32]. RDTs on the other hand produce a comparatively high rate of false positives where Plasmodium antigens are present on the microscopically undetectable gametocytes, even when the disease itself is controlled by the immune system or medical treatment and parasitaemia is below the detection threshold. This can cause microscopy-negative cases to show RDT positive results for up to thirty days even after parasite elimination and clinical remission [30, 33]. The statistical model leveraged this effect to create a quasi-longitudinal perspective, where positive RDTs with negative microscopy results represent children who are currently recovering from malaria. Biologically, this prolonged effect might be a mix of several contributing factors, such as persistent bone-marrow suppression, delayed haemolysis, delayed recovery and false-negative microscopy tests [42].
A second limitation is the way in which the pooled cross-sectional data reflects the patterns of malaria and changes between survey years in Burkina Faso. Since several years and seasons of surveys were pooled for the analysis, the study population is not representative of any malaria point-prevalence in Burkina Faso and thus the data neither reflects malarias seasonal pattern, nor does it reflect progress made in the fight against malaria between 2010 and 2018. It is, however, still comparable to the extremes of anaemia burden and malaria transmission intensity found in West African countries [2, 43, 44].
Thirdly, the fixed-effect method itself also comes with a caveat. It controls for all confounders above the household level but lacks control for the within household confounders, particularly anaemia risk factors that vary between children in a household. These risk factors include nutritional (e.g., iron deficiency) and genetical traits (e.g., sickle-cell anaemia), other infectious diseases (e.g., helminths) and other, frequently interacted factors [45–47]. The modelling approach assumes that these unmeasured confounders are reasonably similar for all children within the household.
Conclusions
In summary, this study proposes a strong estimate of the population-wide effect of malaria on haemoglobin among young children in Burkina Faso, a setting marked by high malaria burden and extremely high anaemia prevalence. The findings of this study shed light on the acute and prolonged effects of infection and the potential gains against severe anaemia by eliminating malaria. Hopefully, these effects will soon be diminished by effective, accessible and affordable malaria control strategies. The household fixed-effects analysis has proven to be a suitable design to quantify these effects in a quasi-experimental setup and makes it possible to draw strong conclusions. Further research should attempt to clarify how genetic relationship and other factors contribute to the risk of acquiring malaria infection and decreased haemoglobin levels. There is a large knowledge gap on the longitudinal change in haemoglobin levels during an acute malaria infection.
Supplementary Information
Additional file 1. Online only supplement. Additional information, explanations and results published only only (S1–S30).
Acknowledgements
We would like to thank ICF and DHS for providing the data. Our special thanks are owed to the thousands of Burkinabe that participated in the extensive surveys and the field workers that collected the data.
Abbreviations
- DHS
Demographic and health surveys
- Hb
Haemoglobin
- MIS
Malaria indicator surveys
- RDT
Rapid diagnostic test
- SSA
Sub-Saharan Africa
Authors’ contributions
TB and TS designed the study. TS, CB, and TB performed the data analysis. TS and CB drafted the manuscript. All co-authors contributed significantly to the revision of the manuscript and provided scientific guidance. All authors read and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Availability of data and materials
All data is available from the DHS website (https://dhsprogram.com/). Codes will be made available upon request.
Declarations
Ethics approval and consent to participate
Not applicable. Since we used only anonymized and untraceable data, this study did not require ethical review from our home institution (EKHD).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. Prevalence of anaemia in children under 5 years (%). Geneva, World Health Organization, 2020. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/prevalence-of-anaemia-in-children-under-5-years-(-). Accessed 03 Mar 2021.
- 2.WHO. World malaria report 2020: 20 years of global progress and challenges. Geneva: World Health Organization, 2020. https://www.who.int/publications/i/item/9789240015791. Accessed 03 Mar 2021.
- 3.Sachs J, Malaney P. The economic and social burden of malaria. Nature. 2002;415:680–685. doi: 10.1038/415680a. [DOI] [PubMed] [Google Scholar]
- 4.The World Bank. Burkina Faso. 2020 [cited 03 Mar 2021]. In: Macro poverty outlook: sub-Saharan Africa. The World Bank Washington DC; [208 - 9]. https://pubdocs.worldbank.org/en/720441492455091991/mpo-ssa.pdf. Accessed 03 Mar 2021.
- 5.Datoo MS, Natama MH, Somé A, Traoré O, Rouamba T, Bellamy D, et al. Efficacy of a low-dose candidate malaria vaccine, R21 in adjuvant Matrix-M, with seasonal administration to children in Burkina Faso: a randomised controlled trial. Lancet. 2021;397:1809–1818. doi: 10.1016/S0140-6736(21)00943-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phillips MA, Burrows JN, Manyando C, van Huijsduijnen RH, Van Voorhis WC, Wells TNC. Malaria. Nat Rev Dis Primers. 2017;3:17050. doi: 10.1038/nrdp.2017.50. [DOI] [PubMed] [Google Scholar]
- 7.White NJ. Anaemia and malaria. Malar J. 2018;17:371. doi: 10.1186/s12936-018-2509-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ekvall H. Malaria and anemia. Cur Opin Hematol. 2003;10:108–114. doi: 10.1097/00062752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Hedberg K, Hightower A, Shaffer N, Paluku KM, Lyamba B, Davachi F, et al. Plasmodium falciparum-associated anemia in children at a large urban hospital in Zaire. Am J Trop Med Hyg. 1993;48:365–371. doi: 10.4269/ajtmh.1993.48.365. [DOI] [PubMed] [Google Scholar]
- 10.Balarajan Y, Ramakrishnan U, Özaltin E, Shankar AH, Subramanian SV. Anaemia in low-income and middle-income countries. Lancet. 2011;378:2123–2135. doi: 10.1016/S0140-6736(10)62304-5. [DOI] [PubMed] [Google Scholar]
- 11.Yang F, Liu X, Zha P. Trends in socioeconomic inequalities and prevalence of anemia among children and nonpregnant women in low- and middle-income countries. JAMA Netw Open. 2018;1:e182899. doi: 10.1001/jamanetworkopen.2018.2899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Plessow R, Arora NK, Brunner B, Tzogiou C, Eichler K, Brügger U, et al. Social costs of iron deficiency anemia in 6–59-month-old children in India. PLoS ONE. 2015;10:e0136581. doi: 10.1371/journal.pone.0136581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tusting LS, Willey B, Lucas H, Thompson J, Kafy HT, Smith R, et al. Socioeconomic development as an intervention against malaria: a systematic review and meta-analysis. Lancet. 2013;382:963–972. doi: 10.1016/S0140-6736(13)60851-X. [DOI] [PubMed] [Google Scholar]
- 14.Holding PA, Snow RW. Impact of Plasmodium falciparum malaria on performance and learning: review of the evidence. Am J Trop Med Hyg. 2001;64:68–75. doi: 10.4269/ajtmh.2001.64.68. [DOI] [PubMed] [Google Scholar]
- 15.Kotepui M, Piwkham D, PhunPhuech B, Phiwklam N, Chupeerach C, Duangmano S. Effects of malaria parasite density on blood cell parameters. PLoS ONE. 2015;10:e-121–57. doi: 10.1371/journal.pone.0121057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Premji Z, Hamisi Y, Shiff C, Minjas J, Lubega P, Makwaya C. Anaemia and Plasmodium falciparum infections among young children in an holoendemic area, Bagamoyo, Tanzania. Acta Trop. 1995;59:55–64. doi: 10.1016/0001-706x(94)00079-g. [DOI] [PubMed] [Google Scholar]
- 17.Ekvall H, Premji Z, Bennett S, Bjorkman A. Hemoglobin concentration in children in a malaria holoendemic area is determined by cumulated Plasmodium falciparum parasite densities. Am J Trop Med Hyg. 2001;64:58–66. doi: 10.4269/ajtmh.2001.64.58. [DOI] [PubMed] [Google Scholar]
- 18.McElroy PD, Ter Kuile FO, Lal AA, Bloland PB, Hawley WA, Oloo AJ, et al. Effect of Plasmodium falciparum parasitemia density on hemoglobin concentrations among full-term, normal birth weight children in western Kenya, IV. The Asembo Bay Cohort Project. Am J Trop Med Hyg. 2000;62:504–512. doi: 10.4269/ajtmh.2000.62.504. [DOI] [PubMed] [Google Scholar]
- 19.Menendez C, Fleming AF, Alonso PL. Malaria-related anaemia. Parasitol Today. 2000;16:469–476. doi: 10.1016/s0169-4758(00)01774-9. [DOI] [PubMed] [Google Scholar]
- 20.Means RT. The anaemia of infection. Bailliere's Best Pract Res Clin Haematol. 2000;13:151–162. doi: 10.1053/beha.1999.0065. [DOI] [PubMed] [Google Scholar]
- 21.Calis JCJ, Phiri KS, Faragher EB, Brabin BJ, Bates I, Cuevas LE, et al. Severe anemia in Malawian children. Malawi Med J. 2016;28:99–107. [PMC free article] [PubMed] [Google Scholar]
- 22.Barnighausen T, Oldenburg C, Tugwell P, Bommer C, Ebert C, Barreto M, et al. Quasi-experimental study designs series-paper 7: assessing the assumptions. J Clin Epidemiol. 2017;89:53–66. doi: 10.1016/j.jclinepi.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 23.Gunasekara FI, Richardson K, Carter K, Blakely T. Fixed effects analysis of repeated measures data. Int J Epidemiol. 2014;43:264–269. doi: 10.1093/ije/dyt221. [DOI] [PubMed] [Google Scholar]
- 24.Anekwe TD, Newell ML, Tanser F, Pillay D, Barnighausen T. The causal effect of childhood measles vaccination on educational attainment: a mother fixed-effects study in rural South Africa. Vaccine. 2015;33:5020–5026. doi: 10.1016/j.vaccine.2015.04.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGovern ME, Herbst K, Tanser F, Mutevedzi T, Canning D, Gareta D, et al. Do gifts increase consent to home-based HIV testing? A difference-in-differences study in rural KwaZulu-Natal, South Africa. Int J Epidemiol. 2016;45:2100–2109. doi: 10.1093/ije/dyw122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ouédraogo M, Rouamba T, Samadoulougou S, Kirakoya-Samadoulougou F. Effect of free healthcare policy for children under five years old on the incidence of reported malaria cases in Burkina Faso by bayesian modelling: “Not only the ears but also the head of the hippopotamus”. Int J Environ Res Public Health. 2020;17:417. doi: 10.3390/ijerph17020417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rouamba T, Nakanabo-Diallo S, Derra K, Rouamba E, Kazienga A, Inoue Y, et al. Socioeconomic and environmental factors associated with malaria hotspots in the Nanoro demographic surveillance area. Burkina Faso BMC Public Health. 2019;19:249. doi: 10.1186/s12889-019-6565-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ouedraogo B, Inoue Y, Kambiré A, Sallah K, Dieng S, Tine R, et al. Spatio-temporal dynamic of malaria in Ouagadougou, Burkina Faso, 2011–2015. Malar J. 2018;17:138. doi: 10.1186/s12936-018-2280-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva, World Health Organization, 2011. http://www.who.int/vmnis/indicators/haemoglobin.pdf. Accessed 03 Mar 2021.
- 30.Dalrymple U, Arambepola R, Gething PW, Cameron E. How long do rapid diagnostic tests remain positive after anti-malarial treatment? Malar J. 2018;17:228. doi: 10.1186/s12936-018-2371-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mathison BA, Pritt BS. Update on malaria diagnostics and test utilization. J Clin Microbiol. 2017;55:2009–2017. doi: 10.1128/JCM.02562-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ashley EA, Pyae Phyo A, Woodrow CJ. Malaria. Lancet. 2018;391:1608–1621. doi: 10.1016/S0140-6736(18)30324-6. [DOI] [PubMed] [Google Scholar]
- 33.Ndour PA, Larréché S, Mouri O, Argy N, Gay F, Roussel C, et al. Measuring the Plasmodium falciparum HRP2 protein in blood from artesunate-treated malaria patients predicts post-artesunate delayed hemolysis. Sci Transl Med. 2017;9:eaaf9377. doi: 10.1126/scitranslmed.aaf9377. [DOI] [PubMed] [Google Scholar]
- 34.Stoltzfus RJ, Mullany L, Black RE. Iron deficiency anemia. In: Ezzati M, Lopez AD, Rodgers AA, Murray CJL, editors. Comparative quantification of health risks : global and regional burden of disease attributable to selected major risk factors. Geneva: World Health Organization; 2004. pp. 163–210. [Google Scholar]
- 35.Kotepui M, Phunphuech B, Phiwklam N, Chupeerach C, Duangmano S. Effect of malarial infection on haematological parameters in population near Thailand-Myanmar border. Malar J. 2014;13:218. doi: 10.1186/1475-2875-13-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bickerton Blackburn CR. Observations on the development of resistance to vivax malaria. Trans R Soc Trop Med Hyg. 1948;42:117–162. [Google Scholar]
- 37.Fanello C, Onyamboko M, Lee SJ, Woodrow C, Setaphan S, Chotivanich K, et al. Post-treatment haemolysis in African children with hyperparasitaemic falciparum malaria; a randomized comparison of artesunate and quinine. BMC Infect Dis. 2017;17:575. doi: 10.1186/s12879-017-2678-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fulgoni VL, 3rd, Agarwal S, Kellogg MD, Lieberman HR. Establishing pediatric and adult RBC reference intervals with NHANES data using piecewise regression. Am J Clin Pathol. 2019;151:128–142. doi: 10.1093/ajcp/aqy116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berzosa P, de Lucio A, Romay-Barja M, Herrador Z, González V, García L, et al. Comparison of three diagnostic methods (microscopy, RDT, and PCR) for the detection of malaria parasites in representative samples from Equatorial Guinea. Malar J. 2018;17:333. doi: 10.1186/s12936-018-2481-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rodulfo H, De Donato M, Mora R, González L, Contreras CE. Comparison of the diagnosis of malaria by microscopy, immunochromatography and PCR in endemic areas of Venezuela. Brazilian J Med Biol Res. 2007;40:535–543. doi: 10.1590/s0100-879x2007000400012. [DOI] [PubMed] [Google Scholar]
- 41.Wangai LN, Karau MG, Njiruh PN, Sabah O, Kimani FT, Magoma G, et al. Sensitivity of microscopy compared to molecular diagnosis of P. falciparum: implications on malaria treatment in epidemic areas in Kenya. Afr J Infect Dis. 2011;5:1–6. doi: 10.4314/ajid.v5i1.66504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Helleberg M, Goka BQ, Akanmori BD, Obeng-Adjei G, Rodriques O, Kurtzhals JAL. Bone marrow suppression and severe anaemia associated with persistent Plasmodium falciparum infection in African children with microscopically undetectable parasitaemia. Malar J. 2005;4:56. doi: 10.1186/1475-2875-4-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Assele V, Ndoh GE, Nkoghe D, Fandeur T. No evidence of decline in malaria burden from 2006 to 2013 in a rural province of Gabon: implications for public health policy. BMC Public Health. 2015;15:81. doi: 10.1186/s12889-015-1456-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ouédraogo A, Tiono AB, Diarra A, Sanon S, Yaro JB, Ouedraogo E, et al. Malaria morbidity in high and seasonal malaria transmission area of Burkina Faso. PLoS ONE. 2013;8:e50036. doi: 10.1371/journal.pone.0050036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Elguero E, Delicat-Loembet LM, Rougeron V, Arnathau C, Roche B, Becquart P, et al. Malaria continues to select for sickle cell trait in Central Africa. Proc Natl Acad Sci USA. 2015;112:7051–7054. doi: 10.1073/pnas.1505665112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Taylor SM, Parobek CM, Fairhurst RM. Haemoglobinopathies and the clinical epidemiology of malaria: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:457–468. doi: 10.1016/S1473-3099(12)70055-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Petry N, Olofin I, Hurrell RF, Boy E, Wirth JP, Moursi M, et al. The proportion of anemia associated with iron deficiency in low, medium, and high human development index countries: a systematic analysis of national surveys. Nutrients. 2016;8:693. doi: 10.3390/nu8110693. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Online only supplement. Additional information, explanations and results published only only (S1–S30).
Data Availability Statement
All data is available from the DHS website (https://dhsprogram.com/). Codes will be made available upon request.