Abstract
Pregnant women have an increased susceptibility to infection by Plasmodium falciparum. Parasites may be present in the placenta yet not detectable in peripheral blood smears by routine light microscopy. In order to determine how frequently misdiagnosis occurs, peripheral blood and placental samples were collected from 1,077 Cameroonian women at the time of giving birth and examined for the presence of malarial parasites by using light microscopy. Results showed that 20.1% of the women who had placental malaria were peripheral blood smear negative. Thus, malarial infection was not detected by microscopic examination of peripheral blood smears from approximately one out of five malaria-infected women. Since P. falciparum parasites secrete histidine-rich protein 2 (HRP-2), we sought to determine if detecting HRP-2 in either peripheral plasma or whole blood might be used to diagnose the presence of parasites “hidden” in the placenta. Samples of peripheral plasma from 127 women with different levels of placental malarial infection were assayed by HRP-2-specific enzyme-linked immunosorbent assay. HRP-2 was detected in 88% of the women with placental malaria who tested negative by blood smear. Additionally, whole blood was obtained from 181 women and tested for HRP-2 with a rapid, chromatographic strip test (ICT). The ICT test accurately detected malarial infection in 89.1% of P. falciparum-infected women. Furthermore, 94% of women with malaria were accurately diagnosed by using a combination of microscopy and the ICT test. Thus, detection of HRP-2 in conjunction with microscopy should improve diagnosis of malaria in pregnant women.
Women living in areas where malaria is endemic have an increased risk of Plasmodium falciparum infection during pregnancy (reviewed in reference 14). Malarial parasites accumulate and multiply within the intervillous spaces of the placenta, creating a condition often referred to as placental malaria. As a result, high numbers of trophozoite and schizont stage parasites may be found in the placenta (4, 13). Within the placenta, parasites develop into trophozoites and schizonts, and their presence often induces an inflammatory-type response resulting in the accumulation of macrophages (5, 12, 27); elevated levels of tumor necrosis factor alpha, gamma interferon, transforming growth factor β, and interleukin-2 (8); and alteration in syncytiotrophoblasts (5, 12, 27, 30). As a result, placental parasitemias increase the risk of a woman delivering a low-birthweight infant due to prematurity or intrauterine growth retardation (reviewed in reference 14). Thus, placental malaria is an important clinical problem, especially for the developing fetus. If properly diagnosed, however, antimalarial chemotherapeutic treatment can be initiated to prevent the problem (29).
Previous studies have reported that parasites may not be detected by microscopy of the peripheral blood of women with placental malaria (3, 7). The proportion of pregnant women, however, who are not diagnosed by routine microscopic examination of peripheral blood smears is unclear. The present study sought to address this question and found that parasites were not detected by microscopy in the peripheral blood smears of 20.9% of the women who had parasites present in the placenta. Thus, the routine method for diagnosing malaria failed to detect parasites in approximately one out of five pregnant women who were infected with malarial parasites, demonstrating the need for an improved diagnostic approach.
Currently, alternative methods for detecting malarial parasites hidden within the placenta are not available. It has been shown that P. falciparum parasites release antigens that circulate in the peripheral blood. In the present study, we sought to determine if detecting the P. falciparum-specific antigen histidine-rich protein 2 (HRP-2) in peripheral blood could be used to diagnose placental malaria. We selected this antigen because Howard et al. demonstrated that P. falciparum cultured in vitro synthesizes and secretes HRP-2 during the trophozoite and schizont stages of development (11). Subsequent studies have shown that HRP-2 is present in the plasma of persons who are infected with P. falciparum (6, 16), is produced by all natural strains and isolates of P. falciparum tested (19), and is apparently antigenically invariant (28). HRP-2 contains multiple tandem repeats of AHHAAD interspersed with AHH and AHHAA (28). As a result, HRP-2 has repetitive B-cell epitopes that allow one to easily detect it by using an antigen capture assay (1, 9, 24, 26). The goal of this project was to determine if assays which detect the malarial antigen HRP-2 could be used to successfully diagnose placental malaria.
MATERIALS AND METHODS
Collection of blood and placental samples.
The study was conducted over a 3-year period (February 1995 to December 1998) in Yaounde, the capital of Cameroon. Women participating in the study had been repeatedly infected with P. falciparum throughout their lives and had developed immunity to the organism. They were essentially healthy at the time of giving birth and did not show clinical signs of malaria. Informed consent was obtained from each woman. Then, ∼8 ml of heparinized venous peripheral blood was collected. Immediately following delivery, the placenta was obtained, and samples of maternal placental blood were collected. To collect the blood, the placenta was placed with the maternal surface upwards, a shallow incision was made with scissors, and blood was collected from the intervillous spaces with a heparinized syringe. In addition, a small piece of placental tissue (∼2.5 cm3) was removed from the center of the placenta and used to prepare impression smears (see below).
Detection of malarial parasites by light microscopy.
Complete parasitological data based on microscopy was available for 1,077 women. In this study, a woman was diagnosed as being infected with P. falciparum (i.e., malaria positive) if parasites were detected by light microscopy in either the peripheral blood or samples collected from the placenta. A woman was considered to be malaria negative if parasites were not found in either site.
Routine methods were used to prepare thick and thin blood smears of the peripheral blood. Following staining with Diff-quick (Baxter International, Inc., Deerfield, Ill.), the slides were examined by two microscopists who scanned through 100 fields of the thin film containing ∼200 erythrocytes each. If parasites were seen, the percent parasitemia was reported based on the number of parasitized erythrocytes per ∼10,000 erythrocytes. If parasites were not found in the thin film, then 200 fields of the thick films were examined. If parasites were again not found, the woman was considered to be peripheral blood smear negative. This microscopic method is routinely used to diagnose malaria (17).
Following preparation of blood smears, heparinized blood samples were centrifuged, and plasma was removed and stored at −20°C. As described below, 127 of these plasma samples were analyzed by HRP-2-specific enzyme-linked immunosorbent assay (ELISA).
In order to detect parasites in the placenta (i.e., placental malaria), thick and thin blood films of maternal placental blood were prepared, stained, and examined for the presence of parasites as described above. In addition, pieces of placental tissues were used to prepare impression smears. In brief, a piece of the placenta (∼1 mm3) was blotted on filter paper and then pressed 6 to 10 times against a glass slide. After drying, impression smears were fixed, stained with Diff-quick, and examined by two microscopists for the presence of malarial parasites. Parasitemias were determined by counting the number of infected cells per 500 erythrocytes seen on impression smears. Impression smears allow the microscopist to detect parasites lodged in the small sinuses located among placental villi (i.e., in the site where they are sequestered). Based on the presence or absence of parasites, women were determined to be positive or negative for placental malaria.
Detection of HRP-2 in plasma by using an HRP-2-specific ELISA.
In November 1996, we began evaluating the possibility of detecting HRP-2 in peripheral plasma as a way of diagnosing placental malaria. Based on the cryopreserved plasma samples available to us at that time, representative samples (n = 127) were selected for evaluation. A total of 74 samples from women with different levels of peripheral and placental parasitemias were evaluated. Of the 74 samples, 20 were from women who had placental malaria but were peripheral blood smear negative (i.e., those who had been misdiagnosed by light microscopy). In addition, plasma collected during the same time period from women who were determined to be malarial parasite negative by microscopy (n = 53) were also tested.
The ELISA used in the present study has been described previously (24, 26). It uses a pair of monoclonal antibodies (MAb) that has been well characterized (16). In brief, microtiter wells (Maxisorp; Nunc, Inc.) were coated with 1 μg of purified MAb 1E1 (immunoglobulin M). Following blocking with 10% Carnation instant milk in 0.1 M phosphate buffered saline (PBS), pH 7.2, containing 0.01% Tween 20 (PBS-Tw), 50 μl of plasma diluted 1:1 with PBS was added, and the mixture was incubated at room temperature for 60 min. Following washing, 50 μl of diluted alkaline phosphatase-labeled MAb 2G12 (immunoglobulin G1) was added for 60 min. Following washing with PBS-Tw, 100 μl of substrate (5-mg tablet of p-nitrophenyl phosphate [Sigma 104; Sigma Chemical Co., St. Louis, Mo.] dissolved in 5 ml of buffer [97 ml of diethanolamine plus 101 mg of Mg2Cl · 6H2O in 800 ml of water, pH 9.6]) was added. After ∼15 min, the optical density (OD) was determined with a BioTech Multiscan ELISA reader at 405 and 630 nm. All samples were assayed in at least duplicate. Plasma from nonpregnant Cameroonian adults who were peripheral blood smear negative (i.e., presumed to be malaria negative), cord blood from Cameroonian newborns (malaria-negative), and blood from unexposed adults in the United States were used as negative controls. The mean OD for negative plasma plus 4 standard deviations was used as a cutoff.
To verify the linearity and sensitivity of the HRP-2-specific ELISA, an extract containing known amounts of in vitro-cultured P. falciparum-parasitized erythrocytes was prepared. In brief, in vitro cultures of P. falciparum (NF-54 strain) were harvested when parasitemias reached ∼1%, and cells were washed and frozen at −65°C. Immediately prior to use, an aliquot was defrosted, serially diluted in PBS-Tw, and used in the assay. An equivalent preparation of uninfected human erythrocytes was prepared and used as a negative control. In addition, the assay was evaluated by using purified recombinant HRP-2, which was kindly provided by R. Howard and B. Pasloske.
Detection of P. falciparum by PCR analysis.
In this study, some samples tested positive for HRP-2 by ELISA but were slide negative for parasites when tested by microscopy. To determine if parasites were present at submicroscopic levels, these samples were analyzed with the nested PCR described by Snounou et al. (22, 23). Cryopreserved erythrocytes from 38 samples were available for study. In brief, cryopreserved erythrocytes were lysed with 0.05% saponin, and freed parasites were pelleted by centrifugation and lysed with 2% sodium dodecyl sulfate. Parasite DNA was purified with phenol-chloroform, precipitated with sodium acetate and ethanol, and amplified with genus-specific primers followed by amplification with P. falciparum-specific primers (22, 23). The amplified DNA was electrophoresed on an agarose gel and visualized with ethidium bromide.
Detection of HRP-2 in whole blood using the ICT malaria Pf Test.
In 1996, the ICT malaria Pf test (Amrad ICT, Sydney, New South Wales, Australia) which detects HRP-2 in whole blood (9) was reported. This test was performed according to the manufacturer’s instructions. In brief, the kit contains a cardboard book with a chromatographic test strip on one side. First, 10 μl of whole blood was applied to the sample pad, which contains a colloidal-gold-labeled MAb to HRP-2 and a lysing agent. Then, 4 drops of the buffer provided in the kit was added, causing the reactants to migrate up the strip and cross a second MAb line. Blood was cleared from the strip by back flushing the strip with the buffer provided. A control line on the membrane turns pink if the test has been conducted properly. Tests in which the control line turned pink but the test line was negative were scored as negative, while those samples for which both the control and test lines were pink were scored as positive. Since the ICT assay uses whole blood (not plasma), between May and November 1996, this test was evaluated by using whole fresh blood from 181 women who agreed to participate.
Statistical analysis.
Since results obtained in the ELISA showed a direct relationship between amount of HRP-2 and OD all associations are reported as parametric Pearson product moment correlations.
RESULTS
Placental and peripheral parasitemias in Cameroonian women.
Microscopic examination of peripheral and placental samples collected at the time of childbirth from 1,077 women showed that 21.9% of the women were infected with malarial parasites (i.e., parasites were detected by microcopy in either peripheral blood smears or placental samples). Among the women who had malaria, 20.9% of those who had placental malaria were peripheral blood smear negative. Placental parasitemias ranged from 0.001 to 65%. The distribution of placental parasitemias among the malaria-positive women is shown in Table 1. As can be seen, the majority of women who were infected with P. falciparum had placental parasitemias between 0.11 and 10%. Approximately 12% of the remaining women had either very high (>10%) or very low (<0.1%) parasitemias. Fewer than 2% of the women in this study were found to have parasites in the peripheral blood but not in the placenta.
TABLE 1.
Percent parasitemias in the peripheral blood of women with different levels of placental malaria
| % Placental parasitemia | No. of samples tested | % Peripheral blood parasitemia
|
% of slides testing negative | ||
|---|---|---|---|---|---|
| Range | Median | Mean ± standard error of the mean | |||
| 0.001–0.1 | 35 | 0.0–0.09 | 0.0 | 0.02 ± 0.004 | 54.3 |
| 0.11–1.0 | 86 | 0.0–0.97 | 0.02 | 0.07 ± 0.02 | 34.9 |
| 1.1–10.0 | 65 | 0.0–2.8 | 0.13 | 0.32 ± 0.06 | 10.8 |
| 10.1–65a | 36 | 0.006–7.5 | 0.54 | 1.55 ± 0.33 | 0 |
The highest parasitemia is reported as 65%.
The data in Table 1 shows the percentages of parasitemia observed in the peripheral blood of women with different degrees of placental malaria. In general, mean peripheral parasitemias increased as placental parasitemias increased. A proportion of women with placental parasitemias below 10% were, however, blood smear negative. For example, 54.3% of women with placental parasitemias less than 0.1%, and 34.9% of women with placental parasitemias between 0.11 and 1.0%, were peripheral blood smear negative (Table 1). Surprisingly, 10.8% of women with placental parasitemias between 1 and 10% were also misdiagnosed. Women with placental parasitemias of greater than 10% were routinely peripheral blood smear positive and accurately diagnosed by microscopy.
Evaluation of the HRP-2-specific ELISA for diagnosing placental malaria in pregnant women.
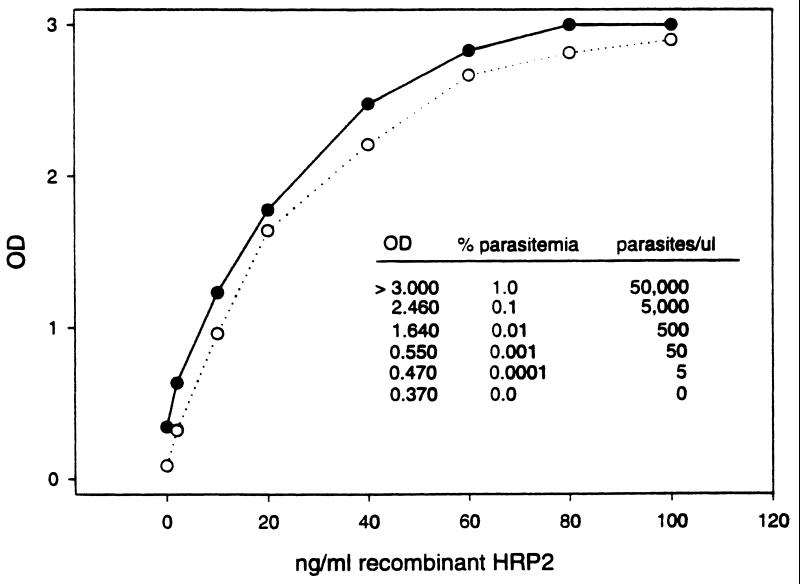
The ELISA used in this study has been previously described (24, 26), but its ranges of linearity and sensitivity have not been reported. Periodically, recombinant HRP-2 (rHRP-2) and extracts containing a known number of P. falciparum-infected erythrocytes and normal erythrocytes were tested in the assay. Representative curves obtained by using rHRP-2 at the beginning and end of the study are shown in Fig. 1. Inserted within the figure are OD values for serial dilutions of P. falciparum-infected erythrocytes. As can be seen, the assay is semiquantitative for 10- to 100-ng samples of rHRP-2, is useful over a wide range of parasitemias, and was stable throughout the study. Using a cutoff of the mean ± 2 standard deviations above the background control (diluent without rHRP-2 or normal erythrocytes), the assay has a lower level of detection of ∼2 to 4 ng of HRP-2 and the ability to detect the equivalent of approximately five parasites per microliter of blood.
FIG. 1.
The HRP-2-specific ELISA. rHRP-2 was used in the assay to demonstrate the relationship between OD and the relative amounts of HRP-2 detected. Two representative curves, one from the beginning of the study in 1996 and one from the end of the study in 1998, are shown. Using a cutoff of mean ± 2 standard deviations (no HRP-2), the assay was found to have a lower limit of detection in the range of 2 to 4 ng of HRP-2. For comparison, OD values for an extract containing different numbers of parasites are included to help evaluate the practical sensitivity of the assay.
In the initial experiment, we sought to compare the level of HRP-2 in peripheral plasma with that in placental plasma, i.e., where the parasites were sequestered, as well as to compare the OD obtained in the ELISA with percent parasitemia. Results (n = 74) showed that there was a significant correlation between the amount of HRP-2 in paired peripheral and placental plasma (r = 0.369, p < 0.001) and a moderate association between placental parasitemias of 1 to 10% and placental HRP-2 levels (r = 0.550, p < 0.02). There was no convincing association, however, between the amount of HRP-2 present in peripheral plasma and peripheral or placental parasitemias.
To evaluate the potential use of the ELISA in diagnosing placental malaria, peripheral plasma samples from women with different levels of placental parasitemias, as well as samples from women who tested malaria negative by light microscopy, were tested with the ELISA. Results from light microscopy and the ELISA were compared (Table 2). The two assays were found to be similar in sensitivity at higher parasitemias, but the ELISA was more sensitive at lower parasitemias (<0.1%) (Table 2). For example, when placental parasitemias were very low (0.001 to 0.1%), only 45.6% of the women had levels of parasites in their peripheral blood which were detectable by microscopy, whereas 66.7% had circulating HRP-2.
TABLE 2.
Percentage of samples that tested positive in the HRP-2-specific ELISA
| % Placental parasitemia | No. of samples testeda | % Testing positive by ELISA | % Testing positive by microscopy |
|---|---|---|---|
| No parasites detected | 53 | 49.1 | 0 |
| 0.001–0.1 | 12 | 66.7 | 45.7 |
| 0.11–1.0 | 32 | 71.9 | 65.1 |
| 1.1–10 | 17 | 82.4 | 89.2 |
| >10 | 12 | 100.0 | 100.0 |
Results of HRP-2-specific ELISA on 126 peripheral blood samples from Cameroonian women.
Of the malaria-positive women chosen for the ELISA study, 20 had placental malaria but were blood smear negative. Among these women, all five with low placental parasitemias (<0.1%) tested positive by ELISA, and 10 of 12 with moderate placental parasitemias (0.1 to 1.0%) tested positive. Overall, ELISA detected the infections in 88% of the malaria-parasite-positive women in this group. Only three samples were available from women with placental parasitemias greater than 1% who were blood smear negative. Data from these samples, plus samples from 26 additional women with high parasitemias (>1%) who were blood smear positive, showed that 89.7% (26 of 29) of these women were also positive for HRP-2 (Table 2). Thus, the ELISA proved to be effective in detecting HRP-2 in the peripheral plasma of women who were infected with malaria.
HRP-2 was also detected by ELISA in 49% of the samples from pregnant women who tested parasite negative by microscopy (Table 2). Because of the apparently high level of false-positive reactions, 38 of the HRP-2-positive, slide-negative samples were analyzed with a PCR-based system for detection of P. falciparum small subribosomal DNA (22). Sixty-five percent of the samples that tested positive for HRP-2 by ELISA also tested positive for P. falciparum by PCR, validating the high sensitivity of the HRP-2-specific ELISA (see Discussion).
Evaluating the ICT strip test with whole blood.
Since the ICT strip test is commercially available and can easily be used by health care workers in many situations, we sought to evaluate its accuracy for detecting malarial infection in pregnant women and, specifically, its potential for detecting placental P. falciparum malaria. Microscopic examination of peripheral blood and placental samples from 181 Cameroonian women showed that 35.4% (64 of 181) of the women had malaria at the time of delivery. Microscopically, parasites were detected in the peripheral blood and placentas of 84% (54/64) of these women; 16% (10 of 64) of the women had placental malaria but were peripheral blood smear negative.
A direct comparison of results obtained by microscopic examination of peripheral blood smears with those from the ICT test showed that the strip test had a sensitivity of 94.4% and a specificity of 90.6% (Table 3), which are similar to those reported for this assay in other situations (9, 10, 18). If one considers, however, that 16% of the women were peripheral blood smear negative but had placental malaria, then the overall accuracy of the test for diagnosing malaria in pregnant women changes (Table 3). The ICT test correctly identified 57 of 64 women who had malaria (89% sensitivity) and had a false-positivity rate of only 5.1% (6 of 117). The specificity of the assay increased to 94.9% when placental malaria was considered (Table 3).
TABLE 3.
Results of the ICT malaria Pf test on 181 peripheral blood samples from Cameroonian women
| ICT test result | Peripheral blood smear microscopy result (%)
|
Combined peripheral blood and placental microscopy result (%)
|
||
|---|---|---|---|---|
| Positive | Negative | Positive | Negative | |
| Positive | 94.4 (51/54) | 9.4 (12/127) | 89.1 (57/64) | 5.1 (6/117) |
| Negative | 5.6 (3/54) | 90.6 (115/127) | 10.9 (7/64) | 94.9 (111/117) |
In summary, of the 64 women who had malaria, 84% (54 of 64) were correctly diagnosed by routine microscopic detection of parasites in peripheral blood smears and 89.1% were correctly diagnosed with the ICT rapid strip test (57 of 64) with a false-positivity rate of 5.1%; however, 93.8% of the women were correctly diagnosed using a combination of microscopy and the ICT test. Thus, detection of HRP-2 in the peripheral blood in conjunction with microscopy should improve diagnosis of malaria during pregnancy, due to an increased detection of parasitemic patients without peripheral parasitemias.
DISCUSSION
As noted above, studies have reported the absence of parasites in the peripheral blood of women with placental malaria (reviewed in reference 3), but the proportion of pregnant women who are not diagnosed by routine microscopic examination of peripheral blood smears is unclear. Based on the examination of samples from 1,077 women, we found that 20.1% of women who had placental malaria tested peripheral blood smear negative by microscopy and that this proportion increased as placental parasitemias decreased. As shown in Table 1, infections in approximately half of the women who had placental parasitemias below 0.1% were not detected by microscopy. Even 10% of women with high placental parasitemias (1 to 10%) tested negative. Of course, accurate diagnosis by microscopy depends upon the availability of good equipment for microscopic analysis, properly stained blood smears, and well-trained technicians. The current study was conducted in a modern research laboratory by highly experienced microscopists who spent a significant amount of time searching for parasites. Thus, many of the low parasitemias recorded here, e.g., 0.001% (which is equivalent to one parasite per 100,000 erythrocytes), could have been missed under less optimal conditions. Thus, in many clinical settings the extent of misdiagnosis would likely be higher than that reported here.
Overall, the results show that detection of HRP-2 in peripheral blood along with microcopy may improve diagnosis. The ELISA used in the present study is highly sensitive and has a lower limit of detection, in the range of ∼2 to 4 ng of rHRP-2 in plasma or approximately five parasites per microliter of whole blood (Fig. 1). The ELISA was field tested in Thailand in 1993 and was reported to have a sensitivity of 98.1% and a specificity of 96.2% when using whole blood (15). In conjunction with another study (2), we screened 166 whole-blood samples from Cameroonian children with fever and found the ELISA to have a sensitivity of 92.0% and a specificity of 92.4% when compared to microscopy. Thus, there was good agreement (in all the studies) between the presence and absence of malarial infection detected by microscopy and the presence or absence of HRP-2. In the study described here, the HRP-2-specific ELISA and microscopy had similar sensitivities for detecting the prevalence of malarial infection in pregnant women when placental parasitemias were greater than 1%, but the ELISA was more sensitive than microscopy at lower parasitemias (Table 2). HRP-2 was detected in the plasma of 88% (15 of 17) of women with placental malaria, less than 1% of whom were blood smear negative. Based on the data in Table 1, this is the group of women in which placental malaria is most often misdiagnosed. We therefore feel that the ELISA would be a good adjunct to light microscopy for diagnosing malaria during pregnancy.
The results shown in Table 2 also reveal that the ELISA detected HRP-2 in 49% of the samples obtained from pregnant women who were diagnosed as being malarial parasite negative; i.e., parasites were not found by microscopy in either peripheral blood smears or thick or thin impression smears of the placenta. The difference between microscopy and ELISA results in the current study on pregnant women was initially surprising, since the rate of false positivity of the ELISA for Cameroonian children (2) and Thai adults (15) was less than 10%. We believe there are two explanations. First, examination of placental impression smears showed the presence of both free hemozoin pigment and pigment within macrophages, indicating the presence of either a current subpatent or a very recent infection. It is well established that HRP-2 may persist in the bloodstream for a period of time (3 to 14 days) following the clearance of parasites (15, 20, 21, 25, 26). Some, but not all, of the above women may fall into this category. Second, as mentioned in the results, one of the authors (R.R.D.) analyzed 38 of the slide-negative, HRP-2-positive samples by PCR (22, 23) and detected parasite DNA in 65% of the samples. Thus, many of the women who tested malarial parasite negative by microscopy were actually infected with low levels of P. falciparum. The HRP-2-specific ELISA is highly sensitive and may be of value when one needs to detect very low levels of placental parasitemia.
Currently, two rapid chromatographic tests are commercially available for detecting HRP-2 in blood. They are the ParaSight-F test (Becton Dickinson and Co.) and the ICT test described herein. Both tests are highly efficient in detecting malarial infection and appear to be approximately equivalent in sensitivity and specificity (10, 18). The ParaSight-F test has been evaluated extensively in a number of different countries (1, 10, 18, 20, 21, 25). We can find no reference, however, to either chromatographic test being examined previously for its ability to diagnose placental malaria in pregnant women. As shown in Table 3, the ICT was found to be quite efficient in detecting malarial infection in pregnant women. Microscopy was efficient for diagnosing malarial infection in 84% of the women with placental malaria; the ICT test had a sensitivity of 89%. Unfortunately, 10.9% of the women who had placental malaria were still not identified by the ICT test. Although placental parasitemias were very low in many of these women, the parasite may still exert a negative effect on maternal-fetal exchange. Consequently, additional research is needed to develop more sensitive approaches for diagnosing placental malaria.
ACKNOWLEDGMENTS
This work was supported by NIAID, NIH, grant UO1 AI35839. The ICT malaria Pf test kits were provided by the manufacturer.
We thank the Honorable Minister of Health for permission, through M. Sosso, to work at the two hospitals; the administrative and nursing staffs at Maternite Principale and Biyem-Assi hospitals for their assistance; V. Titanji and R. Mimpfoundi for cooperative support at the Biotechnology Center, where the laboratory work was conducted; A. Walker-Abbey for valuable discussions; and M. Sosso for his assistance in making this project possible. We also thank the women who contributed samples for participating in the study.
REFERENCES
- 1.Beadle C, Long G W, Weiss W R, McElroy P D, Maret S M, Oloo A J, Hoffman S L. Diagnosis of malaria by detection of Plasmodium falciparum HRP-2 antigen with a rapid dipstick antigen-capture assay. Lancet. 1994;343:564–568. doi: 10.1016/s0140-6736(94)91520-2. [DOI] [PubMed] [Google Scholar]
- 2.Bechem N N, Leke R F G, Tietche F, Taylor D W. Evaluation of a rapid test for histidine rich protein 2 for diagnosis of Plasmodium falciparum infection in Cameroonian children. Trans R Soc Trop Med Hyg. 1999;9:1. doi: 10.1016/s0035-9203(99)90175-x. [DOI] [PubMed] [Google Scholar]
- 3.Brabin B J. An analysis of malaria in pregnancy in Africa. Bull W H O. 1983;61:1005–1016. [PMC free article] [PubMed] [Google Scholar]
- 4.Bray R S, Sinden R E. The sequestration of Plasmodium falciparum infected erythrocytes in the placenta. Trans R Soc Trop Med Hyg. 1979;73:716–719. doi: 10.1016/0035-9203(79)90028-2. [DOI] [PubMed] [Google Scholar]
- 5.Bulmer J N, Rasheed F N, Morrison L, Francis N, Greenwood B M. Placental malaria. II. A semi-quantitative investigation of the pathological features. Histology. 1993;22:219. doi: 10.1111/j.1365-2559.1993.tb00111.x. , 603–609. [DOI] [PubMed] [Google Scholar]
- 6.Desakorn V, Silamut K, Angus B, Sahassananda D, Chotivanich K, Sunthatasamai P, Simpson J, White N J. Semi-quantitative measurement of Plasmodium falciparum antigen PfHRP2 in blood and plasma. Trans R Soc Trop Med Hyg. 1997;91:479–483. doi: 10.1016/s0035-9203(97)90292-3. [DOI] [PubMed] [Google Scholar]
- 7.Desowitz R S, Alpers M P. Placental Plasmodium falciparum parasitemia in East Sepik (Papua New Guinea) women of different parity: the apparent absence of acute effects on mother and foetus. Ann Trop Med Parasitol. 1992;86:95–102. doi: 10.1080/00034983.1992.11812638. [DOI] [PubMed] [Google Scholar]
- 8.Fried M, Muga R O, Misore A O, Duffy P E. Malaria elicits type 1 cytokines in the human placenta: IFN-gamma and TNF-alpha associated with pregnancy outcomes. J Immunol. 1998;160:2523–2530. [PubMed] [Google Scholar]
- 9.Garcia M, Kirimoama S, Marlborough D, Leafasia J, Rieckmann K H. Immunochromatographic test for malaria diagnosis. Lancet. 1996;347:1549. doi: 10.1016/s0140-6736(96)90700-x. [DOI] [PubMed] [Google Scholar]
- 10.Gaye O, Diouf M, Dansokho E F, McLaughlin G, Diallo S. Diagnosis of Plasmodium falciparum malaria using ParaSight F, ICT malaria Pf and malaria IgG CELISA assays. Parasitology. 1998;5:189–192. doi: 10.1051/parasite/1998052189. [DOI] [PubMed] [Google Scholar]
- 11.Howard R J, Uni S, Aikawa M, Aley S B, Leech J H, Lew A M, Wellems T E, Rener J, Taylor D W. Secretion of a malarial histidine-rich protein (PfHRP II) from Plasmodium falciparum-infected erythrocytes. J Cell Biol. 1986;103:1269–1277. doi: 10.1083/jcb.103.4.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leopardi O, Naughten W, Salvia L, Colecchia M, Matteelli A, Zucchi A, Shein A, Muchi J A, Carosi G, Ghione M. Malaric placentas. A quantitative study and clinico-pathological correlations. Pathol Res Pract. 1996;192:892–898. doi: 10.1016/S0344-0338(96)80068-9. [DOI] [PubMed] [Google Scholar]
- 13.McGregor I A. Epidemiology, malaria and pregnancy. Am J Trop Med Hyg. 1984;33:517–525. doi: 10.4269/ajtmh.1984.33.517. [DOI] [PubMed] [Google Scholar]
- 14.Menendez C. Malaria during pregnancy: a priority area of malaria research and control. Parasitol Today. 1995;11:178–183. doi: 10.1016/0169-4758(95)80151-0. [DOI] [PubMed] [Google Scholar]
- 15.Nansiripongsum V, Wilde H, Pamsandang P, Tiersansern P. Field study of an antigen-detection ELISA specific for Plasmodium falciparum. Trans R Soc Trop Med Hyg. 1993;87:32–34. doi: 10.1016/0035-9203(93)90410-r. [DOI] [PubMed] [Google Scholar]
- 16.Parra M E, Evans C B, Taylor D W. Identification of Plasmodium falciparum histidine-rich protein 2 in the plasma of humans with malaria. J Clin Microbiol. 1991;29:1629–1634. doi: 10.1128/jcm.29.8.1629-1634.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Payne D. Use and limitations of light microscopy for diagnosing malaria at the primary health care level. Bull W H O. 1988;66:621–626. [PMC free article] [PubMed] [Google Scholar]
- 18.Pieroni P, Mills C D, Ohrt C, Harrington M A, Kain K C. Comparison of the ParaSight-F test and the ICT malaria PF test with the polymerase chain reaction for the diagnosis of Plasmodium falciparum malaria in travelers. Trans R Soc Trop Med Hyg. 1998;92:166–169. doi: 10.1016/s0035-9203(98)90730-1. [DOI] [PubMed] [Google Scholar]
- 19.Rock E P, Marsh K, Saul A L, Wellems T E, Taylor D W, Maloy W L, Howard R J. Comparative analysis of the Plasmodium falciparum histidine-rich proteins, HRP-I, HRP-II and HRP-III in malaria parasites of diverse origin. Parasitology. 1987;95:209–227. doi: 10.1017/s0031182000057681. [DOI] [PubMed] [Google Scholar]
- 20.Shiff C J, Premji Z, Minjas J N. The rapid manual ParaSight-F test. A new diagnostic tool for Plasmodium falciparum infection. Trans R Soc Trop Med Hyg. 1993;87:646–648. doi: 10.1016/0035-9203(93)90273-s. [DOI] [PubMed] [Google Scholar]
- 21.Singh N, Singh M P, Sharma V P. The use of a dipstick antigen-capture assay for the diagnosis of Plasmodium falciparum infection in a remote forested area of central India. Am J Trop Med Hyg. 1997;56:188–191. doi: 10.4269/ajtmh.1997.56.188. [DOI] [PubMed] [Google Scholar]
- 22.Snounou G, Viriyakosol S, Jarra W, Thaithong S, Brown K N. Identification of the four human parasite species in field samples by the polymerase chain reaction and detection of a high prevalence of mixed infections. Mol Biochem Parasitol. 1993;58:283–292. doi: 10.1016/0166-6851(93)90050-8. [DOI] [PubMed] [Google Scholar]
- 23.Snounou G, Viriyakosol S, Zhu P, Jarra W, Pinheiro L, do Rosario V E, Thaithong S, Brown K N. High sensitivity of detection of human malaria parasites by the use of the nested polymerase chain reaction. Mol Biochem Parasitol. 1993;61:315–320. doi: 10.1016/0166-6851(93)90077-b. [DOI] [PubMed] [Google Scholar]
- 24.Taylor D W, Voller A. The development and validation of a simple antigen detection ELISA for Plasmodium falciparum malaria. Trans R Soc Trop Med Hyg. 1993;87:29–31. doi: 10.1016/0035-9203(93)90409-j. [DOI] [PubMed] [Google Scholar]
- 25.Uguen C, Rabodonirina M, De Pina J J, Vigier J P, Martet G, Maret M, Peyron F. ParaSight-F rapid manual diagnostic test of Plasmodium falciparum infection. Bull W H O. 1995;73:643–649. [PMC free article] [PubMed] [Google Scholar]
- 26.Voller A, Bidwell D E, Chiodini P L. Evaluation of a malaria antigen ELISA. Trans R Soc Trop Med Hyg. 1994;88:188. doi: 10.1016/0035-9203(94)90289-5. [DOI] [PubMed] [Google Scholar]
- 27.Walter P R, Garin Y, Blot P. Placental pathologic changes in malaria. A histologic and ultrastructural study. Am J Pathol. 1982;109:330–342. [PMC free article] [PubMed] [Google Scholar]
- 28.Wellems T E, Rock E P, Maloy W L, Taylor D W, Howard R J. Histidine-rich proteins in Plasmodium falciparum: an update and perspective. UCLA Symp Mol Cell Biol New Ser. 1986;42:47–58. [Google Scholar]
- 29.World Health Organization. 1986. WHO expert committee on malaria, 18th report. WHO Tech. Rep. Ser. 735. [PubMed]
- 30.Yamada M, Steketee R, Abramowsky C, Kida M, Wirima J, Heymann D, Rabbege J, Berman J, Aikawa M. Plasmodium falciparum associated placental pathology: a light and electron microscopic and immunohistological study. Am J Trop Med Hyg. 1989;41:161–168. doi: 10.4269/ajtmh.1989.41.161. [DOI] [PubMed] [Google Scholar]