Dear Editor-in-Chief
Having been detected first in December 2019 in Wuhan, China, COVID-19 has infected more than 209 million people and killed 4,393,512 ones worldwide until August 17, 2021 (1). The disease, which was called pandemic on March 11, 2020 (2), has had significant social and economic effects around the world. Ecological data show that the pandemic has had a significantly higher prevalence and death in more developed and higher income countries so far (3). In this regard, using data related to COVID-19 from World meter (1) and per capita income from World Bank data bases until November 29, 2020, I analyzed the issue. Distribution of COVID-19 death and prevalence between high income countries and others, and regression of the prevalence and deaths from COVID-19 on the countries’ per capita income are performed.
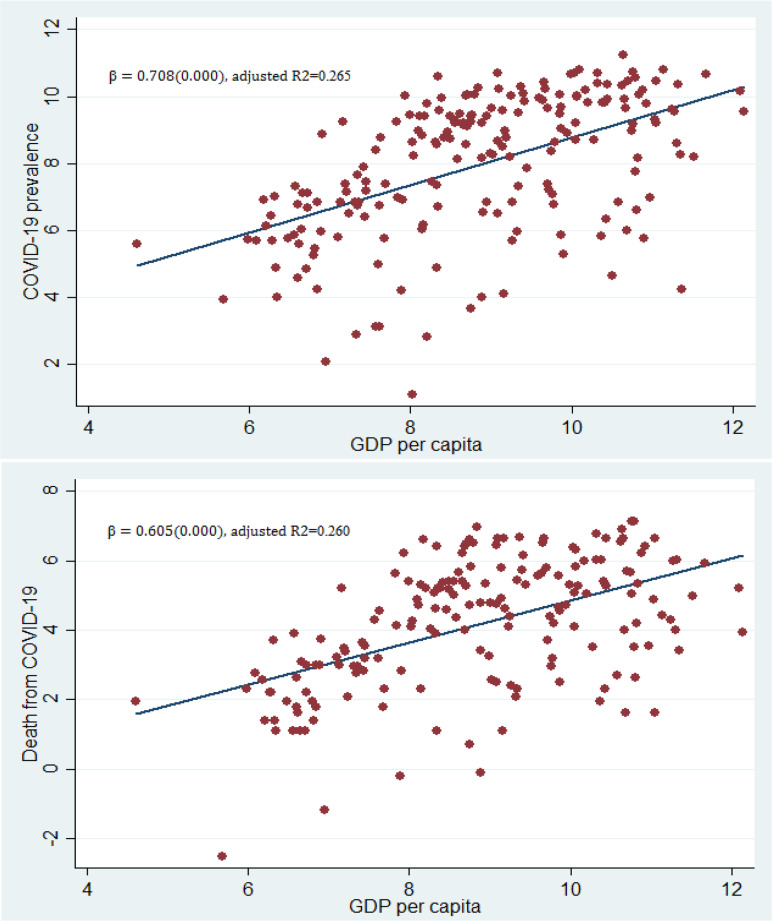
According to the statistical analysis by the author, the prevalence of COVID-19 in high income countries is three time higher than other countries (17371 vs. 6180 per 1 million population). There is also similar status for critical cases and death related COVID-19 (Table 1). Moreover, according to a simple regression estimates, the prevalence and deaths from COVID-19 are significantly related to countries’ per capita income (Fig. 1).
Table 1:
Comparison of some COVID-19 indicators between high income countries and others*
| Comparison indicators | High income countries *** | Other countries |
|---|---|---|
| Prevalence** | 17371.56 | 6180.01 |
| Death** | 289.68 | 147.33 |
| Test** | 401758.46 | 71841.31 |
| Critical cases** | 47.46 | 15.81 |
| GDP per capita (USD) | 43797.13 | 4186.27 |
Distribution of COVID-19 death and prevalence between high income countries and others are reported based on author’s statistical analysis.
Per 1 million population in November 29, 2020
Countries with a GNI per capita of $12,696 or more (according to the word bank: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups)
Fig. 1:
Regression line of COVID-19 prevalence and death rates (per 1 million population) on GDP per capita (current USD)*
In the regression model, which is analyzed by the author, data of COVID-19 mortality and morbidity, and GDP per capita were collected from Worldometer (1) and World Bank data bases, respectively. Moreover, axes are in logarithmic scale
It is so important to assert that the assumption of higher reported COVID-19 prevalence and death rates in higher income countries is according to the only author’s statistical analysis (until November 29, 2020) which is elaborated above. So current letter and the following debates are according to the author’s assumption.
To answer the question why more developed countries are facing a much higher prevalence and death rates than poor countries, the following possibilities are suggested:
-More developed countries usually have older populations (4), and as noted by researchers, age is a key risk factor for spreading and dying from COVID-19 (5). Thus, developed countries are more prone to the outbreak of the disease and its outcomes. According to the United Nations (2017), about 20–25% of the population in Europe and North America are over 60 year old, while the rate is about 5% in Africa and below 15% in other countries (4).
-Having underlying diseases such as diabetes, cardiovascular disease, and other chronic diseases was one the most important risk factors for the COVID-19 especially its severe state and the resulting death (5, 6). There are much more of these risk factors in high-income countries than in other ones. For example, according to the latest Global Burden of Disease statistics (2017), the prevalence (per 100,000 population) of cardiovascular diseases in the countries with high, upper middle, lower middle, and low income was 11075, 7284, 4438 and 3198, respectively. Similarly, the prevalence of diabetes in high, upper middle, lower middle, and low income countries was 9097, 6567, 5414 and 3578 (per 100,000 population), respectively (7).
-In high-income countries where there are more resources and better medical infrastructures (a larger number of more specialized human resources, and greater and more developed medical technology, especially laboratory equipment and diagnostic kits), a much larger number of COVID-19 diagnosis test are performed (1). Consequently, the number of detected cases and deaths is larger. Having weak infrastructures, some poor countries are not able to even address routine population health needs (8).
-There is much lower air transport and passengers in poor countries than in developed ones (9). Therefore, the transmission of the virus from the early places like China, East Asia, and then Europe and the United States, to the poor countries has been less likely.
-Countries with the highest prevalence of COVID-19 (mainly developed countries) are likely to disseminate the data more transparently and more accurately. Williams showed that information transparency had a positive relationship with countries’ income levels (10).
-Finally, other factors such as environmental situation, geographical conditions, socio-demographic factors, and even economic factors may play a role in the spread of the disease, which require to be carefully studied.
In general, it seems that the more risk factors of the disease (age, underlying diseases, etc.), diagnostic tests, air transport, and information transparency in high-income countries lead to the higher prevalence and deaths from COVID-19 compared to lower-income countries.
Footnotes
Conflict of interest
The authors declare that there is no conflict of interests.
References
- 1.Worldometers.info (2020) Worldometer, Dover, Delaware, U.S.A. https://www.worldometers.info/coronavirus/
- 2.WorldHealthOrganization (2020). https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 3.Cifuentes-Faura J. (2021). COVID-19 Mortality Rate and Its Incidence in Latin America: Dependence on Demographic and Economic Variables. Int J Environ Res Public Health, 18 (13):6900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nations U. (2017). World Population Ageing 2017-Highlights. Department of Economic and Social Affairs. https://populationmatters.org/population-numbers?gclid=EAIaIQobChMIkcrk9N3E8gIVCp53Ch2UDwEqEAAYASAAEgKfBvD_BwE
- 5.Wu Z, McGoogan JM. (2020). Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Jama, 323 (13):1239–42. [DOI] [PubMed] [Google Scholar]
- 6.Khan MMA, Khan MN, Mustagir MG, Rana J, Islam MS, Kabir MI. (2020). Effects of underlying morbidities on the occurrence of deaths in COVID-19 patients: A systematic review and meta-analysis. J Glob Health, 10(2): 020503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute for Health Metrics and Evaluation (2020). GBD Results Tool. University of Washington, USA. [Google Scholar]
- 8.Mills A. (2014). Health care systems in low-and middle-income countries. N Engl J Med, 370:552–557. [DOI] [PubMed] [Google Scholar]
- 9.International Civil Aviation Organization (2020). The World Bank. Air transport, passengers carried. https://data.worldbank.org/indicator/IS.AIR.PSGR
- 10.Williams A. (2015). A global index of information transparency and accountability. J Comp Econ, 43:804–824. [Google Scholar]