Abstract
Introduction
Despite the abundance of existing literature on evidence-based nursing practice, knowledge regarding evidence-based leadership, that is, leadership supported by an evidence-based approach, is lacking. Our aim is to conduct a mixed-methods systematic review with qualitative and quantitative studies to examine how evidence is used to solve leadership problems and to describe the measured and perceived effects of evidence-based leadership on nurses and nurse leaders and their performance as well as on organisational and clinical outcomes.
Methods and analysis
We will search the following databases with no year limit or language restrictions: CINAHL (EBSCO), Cochrane Library, Embase (Elsevier), PsycINFO (EBSCO), PubMed (MEDLINE), Scopus (Elsevier) and Web of Science. In addition, the databases for prospectively registered trials and other systematic reviews will be screened. We will include articles using any type of research design as long as the study includes a component of an evidence-based leadership approach. Three reviewers will independently screen all titles, abstracts and full-text articles and two reviewers will extract the data according to the appropriate checklists. The quality of each study will be appraised using specific appraisal tool fitting in study design used in each study. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) grid, PRISMA Protocols, Synthesis Without Meta-analysis and ENTREQ will guide the study process and reporting. Outcomes related to individual or group performance of nurses or nurse managers regarding leadership skills (e.g., communication skills), organisational outcomes (e.g., work environment, costs) and clinical outcomes (e.g., patient quality of life, treatment satisfaction) will be extracted and synthesised.
Ethics and dissemination
This systematic review will not include empirical data, and therefore, ethics approval will not be sought. The results of the review will be disseminated in a peer-reviewed scientific journal and in a conference presentation.
PROSPERO registration number
CRD42021259624.
Keywords: organisational development, protocols & guidelines, health services administration & management, quality in health care
Strengths and limitations of this study.
This mixed-methods systematic review is justified by the lack of synthesised knowledge on impacts of evidence-based leadership in nursing, an issue that is needed to answer current challenges in healthcare.
A comprehensive literature search using several electronic databases and a manual search will be supplemented.
To ensure transparent and complete reporting, the protocol has been written following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols guidelines.
To promote the dissemination and the use of evidence produced, the review findings will be validated in collaboration with nursing associations.
Introduction
The nursing profession has an important role in addressing current and future health needs.1 Today, around 20 million nurses make up nearly half of the global health workforce,2 and still, 5.9 million more nurses will be needed in the future to meet the global demand.3 In improving global health, effective leadership is one of the contributions of nurses,3 and therefore, nurses must be empowered and enabled to lead to fulfil global requirements.4 However, nurse leaders often lack skills in refined problem solving and decision making,5 and their decisions are based on experience, intuition6 7 or personal views.8 Inconclusive, poor-quality or non-representative information can further lead to inappropriate and costly care decisions that impact organisations, staff and patients.9–11
The Royal College of Nursing12 has emphasised the role of leadership in promoting direction, alignment and commitment among teams and organisations. Therefore, leadership requires the ability to understand the situation that needs changing, the ability to communicate and adapt to new behaviours and the ability to secure resources that will help goals be met.13 For these requirements, evidence-based knowledge has an impactful role.14 A large knowledge base already exists related to leadership among different professionals in healthcare.15–18 Previous literature reviews have also focused on the roles and behaviours of leaders in implementing evidence-based knowledge into clinical practice16–19 as well as how leaders can inhibit nurses’ competency and knowledge management in the organisation.20 More recently, literature reviews have focused on how evidence has been used by leaders themselves to solve managerial problems in healthcare. In this task, evidence-based management (EBMgt), defined as how the best available scientific evidence is used, has been incorporated in making managerial decisions. Four elements in practising EBMgt are crucial: external scientific evidence, practitioner’s experience and judgement, stakeholders’ preferences or values, and different contexts and organisational factors.14 21
We systematically searched and found six reviews related to leadership and an evidence-based approach. Young22 focused on definitions and acceptance of EBMgt in healthcare, while Hasanpoor et al23 identified facilitators and barriers, sources of evidence used and the role of evidence in the process of decision making. Both reviews22 23 concluded that EBMgt was emphasised but limitedly used. Other identified problems included a lack of time and a lack of research on management activities, and policy constraints.22 Roshanghalb et al24 concluded that leaders based their decisions mainly on published studies, real-world evidence and experts’ opinions, while Jaana et al25 found that systematic reviews and meta-analyses rarely provided evidence of management-related interventions. In addition, Tate et al10 reviewed the effectiveness of interventions in enhancing leaders’ use of research evidence.
Despite the wide range of existing literature related to an evidence-based approach used by leaders in healthcare contexts, as far as we are aware, the concept of evidence-based leadership has only been used in one review, by Geerts et al,9 who focused on physician leadership development interventions. Therefore, a clear knowledge gap can be identified in the literature regarding how an evidence-based approach could be used to support the role of nurse leaders and what the impact of the evidence is on nurses and nurse leaders themselves as well as on clinical practice and organisational outcomes. This topic is important as EBMgt is already considered to produce the best professional practice.26 However, healthcare leaders in nursing have somehow escaped the call for the use of evidence in their own practice.8 Nurse leaders do not use research evidence in their management practice,10 and they acknowledge personal27 and professional experience26 over research evidence. Evidence-based knowledge in the context of leadership is still important, not only in supporting research or clinical practice but also in guiding management and leadership decisions.9 Therefore, the time has come for nursing leaders to join clinicians in using the strongest evidence available to effect change and guide decision making.28
To promote leadership in nursing,2 we postulate that evidence-based approaches should be used in supporting leadership in nursing.8 To answer the global call for nurses,1 3 this systematic review aims to examine how evidence is used to solve leadership problems and to describe the measured and perceived effects of evidence-based leadership on nurses and nurse leaders and their performance, as well as organisational and clinical outcomes. We will use a mixed-methods approach by combining both qualitative and quantitative studies to provide greater insights into the available literature29 and synthesise the existing knowledge on how evidence is used to solve leadership problems and support leadership in daily nursing practice, and what the impact of the evidence-based leadership style is. The information to be gained by using rigorous research methods is needed for developing nursing leadership practices in the future. As the American Nurses Association has stated, registered nurses should demonstrate leadership in their profession, and therefore, nurses’ leadership competences should be strengthened.30 Our review can direct education efforts for nurse leaders toward more effective leadership styles. The ability of nurse leaders to use and critically appraise research evidence may influence the way policy is enacted and how resources and staff are used to meet certain objectives set by policy, which can influence staff and workforce outcomes.10 The information of this systematic review could, therefore, be used to inform service provisions of the best investment methods for the future nursing workforce. Further, the review could provide direction for researchers in choosing their future research topics to fill the knowledge gap in the effectiveness of evidence-based leadership styles. We, therefore, expect that this systematic review will gain evidence that will benefit nursing leaders in healthcare organisations worldwide.
Study objectives
The overall aim of this mixed-methods systematic review is to examine how evidence is used to solve leadership problems and to describe the measured and perceived effects of evidence-based leadership on nurses and nurse leaders and their performance as well as organisational and clinical outcomes. The review questions are as follows: (1) What leadership problems are solved using an evidence-based approach? (2) What are the main features in evidence-based leadership? (3) What are the perceived effects of evidence-based leadership on nurses’ performance, organisational and clinical outcomes? (4) What are the measured effects of evidence-based leadership on nurses’ performance, organisational and clinical outcomes?
Methods and analysis
Design
In this review, we will use a mixed-methods approach29 combining narrative and quantitative synthesis to appraise and synthesise empirical evidence. In this approach, a comprehensive synthesis of two or more types of data is first performed and then aggregated into a combined synthesis.29 The approach is usable in our review as it provides the potential for gaining a more complete picture and holistic understanding of the topic; our review focuses on a wide range of questions, not only those relating to the effectiveness of a particular intervention but also to describe the existing situation.31
To ensure transparent and complete reporting, this review protocol is designed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA32) grid, PRISMA Protocols (PRISMA-P33), the guideline for Synthesis Without Meta-analysis (SWiM) items34 and the Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) statement.35
Eligibility criteria
Study design
Articles using any type of research design will be included as long as the study includes a topic of leadership and any component of an evidence-based leadership approach.
The population, intervention, comparison, outcome
The population, intervention, comparison, outcome approach will be used to specify the eligibility of studies.
Population (P): Articles should include nurses, nurse managers or other nursing staff working in a healthcare context. They can have an official or unofficial managerial role as leadership occurs whenever a person attempts to influence the behaviour of individuals or a group based on personal goals or for the goals of others congruent with organisational goals.13 Articles involving other healthcare professionals will be excluded if nurses are not clear majority (50% or more) in the sample.
Intervention (I): Leadership refers to the process of when a person attempts to influence the behaviour of individuals or a group in an organisation for any reason,13 while evidence-based leadership is when the behaviour of individuals or a group is affected using an evidence-based approach. We propose that evidence-based leadership is analogous to EBMgt,14 21 but the role or position of the leader may not always be assigned or officially approved of by the organisation.
We assume that evidence-based leadership is a process that includes the following steps: (1) a practitioner identifies a clearly stated leadership problem, question or issue in their practice, (2) organisational evidence or data about the leadership problem or issue are collected and analysed to check for relevance and validity, and the problem is restated, reformulated or made more specific, (3) scientific evidence from published research about the leadership problem is identified and critically appraised, (4) the views of stakeholders (patients, clinicians, family members, etc.) are considered, together with ethical implications of the decision and (5) all sources of information are critically appraised.36 The articles to be included in this review should identify some or all of the five steps of the evidence-based practice process.37 38
Comparison (C): If an included study has used a randomised trial design, we will include another type of intervention as a comparison.
Outcomes
Studies will describe any outcomes related to individual or group performance of nurses or nurse managers regarding leadership skills (e.g., communication skills), organisational outcomes (e.g., work environment, costs), healthcare provider outcomes (e.g., job satisfaction) or clinical outcomes (e.g., patient quality of life, treatment satisfaction).
Other
Articles will be limited to peer-reviewed, published full-text articles. There will be no language restriction. Theoretical papers, statistical reviews, books and book chapters, letters, dissertations, editorials and study protocols will be excluded.
Data sources
A comprehensive literature search, with no specific year limits, will be conducted. The following electronic databases will be used: CINAHL (EBSCO), Cochrane Library (academic database for medicine and health science and nursing), Embase (Elsevier), PsycINFO (EBSCO), PubMed (MEDLINE), Scopus (Elsevier) and Web of Science (academic database across all scientific and technical disciplines, ranging from medicine and social sciences to arts and humanities). These databases will allow for a wide literature search within our review topic. The reference lists of the selected papers will also be screened for additional studies. If a high number of studies are found using a hand search, the search strategy will be modified.39
Search strategy
The search strategy will be elaborated on and implemented prior to the study selection. We will use the PRISMA-P checklist for guidance as well as a controlled vocabulary thesaurus (such as medical subject heading terms, CINAHL headings, PsycINFO thesaurus). The keywords for each database are ‘nurse leader’ or similar terms that describe a nurse’s position as a leader, manager or administrator; ‘evidence-based leadership’ or similar terms that describe practice as being founded on evidence; and ‘leadership’ and its synonyms and other similar terms that describe the actions of nurse leaders. Each keyword has been verified for each database.
The search terms will be combined using the Boolean operators ‘AND’ and ‘OR’. Advice on using keywords to search for studies has been sought from a librarian of the faculty of medicine at the University of Turku. Full search strategies to be used across databases are described in online supplemental file.
bmjopen-2021-055356supp001.pdf (34.8KB, pdf)
Data management
A reference management software will be used to efficiently manage records, document the process and manage duplicate study papers.
Selection process
The study selection process will consist of four steps (figure 1).32 First, titles and abstracts will be independently assessed by three authors (MAV, KH and TL) according to the inclusion criteria. Second, the abstracts of the papers will be screened for relevance and eligibility, by the same three authors (MAV, KH and TL). Third, the full texts of the selected abstracts will be obtained. If access to any full-text article is lacking, we will contact the study authors to obtain the full text or the findings of the study. All full-text articles will then be screened by three authors (MAV, KH and XL) according to the inclusion and exclusion criteria. In cases of discrepancy between the three screening authors, the paper will be discussed with another author (TL). Papers that do not meet the inclusion criteria will be rejected, and the reason for exclusion will be recorded to increase transparency in the selection process. Fourth, the full texts of the studies that meet the inclusion criteria will be obtained for further detailed assessment. The reference lists of the selected papers will also be screened and checked for additional papers that meet the inclusion criteria (JV and GL).
Figure 1.
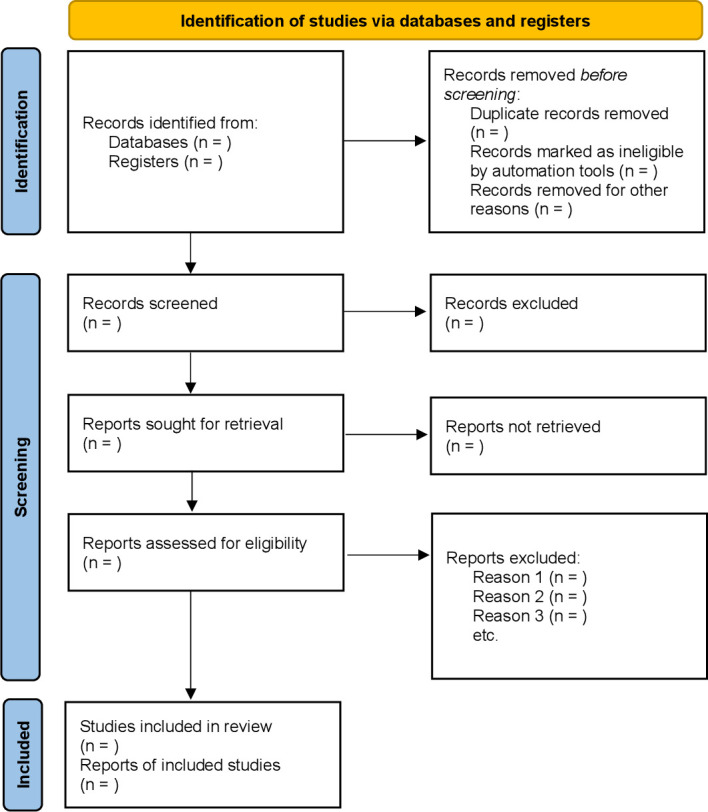
PRISMA flow chart.32 PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Data collection and extraction process
To answer the review questions, specific tables will be created to collect data from selected papers. The effectiveness data will be extracted by three authors (TL, MAV and WC) and the tabled extractions will be reviewed for completeness and accuracy by another author (XL).
Qualitative data to answer the research questions will be extracted from papers included in the review using the standardised data extraction tool from JBI-QARI (Qualitative Assessment and Review Instrument).29 The data extracted will include outcomes significant to the review question and the specific objectives.
Quantitative data will be extracted from papers included in the review using the standardised data extraction tool from JBI-MAStARI (Meta Analysis of Statistics Assessment and Review Instrument).29 The data extracted will include specific details about each study. Details of the evidence-based leadership interventions will be extracted following the TIDIeR (Template for Intervention Description and Replication) checklist40: brief name; why the intervention is essential; materials and procedures; providers and their expertise; models of delivery; location and infrastructure; sessions; tailoring; modifications; planned and actual adherence or fidelity. The intervention data will be extracted by two authors (JV and KH). If available, economic data will be extracted from papers included in the review using the standardised data extraction tool from JBI-ACTUARI (Analysis of Cost, Technology and Utilisation Assessment and Review Instrument).29
Relevant results from included papers will be extracted and inputted into predesigned tables by three authors (YT, SH and WC); the process will be validated with the following steps with the guidance of MAV. First, at the beginning of the extraction process, the authors (YT, SH and WC) will familiarise themselves with study data. Second, the three authors will independently extract data from the first five studies using the preprepared tables. Third, the authors will meet to discuss and determine whether their approaches to data extraction are consistent with each other’s extraction, the research question and the purpose of the review. Fourth, the data extraction form will be refined if any uncertainties are found. The authors will again review a study as many times is necessary to achieve common agreement within this stage.41
Risk of bias in individual studies
The quality of each study will be appraised using different appraisal tools selected based on the study design used in the specific study. Qualitative studies will be assessed using the Critical Appraisal Skills Programme checklists for qualitative research.42 The quantitative studies will be assessed using the Strengthening the Reporting of Observational Studies in Epidemiology checklist for cohort, case–control and cross-sectional studies,43 while the Cochrane Collaboration’s tool for assessing risk of bias in randomised trials will be used to assess the quality of randomised trial articles included in the review.44 In addition, the mixed-methods studies will be appraised using the Mixed Methods Appraisal Tool.45 Three reviewers (YT, SH and XL) will conduct the assessment. Any disagreement between the reviewers will be resolved by discussion or by requesting the assessment of a fourth reviewer (XL).
Data synthesis
In this mixed-methods systematic review, we will use segregated methodology, in which the qualitative, quantitative and economic data are synthesised separately prior to reaching mixed-methods synthesis.46 First, to form a clear descriptive summary of the included studies, a narrative synthesis will be conducted by summarising the tabulated study details. The content of each study will also be summarised to answer the descriptive review objectives.47 With narrative synthesis we are referring to a synthesis of findings from multiple studies that relies primarily on textual approach and the use of words and text to summarise and explain the findings from the included studies.48 Narrative synthesis of effectiveness data will also be used if statistical meta-analysis is not possible or advisable.49 The methods used to synthesise the effects for each outcome and assess the certainty of the synthesis findings will be described and justified when it is not possible to undertake a meta-analysis of effect estimates. This descriptive process will be conducted explicitly and rigorously. Decisions on how to group and synthesise tabulated data will be made based on the review protocol, review questions, and with the support of existing guidelines on how to synthetise and report qualitative systematic reviews (SWiM,34 ENTREQ35). Second, a statistical meta-analysis based on the randomised controlled trial (RCT) studies will be conducted only if the usable data is available. The Grading of Recommendations Assessment, Development and Evaluation will be used to evaluate the quality of evidence.50 Further, economic findings, where possible, will be pooled using JBI-ACTUARI29 and presented in a tabular summary. If this is not possible, findings will be presented in narrative form only. Finally, in a mixed-methods synthesis, qualitative findings will be used to contextualise the meta-analytical results and generate possible reasons behind the quantitative data, when usable.29
To add to the rigorousness of the review, the results will be validated in close collaboration with national and international nursing associations. This will, in turn, offer additional sources of information, perspectives, meaning and applicability to the review results.51 We will invite appropriate stakeholders, around 10–20 nurses or nurse leaders, to take part in the survey. We will first share with them the review results and then ask them to answer the prespecified open-ended questions in written format; the responses will be analysed using content analysis. The stakeholders will then be invited to join a face-to-face meeting to discuss the summary of the feedback. The conclusion of the validation process will be integrated into the review outcomes by reporting the experience in the discussion part of the review. We assume that sharing the preliminary review results with stakeholders is necessary to achieve a higher level of meaning in our review results, support the feedback from the content experts, and offer new perspectives on our preliminary findings.41 We also believe that the validation of the results will offer an ideal mechanism for enhancing the validity of the study outcome while translating the findings for the global audience.
Patient and public involvement
There will be no patient or public involvement in the study.
Ethics and dissemination
No data collection for the systematic review will involve human subjects, and therefore, no ethical approval will be required. The results will be disseminated in a peer-reviewed journal and in a conference presentation.
Discussion
In the course of a decade, the call for evidence has swept the healthcare landscape in medicine and more recently in nursing. As the future of nursing success depends on strong leaders, nurses need to feel secure in their leadership and have confidence that their managers are reliable and educated about the best ways to manage situations.8 Good leadership in health organisations has the potential to positively impact employees’ well-being, for example, an increase in work engagement and a decrease in exhaustion and turnover intention.52 This is highly important as the existing nursing shortage, the ageing of the nursing workforce, and the COVID-19 pandemic has created an alarming situation in healthcare settings globally. The International Council of Nurses has already estimated that up to 13 million nurses will be needed to fill the future global nurse shortage gap.53 Strong evidence-based leadership in nursing is therefore needed more than ever before. Therefore, to attract new generations of nurses to the healthcare business, and to cost-effectively run healthcare organisations, nursing leaders who base their leadership decisions on the best available evidence are needed. Therefore, in this systematic review, we will examine how evidence is used to solve leadership problems and describe the measured and perceived effects of evidence-based leadership on nurses and nurse managers’ performance, organisational and clinical outcomes.
Our systematic review may also include shortcomings and limitations, which need to be taken into account. First, despite a wide search strategy, we may miss studies not included in the major international databases. This could potentially result in less generalisable findings outside of the English language. We also predict that it is not possible to conduct a meta-analysis to reveal the effectiveness of evidence-based leadership if the designs of the studies are too different or if the outcomes measured are not sufficiently similar for an average result across the studies to be meaningful, or if there are concerns about the quality of the studies.54 We may also find a limited number of studies in which all—or even few—of the elements of an evidence-based approach are used. Despite the possible limited number of RCT studies from which to pool quantitative evidence, we still assume that using a narrative synthesis will provide good groundwork for the topic to be used to satisfy future needs in the nursing workforce. On the other hand, our narrative synthesis can hypothetically be biased, especially if selected results are over emphasised without clear justification or the conclusions are made based on subjective interpretations due to a lack of transparency in how the data were presented and how the conclusions were reached in the systematic reviews.55 Other risks in our data synthesis could be a lack of description of the methods used, unclear links between the included data, the synthesis, and the conclusions, and inadequate reporting of the limitations of the synthesis.34
To avoid possible methodological shortcomings, a rigorous data synthesis will be conducted. Our proposed protocol is registered with predefined methods to add transparency and reliability of our review results; a review registration is still lacking in many previous reviews.56 Our review process and its reporting are guided by rigorous guidelines such as PRISMA, PRISMA-P, SWiM and ENTREQ. The results will be stronger and more complete than those of other reviews in terms of a comprehensive literature search. Our systematic review is also strengthened by a mixed-methods approach combining a narrative synthesis and meta-analysis, which both appear to make different contributions to a systematic review and add meaning and value to the findings.29 In addition, the results of the review might have an added value compared with previous systematic reviews concerning leadership and an evidence-based approach, as most existing systematic reviews describe the role of nurse leaders in implementing and maintaining evidence-based nursing. Therefore, our mixed-methods review will fill the gap regarding how nurse leaders themselves use evidence to guide their leadership role and what the measured and perceived impact of evidence-based leadership is in nursing.
Amendments
Any amendments to this protocol will be documented.
Planned start and end date
The review is planned to start on 1 January 2022 and end on 30 June 2022.
Supplementary Material
Acknowledgments
We would like to thank the Central South University, Xiangya School of Nursing and the University of Turku, Department of Nursing Science about their support for the protocol preparation.
Footnotes
Contributors: MAV: conception (generator of the review) and responsible for the study design, identifying preliminary literature for the background, writing the manuscript; TL: identifying preliminary literature for the background, planning search strategy for papers, writing the manuscript; KH: identifying preliminary literature for the background, planning search strategy for papers, writing the manuscript; JV: search strategy for papers, commenting on the manuscript; GL: commenting on the manuscript; YT: commenting on the manuscript; WC: commenting on the manuscript; SH: commenting on the manuscript; XL: conception and commenting on the manuscript.
Funding: The work was supported by the Finnish National Agency of Education, Asia Programme, grant number 26/270/2020 and University of Turku (internal fund 26003424).
Disclaimer: The funders had no role in the study design and will not have any role during its execution, analysis, interpretation of the data, decision to publish, or preparation of the manuscript.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.National Academy of Medicine . The future of nursing 2020-2030: charting a path to achieve health equity: a consensus study from the National Academy of medicine, 2021. Available: https://nam.edu/publications/the-future-of-nursing-2020-2030/ [Accessed 15 Apr 2021].
- 2.The Lancet . 2020: unleashing the full potential of nursing. Lancet 2019;394:1879–9. 10.1016/S0140-6736(19)32794-1 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . Nursing and midwifery, 2020. Available: https://www.who.int/news-room/fact-sheets/detail/nursing-and-midwifery [Accessed 15 Apr 2021].
- 4.Nkengasong JN, Raji T, Ferguson SL, et al. Nursing leadership in Africa and health security. EClinicalMedicine 2021;36:100930. 10.1016/j.eclinm.2021.100930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miltner RS, Jukkala A, Dawson MA, et al. Professional development needs of nurse managers. J Contin Educ Nurs 2015;46:252–8. 10.3928/00220124-20150518-01 [DOI] [PubMed] [Google Scholar]
- 6.Dever KH. Through the eyes of nurse managers in long-term care: identifying perceived competencies and skills. J Gerontol Nurs 2018;44:32–8. 10.3928/00989134-20180322-01 [DOI] [PubMed] [Google Scholar]
- 7.Effken JA, Verran JA, Logue MD, et al. Nurse managers' decisions: fast and favoring remediation. J Nurs Adm 2010;40:188–95. 10.1097/NNA.0b013e3181d40f7c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shingler-Nace A, Gonzalez JZ. Ebm: a pathway to evidence-based nursing management. Nursing 2017;47:43–6. 10.1097/01.NURSE.0000510744.55090.9a [DOI] [PubMed] [Google Scholar]
- 9.Geerts JM, Goodall AH, Agius S. Evidence-based leadership development for physicians: a systematic literature review. Soc Sci Med 2020;246:112709. 10.1016/j.socscimed.2019.112709 [DOI] [PubMed] [Google Scholar]
- 10.Tate K, Hewko S, McLane P, et al. Learning to lead: a review and synthesis of literature examining health care managers' use of knowledge. J Health Serv Res Policy 2019;24:57–70. 10.1177/1355819618786764 [DOI] [PubMed] [Google Scholar]
- 11.Kyratsis Y, Ahmad R, Hatzaras K. Making sense of evidence in management decisions: the role of Research-Based knowledge on innovation adoption and implementation in health care. Southampton: NIHR Journals Library, 2014. [PubMed] [Google Scholar]
- 12.Royal College of Nursing . Leadership, 2021. Available: https://www.rcn.org.uk/clinical-topics/clinical-governance/leadership [Accessed 15 Apr 2021].
- 13.Hersey P, Campbell R. Leadership: a behavioral science approach. CA: Leadership Studies Publishing, 2004. [Google Scholar]
- 14.Briner RB, Denyer D, Rousseau DM. Evidence-based management: concept Cleanup time? Acad Manag Perspect 2009;23:19–32. 10.5465/amp.23.4.19 [DOI] [Google Scholar]
- 15.Reed BN, Klutts AM, Mattingly TJ. A systematic review of leadership definitions, competencies, and assessment methods in pharmacy education. Am J Pharm Educ 2019;83:7520. 10.5688/ajpe7520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berghout MA, Fabbricotti IN, Buljac-Samardžić M, et al. Medical leaders or masters?-A systematic review of medical leadership in hospital settings. PLoS One 2017;12:e0184522. 10.1371/journal.pone.0184522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanks S, Cotton D, Spowart L. Leadership in dental practice: a three stage systematic review and narrative synthesis. J Dent 2020;102:103480. 10.1016/j.jdent.2020.103480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reichenpfader U, Carlfjord S, Nilsen P. Leadership in evidence-based practice: a systematic review. Leadersh Health Serv 2015;28:298–316. 10.1108/LHS-08-2014-0061 [DOI] [PubMed] [Google Scholar]
- 19.Gifford WA, Squires JE, Angus DE, et al. Managerial leadership for research use in nursing and allied health care professions: a systematic review. Implement Sci 2018;13:127. 10.1186/s13012-018-0817-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lunden A, Teräs M, Kvist T, et al. A systematic review of factors influencing knowledge management and the nurse leaders' role. J Nurs Manag 2017;25:407–20. 10.1111/jonm.12478 [DOI] [PubMed] [Google Scholar]
- 21.Goodman JS, Gary MS, Wood RE. Bibliographic search training for evidence-based management education: a review of relevant literatures. AMLE 2014;13:322–53. 10.5465/amle.2013.0188 [DOI] [Google Scholar]
- 22.Young SK. Evidence-Based management: a literature review. J Nurs Manag 2002;10:145–51. 10.1046/j.1365-2834.2002.00309.x [DOI] [PubMed] [Google Scholar]
- 23.Hasanpoor E, Hajebrahimi S, Janati A, et al. Barriers, facilitators, process and sources of evidence for evidence-based management among health care managers: a qualitative systematic review. Ethiop J Health Sci 2018;28:665–80. 10.4314/ejhs.v28i5.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roshanghalb A, Lettieri E, Aloini D, et al. What evidence on evidence-based management in healthcare? MD 2018;56:2069–84. 10.1108/MD-10-2017-1022 [DOI] [Google Scholar]
- 25.Jaana M, Vartak S, Ward MM. Evidence-based health care management: what is the research evidence available for health care managers? Eval Health Prof 2014;37:314–34. 10.1177/0163278713511325 [DOI] [PubMed] [Google Scholar]
- 26.Guo R, Berkshire SD, Fulton LV, et al. Use of evidence-based management in healthcare administration decision-making. Leadersh Health Serv 2017;30:330–42. 10.1108/LHS-07-2016-0033 [DOI] [PubMed] [Google Scholar]
- 27.Liang ZZ, Howard PP, Rasa JJ. Evidence-Informed managerial decision-making: what evidence counts? Asia Pac J Health Manag 2011;6:23–9. [Google Scholar]
- 28.Williams LL. What goes around comes around: evidence-based management. Nurs Adm Q 2006;30:243–51. 10.1097/00006216-200607000-00009 [DOI] [PubMed] [Google Scholar]
- 29.Joanna Briggs Institute . Joanna Briggs Institute reviewers’ manual: 2014 edition, 2014. Available: https://nursing.lsuhsc.edu/JBI/docs/ReviewersManuals/Mixed-Methods.pdf [Accessed 15 Apr 2021].
- 30.American Nurses Association . Ana leadership competency model, 2018. Available: https://www.nursingworld.org/~4a0a2e/globalassets/docs/ce/177626-ana-leadership-booklet-new-final.pdf [Accessed 15 Apr 2021].
- 31.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J 2009;26:91–108. 10.1111/j.1471-1842.2009.00848.x [DOI] [PubMed] [Google Scholar]
- 32.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 34.Campbell M, McKenzie JE, Sowden A, et al. Synthesis without meta-analysis (swim) in systematic reviews: reporting guideline. BMJ 2020;368:l6890. 10.1136/bmj.l6890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012;12:181. 10.1186/1471-2288-12-181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barends E, Rousseau DM, Briner RB. Evidence-Based management: the basic principles. The center for evidence-based management, 2014. Available: https://cebma.org/wp-content/uploads/Evidence-Based-Practice-The-Basic-Principles-vs-Dec-2015.pdf [Accessed 15 Apr 2021].
- 37.Ramis M-A, Chang A, Conway A, et al. Theory-based strategies for teaching evidence-based practice to undergraduate health students: a systematic review. BMC Med Educ 2019;19:267. 10.1186/s12909-019-1698-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sackett DL, Rosenberg WM, Gray JA, et al. Evidence based medicine: what it is and what it isn't. BMJ 1996;312:71–2. 10.1136/bmj.312.7023.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vassar M, Johnson AL, Sharp A, et al. Citation bias in otolaryngology systematic reviews. J Med Libr Assoc 2021;109:62–7. 10.5195/jmla.2021.736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vassar M, Page MJ, Glasbey J, et al. Evaluation of the completeness of intervention reporting in Cochrane surgical systematic reviews using the TIDieR-SR checklist: a cross-sectional study. BMJ Evid Based Med 2021;26:51–2. 10.1136/bmjebm-2020-111417 [DOI] [PubMed] [Google Scholar]
- 41.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Critical appraisal skills programme. CASP qualitative studies checklist, 2019. Available: https://casp-uk.net/casp-tools-checklists/ [Accessed 15 Aug 2021].
- 43.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344–9. 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 44.Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hong QN, Pluye P, bregues, S F. Mixed methods appraisal tool (MMAT) version 2018: user guide. Available: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf [Accessed 15 Aug 2021].
- 46.Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis studies. Res Sch 2006;13:29. [PMC free article] [PubMed] [Google Scholar]
- 47.Centre for Reviews and Dissemination . Systematic reviews: CRD’s guidance for undertaking reviews in healthcare, 2009. Available: https://www.york.ac.uk/media/crd/Systematic_Reviews.pdf [Accessed 15 Apr 2021].
- 48.Popay JH, Roberts A, Sowden M. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC methods programme, 2006. Available: https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf [Accessed 15 Apr 2021].
- 49.Rodgers M, Sowden A. Testing methodological guidance on the conduct of narrative synthesis in systematic reviews: effectiveness of interventions to promote smoke alarm ownership and function. Evaluation 2009;15:49–74. 10.1177/1356389008097871 [DOI] [Google Scholar]
- 50.Guyatt G, Oxman AD, Akl EA, et al. Grade guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383–94. 10.1016/j.jclinepi.2010.04.026 [DOI] [PubMed] [Google Scholar]
- 51.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 52.McKenna J, Jeske D. Ethical leadership and decision authority effects on nurses' engagement, exhaustion, and turnover intention. J Adv Nurs 2021;77:198–206. 10.1111/jan.14591 [DOI] [PubMed] [Google Scholar]
- 53.International Council of Nurses . The global nursing shortage and nurse retention: policy brief, 2021. Available: https://www.icn.ch/sites/default/files/inline-files/ICN%20Policy%20Brief_Nurse%20Shortage%20and%20Retention.pdf [Accessed 15 Apr 2021].
- 54.Cochrane Library . About Cochrane reviews, 2021. Available: https://www.cochranelibrary.com/about/about-cochrane-reviews [Accessed 15 Aug 2021].
- 55.Campbell M, Katikireddi SV, Sowden A, et al. Lack of transparency in reporting narrative synthesis of quantitative data: a methodological assessment of systematic reviews. J Clin Epidemiol 2019;105:1–9. 10.1016/j.jclinepi.2018.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tawfik GM, Giang HTN, Ghozy S, et al. Protocol registration issues of systematic review and meta-analysis studies: a survey of global researchers. BMC Med Res Methodol 2020;20:213. 10.1186/s12874-020-01094-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-055356supp001.pdf (34.8KB, pdf)


