Abstract
Background
Autistic spectrum disorder (ASD) is an increasingly recognised neurodevelopmental condition; that is, a neurologically‐based condition which interferes with the acquisition, retention or application of specific skills. ASD is characterised by challenges with socialisation and communication, and by stereotyped and repetitive behaviours. A stereotyped behaviour is one which is repeated over and over again and which seems not to have any useful function. ASD often co‐occurs with mental health disorders, including obsessive compulsive disorder (OCD). People with ASD may show certain cognitive differences (i.e. differences in ways of thinking) which influence their response to therapies. Thus, there is a need for evidence‐based guidelines to treat mental health issues in this group.
OCD, a common condition characterised by repeated obsessional thoughts and compulsive acts, occurs with greater frequency in persons with ASD than in the general population. Genetic, anatomic, neurobiological and psychological factors have been proposed to explain this co‐occurrence. However, care should be taken to distinguish stereotyped and repetitive behaviours characteristic of ASD from obsessive compulsive acts in OCD.
Cognitive behavioural therapy (CBT) is the recommended treatment for OCD, but studies have suggested that this treatment may be less effective in those with OCD co‐occurring with ASD. Hence, modifications to CBT treatment may be helpful when treating OCD co‐occurring with ASD to optimise outcomes.
Objectives
To assess the effectiveness of behavioural and cognitive behavioural therapy for obsessive compulsive disorder (OCD) in children and adults with autism spectrum disorder (ASD).
Search methods
We searched for studies in the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Embase, PsycINFO, five other bibliographic databases, international trial registries and other sources of grey literature (to 24 August 2020). We checked the reference lists of included studies and relevant systematic reviews to identify additional studies missed from the original electronic searches. We contacted subject experts for further information when needed.
Selection criteria
We included randomised controlled trials (RCTs), cross‐over, cluster‐ and quasi‐randomised controlled trials involving both adults and children with diagnoses of OCD and ASD. We included studies of participants with co‐occurring conditions (i.e. those experiencing other mental illnesses or neurodevelopmental conditions at the same time), but we did not include individuals who had a co‐occurring global learning difficulty. Treatment could be in any setting or format and include behavioural therapy (BT) and cognitive behavioural therapy (CBT), which may have been adapted for those with ASD. Comparator interventions included no treatment, waiting list, attention placebo (where the control group receives non‐specific aspects of therapy, but not the active ingredient) and treatment as usual (TAU, where the control group receives the usual treatment, according to accepted standards).
Data collection and analysis
Three review authors independently screened studies for inclusion. The authors extracted relevant data from the one eligible study, assessed the risk of bias and certainty of evidence (GRADE). Outcomes of interest were changes in OCD symptoms and treatment completion (primary outcome), and severity of depressive symptoms, anxiety symptoms and behavioural difficulties, as well as degree of family accommodation (secondary outcomes). We did not conduct meta‐analyses as only one study met the selection criteria.
Main results
We included only one RCT of 46 participants in our analysis. This study compared CBT for OCD in persons with high‐functioning ASD with a control group who received anxiety management only. There were no differences in rates of treatment completion between the CBT (87%) and anxiety management (87%) groups (risk ratio (RR) 1.00, 95% confidence interval (CI) 0.80 to 1.25; low‐certainty evidence). Behavioural difficulties were not included as an outcome measure in the study. This study showed that there may be a benefit at the end of treatment favouring CBT compared with anxiety management in OCD symptoms (mean difference (MD) ‐3.00, 95% CI ‐8.02 to 2.02), depression symptoms (MD ‐1.80, 95% CI ‐11.50 to 7.90), anxiety symptoms (MD ‐3.20, 95% CI ‐11.38 to 4.98), and quality of life (MD 5.20, 95% CI ‐1.41 to 11.81), but the evidence was of low certainty.
Authors' conclusions
Evidence is limited regarding the efficacy of CBT for treatment of OCD in ASD. There is much scope for future study, not only examining the efficacy of CBT for OCD in ASD, but also the particular ways that OCD manifests in and affects people with ASD and the role of the family in treatment response.
Plain language summary
Behavioural and cognitive behavioural therapy for obsessive compulsive disorder (OCD) in individuals with autism spectrum disorder (ASD)
Aim of the review
The aim of the review is to see if cognitive behavioural therapy (CBT) can help people who have OCD who also have ASD.
Background
People who have been given a diagnosis of ASD tend to have certain things in common. They often understand social interactions and communication differently to other people. People with ASD may also be less flexible in their thinking than other people, which may make it more difficult for them to use psychological therapies in the way that they are usually presented. The opinions of people with ASD are valuable in helping clinicians decide which research areas related to ASD should take priority.
Someone who has been diagnosed with OCD has certain symptoms which, to some extent, affect how they are able to get on with their lives. Someone with OCD has persistent thoughts, although they don't want the thoughts and often think that the thoughts are unreasonable. These thoughts are often worries about themselves or someone else being harmed or about something not being perfect or just right. Sometimes the person with OCD feels as if they have to think thoughts or do actions repeatedly to 'make things right', even though they often really know that they don't need to. The repeated actions might be something like washing their hands.
Research has shown that people with ASD are more likely to develop OCD. People may have certain genes that make them more likely to develop both ASD and OCD, or it may be that the way people with ASD tend to think makes them more likely to have OCD.
Cognitive behavioural therapy (CBT) has been used for a long time to treat OCD. CBT is usually carried out by visiting a therapist, but it can be delivered in different ways, such as online. CBT involves talking about the repeated thoughts that occur and helping the person manage and reduce them, and also involves trying to carry out compulsive actions less often. Because people with ASD sometimes have a different way of thinking and communicating, clinicians have wondered if CBT would be as useful to treat OCD in people with ASD as it is in people who have OCD but don't have ASD. Other researchers have devised ways to change the way that CBT is delivered to people with ASD to help them to get the most out of the treatment, and this is called 'adapted CBT'. Studies have shown that adapted CBT is useful for some anxiety disorders that occur in ASD. However, not as many studies have looked at how adapted CBT might be useful for OCD in people with ASD.
Search
We searched for randomised controlled trials of delivery of CBT to people with OCD who also had ASD. A randomised controlled trial is a trial where the participants are randomly allocated to CBT or another treatment group so that the people running the trial have no say about and do not know to which group the participants belong. The other treatment group is called the control group. In these studies, the people in the control group do not receive CBT, but they may have sessions with their therapists that do not include CBT, or they may be on a waiting list. If meeting with your therapist or waiting for time to pass were just as helpful as CBT, for example, then the results would be less likely to show a difference between the outcomes of the treatment group and the control group. Conversely, if CBT was more effective, then we might expect to see the CBT group doing better than the control group. Therefore, at the end of each trial, when the results in the treatment group are compared to the results in the control group, it gives information about how effective CBT might be for people with OCD and ASD. The evidence in this review is current to August 2020.
Conclusion
We found that there was only one published randomised controlled trial of delivery of CBT to people with OCD and ASD that met our search criteria. The control group in this trial was given a treatment called 'anxiety management' which helped the participants to manage anxiety but did not help them to deal specifically with repeated thoughts and actions, as CBT does. This study aimed to see if either anxiety management or CBT was better at treating OCD in people with ASD, but the study did not find a difference in response between the two treatments.
Summary of findings
Summary of findings 1. Cognitive behavioural therapy compared to anxiety management for obsessive compulsive disorder (OCD) in people with autism spectrum disorder (ASD).
| Cognitive behavioural therapy compared to anxiety management for obsessive compulsive disorder (OCD) in people with autism spectrum disorder (ASD) at post‐treatment | |||||
| Patient or population: obsessive compulsive disorder (OCD) in individuals with autism spectrum disorder (ASD) Setting: any settings (e.g. primary care, secondary care) Intervention: cognitive behavioural therapy (CBT) Comparison: anxiety management (AM) | |||||
| Outcomes Follow‐up | № of participants (studies) | Certainty of the evidence (GRADE) | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | |
| Risk with comparator | Risk difference with CBT intervention | ||||
| Treatment efficacy (change in OCD score), end of treatment. Measured by Y‐BOCs Score range: 0 to 40 (higher score = more severe symptoms) |
40 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | ‐ | The mean change in Y‐BOCs score in the comparator group was ‐4.3 | MD 3.00 lower (8.02 lower to 2.02 higher) |
| Total number of dropouts, end of treatment | 46 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | RR 1.00 (0.22 to 4.45) | Study population | |
| 130 per 1000 | 0 fewer per 1000 (29 fewer to 580 more) | ||||
| Quality of life, end of treatment Measured by WSAS Score range: 0 to 40 (higher score = higher disability) |
34 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | ‐ | The mean change in quality of life score in the comparator group was ‐0.7 | MD 5.2 higher (1.41 lower to 11.81 higher) |
| Severity of depressive symptoms, end of treatment Measured by BDI Score range: 0 to 63 (higher score = more severe symptoms) |
34 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | ‐ | The mean change in depressive symptoms score in the comparator group was 0.4 | MD 1.8 lower (11.5 lower to 7.9 higher) |
| Severity of anxiety symptoms, end of treatment Measured by BDI Score range: 0 to 63 (higher score = more severe symptoms) |
34 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | ‐ | The mean change in anxiety symptoms score in the comparator group was 0.6 | MD 3.2 lower (11.38 lower to 4.98 higher) |
| Behavioural difficulties, end of treatment | No data reported | No data reported | No data reported | No data reported | No data reported |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | |||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
aDowngraded one level: combination of domains with high risk and unclear risk of bias. bDowngraded one level: the 95% confidence interval crosses benefit and no benefit.
Background
Description of the condition
Autism spectrum disorder
ASD is common, and a prevalence of 0.9% was found in an American study of 310,000 children aged eight years (Rice 2009). Subsequent studies found higher prevalences: for example, 2016 data from the USA found a prevalence of 1.6% in children aged four years (Maenner 2020), and 1.85% in children aged eight years (Shaw 2020).
ASD covers a wide spectrum of functioning, from people who are able to function well in almost all areas of life, to those who may not fully achieve independent living. In the past, 'Asperger's syndrome' was a term used to denote individuals who were high functioning, although this term is now used less often. Studies often refer to individuals with 'high‐functioning autism'. It should be noted that this is an informal term applied to people with ASD deemed to be able to function better than other people with ASD, and that there is no consensus on its definition. ASD is widely recognised as a heterogeneous condition, with different causes in different individuals, manifesting at different stages and in different ways in development, and having different subtypes (Masi 2017). People with ASD may have cognitive styles that differ from people without autism, possibly including strengths in systematising (i.e. the drive to analyse systems, in order to understand and predict outcomes), an increased attention to detail, together with a decreased attention to global information (Baron‐Cohen 2004; O'Connor 2008).
The two main classification systems, the International Classification of Diseases ‐ 10th Revision (ICD‐10, WHO 1992), and the Diagnostic and Statistical Manual of Mental Disorders ‐ 5th Edition (DSM‐5, APA 2013), differ in the way they classify ASD. The ICD‐10 classifies childhood autism, along with several other disorders of psychological development, under the heading 'pervasive developmental disorders' (PDDs). These are defined by abnormal functioning in social interaction and communication, and restricted, stereotyped and repetitive behaviour. PDDs include both autism and Asperger's syndrome in ICD‐10. Childhood autism is characterised in the ICD‐10 by difficulties in social interaction and communication, and restrictive, repetitive and stereotyped patterns of behaviours, interests and activities. Stereotyped behaviours may be expressed verbally or as movements, or both (Casey 2007). The ICD‐10 criteria for Asperger’s syndrome are similar to those of autism, but there is no significant delay in spoken and receptive language, or in cognitive development. The newest version of this classification system, the ICD‐11, will come into use in January 2022. The ICD‐11 incorporates both childhood autism and Asperger's syndrome under a single category, and adds information about intellectual functioning and language abilities to capture the full range of presentations (Reed 2019). The DSM‐5 also no longer separates Asperger’s syndrome and autism, including both under the heading 'autism spectrum disorder' (ASD). The DSM‐5 criteria specify deficits in social communication and interaction, and restricted, repetitive patterns of behaviour. Sensory difficulties (for example, decreased or heightened sensitivity to sounds or smells) are included under restricted, repetitive behaviour. The DSM‐5 also specifies indicators of severity and need for support, and whether there are other comorbid conditions.
In this review, the diagnoses of Asperger’s syndrome and autism are included under the umbrella of ASD as they share the same characteristics (Macintosh 2004).
The heterogeneity of ASD as a condition can make it difficult to compare studies (Havdahl 2019).
Obsessive compulsive disorder
Obsessive compulsive disorder (OCD) occurs worldwide, affects approximately 2 percent of the population and can be associated with significant limitations in everyday functioning in affected individuals (Angst 2004; Kessler 2005). OCD usually first occurs in childhood or early adulthood, and the course is variable (Stewart 2004).
OCD is characterised by recurrent obsessional thoughts or compulsive acts. Obsessional thoughts are stereotyped (i.e. they take a very similar form each time they occur) and comprise repeated thoughts, images or impulses that are distressing to and often resisted by the individual. These ideas and images often carry notions of potential harm to others or the individual themselves; for example, the notion that contamination by germs, through touching a surface, might cause a fatal disease. These ideas are recognised as belonging to the person themselves, and they cause anxiety. Compulsive acts comprise repeated stereotyped behaviours or mental acts, the goal of which is to prevent anxiety or distress and not to provide pleasure or gratification. Compulsive acts are perceived to be preventing a feared outcome which can objectively be said to be unlikely. They are often recognised by the person suffering from OCD to be pointless and ineffective in preventing a feared outcome, although the level of insight may vary.
The DSM‐5 diagnostic criteria are similar to those in the ICD ‐10, although there are some differences in the way OCD is classified by the two classification systems. In the ICD‐10, OCD is classed as an anxiety disorder; symptoms must be present on most days for at least two weeks and be a source of distress or interfere with activities. In the forthcoming ICD‐11, OCD will no longer be classed as an anxiety disorder but will be classified under 'Obsessive‐compulsive and related disorders'. In the ICD‐11, there are slight changes in the definition of symptoms, and affective experiences (i.e. experiences related to mood, feeling or attitude) other than anxiety have been added, such as 'disgust' and a 'sense of incompleteness' (Reed 2019). The ICD‐11 has also added specifiers regarding the individual's degree of insight (i.e. the extent to which obsessional thoughts are believed to be true or false). In the DSM‐5, OCD is not classed as an anxiety disorder. It also specifies an individual's degree of insight and the presence or absence of tics.
OCD and ASD
As repetitive behaviours are a common feature of both OCD and ASD, researchers have suggested a possible association between the two disorders (Bejerot 2001; Ivarsson 2008; Kushi 2019; Leyfer 2006; Mack 2010; Martin 2020; Russell 2005; Stewart 2016). For example, they might share common underlying causes, so that they might occur together in the same person more often than would be expected (Kuno 2018; Liu 2019). Someone with ASD who also meets the criteria for OCD may face additional burdens, leading to more difficulties in everyday functioning (Martin 2020). We describe various aspects of the relationship between OCD and ASD below.
Rate of co‐occurrence of OCD and ASD
Studies have indicated that OCD is common in people with ASD, although there is some variability between estimates in studies, and studies involving clinical samples may not reflect the general population (Leyfer 2006; Mack 2010; Martin 2020).
In a meta‐analysis of co‐occurring mental health diagnoses in the autism population, Lai and colleagues found a pooled prevalence for OCD of 9% in individuals with autism (Lai 2019). However, Meier and colleagues found that only 4% of individuals with ASD had co‐occurring OCD (Meier 2015). In a longitudinal analysis of a large population sample, they found that individuals first diagnosed with ASD had a two times higher chance of being subsequently diagnosed with OCD, and that individuals with OCD had a nearly four times greater risk of subsequently being diagnosed with ASD (Meier 2015).
A large meta‐analysis of 31 studies, including 2121 young people with ASD, found that 17.4% met the criteria for OCD (Van Steensel 2011).
Russell and colleagues found that up to 50% of their patients with ASD reported at least moderate levels of interference from OCD symptoms, although this study was carried out in a clinic specialising in treating people with high levels of co‐occurring conditions (Russell 2005). The authors point out that it is difficult to reliably diagnose mental health conditions in people with autism, since the interview schedules used are designed for the non‐autistic population.
It can be seen that studies have found that people with ASD are more likely to meet the diagnostic criteria for OCD (Van Steensel 2011), and that people diagnosed with OCD are more likely to have autistic traits or ASD (Anholt 2010; Bejerot 2001; Ivarsson 2008; Martin 2020; Stewart 2016).
Symptoms in individuals with OCD co‐occurring with ASD versus those with OCD alone
Studies have found differences and similarities between people meeting the criteria for OCD alone and those meeting the criteria for both OCD and ASD. It should be noted that the level of functioning of people with ASD is very different across the studies, leading to a variability – for example, in the levels of insight and perception of symptoms in participants – which will impact on findings. Russell 2005 compared people with high‐functioning ASD co‐occurring with OCD to people with OCD alone, and found a similar frequency of obsessions and compulsions between the two groups but more somatic obsessions (i.e. obsessions that call attention to bodily processes such as breathing or bodily sensations) and checking compulsions in those with OCD alone. McDougle 1995 reported fewer thoughts with aggression, contamination, sexual, religious, symmetric and somatic content amongst people with OCD and autism compared to people with OCD alone, but in this study, the people with autism were not highly functioning and 15 were non‐verbal. Some people with OCD have a greater than usual sense of responsibility, where they define their thoughts and actions in terms of the harm they could cause to themselves other others. Ekman 2018 found that people with both OCD and ASD scored lower on scales measuring beliefs about responsibility (the Responsibility Attitude Scale (RAS) and the Responsibility Interpretations Scale (RIS)), than people with OCD alone or a control group without OCD or ASD. Ruta 2010 compared children with OCD with children with ASD and no diagnosis of OCD, and found that children with OCD had slightly higher frequencies of contamination, aggression and checking compulsions but that children with ASD displayed higher frequencies of hoarding compulsions.
Reasons for co‐occurrence of OCD and ASD
Genetic, anatomic, biochemical and medical reasons have been considered for the co‐occurrence of OCD and ASD.
Liu 2019 investigated a possible association between OCD and ASD at the genetic level, with their results supporting possible complex genetic associations between the two disorders.
Kuno 2018 suggested that variations in white matter features may be associated with autistic traits in OCD. However, the study had a number of limitations, and the authors recommend that future studies have larger sample sizes and a number of other improvements (Kuno 2018). Carlisi and colleagues found similar deficits in both ASD and OCD in a brain region called the dorsomedial pre‐frontal cortex, as well as differences in both ASD and OCD in a network of neurones regulating the basal ganglia (Carlisi 2017). These two areas of the brain may be involved in the ability to stop a behaviour or response. Thus, it is interesting that these differences are apparent in both ASD and OCD since, in both conditions, difficulties in stopping responses (inhibition) are seen, although the difficulties in stopping responses manifest in different ways (Carlisi 2017).
Certain neurotransmitters (e.g. glutamine and serotonin) may act differently in the brains of those with ASD and those with OCD (Greenberg 2009; Neuhaus 2010).
Other risk factors, such as infections, perinatal problems and older paternal age, have been associated with the development of both ASD and OCD (Akaltun 2017; Geller 2008; Shuid 2021; Wu 2012; Wu 2016; Yong 2021).
Other authors have questioned the validity of ASD, attention deficit hyperactivity disorder (ADHD), and OCD as distinct conditions (Kushi 2019). Lai 2019 highlighted the differences between individuals who are given the label of ASD with respect to intellectual level and the pattern and severity of difficulties, which makes the search for reasons for co‐occurrence of the two disorders difficult to tease out.
Diagnosing OCD in people with ASD
The fact that repetitive behaviours are characteristic of both OCD and ASD can lead to diagnostic confusion (Perez 2012), and either under‐diagnosis or over‐diagnosis. In OCD, repetitive behaviours are often perceived as ego‐dystonic (i.e. they are in conflict with a person’s self–perception and are distressing) and are often resisted. In ASD, repetitive behaviours that are not related to OCD were traditionally thought to be perceived by the person as ego‐syntonic (i.e. they are often pleasurable, not resisted, and are not usually distressing).
Studies attempting to confirm that the repetitive behaviours in ASD and OCD are distinct have shown some conflicting results. Ruzzano 2015 investigated repetitive behaviours using a network analysis (a mathematical technique which analyses the relationships between multiple data points). The data included clinician perceptions and symptoms from ASD and OCD measures. On analysing the data, the authors found that they fell into two distinct clusters or groups, with little relationship between the clusters, suggesting that repetitive behaviours in ASD and repetitive behaviours in OCD are distinct from each other (Ruzzano 2015). However, other studies suggest ego‐dystonic elements in repetitive behaviours in ASD. For example, a recent study noted that children were able to articulate subjective distress associated with repetitive behaviours associated with ASD, even when their parents and clinicians had not perceived such distress, indicating that the repetitive behaviours associated with ASD are not always pleasurable and that they can be distressing (Santore 2020).
Specialist tools to diagnose OCD in children with ASD have been developed. The 'Children's Yale‐Brown Obsessive Compulsive Scale in Autism Spectrum Disorder' is a tool used to diagnose OCD in children with ASD (Scahill 2014).
Description of the intervention
Treatments for OCD include psychological therapies as well as pharmacological therapies, such as selective serotonin reuptake inhibitors (SSRIs) (Soomro 2008), and some antipsychotic medications (Komossa 2010). For milder cases of OCD, National Institute for Health and Care Excellence (NICE) guidelines recommend psychological therapies as the first‐line treatment (NICE 2005).
An established psychological therapy for treating OCD is behavioural therapy, which includes exposure and response prevention (ERP). ERP exposes the individual to the anxiety provoked by their obsessional thoughts, then seeks to reduce and eliminate the use of rituals or repetitive behaviours that are performed by the individual to reduce this anxiety. Relaxation therapy techniques are used to help control the anxiety. Cognitive therapy is often combined with behavioural therapy and ERP. Cognitive therapy is based on the principle that certain thoughts fuel obsessions and compulsions, and it aims to modify these thoughts. CBT is a psychotherapeutic intervention that combines cognitive therapy and behavioural therapy/ERP. It is the primary intervention recommended by current NICE guidance (NICE 2005). The use of CBT in adults and children with OCD is supported by systematic reviews, including two Cochrane Reviews (Gava 2009; O'Kearney 2006; Olatunji 2013).
NICE guidelines do not specify treatments for people with co‐occurring OCD and ASD. However, they recommend that for children and adults with ASD and coexisting mental health problems, psychosocial and pharmacological interventions are offered in line with NICE guidance for the mental health problem in question (NICE 2012; NICE 2013). One study found that people with co‐occurring OCD and ASD were more likely to be prescribed medication, made smaller gains with therapy, and used services for longer than those with ASD alone or OCD alone (Martin 2020).
Concerns have been raised about the effectiveness of psychological therapies in people with ASD because of their differing cognitive processes (Hauck 1995). However, other research has challenged this position (Dahlgren 2003), and has confirmed that CBT may be helpful for anxiety disorders in children with ASD (Sofronoff 2005; Van Steensel 2015).
Studies have reported favourable results for CBT in people with OCD (Iniesta‐Sepulveda 2018), but response and remission have been reported to be lower for people with OCD and co‐occurring ASD (Murray 2015; Tsuchiyagaito 2017). Adaptations to CBT are useful for persons with ASD (Kose 2018). One RCT of adolescents and adults found no statistically significant difference between CBT and anxiety management (including psycho‐education and general anxiety management techniques), in terms of symptom severity (Russell 2013).
Recently, new forms of CBT have been proposed for persons with co‐occurring ASD and OCD, including intensive cognitive behavioural therapy (Iniesta‐Sepulveda 2018), function‐based CBT (Vause 2017), and family‐based CBT (Nadeau 2014; Storch 2020). Iniesta‐Sepulveda 2018 carried out a preliminary study looking at the effectiveness of an individualised, intensive CBT protocol for OCD in adolescents with ASD. The CBT was modified for people with ASD. Participants received between 24 and 80 daily CBT sessions, and the authors report that 78% responded to treatment with large treatment effects. However, the general applicability of this form of CBT may be limited because it is labour‐intensive and uses a degree of inpatient work.
Function‐based CBT is a novel approach combining the principles of CBT with applied behavioural analysis (ABA). ABA is a technique which tries to understand the function of a behaviour and reinforce alternative, adaptive patterns of behaviour. It is commonly used to treat challenging behaviour in people with learning disabilities. ABA has been the source of controversy as it can be seen as forcing people with ASD to conform to neurotypical types of behaviour, not taking into account the feelings and preferences of the individual with ASD (Milton 2018). Single case studies have evaluated ABA as a technique to treat 'OCD‐like' or 'higher‐level restricted and repetitive behaviours' in young people with ASD and a learning disability (Kuhn 2009). Hence, in using a combination of ABA and CBT, function‐based CBT recognises the possible difficulty in distinguishing between the repeated actions typical of compulsions in OCD and repeated actions seen in ASD, and takes the approach of treating both putative aspects of the repeated actions with the same therapy. Vause and colleagues randomly assigned 37 children to function‐based CBT or to treatment as usual (TAU) (Vause 2017). They state that their results suggest that function‐based CBT shows promise in decreasing behaviours and improving quality of life (Vause 2017).
In family‐based CBT, the focus is on providing the child and parent with tools to understand, manage and reduce OCD symptoms. Family‐based CBT includes parenting strategies and graded exposure to feared situations within the context of the family unit (Nadeau 2014; Storch 2020).
How the intervention might work
ERP combined with cognitive therapy repeatedly exposes people with OCD to a feared stimulus, whilst asking them to refrain from carrying out compulsive behaviours. Before treatment, the individual feels that they are reducing the anxiety by carrying out compulsive behaviours, which may be seen as warding off a feared outcome, whereas they have actually been unwittingly reinforcing the anxiety through these compulsive behaviours. The behavioural element of CBT (ERP) involves the individual purposely avoiding carrying out the compulsive behaviours, repeatedly triggering the anxiety which then naturally diminishes over time when the feared outcome does not occur. As a result, the maladaptive thinking which maintains the disorder is diminished. Cognitive therapy directly addresses the maladaptive thoughts associated with the compulsive behaviours (for example, 'If I do not wash my hands, I will become ill and die'), and helps the individual to understand their illogicality.
CBT is assumed to work in a similar way in people with ASD but may need adaptations, because of possible differences in cognitive style between people with and without a diagnosis of ASD. The adaptations are designed to utilise specific strengths that people with ASD might have – for example, attention to detail, or a great interest in a particular area or topic – whilst supporting areas in which they may be weaker. Five case reports of treatment of OCD with CBT in children and adolescents with ASD highlight some of the adaptations that may be useful, including emphasising the behavioural aspects of CBT and relying more on concrete practical and verbal interventions than on discursive discussion (Elliott 2014; Lehmkuhl 2008; Lord 1995; Nadeau 2014; Reaven 2010). Specific techniques included a high level of parental or teacher involvement, use of visual cues, charts and strategies, social stories, involvement of the individual in decision‐making and planning, use of simple coping statements, behavioural reward systems, psycho‐education and simple relaxation exercises. Factors associated with a good outcome in these case reports included the ego‐dystonic nature of symptoms, motivation, ability to self–reflect and self–monitor, ability to externalise, verbal ability and parental support. Family factors were also associated with good outcomes in a randomised controlled trial of CBT versus anxiety management for treatment of OCD with co‐occurring ASD (Murray 2015).
A recent review highlighted the usefulness of modifications of the standard CBT protocol for individuals with OCD and ASD, such as parental involvement, use of visual rather than written or spoken information, personalised treatment metaphors, self‐monitoring, positive reinforcement, and use of clear language and instructions (Kose 2018).
Why it is important to do this review
OCD and ASD often co‐occur and are associated with limitations in functioning. There are challenges in diagnosing OCD in persons with ASD. There is limited evidence for the clinical guidance available for the treatment of OCD in people with ASD, and currently available treatments may need to be adapted for this population. As ASD is increasingly recognised in both adult and child populations, research on the efficacy of established models of treatment for mental disorder in individuals with ASD is increasing. We may soon be better able to clarify the efficacy of behavioural therapy and CBT, including adaptations to these therapies, for the treatment of OCD in individuals with ASD.
There have been other review articles, but their inclusion criteria allowed for non‐RCT studies. For example, Kose 2018 reviewed current research on the effectiveness of CBT for individuals with ASD and OCD, and included three RCTs, one case control study, two single subject experimental designs, and five case studies. Kose 2018 concluded that the small number of studies, and the even smaller number of studies with control groups, limited the ability to draw conclusions about the efficacy of CBT in co‐occurring ASD with OCD. Bedford 2020 looked at the co‐occurrence, assessment and treatment of OCD in children and adults with ASD, without the use of rigorous inclusion criteria and limited to the years 2015 to 2020.
Objectives
To assess the effectiveness of behavioural and cognitive behavioural therapy for obsessive compulsive disorder (OCD) in children and adults with autism spectrum disorder (ASD).
Methods
Criteria for considering studies for this review
Types of studies
RCTs, cross‐over, cluster‐ and quasi‐randomised controlled trials were eligible for inclusion. Trials where the authors did not explicitly state that the trial was randomised but randomisation could not be ruled out were also eligible for inclusion. However, we did not identify any quasi‐randomised trials.
Types of participants
Participant characteristics
We included participants of any age, both adult (18 years and over) and paediatric (younger than 18 years), in the review.
Diagnosis
Ideally, all participants received diagnoses from studies using validated tools based on standardised diagnostic criteria, such as the ICD‐10 (WHO 1992), or the DSM‐4 or DSM‐5 (APA 2013), for both ASD and OCD (including Asperger's syndrome in ICD‐10). We anticipated that studies might not include information about how diagnoses were made, so we did not stipulate certain criteria. When the appropriate diagnostic criteria were confirmed to be met as described above, we noted this.
Participants who did not meet the full criteria for full syndrome autism or Asperger's syndrome, such as those with atypical autism or pervasive developmental disorder not otherwise specified, were not included. Some studies of CBT for individuals with ASD might include other psychiatric diagnoses such as anxiety disorders, as well as OCD. We included these studies as long as the diagnosis of ASD met the criteria described above, and pre‐ and post‐treatment measurements of OCD symptoms were included. Pre‐treatment measurement of OCD symptoms must also have met diagnostic criteria, as above.
Co‐occurring conditions
Studies of participants with co‐occurring conditions, including other psychiatric disorders, neurodevelopmental disorder, or learning difficulties, were eligible for inclusion. It should be noted that the diagnosis of OCD may be problematic for those with more severe global learning difficulties. It was therefore not possible to include studies in individuals where global learning difficulties preclude a diagnosis of OCD.
Setting
We included any setting for therapy: inpatient, day patient, or outpatient.
Types of interventions
Experimental interventions
Experimental interventions included behavioural therapy (i.e. ERP and other behaviour therapy techniques, such as graded exposure and relaxation therapy, breathing management and distraction techniques, either alone or in combination) and CBT. We included studies of interventions in any delivery format; for example, in groups or via the Internet.
We included adaptations of behavioural therapy and CBT for people with OCD and ASD, as long as interventions still followed the general principles of the original models of therapy.
Comparator interventions
Comparator interventions included no treatment, waiting list, attention placebo, and treatment as usual (TAU). TAU could include allocation of a case worker or involvement in groups where supportive counselling or help with problem‐solving could be accessed, but where formal CBT was not provided.
Types of outcome measures
We classified outcome measures as either primary or secondary outcomes.
Primary outcomes
Treatment efficacy: change in core OCD symptomatology compared to measures of symptomatology at baseline, measured on a validated OCD symptom rating scale, including the Yale‐Brown Obsessive Compulsive Scale (Y‐BOCS) which is considered the ‘gold standard’ measure of OCD symptoms (Rosenfeld 1992), the children’s version (CY‐BOCS) (Storch 2004), the National Institute of Mental Health Global Obsessive Compulsive Score, and the Obsessive Compulsive Inventory–Revised (Foa 2002).
Total number of dropouts
Secondary outcomes
Quality of life, measured using recognised rating scales; for example, the World Health Organization Quality of Life index (WHO 1997)
Severity of depressive symptoms using a standardised scale; for example, the Beck Depression Inventory (BDI, Beck 1961)
Severity of anxiety symptoms using standardised scales; for example, the Hospital Anxiety and Depression Scale (HADS, Zigmond 1982) and the children's equivalent, the Children's Depression Inventory (Kovacs 1985)
Level of behavioural difficulties using standardised scales; for example, the Child Behaviour Checklist (Achenbach 1983)
Family accommodation using standardised scales; for example, Family Accommodation Scale Parent Report (Flessner 2009). This outcome was not initially included in the protocol but was added during the review as there was a consensus amongst review authors that this was an important outcome to consider. The authors of the included study used the Family Accommodation Scale Parent Report (FAS PR) (Flessner 2009), where an informant rates 13 items related to the accommodation of symptoms by the family, such as provision of reassurance or modification of home routines, on a 5‐point scale.
Timing of outcome assessment
We categorised outcomes at end point (post‐treatment) or follow‐up, or remission from OCD status, into short‐term (up to six weeks from the last treatment session), medium‐term (six weeks to six months from the last treatment session) and long‐term (six months or longer after the last treatment session) outcomes.
Hierarchy of outcome measures
If studies used multiple measures and one of the measures was the Y‐BOCS or CY‐BOCS, then we included the Y‐BOCS or CY‐BOCS measure in the review, as these are considered the gold standard measures of OCD symptoms. If a study used multiple measures not including the Y‐BOCS, then we included the rating scale with the best assessed reliability and validity after peer discussion, i.e. discussion amongst review authors.
Search methods for identification of studies
Electronic searches
All searches were conducted on 22 September 2019 and updated on 24 August 2020 (unless otherwise stated).
CCMD's information specialist searched the Group's specialised register (CCMDCTR) using key terms (Appendix 1).
We screened the results for behavioural and cognitive behavioural interventions.
The CCMD information specialist conducted complementary searches of the following bibliographic databases using keywords, subject headings, and search syntax appropriate to each resource (Appendix 2).
Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 8) in the Cochrane Library (searched 24 August 2020).
MEDLINE Ovid (1946 to 24 August 2020).
Embase Ovid (1974 to 24 August 2020).
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature; 1982 to 23 September 2019).
PsycINFO Ovid (all years to 24 August 2020).
Sociological Abstracts Proquest (1963 to 24 August 2020).
Web of Science ‐ Core Collection (all years to 24 August 2020).
ERIC ProQuest (Educational Resources Information Center; 1966 to 24 August 2020).
The CCMD information specialist conducted searches on international trial registries to identify unpublished or ongoing studies, or both, in the World Health Organization's trials portal (ICTRP) and ClinicalTrials.gov.
We applied no restrictions on date, language or publication status in the searches. Where required, we used translation services to access materials in languages other than English to reduce the possibility of language bias.
We checked for retractions and errata once all included studies had been selected. We also ensured that multiple (secondary) publications were matched to the parent study and not represented more than once in the analysis.
Searching other resources
We conducted complementary searches on the websites of the following sources of grey literature for additional data.
Electronic Theses Online Service (EThOS) ‐ British Library (ethos.bl.uk/Home.do).
DART ‐ Europe e‐theses Portal (dart-europe.org/basic-search.php).
Networked Digital Library of Theses and Dissertations (NDLTD) (search.ndltd.org).
Open Access Theses and Dissertations (OATD) (oatd.org).
Proquest Dissertations & Theses Global (search.proquest.com/pqdtglobal/dissertations/).
Open Grey (www.opengrey.eu).
Reference lists
We checked the reference lists of all included studies and relevant systematic reviews to identify additional studies missed from the original electronic searches (for example, unpublished or in‐press citations).
Correspondence
We contacted trialists and subject experts for information on unpublished or ongoing studies or to request additional trial data.
Data collection and analysis
Selection of studies
After excluding duplicate records, at least two review authors (SE, EU, DM, KM, MK, NM) independently screened titles and abstracts for inclusion using Covidence (Covidence 2020). We coded potentially relevant records as 'include' and irrelevant records as 'exclude'. We retrieved the full‐text study reports of potentially eligible studies, and at least two review authors (SE, EU, DM, MK) independently examined them for compliance with eligibility criteria. Reasons for exclusion of ineligible studies were identified and recorded. We resolved any disagreements through discussion or, if required, through consultation with a third author (NM). We collated multiple reports that related to the same study so that each study, rather than each report, was the unit of interest of the review. Where appropriate, we corresponded with the investigators to clarify study eligibility. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram and 'Characteristics of excluded studies' tables.
Data extraction and management
Two authors (DM, MK) independently extracted and collated data on a data extraction form in Covidence (Covidence 2020). We resolved disagreements through discussion, or in consultation with a third author (NM), if necessary.
Information collected in the data extraction form included:
participant data: age, sex, severity of condition, diagnostic criteria used to diagnose ASD and OCD if indicated (APA 2013; WHO 1992), inclusion and exclusion criteria;
methods: study design, total duration of study, number of study centres and location (country), study setting, withdrawals, date of study;
types and application of interventions for study and comparison groups, including qualification of therapist, format (individual/group, face‐to‐face/ online or remote support), and adaptations to original therapy model;
outcome measures, including primary and secondary outcomes and the time points data were collected, including post‐treatment measures;
notes: funding for trial, reported conflicts of interest.
Assessment of risk of bias in included studies
Two review authors (SE, EU, DM, MK) independently assessed the risk of bias for the one included study, using Cochrane's risk of bias tool, version one (Higgins 2017). We resolved any disagreements through discussion or by involving a third review author (NM). We assessed these domains for risk of bias:
sequence generation;
allocation concealment;
blinding of participants and personnel;
blinding of outcome assessment;
incomplete outcome data for main outcomes or class of outcomes: this included whether reasons for missing outcome data were recorded and whether the reasons for the missing data were likely to be related to outcome;
selective outcome reporting;
other sources of bias; for example, discrepancies in the level of therapist qualification, treatment fidelity, manualisation of therapy, i.e. use of guidelines or a manual for therapy administration maximising consistency of administration, and researcher conflict of interest.
For cluster‐RCTs and cross‐over trials, we planned to use the templates specifically designed to assess these types of trials, with the same five domains.
We assessed all domains as having 'low', 'unclear', or 'high' risk of bias. We provided a supporting quotation from the study report together with a justification for our judgement in the risk of bias table. We have described and presented the risk of bias data graphically in the text.
For blinding of participants and personnel, blinding of outcome assessment and incomplete outcome data, we considered the risk of bias separately for different outcomes, if applicable.
Measures of treatment effect
We analysed dichotomous data by calculating risk ratios (RRs) and 95% confidence intervals (CIs) for each comparison, using Review Manager 5 (RevMan 5) (Review Manager 2014).
For continuous data, we used the mean difference (MD) and 95% CIs for outcomes on the same scale. We planned to use the standardised mean difference (SMD) to measure the treatment effect if different rating scales were used in different studies, but as only one study was included, this was unnecessary.
We planned to include studies using both change from baseline and final value scores. Skewed data, reported as medians or interquartile ranges, were not available but would have been presented in narrative form had they been.
Unit of analysis issues
We included no cluster‐randomised, cross‐over or multi‐arm trials in our review. If such trials had met inclusion criteria, we would have managed these using appropriate statistical analyses from the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021, hereafter referred to as the Cochrane Handbook).
Dealing with missing data
Where required, we contacted the original investigators to request missing data.
We planned to deal with missing dichotomous data through three sensitivity analyses. In the intention‐to‐treat (ITT) analysis, we would have assumed that participants who dropped out after randomisation had negative outcomes. We also planned to calculate best and worse case scenarios for the clinical response outcome, where we would have assumed that dropouts in the active treatment group had positive outcomes and those in the control group had negative outcomes (best case scenario), and that dropouts in the active treatment group had negative outcomes and those in the control group had positive outcomes (worst case scenario). However, insufficient data were available to conduct these analyses.
Where there were missing continuous data, we used only available case data. If SDs were not available from trial authors, we would have calculated these from P values, t‐values, confidence intervals, or standard errors. However, these were reported in the one included trial.
Assessment of heterogeneity
If more than one study had been included, we planned to assessed heterogeneity using the I2 statistic, which describes the variability in effect estimates due to heterogeneity rather than sampling error (chance). We would have considered I2 values in terms of the rules of thumb reported in the Cochrane Handbook (Higgins 2021). Our interpretation of I2 would have taken into account the magnitude and direction of effects and the strength of evidence for heterogeneity (for example, the P value from the Chi2 test).
Assessment of reporting biases
A comprehensive search was undertaken for studies meeting eligibility criteria for the review. Multiple sources were searched, including grey literature and trial registries, to reduce publication bias. We intended to test for publication bias by visual inspection of funnel plots. However, for sufficient power, at least 10 studies are needed for a funnel plot, though the number needed depends on the size of the studies and on the treatment effect. For continuous outcomes with intervention effects measured as mean differences, we intended to use Egger's test to test for funnel plot asymmetry. However, Egger's test should also not be used if there are fewer than 10 studies in the meta‐analysis (Egger 1997).
Data synthesis
Given sufficient data, we planned to present details of outcome data in the form of summary tables, forest plots and meta‐analyses, including comparisons and subgroup analyses.
Additionally, we planned to carry out meta‐analysis if there was a sufficient number of studies and if they were sufficiently similar (i.e. the treatments, participants and the underlying clinical question were similar enough for pooling) (Deeks 2011; Valentine 2010). We planned to use a random‐effects model for the data, as we anticipated significant heterogeneity between studies. However, if there was a very small number of studies, then it would not have been possible to estimate Tau2 with a sufficient level of precision, and a fixed‐effect model may have been the only viable option. As we included only one study, we narratively synthesised this study, in the form of a structured summary of the study's characteristics and findings.
Subgroup analysis and investigation of heterogeneity
We intended to undertake the following subgroup analyses.
Presence or absence of global intellectual disability, verified by appropriate testing of intelligence and functioning in the study, as therapy may be more challenging in those with intellectual disabilities.
Mode of delivery of intervention (i.e. individual or group sessions) as there may be differences in efficacy between the two modalities.
Treatment effects by type of non‐active comparator (no treatment, waiting list, attention placebo, psychological placebo, and treatment as usual).
Behavioural therapy/ERP alone and CBT, as these constitute treatments with different elements.
However, as only one study was included, subgroup analyses were not possible.
Sensitivity analysis
We planned to conduct the following sensitivity analyses for the primary outcome of treatment efficacy.
Excluding studies that had more than one of the following issues: more than 50% dropout rate, a high risk of reporting bias (Wiltshire 2017), or a high risk of allocation concealment.
Excluding quasi‐randomised studies due to the risk of systematic bias in such trials arising from the lack of true randomisation.
If issues were identified which warranted further investigation, we would have undertaken unplanned sensitivity analyses ‐ for example, to investigate the effect of an outlier on the results. However, sensitivity analyses were not possible since only one study was included.
Summary of findings and assessment of the certainty of the evidence
We created a summary of findings table for the comparison of treatment (CBT/behavioural therapy) versus non‐active comparators. The summary of findings table included all outcomes of interest: treatment efficacy, dropouts, quality of life, depression symptoms, anxiety symptoms and behavioural difficulties. Effect sizes and 95% CIs were included.
One review author (NM) performed an assessment of the certainty of the evidence following the GRADE approach (Higgins 2021), and using GRADEpro software (www.gradepro.org). A second author (DM) checked all GRADE assessments. We justified all decisions to downgrade or upgrade the certainty of the evidence using footnotes, and made comments to aid the reader's understanding of the review, where necessary.
We created the summary of findings table before writing our abstract, discussion, and conclusions, so that we could consider the impact of the certainty of the evidence for each outcome on our confidence in these findings. Our confidence in the mean treatment effects are reflected in the interpretation of the results, which informed the abstract, plain language summary and discussion sections of this review.
Results
Description of studies
We included one study, Russell 2013, a randomised controlled trial in which the main comparison was CBT versus anxiety management. This study is described below (Included studies).
Results of the search
The searches retrieved 4636 records and two further studies were identified from following up on trial registries. Of these, we removed 471 duplicates, and screened the remaining 4167 records by title and abstract. Of these, we excluded 4108 records after this initial screening process. We assessed the remaining 59 full‐text records, and included only one study (two records) in this review (Figure 1).
1.
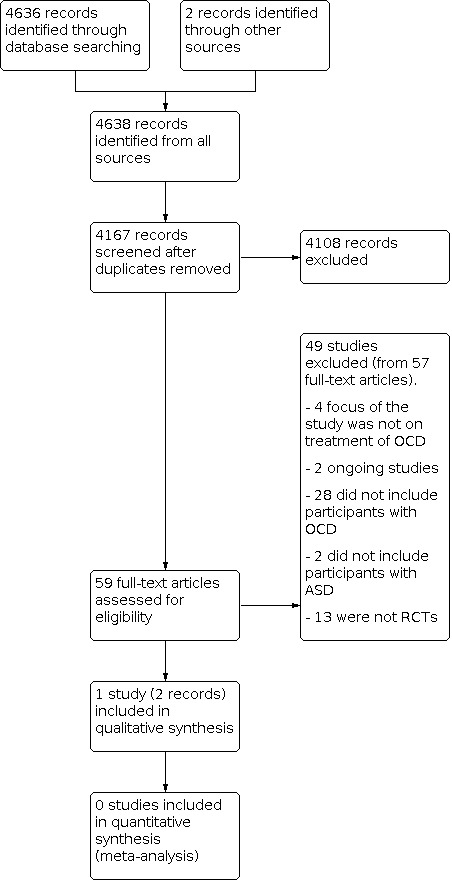
Study flow diagram
Included studies
We included only one study in this review (Russell 2013), and describe it below. Russell 2013 is a randomised controlled trial comparing CBT for OCD in people with high‐functioning ASD.
Recruitment of participants
Participants were recruited from specialist ASD clinics, specialist adult and paediatric OCD clinics, and generic child and adult mental health services. They had a confirmed diagnosis of ASD, verbal intelligence quotient (IQ) greater than 70, with co‐occurring OCD and were aged between 14 and 65 years. Participants with significant comorbidities (current psychotic symptoms, a current episode of major depression, uncontrolled epilepsy or current substance misuse) were excluded, and there had been no changes to psychiatric medication in the six weeks prior to study entry. Diagnosis of ASD was confirmed using well‐recognised and validated rating scales, the Autism Diagnostic Interview (ADI) (Le Couter 1989), and the Autism Diagnostic Observation Schedule (ADOS) (Lord 1989).
Diagnosis of OCD was confirmed by including only those with a score greater than 16 on the Y‐BOCS (Kim 1990). The MINI 5.0 neuropsychiatric interview, a short structured diagnostic interview (Sheehan 2000), was also used to assess other co‐occurring psychiatric diagnoses and to confirm the presence of OCD. To distinguish between obsessions and compulsions and the stereotypic behaviours and interests occurring in ASD, participants were asked to define what an obsession was. Participants who offered a definition consistent with an obsessive‐compulsive symptom were prompted to report any similar experiences they had before the Y‐BOCS was administered. If the participant thought that an obsession was something that someone was very interested in, a definition was offered and the participant was again prompted to report their own experiences. If the participant did not understand the definition or did not offer any relevant experiences, then an example was given. The same procedure was completed for compulsions. Symptoms were only rated if they caused discomfort or interfered with functioning. In addition, two raters rated the Y‐BOCS and both raters' ratings were taken into account in the final scoring. The presence of obsessions and compulsions was not recorded unless they were ego‐dystonic (i.e. unwanted and not in keeping with a person's natural thoughts and inclinations) and compulsions were resisted and recognised as excessive. This procedure had also been used in a previous study (Russell 2005).
Study design
Treatment group (cognitive behavioural therapy (CBT))
Therapists used a manual outlining ASD adaptations to standard CBT for OCD. The following adaptations were used.
Making sure that required emotional understanding was in place, including understanding and differentiating emotions, particularly anxiety, and making links between thoughts, feelings and behaviours.
Educational sessions about understanding and rating anxiety were provided if needed, before introducing the treatment rationale.
Visual tools, use of concrete examples and a participant's special interests were used as a way to convey psychological concepts.
Therapists used a structured and directive approach to the sessions and to homework tasks.
CBT was predominantly ERP‐based and was conducted in a hierarchical fashion (i.e. ERP tasks became progressively more challenging as the therapy progressed). An average of 10 ERP homework tasks was set and compliance was 79%. Cognitive methods to help individuals to test out OCD and anxiety‐related beliefs were less frequently employed.
Control group (anxiety management)
The control group was designed to ensure that any treatment effects were due to the specific techniques used in CBT, and anxiety management provided therapist contact, psycho‐education about anxiety, and general anxiety reduction techniques, but it did not contain any ERP or any cognitive strategies addressing OCD‐related beliefs. Delivery of anxiety management was manualised, i.e. performed according to specific guidelines or a manual for administration, to ensure consistency, and comprised eight modules including education about anxiety, diaphragmatic breathing and practice, education about mood, healthy habits and problem‐solving.
Duration of treatment
Up to 20 therapist sessions of approximately one hour per session were allowed in both study arms, as clinical experience indicated that longer treatment durations might be needed in individuals with ASD. The four treating therapists were all clinical psychologists with extensive experience and further education in treating OCD in young people and adults. Cases were randomly allocated to a therapist. The manualised CBT was used in three cases prior to the start of the study to check out feasibility, allow training in working with people with ASD and to gain a user perspective. Supervision was provided by an experienced consultant clinical psychologist.
Treatment fidelity and therapist allegiance
To assess treatment fidelity, 20% of cases were audio recorded at random to ensure treatment fidelity (i.e. that the same treatment was offered to all participants in each arm).
To assess therapist allegiance (i.e. that the treatments only contained the therapeutic elements that they were meant to), all sessions were recorded and 20% of these recordings were randomly selected and rated by an independent therapist, outside of the clinical trial, who was blind to the treatment arm and was asked to rate whether the session contained OCD‐targeted interventions such as ERP or cognitive therapy.
Outcomes
Outcomes relevant to this review were of OCD symptoms using the YBOCS total severity rating (Kim 1990), depressive symptoms using the Beck Depression Inventory (Beck 1996; Beck 2001), anxiety symptoms using the Beck Anxiety Inventory (Beck 1998), and day to day functioning using the Work and Social Adjustment Scale (Mundt 2002).
Assessors who were blind to treatment group, and who were trained clinicians experienced in administering the Y‐BOCS and interviewing people with ASD, rated symptoms at six time points: before treatment (no more than four weeks before the first treatment session), at end of treatment (one week after the final session) and at one‐, three‐, six‐ and twelve‐month follow‐up. To assess the validity of the blinding procedure, blind assessors were asked to complete a questionnaire at each assessment point, indicating to which arm of the trial they thought a participant was allocated. They had to say why they had made that decision, giving one of the following reasons: (a) a random decision, (b) revealed by the participant, or (c) due to clinical improvement. The questionnaire was completed in 80% of cases, and none of the assessors cited (b) as their reason for choice of treatment group. The blind assessors were correct in their assignment of treatment group in 60% of cases.
Primary outcome
The primary outcome measure was the Y‐BOCS total severity rating, a severity scale of OCD symptoms (Kim 1990). The Y‐BOCS is a 10‐item, clinician‐administered scale and the most widely‐used rating scale for OCD. It provides five rating dimensions for both obsessions and compulsions. All items are scored on a 4‐point scale from 0 = "no symptoms" to 4 = "extreme symptoms." Scores range from 0 to 40, with higher scores representing more serious symptoms.
Secondary outcomes
The outcomes below were self‐report outcomes, i.e. participants reported directly about their own symptoms, apart from the Spence Childrens' Anxiety Scale, which can be completed by either the child or the parent.
Secondary outcome, severity of depressive symptoms, as measured by the Beck Depression Inventory (BDI) for adults: a 21‐item scale of common symptoms of depression on a 4‐point scale of severity (Beck 1996). The BDI‐Youth was used for youth (14 to 18 years) (Beck 2001). It uses a Likert scale ranging from 0 to 3, with an overall range of 0 to 63 (higher scores indicating more severe symptoms).
Secondary outcome, severity of anxiety symptoms, as measured by the Beck Anxiety Inventory (BAI) for adults: a 21‐item scale of common symptoms of anxiety rated on a 4‐point scale of severity with an overall range of 0 to 63 (higher scores indicating more severe symptoms) (Beck 1998). Severity of anxiety symptoms were measured in youth (aged 14‐18 years) using the Spence Childrens' Anxiety Scale (SCAS) (Spence 1998), a 45 item scale which can be filled out by the child or a parent.
Secondary outcome, quality of life, as measured by The Work and Social Adjustment Scale (WSAS) for adults and youth, a short 5‐item scale rated on a 9‐point severity scale, rating ability to work, home management, social leisure activities and private leisure activities (Mundt 2002). Scores range from 0 to 40, with higher scores indicating more severe disability.
Power analysis
Data from a pilot study indicated that, in order to detect statistically significant differences between groups on the primary outcome measure, 19 participants would be needed for each of the CBT and anxiety management treatment groups, respectively (Russell 2009).
Data analysis
Authors assessed differences in symptoms or demographics, pre‐treatment, between groups, using independent t‐tests and Chi2 tests. Authors conducted an ANCOVA (Analysis of covariance) on the primary outcome measure at the end of treatment. The ANCOVA is a statistical technique which tests whether the variable of interest has an effect on outcome after adjusting for the effects of other variables that are not of interest. The authors used repeated measures analysis of variance to detect changes between the pre‐treatment timepoint and post‐treatment timepoint in the anxiety management and CBT groups. Effect sizes were calculated using Cohen's d. All analyses were intention‐to‐treat and pretreatment scores were not carried forward where outcome data were not available.
Excluded studies
In accordance with guidance provided by the Cochrane Handbook, we have only provided references for studies that appeared to meet the eligibility criteria but, on closer inspection, did not meet them (see 'Characteristics of excluded studies' for the reasons we excluded these records). However, for transparency, we have included the full list of exclusion reasons and their associated numbers, both in this section and in the PRISMA flow chart (Figure 1).
After obtaining full‐text reports, we excluded 49 studies (57 records) for the following reasons: 28 studies because the participants were not diagnosed with OCD; 13 because they were not RCTs, quasi‐RCTs, cross‐over or cluster trials; 4 studies in which the focus was not on the treatment of OCD; and 2 studies because participants did not have ASD. It was noted that one of these two studies, Wolters 2016, did attempt to measure autistic symptoms; however, this was an outcome measure, not a criterion for inclusion of the participants.
Risk of bias in included studies
We have summarised the results of the risk of bias assessments for the sole included study in Figure 2. We judged the risk of bias as being high for the allocation concealment and blinding domains, and unclear for incomplete outcome data and other biases, and low for random sequence generation and selective reporting.
2.

Review authors' risk of bias judgements
Allocation
We judged allocation (selection bias) with respect to sequence generation as low risk of bias. Participants were randomised to the CBT or anxiety management arm using a random number table (1:1 ratio) managed by an investigator who was part of the trial management committee but not a treating therapist. We noted that computer‐generated allocation would have reduced the risk of allocation bias further.
We assessed allocation concealment as high risk of bias. The authors did not make a clear attempt to describe how concealment was maintained.
Blinding
We judged risk of performance bias as high because maintenance of allocation concealment would have been problematic due to the easily perceived differences in content of psychological therapies in the two treatment arms. This is a common difficulty in psychosocial studies.
We assessed risk of detection bias as high for all outcomes, as blinding of participants and personnel for all outcomes is problematic in a psychosocial study. True blinding can be difficult to achieve in psychosocial studies, but pragmatic steps were taken to minimise bias in this study. For example, therapists allocated the task of listening to recordings to ensure treatment fidelity were independent, blind to the treatment condition and outside of the clinical trial.
We assessed risk of detection bias as high for self‐reported outcomes as participants were not blinded to group allocation.
We judged risk of detection bias for clinician‐administered outcomes as low. The authors took steps to demonstrate that assessors who rated before treatment and at one, three, six and twelve months afterwards, were blind to treatment group. In order to address the validity of the blinding procedure, the assessors were asked to complete a questionnaire at each point, noting which participants were in each treatment group and to indicate if their decision was a random decision, revealed by the participant or due to clinical improvement. It was notable that the assessors were only accurate in their assignment of treatment group in 60% of cases, and in no case was the allocation group revealed by the participant. Assessors described their choice as random in 75% of cases, and in 45% of cases, clinical improvement was also cited as a reason for assignment to a particular group.
Incomplete outcome data
We judged risk of attrition bias as unclear as the picture was mixed. Missing data were not accounted for in the analyses. Twenty‐three participants were randomised to each of the two treatment groups; 20 in each group completed treatment and the number of dropouts in each group was the same. In terms of missing data, Y‐BOCS ratings were available for all participants at the start of treatment, 20 in the CBT group and 20 in the anxiety management group at the end of treatment, and 18 in the CBT group and 17 in the anxiety management group at one month follow‐up. The authors state that there was more attrition after the end of treatment for self‐report measures, which included secondary outcome measures (e.g. BDI, BAI and WSAS) than for the Y‐BOCS. It should be noted that, although dropout was relatively low from allocation to treatment completion, from allocation to one month follow‐up, data on about one‐quarter of participants became unavailable due to discontinuation of the intervention or loss to follow‐up.
Selective reporting
We assessed the risk of bias for this domain as unclear. Although the methods of the trial were included in a registry, this was completed retrospectively. Therefore, we could not ascertain whether alterations were made after the protocol stage. Outcomes mentioned in the methods section were reported in the results.
Although authors reported cross‐over data after one month post‐intervention follow‐up, these data were based on a small number of participants, and this was not planned in their protocol. Therefore, we did not include these data in our review.
Other potential sources of bias
We rated the risk of other potential sources of bias as unclear. The authors stated that the CBT group contained more participants who endorsed hoarding symptoms compared to the anxiety management group, and that this may have had an influence on the results, as hoarding symptoms are considered more difficult to treat with CBT. However, it should be noted that the Y‐BOCS is not a validated instrument to assess hoarding disorder.
There may have been subtle degrees of adaptation of the intervention across the two arms, occurring on an individual case basis, which might not be picked up by fidelity recordings.
Effects of interventions
See: Table 1
Of the 75 people referred, 23 participants were allocated to each treatment arm. No substantial baseline differences were noted between treatment groups on ADOS, verbal IQ, gender, age or pretreatment symptom scores. There was a mean difference of three sessions (MD 3.00, 95% confidence interval (CI) ‐5.98 to ‐0.01) favouring attendance in the CBT arm (17.43, SD = 4.3) compared to the anxiety management arm (14.43, SD = 5.3).
Although we had intended to include outcomes for children and adults separately, the included study did not report data separately for these populations (Russell 2013). Therefore, all results discussed below are based on a combined population of children and adults.
Primary outcomes
Yale‐Brown Obsessive Compulsive Scale (Y‐BOCS) total (continuous outcome)
At the end of treatment, although treatment differences (MD ‐3.00, 95% CI ‐8.02 to 2.02; low‐certainty evidence) favoured the CBT group, the 95% CI indicated a high level of imprecision. ANCOVA analyses controlling for pretreatment Y‐BOCS severity ratings found similar results.
At one month follow‐up, differences between groups were slightly smaller (MD ‐2.00, 95% CI ‐6.58 to 2.58).
Response on the Y‐BOCS may have been associated with family accommodation score (FAS) at baseline. This may impact on comparisons between CBT and control groups as FAS scores may have been higher in the CBT group at baseline. The group categorised as responding to treatment had reported substantially lower scores on the FAS at baseline compared to non‐responders (MD 11.31, 95% CI ‐22.89 to 0.28). However, these differences on the FAS declined at the end of treatment.
Total number of dropouts (dichotomous outcome)
There were no differences in completion rates for CBT (13%) and anxiety management (13%) groups (RR 1.00, 95% CI 0.22 to 4.45; low‐certainty evidence).
Secondary outcomes
Depression symptoms (Beck Depression Inventory, BDI) (continuous outcome)
At the end of treatment, the CBT group reported fewer depression symptoms compared with the anxiety management group (MD ‐1.80, 95% CI ‐11.50 to 7.90; low‐certainty evidence) but the width of the 95% CI shows a high level of imprecision.
At one month follow‐up, the difference between groups was slightly less (MD ‐1.30, 95% CI ‐ 10.56 to 7.96) but the 95% CI shows the estimate is highly imprecise.
Anxiety symptoms (Beck Anxiety Inventory, BAI) (continuous outcome)
At the end of treatment, the CBT group reported fewer anxiety symptoms compared with the anxiety management group (MD ‐3.20, 95% CI ‐11.38 to 4.98; low‐certainty evidence) but with a high level of imprecision as shown by the width of the 95% CI.
At one month follow‐up, as with other outcomes, the difference declined (MD ‐1.80, 95% CI ‐9.66 to 6.06) and there remained a high level of imprecision in this estimate.
Quality of life (Work and Social Adjustment Scale, WSAS) (continuous outcome)
At the end of treatment, as with all other outcomes, differences favoured the CBT group (MD 5.20, 95% CI ‐1.41 to 11.81, low‐certainty evidence) but with a high level of imprecision indicated by the wide 95% CI.
At one month follow‐up, there was a substantial decline in the quality of life for the CBT group, and the difference slightly favoured the anxiety management group (MD ‐1.61, 95% CI ‐6.86 to 3.66) but with a high level of imprecision.
Family accommodation (Family Accommodation Scale Parent Report, FAS PR) (continuous outcome)
FAS PR score was higher in the CBT group compared with the anxiety management group at the end of treatment (MD 5.60, 95% CI ‐7.25 to 18.45) but with a high level of imprecision indicated by the wide 95% CI.
At one month follow‐up, the difference in FAS PR scores between groups was smaller, but still greater for the CBT group (MD 3.30, 95% CI ‐9.15 to 15.75), with a high level of imprecision.
Discussion
This review aimed to assess the effectiveness of behavioural therapy and cognitive behavioural therapy (CBT) for OCD in children and adults with ASD.
Summary of main results
We systematically reviewed the literature to assess the effectiveness of behavioural therapy and CBT for OCD in children and adults. We searched the literature for RCTs, cross‐over, cluster‐ and quasi‐randomised controlled trials. A number of trials of CBT for co‐occurring anxiety disorder and ASD included people with OCD, but the numbers of people with OCD were small in these studies. One small RCT (46 participants), describing the use of CBT for OCD in ASD compared to individuals treated with anxiety management, met our inclusion criteria (Russell 2013). This study showed little or no benefit at the end of treatment favouring CBT compared to anxiety management in OCD symptoms (MD ‐3.00, 95% CI ‐8.02 to 2.20), depression symptoms (MD ‐1.80, 95% CI ‐11.50 to 7.90), anxiety symptoms (MD ‐3.20, 95% CI ‐11.38 to 4.98), and quality of life (MD 5.20, 95% CI ‐ 1.41 to 11.81) but the 95% CIs were very wide, reflecting the limited amount of data included in our review. We judged the evidence to be of low certainty.
Family accommodation was higher in the CBT group compared with the control group, although as above, there was substantial imprecision due to data only being available for one small study.
Overall completeness and applicability of evidence
The evidence base for the use of CBT for the treatment of OCD co‐occurring with ASD is very small. We found and included only one RCT in this review. We conducted an extensive search of the literature, including grey literature, to minimise the risk of missing relevant studies. There are limitations in the methods used in the included study; namely, using CBT as intervention and anxiety management as comparator. The adapted components of anxiety management used in the study have significant potential overlaps with the behavioural activation component of CBT, hence introducing a potential confounder which is difficult to adjust for and which impacts on the applicability of results.
However, we acknowledge that some of these challenges are generic to trial design in the psychotherapy arena. Authors have also attempted to harmonise treatment fidelity by ensuring that 20% of cases were assessed at random, which increases the generalisability of the review and is a welcome addition in such interventions.
It is important to note that individuals who endorsed hoarding symptoms who were included in this study may no longer be classified as suffering from OCD in future studies due to the new classification of 'hoarding disorder' in the DSM‐5. As hoarding disorder is not readily treatable with CBT, future studies of CBT for OCD, using the new classification system, may be more likely to show positive results.
The study included people aged 14 to 65 years old, with a verbal IQ cut‐off of 70. Thus, the study is limited in scope in terms of applicability to all clinical groups. The main outcome analysis was repeated excluding those aged 14 to 16 years, and this did not affect the pattern of results.
Quality of the evidence
Interventions for OCD in people with ASD represent an emerging research area. It is therefore unsurprising that we included only one RCT in our review. This was a relatively small trial (46 participants) so the benefits of randomisation for balancing prognostic factors across groups are less apparent. However, we did not identify any important baseline differences between groups.
We identified potential concerns related to a lack of allocation concealment used in the included RCT. In addition, psychological interventions cannot blind participants receiving and personnel delivering these interventions. On average, these risks of bias lead to an overestimate of the effectiveness of interventions (Savovic 2015). An additional concern was attrition bias, particularly for self‐reported outcomes, where approximately one‐quarter of participants dropped out.
Outcome assessors were blinded to which treatments participants were allocated, which is likely to reduce the risk of bias. In addition, efforts were made to assess fidelity to intervention manuals. It appears there were acceptable levels of fidelity for therapists conducting the CBT intervention.
An additional factor to consider in the interpretation of the results was the nature of the comparator (anxiety management). This was a relatively active control which may impact on the magnitude of between‐group differences with the CBT intervention. Given that people with ASD may be more likely to experience difficulties with processing and identifying emotions (Hill 2004), the element of teaching about emotions and how to recognise them in the anxiety management control arm may have helped participants learn how to understand and manage difficult emotions relating to the OCD. The positive interpersonal contact related to any talking therapy may also have had a positive impact on symptomatology in this group of individuals who, due to social and mental health issues, may be likely to be socially isolated.
Potential biases in the review process
We identified a number of RCTs which included participants with a diagnosis of OCD (Storch 2015; Storch 2020; Wood 2009; Wood 2015). However, the focus of these studies was not on the treatment of OCD and numbers of participants with OCD were very low. Wood 2009 had eight people with OCD in the treatment group and nine in the control group; Storch 2020 had one person with OCD in the treatment group and four in the control group; Wood 2015 had two people with OCD in the treatment group and one in the control group; and Storch 2015 had three in the treatment group and one in the control group.
In addition, while we thoroughly searched for ongoing or unpublished studies, it is difficult to rule out if there are any additional studies relevant to our review which may have impacted on our conclusions. A further potential bias in the review process was the post‐hoc inclusion of family accommodation as an outcome in our review. However, we think any potential biases are likely to be minor as this is a clinically important outcome and the results were similar across all outcomes.
Agreements and disagreements with other studies or reviews
We identified two other review articles. Kose 2018 included a wider variety of lower‐quality studies, limiting the applicability of results. Kose 2018 included two RCTs which we excluded: Vause 2017, which was excluded from our review as obsessive compulsive behaviours were measured rather than obsessive compulsive disorder; and Wolters 2016, which was excluded from our review as the Children's Social Behaviour Questionnaire was used to examine ASD symptoms in the children as an outcome measure, not as a criterion for inclusion of the participants.
The second review article, Bedford 2020, looked at the co‐occurrence, assessment and treatment of OCD in children and adults with ASD. This was a wide‐ranging review without rigorous inclusion criteria which looked at research from 2015 to 2020. There are no areas of disagreement with our review.
Authors' conclusions
Implications for practice.
The literature indicates that a clear diagnosis of obsessive compulsive disorder (OCD) in people with autism spectrum disorder (ASD) is important in order to differentiate compulsions associated with OCD from stereotyped and repetitive behaviours seen in ASD. Cognitive behavioural therapy (CBT) may be less effective in people with ASD than in people with OCD without co‐occurring ASD (Murray 2015; Tsuchiyagaito 2017), and modifications may be required. Our review indicates that CBT may be an effective treatment for OCD co‐occurring with ASD, although evidence is very limited. There is not yet clear evidence that CBT is more effective than anxiety management.
Awareness and understanding of adaptations to CBT for people with OCD co‐occurring with ASD may be helpful for clinicians treating this group of individuals. Possible adaptations may include taking time to ensure that people can identify and understand their own emotions and that they understand the links between cognitions, emotions and behaviours. Style of delivery may also need to be adapted; for example, using concrete language, focusing more on exposure and response prevention (ERP) than the cognitive elements of CBT, using individuals' own special interests to promote engagement and understanding, and visual rather than verbal presentation of information. The efficacy of new and innovative forms of CBT for this population (such as function‐based CBT and intensive CBT), and the subgroups of individuals for whom these therapies might be most helpful, may be explored in clinical practice.
It may be helpful for clinicians to attempt to understand individuals' views of their difficulties. As outlined in the Discussion, people with ASD may have different perceptions of their OCD, have different aims for treatment, and experience different obstacles to treatment than people without ASD. Information gained about individuals' views may improve understanding of their motivators towards change, and thus help clinicians enhance the efficacy of their treatment protocols as well as opening up avenues for further research.
In summary, clinicians trained in treating OCD using CBT may be able to work effectively with people with co‐occurring ASD and OCD, and appropriate protocols adapted for CBT may be useful.
Implications for research.
Co‐occurring OCD and ASD is common and may cause a significant impairment of functioning. The views of patient groups will be invaluable in setting the research agenda. The following may be areas for future research.
First, in the included study, there was a clear protocol to distinguish compulsive actions from restricted repetitive behaviours (RRBs) in this client group. However, some authors have suggested an overlap in phenomenology between compulsions and RRBs (Perez 2012). Further descriptive studies may help to develop an understanding of the phenomenology of stereotyped and repetitive behaviours in ASD and their relationship to obsessional compulsive behaviours in OCD, in order to clarify characteristics that separate them and areas in which they overlap. This may inform development of treatment protocols and the development of tools for diagnosing OCD in ASD.
Second, in our review, we found that there were a number of trials of CBT for co‐occurring anxiety disorder and ASD (Storch 2015; Storch 2020; Wood 2009; Wood 2015). These trials included people with OCD under the umbrella of anxiety disorders. The numbers of people with OCD were small in these studies, and the outcomes for people with OCD were not measured separately from the other participants. The separation of OCD from anxiety disorders in the Diagnostic and Statistical Manual of Mental Disorders ‐ 5th Edition (DSM‐5) and the International Classification of Diseases ‐ 11th Revision (ICD‐11) may facilitate more focused research on the use of CBT for people with ASD and OCD alone.
Third, future studies could compare the perception of symptoms, perceived functional impact of symptoms, and treatment outcome goals in people with OCD and co‐occurring ASD compared to people with OCD without co‐occurring ASD. This may help clinicians to optimise treatment engagement and therefore response in those with co‐occurring ASD and OCD.
Fourth, we have highlighted in our review how differences in cognitive style may impact on the ability of people with ASD to make use of CBT for OCD symptoms without some modification to the CBT. Future studies should clarify which modifications are most effective in treatment of OCD in ASD and compare the outcomes for modified CBT with the outcomes for both unmodified CBT and anxiety management.
Fifth, our included study describes the impact of ASD and OCD co‐occurrence on lifestyle, including possible poorer employment prospects in our group and hence greater social isolation, which may impact on individuals' ability to access treatments. Future studies could usefully examine both inherent and systemic barriers to implementation of treatment in this group, which may include access and stigma issues as well as service barriers.
Sixth, efforts should be made to involve service users in future research endeavours. There are initiatives to involve the ASD community as stakeholders in setting research objectives (Roche 2020). For example, Autistica is an independent organisation which brings together people with ASD, carers and clinicians to prioritise research projects (www.autistica.org.uk/).
Seventh, our included study indicated that family accommodation to symptoms was associated with poorer treatment response. Future studies could examine the understanding of OCD in families of people diagnosed with co‐occurring ASD and OCD; for example, whether families can separate symptoms of OCD from those of repetitive and stereotyped behaviours in ASD, and families' understanding of the role of the family in recovery.
Finally, in the experience of the authors, co‐occurring mental health issues are common in people with comorbid ASD and OCD, including intellectual disabilities, and these can impact on treatment response. Studies recruiting people with the full range of co‐occurring conditions usually seen in clinical practice may be useful in understanding how further co‐occurring conditions may affect response to treatment (Lai 2019). Conversely, further RCTs on treatment of OCD in people with ASD with CBT using more homogeneous samples than in the included study may increase the power of future studies. In particular, in view of the heterogeneity of ASD, restriction of the sample to particular subtypes of ASD (for example, confining recruitment to a particular age or IQ level) might offer information about the relationship between subtypes of ASD and particular conditions which may co‐occur with ASD (Havdahl 2019).
History
Protocol first published: Issue 11, 2018
Notes
None
Acknowledgements
Authors of the protocol: we thank Brid McMahon and Alison Leech who, along with Sarah Elliott, authored the protocol for this review.
We thank the editorial team of Cochrane Common Mental Disorders for providing guidance during review development, and Kath Wright and Sarah Dawson who helped develop and run the search strategies.
The authors and the Cochrane Common Mental Disorders Editorial Team are grateful to the following peer reviewers for their time and comments: Georgina Cox, Helen Fulbright, Nuala Livingstone and Lindsay Robertson. They would also like to thank Faith Armitage for providing copy‐editing.
CRG Funding Acknowledgement: the National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Common Mental Disorders Group.
Disclaimer: the views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health and Social Care.
Appendices
Appendix 1. Cochrane Common Mental Disorders Controlled Trials Register (CCMDCTR)
The Cochrane Common Mental Disorders Group (CCMD) maintains two archived clinical trials registers at its editorial base in York, UK: a references register and a studies‐based register. The CCMDCTR References Register contains over 40,000 reports of RCTs in depression, anxiety and neurosis. Approximately 50% of these references have been tagged to individual coded trials. The coded trials are held in the CCMDCTR Studies Register, and records are linked between the two registers through the use of unique study ID tags. Coding of trials is based on the EU‐Psi coding manual, using a controlled vocabulary (please contact the CCMD information specialists for further details). Reports of trials for inclusion in the Group's registers were collated from routine (weekly), generic searches of MEDLINE (1950 to 2016), Embase (1974 to 2016), and PsycINFO (1967 to 2016); quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL); and review‐specific searches of additional databases. Reports of trials were also sourced from international trial registers via the WHO trials portal (the International Clinical Trials Registry Platform (ICTRP)), pharmaceutical company websites, and handsearching of key journals, conference proceedings, and other (non‐Cochrane) systematic reviews and metal‐analyses.
Details of CCMD's generic search strategies (used to identify RCTs) can be found on the Group's website, with an example of the core MEDLINE search displayed below.
The CCMDCTR is up to date as of June 2016 only, when the Editorial Group moved from the University of Bristol to the University of York.
Core search strategy used to inform the Cochrane Common Mental Disorders Group's specialised register: OVID MEDLINE A weekly search alert based on condition + RCT filter only 1. [MeSH Headings]: eating disorders/ or anorexia nervosa/ or binge‐eating disorder/ or bulimia nervosa/ or female athlete triad syndrome/ or pica/ or hyperphagia/ or bulimia/ or self‐injurious behavior/ or self mutilation/ or suicide/ or suicidal ideation/ or suicide, attempted/ or mood disorders/ or affective disorders, psychotic/ or bipolar disorder/ or cyclothymic disorder/ or depressive disorder/ or depression, postpartum/ or depressive disorder, major/ or depressive disorder, treatment‐resistant/ or dysthymic disorder/ or seasonal affective disorder/ or neurotic disorders/ or depression/ or adjustment disorders/ or exp antidepressive agents/ or anxiety disorders/ or agoraphobia/ or neurocirculatory asthenia/ or obsessive‐compulsive disorder/ or obsessive hoarding/ or panic disorder/ or phobic disorders/ or stress disorders, traumatic/ or combat disorders/ or stress disorders, post‐traumatic/ or stress disorders, traumatic, acute/ or anxiety/ or anxiety, castration/ or koro/ or anxiety, separation/ or panic/ or exp anti‐anxiety agents/ or somatoform disorders/ or body dysmorphic disorders/ or conversion disorder/ or hypochondriasis/ or neurasthenia/ or hysteria/ or munchausen syndrome by proxy/ or munchausen syndrome/ or fatigue syndrome, chronic/ or obsessive behavior/ or compulsive behavior/ or behavior, addictive/ or impulse control disorders/ or firesetting behavior/ or gambling/ or trichotillomania/ or stress, psychological/ or burnout, professional/ or sexual dysfunctions, psychological/ or vaginismus/ or Anhedonia/ or Affective Symptoms/ or *Mental Disorders/
2. [Title/Author Keywords]: (eating disorder* or anorexia nervosa or bulimi* or binge eat* or (self adj (injur* or mutilat*)) or suicide* or suicidal or parasuicid* or mood disorder* or affective disorder* or bipolar i or bipolar ii or (bipolar and (affective or disorder*)) or mania or manic or cyclothymic* or depression or depressive or dysthymi* or neurotic or neurosis or adjustment disorder* or antidepress* or anxiety disorder* or agoraphobia or obsess* or compulsi* or panic or phobi* or ptsd or posttrauma* or post trauma* or combat or somatoform or somati#ation or medical* unexplained or body dysmorphi* or conversion disorder or hypochondria* or neurastheni* or hysteria or munchausen or chronic fatigue* or gambling or trichotillomania or vaginismus or anhedoni* or affective symptoms or mental disorder* or mental health).ti,kf.
3. [RCT filter]: (controlled clinical trial.pt. or randomized controlled trial.pt. or (randomi#ed or randomi#ation).ab,ti. or randomly.ab. or (random* adj3 (administ* or allocat* or assign* or class* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or subsitut* or treat*)).ab. or placebo*.ab,ti. or drug therapy.fs. or trial.ab,ti. or groups.ab. or (control* adj3 (trial* or study or studies)).ab,ti. or ((singl* or doubl* or tripl* or trebl*) adj3 (blind* or mask* or dummy*)).mp. or clinical trial, phase ii/ or clinical trial, phase iii/ or clinical trial, phase iv/ or randomized controlled trial/ or pragmatic clinical trial/ or (quasi adj (experimental or random*)).ti,ab. or ((waitlist* or wait* list* or treatment as usual or TAU) adj3 (control or group)).ab.)
4. (1 and 2 and 3)
Records were screened for reports of RCTs within the scope of the Cochrane Common Mental Disorders Group. Secondary reports of RCTs were tagged to the appropriate study record. Similar weekly search alerts were also conducted on OVID Embase and PsycINFO, using relevant subject headings (controlled vocabularies) and search syntax, appropriate to each resource.
CCMDCTR search startegy for this review
CCMD's information specialist searched the Group's specialised register (CCMDCTR) using the following terms (condition and population only):
(i) CCMDCTR‐Studies Register: (Condition = obsess* or compulsi* or OCD or "anxiety disorder*") and (Condition or Comorbidity = autis* or asperger*) (ii) CCMDCTR‐References Register: ((obsess* or compulsi* or OCD or "anxiety disorder*") and (autis* or asperger* or kanner* or ASD or ASDs or (childhood and schizophren*) or (pervasive and development* and disorder*) or PDD or PDDs):ti,ab,kw,ky,mh,mc,emt
[Key to field tags. ti:title; ab:abstract; kw:keywords; ky:other keywords; mh:MeSH headings; mc:MeSH check words; emt:EMTREE headings]
Appendix 2. Other database searches
Cochrane Central Register of Controlled Trials (CENTRAL) (Issue 8 of 12, 2020) #1. (obsess* or compulsi* or OCD) #2. MeSH descriptor OBSESSIVE COMPULSIVE DISORDER, this term only #3. MeSH descriptor OBSESSIVE BEHAVIOR, this term only #4. MeSH descriptor COMPULSIVE BEHAVIOR explode all trees #5. (anxiety NEXT disorder*) #6. MeSH descriptor ANXIETY DISORDERS, this term only #7. (#1 or #2 or #3 or #4 or #5 or #6) #8. MeSH descriptor CHILD DEVELOPMENT DISORDERS, PERVASIVE explode all trees #9. (autis* or asperger* or kanner* or ASD or ASDs) #10. (childhood NEXT schizophren*) #11. ((pervasive and development* and disorder*) or PDD or PDDs) #12. (#8 or #9 or #10 or #11) #13. MeSH descriptor COMORBIDITY, this term only #14. (comorbid* or co‐morbid* or co‐occur* or cooccur* or concurren*).mp. #15. (#13 or #14) #16. (#12 and (#7 or #15)) [Final Set= ASD and (OCD or Comorditity)]
MEDLINE(R) ALL (Ovid) <1946 to 24 August 2020> Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 (obsess$ or compulsi$ or OCD).ti,ab,kf. 2 exp Obsessive‐Compulsive Disorder/ 3 Obsessive Behavior/ 4 exp Anxiety Disorders/ 5 anxiety disorder$.ti,ab,kf. 6 (1 or 2 or 3 or 4 or 5) 7 Neurodevelopmental Disorders/ 8 exp Autism Spectrum Disorder/ 9 exp Child Development Disorders, Pervasive/ 10 Schizophrenia, Childhood/ 11 (autis$ or asperger$ or kanner$ or ASD or ASDs or ASC).ti,ab,kf. 12 ((childhood$ adj3 schizophren$) or early onset schizophrenia).ti,ab,kf. 13 ("pervasive development$ disorder$" or PDD or PDDs).ti,ab,kf. 14 (7 or 8 or 9 or 10 or 11 or 12 or 13) 15 (comorbid$ or co morbid$ or co occur$ or cooccur$ or concurren$).mp. 16 Comorbidity/ 17 "Diagnosis, Dual (Psychiatry)"/ 18 (15 or 16 or 17) 19 controlled clinical trial.pt. 20 randomized controlled trial.pt. 21 (randomi#ed or randomi#ation or randomi#ing).ti,ab,kf. 22 (RCT or "at random" or (random* adj3 (administ* or allocat* or assign* or class* or cluster or control* or determine* or divide* or division or distribut* or expose* or fashion or number* or place* or pragmatic or quasi or recruit* or split or subsitut* or treat*))).ti,ab,kf. 23 placebo*.ab,ti,kf. 24 trial.ab,ti,kf. 25 groups.ab. 26 (control* and (trial or study or group*) and (placebo or waitlist* or wait* list* or ((treatment or care) adj2 usual))).ti,ab,kf,hw. 27 ((single or double or triple or treble) adj2 (blind* or mask* or dummy)).ti,ab,kf. 28 double‐blind method/ or random allocation/ or single‐blind method/ 29 or/19‐28 30 exp animals/ not humans.sh. 31 (29 not 30) 32 ((treatment* adj2 usual) or TAU or ((standard or routine or usual) adj care)).ti,ab,kf. 33 (waitlist* or wait* list* or (waiting adj (condition or control)) or WLC).ti,ab,kf. 34 (delay* treatment* or no treatment* or non treatment* or nontreatment* or minim* treatment* or untreated group* or untreated control* or without any treatment).ti,ab,kf. 35 (untreated adj3 (patients or participants or subjects or group* or control*)).ti,ab,kf. 36 (no intervention* or non intervention* or non‐intervention* or without any intervention*).ti,ab,kf. 37 ("receiv* nothing" or "standard control").ti,ab,kf. 38 ("no therap*" or "non therap*" or nontherap* or "minim* therap*" or "no contact" or pseudotherap* or "therap* as usual" or "usual therap*").ti,ab,kf. 39 ("reference group" or "observation group").ti,ab,kf. 40 ("convention* treatment" or "conventional *therap*" or "standard treatment*").ti,ab,kf. 41 ((attention or psychological) adj2 placebo).ti,ab,kf. 42 or/32‐41 43 (31 or 42) 44 (14 and (6 or 18) and 43)
Embase (Ovid) <1974 to 24 August 2020> Search Strategy ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 (obsess$ or compulsi$ or OCD).ti,ab,hw. 2 exp obsessive compulsive disorder/ 3 obsession/ 4 compulsion/ 5 anxiety disorder/ 6 anxiety disorder$.ti,ab,hw. 7 (1 or 2 or 3 or 4 or 5 or 6) 8 autism/ or asperger syndrome/ or childhood disintegrative disorder/ or "pervasive developmental disorder not otherwise specified"/ or rett syndrome/ 9 (autis$ or asperger$ or kanner$ or ASD or ASDs or ASC).ti,ab,hw. 10 ((childhood$ adj3 schizophren$) or early onset schizophrenia).ti,ab,hw. 11 ("pervasive development$ disorder$" or PDD or PDDs).ti,ab,hw. 12 neurodevelopmental disorder$.ti,ab,hw. 13 (8 or 9 or 10 or 11 or 12) 14 (comorbid$ or co morbid$ or co occur$ or cooccur$ or concurren$).mp. 15 comorbidity/ 16 dual diagnosis.ti,ab,hw. 17 (14 or 15 or 16) 18 randomized controlled trial/ 19 randomization.de. 20 Controlled clinical trial/ and (Disease management or Drug Therapy or Prevention or Rehabilitation or Therapy).fs. 21 *clinical trial/ 22 placebo.de. 23 placebo.ti,ab. 24 trial.ti. 25 (randomi#ed or randomi#ation or randomi#ing).ti,ab,kw. 26 (RCT or "at random" or (random* adj3 (administ* or allocat* or assign* or class* or cluster* or control* or determine* or divide* or division or distribut* or expose* or fashion or number* or place* or pragmatic* or recruit* or split or subsitut* or treat*))).ti,ab,kw. 27 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 28 (control* and (trial or study or group) and (placebo or waitlist* or wait* list* or ((treatment or care) adj2 usual))).ti,ab,kw,hw. 29 or/18‐28 30 ((animal or nonhuman) not (human and (animal or nonhuman))).de. 31 (29 not 30) 32 (13 and (7 or 17) and 31)
CINAHL(Cumulative Index to Nursing and Allied Health Literature) (EBSCOhost) (1982 to 23 September 2019) [Not searched for the update in Aug 2020, as CINAHL RCTS now part of CENTRAL]
Search Terms Search Options S1 TI ( obsess* or compulsi* or OCD ) OR AB ( obsess* or compulsi* or OCD ) OR SU ( obsess* or compulsi* or OCD ) S2 (MH "Obsessive‐Compulsive Disorder") S3 (MH "Compulsive Behavior") S4 (MH "Compulsive Personality Disorder") S5 (MH "Anxiety Disorders+") S6 TI "anxiety disorder*" OR AB "anxiety disorder*" OR SU "anxiety disorder*" S7 S1 OR S2 OR S3 OR S4 OR S5 OR S6 S8 (MH "Child Development Disorders, Pervasive+") S9 (MH "Autistic Disorder") OR (MH "Asperger Syndrome") S10 (MH "Schizophrenia, Childhood") S11 TI ( autis* or asperger* or kanner* or ASD or ASDs or ASC ) OR AB ( autis* or asperger* or kanner* or ASD or ASDs or ASC ) OR SU ( autis* or asperger* or kanner* or ASD or ASDs or ASC ) S12 TI childhood* N3 schizophren* OR AB childhood* N3 schizophren* OR SU childhood* N3 schizophren* S13 TI "early onset schizophrenia" OR AB "early onset schizophrenia" OR SU "early onset schizophrenia" S14 TI "pervasive development* disorder*" OR AB "pervasive development* disorder*" OR SU "pervasive development* disorder*" S15 TI ( PDD or PDDs ) OR AB ( PDD or PDDs ) OR SU ( PDD or PDDs ) S16 S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 S17 (MH "Diagnosis, Dual (Psychiatry)") S18 (MH "Comorbidity") S19 TI ( comorbid* or "co morbid*" or "co occur*" or cooccur* or concurren* ) OR AB ( comorbid* or "co morbid*" or "co occur*" or cooccur* or concurren* ) OR SU ( comorbid* or "co morbid*" or "co occur*" or cooccur* or concurren* ) S20 S17 OR S18 OR S19 S21 S7 OR S20 S22 S16 AND S21 S23 (MH "Randomized Controlled Trials") S24 (MH "Clinical Trials") S25 (MH "Comparative Studies") S26 (MH "Evaluation Research") S27 TI ( randomi#ed or randomi#ation or randomi#ing ) OR TI ( RCT or "at random" or (random* N3 (administ* or allocat* or assign* or class* or cluster or control* or determine* or divide* or division or distribut* or expose* or fashion or number* or place* or pragmatic or quasi or recruit* or split or subsitut* or treat*) ) OR TI placebo* OR TI trial OR TI groups OR TI ( (control* and (trial or study or group*) and (placebo or waitlist* or wait* list* or ((treatment or care) N12 usual))) ) OR TI ( ( ... S28 AB ( randomi#ed or randomi#ation or randomi#ing ) OR AB ( RCT or "at random" or (random* N3 (administ* or allocat* or assign* or class* or cluster or control* or determine* or divide* or division or distribut* or expose* or fashion or number* or place* or pragmatic or quasi or recruit* or split or subsitut* or treat*) ) OR AB placebo* OR AB trial OR AB groups OR AB ( (control* and (trial or study or group*) and (placebo or waitlist* or wait* list* or ((treatment or care) N12 usual))) ) OR AB ( ( ... S29 (S23 OR S24 OR S25 OR S26 OR S27 OR S28 )
PsycINFO (Ovid) (all years to 24 August 2020) Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1. (obsess* or compulsi* or OCD).ti,ab,id. 2. OBSESSIVE COMPULSIVE DISORDER/ 3. OBSESSIONS/ 4. exp COMPULSIONS/ 5. OBSESSIVE COMPULSIVE PERSONALITY DISORDER/ 6. anxiety disorder*.ti,ab.id. 7. ANXIETY DISORDERS/ 8. or/1‐7 9. exp PERVASIVE DEVELOPMENTAL DISORDERS/ 10. CHILDHOOD SCHIZOPHRENIA/ 11. (autis* or asperger* or kanner* or ASD or ASDs).ti,ab,id. 12. (childhood adj3 schizophren*).ti,ab,id. 13. ((pervasive and development* and disorder*) or PDD or PDDs).ti,ab,id. 14. or/9‐13 15. (comorbid* or co morbid* or co occur* or cooccur* or concurren*).mp. 16. COMORBIDITY/ or DUAL DIAGNOSIS/ 17. or/15‐16 18. treatment effectiveness evaluation.sh. 19. clinical trials.sh. 20. mental health program evaluation.sh. 21. randomly.ab. 22. randomi#ed.ti,ab,id. 23. (study or trial).ti. 24. ((singl* or doubl* or trebl* or tripl*) adj3 (blind* or mask* or dummy)).mp. 25. (control* adj3 (trial* or study or studies or group*)).ti,ab,id. 26. treatment outcome.md. 27. (waitlist* or wait* list*).ti,ab,id. 28. ((convention* or standard) adj (treatment* or therap* or psychotherap*)).ti,ab,id. 29. ((treatment* adj2 usual) or TAU or ((routine or standard or usual) adj2 (care or medication*))).ti,ab,id. 30. (“no" treatment* or non treatment* or nontreatment* or minim* treatment* or untreated group* or untreated control* or without any treatment).ti,ab,id. 31. (“no" intervention* or non intervention* or without any intervention*).ti,ab,id. 32. (("no" adj (contact or therap*)) or non therap* or nontherap* or minim* therap* or pseudotherap* or therap* as usual or usual therap*).ti,ab,id. 33. (untreated adj3 (patients or participants or subjects or group* or control*)).ti,ab,id. 34. (receiv* nothing or standard control or reference group or observation* group).ti,ab,id. 35. or/18‐34 34. (14 and (8 or 17) and 35)
Sociological Abstracts (ProQuest) (1963 to 24 August 2020)
((MAINSUBJECT.EXACT.EXPLODE("Autism") OR (ti(autis* OR asperger* OR kanner* OR ASD OR ASDs OR ASC) OR ab(autis* OR asperger* OR kanner* OR ASD OR ASDs OR ASC) OR su(autis* OR asperger* OR kanner* OR ASD OR ASDs OR ASC)) OR (ti(childhood* NEAR/3 schizophren*) OR ab(childhood* NEAR/3 schizophren*) OR su(childhood* NEAR/3 schizophren*)) OR (ti("early onset schizophrenia") OR ab("early onset schizophrenia") OR su("early onset schizophrenia")) OR (ti("pervasive development* disorder*") OR ab("pervasive development* disorder*") OR su("pervasive development* disorder*")) OR (ti(PDD OR PDDs) OR ab(PDD OR PDDs) OR su(PDD OR PDDs))) AND (((ti(obsess* OR compulsi* OR OCD) OR ab(obsess* OR compulsi* OR OCD) OR su(obsess* OR compulsi* OR OCD)) OR MAINSUBJECT.EXACT("Anxiety")) OR ((ti(comorbid* OR "co morbid*" OR "co occur*" OR cooccur* OR concurren*) OR ab(comorbid* OR "co morbid*" OR "co occur*" OR cooccur* OR concurren*) OR su(comorbid* OR "co morbid*" OR "co occur*" OR cooccur* OR concurren*) OR MAINSUBJECT.EXACT("Comorbidity")) OR (ti("dual diagnosis") OR ab("dual diagnosis") OR su("dual diagnosis"))))) OR (ti(neurodvelopment* disorder*) OR ab(neurodevelopment* disorder*) OR su(neurodevelopment* disorder*))
Web of Science Science Citation Core Collection (all years to 24 August 2020) SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH, ESCI
(TS=(obsess* or compulsi* or OCD) OR TS=(anxiety NEAR/2 disorder*) OR TS=(comorbid* or "co morbid*" or "co occur*" or cooccur* or concurren*) OR TS=("dual diagnosis")) AND (TS=(autis* or asperger* or kanner* or ASD or ASDs or ASC) OR TS=(childhood* NEAR/3 schizophren*) OR TS=("early onset*" NEAR/3 schizophren*) OR TS=(early‐onset* NEAR/3 schizophren*) OR TS=(pervasive NEAR/2 development*) OR TS=((pervasive NEAR/2 development*) OR (“neurodevelopment* disorder*”))) AND (TI= (randomi?ed or randomi?ation or randomi?ing) OR TI=(RCT or "at random" or (random* NEAR/3 (administ* or allocat* or assign* or class* or cluster or control* or determine* or divide* or division or distribut* or expose* or fashion or number* or place* or pragmatic or quasi or recruit* or split or subsitut* or treat*) )) OR TI= ((control* and (trial or study or group*) and (placebo or waitlist* or wait* list* or ((treatment or care) NEAR/12 usual)))) OR TI= (((single or double or triple or treble) NEAR/12 (blind* or mask* or dummy))) OR AB= (randomi?ed or randomi?ation or randomi?ing) OR AB=(RCT or "at random" or (random* NEAR/3 (administ* or allocat* or assign* or class* or cluster or control* or determine* or divide* or division or distribut* or expose* or fashion or number* or place* or pragmatic or quasi or recruit* or split or subsitut* or treat*) )) OR AB= ((control* and (trial or study or group*) and (placebo or waitlist* or wait* list* or ((treatment or care) NEAR/12 usual)))) OR AB= (((single or double or triple or treble) NEAR/12 (blind* or mask* or dummy))))
ERIC (Educational Resources Information Center) (EBSCOhost) (1966 to 24 August 2020)
S1 DE "Anxiety Disorders" S2 TI ( obsess* or compulsi* or OCD ) OR AB ( obsess* or compulsi* or OCD ) OR SU ( obsess* or compulsi* or OCD ) OR DE ( obsess* or compulsi* or OCD ) OR KW ( obsess* or compulsi* or OCD ) S3 TX anxiety N2 disorder* S4 S1 OR S2 OR S3 S5 DE "Pervasive Developmental Disorders" S6 DE "Asperger Syndrome" S7 TI ( autis* or asperger* or kanner* or ASD or ASDs or ASC ) OR AB ( autis* or asperger* or kanner* or ASD or ASDs or ASC ) OR SU ( autis* or asperger* or kanner* or ASD or ASDs or ASC ) OR DE ( autis* or asperger* or kanner* or ASD or ASDs or ASC ) OR KW ( autis* or asperger* or kanner* or ASD or ASDs or ASC ) S8 TX childhood* N3 schizophren* S9 TX "early onset" N3 schizophren* S10 TI pervasive N2 "development* disorder*" OR AB pervasive N2 "development* disorder*" OR SU pervasive N2 "development* disorder*" OR DE pervasive N2 "development* disorder*" OR KW pervasive N2 "development* disorder*" S11 TX PDD or PDDs S12 S5 OR S6 OR S7 OR S8 OR S10 OR S11 S13 DE "Comorbidity" S14 TX comorbid* or "co morbid*" or "co occur*" or cooccur* or concurren* S15 TX "dual diagnosis" S16 S13 OR S14 OR S15 S17 S4 AND S12 AND S16 S18 DE "Randomized Controlled Trials" S19 DE "Evaluation Research" S20 TI ( randomi?ed or randomi?ation or randomi?ing ) OR TI ( RCT or "at random" or (random* N3 (administ* or allocat* or assign* or class* or cluster or control* or determine* or divide* or division or distribut* or expose* or fashion or number* or place* or pragmatic or quasi or recruit* or split or subsitut* or treat*) ) OR TI placebo* OR TI trial OR TI groups OR TI ( (control* and (trial or study or group*) and (placebo or waitlist* or wait* list* or ((treatment or care) N12 usual))) ) OR TI ( ( ... S21 AB ( randomi?ed or randomi?ation or randomi?ing ) OR AB ( RCT or "at random" or (random* N3 (administ* or allocat* or assign* or class* or cluster or control* or determine* or divide* or division or distribut* or expose* or fashion or number* or place* or pragmatic or quasi or recruit* or split or subsitut* or treat*) ) OR AB placebo* OR AB trial OR AB groups OR AB ( (control* and (trial or study or group*) and (placebo or waitlist* or wait* list* or ((treatment or care) N12 usual))) ) OR AB ( ( ... S22 S18 OR S19 OR S20 OR S21 S23 S17 AND S22
Data and analyses
Comparison 1. Cognitive behavioural therapy intervention versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Treatment efficacy (change in OCD score) [YBOCS] | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐3.00 [‐8.02, 2.02] |
| 1.2 Total number of dropouts | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.22, 4.45] |
| 1.3 Severity of depressive symptoms (BDI) | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | ‐1.80 [‐11.50, 7.90] |
| 1.4 Severity of anxiety symptoms (BAI) | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | ‐3.20 [‐11.38, 4.98] |
| 1.5 Quality of life (Work and Social Adjustments Scale) | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 5.20 [‐1.41, 11.81] |
| 1.6 Family Accommodation Scale | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 5.60 [‐7.25, 18.45] |
1.1. Analysis.

Comparison 1: Cognitive behavioural therapy intervention versus control, Outcome 1: Treatment efficacy (change in OCD score) [YBOCS]
1.2. Analysis.

Comparison 1: Cognitive behavioural therapy intervention versus control, Outcome 2: Total number of dropouts
1.3. Analysis.

Comparison 1: Cognitive behavioural therapy intervention versus control, Outcome 3: Severity of depressive symptoms (BDI)
1.4. Analysis.

Comparison 1: Cognitive behavioural therapy intervention versus control, Outcome 4: Severity of anxiety symptoms (BAI)
1.5. Analysis.

Comparison 1: Cognitive behavioural therapy intervention versus control, Outcome 5: Quality of life (Work and Social Adjustments Scale)
1.6. Analysis.

Comparison 1: Cognitive behavioural therapy intervention versus control, Outcome 6: Family Accommodation Scale
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Russell 2013.
| Study characteristics | ||
| Methods | Participants randomised to two treatment groups, matched in duration | |
| Participants | 46 adolescents and adults with ASD and comorbid OCD | |
| Interventions | Two treatment groups: (1) CBT for OCD; (2) anxiety management | |
| Outcomes | Primary outcome measure: Y‐BOCS | |
| Notes | Anxiety management and CBT both effective in treating comorbid OCD in young people and adults with ASD, but there was no statistically significant difference between the two treatments. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table (1:1 ratio) managed by an investigator who was not a treating therapist. |
| Allocation concealment (selection bias) | High risk | No clear attempt to describe how concealment was maintained. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Maintenance of allocation concealment would be problematic due to the easily perceived differences in content of psychological therapies in the two treatment arms. This is a common difficulty in psychosocial studies. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Authors took measures to check the blinding procedure and minimise risk for clinician‐reported outcomes, but the risk of detection bias for self‐reported outcomes remains high. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Twenty out of 23 participants in each group completed treatment and some participants who did complete treatment did not complete all self‐report measures one month post‐treatment. |
| Selective reporting (reporting bias) | Low risk | Trial registration available online but registered retrospectively. |
| Other bias | Unclear risk | Some concerns regarding degree of adaptation of the intervention across the two arms, the detailed analysis plan for the cross‐over subset and dispersion across data for the hoarding data. |
AM: anxiety management; ASD: autism spectrum disorder; CBT: cognitive behavioural therapy; OCD: obsessive compulsive disorder; Y‐BOCS: Yale‐Brown Obsessive Compulsive Scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Storch 2015 | Focus of the study was not on treatment of OCD |
| Storch 2020 | Focus of the study was not on treatment of OCD |
| Vause 2017 | The study examined obsessive compulsive behaviour as an outcome but participants had not been diagnosed with OCD. |
| Vause 2020 | The study examined obsessive compulsive behaviour as an outcome but participants had not been diagnosed with OCD. |
| Wolters 2016 | The study measured autism symptoms as an outcome but participants had not been diagnosed with ASD. |
| Wood 2009 | Focus of the study was not on treatment of OCD |
| Wood 2015 | Focus of the study was not on treatment of OCD |
ASD: autism spectrum disorder; OCD: obsessive compulsive disorder
Characteristics of ongoing studies [ordered by study ID]
NCT02977962.
| Study name | Treatment of Anxiety in Late Adolescents with Autism (TALAA) |
| Methods | RCT |
| Participants | 44 participants, 16 to 21 years old. Inclusion criteria
Exclusion criteria
|
| Interventions | CBT: consisting of 16 weekly sessions up to 90 minutes each that helps the participant learn to cope with anxiety by facing fears, thinking more logically, and calming oneself. TAU: participants randomised to this condition will wait for a period of 16 weeks before receiving treatment in the context of the study. During this time, youth may receive psychotherapy and/or initiate or change current psychiatric medication (if applicable). |
| Outcomes | Change from baseline in anxiety severity on the Hamilton Anxiety Scale after 16 weeks of treatment. Change from baseline in anxiety severity on the Clinical Global Impressions Scale after 16 weeks of treatment. |
| Starting date | 30 November 2016 |
| Contact information | Adam B Lewin: alewin@health.usf.edu |
| Notes |
NCT04111874.
| Study name | Parent‐led cognitive‐behavioral teletherapy for anxiety in youth with ASD |
| Methods | RCT |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Experimental: low‐intensity therapist assistance (LTA). Parents will receive four 30‐minute supportive video calls with a therapist over the 12 weeks of treatment. Active comparator: standard therapist assistance (STA). Parents will receive ten 60‐minute supportive video calls with a therapist over the 12 weeks of treatment. |
| Outcomes | Primary outcome measures
Secondary outcome measures
|
| Starting date | 1 October 2019 |
| Contact information | Eric Alan Storch |
| Notes |
ASD: autism spectrum disorder; CBT: cognitive behavioural therapy; DSM: Diagnostic and Statistical Manual of Mental Disorders; IQ: intelligence quotient; OCD: obsessive compulsive disorder; RCT: randomised controlled trial; TAU: treatment as usual
Differences between protocol and review
In the protocol, we had stated under 'Data extraction and management' that we would pilot the data extraction form on at least three included studies. As only one study was included, we piloted the form on the one included study.
We have included the Family Accommodation Scale Parent Report (FAS PR) under the heading 'Secondary outcomes', as we consider this to be a valuable area to explore in future reviews (Flessner 2009). This outcome was not initially included in the protocol but was added during the review as there was a consensus amongst authors that this was an important outcome to consider.
Contributions of authors
SE conceived the review and, together with the other authors of the protocol (see acknowledgements section), contributed to the conception and design of the protocol.
SE, MK, KM, DM, EU and NM contributed to the title and abstract screening of studies. SE, EU, DM and MK contributed to the full‐text screening of studies. DM and MK contributed to the data extraction. SE, MK, EU, DM and NM contributed to the risk of bias assessments. All authors contributed to the drafting and revising of the draft for important intellectual content.
Sources of support
Internal sources
-
North West Boroughs Healthcare NHS Foundation Trust, UK
Provided research time.
External sources
-
Cochrane, UK
Formal training course and informal support.
-
National Institue for Health Research (NIHR) , UK
Cochrane Infrastructure funding to the Common Mental Disorders Cochrane Review Group supported DM, EU and NM time on this review.
Declarations of interest
SE: none DM: none KM: none EU: none MK: none NM: none
New
References
References to studies included in this review
Russell 2013 {published data only}
- Russell AJ, Jassi A, Fullana MA, Mack H, Johnston K, Heyman I, et al. Cognitive behaviour therapy for comorbid obsessive-compulsive disorder in high-functioning autism spectrum disorders: a randomised controlled trial. Depression and Anxiety 2013;30(8):697-708. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Storch 2015 {published data only}
- NCT01563003. Cognitive behavioral therapy for anxiety disorders in adolescents with autism. ClinicalTrials.gov/show/NCT01563003 (first received 26 March 2012).
- Storch EA, Lewin AB, Collier AB, Arnold E, De Nadai AS, Dane BF, et al. A randomized controlled trial of cognitive-behavioral therapy versus treatment as usual for adolescents with autism spectrum disorders and comorbid anxiety. Depression and Anxiety 2015;32:174-81. [DOI: 10.1002/da.22332] [DOI] [PMC free article] [PubMed] [Google Scholar]
Storch 2020 {published data only}
- Storch EA, Schneider SC, De Nadai AS, Selles RR, McBride NM, Grebe SC, et al. A pilot study of family-based exposure-focused treatment for youth with autism spectrum disorder and anxiety. Child Psychiatry & Human Development 2020;51(2):209-19. [DOI: 10.1007/s10578-019-00923-3] [DOI] [PubMed] [Google Scholar]
Vause 2017 {published data only}
- Vause T, Neil N, Jaksic H, Jackiewicz G, Feldman M. Preliminary randomized trial of function-based cognitive-behavioral therapy to treat obsessive compulsive behavior in children with autism spectrum disorder. Focus on Autism and Other Developmental Disabilities 2017;32(3):218-28. [DOI: 10.1177/1088357615588517] [DOI] [Google Scholar]
Vause 2020 {published data only}
- Vause T, Jaksic H, Neil N, Frijters JC, Jackiewicz G, Feldman M. Functional behavior-based cognitive-behavioral therapy for obsessive compulsive behavior in children with autism spectrum disorder: a randomized controlled trial. Journal of Autism & Developmental Disorders 2020;50(7):2375-88. [DOI: ] [DOI] [PubMed] [Google Scholar]
Wolters 2016 {published data only}
- Wolters LH, de Haan E, Hogendoorn SM, Boer F, Prins PJ. Severe pediatric obsessive compulsive disorder and co-morbid autistic symptoms: effectiveness of cognitive behavioral therapy. Journal of Obsessive-Compulsive and Related Disorders 2016;10:69-77. [DOI: 10.1016/j.jocrd.2016.06.002] [DOI] [Google Scholar]
Wood 2009 {published data only (unpublished sought but not used)}
- Drahota A, Wood J, Sze K, Dyke M. Effects of cognitive behavioral therapy on daily living skills in children with high-functioning autism and concurrent anxiety disorders. Journal of Autism & Developmental Disorders 2011;41(3):257-65. [DOI: 10.1007/s10803-010-1037-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drahota AM, Wood JJ. Intervening with Independent Daily Living Skills for High-functioning Children with Autism and Concurrent Anxiety Disorders. Los Angeles (USA): Ann Arbor University of California, 2008. [Google Scholar]
- NCT00280670. CBT for comorbid anxiety disorders in children with autism, Asperger syndrome, or PDD-NOS (BIACA). ClinicalTrials.gov/show/NCT00280670 (first received 23 January 2006).
- Wood J, Drahota A, Sze K, Har K, Chiu A, Langer D. Cognitive behavioural therapy for anxiety in children with autism spectrum disorders: a randomised, controlled trial. Journal of Child Psychology and Psychiatry 2009;50(3):224-34. [DOI: 10.1111/j.1469-7610.2008.01948.x.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wood 2015 {published data only}
- NCT01177969. CBT for anxiety disorders in autism: adapting treatment for adolescents. ClinicalTrials.gov/show/NCT01177969 (first received 9 August 2009).
- Wood JJ, Ehrenreich-May J, Alessandri M, Fujii C, Renno P, Laugeson E, et al. Cognitive behavioral therapy for early adolescents with autism spectrum disorders and clinical anxiety: a randomized, controlled trial. Behavior Therapy 2015;46(1):7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
NCT02977962 {published data only}
- NCT02977962. Treatment of anxiety in late adolescents with autism (TALAA). Clinicaltrials.gov/show/NCT02977962 (first received 30 Novemver 2016).
NCT04111874 {published data only}
- NCT04111874. Parent-led cognitive-behavioral teletherapy for anxiety in youth with ASD. ClinicalTrials.gov/show/NCT04111874 (first received 1 October 2019).
Additional references
Achenbach 1983
- Achenbach TM, Edelbrock CS. Manual for the Child Behaviour Checklist and Revised Child Behaviour Profile. Burlington (VT): University of Vermont Department of Psychiatry, 1983. [Google Scholar]
Akaltun 2017
- Akaltun I, Kara S, Kara T. The relationship between toxoplasma Gondii IgG antibodies and generalized anxiety disorder and obsessive-compulsive disorder in children and adolescents. Nordic Journal of Psychiatry March 2017;72(1):57-62. [DOI] [PubMed] [Google Scholar]
Angst 2004
- Angst J, Gamma A, Endrass J, Goodwin R, Ajdacic V, Eich D, et al. Obsessive-compulsive severity spectrum in the community: prevalence, comorbidity and course. European Archives of Psychiatry and Clinical Neuroscience 2004;254(3):156-64. [DOI] [PubMed] [Google Scholar]
Anholt 2010
- Anholt GE, Cath DC, Van Oppen P, Eikelenboom M, Smit JH, Van Megen H, et al. Autism and ADHD symptoms in patients with OCD: are they associated with specific OC symptom dimensions or OC symptom severity? Journal of Autism and Developmental Disorders 2010;40(5):580-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
APA 2013
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders. 5th edition. Arlington (VA): American Psychiatric Publishing, Inc, 2013. [Google Scholar]
Baron‐Cohen 2004
- Baron-Cohen S. The cognitive neuroscience of autism. Journal of Neurology, Neurosurgery & Psychiatry 2004;75(7):945-8. [DOI: 10.1136/jnnp.2003.018713] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4:561-71. [DOI] [PubMed] [Google Scholar]
Beck 1996
- Beck J, Steer R, Brown G. Manual for the Beck Depression Inventory-II. 2nd edition. San Antonio (TX): Psychological Corporation, 1996. [Google Scholar]
Beck 1998
- Beck A, Epstein N, Brown G, Steer R. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology 1998;56(6):893-7. [DOI] [PubMed] [Google Scholar]
Beck 2001
- Beck J, Beck A, Jolly B. Manual for the Beck Youth Inventories of Emotional and Social Impairment. 1st edition. San Antonio (TX): Psychological Corporation, 2001. [Google Scholar]
Bedford 2020
- Bedford SA, Hunsche MC, Kerns CM. Co-occurrence, assessment and treatment of Obsessive Compulsive Disorder in children and adults with Autism Spectrum Disorder. Current Psychiatry Reports 2020;53:1603-11. [DOI] [PubMed] [Google Scholar]
Bejerot 2001
- Bejerot S, Nylander L, Lindström E. Autistic traits in obsessive-compulsive disorder. Nordic Journal of Psychiatry 2001;55(3):169-76. [DOI] [PubMed] [Google Scholar]
Carlisi 2017
- Carlisi C, Normal L, Murphy C, Chrisakou A, Chantiluke K, et al. Shared and disorder-specific neurocomputational mechanisms of decision-making in autism spectrum disorder and obsessive-compulsive disorder. Cerebral Cortex 2017;27(12):5804-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Casey 2007
- Casey P, Kelly B. Fish's Clinical Psychopathology. Signs and Symptoms in Psychiatry. 3rd edition. Vol. 1. London (UK): Royal College of Psychiatrists, 2007. [Google Scholar]
Covidence 2020 [Computer program]
- Covidence. Melbourne, Australia: Veritas Health Innovation, accessed 17 June 2020. Available at covidence.org.
Dahlgren 2003
- Dahlgren S, Sandberg AD, Hjelmquist E. The non-specificity of theory of mind deficits: evidence from children with communication disabilities. European Journal of Cognitive Psychology 2003;15:129-55. [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG. Chapter 9: Identifying and measuring heterogeneity. In: Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ekman 2018
- Ekman E, Arto J. The cognitive profile of persons with Obsessive Compulsive Disorder with and without Autistic Spectrum Disorder. Clinical Practice & Epidemiology in Mental Health 2018;14:304-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elliott 2014
- Elliott S, Fitzsimons L. Modified CBT for treatment of OCD in a 7-year-old boy with ASD - a case report. Journal of Child and Adolescent Psychiatric Nursing 2014;27:156-9. [DOI] [PubMed] [Google Scholar]
Flessner 2009
- Flessner C, Sapyta J, Garcia A. Examining the psychometric properties of the Family Accommodation Scale-Parent Report (FAS-PR). Journal of Psychopathology and Behavioural Assessment 2009;31(1):38-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Foa 2002
- Foa EB, Huppert JD, Leiberg S, Langnerr R, Kichic R, Hajcak G, et al. The Obsessive-Compulsive Inventory: development and validation of a short version. Psychological Assessment 2002;14:485-96. [PubMed] [Google Scholar]
Gava 2009
- Gava I, Barbui C, Aguglia E, Carlino D, Churchill R, De Vanna M, et al. Psychological treatments compared with treatment as usual for obsessive compulsive disorder. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD005333. [DOI: 10.1002/14651858.CD005333.pub2] [DOI] [PubMed] [Google Scholar]
Geller 2008
- Geller D, Wieland N, Carey K, Vivas F, Petty C et al. Perinatal factors affecting expression of obsessive compulsive disorder in children and adolescents. Journal of Child and Adolesceny Psychopharmacology 2008;18:373-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Greenberg 2009
- Greenberg B, Altemus M, Murphy D. The role of neurotransmitters and neurohormones in obsessive-compulsive disorder. International Review of Psychiatry 2009;9(1):31-44. [Google Scholar]
Hauck 1995
- Hauck M, Fein D, Waterhouse L, Feinstein C. Social initiations by autistic children to adults and other children. Journal of Autism and Developmental Disorders 1995;25(6):579-95. [DOI] [PubMed] [Google Scholar]
Havdahl 2019
- Havdahl A, Bishop S. Heterogeneity in prevalence of co-occurring psychiatric conditions in autism. Lancet Psychiatry 2019;6:794-5. [DOI] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Altman DG, Sterne JA, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (updated June 2017). Cochrane, 2017. Available from handbook.cochrane.org.
Higgins 2021
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane 2021. Available from www.training.cochrane.org/handbook.
Hill 2004
- Hill E, Berthoz S, Frith U. Cognitive processing of own emotions in individuals with autism spectrum disorders and their relatives. Journal of Autism and Developmental Disorders 2004;4:229-35. [DOI] [PubMed] [Google Scholar]
Iniesta‐Sepulveda 2018
- Iniesta-Sepulveda M, Nadeau JM, Ramos A, Kay B, Reimann BC, Storch EA. An initial case series of intensive cognitive-behavioural therapy for Obsessive Compulsive Disorder in adolescents with Autism Spectrum Disorder. Child Psychiatry & Human Development 2018;49(1):9-19. [DOI] [PubMed] [Google Scholar]
Ivarsson 2008
- Ivarsson T, Melin K. Autism spectrum traits in children and adolescents with Obsessive-Compulsive Disorder (OCD). Journal of Anxiety Disorders 2008;22(6):969-78. [DOI] [PubMed] [Google Scholar]
Kessler 2005
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSMIV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 2005;62:59-62. [DOI] [PubMed] [Google Scholar]
Kim 1990
- Kim SW, Dysken MW, Kuskwoski M. The Yale-Brown Obsessive Compulsive Scale: a reliability and validity study. Psychiatry Research 1990;34(1):99-106. [DOI] [PubMed] [Google Scholar]
Komossa 2010
- Komossa K, Depping AM, Meyer M, Kissling W, Leucht S. Second-generation antipsychotic drugs for obsessive compulsive disorder. Cochrane Database of Systematic Reviews 2010, Issue 12. Art. No: CD008141. [DOI: 10.1002/14651858.CD008141.pub2] [DOI] [PubMed] [Google Scholar]
Kose 2018
- Kose LK, Fox L, Storch EA. Effectiveness of cognitive behavioural therapy for individuals with autism spectrum disorders and comorbid obsessive - compulsive disorder: a review of the research. Journal of Developmental & Physical Disabilities 2018;30(1):69-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kovacs 1985
- Kovacs M. The Children's Depression Inventory. Psychopharmacology Bulletin 1985;21:995-8. [PubMed] [Google Scholar]
Kuhn 2009
- Kuhn D, Hardesty S, Sweeney N. Assessment and treatment of excessive straightening and destructive behaviour in an adolescent diagnosed with Autism. Journal of Applied Behavioural Analysis 2009;42:355-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuno 2018
- Kuno M, Yoshiyuki H, Shimizu E. White matter features associated with autistic traits in obsessive compulsive disorder. Front Psychiatry 2018;9:216. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kushi 2019
- Kushi A, Anagnostoa E, Hammill C, Duez P, Brian J, Iaboni A, et al. Examining the overlap and heterogeneity in ASD, ADHD and OCD: a data driven diagnosis agnostic approach. Translational Psychiatry 2019;9:318. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lai 2019
- Lai M, Kassee C, Besney R, Bonato S, Hull L, et al. Prevalence of co-occurring mental health diagnoses in the autism population: a systematic review and meta-analysis. Lancet Psychiatry 2019;6:819-29. [DOI] [PubMed] [Google Scholar]
Le Couter 1989
- Le Couter A, Rutter M, Lord C, Rios P, Robertson S, Holdgrafer M, et al. Autism Diagnostic Interview: a standardized investigator-based instrument. Journal of Autism and Developmental Disorders 1989;19(3):363-87. [DOI] [PubMed] [Google Scholar]
Lehmkuhl 2008
- Lehmkuhl H, Storch E, Bodfish J, Geffken G. Brief report: exposure and response prevention for Obsessive Compulsive Disorder in a 12-year-old with autism. Journal of Autism and Developmental Disorders 2008;38:977-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leyfer 2006
- Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, et al. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. Journal of Autism and Developmental Disorders 2006;36(7):849-61. [DOI] [PubMed] [Google Scholar]
Liu 2019
- Liu D, Cao H, Kural K, Fang Q, Zhang F. Integrative analysis of shared genetic pathogenesis by Autism Spectrum Disorder and Obsessive Compulsive Disorder. Bioscience Reports 2019;39(12):BSR20191942. [DOI: 10.1042/BSR20191942] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lord 1989
- Lord C, Rutter M, Goode S, Le Couteur A. Autism Diagnostic Observation Schedule: A standardised observation of communicative and social behaviour. Journal of Autism and Developmental Disorders 1989;19:185-212. [DOI] [PubMed] [Google Scholar]
Lord 1995
- Lord C. Treatment of a high-functioning adolescent with autism: a cognitive-behavioural approach. In: Reinecke M, Dattilio F, Freeman A, editors(s). Cognitive Therapy with Children and Adolescents: A Casebook for Clinical Practice. 1st edition. New York (NY): Guilford, 1995:394-404. [Google Scholar]
Macintosh 2004
- Macintosh KE, Dissanayaka C. The similarities and differences between Autistic disorder and Asperger's disorder: a review of the empirical evidence. Journal of Child Psychology and Psychiatry 2004;45(3):421-34. [DOI] [PubMed] [Google Scholar]
Mack 2010
- Mack H, Fullana MA, Russell AJ, Mataix-Cols D, Nakatani E, Heyman I. Obsessions and compulsions in children with Asperger's syndrome or high-functioning Autism: a case control study. Australia and New Zealand Journal of Psychiatry 2010;44(12):1082-88. [DOI] [PubMed] [Google Scholar]
Maenner 2020
- Maenner MJ, Shaw KA, Baio J, Washington A, Patrick M, DiRienzo M, et al. Prevalence of Autism Spectrum Disorder among children aged 8 years - Autism and Developmental Disabilities Network, 11 sites, United States, 2016. MMWR Surveillance Summaries 2020;64(4):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martin 2020
- Martin A, Jassi A, Cullen A, Broadbent M, Downs J, Krebs G. Co-occurring obsessive compulsive disorder and autism spectrum disorder in young people: prevalence, clinical characteristics and outcomes. European Child & Adolescent Psychiatry 2020;29(11):1603-11. [DOI: 10.1007/s00787-020-01478-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
Masi 2017
- Masi A, DeMayo M, Glozier N, Guastella A. An overview of Autism Spectrum Disorder, heterogeneity and treatment options. Neuroscience Bulletin 2017;33(2):183-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
McDougle 1995
- McDougle CJ, Kresch LE, Goodman WK, Naylor ST, Volkmar FR, Cohen DJ, et al. A case-controlled study of repetitive thoughts and behaviour in adults with autistic disorder and obsessive compulsive disorder. American Journal of Psychiatry 1995;152(5):772-7. [DOI] [PubMed] [Google Scholar]
Meier 2015
- Mier SM, Petersen L, Schendel DE, Mattheisen M, Mortensen PB, Mors O. Obsessive-Compulsive disorder and Autism Spectrum disorders: longitudinal and offspring risk. PLoS One Nov 2015;10:e0141703. [DOI] [PMC free article] [PubMed] [Google Scholar]
Milton 2018
- Milton D, on behalf of the Neurodiversity Manifesto Steering Group. A critique of the use of Applied Behavioural Analysis (ABA). kar.kent.ac.uk/69268/ (accessed 1 September 2021).
Mundt 2002
- Mundt J, Marks I, Greist J, Shear K. The work and social adjustment scale: a simple accurate measure of impairment in functioning. British Journal of Psychiatry 2002;180:461-4. [DOI] [PubMed] [Google Scholar]
Murray 2015
- Murray K, Jassi A, Mataix-Cols D, Barrow D, Krebs G. Outcomes of cognitive behaviour therapy for obsessive-compulsive disorder in young people with and without autism spectrum disorders: a case controlled study. Psychiatry Research 2015;28(1):8-13. [DOI] [PubMed] [Google Scholar]
Nadeau 2014
- Nadeau J, Arnold E, Storch E, Lewin A. Family cognitive-behavioural treatment for a child with autism and comorbid obsessive compulsive disorder. Clinical Case Studies 2014;13(1):22-36. [Google Scholar]
Neuhaus 2010
- Neuhaus E, Beauchaine TP, Bernier R. Neurobiological correlates of social functioning in Autism. Clinical Psychology Review 2010;30(6):733-48. [DOI] [PubMed] [Google Scholar]
NICE 2005
- National Institute for Health and Care Excellence. Obsessive-compulsive disorder and body dysmorphic disorder: treatment. Clinical guideline 31; November 2005. www.nice.org.uk/guidance/cg31 (accessed 17 June 2020).
NICE 2012
- National Institute for Health and Care Excellence. Autism Spectrum Disorder in adults: diagnosis and management. Clinical guideline 142; June 2012. www.nice.org.uk/guidance/cg142 (accessed 17 June 2020).
NICE 2013
- National Institute for Health and Care Excellence. Autism spectrum disorder in under 19s: support and management. Clinical guideline 170; August 2013. www.nice.org.uk/guidance/cg170 (accessed 17 June 2020).
O'Connor 2008
- O'Connor K, Kirk I. Brief report: atypical social cognition and social behaviours in autism spectrum disorder: a different way of processing rather than impairment. Journal of Autism and Developmental Disorders 2008;38(10):1989-97. [DOI] [PubMed] [Google Scholar]
O'Kearney 2006
- O'Kearney RT, Anstey K, Von Sanden C. Behavioural and cognitive behavioural therapy for obsessive compulsive disorder in children and adolescents. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No: CD004856. [DOI: 10.1002/14651858.CD004856.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Olatunji 2013
- Olatunji BO, Davis ML, Powers MB, Smits JA. Cognitive-behavioural therapy for obsessive-compulsive disorder: a meta-analysis of treatment outcome and moderators. Journal of Psychiatric Research 2013;47(1):33-41. [DOI] [PubMed] [Google Scholar]
Perez 2012
- Perez P. Differential diagnosis between obsessive compulsive disorder and restrictive and repetitive behavioural patterns, activities and interests in autism spectrum disorders. Revista de Psiquiatria y Salud Mental 2012;6(4):178-86. [DOI] [PubMed] [Google Scholar]
Reaven 2010
- Reaven J, Hepburn S. Cognitive-behavioural treatment of obsessive-compulsive disorder in a child with Asperger syndrome. Autism 2003;7:145-64. [DOI] [PubMed] [Google Scholar]
Reed 2019
- Reed G, First M, Kogan C, Hyman S, Gureje O, et al. Innovations and changes in the ICD-11 classification of mental, behavioural and neurodevelopmenetal disorders. World Psychiatry 2019;18(1):3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rice 2009
- Rice C. Prevalence of autism spectrum disorders - autism and developmental disabilities monitoring network, United States, 2006. Morbidity and Mortality Weekly Report 2009;58(SS10):1-20. [PubMed] [Google Scholar]
Roche 2020
- Roche L, Adams D, Clark M. Research priorities of the autism community: a systematic review of key stakeholder perspectives. Autism 2020;2:336-48. [DOI] [PubMed] [Google Scholar]
Rosenfeld 1992
- Rosenfeld R, Dar R, Anderson D, Kobak K, Greist J. A computer-administered version of the Yale-Brown Obsessive Compulsive Scale. Psychological Assessment 1992;4:329-32. [Google Scholar]
Russell 2005
- Russell AJ, Mataix-Cols D, Anson M, Murphy DG. Obsessions and compulsions in Asperger Syndrome and high-functioning Autism. British Journal of Psychiatry 2005;186:525-8. [DOI] [PubMed] [Google Scholar]
Russell 2009
- Russell A, Mataix-Cols D, Anson MA, Murphy DG. Psychological treatment for obsessive compulsive disorder in people with autism spectrum disorders - a pilot study. Psychotherapy and Psychosomatics 2009;78:59-61. [DOI] [PubMed] [Google Scholar]
Ruta 2010
- Ruta L, Mugno D, D'Arrigo V, Vitiello B, Mazzone L. Obsessive-compulsive traits in children and adolescents with autism. European Child and Adolescent Psychiatry 2010;19:17-24. [DOI] [PubMed] [Google Scholar]
Ruzzano 2015
- Ruzzano L, Borsboom D, Geurts HM. Repetitive behaviours in autism and obsessive compulsive disorder: new perspectives from a network analysis. Journal of Autism and Developmental Discorders 2015;45:192-202. [DOI] [PubMed] [Google Scholar]
Santore 2020
- Santore L, Gerber A, Gioia A, Bianchi R, Talledo F, Peris T, et al. Felt but not seen: observed restricted repetitive behaviours are associated with self report but not parent report obsessive compulsive disorder. Autism 2020;24:983-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Savovic 2015
- Savovic J, Turner R, Mawdsley D, Higgins J, Sterne J. A new large-scale meta-epidemiological study on bias in randomized trials using routinely collected risk-of-bias assessments by Cochrane reviewers: results from the ROBES study. Trials 2015;16(Suppl 2):P168. [Google Scholar]
Scahill 2014
- Scahill L, Dimitropoulos A, McDougle C, Aman M, Feurer I, et al. Children's Yale-Brown Obsessive Compulsive Scale in Autism Spectrum Disorder: component structure and correlates of symptom checklist. Journal of the American Academy of Child and Adolescent Psychiatry 2013;53(1):97-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shaw 2020
- Shaw KA, Maenner MJ, Baio J, Washington A, Christensen DL, Wiggins LD, et al. Early identification of autism spectrum disorder among children aged 4 years - Early Autism and Developmental Disabilities Monitoring Network, Six Sites, United States, 2016. MMWR Surveillance Summaries 2020;69:1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sheehan 2000
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry 1998;59 Suppl 20:22-33;quiz 34-57. [PubMed]
Shuid 2021
- Shuid A, Jayusman P, Shuid N, Ismail J, Norazlin K et al. Association between viral infections and risk of autistic disorder: an overview. International Journal of Environmental Research and Public Health March 2021;18(6):2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sofronoff 2005
- Sofronoff K, Attwood T, Hinton S. A randomised controlled trial of a CBT intervention for anxiety in children with Asperger syndrome. Journal of Child Psychology and Psychiatry 2005;46(11):1152-60. [DOI] [PubMed] [Google Scholar]
Soomro 2008
- Soomro GM, Altman D, Rajagopal S, Oakley-Browne M. Selective serotonin re-uptake inhibitors (SSRIs) versus placebo for obsessive compulsive disorder (OCD). Cochrane Database of Systematic Reviews 2008, Issue 1. Art. No: CD001765. [DOI: 10.1002/14651858.CD001765.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Spence 1998
- Spence SH. A measure of anxiety symptoms among children. Behaviour Research and Therapy 1998;36:545-66. [DOI] [PubMed] [Google Scholar]
Stewart 2004
- Stewart SE, Geller DA, Jenike M, Pauls D, Shaw D, Mullin B, et al. Long term outcome of pediatric obsessive-compulsive disorder: a meta-analysis and qualitative review of the literature. Acta Psychiatrica Scandinavica 2004;110(1):4-13. [DOI] [PubMed] [Google Scholar]
Stewart 2016
- Stewart, E, Cancilliere MK, Franklin M. Elevated autism spectrum disorder traits in young children with OCD. Child Psychiatry and Human Development 2016;47(6):993-1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Storch 2004
- Storch EA, Murphy TK, Geffken GR, Soto O, Sajid M, Allen P, et al. Psychometric evaluation of the Childrens' Yale-Brown Obsessive-Compulsive Scale. Psychiatry Research 2004;129:91-8. [DOI] [PubMed] [Google Scholar]
Tsuchiyagaito 2017
- Tsuchiyagaito A, Hirano Y, Asano K, Oshima F, Nagaoka S, Takebayashi Y, et al. Cognitive-behavioural therapy for obsessive-compulsive disorder with and without autism spectrum disorder: grey matter differences associated with poor outcome. Frontiers in Psychiatry 2017;15(8):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
Valentine 2010
- Valentine JC, Pigott TD, Rothstein HR. 'How many studies do you need?'. A primer on statistical power for meta-analysis. Journal of Educational and Behavioural Statistics 2010;Volume 35:215-47. [Google Scholar]
Van Steensel 2011
- Van Steensel FJ, Bögels SM, Perrin S. Anxiety disorders in children and adolescents with autistic spectrum disorders: a meta-analysis. Clinical Child and Family Psychology Review 2011;14(3):302-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Steensel 2015
- Van Steensel F, Bogels S. CBT for anxiety disorders in children with and without autism spectrum disorders. Journal of Consulting and Clinical Psychology June 2015;83(3):512-23. [DOI] [PubMed] [Google Scholar]
WHO 1992
- World Health Organization (WHO). The International Classification of Disease. Geneva (Switzerland): World Health Organization, 1992. [Google Scholar]
WHO 1997
- World Health Organization. WHOQOL: Measuring Quality of Life. www.who.int/healthinfo/survey/whoqol-qualityoflife/en/ (accessed 17 June 2020).
Wiltshire 2017
- Wiltshire C. The problem of reporting bias in behavioural intervention studies: lessons from the PACE trial. Journal of Health Psychology 2017;22(9):1128-33. [DOI] [PubMed] [Google Scholar]
Wu 2012
- Wu Y, Liu X, Deng W, Zhao G, Wang Q, et al. Advanced paternal age increases the risk of schizophrenia and obsessive-compulsive disorder in a Chinese Han population. Psychiatry Research 2012;198:353-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2016
- Wu S, Wu F, Ding Y, Hou J, Bi J, et al. Advanced parental age and autism risk in children: a systematic review and meta-analysis. Acta Psychiatrica Scandinavica 2017;135(1):29-41. [DOI] [PubMed] [Google Scholar]
Yong 2021
- Yong Z, Yunlong D, Gao Y, Xuena X, Yanli X, et al. Prenatal, perinatal, and postnatal factors associated with autism spectrum disorder cases in Xuzhou, China. Translational Pediatrics 2021;10(3):635-646. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zigmond 1982
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavia 1982;67(6):361-70. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Elliott 2018
- Elliott SJ, McMahon BM, Leech AM. Behavioural and cognitive behavioural therapy for obsessive compulsive disorder (OCD) in individuals with autism spectrum disorder (ASD). Cochrane Database of Systematic Reviews 2018, Issue 11. Art. No: CD013173. [DOI: 10.1002/14651858.CD013173] [DOI] [PMC free article] [PubMed] [Google Scholar]


