Abstract
Background
Seasonal influenza vaccination is highly recommended for healthcare workers (HCWs) every year to protect them and reduce the risk of disease transmission at workplaces. Relatively few studies addressed influenza vaccination in the Eastern Mediterranean Region.
Objectives
The main objective of this study was to explore the attitudes, beliefs and practice of Egyptian HCWs towards seasonal influenza vaccine.
Methods
This is a nationwide cross‐sectional study. Data were collected through self‐administered structured questionnaire. A sample of 3534 HCWs (physicians and nurses) was collected from different levels of healthcare facilities.
Results
The proportion of seasonal influenza vaccine uptake during the last season was 30.7% while the percentage of ever vaccinated was 46.8%. The most identified reason for non‐compliance was lack of trust about vaccine efficacy and its adverse events. Around 80% of participants expressed positive attitude towards influenza vaccine and the vast majority (98%) agreed to uptake the vaccine during pandemic. There was significant positive association between attitude score and influenza vaccine uptake. Raising awareness about vaccine and ensuring vaccine availability were the main suggestions by HCWs to improve vaccine uptake.
Conclusions
Although there was positive attitude towards influenza vaccine, yet vaccination coverage was suboptimal particularly among those working in university hospitals. Educational messages and operational strategies addressing motivators and barriers that emerged from this study are needed to optimize vaccine uptake.
Keywords: attitude, belief, cross sectional study, Egypt, healthcare workers, influenza vaccination, practice
1. INTRODUCTION
Globally, annual influenza vaccination rates among healthcare workers (HCWs) are almost low despite recommendations from WHO and national public health institutions of many countries. 1
Unvaccinated HCWs are an important source of nosocomial influenza. Transmission of influenza virus from patients to HCWs, from HCWs to patients and among HCWs has been well documented. 2 , 3 The possible consequences of infected HCWs include increased morbidity and mortality among patients at risk of contracting influenza and a high rate of sickness absenteeism among HCWs themselves resulting in shortage of staff, additional burden on the health system and reduce the healthcare quality. 4 , 5
Influenza vaccination is the most effective strategy for the prevention of influenza virus infection and the potentially severe complications. The World Health Organization (WHO) and the Advisory Committee on Immunization Practices (ACIP) recommend that HCWs should be vaccinated annually against influenza. It is also recommended that healthcare organizations implement policies and procedures to encourage HCWs vaccination. 3 Ahmed and colleagues found that vaccination of HCWs significantly reduced influenza‐like illness and all‐cause mortality among patients. 5
Relatively, few studies addressed influenza vaccination in the Eastern Mediterranean Region. 6 In a study among HCWs in three Middle East countries, the vaccination rate was 24.7%, 67.2% and 46.4% in United Arab Emirates, Kuwait and Oman, respectively. Moreover, the different variables associated with the non‐compliance of HCWs to the annual influenza vaccination were lack of time (31.8%) followed by unawareness of vaccine availability (29.4%), unavailability of vaccine (25.4%), doubts about vaccine efficacy (24.9%), lack of information about importance (20.1%) and concerns about its side effects (17.3%). 7
Recent WHO Strategic Advisory Group of Experts (SAGE) on Immunization for influenza vaccination recommended HCWs as one of the highest priority groups for receipt of influenza vaccines during the current COVID‐19 pandemic. 8
To our knowledge, this is the first study among HCWs in Egypt tackling influenza vaccination. The purpose of the present nationwide study is to explore attitudes, beliefs and practice of HCWs in Egypt regarding seasonal influenza vaccination. The ultimate goal is to gather data to plan future interventions and policies aiming at increasing influenza vaccination coverage among Egyptian HCWs.
2. METHODOLOGY
2.1. Study settings
A nationwide cross‐sectional study was conducted between June and October 2019 in 11 governorates representing different country regions. From Middle region, both Cairo and Giza governorates were selected purposively as they include all types of healthcare services and large number of HCWs. From South region, three governorates were randomly selected: Fayoum, Menia and Assiut. From North region, 5 governorates were randomly selected: Qalyoubia, Gharbia, Menoufia, Sharkia and Alexandria while one governorate was selected from Suez Canal zone (Port Saied).
From each selected governorate, the capital city was purposively included to ensure the representation of all healthcare service levels provided by MOHP, in addition to the university hospitals.
2.2. Study participants
Physicians and nurses of the selected healthcare facilities were asked to participate in the study. Many specialties were included in the study particularly those working in Intensive Care Units (ICU), Neonatal Intensive Care Units (NICU), chest hospitals and fever hospitals. Also, HCWs in the departments of internal medicine, paediatrics and primary health care were represented in the sample. Eligible subjects were physicians and nurses providing health care to patients, while those with no or minimal contact with patients and those with less than 1‐year in‐job experience were excluded.
2.3. Sample size determination
Sample size was calculated using influenza vaccine uptake of 28.2% as estimated in Eastern Mediterranean regions, 6 using 95% confidence level and 5% margin error. During calculation, we considered the average number of HCWs (physicians and nurses) per governorate = 12 000. Accordingly, the sample size required was 303 HCWs. As the study was conducted in 11 governorates, the total sample size required was =303 × 11 = 3333 HCWs. Using an estimated response rate of 90%, the required sample increased to 3703. Sample size was calculated by the software program Epi Info version 7.0 for Windows. CDC ‐ Atlanta, USA. 9
2.4. Study tool
A structured self‐administered questionnaire was designed to be distributed to target study subjects at their workplaces. The questionnaire included selected socio‐demographics information, in addition to questions on HCWs beliefs, attitudes and practice regarding seasonal influenza vaccination.
Healthcare workers beliefs were assessed using questions on who is mostly in need of influenza vaccine, measures taken in case of exposure to influenza patient, beliefs of vaccine effectiveness and safety, and vaccine acceptability. While the attitude questions were developed using 5 points Likert scale to assess HCWs attitude towards influenza infection severity and complications, having concerns of getting the infection or transmitting influenza to their families, importance of and planning to have the vaccine next season and the need for providing the vaccine free of charge.
Practice questions included ever having influenza vaccine and being vaccinated last season and reasons for getting or rejecting uptake of influenza vaccine.
The tool was piloted and revised based on the answers of 60 HCWs (30 physicians and 30 nurses). Reliability and validity of the tool were assessed by experts in public health and epidemiology before distribution (Cronbach's Alpha was 0.83). Data collectors and field supervisors were trained before starting field visits to healthcare facilities.
2.5. Data management and statistical analysis
The data were reviewed for completeness and consistency. Double data entry was performed using Microsoft Excel 2010. The statistical analysis included descriptive statistics as frequency, percentage, odds ratio (OR) and their 95% CI. Attitude questions were analysed using a Likert scoring system of 1‐5, attitude was considered positive if scores were (>75%) of total scores, neutral between (60 and 75%) and negative if scores are (< 60%) of total scores.
For bivariate analysis, statistical comparisons were performed using Pearson's Chi‐square test. Thereafter, univariate and multivariable logistic regression models were applied to identify the predictor variables associated with influenza vaccination uptake during last season. The level of significance was set at P < .05. Statistical analyses were performed using the Statistical Package for the Social Sciences (IBM‐SPSS) version 21.0 (IBM Corporation).
3. RESULTS
Of 3710 HCWs asked to participate, 3534 responded and filled the questionnaire (response rate = 95.3%) including 1745 were physicians (49.4%). Two thirds of respondents were females, and 71.5% were less than 40 years old. Around 70% of HCWs were affiliated to MOHP healthcare facilities while the rest were working in university hospitals. Table 1 illustrates the demographic characteristics of the study participants.
TABLE 1.
Socio‐demographic characteristics of study participants (n = 3534)
| Characteristics | Category | Frequency | Percentage |
|---|---|---|---|
| Age groups (years) | <30 years | 1189 | 33.6 |
| 30‐39 | 1341 | 37.9 | |
| 40‐49 | 653 | 18.5 | |
| ≥50 | 351 | 9.9 | |
| Gender | Males | 1186 | 33.6 |
| Females | 2348 | 66.4 | |
| Occupation | Doctor | 1745 | 49.4 |
| Nurse | 1789 | 50.6 | |
| Education | Secondary (nurses) | 1378 | 39.0 |
| University (bachelor) | 1182 | 33.4 | |
| Post University | 974 | 27.6 | |
| Type of facility | MOHP (general and district hospitals) | 859 | 24.3 |
| MOHP‐ Chest hospitals | 1078 | 30.5 | |
| MOHP‐ Fever and infectious diseases hospitals | 177 | 5.0 | |
| MOHP ‐ PHCs | 351 | 9.9 | |
| University hospitals | 1069 | 30.2 | |
| Work experience (in years) | 1‐5 | 1171 | 33.1 |
| 6‐10 | 783 | 22.2 | |
| 11‐20 | 967 | 27.4 | |
| >20 | 613 | 17.3 | |
| Specialty | Chest | 1140 | 32.2 |
| Internal medicine | 824 | 23.3 | |
| Intensive care | 465 | 13.1 | |
| Paediatrics | 447 | 12.6 | |
| General practitioner | 341 | 9.6 | |
| Tropical and infectious diseases | 190 | 5.4 | |
| Others (lab, radiology) | 127 | 3.6 | |
| Tobacco smoking | Non‐smokers | 3247 | 91.9 |
| Current smokers | 184 | 5.2 | |
| Ex‐smokers | 103 | 2.9 | |
| Chronic illness (any) | Yes | 716 | 20.3 |
| No | 2818 | 79.3 |
3.1. Vaccination status
Of 3534 respondents, 1653 (46.8%) reported having influenza vaccine at least one time, 342/1653 (20.7%) mentioned they had it once and around 40% gave history of 2 to 4 times uptake of the vaccine (Table 2).
TABLE 2.
Seasonal influenza vaccination uptake by HCWs and their confidence level towards influenza vaccine
| Category | No. | Percentage | |
|---|---|---|---|
| Ever vaccinated before | Yes | 1653 | 46.8 |
| No | 1881 | 53.2 | |
| No. of times of vaccinations before (n = 1653) | Once | 342 | 20.7 |
| 2‐4 | 663 | 40.1 | |
| ≥5 | 227 | 13.8 | |
| Don't remember | 421 | 25.4 | |
| Vaccination during last season | Yes | 1085 | 30.7 |
| No | 2449 | 69.3 |
Among those who had ever been vaccinated, the main reasons for vaccination were as follows: vaccine is effective and safe (70.2%), it prevents influenza (34.1%), is free of charge (30.6%) and HCWs are at risk of getting influenza infection (25.0%) (Figure 1).
FIGURE 1.
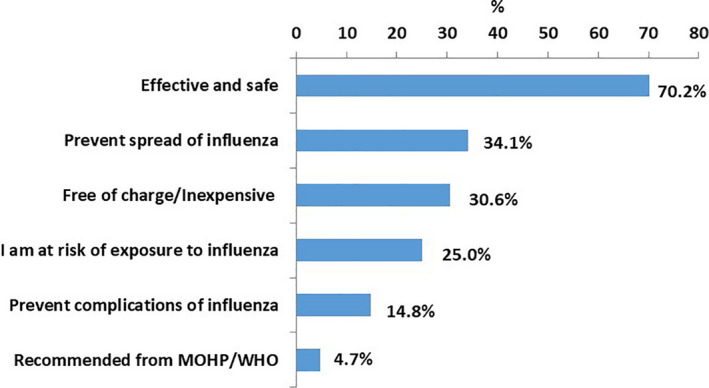
Main reasons of getting the influenza vaccine
While among those who did not get the vaccine during the last season, the main reasons not to get vaccinated were as follows: vaccine is ineffective (28.5%), it causes complications and adverse events (25.1%), and vaccine expenses (18.9%) (Figure 2).
FIGURE 2.
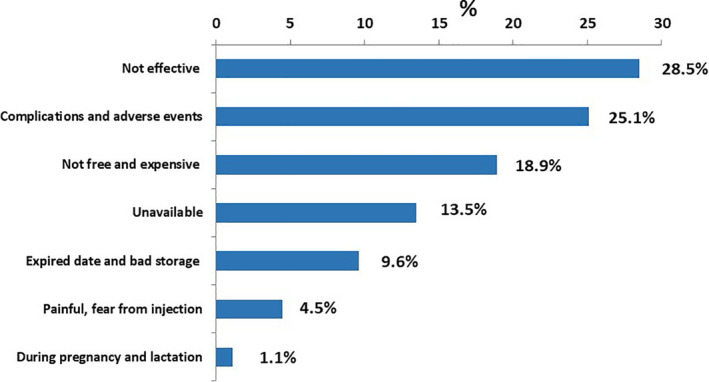
Reasons for rejecting uptake of influenza vaccine among HCWs
3.2. HCWs beliefs and attitude towards influenza vaccination
Although 1292 (36.6%) think that the vaccine is effective in prevention of the disease, yet 2891 (81.8%) agreed to have the vaccine if available and free of charge, and 3463 (98.0%) agree to be vaccinated during pandemics (Table 3). The recommended groups to be vaccinated identified by participants included HCWs (82.2%) elderly people (77.5%), patients with chronic illnesses (68.9%), while only 49.3% identified pregnant women as a target group for influenza vaccination (Table 3). Of all respondents, 84.4% believed that the most effective measure for influenza prevention is frequent hand washing (84.4%) followed by avoid touching eyes, nose and mouth (84.1%) while 73.3% mentioned vaccine as the most effective measure (Table 3).
TABLE 3.
HCWs beliefs towards Seasonal influenza vaccination
| Question | Correct answer | |
|---|---|---|
| No. | % | |
| Vaccination is especially important for | ||
| Healthcare workers | 2905 | 82.2 |
| Elderly | 2739 | 77.7 |
| Pregnant women | 1742 | 49.3 |
| Children aged 6‐59 months | 2400 | 67.9 |
| Individuals with specific chronic medical conditions | 2435 | 68.9 |
| Influenza vaccine is effective and safe | 1292 | 36.6 |
| Most effective measures for influenza prevention at healthcare settings | ||
| Vaccination | 2591 | 73.3 |
| Frequent hand washing | 2999 | 84.9 |
| Avoid touching eyes, nose and mouth | 2973 | 84.1 |
| Avoid direct contact with patients whenever possible | 2822 | 79.9 |
| Wear face mask when in contact with patient | 2820 | 79.8 |
| Vaccination acceptability | No. | % |
| I agree to take the vaccine if available at workplace and free of charge | 2891 | 81.8 |
| I agree to take the vaccine during pandemics | 3463 | 98.0 |
Most of the participants (85.2%) understand that HCWs are at higher risk of getting influenza during work, and most of them realize that it is important to have the vaccine to protect themselves, prevent disease transmission to their patients and families (88.6%, 91.5% and 93.0%, respectively) (Figure 3). Almost half of participants (42.8%) think that influenza is a mild disease and around 28.2% believe that influenza does not cause a lot of serious illness. Most of participants recommend that the vaccination for influenza should be mandatory for HCWs in Egypt and free of charge (79.9% and 91.6%, respectively) and 76.2% are planning to get the vaccine next season. Results showed that 2,823 (79.8%) of HCWs had positive attitude towards influenza vaccination, 635 (18.0%) had neutral attitude and only 76 (2.2%) are having negative attitude (Figure 3).
FIGURE 3.
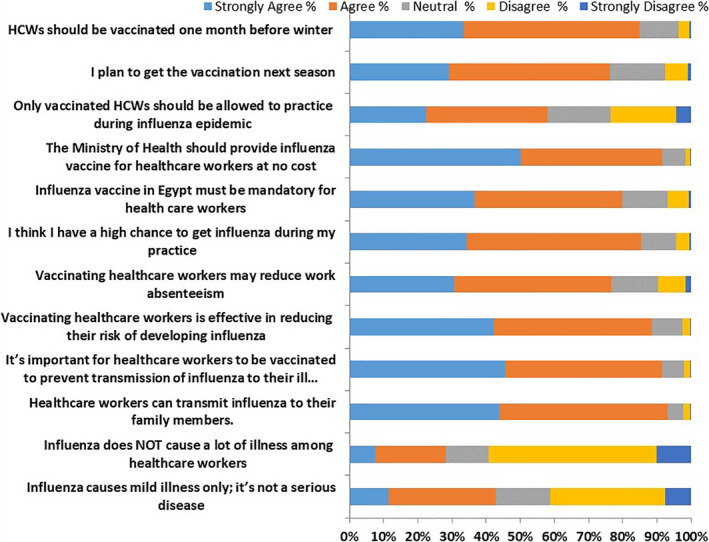
Attitudes of HCWs towards seasonal influenza vaccination
3.3. Predictors of influenza vaccination in HCWs
Overall, 1085 (30.7%) had been vaccinated in the last season (Table 2). Socio‐demographic factors associated with vaccine uptake during the last season revealed that vaccination rate was significantly higher in participants older than 30 years of age, in females, nurses who had secondary school education, working for MOHP health facilities, chest and infectious diseases hospitals, having experience >5 years and specialized HCWs (P values <.001) (Table 4).
TABLE 4.
Association of socio‐demographic characteristics with vaccine uptake in the last season
| Category | Total | Vaccine uptake No. (%) | Unadjusted OR (95% CI)# | P value | |
|---|---|---|---|---|---|
| Age groups (years) | <30 years® | 1189 | 189 (15.9) | – | <.001 |
| 30‐39 | 1341 | 433 (32.3) | 2.52 (2.08‐3.06) | ||
| 40‐49 | 653 | 278 (42.6) | 3.92 (3.15‐4.89) | ||
| ≥50 | 351 | 185 (52.7) | 5.90 (4.54‐7.65) | ||
| Gender | Males® | 1186 | 326 (27.5) | – | .003 |
| Females | 2348 | 759 (32.3) | 1.26 (1.08‐1.47) | ||
| Occupation | Doctor® | 1745 | 465 (26.6) | – | <.001 |
| Nurse | 1789 | 620 (34.7) | 1.46 (1.29‐1.69) | ||
| Education | University grade® | 1189 | 226 (19.0) | – | <.001 |
| Post‐graduate | 974 | 336 (34.5) | 2.44 (1.84‐2.73) | ||
| Secondary nursing school | 1371 | 528 (38.1) | 2.69 (2.23‐3.20) | ||
| Type of facility | University hospitals® | 1069 | 77 (7.2) | – | <.001 |
| General and district hospitals$ | 859 | 263 (30.6) | 5.69 (4.33‐7.47) | ||
| Chest hospitals$ | 1078 | 603 (55.9) | 16.36 (12.60‐21.24) | ||
| Infectious diseases hospitals$ | 177 | 98 (55.4) | 15.98 (10.97‐23.28) | ||
| Primary healthcare units$ | 351 | 44 (12.5) | 1.85 (1.25‐2.73) | ||
| Work experience (years) | 1‐5® | 1171 | 139 (11.9) | – | <.001 |
| 6‐10 | 783 | 237 (30.3) | 3.22 (2.55‐4.07) | ||
| 11‐20 | 967 | 425 (44.0) | 5.82 (4.68‐7.24) | ||
| >20 | 613 | 284 (46.3) | 6.41 (5.05‐8.13) | ||
| Specialty | Intensive care | 465 | 133 (28.6) | 4.23 (2.21‐8.09) | <.001 |
| Chest | 1140 | 610 (53.5) | 12.14 (6.47‐22.77) | ||
| Tropical and infectious diseases | 190 | 72 (37.9) | 6.44 (3.25‐12.76) | ||
| Internal medicine | 824 | 137 (16.6) | 2.10 (1.10‐4.01) | ||
| Paediatrics | 447 | 82 (19.3) | 2.37 (1.22‐4.60) | ||
| Family physicians | 341 | 40 (11.7) | 1.40 (0.70‐2.82) | ||
| Others (lab/dermatology/radio‐diagnosis/surgery/)® | 127 | 11 (8.7) | – | ||
| Tobacco smoking | Non‐smokers | 3247 | 1000 (30.8) | 1.32 (0.84‐2.07) | .445 |
| Current smokers | 184 | 59 (32.1) | 1.40 (0.81‐2.40) | ||
| Ex‐smokers® | 103 | 26 (25.2) | – |
$ = MOHP, ® = Reference group, # = Using univariate logistic regression.
There was a significant positive association between attitudes score and influenza vaccine uptake. HCWs with positive attitudes score were 6.39 times more likely to be vaccinated compared to HCWs with negative score (P < .001). Also, HCWs who expressed confidence towards influenza vaccine efficacy were more likely to be vaccinated than non‐confident HCWs (OR = 5.49, 95% CI = 4.29‐7.03). HCWs who suffered from any chronic diseases were more likely to uptake the influenza vaccine (OR = 1.55, 95% CI = 1.30‐1.84) than HCWs with no past history of chronic illnesses (Table 5).
TABLE 5.
Univariate logistic regression of attitude score, confidence towards influenza vaccine efficacy and history of chronic illnesses with vaccination uptake in the last season
| Category | Total | Vaccine uptake no. (%) | Unadjusted OR (95% CI)# | P value | |
|---|---|---|---|---|---|
| Attitude score | Negative® | 76 | 6 (7.9) | – | <.001 |
| Neutral | 635 | 80 (12.6) | 1.68 (0.71‐4.00) | ||
| Positive | 2823 | 999 (35.4) | 6.39 (2.77‐14.76) | ||
| Confident towards vaccine efficacy | Not confident® | 615 | 95 (15.0) | – | <.001 |
| Neutral | 1627 | 358 (22.0) | 1.60 (1.25‐2.06) | ||
| Confident | 1292 | 635 (49.1) | 5.49 (4.29‐7.03) | ||
| Chronic Illness (any chronic illness) | No® | 2818 | 2008 (71.3) | – | <.001 |
| Yes | 716 | 441 (61.6) | 1.55 (1.30‐1.84) | ||
| Hypertension | No® | 3127 | 903 (28.9) | – | <.001 |
| Yes | 407 | 182 (44.7) | 1.99 (1.62‐2.46) | ||
| Diabetes Mellitus | No® | 3284 | 977 (29.8) | – | <.001 |
| Yes | 250 | 108 (43.2) | 1.80 (1.38‐2.33) | ||
| Heart Diseases | No® | 3440 | 1049 (30.5) | – | .106 |
| Yes | 94 | 36 (38.3) | 1.42 (0.93‐2.16) | ||
| Other chronic diseases (eg renal, COPD etc) | No® | 3305 | 1009 (30.5) | – | .339 |
| Yes | 229 | 76 (33.2) | 1.13 (0.85‐1.50) |
#: using univariate logistic regression, ® = Reference group.
The variables that remained significant after performing multivariate logistic regression included nurses who had secondary school education, working at MOHP healthcare facilities, confidence in influenza vaccine effectiveness and safety, positive attitude towards vaccination, work experience >5 years and specialized HCWs (Table 6).
TABLE 6.
Multivariate logistic regression of socio‐demographic, job characteristics and behavioural factors with vaccination uptake in the last season
| Factor | Category | Adjusted OR (95% CI)# | P value |
|---|---|---|---|
| Education | University® | – | |
| Post university | 1.07 (0.81‐1.41) | .651 | |
| Secondary nursing school | 1.50 (1.10‐2.04) | .011 | |
| Type of facility | University hospitals® | – | |
| General and district hospitals$ | 5.07 (3.76‐6.85) | <.001 | |
| Chest hospitals$ | 7.70 (5.74‐10.32) | <.001 | |
| Infectious diseases hospitals$ | 9.91 (6.30‐15.61) | <.001 | |
| Primary healthcare centre$ | 2.52 (1.36‐4.65) | .003 | |
| Specialty | Others® | – | |
| Intensive care | 5.96 (2.96‐12.00) | <.001 | |
| Chest | 6.55 (3.341‐12.84) | <.001 | |
| Tropical & infectious diseases | 3.40 (1.57‐7.36) | .002 | |
| Internal medicine | 3.00 (1.52‐5.93) | .002 | |
| Paediatrics | 2.26 (1.12‐4.55) | .022 | |
| Family physicians | 2.26 (0.97‐5.24) | .058 | |
| Work experience (years) | 1‐5® | – | |
| 6‐10 | 2.44 (1.85‐3.21) | <.001 | |
| 11‐20 | 3.13 (2.40‐4.10) | <.001 | |
| >20 | 2.77 (2.06‐3.74) | <.001 | |
| Attitude score | Negative® | – | |
| Neutral | 1.68 (0.66‐4.30) | .280 | |
| Positive | 3.42 (1.38‐8.50) | .008 | |
| Confident towards vaccine efficacy | Not confident® | – | |
| Neutral | 1.57 (1.18‐2.08) | .002 | |
| Confident | 3.58 (2.70‐4.75) | <.001 |
# = using Multivariate logistic regression, ® = Reference group, $ = MOHP facilities.
NB Variables that entered at the beginning of the model but not included in the final model were age groups, gender, profession and chronic diseases.
The most common suggestions raised by participants to improve the coverage rate of influenza vaccine uptake among healthcare professionals were health education about influenza vaccine particularly about efficacy and safety was mentioned by 27.3% of the respondents followed by availability of the vaccine at work (21.9%). Other suggestions included mandatory influenza vaccination for all HCWs (11.6%) and offering vaccine free of charge or inexpensive/ reasonably priced (9.6%) (Figure 4).
FIGURE 4.
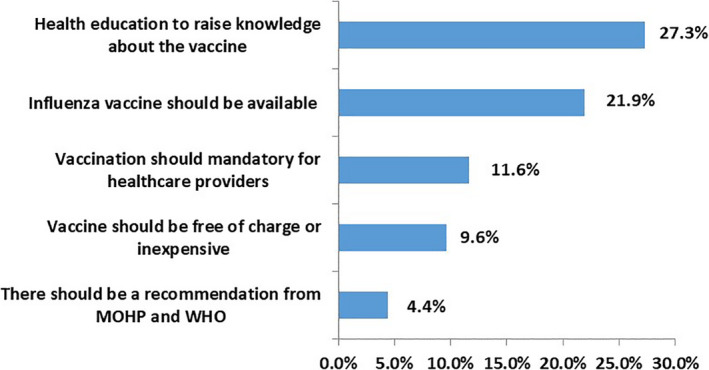
Suggestions from healthcare workers to improve influenza vaccine uptake (N = 3534)
4. DISCUSSION
The present study is the first study to estimate influenza vaccination coverage among Egyptian HCWs and explore their beliefs and attitudes towards seasonal influenza vaccination to improve vaccination coverage among them.
The current study demonstrates a vaccination ever uptake rate among HCWs equal to 46.8% and about 31% in the last season prior to the study. These rates are higher than that reported from EMR (28.2%), 6 UAE (24.7%), 7 India (4.4%), 3 China (6.8%) 10 and Pakistan (8.84%), 11 while they are lower than the vaccination uptake among HCWs in Saudi Arabia (67.6%), 12 and the rates (60% and 80%) reported from developed countries. 13 , 14 , 15 , 16
The reasons for lower vaccination rate in developing countries could include lack of national vaccination strategies, level of awareness of HCWs towards influenza vaccination and the vaccine cost. This could be supported by the higher vaccination rate encountered in this study among HCWs of chest and infectious diseases hospitals affiliated to MOHP who are provided the vaccine free of charge.
In the present study, higher vaccine coverage was observed among female HCWs than males, and this is similar with literature data. 17 , 18 , 19 Our finding could suggest higher confidence in the efficacy of the vaccine among females compared with males. Moreover, the higher rates of vaccination observed among older age group (≥50 years) in our study was also reported from other studies, 20 , 21 , 22 , 23 , 24 a finding that could be explained by longer experience and higher risk of severe infection.
The international literature reports higher vaccination coverage rates of physicians than other HCWs. 14 , 17 , 25 However, the present study showed higher coverage among nurses (34.7%) compared with physicians (27.5%). This is in line with the results of a study from Brazil which showed 69% coverage among nurses versus 49.1% among physicians. 13 We may relate our results to the higher positive attitude among nurses than physicians. Other studies from Saudi Arabia, Australia and Ireland revealed no significant differences in vaccination coverage among the different professions. 12 , 15 , 26
Higher rates of vaccine coverage were found among staff working in related hospitals (such as chest/fever and infectious diseases hospitals) and specialty (such as chest/tropical and infectious diseases). The main factor underlining this finding is offering the seasonal influenza vaccination free of charge to all HCWs in fever/chest hospitals affiliated to MOHP. Furthermore, HCWs in fever/chest hospitals could have higher perception of risk of exposure to influenza infection than HCWs in other specialties. This is in line with a study by Black and colleagues who revealed that coverage was highest among HCWs working in locations where vaccination was required and provided on site at no cost, highlighting the importance of availability of vaccination at workplace. 14
The current study identified some gaps in the attitudes and beliefs among HCWs in Egypt which included perceiving influenza as a mild disease, a finding reported from other studies. 27 , 28 Just as reported in previous studies that 27% to 47% of HCWs think that influenza vaccine could cause post vaccination adverse events, 16 , 27 , 29 , 30 25.1% of our respondents shared this misconception. Both findings could explain the suboptimal rate of vaccination observed in our study. In spite that most of participating HCWs agreed that influenza vaccine could be effective in reducing their risk of developing influenza, yet lower percent were planning to get the vaccine next season. Although there is a sound attitude towards influenza vaccination among the participating HCWs, yet it is inconsistent with their practices.
It is noteworthy that about 80% of the participants in our study agreed with the implementation of a compulsory seasonal vaccination strategy in healthcare settings. This issue is under debate in the scientific and public health community. 31 , 32 Interestingly, this observation is in disagreement with previous data reporting that mandatory vaccination programmes were in fact badly perceived by European HCWs. 33
This large representative group of participants allowed us to identify the main reasons that contributed to HCWs' decisions on influenza vaccination. The prevalent role of vaccine safety in determining flu vaccination uptake has been previously reported 34 , 35 and has been identified in the current study as the principle reason for accepting vaccination among those who had ever been vaccinated. Same result was reported in other studies and surveys. 27 , 36 , 37 , 38 The second powerful motivator in our study was the desire to prevent the spread of infection to others (patients/family/colleagues). Also, other investigators have reported the desire to protect others as the highest rated motive for vaccination. 15 Nevertheless, many studies have demonstrated that self‐protection and protection of family members and other people close to HCWs are main factors motivating HCWs to receive flu vaccination. 16 , 18 , 39
Low vaccine cost was mentioned by 30% of participants to be a cause of accepting vaccination. Added to that, affording it for free or at low cost was one of their recommendations to improve the vaccine uptake. Also most of our participants were more willing to get vaccinated in the future if the vaccine is offered for free by the government.
Adherence to recommendations by MOHP or WHO was a weak driving factor for vaccine uptake as it was reported by only 4.4% of our participants; however, this was one of the principal reasons for immunization of HCWs in the study by Black and colleagues. 14
Among the study non‐vaccinated HCWs, one of the major concerns was the perceived lack of efficacy of the vaccine, a finding previously reported in other studies. 27 , 36 Furthermore, mistrust of the vaccine storage and expiration date was a reason for rejecting vaccine uptake and is in line with what was reported among European HCWs. 40 Clarifying misconceptions about vaccine safety and efficacy should play an essential role in any future educational campaigns. The cost of the vaccine has been previously reported as a possible barrier against influenza vaccine acceptance, 41 , 42 and was also one of the important reasons for declining vaccine uptake by the participating HCWs. In addition, the unavailability of the vaccine calls for concerted efforts to increase HCWs awareness and increase places where vaccine is available in appropriate quantities and timing.
4.1. Strengths and limitations
The strengths of our study are related to the appropriate sample size of HCWs represented from all the regions across the country and covering different levels of healthcare facilities, the high response rate and the different clinical areas represented. We believe that the questionnaire's design was able to capture the real preferences of HCWs.
However, there are some limitations in this study. First, influenza vaccination status was self‐reported by respondents, not subject to independent verification, and potentially influenced by social desirability bias. Recall bias is another potential limitation. Also, this study enrolled HCWs affiliated to governmental sectors (MOHP and university) while those working in private sectors were not included in the study sample, however, most of HCWs in governmental settings also work in private sectors.
5. CONCLUSION AND RECOMMENDATIONS
In conclusion, influenza vaccine coverage is suboptimal among HCWs in Egypt. Low rates stem from a variety of reasons ranging from inadequacy of knowledge to misperceptions and fears regarding vaccine efficacy and safety, in addition to high cost and unavailability. These findings should be used to customize and improve any future promotion campaigns, in order to overcome the identified barriers. Also, operational strategies addressing vaccination accessibility at workplace need to be implemented to improve vaccine uptake.
Participants in this study were mostly having positive attitudes and beliefs towards influenza vaccine, and this provides better opportunity to improve vaccine coverage through the tailored health education campaigns and operational strategies which hinder the barriers that limit compliance to vaccination.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
Sally Adel Hakim: Data curation (equal); Formal analysis (equal); Investigation (equal); Methodology (equal). Wagdy Amin: Data curation (equal); Investigation (equal); Methodology (equal). Mohamed Farouk Allam: Conceptualization (equal); Data curation (equal); Formal analysis (equal); Investigation (equal); Methodology (equal). Asmaa Fathy: Data curation (equal); Formal analysis (equal); Methodology (equal). Amira Mohsen: Conceptualization (equal); Data curation (equal); Formal analysis (equal); Funding acquisition (lead); Investigation (equal); Methodology (equal).
ETHICAL APPROVAL
Verbal informed consent from each participant was obtained before delivering the questionnaire to him/her. We considered filling the questionnaire and returning it back to data collector as a confirmed consent. Each HCW participated in the study was informed about the aim of the research and the voluntary decision to accept or refuse participation. Approval from the Research Ethics Committee (REC) of the Ministry of Health and Population (MOHP)—Central Directorate for Research and Health Development was issued before conducting the study (REC number: FWA00016183) and REC approval of the Faculty of Medicine—Ain Shams University was also obtained. Administrative approvals were obtained before the beginning of the study from the health directorates and the directors of university hospitals.
ACKNOWLEDGEMENT
The authors cordially acknowledge all HCWs who participated in this study. We thank all team staff who supervised the data collection.
Hakim SA, Amin W, Allam MF, Fathy AM, Mohsen A. Attitudes, beliefs and practice of Egyptian healthcare workers towards seasonal influenza vaccination. Influenza Other Respi Viruses. 2021;15(6):778-788. 10.1111/irv.12868
Funding information
This research was funded from the World Health Organization Representative Office in Egypt, award number 61722
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author after permission from relevant authority to release data and upon reasonable request.
REFERENCES
- 1. Hollmeyer H, Hayden F, Mounts A, Buchholz U. Review: interventions to increase influenza vaccination among healthcare workers in hospitals. Influenza Other Respir Viruses. 2013;7(4):604‐621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. De Serres G, Skowronski DM, Ward BJ, et al. Influenza vaccination of healthcare workers: critical analysis of the evidence for patient benefit underpinning policies of enforcement. PLoS ONE. 2017;12(1):e0163586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bali NK, Ashraf M, Ahmad F, et al. Knowledge, attitude, and practices about the seasonal influenza vaccination among healthcare workers in Srinagar, India. Influenza Other Respir Viruses. 2013;7(4):540‐545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gianino MM, Politano G, Scarmozzino A, et al. Estimation of sickness absenteeism among Italian healthcare workers during seasonal influenza epidemics. PLoS ONE. 2017;12(8):e0182510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ahmed F, Lindley MC, Allred N, Weinbaum CM, Grohskopf L. Effect of influenza vaccination of healthcare personnel on morbidity and mortality among patients: systematic review and grading of evidence. Clin Infect Dis. 2014;58:50‐57. [DOI] [PubMed] [Google Scholar]
- 6. Zaraket H, Melhem N, Malik M, Khan WM, Sbaibo G, Abubakar A. Review of seasonal influenza vaccination in the Eastern Mediterranean region: policies, use and barriers. Infect Public Health. 2019;12(4):472‐478. [DOI] [PubMed] [Google Scholar]
- 7. Abu‐Gharbieh E, Fahmy S, Rasool BA, Khan S. Influenza vaccination: healthcare workers attitude in three Middle East countries. Int J Med Sci. 2010;7(5):319‐325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. WHO SAGE Seasonal Influenza Vaccination Recommendations during the COVID‐19 Pandemic. Interim guidance 21 September 2020. https://www.who.int/immunization/policy/position_papers/Interim_SAGE_influenza_vaccination_recommendations.pdf?ua=1. Accessed September 25, 2020.
- 9. Epi Info version 7.0 for Windows. CDC – Atlanta, USA. https://www.cdc.gov/epiinfo/support/downloads.html. Accessed May 15, 2019.
- 10. Ma YY, Zhang LJ, Shi Y, et al. A survey on the current status and related factors of influenza vaccination among health care workers in tertiary hospitals of Xining city during the influenza epidemic season from 2017 to 2018. Zhonghua Yu Fang Yi Xue Za Zhi. 2019;53(10):1018‐1021. [DOI] [PubMed] [Google Scholar]
- 11. Ali I, Ijaz M, Rehman IU, Rahim A, Ata H. Knowledge, attitude, awareness, and barriers toward influenza vaccination among medical doctors at tertiary care health settings in Peshawar, Pakistan–A cross‐sectional study. Front Public Health. 2018;27(6):173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alshammari TM, Yusuff KB, Aziz MM, Subaie GM. Healthcare professionals' knowledge, attitude and acceptance of influenza vaccination in Saudi Arabia: a multicenter cross‐sectional study. BMC Health Serv Res. 2019;19:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Souza TP, Lobao WM, Santos CAST, Almeida MDCC, Moreira Junior ED. Factors associated with the acceptance of the influenza vaccine among health workers: knowledge, attitude and practice. Cien Saude Colet. 2019;24(8):3147‐3158. [DOI] [PubMed] [Google Scholar]
- 14. Black CL, Yue X, Ball SW, et al. Influenza vaccination coverage among health care personnel‐United States, 2017–18 influenza season. MMWR Morb Mortal Wkly Resp. 2018;67(38):1050‐1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Knowler P, Barrett M, D. Watson AR. Attitudes of healthcare workers to influenza vaccination. Infection Dis Health. 2018;23(3):156‐162. [DOI] [PubMed] [Google Scholar]
- 16. Učakar V, Kraigher A. Acceptance of seasonal influenza vaccination among Slovenian physicians, 2016. Zdr Varst. 2019;58(1):47‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Genovese C, Picerno IAM, Trimarchi G, et al. Vaccination coverage in healthcare workers: a multicenter cross‐sectional study in Italy. J Prev Med Hyg. 2019;60:E12‐E17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rehmani R, Memon JI. Knowledge, attitudes and beliefs regarding influenza vaccination among healthcare workers in a Saudi hospital. Vaccine. 2010;28(26):4283‐4287. [DOI] [PubMed] [Google Scholar]
- 19. Abu Hammour W, Al‐Saleh S. Knowledge, attitudes, and practice of healthcare workers toward influenza vaccination at Al Jalila Children's Specialty Hospital (AJH, Dubai, UAE). Int J Pediatr Adolesc Med. 2019;6(1):16‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Massin S, Ventelou B, Nebout A, Verger P, Pulcini C. Cross‐sectional survey: risk‐averse French general practitioners are more favorable toward influenza vaccination. Vaccine. 2015;33:610‐614. [DOI] [PubMed] [Google Scholar]
- 21. Di Gregori V, Franchino G, Marcantoni C, Simone B, Costantino C. Logistic regression of attitudes and coverage for influenza vaccination among Italian Public Health medical residents. J Prev Med Hyg. 2014;55(4):152‐157. [PMC free article] [PubMed] [Google Scholar]
- 22. Alicino C, Iudici R, Barberis I, et al. Influenza vaccination among healthcare workers in Italy. Hum Vaccin Immunother. 2015;11(1):95‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Restivo V, Costantino C, Mammina C, Vitale F. Influenza like illness among medical residents anticipates influenza diffusion in general population: data from a national survey among Italian medical residents. PLoS ONE. 2016;11(12):e0168546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gilardi F, Castelli Gattinara G, Vinci MR, et al. Seasonal influenza vaccination in health care workers. A pre‐post intervention study in an Italian paediatric hospital. Int J Environ Res Public Health. 2018;15(5):E841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals–a review of studies on attitudes and predictors. Vaccine. 2009;27(30):3935‐3944. [DOI] [PubMed] [Google Scholar]
- 26. Hogan V, Lenehan M, Hogan M, Natin DP. Influenza vaccine uptakeand attitudes of healthcare workers in Ireland. Occup Med (Lond). 2019;69(7):494‐499. [DOI] [PubMed] [Google Scholar]
- 27. Khazaeipour Z, Ranjbarnovin N, Hoseini N. Influenza immunization rates, knowledge, attitudes and practices of healthcare workers in Iran. J Infect Dev Ctries. 2010;4(10):636‐644. [DOI] [PubMed] [Google Scholar]
- 28. Esposito S, Tremolati E, Bellasio M, et al. Attitudes and knowledge regarding influenza vaccination among hospital health workers caring women and children. Vaccine. 2007;25:5283‐5289. [DOI] [PubMed] [Google Scholar]
- 29. Hosamirudsari H, Kanavee AR, Ghanbari M, Akbarpour S, Alimohamadi Y. Assessment of the belief and attitudes of Iranian healthcare personnel's toward the influenza infection and influenza vaccination. J Prev Med Hyg. 2019;60:E178‐E183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Halpin C, Reid B. Attitudes and beliefs of healthcare workers about influenza vaccination. Nursing Older People. 2019;31(2):32‐39. [DOI] [PubMed] [Google Scholar]
- 31. Galanakis E, D'Ancona F, Jansen A, et al. The issue of mandatory vaccination for healthcare workers in Europe. Expert Rev Vaccines. 2014;13:277‐283. [DOI] [PubMed] [Google Scholar]
- 32. Dubov A, Phung C. Nudges or mandates? The ethics of mandatory flu vaccination. Vaccine. 2015;33:2530‐2535. [DOI] [PubMed] [Google Scholar]
- 33. Kassianos G. Willingness of European healthcare workers to undergo vaccination against seasonal influenza: current situation and suggestions for improvement. Drugs Context. 2015;4:212268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Maltezou HC, Poland GA. Vaccination policies for healthcare workers in Europe. Vaccine. 2014;32:4876‐4880. [DOI] [PubMed] [Google Scholar]
- 35. Bellia C, Setbon M, Zylberman P, Flahault A. Healthcare worker compliance with seasonal and pandemic influenza vaccination. Influenza Other Respir Viruses. 2013;7(Suppl 2):97‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Blank PR, Schwenkglenks M, Szucs TD. Influenza vaccination coverage rates in five European countries during season 2006/07 and trends over six consecutive seasons. BMC Public Health. 2008;8:272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Janks M, Cooke S, Odedra A, Kang H, Bellman M, Jordan RE. Factors affecting acceptance and intention to receive pandemic influenza A H1N1 vaccine among primary school children: a cross‐sectional study in Birmingham, UK. Influenza Res Treat. 2012;2012:182565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Malosh R, Ohmit SE, Petrie JG, Thompson MG, Aiello AE, Monto AS. Factors associated with influenza vaccine receipt in community dwelling adults and their children. Vaccine. 2014;32:1841‐1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bonaccorsi G, Santomauro F, Porchia BR, et al. Beliefs and opinions of health care workers and students regarding influenza and influenza vaccination in Tuscany, Central Italy. Vaccines (Basel). 2015;3:137‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Karafillakis E, Dinca I, Apfel F, et al. Vaccine hesitancy among healthcare workers and their patients in Europe—a qualitative study. Vaccine. 2016;34(41):5013‐5020. [DOI] [PubMed] [Google Scholar]
- 41. World Health Organization (WHO) Global Influenza Programme . Seasonal Influenza Vaccine Use in Low and Middle Income Countries in the Tropics and Subtropics – A Systematic Review. 2015. http://www.who.int/influenza/resources/publications/9789241565097/en/. Accessed December 15, 2019.
- 42. Yaqub O, Castle‐Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Soc Sci Med. 2014;112:1‐11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author after permission from relevant authority to release data and upon reasonable request.


