Abstract
Background:
High risk blood transfusions can cause a lot of financial and psychological burden to the community. The prevalence of Hepatitis B is useful for evaluating the blood products’ safety and donor selection methods. We aimed to predict the prevalence of hepatitis B in Iranian blood donors from 2000–2016.
Methods:
Positive cases of hepatitis B from 2006 to 2014 were collected from Iranian Blood Transfusion Organization. This database was classified according to the age, provinces, and type of donation. Data was not existed in all subnational levels and all years, therefore, for predicting the hepatitis B prevalence, two separate, Spatio-temporal and mixed model (GLMM) were developed.
Results:
At the national level, the hepatitis B prevalence declined from 0.69 (0.51 to 0.90) in 2000 to 0.27 (0.21 to 0.33) in 2016. In first-time, regular, and repeated donors, this prevalence declined from 2.31 (1.74 to 2.31), 0.26 (0.19 to 0.34), and 0.51 (0.38 to 0.68) in 2000 to 0.87 (0.69 to 1.09), 0.09 (0.07 to 0.12), and 0.19 (0.14 to 0.24) in 2016. At the provincial level, the highest and lowest prevalence in 2016 was observed in North Khorasan and Gilan. With increasing age, the average prevalence of hepatitis B, increased.
Conclusion:
Prevalence of hepatitis B in Iranian blood donors has been reduced significantly over 17 years, but still new cases of hepatitis B are reported. By precise monitoring the donor selection process and implementing more sensitive laboratory screening, we can reduce the risk of new infectious agents.
Keywords: Hepatitis B, Prevalence, Blood donors
Introduction
High risk and unhealthy blood transfusions can lead to the transmission of blood-borne infections (1). Healthy blood transfusions, affect the lives of the patient and also the people who communicate with the patients (2). It will also cause a lot of financial and psychological burden on the community. The health of blood and blood products depends on the health status of the blood donors, the prevalence of blood-borne diseases and the sensitivity of screening tests (3). Assessing the rate of blood-borne infections in donors helps us to evaluate the function of the blood-transfusion organization in maintaining the quality of healthy blood. In addition, this information can be used to assess the prevalence of the disease in blood donors and used to estimate the prevalence of hepatitis in the community (4, 5).
Africa and Asia have the largest HBV epidemics, globally. HBV prevalence among blood donors was reported 1.99% (95% CI: 1.84–2.14) and 1.62% (95% CI: 1.36–1.88) in the EMRO and Middle Eastern countries. The prevalence among blood donors in neighborhood countries were 5.05% in Yemen, 3.02% in Saudi Arabia, 2.84% in Pakistan, 1.68% in Turkey, 1.58% in Egypt, 0.67% in Iraq, and 0.58% in Iran(6).
The epidemiological prevalence of blood-borne diseases in the blood donor’s population is useful for evaluating the blood and blood products’ health, the effectiveness of donor selection methods and risk assessment with the transmission of transfusion-transmitted infections. Changes in the prevalence of infectious diseases during time can indicate a change in risk factors in the community (4, 5).
Therefore, we aimed to determine the spatiotemporal analysis of the prevalence of hepatitis B in blood donors to provide an image for evaluating the performance and future estimates of the prevalence in Iran.
Materials and Methods
The data of all HBV positive blood donors from 2006 to 2014 were collected from Iranian blood transfusion organization. The data of donors in these years were classified according to the age, region, and type of donation (First time, regular, repeated). First time donors means donor donated his/her blood for first time. Regular blood donor is a person who donate his /her blood three to four times per year. Repeated blood donor is a person who had at least on blood donation. We predict the prevalence of hepatitis B from 2000 to 2016 using following modeling.
Model development
The registered data did not exist in all provincial levels and all years, therefore, in predicting the prevalence of hepatitis B among donors, there will be inappropriate data for many provinces and years. In order to address the problem of lost data and estimation of the gaps, and uncertainty intervals, two separate statistical models of the Spatio-temporal and mixed-space model (GLMM) were developed. To perform GLMM, 1000 times simulation was done on points of data to minimize the uncertainty intervals. Then, the Autoregressive conditional parent (CAR) is used for the spatiotemporal random effects model. The points of data that are geographically neighboring are expected to be more linked than other points of data. This model “lend information” from nearby provinces to improve the estimation for missing values or a small number of observations. The simulation was also done 1000 times on spatiotemporal analysis model, and finally, one million simulated data were combined for final results (7–9).
Model Validity
The model’s validity was examined by cross-validity and investigating the distribution of the observed and predicted data by the plot. Over 90% of the crude data were distributed in the predicted uncertainty range. The correlation between fitted value and observed value was r= 0.85 and acceptable. Nearly 94% of the crude data were distributed in predicted uncertainty range (10).
All the analyses were performed with STATA software ver. 14.0 (Stata Corp, College Station, TX, USA) and for plots, we used R statistical software version 3.4.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Overall, the prevalence of hepatitis B declined from 0.69 (95% uncertainty, 0.51 to 0.90) in 2000 to 0.27 (95% uncertainty, 0.21 to 0.33) in 2016. Table 1 shows the prevalence of hepatitis B over the course of 17 years. By increasing age of blood donors, the overall prevalence of hepatitis B enlarged at national and provincial level (Table 2 and Fig. 1). The hepatitis B vaccination program have been established in Iran since 1994 and the prevalence of hepatitis B in blood donors were reduced in vaccinated cohort comparing to unvaccinated cohort but it was not statistically significant (Table 2).
Table 1:
Prevalence of Hepatitis B in Blood donors
| National | Total |
|---|---|
| 2000 | 0.69(0.51–0.90) |
| 2001 | 0.65(0.49–0.83) |
| 2002 | 0.61(0.47–0.78) |
| 2003 | 0.57(0.45–0.72) |
| 2004 | 0.54(0.43–0.68) |
| 2005 | 0.51(0.41–0.63) |
| 2006 | 0.64(0.52–0.78) |
| 2007 | 0.55(0.45–0.67) |
| 2008 | 0.46(0.38–0.56) |
| 2009 | 0.41(0.34–0.50) |
| 2010 | 0.37(0.30–0.44) |
| 2011 | 0.31(0.25–0.38) |
| 2012 | 0.28(0.23–0.34) |
| 2013 | 0.25(0.20–0.31) |
| 2014 | 0.30(0.24–0.37) |
| 2015 | 0.28(0.22–0.35) |
| 2016 | 0.27(0.21–0.33) |
Table 2:
Hepatitis B Prevalence in 2016 by Age at National Level
| Age group (yr) | Hepatitis B prevalence |
|---|---|
| <20 | 0.15(0.12,0.19) |
| 21–25 | 0.17(0.13,0.21) |
| 26–30 | 0.17(0.13,0.21) |
| 31–35 | 0.2(0.16,0.25) |
| 36–40 | 0.24(0.19,0.3) |
| 41–45 | 0.3(0.24,0.38) |
| 46–50 | 0.37(0.29,0.46) |
| 51–55 | 0.53(0.42,0.66) |
| 56–60 | 0.77(0.61,0.96) |
| 61–65 | 1.23(0.95,1.56) |
Fig. 1:
Prevalence of Hepatitis B In 2000 And 2016 by Age And Type of Donation at the National Level
Prevalence of hepatitis B in First-time blood donors
In general, at the national level, the prevalence of hepatitis B in first-time donors declined 2.6 from 2.31 (95% uncertainty, 1.74 to 2.31) in 2000 to 0.87 (95% uncertainty, 0.69 to 1.09) in 2016 with a negative decrease of 9.73% (Table 3 and Fig. 2).
Table 3:
Hepatitis B Prevalence Among Blood Donors
| National /provincial | 2000 | 2016 | ||||
|---|---|---|---|---|---|---|
| First Time | Repeated | Regular | First Time | Repeated | Regular | |
| Markazi | 2.75(2.06,3.57) | 0.62(0.46,0.82) | 0.31(0.23,0.42) | 1.04(0.82,1.3) | 0.23(0.17,0.29) | 0.12(0.09,0.15) |
| Gilan | 1.17(0.87,1.56) | 0.26(0.19,0.35) | 0.13(0.09,0.18) | 0.44(0.33,0.56) | 0.09(0.07,0.12) | 0.05(0.04,0.06) |
| Mazandaran | 1.79(1.38,2.31) | 0.4(0.3,0.52) | 0.2(0.15,0.26) | 0.67(0.54,0.83) | 0.15(0.12,0.19) | 0.07(0.06,0.09) |
| Azarbaijan East | 2.93(2.23,3.77) | 0.66(0.49,0.86) | 0.33(0.25,0.44) | 1.11(0.88,1.38) | 0.24(0.19,0.31) | 0.12(0.09,0.16) |
| Azarbaijan West | 3.04(2.31,3.91) | 0.68(0.51,0.89) | 0.35(0.26,0.46) | 1.15(0.92,1.44) | 0.25(0.2,0.32) | 0.13(0.1,0.16) |
| Kermnshah | 2.47(1.84,3.23) | 0.55(0.4,0.73) | 0.28(0.2,0.37) | 0.93(0.73,1.18) | 0.2(0.16,0.26) | 0.1(0.08,0.13) |
| Khuzestan | 1.55(1.17,2.01) | 0.34(0.25,0.45) | 0.17(0.13,0.23) | 0.58(0.46,0.72) | 0.13(0.1,0.16) | 0.06(0.05,0.08) |
| Fars | 1.5(1.14,1.94) | 0.33(0.25,0.43) | 0.17(0.12,0.22) | 0.56(0.45,0.7) | 0.12(0.1,0.15) | 0.06(0.05,0.08) |
| Kerman | 2.59(1.98,3.34) | 0.58(0.44,0.76) | 0.29(0.22,0.39) | 0.98(0.78,1.21) | 0.21(0.17,0.27) | 0.11(0.08,0.14) |
| Khorasan Razavi | 1.98(1.5,2.54) | 0.44(0.33,0.57) | 0.22(0.16,0.29) | 0.74(0.6,0.91) | 0.16(0.13,0.21) | 0.08(0.06,0.1) |
| Isfahan | 1.4(1.05,1.83) | 0.31(0.23,0.41) | 0.15(0.11,0.21) | 0.52(0.41,0.65) | 0.11(0.09,0.14) | 0.06(0.04,0.07) |
| Sistan and Baluchestan | 4.87(3.76,6.15) | 1.13(0.85,1.45) | 0.57(0.43,0.75) | 1.9(1.53,2.33) | 0.42(0.33,0.53) | 0.21(0.17,0.27) |
| Kurdistan | 3.45(2.6,4.49) | 0.78(0.58,1.03) | 0.4(0.29,0.53) | 1.32(1.03,1.65) | 0.29(0.22,0.37) | 0.15(0.11,0.19) |
| Hamedan | 2.88(2.16,3.78) | 0.65(0.47,0.87) | 0.33(0.24,0.44) | 1.09(0.86,1.38) | 0.24(0.18,0.31) | 0.12(0.09,0.15) |
| Chaharmahal and Bakhtiari | 3.27(2.43,4.3) | 0.74(0.54,0.99) | 0.37(0.27,0.5) | 1.25(0.97,1.6) | 0.27(0.21,0.36) | 0.14(0.1,0.18) |
| Lorestn | 2.68(2.04,3.48) | 0.6(0.45,0.8) | 0.3(0.22,0.4) | 1.02(0.81,1.27) | 0.22(0.17,0.28) | 0.11(0.09,0.14) |
| Ilam | 3.67(2.69,4.9) | 0.84(0.59,1.14) | 0.42(0.3,0.58) | 1.41(1.06,1.83) | 0.31(0.23,0.41) | 0.16(0.11,0.21) |
| Kohgiluyeh and Boyer Ahmad | 2.6(1.91,3.44) | 0.58(0.41,0.79) | 0.29(0.21,0.4) | 0.98(0.75,1.27) | 0.22(0.16,0.28) | 0.11(0.08,0.14) |
| Bushehr | 2.1(1.54,2.82) | 0.47(0.33,0.64) | 0.23(0.17,0.32) | 0.79(0.6,1.03) | 0.17(0.13,0.23) | 0.09(0.06,0.12) |
| Zanjan | 3.1(2.29,4.08) | 0.7(0.5,0.94) | 0.35(0.26,0.48) | 1.18(0.9,1.52) | 0.26(0.19,0.34) | 0.13(0.1,0.17) |
| Semnan | 3.33(2.5,4.33) | 0.75(0.55,1.01) | 0.38(0.28,0.51) | 1.27(0.99,1.61) | 0.28(0.21,0.36) | 0.14(0.11,0.18) |
| Yazd | 2.11(1.57,2.79) | 0.47(0.34,0.63) | 0.24(0.17,0.32) | 0.8(0.61,1.02) | 0.17(0.13,0.23) | 0.09(0.07,0.12) |
| Hormozgan | 3.27(2.46,4.23) | 0.74(0.54,0.97) | 0.37(0.28,0.49) | 1.25(0.98,1.57) | 0.27(0.21,0.35) | 0.14(0.11,0.18) |
| Tehran | 1.38(1.06,1.76) | 0.3(0.23,0.39) | 0.15(0.12,0.2) | 0.51(0.42,0.62) | 0.11(0.09,0.14) | 0.06(0.04,0.07) |
| Ardabil | 4.4(3.34,5.63) | 1.01(0.75,1.33) | 0.51(0.38,0.68) | 1.7(1.34,2.13) | 0.38(0.29,0.48) | 0.19(0.14,0.24) |
| Qom | 3.2(2.37,4.21) | 0.72(0.52,0.97) | 0.36(0.26,0.5) | 1.22(0.94,1.56) | 0.27(0.2,0.35) | 0.13(0.1,0.18) |
| Qazvin | 2.43(1.77,3.26) | 0.54(0.39,0.74) | 0.27(0.19,0.38) | 0.92(0.69,1.2) | 0.2(0.15,0.27) | 0.1(0.07,0.13) |
| Golestan | 5.14(3.97,6.5) | 1.19(0.9,1.55) | 0.61(0.46,0.79) | 2(1.6,2.46) | 0.44(0.35,0.56) | 0.22(0.18,0.28) |
| Khorasan North | 5.37(4.08,6.91) | 1.25(0.92,1.68) | 0.64(0.46,0.85) | 2.1(1.64,2.64) | 0.47(0.35,0.6) | 0.24(0.18,0.31) |
| Khorasan South | 4.44(3.28,5.85) | 1.02(0.74,1.39) | 0.52(0.37,0.7) | 1.72(1.31,2.2) | 0.38(0.28,0.5) | 0.19(0.14,0.25) |
| Alborz | 2.46(1.65,3.57) | 0.55(0.36,0.81) | 0.28(0.18,0.41) | 0.93(0.66,1.28) | 0.2(0.14,0.29) | 0.1(0.07,0.14) |
| Iran | 2.31(1.75,2.31) | 0.51(0.38,0.68) | 0.26(0.19,0.35) | 0.88(0.69,1.1) | 0.19(0.15,0.25) | 0.09(0.07,0.12) |
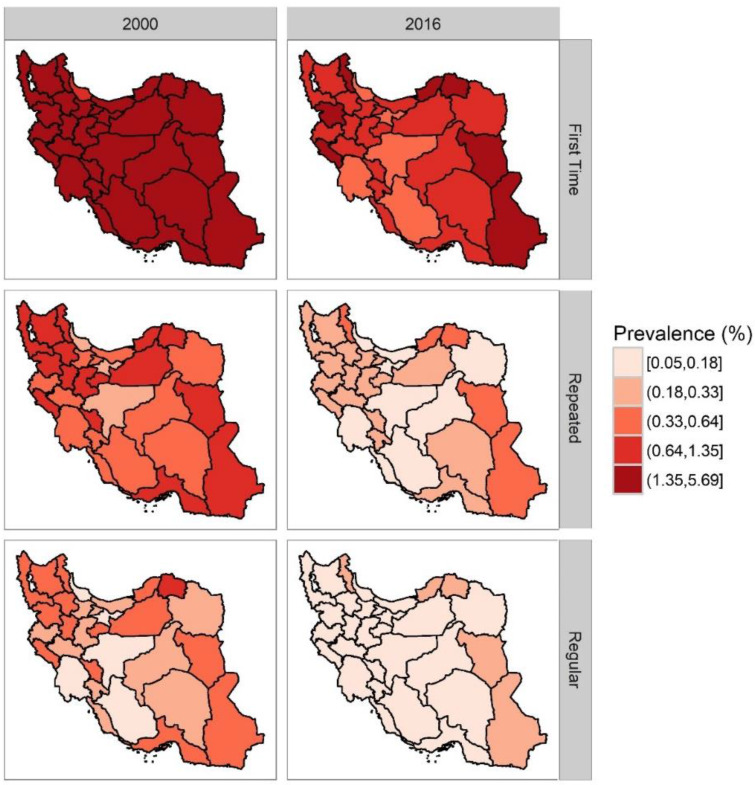
Fig 2:
Trend of Hepatitis B Prevalence In 2000 To 2016 by Type of Donation at the National Level
Overall, the mean prevalence of hepatitis B at the national level was increased from 0.34 (95% uncertainty, 0.26 to 0.43) in 15 to 20 yr age group, to 2.79% (95% uncertainty, 2.16 to 3.47) in 60–65 yr age group is in 2016 (Fig. 1).
In the province, the highest and lowest incidence of hepatitis B in 2016 was North Khorasan and Gilan with 2.09 (95% uncertainty between 1.06 and 2.06) and 0.43 (95% confidence intervals 0.33 to 0.56), respectively. The provinces with the highest prevalence are 4.8 times more prevalent than other provinces. During the 17 years of the study, the prevalence of hepatitis B in all provinces has declined dramatically (Table 3 and Fig. 3).
Fig 3:
Prevalence of Hepatitis B Changes at National and Provincial levels in 2000 and 2016
Overall, with an increase in age in 2016, the average prevalence of hepatitis B in all provinces increases. This trend has been the same for most of the provinces in recent years.
Prevalence of hepatitis B in regular blood donors
Generally, at the national level, the prevalence of hepatitis B in regular donors declined 2.8 times from 0.26 (95% uncertainty, 0.19 to 0.34) in 2000 to 0.09 (95% uncertainty, 0.07 to 0.12) in 2016 (Table 3 and Fig. 2).
In total, with increasing age, the average prevalence of hepatitis B at the national level was changed from 0.03 (95% uncertainty, 0.02–0.04) in 15 to 20 yr to 0.3 (95% uncertainty, 0.23 to 0.4%) in 60–65 yr in 2016 (Fig. 1).
At the provincial level, once more, the highest and lowest prevalence of hepatitis B in 2016 was North Khorasan and Gilan, with 0.23 (95% uncertainty between 0.17 and 0.30) and 0.04 (95% confidence interval 0.03 to 0.06). The provinces with the highest prevalence are 5.75 times more prevalent than the other provinces (Table 3 and Fig. 3).
The prevalence of hepatitis B in all provinces declined and enlarged with increasing age similar to first-time blood donors.
Prevalence of hepatitis B in repeated blood donors
At the national level, the prevalence of hepatitis B in repeated donors was declined 2.68 times from 0.51 (95% uncertainty, from 0.38 to 0.68) in 2000 to 0.19 (95% uncertainty, 0.14 to 0.24) in 2016 (Table 3 and Fig 2). With the increase in age, the mean prevalence of hepatitis B in the national level was 0.07 (95% uncertainty, 0.05–0.09) in 15 to 20 yr to 0.61% (95% uncertainty, 0.46 to 0.79) in 60 –65 yr in 2016 (Fig. 1).
North Khorasan and Gilan with 0.46 (95% uncertainty of 0.35 to 0.60) and 0.09 (95% confidence interval 0.07 to 0.12) respectively were the most prevalent provinces. The provinces with the highest prevalence are about 5.11 times more prevalent than other provinces. Age trend and year trend was similar to other types of blood donation (Table 3 and Fig. 3).
Discussion
There is a downward trend in the prevalence of hepatitis B at the national and provincial level of Iran from 2000 to 2016. This pattern is similar in first time and regular and repeated blood donors. The prevalence is lower in regular blood donors compared to first-time blood donors’. Furthermore, the prevalence is increased with increasing age in all time periods and regions.
The prevalence of hepatitis B was from 0.1% to 0.5% in American and Western Europeans to 5% and 15% in Asia and China (11). In Canada, the prevalence of hepatitis B in regular blood donors was reported 0.007% in 2006 (12). The prevalence of hepatitis B among donors is 3.13% in 2000–2005 (13). In Thailand, the prevalence of hepatitis B among donors decreased from 7% in 1998 to 2.6% in 2009 (14). The evaluation of HBs Ag infection was high in East Mediterranean and Middle Eastern countries with a prevalence of 0.58% among blood donors. The prevalence is higher in Yemen and Djibouti than East Mediterranean and Middle Eastern countries, by up to 5.05% and 10.4%, respectively. The high prevalence in these countries could be on account of low public awareness in general population (15), unsafe blood donation and transfusion (16), and high prevalence of HBV in the general population (17). In contrast, the prevalence of hepatitis B among iranian blood donors based on this study is lower than those in East Mediterranean and Middle Eastern countries and is similar to low risk countries.
A recent report from blood donors indicates that the prevalence of hepatitis B in the blood donors decreased from 1.79% in 1998 to 0.41% in 2007 (18). This was 0.25% in Tehran (4). The prevalence of hepatitis B among blood donors was reported at 0.38% in 2014 (4). These estimates are similar to estimates in the recent study in the same period of time (0.30). From 1996 to 2014, approximately 30 studies have been published from Iran, with a sample size ranging from 478 to 14599783 people, and the prevalence of hepatitis B had been reported to be 2.5% to 0.1% in Iran. The qualities of all articles were not good and it could be as a result of variable sources. One of the major problems is the data was not gathered for research purpose. This demonstrates the need for more extensive studies based on full and original data on this issue (19). Overall, based on a recent meta-analysis on the prevalence of hepatitis B in donors, the prevalence has decreased in blood donors, which is similar to the findings of this study. Between 1996 and 2008, the prevalence was 0.7% (19). Another study reported a decrease in the prevalence of hepatitis B among Iranian blood donors for 0.8% from 2000 to 2008 (6).
The lower prevalence of hepatitis B in Iranian blood donors compare to East Mediterranean and Middle Eastern countries can be as a result of effective screening and selection of appropriate donors, and the effectiveness of HBV vaccination program and coverage (4, 20). In Fars, the prevalence dropped from 0.4 to 0.3 in 2012. In Bushehr, in 2005–2006, the prevalence reduced from 0.3 to 0.2. In Qazvin, in 2001, the prevalence decrease from 1 to 0.4 percent. In Gilan, Mazandaran, Golestan, and Semnan, the prevalence was more than the average population (0.7%) (19). The results of this study showed a similar trend at the provincial level in the mentioned years. Also, the hepatitis B prevalence was lower in regular blood donors compared to first-time blood donors confirmed by other studies (18, 21).
Therefore, policymakers can decide on the basis of the existing process to maintain and attract the donor with a higher sensitivity. Based on the recommendations of WHO to reduce the risk of hepatitis following transfusion (PTH), all donated units and their products should be screened for HBsAg using ELISA (22). Despite the adoption of accurate advanced screening methods, and implementation of these methods by blood transfusion centers in different countries, still, cases of hepatitis after transfusion are reported (23). According to the results of this study, it is not eliminated in Iranian blood donors, as well. Although blood transfusion is considered an effective treatment for very anemic patients, trauma and surgical problems, the risk of potential viral and bacterial infections following transfusion exists. The precise donor selection and screening with sensitive tests for pathogens can greatly reduce the risk of infectious agents (3, 24). Blood transfusion centers have developed educational programs and screening methods aimed at reducing the risk of transmission of transfusion-related viral infections. Other efforts are also being undertaken to properly select and monitor the behavior of donors.
The limitation of the recent study was the lack of data by age over 17 yr in 30 provinces. The data gathered before 2006 were not digitally recorded in all provinces so were not reliable. However, the strength of this study was to predict hepatitis B prevalence among blood donors for 10 age group, 30 provinces, and national level, and 17 years using advanced statistical methods filled all data gaps and elucidate the pattern and trends of blood donor’s hepatitis B for policymakers. It is recommended to do future studies on sex pattern in all provinces to have a complete illustrate of Hepatitis B prevalence in Iranian blood donors.
Conclusion
Prevalence of hepatitis B in Iranian blood has been donors reduced significantly over 17 years, but still hepatitis B in blood donors are reported. The precise monitoring of donor selection process and the laboratory screening of donated blood with sensitive tests can reduce the risk of infectious agents.
Acknowledgements
Authors would like to thank all the collaborators on this project in Iranian Blood Transfusion Organization and the Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, and Iran University of Medical Sciences. No funding was received for this study.
Footnotes
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, redundancy, etc.) have been completely observed by the authors.
Conflict of interest
The authors declare that there is no conflict of interests.
References
- 1.Bennett JE, Dolin R, Blaser MJ. (2014). Principles and practice of infectious diseases. ed. Elsevier Health Sciences. [Google Scholar]
- 2.Buseri FI, Muhibi MA, Jeremiah ZA. (2009). Sero-epidemiology of transfusion-transmissible infectious diseases among blood donors in Osogbo, south-west Nigeria. Blood Transfus, 7(4):293–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.La Torre G, Saulle R. (2016). Risk factors from HBV infection among blood donors: A systematic review. Asian Pacific J Trop Biomed, 6:344–349. [Google Scholar]
- 4.Pourfathollah AA. (2014). Changes in frequency of HBV, HCV, HIV and syphilis infections among blood donors in Tehran province 2005–2011. Arch Iran Med, 17(9):613–20. [PubMed] [Google Scholar]
- 5.Bhawani Y, Rao PR, Sudhakar V. (2010). Seroprevalence of transfusion transmissible infections among blood donors in a tertiary care hospital of Andhra Pradesh. Biol Med, 2:45–48. [Google Scholar]
- 6.Babanejad M, Izadi N, Najafi F, Alavian SM. (2016). The HBsAg Prevalence among blood donors from Eastern Mediterranean and Middle Eastern countries: a systematic review and meta-Analysis. Hepat Mon, 16 (3): e35664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohammadi Y, Parsaeian M, Farzadfar F, Kasaeian A, Mehdipour P, Sheidaei A, Mansouri A, Moghaddam SS, Djalalinia S, Mahmoudi M. (2014). Levels and trends of child and adult mortality rates in the Islamic Republic of Iran, 1990–2013; protocol of the NASBOD study. Arch Iran Med, 17 (3):176–81. [PubMed] [Google Scholar]
- 8.Peykari N, Ghajarieh Sepanlou S, Djalalinia S, Kasaeian A, Parsaeian M, Ahmadvand A, Koohpayehzadeh J, Damari B, Jamshidi HR, Larijani B, Farzadfar F. (2014). National and Sub-national Prevalence, Trend, and Burden of Metabolic Risk Factors (MRFs) in Iran: 1990 – 2013, Study Protocol. Arch Iran Med, 17(1):54–61. [PubMed] [Google Scholar]
- 9.Ashrafi E, Mohammadi S-F, Fotouhi A, Lashay A, Asadi-lari M, Mahdavi A, Jabbarvand M, Sobhani S, Farzadfar F. (2014). National and Sub-national Burden of Visual Impairment in Iran1990–2013; Study Protocol. Arch Iran Med, 17(12):810–5. [PubMed] [Google Scholar]
- 10.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY. (2012). Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet, 380:2095–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Busch M. (2000). HIV, HBV and HCV: new developments related to transfusion safety. Vox sang, 78 Suppl 2:253–256. [PubMed] [Google Scholar]
- 12.O’Brien SF, Xi G, Fan W, Yi QL, Fearon MA, Scalia V, Goldman M. (2008). Epidemiology of hepatitis B in Canadian blood donors. Transfusion, 48(11):2323–2330. [DOI] [PubMed] [Google Scholar]
- 13.Bajubair MA, Elrub AA, Bather G. (2008). Hepatic viral infections in Yemen between 2000--2005. Saudi Med J, 29(6):871–874. [PubMed] [Google Scholar]
- 14.Phikulsod S, Oota S, Tirawatnapong T, Sakuldamrongpanich T, Chalermchan W, Louisirirotchanakul S, Tanprasert S, Chongkolwatana V, Kitpoka P, Phanuphak P. (2009). One‐year experience of nucleic acid technology testing for human immunodeficiency virus Type 1, hepatitis C virus, and hepatitis B virus in Thai blood donations. Transfusion, 49(6):1126–1135. [DOI] [PubMed] [Google Scholar]
- 15.Manzoor I, Hashmi N, Daud S, Ajmal S, Fatima H, Rasheed Z, Syed S. (2009). Seroprevalence of transfusion transmissible infections (TTIS) in blood donors. Biomedica, 25:154–8. [Google Scholar]
- 16.Ali SA, Donahue RM, Qureshi H, Vermund SH. (2009). Hepatitis B and hepatitis C in Pakistan: prevalence and risk factors. Int J Infec Dis, 13(1):9–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Redwan N, Ahmed M, Barnawi M. (2012). Prevalence study of Hepatitis B virus (HBV) infection by serological techniques in Jeddah, Saudi Arabia. Life Sci J, 9:5442–8. [Google Scholar]
- 18.Amini Kafi‐abad S, Rezvan H, Abolghasemi H, Talebian A. (2009). Prevalence and trends of human immunodeficiency virus, hepatitis B virus, and hepatitis C virus among blood donors in Iran, 2004 through 2007. Transfusion, 49(10):2214–2220. [DOI] [PubMed] [Google Scholar]
- 19.Sajad Alizadeh IP, Sayehmiri Kouresh, Pakzad Reza, Darvishi Parisa. (2014). Prevalence of Hepatitis B among Blood Donors in Iran: A Systematic Review and Meta-analysis. Asian J. Biol. Sci., 7:35–46. [Google Scholar]
- 20.Mirrezaie SM, Saber HR, Hajibeigi B, Salekmoghaddam E, Abbasian A, Alavian SM. (2014). Impact of HBV vaccination on prevalence of hepatitis B virus infection among volunteer blood donors in Tehran-Iran. Shiraz E-Medical Journal, 15.
- 21.Porolajal J, Majdzadeh R. (2009). Prevalence of chronic Hepatitis B infection in Iran. Iranian Journal of Epidemiology, 4:1–8. [PMC free article] [PubMed] [Google Scholar]
- 22.WHO (2017). Guidelines on hepatitis b and c testing.:36–44. https://apps.who.int/iris/bitstream/handle/10665/254621/9789241549981-eng.pdf
- 23.Candotti D, Allain J-P. (2009). Transfusion-transmitted hepatitis B virus infection. J Hepatol, 51(4):798–809. [DOI] [PubMed] [Google Scholar]
- 24.Rezaei N, Amini‐Kafiabad S, Maghsudlu M, Abolghasemi H. (2016). Risk factor analysis of hepatitis C virus seropositivity in Iranian blood donors: a case‐control study. Transfusion, 56(7):1891–1898. [DOI] [PubMed] [Google Scholar]