Abstract
Background
Insufficient physical activity is one of four primary risk factors for non‐communicable diseases such as stroke, heart disease, type 2 diabetes, cancer and chronic lung disease. As few as one in five children aged 5 to 17 years have the physical activity recommended for health benefits. The outside‐school hours period contributes around 30% of children's daily physical activity and presents a key opportunity for children to increase their physical activity. Testing the effects of interventions in outside‐school hours childcare settings is required to assess the potential to increase physical activity and reduce disease burden.
Objectives
To assess the effectiveness, cost‐effectiveness and associated adverse events of interventions designed to increase physical activity in children aged 4 to 12 years in outside‐school hours childcare settings.
Search methods
We searched CENTRAL, MEDLINE, Embase, ERIC and SportsDISCUS to identify eligible trials on 18 August 2020. We searched two databases, three trial registries, reference lists of included trials and handsearched two physical activity journals in August 2020. We contacted first and senior authors on articles identified for inclusion for ongoing or unpublished potentially relevant trials in August 2020.
Selection criteria
We included randomised controlled trials, including cluster‐randomised controlled trials, of any intervention primarily aimed at increasing physical activity in children aged 4 to 12 years in outside‐school hours childcare settings compared to usual care. To be eligible, the interventions must have been delivered in the context of an existing outside‐school hours childcare setting (i.e. childcare that was available consistently throughout the school week/year), and not set up in the after‐school period for the purpose of research. Two review authors independently screened titles and abstracts of identified papers with discrepancies resolved via a consensus discussion. A third review author was not required to resolve disagreements.
Data collection and analysis
Two review authors independently extracted data and assessed the risk of bias of included trials with discrepancies resolved via a consensus discussion; a third review author was not required to resolve disagreements. For continuous measures of physical activity, we reported the mean difference (MD) with 95% confidence intervals (CIs) in random‐effects models using the generic inverse variance method for each outcome. For continuous measures, when studies used different scales to measure the same outcome, we used standardised mean differences (SMDs). We conducted assessments of risk of bias of all outcomes and evaluated the certainty of evidence (GRADE approach) using standard Cochrane procedures.
Main results
We included nine trials with 4458 participants. Five trials examined the effectiveness of staff‐based interventions to change practice in the outside‐school hours childcare setting (e.g. change in programming, activities offered by staff, staff facilitation/training). Two trials examined the effectiveness of staff‐ and parent‐based interventions (e.g. parent newsletters/telephone calls/messages or parent tool‐kits in addition to staff‐based interventions), one trial assessed staff‐ and child‐based intervention (e.g. children had home activities to emphasise physical activity education learnt during outside‐school hours childcare sessions in addition to staff‐based interventions) and one trial assessed child‐only based intervention (i.e. only children were targeted).
We judged two trials as free from high risk of bias across all domains. Of those studies at high risk of bias, it was across domains of randomisation process, missing outcome data and measurement of the outcome.
There was low‐certainty evidence that physical activity interventions may have little to no effect on total daily moderate‐to‐vigorous physical activity compared to no intervention (MD 1.7 minutes, 95% CI –0.42 to 3.82; P = 0.12; 6 trials; 3042 children). We were unable to pool data on proportion of the OSHC session spent in moderate‐to‐vigorous physical activity in a meta‐analysis. Both trials showed an increase in proportion of session spent in moderate‐to‐vigorous physical activity (moderate‐certainty evidence) from 4% to 7.3% of session time; however, only one trial was statistically significant. There was low‐certainty evidence that physical activity interventions may lead to little to no reduction in body mass index (BMI) as a measure of cardiovascular health, compared to no intervention (SMD –0.17, 95% CI –0.44 to 0.10; P = 0.22; 4 trials, 1684 children). Physical activity interventions that were delivered online were more cost‐effective than in person. Combined results suggest that staff‐and‐parent and staff‐and‐child‐based interventions may lead to a small increase in overall daily physical activity and a small reduction or no difference in BMI. Process evaluation was assessed differently by four of the included studies, with two studies reporting improvements in physical activity practices, one reporting high programme satisfaction and one high programme fidelity. The certainty of the evidence for these outcomes was low to moderate. Finally, there was very low‐certainty evidence that physical activity interventions in outside‐school hours childcare settings may increase cardiovascular fitness.
No trials reported on quality of life or adverse outcomes. Trials reported funding from local government health grants or charitable funds; no trials reported industry funding.
Authors' conclusions
Although the review included nine trials, the evidence for how to increase children's physical activity in outside‐school hours care settings remains limited, both in terms of certainty of evidence and magnitude of the effect. Of the types of interventions identified, when assessed using GRADE there was low‐certainty evidence that multi‐component interventions, with a specific physical activity goal may have a small increase in daily moderate‐to‐vigorous physical activity and a slight reduction in BMI. There was very low‐certainty evidence that interventions increase cardiovascular fitness. By contrast there was moderate‐certainty evidence that interventions were effective for increasing proportion of time spent in moderate‐to‐vigorous physical activity, and online training is cost‐effective.
Plain language summary
Do physical activity interventions in outside‐school hours care services help increase children's overall daily physical activity?
Key messages
To date, physical activity programmes in outside‐school hours childcare services may marginally increase moderate‐to‐vigorous physical activity. However, the increase may be too small to have a meaningful impact on children's overall daily activity level.
Why is it important to increase children's physical activity in this setting?
Only 20% of children aged 5 to 17 years engage in enough physical activity to reduce the risk of non‐infectious diseases (such as heart disease and diabetes). The time outside‐school hours is a good opportunity for children to get more exercise to improve their health and well‐being. Given the millions of children who attend outside‐school hours childcare services across the world, using this setting may be a good way to increase these children's overall daily physical activity.
We wanted to know whether physical activity programmes made a difference to overall daily physical activity in children aged 4 to 12 years in outside‐school hours childcare settings.
What did we do?
We searched electronic databases and relevant journals to find studies. We included any randomised study (in which people have the same chance of being given the intervention or not) that looked at programmes to increase physical activity in outside‐school hours care settings. We compared and summarised the results of the studies and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did we find?
We included nine studies with 4458 children taking part. Five studies focussed on staff‐based programmes to change practice in the outside‐school hours childcare setting (for example, change in programming, activities offered, staff facilitation). Two studies used staff and parent strategies (for example, newsletters sent home with parent information, parent tool‐kits added to the staff strategies), one study used staff and child‐based programmes (for example, children had home activities to emphasise physical activity education added to the staff strategies) and one study used child‐only intervention strategies. Taken together, the results suggest that staff‐and‐parent‐ and staff‐and‐child‐based interventions may lead to a small or no increase in overall daily physical activity. They may also cause a small or no reduction in body mass index (a measure of body fat based on height and weight) and improve cardiovascular fitness. Only one study looked at whether the benefits and use of the programme were at least worth what was paid for them. This study found online training of staff for physical activity programmes is more affordable than in‐person training. None of the studies reported on unwanted effects or how the intervention affected children's well‐being.
What were the limitations of the evidence?
All studies included in this review were from high‐income countries (the USA and Norway), so we do not know if the results would be similar in low‐ and middle‐income countries. More research from a bigger range of countries and including other strategies not typically studied using random methods would broaden and strengthen the evidence available.
How up‐to‐date is this evidence?
The evidence is current to August 2020.
Summary of findings
Summary of findings 1. Summary of Findings Table ‐ Interventions in outside‐school hours childcare settings for promoting physical activity among schoolchildren aged to 4 to 12 years.
| Interventions in outside‐school hours childcare settings for promoting physical activity among schoolchildren aged to 4 to 12 years | ||||||
| Patient or population: health problem or population Setting: Outside‐school hours childcare services Intervention: Intervention Comparison: Control | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with Control | Risk with Intervention | |||||
| Total daily moderate‐to‐vigorous physical activity (MVPA) assessed with: accelerometry, wrist‐worn activity monitors and self‐report data follow up: range 6 weeks to 2 years | The mean total daily moderate‐to‐vigorous physical activity (MVPA) was 21.8 minutes a | MD 1.7 minutes more (0.42 fewer to 3.82 more) | ‐ | 3036 (6 RCTs) | ⊕⊕⊝⊝ LOW b,c | Physical activity interventions in outside‐school hours settings may result in little to no difference in total daily MVPA |
| Proportion of care session spent in MVPA (% session spent in MVPA) follow up: range 1 years to 2 years | Findings from both randomised controlled trials (RCTs) reported improvements in proportion of session time spent in MVPA ranging from 4% to 7.3%; however, results were only sustained in 1 trial. One trial found an improvement in the intervention groups for accumulating 30 minutes of MVPA at 12 months with 972 boys and girls compared to the 1018 boys and girls in the control group (intervention: 7.3%, 95% CI 1.4% to 13.1%; OR 2.26, 95% CI 1.35 to 3.80; control: 6.8%, 95% CI 1.6% to 12.1%; OR 2.85, 1.43 to 5.68). By contrast, 1 trial found no difference from baseline for both the intervention and control groups at 2‐year follow‐up (134 (59%) children with intervention vs 112 (55%) children with control; P = 0.46). | 2236 (2 RCTs) | ⊕⊕⊕⊝ MODERATE b | Physical activity interventions in outside‐school hours may result in a small increase in time spent in MVPA or accumulating 30 minutes of MVPA in outside‐school hours care settings based on moderate‐certainty evidence | ||
| Cardiovascular fitness (3‐minute endurance test) follow up: 9 months | The mean cardiovascular fitness (3‐minute endurance test) was 14.19 m | mean 45.38 m more (0 to 0 ) | ‐ | 141 (1 RCT) | ⊕⊝⊝⊝ VERY LOW c,d | Physical activity interventions in outside‐school hours childcare settings may have resulted in improved cardiovascular fitness based on very low‐certainty evidence. |
| Cost‐effectiveness assessed with: USD follow up: 9 months | Limited evidence (1 study) that online training (USD 6383) was more cost‐effective option than in‐person training (USD 24,402) for providing overall training to outside‐school hours care services when implementing a new programme. | (1 RCT) | ⊕⊕⊕⊝ MODERATE e | Physical activity interventions that provided staff training were more cost‐effective online than in‐person. | ||
| Adverse outcomes ‐ not reported | No studies reported adverse outcomes | ‐ | ‐ | No information on adverse outcomes from interventions to increase physical activity in outside‐school hours childcare settings. | ||
| Quality of life ‐ not reported | No studies reported quality of life | ‐ | ‐ | No information on quality of life from interventions to increase physical activity in outside‐school hours childcare settings. | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; MD: Mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
| See interactive version of this table: https://gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_416926985098468622. | ||||||
a. Control group score based on Beets 2015 at low risk of bias and high precision with largest sample size. Data from boys and girls were combined using formula in Cochrane Handbook for Systematic Review of Interventions Section 6.5.2.10. b. Downgraded one level due to inconsistency of results – substantial heterogeneity (I2 = 66%). c. Downgraded one level due to wide confidence intervals. d. Downgraded two levels as study at high risk of bias across domains relating to missing outcome data and measurement of the outcome. e. Downgraded one level due to some concerns of risk of bias relating to deviations from intended intervention.
Background
Description of the condition
Non‐communicable diseases (NCDs), such as stroke, heart disease, type 2 diabetes, cancer and chronic lung disease, are responsible for approximately 70% of deaths worldwide (Ding 2016). The rise in the prevalence of NCDs is primarily due to four major risk factors: tobacco use, harmful use of alcohol, poor diet and physical inactivity (WHO 2018a). Lack of physical activity has been identified as a universal issue that requires global intervention (Ding 2016). Literature has demonstrated the effect of physical inactivity on morbidity and premature mortality (Ding 2016). The resultant economic burden on healthcare systems has been estimated internationally at approximately USD 53,800 million, with countries with a higher human development index impacted more with economic costs, whilst countries of middle‐to‐low human development have greater disease burden (Ding 2016).
Physical activity provides an array of health benefits across the lifespan. In adulthood, physical activity has been linked to improved cardiovascular health and reduced rates of overweight and obesity, cancer and other NCDs (Reiner 2013). Moderate‐to‐vigorous physical activity (MVPA) is activity that induces energy expenditure greater than 3 METs (metabolic equivalents), such as brisk walking, running, dancing and competitive sports (WHO 2018b). In children, MVPA is associated with many health‐related benefits, including improved aerobic fitness, cognitive abilities and self‐confidence, together with reduced cardiovascular risk and depression rates (Sterdt 2014). Evidence suggests that people who participate in regular physical activity in childhood are more likely to be physically active as adults (Jones 2013; Tammelin 2014). Despite these benefits, numerous studies have found that children's physical activity levels have been declining in recent decades (Bassett 2015; Dalene 2018; Dollman 2005), with outdoor play (Bassett 2015), active transport (Bassett 2015; Booth 2015; Dollman 2005), and physical education implicated in particular (Bassett 2015; Dollman 2005). Given the wide‐ranging impacts of physical activity for children's health and well‐being, international guidelines have been developed.
The World Health Organization's (WHO) physical activity and sedentary behaviour guidelines for children aged 5 to 17 years recommend that children attain at least 60 minutes of MVPA and no more than two hours of recreational screen time daily (e.g. activities for recreation/enjoyment such as computer or tablet use, television viewing and inactive video gaming, not screen activities related to homework/learning) (WHO 2020). However, recent evidence suggests that most children fail to meet these guidelines. For example, pooled data from the International Children's Accelerometry Database (ICAD), an international consortium of accelerometry data, combined results from Europe, Australia, North America and South America. Longitudinal results from 1997 to 2009 found that only 9% of boys and 2% of girls aged 5 to 17 years achieved the recommended 60 minutes of MVPA every day (Cooper 2015). Likewise, the Active Healthy Kids Global Alliance (Aubert 2018), which involves children from 49 countries of varying human development index, found that only 20% of children aged 5 to 17 years achieved the recommended amount of physical activity based on the WHO guidelines (Aubert 2018). This result is estimated to be lower for children from low socioeconomic status (SES), with research demonstrating the lower the SES, the higher the levels of sedentary behaviour and lower levels of MVPA (Drenowatz 2010).
To date, many children's physical activity interventions have been delivered in the school setting, with efforts aimed at improving the school curriculum to include physical activity as part of traditional learning, specific physical education lessons, and changes to the school environment or school policies, or both (Atkin 2011). However, delivery in the school setting has limitations. For example, it appears that behaviour changes achieved at school are not carried through to the outside‐school hours period (Atkin 2011). In addition, overcrowding of the school curriculum has resulted in declining willingness for schools to take on physical activity interventions (Beets 2009). In contrast, the outside‐school hours period (before and after school) presents a relatively underexplored, and potentially more flexible, time in which to intervene on children's physical activity.
The outside‐school hours period refers to the hours of the day before and after the structured school day, typically between 7.00 a.m. and 8.30 a.m. and 3.00 p.m. and 6.00 p.m., although this varies across countries. During these hours, children may be home or have the opportunity to participate in organised activities such as sports, scouts, dancing and art lessons, or children may attend formalised childcare (e.g. outside‐school hours care (OSHC) in Australia or after‐school programmes (ASP) in the USA). There is a global shift in adults' work practices that has affected where and what school‐aged children do during the outside‐school hours period. Figures from the Organisation for Economic Co‐operation and Development (OECD), which combined economic and social well‐being data from 36 countries across five continents, showed that, on average, in 2016, 56% of children lived in households where all adults were in work (combination of full‐time and part‐time); 34% had one adult in work; and just under 10% resided in a household where no adult worked. This is in stark contrast to historic data from the OECD in 1999, in which only 30% of all adults worked. Hence, the increased need for formalised outside‐school hours childcare has become a global phenomenon (OECD 2016).
The OECD data from 2016 suggest that approximately 28% of all 6‐ to 11‐year‐old children attending school attend outside‐school hours childcare. The rate is higher in Nordic countries such as Denmark and Sweden, with outside‐school hours childcare use at 60%, which coincides with both parents working in 70% of households. In contrast, the use of outside‐school hours childcare is estimated to be as low as 6% to 8% in some Southern European countries (Italy and Spain) (OECD 2018). In the USA in 2014, it was estimated that 10.2 million, or 18%, of school‐aged children attended an after‐school childcare programme (Afterschool Alliance 2014). This steadily rose from 11% in 2004 to 15% in 2009. There were similar trends in Australia, with approximately 10% of children between the ages of 4 and 12 years attending after‐school childcare services in 2017, compared to 8% in 2011 (ABS 2017). The increased use of such services suggests that outside‐school hours childcare is an increasingly important setting in which to deliver physical activity programmes to address inactivity.
There have been no attempts to date to synthesise evidence regarding physical activity interventions delivered in the outside‐school hours childcare setting. However, there have been two related systematic reviews that examined the efficacy of after‐school physical activity programmes. A 2011 review by Atkin and colleagues included nine studies, of which three positively impacted physical activity and six found no change (Atkin 2011). Results suggested that programmes specifically targeting physical activity (as opposed to targeting physical activity with other health behaviours such as diet) may be more effective (Atkin 2011). Mears and Jago's 2016 review found 15 studies, of which six were included in a meta‐analysis (Mears 2016). Again, the evidence for programme efficacy was mixed, with a small pooled intervention effect of just five minutes per day increased MVPA (Mears 2016). However, these reviews only incorporate data up to early 2015, and examined programmes delivered in the after‐school period generally, rather than in the after‐school childcare setting specifically. A contemporary and more focused review of the evidence is therefore warranted.
Description of the intervention
For the purpose of this review, the intervention of interest was any programme delivered in the outside‐school hours childcare setting (i.e. consistent childcare programmes provided in the hours before or after school or during the school holiday period, or a combination of these) that aims to increase physical activity. We anticipated a variety of intervention approaches, including programmes focused solely on physical activity as well as those intervening on physical activity in conjunction with other behaviours (e.g. diet). In addition, programmes may have included staff training in facilitation of active play; timetabling changes; provision of equipment for active play; provision of activities for active play; teaching physical literacy; or changes in policies at a district, state or national level.
How the intervention might work
The physical activity intervention may work through a variety of pathways, such as increasing opportunity for children to engage in physical activity (e.g. through timetabling changes with increased time allocated to outdoor play, or through provision of equipment that facilitates active play); increasing the intensity of activity during existing active playtime (e.g. by staff training that assists staff to run games that encourage children to be more vigorously active or improve children's physical literacy, or both, i.e. the knowledge, motivation and skills to be active); or by removing competing activities that discourage children from being active (e.g. removing or limiting access to recreational screen devices and other sedentary pursuits). Policies may be implemented, as in North America where the YMCA adopted the Healthy Eating and Physical Activity Standards (HEPA), which states that children must achieve at least 30 minutes of MVPA daily in the ASP, as a way to help children achieve at least half of their recommended daily MVPA requirements (Beets 2018). This is similar in other countries where guidelines for physical activity in the after‐school childcare setting exist and are implemented as part of standard care (e.g. the Ontario Ministry for Education – Canada) (Ontario Ministry of Education 2017).
Why it is important to do this review
Given the significant health and economic impacts of physical inactivity globally, interventions are needed to address and improve this issue. More than one in four children internationally attend outside‐school hours childcare programmes, and rates are rising, suggesting that this presents an increasingly important setting for children's physical activity interventions. There have been no systematic reviews on physical activity interventions in the only outside‐school hours childcare settings to date. Much of the existing evidence comes from short‐term ASPs (e.g. summer camps) set up by researchers to deliver targeted PA interventions for specific populations (e.g. African American girls or overweight children) (Baranowski 2003; Barbeau 2007; Weintraub 2008). The findings of such studies may not be generalised to outside‐school hours childcare settings, which service more diverse populations and operate on an ongoing basis in different contexts. However, there is increased policy and programme interest by governments and other agencies in this setting as an opportunity to promote child health. To guide such policy and practice decision, a systematic review synthesising the effects of interventions delivered in the outside‐school hours childcare setting is required.
Objectives
To assess the effectiveness, cost‐effectiveness and associated adverse events of interventions designed to increase physical activity in children aged 4 to 12 years in outside‐school hours childcare settings.
Methods
Criteria for considering studies for this review
Types of studies
Based on the criteria from the Cochrane Effective Practice and Organisation of Care Group (EPOC), we included randomised controlled trials (RCTs) (including cluster‐RCTs) in the review. We excluded study designs using non‐random assignment to groups and crossover trials using random assignment due to carry‐over effect. There were no exclusions based on sample size, length of follow‐up, language or country.
Types of participants
Participants were primary/elementary school‐aged children attending outside‐school hours childcare services, where the children were predominantly aged 4 to 12 years. For the purpose of this review, we defined 'outside‐school hours childcare services' as formal, structured, ongoing group childcare services that operated prior to or following (or both) the usual school operational hours on days when children attended school. These services may also have been offered during school holidays. These included childcare services provided either by schools or third‐party providers such as community organisations or for‐profit private providers. Programmes provided by sporting clubs (e.g. soccer training during the week for weekend games) or other specific activity groups (e.g. gymnastics/scouts/dance clubs) or temporary physical activity programmes offered outside of school (e.g. dance programmes set up for the after‐school period) were excluded.
Types of interventions
Any intervention aimed at increasing physical activity levels in the outside‐school hours childcare setting was eligible for inclusion. Examples included changes to activity schedules to increase opportunity for physical activity; environmental interventions (e.g. increasing the availability of activity play equipment, or access to areas conducive to physical activity; facilitated activities aimed at increasing physical activity (e.g. games or sports led by a facilitator); or regulatory interventions (e.g. implementation of policy related to physical activity at a district, state or national level). We included interventions that focussed solely on increasing physical activity, as well as those that aimed to increase physical activity in addition to affecting other health behaviours (e.g. improved diet) or health conditions (e.g. obesity).
To be eligible, the intervention must have been delivered in the context of an existing outside‐school hours childcare setting (i.e. childcare that was available consistently throughout the school week/year). The childcare service may have been operated by schools, community groups or non‐government organisations (e.g. YMCA), or third‐party providers (e.g. private childcare companies) in a school, community setting or childcare‐specific facility. We included interventions that involved strategies targeting physical activity in other contexts, such as the home or school, only if two review authors (RV and CM/LL/AP) judged the majority of the intervention (>75%) to have occurred in the outside‐school hours childcare setting. Programmes based in clinical settings (e.g. hospital‐based exercise programme after school for weight loss) were not eligible for inclusion. Interventions that were delivered across multiple settings (e.g. school, sport or recreation facility) as well as outside‐school hours childcare settings were excluded.
Comparators were usual care (i.e. outside‐school hours childcare with no physical activity intervention); attention‐matched control groups (i.e. where the control group received a placebo to mimic time and attention given to intervention group participants); wait‐list control groups (i.e. where the control group received the intervention after the active intervention group) or alternative interventions (i.e. where a study compared two alternative forms of physical activity intervention).
Types of outcome measures
Primary outcomes
Total daily MVPA (minutes per day): assessed by direct observation (using a standardised, validated direct‐observation tool), accelerometry, self‐report (i.e. from children or childcare staff or both, reported using a validated questionnaire), heart rate monitor or wrist‐worn activity monitor (including pedometers and consumer‐level devices where results were extrapolated to minutes in MVPA). It was anticipated data would be expressed in terms of baseline and postintervention mean values (and standard deviations (SD)) or change scores.
Secondary outcomes
Proportion of the care session spent in MVPA (e.g. through direct observation, self‐report or accelerometry).
-
Cardiovascular health:
body mass index (BMI) (as BMI, BMI z‐score, BMI percentile including both self‐report and objectively measured height and weight for BMI calculation);
cardiovascular fitness (e.g. 20‐metre shuttle run test);
blood pressure.
-
Evaluation outcomes:
process evaluation (i.e. was the intervention implemented as intended and assessed);
cost evaluation (e.g. cost‐effectiveness between interventions, cost of programme elements);
feasibility (which may be referred to as acceptability or feasibility, e.g. Likert rating of ease of delivery of intervention).
-
Adverse outcomes:
any measures of adverse effects identified by studies including musculoskeletal injuries, or any psychological distress as a result of interventions.
Quality of life measures (based on results from validated measurement tools, e.g. Paediatric Quality of Life Inventory (PedsQoL) and KINDL).
Search methods for identification of studies
Electronic searches
We searched the following databases on the 18 August 2020 (initial search September 2019):
the Cochrane Library (including the Cochrane Central Register of Controlled Trials (CENTRAL) (inception to 10 August 2020);
MEDLINE Ovid (1946 to 10 August 2020);
Embase Ovid (1974 – 10 August 2020);
ERIC via ProQuest platform (Education Resources Information Center) (1966 to 10 August 2020);
SportDISCUS via EBSCO platform (inception to 10 August 2020).
The search strategy for MEDLINE (Appendix 1), was translated for the other databases (Appendix 2; Appendix 3; Appendix 4; Appendix 5; Appendix 6). There were no language or date limits applied.
Searching other resources
We searched three trial registries in August 2020: ClinicalTrials.gov (clinicaltrials.gov), EU Clinical Trials Register (www.clinicaltrialsregister.eu), and Australian New Zealand Clinical Trials Registry (www.anzctr.org.au).
We searched for grey literature in Trove, ProQuest Dissertations and Theses Global databases (Appendix 7; Appendix 8) We conducted handsearches of the reference lists of included articles and citation tracking (forward citing) to identify relevant articles. We handsearched all publications in 2018 to 2020 for two relevant journals (International Journal of Behavioural Nutrition and Physical Activity and American Journal of Preventive Medicine), since these were the key journals in which included articles were most frequently published. Finally, we contacted first and senior authors on articles identified for inclusion for ongoing or unpublished research, using the author contact details provided in the publications.
Data collection and analysis
Selection of studies
All references identified through the search strategy were downloaded into Endnote Version X8 (EndNote), which removed duplicate references, with results then imported into Covidence systematic review software for screening (Covidence 2018). Two review authors (RV and KB/LL/AP) independently screened the references for potential inclusion based on title and abstract. Review authors were not blinded to study author or journal. A third review author was planned to be used to mediate any disagreements until consensus was reached, however, this was not required. We contacted the study authors directly for any papers with insufficient detail to determine eligibility. We obtained the full texts of studies deemed potentially eligible for inclusion, and two review authors (RV and AP) independently assessed them for eligibility against the inclusion criteria. Those studies deemed as ineligible were recorded with reasons for ineligibility in the Characteristics of excluded studies table. We created a flow chart following the PRISMA protocol to illustrate this process (Moher 2009).
Data extraction and management
Two review authors (RV and CM/TF/AP) independently extracted data onto a piloted data extraction form developed for this review with discrepancies resolved via consensus discussion (see Appendix 8). If the information required for data extraction was not available from the published report or was unclear, we attempted to contact authors directly, recording date and method of contact. We contacted four authors between April and May 2020 via email, and received all missing data from them via email (Annesi 2017; Beets 2015; Branscum 2013; Brown 2018).
We extracted the following data.
-
Background and general information:
date of extraction, review author ID, title, published or unpublished, authors, year of publication, country, contact address, study country, language of publication, source of study, funding, conflicts of interest.
-
Basic study details:
sample size, participant characteristics, attrition rates.
-
Population and setting:
description of population and setting, characteristics of participants (age, gender, location, SES, etc.), recruitment strategy.
-
Methods:
aim of intervention, allocation method, number of study arms, description of study arms, sample size per study arm, start date, end date, duration of participation.
-
Participants:
total number randomised; presence of baseline imbalances; if there was an imbalance, description of such; number of withdrawals/exclusions; sex of children; mean age; race/ethnicity; SES.
-
Intervention group:
number randomised, number measured at baseline, number measured at follow‐up, intervention details, duration of intervention, delivery/providers of intervention.
-
Comparison group:
number randomised, number measured at baseline, number measured at follow‐up, comparison/usual care details, delivery/providers of comparison.
-
Outcomes:
for each outcome: measurement tool, psychometric properties of tool, assessor (i.e. person who performed assessments), whether missing data were imputed, units, measure of intervention effect or mean effect of intervention for each study arm.
-
Other relevant information:
cost of intervention (if available), reported limitations, process evaluation, other as appropriate.
Assessment of risk of bias in included studies
Two review authors (RV and AP/TF) assessed risk of bias at the outcome level for each of the included studies using the Cochrane RoB 2 tool (Sterne 2019), as described in the Cochrane Handbook for Systematic Review of Interventions (Higgins 2020).
For the selected primary and secondary outcomes within an included randomised study, we assessed the following risk of bias domains: randomisation process, deviation from intended interventions (effect of assignment to intervention), missing outcome data, measurement of the outcome and bias in selection of the result. For the selected outcomes within included cluster‐RCTs, in addition to the RoB 2 tool, we used the RoB 2 tool specific for cluster‐RCTs as per the Cochrane Handbook for Systematic Review of Interventions (Sterne 2019): randomisation process, timing to randomisation, deviations from intended interventions (effect of assignment to intervention), missing outcome data, measurement bias, reporting bias, overall risk of bias and bias arising from identification or recruitment of individual participants within clusters (Higgins 2020).
We assigned a 'high' risk of bias to an outcome when the trial was at a high risk of bias in at least one of the following domains: randomisation process, deviation from intended interventions, missing outcome data, measurement of the outcome and bias in selection of the result. It was also assigned a high risk of bias for an outcome if it was judged to have some concerns for multiple domains in a way that substantially lowered confidence in the result (Sterne 2019).
We assigned a judgement of 'some concerns' to the study if the outcome was judged to have some concerns in at least one domain and no 'high' risk of bias in any domains (randomisation process, deviation from the intended interventions, missing outcome data, measurement of the outcome and bias in the selection of the result) (Sterne 2019). We assigned a 'low' risk of bias to the study when the outcome was at low risk of bias on all criteria (Sterne 2019). Two review authors (RV and TF/AP) independently made all judgements, and resolved any discrepancies by consensus discussion.
Measures of treatment effect
We used RevMan Web to manage data and perform meta‐analyses (RevMan Web). We expressed treatment effects as mean differences (MD) with 95% confidence intervals (CIs). All outcome data suitable for meta‐analysis were either postintervention or change‐from‐baseline measures or overall intervention effect estimates adjusted for clustering (for cluster‐RCTs). We identified one trial that reported results by subgroups for the primary outcome (minutes per day MVPA) for both study arms (intervention and control) (Beets 2015). Beets 2015 reported results according to gender (boys; girls). For this trial, we combined subgroup data for each study arm separately using the formulae outlined in the Cochrane Handbook for Systematic Review of Interventions before entering them into RevMan Web (Section 6.5.2.10; Higgins 2020b).
For continuous measures of physical activity (primary outcome), we reported the MD with 95% CIs in random‐effects models using the generic inverse variance method for each outcome. For the physical activity meta‐analysis, we combined studies that report postintervention data only (Branscum 2013; Dzewaltowski 2010a) with those reporting 'change‐from‐baseline' data (Beets 2015; Brown 2018; Cradock 2016; Riiser 2020) using the MD method before being entered into RevMan Web (Section 6.5.2.1; Higgins 2020b).
For continuous measures of cardiovascular health such as BMI (secondary outcome), when studies used different scales to measure the same outcome, we used standardised mean differences (SMDs) with 95% CIs. We identified one trial that reported results for multiple intervention arms for the secondary outcome (BMI) (Economos 2020). For this trial, we combined multiple intervention arm data using the formulae outlined in the Cochrane Handbook for Systematic Review of Interventions (Section 6.5.2.10; Higgins 2020b).
Where relevant, we calculated conversions between standard error (SE), SD and 95% CIs before entering data into RevMan Web to enable pooled synthesis (Cochrane Handbook for Systematic Review of Interventions; Sections 6.3.1 and 6.5.2.2; Higgins 2020).
We synthesised outcomes that could not be meta‐analysed narratively (secondary outcomes including proportion of care session spent in MVPA, cardiovascular health measures, evaluation outcomes) following the Synthesis Without Meta‐analysis (SWiM) protocol (Campbell 2020)
Cluster‐randomised controlled trials
We examined all cluster‐RCTs for unit of analysis errors. We followed the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions for inclusion of cluster‐RCTs (Higgins 2020). We identified three of the five included trials that provided a direct estimate of the intervention effect accounting for clustering; we used this in the meta‐analysis for the primary outcome (duration of MVPA) (Beets 2015; Cradock 2016; Riiser 2020). Where cluster‐RCTs reported results unadjusted for clustering (Annesi 2017; Branscum 2013), we calculated inflated SE for the outcome means to enable individual‐level pooling with the other studies reporting the same outcome in random‐effects models using the generic inverse variance method (Cochrane Handbook for Systematic Reviews of Interventions; Section 23.1.5) (Higgins 2020). Both Beets 2015 and Cradock 2016 were cluster‐RCTs and correctly reported the results of analyses that were appropriately adjusted for clustering (SEs inflated by the intracluster correlation coefficient (ICC)); therefore, corrections to their SEs were not required. The ICC reported in Cradock 2016 (ICC = 0.13) was used to calculate inflated SEs where relevant. Cradock 2016 was chosen as it was the only study that both accounted for clustering and reported an ICC for the outcome of interest (total daily MVPA). These trials were combined with results from individual RCTs (Branscum 2013; Brown 2018) and cluster‐RCTs (Dzewaltowski 2010a) reporting means for each study arm separately. We pooled data in a random‐effects model using the generic inverse variance method (Cochrane Handbook for Systematic Reviews of Interventions; Section 23.1.5; Higgins 2020).
Repeated measures
In studies where repeated measures were taken postintervention, we used the longest follow‐up period for analysis.
Multiple intervention groups
One study had multiple intervention groups for the secondary outcome BMI (Economos 2020). To create a single pairwise comparison, we combined the continuous data as outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Section 6.5.2.10; Higgins 2020b).
Dealing with missing data
In the case of missing data, we first contacted the study's corresponding author to request the missing data where possible (e.g. when a study was identified as abstract only), as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2020). We did not impute any other missing values. We successfully obtained all data from study authors or calculated them from available published information.
Assessment of heterogeneity
We assessed heterogeneity via visual inspection of forest plots, the Chi2 test, and the I2 statistic (Higgins 2020). We used the I2 statistic to quantify heterogeneity among the trials in each analysis. If we found 'considerable' heterogeneity according to predefined thresholds, we reported it and explored possible causes with prespecified subgroup analyses.
In doing this, we followed the threshold recommendations outlined in Section 9.5.2 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2020):
0% to 40%: might not be important;
30% to 60%: moderate heterogeneity;
50% to 90%: substantial heterogeneity;
75% to 100%: considerable heterogeneity.
Assessment of reporting biases
There was an insufficient number of studies to include the use of funnel plots as a visual representation of reporting biases (fewer than 10) as per the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions (Section 13.3.5.4; Higgins 2020).
Data synthesis
We conducted analyses using Review Manager Web (RevMan Web), employing generic inverse variance, random‐effects models. Random‐effects models were used based on the assumption that the true effect might vary between studies given differences in interventions employed across studies.
We used estimates of intervention effect and SE to calculate the effect size. Where possible (i.e. the outcome data collected were sufficiently complete and in the same format), we conducted meta‐analyses. There were sufficient and appropriate data available to conduct meta‐analyses for measures of:
-
primary outcome:
total daily MVPA (minutes);
-
secondary outcomes:
-
cardiovascular health:
BMI/BMI z‐score.
-
Secondary outcomes including proportion of care session spent in MVPA cardiovascular health outcomes (BMI percentile, cardiovascular fitness) and process evaluation outcomes, were unable to be meta‐analysed due to different effect methods (proportion care session spent in MVPA, process evaluation, BMI percentile) and limited evidence (cardiovascular fitness). There were no data available to for quality of life or adverse effects. We performed a narrative synthesis according to the review objectives using the SWiM method (Campbell 2020). We synthesised findings by outcome, and within the study, synthesised effects by comparison. We included an 'Overview of synthesis and included studies', where we reported the comparison, the primary implementation outcome measures and the effect sizes for these measures (or median effect size and range of effects where multiple measures of the same outcome were reported) for each study and the overall risk of bias.
We considered the clinical significance of results for the primary outcome (physical activity) in the context of whole‐day physical activity, that is, whether the effects of any increase in MVPA were of sufficient magnitude to substantially contribute to achievement of WHO‐recommended daily MVPA of 60 minutes for children aged 5 to 17 years.
Subgroup analysis and investigation of heterogeneity
There were no subgroup analyses to explore heterogeneity of the primary outcome (duration of MVPA) based on population, age or outcome. We examined intervention length in an exploratory analysis.
Sensitivity analysis
We performed a sensitivity analysis by removing those studies assessed as high risk of bias. For the duration of MVPA (primary outcome), one study was at high risk of bias (Branscum 2013). Likewise, BMI (secondary outcome) meta‐analysis had two of the four included studies in the meta‐analysis that were at high risk of bias (Annesi 2017; Economos 2020). The method of analysis replicated the main physical activity meta‐analysis (random‐effects model using the generic inverse‐variance method).
Summary of findings and assessment of the certainty of the evidence
Two review authors (RV and LW) used the GRADE approach to assess the certainty of the evidence for the outcomes addressed in the included studies (Guyatt 2013). The GRADE approach uses select criteria to determine the certainty of the evidence by assessing the methodological quality at an outcome level, heterogeneity, directness of evidence, precision of evidence and risk of publication bias (Guyatt 2013). The outcomes were graded as follows.
High certainty: further research is very unlikely to change our confidence in the effect estimate.
Moderate certainty: further research is likely to have an important impact on our confidence in the effect estimate and may change the estimate.
Low certainty: further research is very likely to have an important impact on our confidence in the effect estimate and may change the estimate.
Very low certainty: we are very uncertain about the effect estimate.
We exported data from RevMan Web into GRADEpro GDT software (GRADEpro GDT 2015) to produce a summary of findings table, which was then directly imported into RevMan Web. Summary of findings tables allowed for details for each outcome assessed to be collated, such as the assessment tools used, follow‐up range, timing of follow‐up, study design, number of studies, total sample sizes, effect estimates and certainty of the evidence. We generated the table based on the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions and included 1. a list of all primary and secondary outcomes in the review, 2. a description of intervention effect, 3. the number of participants and studies addressing each outcome and 4. a grade for the overall certainty of the body of evidence for each outcome. We resolved any disagreements through discussion with a third review author (CM/LL/AP). We prioritised the following primary and secondary outcomes in the following order from 'critical' to 'important' for the summary of findings table.
Total daily MVPA (primary outcome).
Proportion of care session spent in MVPA (secondary outcome).
Cardiovascular health: BMI (secondary outcome).
Cardiovascular health: cardiovascular fitness (secondary outcome).
Evaluation outcomes: cost‐effectiveness (secondary outcome).
Adverse outcomes (secondary outcome).
Quality of life (secondary outcome).
This order of priority was based on importance to the review question and ratings of importance (not important through to critically important) by the authorship group. Process evaluation outcomes (including feasibility) were not included in the summary of findings table as they were descriptive measures rather than measures of effect of trial outcome and therefore not appropriate to include. While all the outcomes reported in the review were considered of potential interest to end‐users (other cardiovascular health outcomes such BMI percentile, cardiovascular fitness and blood pressure) were also not included in the summary of findings table as BMI and BMI z‐score were considered priority outcomes for inclusion in the summary of findings table.
We used the five GRADE considerations (risk of bias, inconsistency, indirectness, imprecision and publication bias) to assess the certainty of the body of evidence as it related to the trials that contributed data to the meta‐analyses for the prespecified outcomes. We used methods and recommendations described in Section 14.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2020), using GRADEpro GDT software (GRADEpro GDT 2015). We justified all decisions to downgrade the certainty of trials using footnotes, and made comments to aid readers' understanding of the review where necessary.
Results
Description of studies
See Characteristics of included studies and Characteristics of excluded studies tables.
Results of the search
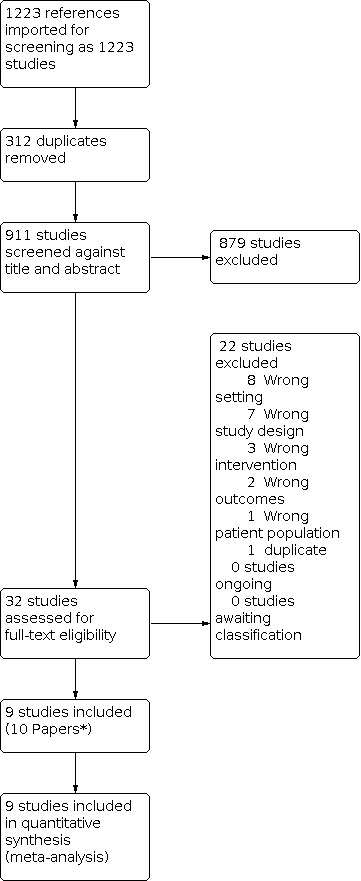
The electronic search yielded 1223 results, from which 312 duplicates were removed. We found no additional records from trial, handsearching key journals, reviewing the reference lists of included studies or contacting experts in the field of children's physical activity in the outside‐school hours childcare setting. Four study authors (RV, LL, KB and AP) conducted screening of titles and abstracts. A total of 32 studies underwent full‐text review, by three authors (RV, AP and CM), from which nine studies (10 papers) were included in the review (see Figure 1).
1.
*Weaver 2015 paper reported on the process evaluation of the study conducted by Beets 2015 i.e. Beets and Weaver was the same study, reporting different outcomes, of which both outcomes were relevant to this systematic review
Included studies
This review included nine trials (reported in 10 papers) with a total of 3458 children. One trial was reported in two papers. The first paper reported physical activity (Beets 2015), and the second paper reported the process evaluation outcome (Weaver 2015) of the same trial. See Overview of synthesis and included studies (OSIS) for summary information (Table 2).
1. Overview of synthesis and included studies.
|
Study, country of conduct |
Study design | Overall risk of bias (outcome level) | Population (sample size) | Intervention characteristics (target audience, theoretical basis) | Outcome domains | Specific outcome measures | Time point of measurement | Method of synthesis | Result |
| Outcome: total daily MVPA | |||||||||
|
Beets 2015 US |
Cluster‐RCT | Low | Children aged 6–12 years (972 intervention; 1018 control) | Outside‐school hours childcare service staff; systems change theory | Physical activity intensity | Accelerometry ActiGraphy GT3X+ | Baseline, 12 months | MA |
Change scores baseline to 12 months: Intervention boys: +4 min/day MVPA Control boys: +0.6 min/day MVPA; between‐group difference P = 0.982 Intervention girls: +1.7 min/day MVPA Control girls: 0 change between‐group difference P = 0.989 |
|
Branscum 2013 US |
RCT | High | Children aged 8–11 years (31 intervention; 34 control) | Children attending outside‐school hours childcare service; social cognitive theory and knowledge‐based theory | Physical activity intensity | School physical activity and nutrition questionnaire | Pre‐ and post‐test (6 weeks), 3 months | MA |
Change scores baseline to longest follow‐up (3 months): Intervention mean: +36.48 (SD 0.99) min/MVPA Control mean: +35.29 (SD 20.26) min/MVPA P = 0.004 |
|
Brown 2018 US |
RCT | Some concerns | Children aged 6–9 years (11 intervention; 11 control) | Staff, children and families attending outside‐school hours childcare service; ecological model of physical activity |
Physical activity intensity | Wrist‐worn activity monitors | Pre‐ and post‐ test (11 weeks) | MA |
Change scores baseline to 11 weeks: Intervention mean: 115.2 (SD 34.9), 95% CI 90.2 to 140.2 min MVPA/week Control mean: 96.7 (SD 58.4), 95% CI 54.9 to 138.5 min MVPA/week P = 0.401 |
|
Cradock 2016 US |
Cluster‐RCT | Some concerns | Children aged 5–12 years (mean 7.8 years) (182 intervention; 220 control) |
Outside‐school hours childcare staff; socio‐ecological model and participatory research approach | Physical activity intensity | Accelerometry ActiGraph GT3X+ | Baseline, 6 months | MA |
Change score baseline to 6 months: Intervention: 8.7 min/day, ICC 0.13 Control: 9.2 min/day Adjusted change: –1.0, 95% CI –3.3 to 1.3 P = 0.40 |
|
Dzewaltowski 2010a US |
Cluster‐RCT | Low | 4th grade students (134 intervention; 112 control) | Outside‐school hours childcare service staff and children attending service; social cognitive theory | Physical activity intensity | Accelerometry – ActiGraph GT1M | Baseline, 12 months, 24 months | MA |
Change score baseline to longest follow‐up (24 months): Intervention mean: 15.9 (SD 9.6) min/day MVPA Control mean: 15.1 (SD 6.3) min/day MVPA P = 0.80 |
|
Riiser 2020 Norway |
Cluster‐RCT | Some concerns | First‐graders (aged 5–6 years) (229 intervention; 227 control) | School physiotherapists and outside‐school hours childcare service staff; self‐determination theory | Physical activity intensity | Accelerometry – ActiGraph GT3X | Baseline, post‐test (7 months), 1 year postintervention (19 months postbaseline) | MA |
Change scores baseline to 1 year follow‐up (19 months from baseline): non‐significant positive change in MVPA min/hour intervention vs control mean 0.55, 99% CI –0.55 to 1.64 MVPA min/hour |
| Outcome: proportion of the care session spent in MVPA | |||||||||
|
Beets 2015 US |
Cluster‐RCT | Low | Children aged 6–12 years (972 intervention; 1018 control) | Outside‐school hours childcare service staff; systems change theory | % of children meeting 30‐minute MVPA goal | Accelerometry ActiGraph GT3X+ | Baseline, 12 months | NS |
Intervention vs control group Boys: 7.3% increase, 95% CI 1.4 to 13.1; OR 2.26, 95% CI 1.35 to 3.80 Girls: 6.8% increase, 95% CI 1.6 to 12.1%; OR 2.85, 95% CI 1.43 to 5.68 |
|
Dzewaltowski 2010a US |
Cluster‐RCT | Low | 4th grade students (134 intervention; 112 control) | Outside‐school hours childcare service staff and children attending service; social cognitive theory | % session spent in MVPA | Accelerometry ActiGraph GT1M | Baseline, 12 months | NS | Children in intervention group spent 4% more of session time in MVPA compared to control group but not significantly different (P = 0.46) |
| Outcome: cardiovascular health: BMI/BMI z‐score | |||||||||
|
Annesi 2017 US |
Cluster‐RCT | High | Children aged 9–12 years (86 intervention; 55 control) | Outside‐school hours childcare staff; social cognitive theory | BMI | Calibrated digital scale and stadiometer | 3 months; 9 months | MA |
Change from baseline to longest follow‐up (9 months) Intervention mean: 0.13 (SD 0.86), 86 children Control mean: 0.6 (SD 0.97), 55 children P < 0.010 |
|
Brown 2018 US |
RCT |
Some concerns | Children aged 6–9 years (11 intervention; 11 control) | Staff, children and families attending outside‐school hours childcare service; ecological model of physical activity |
BMI | Digital scales and portable stadiometer | Pre‐ and post‐test (11 weeks) | MA |
Change score baseline to longest follow‐up: Intervention mean: –0.34 (SD 0.83), 95% CI –0.89 to 0.22 Control mean: 0.67 (SD 2.35), 95% CI –0.91 to 2.25 P = 0.196 |
|
Dzewaltowski 2010a US |
Cluster‐RCT | Low | 4th grade students (134 intervention; 112 control | Outside‐school hours childcare service staff and children attending service; social cognitive theory | BMI and BMI z‐score | Portable stadiometer and digital scales and CDC growth curves to obtain z‐value |
Baseline, 12 months, 24 months | MA |
Change score: Intervention: MD 0.1 (SE 0.3) Control: MD 0.2 (SD 0.3) P = 0.17 |
|
Economos 2020 US |
Cluster‐RCT | High | Children aged 6–9 years (25 intervention 1; 33 intervention 2; 25 control) | Children and families attending outside‐school hours childcare services | BMI and BMI z‐score | Portable stadiometer and digital scales and CDC growth curves to obtain z‐value |
Baseline, 24 months | MA |
Change score: Intervention 1: MD 0.02 (SE 0.02) P = 0.13 Intervention 2: MD 0.05 (SE 0.03) P = 0.369 Control: MD 0.08 (SE 0.03) P < 0.01 |
| Outcome: cardiovascular health: BMI percentile | |||||||||
|
Beets 2015 US |
Cluster‐RCT | Low | Children aged 6–12 years (972 intervention; 1018 control) | Outside‐school hours childcare service staff; systems change theory | BMI‐for‐age percentile categories | % of children in age–sex‐BMI categories: < 85th percentile; 85–95th percentile; > 95th percentile | Baseline, 12 months | NS |
Intervention < 85th pre: 71.5%, post: 68.2%; 85–95%: pre: 20%, post: 21%; > 95th: pre: 8.5%, post 10.8% Control < 85th pre: 59%, post: 62.8%; 85–95th: pre: 22.1%, post: 21.3% > 95th: pre: 19%, post 15.9% P < 0.001 (baseline between‐group difference) |
|
Branscum 2013 US |
RCT | High | Children aged 8–11 years (31 intervention; 34 control) | Outside‐school hours childcare service; social cognitive theory and knowledge‐based theory | BMI‐for‐age percentile | Raw BMI converted to BMI percentile using CDC calculator (ED) | Pre‐test and 3 months | NS |
Intervention Pretest: mean 60.15 (SD 26.39) Follow‐up: mean 59.23 (SD 26.31) Control Pretest: mean 55.52 (SD 27.96) Follow‐up: mean 57.26 (SD 27.84) P = 0.567 between‐group differences |
| Outcome: cardiovascular health: fitness | |||||||||
|
Annesi 2017 US |
Cluster‐RCT | High | Children aged 9–12 years (86 intervention; 55 control) | Outside‐school hours childcare staff; social cognitive theory | Cardiovascular fitness | 3‐minute test (distance covered walking or running) (ED) | Baseline; 3 months; 9 months | NS |
Change from baseline to month 3 Intervention mean 22.12 (SD 85.58) m Control –4.48 (SD 54.56) m, F = 4.21 (0.03) P < 0.05 Change from baseline to month 9:Intervention mean 45.38 (SD 90.31) m Control mean 14.19 (SD 81.02) m F = 4.35 (0.03) P < 0.05 |
| Outcome: process evaluation | |||||||||
|
Brown 2018 US |
RCT | Some concerns | Children 6–9 years (11 intervention; 11 control) | Staff, children and families attending outside‐school hours childcare service; ecological model of physical activity |
Child participation in programme; parent satisfaction; family participation in programme | % children attending ≥ 25 sessions | 11 weeks | NS | 91% |
| Likert scale (1 = unhappy to 5 = very happy) | Mean Likert score 4 | ||||||||
| % uptake of programme components | 33% of children completed home activities, 58% of families participated in study information sessions, 80–100% participation in family nights | ||||||||
|
Branscum 2013 US |
RCT | High | Children aged 8–11 years (31 intervention; 34 control) | Children attending outside‐school hours childcare service; social cognitive theory and knowledge‐based theory | Fidelity; programme dose; programme reach; context | Planned intervention scored against actual implementation of 8 sessions | 3 months | NS | 91–100% of session run as planned |
| Time taken to implement lesson (goal 4 lessons of 30 minutes' duration |
Intervention services mean 31 (SD 1.47) min, control services mean 31 (SD 1.35) min; P > 0.477 | ||||||||
| Child attendance at each lesson |
70% of children attended 4 lessons, no difference between groups in number of lessons attended; P = 0.859 | ||||||||
| Field notes documenting presence of similar or competing programmes implemented during the course and during pretesting children asked about number of times taught about health eating and physical activity | ANOVA results no differences between groups for participation in either type of programme (healthy eating, P = 0.06; physical activity, P = 0.55), actual ANOVA report not provided in manuscript | ||||||||
|
Lee 2019 US |
RCT | Some concerns | Children aged 8–15 years (34 intervention; 19 control) | Staff working at outside‐school hours childcare service; Proctors conceptual model for implementation research | After‐school practice changes; reach; cost; adoption; fidelity | OSNAP‐OPAT score (purpose‐designed score) |
Baseline, 12 months | NS | Intervention sites participating in the in‐person training had a significantly larger increase in the aggregate after‐school practice score compared with control sites (mean + 0.44, 95% CI 0.02 to 0.86; P = 0.04); intervention sites participating in online training did not have significant change in practice score compared to control sites (mean 0.28, 95% CI –0.18 to 0.73; P = 0.24) |
| Number of staff attending training | Mean 23 people attending training in‐person compared to 11 with online training | ||||||||
| Cost | In‐person: USD 24,402; online: USD 6383 | ||||||||
| OSHC directors' self‐reported goals | Common goals were related to PA, and fruit and vegetable offerings | ||||||||
| Likert rating 1–5 (1 = needs improving, 5 = excellent/very clear) of how well learning objectives delivered as intended | Mean score 4.1 (range 3.6–4.4) | ||||||||
|
Weaver 2015 US |
Cluster‐RCT | Low | Children aged 6–12 years (972 intervention; 1018 control) | Outside‐school hours childcare service staff; systems change theory | Overall implementation score | STEPs score (purpose designed tool) Physical activity median index score (range) |
12 months | NS |
Intervention mean 21.5 (range 12.0–29.0) Control mean 9.5 (range 5.0–17.0) P < 0.001 |
BMI: body mass index; CDC: Center for Disease Control and Prevention; ED: effect direction; ICC: intracluster correlation coefficient; MA: meta‐analysis; MD: mean difference; min: minute; MVPA: moderate‐to‐vigorous physical activity; NS: narrative synthesis; NS: not significant; OSHC: outside‐school hours care; OPAT: Observational Practice Assessment Tool; OR: odds ratio; OSNAP: Out‐of‐School Nutrition and Physical Activity; PA: physical activity; RCT: randomised controlled trial; SD: standard deviation; SE: standard error; STEPs: Strategies to Enhance Practice.
Study design
Six were cluster‐RCTs (Annesi 2017; Beets 2015/Weaver 2015; Cradock 2016; Dzewaltowski 2010a; Economos 2020; Riiser 2020), and three were individually assigned RCTs (Branscum 2013; Brown 2018; Lee 2019).
Setting
Eight studies were conducted in the US (Annesi 2017; Beets 2015/Weaver 2015; Branscum 2013; Brown 2018; Cradock 2016; Dzewaltowski 2010a; Economos 2020; Lee 2019), with one study conducted in Norway (Riiser 2020). Studies were conducted between 1999 and 2017. All included studies were based in formal, structured, group outside‐school hours childcare services that operated prior to and following the school day during the school term. These were in a YMCA (Annesi 2017; Branscum 2013; Lee 2019); in existing outside‐school hours childcare providers in the school (Brown 2018; Dzewaltowski 2010a; Riiser 2020), or described as being across a variety of providers for the school district (Beets 2015/Weaver 2015; Cradock 2016; Economos 2020).
Seven studies provided clear information regarding the source of study funding (Beets 2015/Weaver 2015; Branscum 2013; Cradock 2016; Dzewaltowski 2010a; Economos 2020; Lee 2019; Riiser 2020), while the remaining two provided details about consumer involvement but did not explicitly state if funding was provided (Annesi 2017; Brown 2018). No industry funding was reported.
Participants
Children were the main participants in all the included trials, despite some interventions being targeted at staff (Annesi 2017; Beets 2015/Weaver 2015; Brown 2018; Branscum 2013; Cradock 2016; Dzewaltowski 2010a; Economos 2020; Lee 2019; Riiser 2020). Children's ages ranged from 6 to 15 years, with only data for children aged 12 years and younger included. Seven studies reported sex with a mean 51% boys (Annesi 2017; Beets 2015/Weaver 2015; Branscum 2013; Cradock 2016; Dzewaltowski 2010a; Economos 2020; Riiser 2020). Six studies reported race, with 48% of participants classified as white (Annesi 2017; Branscum 2013; Cradock 2016; Dzewaltowski 2010a; Economos 2020; Lee 2019). Brown 2018 only reported the percentage of American Indian children in the study. Five studies described the socioeconomic characteristics of the children attending the outside‐school hours childcare services (Annesi 2017; Beets 2015/Weaver 2015; Brown 2018; Dzewaltowski 2010a; Economos 2020). In four studies, the outside‐school hours childcare educators were targeted by the intervention, in addition to the children (Beets 2015/Weaver 2015; Brown 2018; Cradock 2016; Dzewaltowski 2010a). These interventions targeted staffs' ability to implement the physical activity programme and assess the impact on children's physical activity.
Interventions
Seven studies had the primary aim to increase physical activity in the outside‐school hours childcare setting (Beets 2015/Weaver 2015; Branscum 2013; Brown 2018; Cradock 2016; Dzewaltowski 2010a; Lee 2019; Riiser 2020), while Annesi 2017 had the primary aim to reduce BMI, and Economos 2020 aimed to improve bone strengthening in addition to increasing physical activity. All studies reported that their intervention strategies were theoretically based. The interventions were based on the following theories: the social cognitive theory (Annesi 2017; Branscum 2013; Dzewaltowski 2010a), systems change theory (Beets 2015/Weaver 2015), knowledge‐based theory (Branscum 2013), ecological model of physical activity (Brown 2018), socio‐ecological model (Cradock 2016), self‐determination theory (Riiser 2020), and ecological developmental systems approach (Dzewaltowski 2010a).
The duration of the interventions employed in the studies ranged from four weeks (Branscum 2013) to two years (Dzewaltowski 2010a). For seven studies, follow‐up was greater than six months (Annesi 2017; Beets 2015/Weaver 2015; Cradock 2016; Dzewaltowski 2010a; Economos 2020; Lee 2019; Riiser 2020). The shortest follow‐up was six weeks (Branscum 2013), and the longest follow‐up was two years (Dzewaltowski 2010a; Economos 2020). Interventions were categorised as staff‐based (i.e. targeted solely towards staff) (Annesi 2017; Beets 2015/Weaver 2015; Cradock 2016; Lee 2019; Riiser 2020), child‐based (i.e. targeted solely towards children) (Branscum 2013), or a combination of staff‐ and child‐based (Dzewaltowski 2010a), or combination of staff‐ and parent‐based (Brown 2018; Economos 2020).
Staff‐based interventions typically consisted of an initial training session of OSHC staff with study personnel, which varied in duration from one session of three to eight hours or three sessions of three hours with the goal to train staff to increase children's enjoyment and participation in MVPA conducive activities (Annesi 2017; Beets 2015/Weaver 2015; Cradock 2016; Dzewaltowski 2010a; Economos 2020; Lee 2019; Riiser 2020). Staff where then provided with ongoing support throughout the duration of the intervention period in most staff‐based intervention studies, which recommended 30 to 40 minutes of MVPA be achieved during OSHC sessions (Beets 2015/Weaver 2015; Cradock 2016; Dzewaltowski 2010a; Economos 2020; Lee 2019; Riiser 2020). The physical activity goal varied significantly between interventions; four had a specific MVPA goal (Annesi 2017; Beets 2015/Weaver 2015; Brown 2018; Cradock 2016), while others only had a goal to provide 30 minutes of physical activity (Dzewaltowski 2010a; Lee 2019), and another study only provided a vigorous physical activity goal of 20 minutes during OSHC sessions (Economos 2020). Riiser 2020 did not provide an MVPA or vigorous physical activity goal, but rather the goal for staff was to provide play‐based opportunities for physical activity. All but one study (Brown 2018) took place in the physical location of the OSHC service. Brown 2018 differed by taking children off site to work with after‐school care staff and study staff to engage in 40 minutes of targeted MVPA that were more like a physical education lessons.
Child‐based interventions focussed on health messaging to children to encourage them to participate in healthy lifestyle patterns for increasing physical activity, good nutrition behaviours (Branscum 2013; Dzewaltowski 2010a), and reducing recreational screen time (Dzewaltowski 2010a). Children were required to complete a task to demonstrate this learning. This occurred during the intervention to create a final product by the end of the intervention period (Branscum 2013; Dzewaltowski 2010a).
In addition to staff‐based interventions, three studies provided various resources for parents (Annesi 2017; Brown 2018; Economos 2020). This included resources such as newsletters, educational fact‐sheets, ideas for ways to support health physical activity and nutrition practices at home and in the community (Annesi 2017; Economos 2020), or physical resources, such as a cooler bag with recipe kits, strength and flexibility bands, and pedometers (Brown 2018).
Outcomes
All studies included assessments of children's physical activity and other measures of cardiovascular health (six measured BMI, one measured cardiovascular fitness and four measured process evaluation outcomes. Two studies had physical activity as the primary outcome of interest (Beets 2015/Weaver 2015; Cradock 2016). BMI was the primary outcome of interest for three trials (Annesi 2017; Branscum 2013; Dzewaltowski 2010a). Brown 2018 did not have BMI or physical activity as their primary outcome and used feasibility of the pilot intervention instead; however, the secondary outcomes were BMI and time spent in MVPA.
Primary outcomes
Total daily moderate‐to‐vigorous physical activity (minutes)
Four studies used accelerometry to assess physical activity (Beets 2015/Weaver 2015; Cradock 2016; Dzewaltowski 2010a; Riiser 2020), one study used wrist‐worn activity monitors (Brown 2018), and one study used a self‐report questionnaire of physical activity (Branscum 2013).
Secondary outcomes
Proportion of the care session spent in moderate‐to‐vigorous physical activity
Two trials used group‐based measures, such as the proportion of the care session spent in MVPA or categories such as "sufficiently active" determined through observational tools (e.g. SOPLAY (System for Observing Play and Leisure Activity in Youth)) (Beets 2015/Weaver 2015; Dzewaltowski 2010a).
Cardiovascular health
Five studies objectively measured BMI (Annesi 2017; Beets 2015/Weaver 2015; Branscum 2013; Brown 2018; Dzewaltowski 2010a), reported as BMI (Annesi 2017; Brown 2018; Dzewaltowski 2010a), BMI z‐score (Brown 2018; Dzewaltowski 2010a; Economos 2020), or BMI percentile (Beets 2015/Weaver 2015; Branscum 2013; Brown 2018).
One study measured cardiovascular fitness using a three‐minute endurance test (Annesi 2017).
Evaluation outcomes (including cost‐effectiveness)
Four studies assessed intervention feasibility outcomes and process evaluation data (Branscum 2013; Brown 2018; Lee 2019; Weaver 2015). Branscum 2013 assessed fidelity, programme dose, programme reach and context. Brown 2018 reported feasibility by recording recruitment, intervention participation and assessment completeness throughout the study. Parents of children in the study were invited to complete questionnaires on their satisfaction using Likert scales. Weaver 2015 assessed components of the ASP deemed critical to the Strategies to Enhance Practice (STEPs) programme. This included assessment of staff using System of Observing Staff Promotion of Physical Activity and Nutrition (SOSPAN) and assigning a STEPs value score to determine how well the centres were achieving the components of the STEPs programme. Lee 2019 assessed after‐school practice changes, programme reach, cost of in‐person versus online, adoption of programme components and fidelity (in‐person model only) using a purpose designed OSNAP (Out‐of‐School Nutrition and Physical Activity)‐OPAT (Observational Practice Assessment Tool) to gauge improvements in outside‐school hours childcare services practice. These were all descriptive measures and not assessments of outcome effect.
Adverse outcomes
No studies reported adverse outcomes.
Quality of life
No studies reported quality of life.
Excluded studies
There were 22 excluded studies. Reasons for exclusion included wrong study design (seven), wrong setting (eight), wrong intervention (three), wrong outcomes (two), wrong population (one) and duplicate (one). Six studies were excluded from this review because of the setting as despite being during the after‐school period or outside‐school hours childcare setting, the interventions were not delivered in the context of an existing outside‐school hours childcare setting (i.e. childcare that was available consistently throughout the school week/year). Some studies were only set up for the purpose of testing an intervention during the outside‐school hours period, and after the intervention was completed, the outside‐school hours childcare was no longer available.
Risk of bias in included studies
Risk of bias assessments for each outcome, including all domain judgements and support for judgement, is located in the risk of bias section (see Characteristics of included studies table), at the side of all forest plots and in Table 2. To access further detailed risk of bias assessment data, see Risk of Bias Assessment (external link).
Risk of bias of outcomes across all studies was similar and predominately of 'some concerns'. Study authors tended to report poorly on deviations from intended interventions.
Primary outcome
Total daily moderate‐to‐vigorous physical activity
Six studies reported MVPA (Beets 2015/Weaver 2015; Branscum 2013; Brown 2018; Cradock 2016; Dzewaltowski 2010a; Riiser 2020). Two of the studies were at low risk of bias (Beets 2015/Weaver 2015; Dzewaltowski 2010a), three with some concerns (Brown 2018; Branscum 2013; Riiser 2020), and one at high of risk of bias (Branscum 2013) with regard to deviations from intended interventions, deviations from intended interventions, missing outcome data, measurement of the outcome and selection of the reported result. Of those six studies, four were cluster‐RCTs (Beets 2015/Weaver 2015; Cradock 2016; Dzewaltowski 2010a; Riiser 2020), and all were at low risk of bias arising from the timing of identification and recruitment of participants in relation to timing of randomisation. Finally, only one study was at high risk of bias for missing outcome data and measurement of the outcome and some concerns relating to the randomisation process, deviations from the intended interventions and selection of the reported result (Branscum 2013). It did not report the randomisation process clearly in the published paper, did not provide clear information on how deviations were managed or did not provide information on a prespecified statistical plan.
Secondary outcomes
Proportion of session spent in moderate‐to‐vigorous physical activity
Two studies reported proportion of after‐school care session spent in MVPA (Beets 2015/Weaver 2015; Dzewaltowski 2010a). Both were at low risk of bias across all domains of the RoB 2 tool.
Cardiovascular health: body mass index and z‐score
Four studies reported BMI (Annesi 2017; Brown 2018; Dzewaltowski 2010a; Economos 2020). Similar to the MVPA outcome, there was variability in the risk of bias assessments in that three studies were at high risk of bias. These were in the domains of randomisation process (Economos 2020), missing outcome data (Annesi 2017), and measurement of the outcome (Economos 2020). This raises some concerns around the overall risk of bias of the results for this particular outcome. Of those four included studies, three were cluster‐RCTs (Annesi 2017; Dzewaltowski 2010a; Economos 2020). They varied in their risk of bias in relation to the timing of identification and recruitment of participants in relation to timing of randomisation. Only one study was at low risk of bias (Dzewaltowski 2010a), while one was of some concerns (Annesi 2017), and one was at high risk of bias (Economos 2020).
Cardiovascular measures: body mass index percentile
Two studies reported BMI percentile (Beets 2015/Weaver 2015; Branscum 2013). These varied significantly in risk of bias, with Beets 2015/Weaver 2015 at low risk of bias across all domains, and Branscum 2013 overall at high risk of bias. This was in relation to some concerns with randomisation process, deviations from the intended interventions and selection of the reported results, while it was at high risk of bias in missing outcome data. This raises some concerns around the overall risk of bias for this particular outcome due to the significant variability in results.
Cardiovascular measures: cardiovascular fitness
Only one study reported cardiovascular endurance using a three‐minute test and was at overall high risk of bias due missing outcome data and measurement of the outcome (Annesi 2017).
Process evaluation
Four studies reported process evaluation (Branscum 2013; Brown 2018; Lee 2019; Weaver 2015). There was significant variability in the results with one considered at overall high risk of bias (Branscum 2013), and two with some concerns (Brown 2018; Lee 2019). These were in the domains of randomisation process (Branscum 2013), deviations from the intended interventions (Branscum 2013; Brown 2018; Lee 2019), missing outcome data (Branscum 2013), measurement of the outcome (Branscum 2013; Brown 2018), and selection of the reported result (Branscum 2013).
Effects of interventions
See: Table 1
We grouped studies according to their outcomes. These are presented as primary and secondary outcomes meta‐analysed, followed by secondary outcomes which were synthesised narratively.
Primary outcome
Daily moderate‐to‐vigorous physical activity
Six studies reported postintervention total daily minutes of MVPA data or change in total daily minutes of MVPA (post–pre) that could be meta‐analysed (Beets 2015Weaver 2015; Branscum 2013; Brown 2018; Cradock 2016; Dzewaltowski 2010a; Riiser 2020). We considered outcomes at the longest follow‐up point recorded for each study. Studies used a variety of measures for total daily MVPA including accelerometry (Beets 2015/Weaver 2015; Cradock 2016; Dzewaltowski 2010a; Riiser 2020), wrist‐worn activity monitors (Brown 2018) and self‐report questionnaire (Branscum 2013). We combined results from these studies, with a larger value signifying a greater improvement in total daily MVPA.
Meta‐analysis pooling postintervention and change in total daily minutes of MVPA (follow‐up range: 11 weeks to three years) from trials comparing a physical activity intervention to control group revealed overall little to no difference in minutes of MVPA (MD 1.70, 95% CI –0.42 to 3.82; Z = 1.57, P = 0.12; 6 trials, 3036 participants; low‐certainty evidence; Analysis 1.1).
1.1. Analysis.

Comparison 1: Measures of physical activity, Outcome 1: MVPA (daily minutes), longest follow‐up
One study was at high risk of bias (Branscum 2013). Removing this study in a sensitivity analysis did not affect the result (MD 1.68, 95% CI –0.54 to 3.91; Z = 1.48, P = 0.14; 5 trials, 2971 participants; low‐certainty evidence; Analysis 1.2).
1.2. Analysis.

Comparison 1: Measures of physical activity, Outcome 2: MVPA (daily minutes) – sensitivity high risk of bias removed
Secondary outcomes
Proportion of care session spent in moderate‐to‐vigorous physical activity
Two studies assessed the proportion of the session spent in MVPA (Beets 2015/Weaver 2015; Dzewaltowski 2010a), which together provided moderate‐certainty evidence of the effects of physical activity interventions on increasing the proportion of the OSHC session spent in MVPA.
Beets 2015/Weaver 2015 found an improvement in the intervention groups for accumulating 30 minutes of MVPA at 12 months with 972 boys and girls compared to the 1018 boys and girls in the control group (intervention: 7.3%, 95% CI 1.4% to 13.1%; OR 2.26, 95% CI 1.35 to 3.80; control: 6.8%, 95% CI 1.6% to 12.1%; OR 2.85, 1.43 to 5.68).
By contrast, Dzewaltowski 2010a found no difference from baseline for both the intervention and control groups at two‐year follow‐up (134 (59%) children with intervention versus 112 (55%) children with control; P = 0.46; Table 2).
Cardiovascular health: body mass index and z‐score
Three studies provided a measure of BMI (Annesi 2017; Brown 2018; Dzewaltowski 2010a), and one study provided a measure of BMI z‐score (Economos 2020) for the physical activity intervention group compared with the control group, which was either usual outside‐school hours childcare (three studies) or an active control (one study). We considered outcomes at the longest follow‐up reported for each study.
Meta‐analysis of postintervention data (follow‐up range: 11 weeks to three years) from four trials comparing physical activity intervention to no intervention demonstrated little to no effect of interventions in reducing BMI/BMI z‐score (SMD –0.17, 95% CI –0.44 to 0.10; Z = 1.23, P = 0.22; 4 trials, 1684 participants; low‐certainty evidence; Analysis 2.1).
2.1. Analysis.

Comparison 2: Cardiovascular measures, Outcome 1: Body mass index (BMI) + BMI z‐score
Sensitivity analysis removed two studies at high risk of bias (Annesi 2017; Economos 2020). This made little difference to the result of change in BMI/BMI z‐score (SMD –0.34, 95% CI –1.13 to –0.45; Z = 0.85, P = 0.39; 2 trials, 268 participants; low‐certainty evidence; Analysis 2.2).
2.2. Analysis.

Comparison 2: Cardiovascular measures, Outcome 2: BMI + BMI z score – sensitivity high risk of bias removed
Cardiovascular measures: body mass index percentile and cardiovascular fitness
Two studies provided measures of weight status (Beets 2015/Weaver 2015; Branscum 2013). One reported BMI‐for‐age percentile (Branscum 2013), while the other reported percentage of children categorised as being normal weight, overweight and obese (based on BMI‐for‐age percentile categories less than 85th percentile; 85th to 95th percentile, and greater than 95th percentile). Branscum 2013 reported no significant differences in BMI‐for‐age percentile between the intervention and control groups at three months (longest follow‐up) (P = 0.567). Beets 2015/Weaver 2015 reported no change in percentage of children categorised as being normal weight or overweight between the intervention and control group across 12 months. However, they did report an improvement favouring the control group for percentage of children categorised as being obese (P < 0.001).
One study assessed cardiovascular fitness using a three‐metre endurance test (Annesi 2017), and reported an improvement in the intervention group at both three and nine months relative to the control group (P < 0.05). There was very low certainty of evidence for this outcome, due to high risk of bias for this study. Results are summarised in Table 2.
Cost‐effectiveness and process evaluation
One study reported the cost‐effectiveness of running physical activity interventions in OSHC, specifically the training of staff (Lee 2019). There was moderate‐certainty evidence that online training (USD 6383) was more cost‐effective than in‐person training (USD 24,402) for providing overall training to OSHC services when implementing a new programme. The trial also reported that more staff attended training for the in‐person condition compared with online training (no P value provided) and that OSHC directors set similar practice improvement goals in both the in‐person and online groups (Table 2).
Four studies provided descriptive assessment of process evaluation (Branscum 2013; Brown 2018; Lee 2019; Weaver 2015). Two studies reported improvements in physical activity practices in intervention compared with control sites, based on purpose‐designed, study‐specific validated scoring tools (Lee 2019: P = 0.04; Weaver 2015: P < 0.01). Brown 2018 described high levels of programme attendance (91% of children completed the programme), family involvement (33% to 100% for various programme components) and high parent satisfaction; however, they reported no P values due to the pilot nature of the trial. Branscum 2013 described that programme fidelity was high (91% to 100% of sessions delivered as planned), and that intervention and control conditions were similar for time taken for implementation and child attendance rates (Table 2).
Adverse outcomes
No studies reported adverse outcomes.
Quality of life measures
No studies reported quality of life measures.
Discussion
Summary of main results
This review examined physical activity interventions in outside‐school hours childcare settings evaluated in RCTs relative to usual outside‐school hours childcare programming. Of the included trials, six assessed physical activity with meta‐analysis suggesting that the interventions had little to no effect on total daily MVPA (Beets 2015Weaver 2015; Branscum 2013; Brown 2018; Cradock 2016; Dzewaltowski 2010a; Riiser 2020), and four assessed BMI with meta‐analysis indicating little to no effect (Annesi 2017; Branscum 2013; Dzewaltowski 2010a; Economos 2020). The finding of the interventions having little to no effect on MVPA held regardless of length of follow‐up (longest follow‐up assessed) and removal of studies at high risk of bias. There were no data on adverse effects or potential impact of the interventions on quality of life. Collectively, the findings of the review suggest that despite some promise for physical activity interventions in the outside‐school hours childcare setting, this is an under‐researched area, and that further research assessing the effects of interventions in this setting is likely to be useful.
The studies used a wide variety of intervention approaches to increase physical activity. Many studies included multiple components, targeted at multiple levels of influence (i.e. child‐level, staff‐level and setting‐level intervention elements). Few clear patterns emerged regarding the most effective intervention components, though review findings did suggest that studies that used a specific MVPA goal as part of their intervention programme may have had greater increases in total daily MVPA (Beets 2015Weaver 2015; Dzewaltowski 2010a).
There are a number of possible explanations for the lack of measurable effect on children's BMI found in this review. First, many studies were relatively short in duration, which may have been insufficient to impact adiposity, which accumulates over a prolonged period (Harris 2009). Second, children's BMI is a "whole‐of‐day" outcome, influenced both by their activity and dietary patterns in outside‐school hours childcare settings, and the activity and dietary patterns in other settings (e.g. at home and at school) (D'Souza 2020). Thus, it is possible that even if positive changes took place in the outside‐school hours childcare settings, they may have been offset or compensated for by activities in the other settings. Finally, due to the settings‐based nature of these studies, in many cases, the children measured at follow‐up were not necessarily the same children who were measured at baseline. Given this, there is likely to be considerable variation in the data, making intervention effects difficult to detect.
Overall completeness and applicability of evidence
We found few trials for this review (nine studies, 10 papers), and the total number of children involved in those trials was small. This contrasts with other childhood settings‐based physical activity intervention research (e.g. school‐based and early years childcare settings) which have a far larger evidence base of high‐quality research. In terms of outside‐school hours childcare settings physical activity intervention studies, there have been numerous other trials that were ineligible for this review, for example, due to their research design (e.g. for being quasi‐randomised or crossover trials) or contextual factors (i.e. ASPs set up for the research purposes, rather than being delivered in the context of an existing outside‐school hours childcare service). While such studies provide lower‐quality evidence (due to lack of having a true control group, lower ecological validity), such studies may have provided clues about promising intervention strategies.
All trials included in this review were conducted in high‐income countries (the US and Norway). While some individual studies were at lower SES groups within high‐income countries (e.g. Brown 2018), the applicability of the results to low‐ and middle‐income countries is questionable. Future research conducted in a greater range of countries and exploring other intervention approaches would broaden and strengthen the evidence base.
Quality of the evidence
GRADE assessment of the certainty of evidence in this review varied according to the outcomes, ranging from low to moderate. The outcome for which the certainty of the evidence was moderate was percentage of sessions spent in MVPA; however, the differing reporting meant this outcome could not be meta‐analysed. The certainty of the evidence for the MVPA outcome was low. It was downgraded based on inconsistency (due to moderate heterogeneity and small sample size) and imprecision (wide CI of meta‐analysis result). The certainty of the evidence for percentage of session spent in MVPA data was moderate due to it being downgraded in a single domain (inconsistency in the size of the effect). For the BMI findings, certainty was low due to the presence of risk of bias in three domains: the randomisation process (Economos 2020), missing outcome data (Annesi 2017), and measurement of the outcome (Economos 2020), which resulted in the risk of bias score being reduced to very serious. This suggests that there can be little confidence in the meta‐analysis findings regarding the impact of interventions in outside‐school hours childcare on MVPA time. In future, the quality of evidence, and therefore the certainty in findings, will improve as the evidence base grows (large number of studies) and as study designs become stronger (e.g. using larger sample sizes, leading to narrower CIs, and using more rigorous methodologies, such as stringent randomisation procedures).
Potential biases in the review process
The review used a comprehensive and rigorous methodology, including a broad search strategy, the screening of trials and extraction of data by two review authors independently, and the appraisal of risk of bias of outcomes within the included trials. While the review did not have any language limits, there may have been non‐English publications that were not identified by the search strategy, potentially introducing bias. This review was limited to RCTs and cluster‐RCTs in an attempt to assess the effectiveness of the interventions, which have been rigorously evaluated, thereby reducing the potential for confounding associated with non‐randomised and non‐controlled designs. The strict eligibility criteria of the review will have reduced the potential for bias, but in doing so, necessarily focusses on a subset of physical activity intervention research that has been conducted in outside‐school hours settings.
Agreements and disagreements with other studies or reviews
This is the first Cochrane Review examining physical activity interventions in outside‐school hours childcare settings in children aged 4 to 12 years. There have been four other non‐Cochrane systematic reviews conducted in this field (published between 2009 and 2016). These other systematic reviews assessed physical activity interventions that occurred in children between the ages of 5 and 18 years, and were in the after‐school time frame, but not exclusively in the outside‐school hours childcare setting (i.e. they included programmes set up temporarily for increasing physical activity). The most recent review assessed after‐school interventions in children and adolescents aged between 5 and 18 years (Mears 2016). In contrast to our review, Mears 2016 included RCTs, pilot RCTs, cross‐sectional RCTs, quasi‐experimental, longitudinal and cross‐sectional studies. Six studies were included for meta‐analysis, using a combination of accelerometry and self‐reported data to determine the MD in minutes per day of MVPA. They found an MD of 4.84 minutes/day of MVPA (95% CI –0.94 to 10.61; I2 = 70%). The findings of their meta‐analysis also suggested a small change in minutes per day of MVPA, which was not significant, and of questionable clinical significance. Similar to our review, they found evidence of heterogeneity and wide CIs.
Earlier reviews were conducted by Atkin 2011, Beets 2009, and Pate 2009. Of these earlier reviews, only Beets 2009 conducted a meta‐analysis. Of the 15 RCTs and quasi‐RCTs included in Beets 2009, six studies could be included in a meta‐analysis on physical activity (combining light physical activity, MVPA and vigorous physical activity), resulting in a pooled effect size of 0.44 (95% CI 0.28 to 0.60; I2 = 43%). This result was different to our review and that of Mears 2016, with a medium effect size on physical activity. This was not for MVPA exclusively, and rather all physical activity and thus not directly comparable to the current review. Both Atkin 2011 and Pate 2009 provided a narrative summary of the results, which assessed after‐school interventions either conducted in structured programmes or childcare, in children aged 5 to 18 years. Neither review attempted to meta‐analyse the data and both summarised the body of evidence for the physical activity interventions as having mixed effectiveness.
Authors' conclusions
Implications for practice.
This review highlights that there is a limited evidence base to guide outside‐school hours childcare practices. Collectively, the findings suggest that interventions did not substantially improve primary (moderate‐to‐vigorous physical activity (MVPA)) or secondary (body mass index (BMI), proportion of time spent in MVPA) outcomes in this setting and this is likely due to the variation in intervention methods among included trials. In those studies that showed improvements in physical activity, multi‐component interventions had better results. These multi‐component interventions consisted of a physical activity guideline against which services could aim for and measure physical activity in the setting. In addition, they provided initial and ongoing staff training, which appeared to provide ongoing effects. Staff‐led sessions were also a component of successful interventions. One trial demonstrated the greatest improvement in MVPA by running separate site staff‐led programmes during care sessions (Brown 2018); however, interventions that take this approach would require considerable ongoing resources to provide such services and may not be sustainable. Involvement of children and families, through education and resources was another approach that showed benefits and as such should be an important consideration for practice.
Implications for research.
Our findings show there is considerable scope to improve the evidence base to support the implementation of interventions to increase physical activity in outside‐school hours childcare settings. There was a limited number of randomised controlled trials (RCTs) for inclusion in this review, and a lack of high‐quality evidence. Of those studies included in the review, trials that had a focus on staff‐based interventions, with ongoing support and structure provided by a clear guideline showed the greatest improvement in primary (MVPA), and secondary (proportion of time spent in MVPA, BMI) outcomes. The findings suggest the use of a guideline for the setting is an important tool to gauge effectiveness of the outside‐school hours childcare practice on increasing physical activity. The variability in the results may suggest that the physical activity recommendation used in these trials may have been insufficient to demonstrate large increases in physical activity. This is consistent with previous research. Evidence suggests that even if there is a slight increase in time allocated to physical activity, this may only show a small increase in MVPA (Brazendale 2015). This may suggest that substantial increases in time allocated to physical activity, along with providing more staff training and engagement with children is a way to achieve increased MVPA. Additionally, future research should assess and report on wholistic measures of health such as well‐being, academic achievement, adverse effects and cost‐effectiveness of interventions to ensure essential evidence is produced and made available to assist outside‐school hours childcare services to implement such physical activity strategies.
This review identified opportunities for future research targeting interventions to increase physical activity in outside‐school hours childcare settings such as:
use of a guideline to standardise practice in outside‐school hours childcare which complements the World Health Organization physical activity and sedentary behaviour guideline for children aged 5 to 18 years;
use of educational materials and training for staff, coupled with ongoing support to assist with implementation and maintenance of changes in daily practice;
investigating the impact of interventions on physical activity for children from low‐ and middle‐income countries, in high‐income countries in minority or indigenous communities in outside‐school hours childcare settings;
investigating the impact of interventions on more wholistic measures of health such as children's well‐being and academic performance;
examination of the cost‐effectiveness of interventions found to be efficacious.
History
Protocol first published: Issue 7, 2019
Risk of bias
Risk of bias for analysis 2.1 Body mass index (BMI) + BMI z‐score.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Annesi 2017 | Low risk of bias | Nil issue with randomisation process, clearly explained procedure and no issues with baseline difference. | Low risk of bias | Minor deviations from the required protocol were typically corrected through direct interactions between the study staff and after‐school care counsellors. | High risk of bias | lack of information in published report about number of participants who completed follow up assessments and how the missingness of the data could have impacted the results. | Low risk of bias | Appropriate methods for measuring BMI implemented. | Some concerns | Appropriate analysis used based on information available in published report. | High risk of bias | Overall high risk of bias due to lack of information in published report about number of participants who completed follow up assessments and how the missingness of the data could have impacted the results. |
| Brown 2018 | Low risk of bias | Participants were allocated in a random, concealed manner with equal allocation to reduce the risk of baseline differences between intervention groups. | Some concerns | Both participants and those delivering the intervention were aware of intervention received. There was no information to support deviations from the intended intervention. | Low risk of bias | All but one participant completed baseline and follow up data. | Low risk of bias | Appropriate measures used to assess outcome of interest, however study staff provided the intervention and also completed the assessments which may introduce potential for risk of bias. | Low risk of bias | Published statistical plan in report. | Some concerns | Overall some concerns due to participants and study staff aware of intervention delivered, and the measure of the outcome by study staff aware of allocation, however was clearly reported in published trial. |
| Dzewaltowski 2010a | Low risk of bias | Generation of randomisation sequence and concealment were adequate, with no baseline differences that would suggest an issue with the randomisation process. | Low risk of bias | Both participants and those delivering the intervention were aware of intervention received but there were no deviations from intended interventions and the analysis was appropriate. | Low risk of bias | No issues with missing outcome data. | Low risk of bias | No information on whether outcome assessors were aware of intervention, however given the objective nature of the results unlikely to have affected outcome measurement. | Low risk of bias | Protocol not registered, but an appropriate statistical plan explicitly documented in published paper. | Low risk of bias | Overall low risk of bias across all domains. |
| Economos 2020 | High risk of bias | No information provided in published manuscript or answer to correspondence to study author. Therefore high risk of issue with random allocated and intervention concealment. Does report on baseline balancing. | Some concerns | Both participants and those delivering the intervention were aware of intervention received. There was no information to support deviations from the intended intervention. | Low risk of bias | Clear reporting of all data available for participants at various stages of intervention. | High risk of bias | Whilst the method for measuring the outcome of interest (BMI) was appropriate, no information is available to clarify if trained research staff were aware of the intervention received by study participants and if this may have affected results. | Some concerns | Some concerns due to the lack of information on prespecified analysis plan | High risk of bias | High risk of bias across randomisation process, measurement of the outcome, deviations from the intended interventions and selection of reported results. |
Acknowledgements
We acknowledge the help and support of Jodie Doyle, Managing Editor for Cochrane Public Health (CPH). We acknowledge the help of the academic librarians, Carole Gibbs (University of South Australia), Sarah McQuillen (University of South Australia) and Debbie Booth (University of Newcastle), for their assistance with the search strategy. Finally, Kerry Dawn and Teresa Moore from the Cochrane Method Support Unit for their assistance with the use and summary of the Cochrane RoB 2 tool.
We also acknowledge the CPH editors involved in assessing this review, as well as external referees, Dulce Estêvão and Marwa Saleh.
Appendices
Appendix 1. MEDLINE search strategy
| Line | Term | Results |
| 1 | exp Child/ | 1,946,540 |
| 2 | school teacher/ | 1696 |
| 3 | (child* or preschool* or pre school* or school age* or schoolage* or schoolboy* or schoolgirl* or school student* or boy? or girl? or teacher? or facilitator? or educator? or instructor?).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub‐heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms | 2,669,553 |
| 4 | 1 or 2 or 3 | 2,669,553 |
| 5 | exp exercise/ | 204,192 |
| 6 | motor activity/ | 97,557 |
| 7 | exp physical fitness/ | 31,507 |
| 8 | "Physical Education and Training"/ | 13,636 |
| 9 | walking/ | 34,126 |
| 10 | stair climbing/ | 190 |
| 11 | exp sports/ | 188,593 |
| 12 | dancing/ | 2982 |
| 13 | exp exercise therapy/ | 53,104 |
| 14 | (exercis* or physical* activ* or physical education or physical training or motor activity or fitness or aerobic? or walk* or stair climb* or climb* stair? or sport* or athletics or athletic performance or physical endurance or baseball or basketball or bicycling or cycling or boxing or football or golf or gymnastics or hockey or martial arts or tai ji or tai chi or mountaineering or tennis or badminton or run or running or ran or "track and field" or jog or jogging or jogged or cross country or orienteering or skating or skiing or volleyball or swim or swimming or swam or weight lifting or wrestling or dance or dancing or danced or yoga or active lifestyle).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub‐heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 1,109,352 |
| 15 | or/5‐14 | 1,119,901 |
| 16 | (after school* or afterschool* or before school* or out of school* or outside school hours or OOSH or vacation or holiday or OSHC or ASP).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub‐heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 42,612 |
| 17 | randomized controlled trial.pt. | 523,440 |
| 18 | controlled clinical trial.pt. | 94,075 |
| 19 | randomized.ab. | 513,079 |
| 20 | placebo.ab. | 216,224 |
| 21 | clinical trials as topic.sh. | 194,742 |
| 22 | randomly.ab. | 352,994 |
| 23 | trial.ti. | 236,747 |
| 24 | 17 or 18 or 19 or 20 or 21 or 22 or 23 | 1,352,842 |
| 25 | exp animals/ not humans.sh. | 4,790,230 |
| 26 | 24 not 25 | 1,246,009 |
| 27 | 4 and 15 and 16 | 1354 |
| 28 | 26 and 27 | 261 |
Appendix 2. CENTRAL database via the Cochrane Library search strategy
| Line | Term | Results |
| 1 | child* OR preschool* OR (pre NEXT school*) OR "school age" OR schoolgirl? OR schoolboy? OR "school student" OR boy? OR girl? OR teacher? OR facilitator? OR educator? OR instructor? | 285,704 |
| 2 | MeSH Descriptor: [Child] explode all trees | 56,346 |
| 3 | MeSH Descriptor: [School Teacher] explode all trees | 122 |
| 4 | #1 or #2 or #3 | 192,893 |
| 5 | MeSH Descriptor: [Exercise] explode all trees | 24,831 |
| 6 | MeSH Descriptor: [Motor Activity] this term only | 3714 |
| 7 | MeSH Descriptor: [Physical Fitness] explode all trees | 3329 |
| 8 | MeSH Descriptor: [Physical Education and Training] this term only | 1601 |
| 9 | MeSH Descriptor: [Walking] this term only | 4156 |
| 10 | MeSH Descriptor: [Stair Climbing] this term only | 15 |
| 11 | MeSH Descriptor: [Sports] explode all trees | 15,706 |
| 12 | MeSH Descriptor: [Dancing] this term only | 173 |
| 13 | MeSH Descriptor: [Exercise Therapy] explode all trees | 13,955 |
| 14 | exercis* OR (physical* NEXT activ*) OR “physical education” OR “physical training” OR “motor activity” OR fitness OR aerobic? OR walk* OR (stair? near/1 climb*) OR (climb* near/1 stair?) OR sport* OR athletics OR “athletic performance” OR “physical endurance” OR baseball OR basketball OR bicycling OR cycling OR boxing OR football OR golf OR gymnastics OR hockey OR “martial arts” OR “tai ji” OR “tai chi” OR mountaineering OR tennis OR badminton OR run OR running OR ran OR "track and field" OR jog OR jogging OR jogged OR “cross country” OR orienteering OR skating OR skiing OR volleyball OR swim OR swimming OR swam OR “weight lifting” OR wrestling OR dance OR dancing OR danced OR yoga OR “active lifestyle”): ti,ab,kw | 184,464 |
| 15 | #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 | 184,886 |
| 16 | ((after OR before OR “out of”) NEXT school*) or "outside school hours" or OOSH or vacation or holiday or OSHC or ASP | 2292 |
| 17 | #4 AND #5 AND #16 Selected LIMITS – In Trials |
194 |
[Enter text here]
Appendix 3. Embase search strategy
| Line | Term | Results |
| 1 | exp Child/ | 3,131,824 |
| 2 | school teacher/ | 1723 |
| 3 | (child* or preschool* or pre school* or school age* or schoolage* or schoolboy* or schoolgirl* or school student* or boy? or girl? or teacher? or facilitator? or educator? or instructor?).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] | 3,344,771 |
| 4 | 1 or 2 or 3 | 3,945,463 |
| 5 | fitness/ | 41,593 |
| 6 | exp exercise/ | 386,561 |
| 7 | walking/ | 74,255 |
| 8 | stair climbing/ | 1325 |
| 9 | exp sport/ | 183,424 |
| 10 | dancing/ | 5499 |
| 11 | kinesiotherapy/ | 36,364 |
| 12 | physical activity/ | 169,345 |
| 13 | motor activity/ | 51,053 |
| 14 | (exercis* or physical* activ* or physical education or physical training or motor activity or fitness or aerobic? or walk* or stair climb* or climb* stair? or sport* or athletics or athletic performance or physical endurance or baseball or basketball or bicycling or cycling or boxing or football or golf or gymnastics or hockey or martial arts or tai ji or tai chi or mountaineering or tennis or badminton or run or running or ran or "track and field" or jog or jogging or jogged or cross country or orienteering or skating or skiing or volleyball or swim or swimming or swam or weight lifting or wrestling or dance or dancing or danced or yoga or active lifestyle).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] | 1,551,277 |
| 15 | or/5‐14 | 1,574,533 |
| 16 | (after school* or afterschool* or before school* or out of school* or outside school hours or OOSH or vacation or holiday or OSHC or ASP).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub‐heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 51,645 |
| 17 | 4 and 15 and 16 | 1774 |
| 18 | randomized controlled trial/ | 652,794 |
| 19 | controlled clinical trial/ | 470,309 |
| 20 | "controlled clinical trial (topic)"/ | 11,496 |
| 21 | placebo.ab. | 317,679 |
| 22 | randomized.ab. | 744,030 |
| 23 | randomly.ab. | 473,912 |
| 24 | trial.ti. | 333,613 |
| 25 | Or/18‐24 | 1,746,588 |
| 26 | exp animal/ not human/ | 5,732,587 |
| 27 | 25 not 26 | 1,591,071 |
| 28 | 17 and 27 | 297 |
Appendix 4. ERIC search strategy
| Line | Searched for | Results |
| 1 | MAINSUBJECT.EXACT.EXPLODE("Children") | 108,731 |
| 2 | MAINSUBJECT.EXACT("Teachers") | 11,816 |
| 3 | child* OR preschool* OR "pre school*" OR "school age*" OR schoolage* OR schoolboy* OR schoolgirl* OR "school student" OR boy? OR girl? OR teacher? OR facilitator? OR educator? OR instructor? | 859,262 |
| 4 | S1 OR S2 OR S3 | 861,924 |
| 5 | MAINSUBJECT.EXACT.EXPLODE("Physical Activities") | 19,686 |
| 6 | MAINSUBJECT.EXACT.EXPLODE("Physical Fitness") | 4143 |
| 7 | MAINSUBJECT.EXACT.EXPLODE("Exercise") | 2275 |
| 8 | exercis* OR "physical* activ*" OR "physical education" OR "physical training" OR "motor activity" OR fitness OR aerobic? OR walk* OR "stair climb*" OR "climb* stair?" OR sport* OR athletics OR "athletic performance" OR "physical endurance" OR baseball OR basketball OR bicycling OR cycling OR boxing OR football OR golf OR gymnastics OR hockey OR "martial arts" OR "tai ji" OR "tai chi" OR mountaineering OR tennis OR badminton OR run OR running OR ran OR "track and field" OR jog OR jogging OR jogged OR "cross country" OR orienteering OR skating OR skiing OR volleyball OR swim OR swimming OR swam OR "weight lifting" OR wrestling OR dance OR dancing OR danced OR yoga OR "active lifestyle" | 93,120 |
| 9 | S5 OR S6 OR S7 OR S8 | 93,120 |
| 10 | MAINSUBJECT.EXACT.EXPLODE("After School Programs") | 3237 |
| 11 | "after school*" OR "afterschool*" OR "before school*" OR "out of school*" OR "outside school hours" OR vacation OR holiday OR OSHC OR OOSH OR ASP | 13,427 |
| 12 | S10 OR S11 | 13,427 |
| 13 | S4 AND S9 AND S12 | 1040 |
| 14 | noft(("randomi?ed controlled trial")) | 1498 |
| 15 | noft("controlled clinical trial") | 24 |
| 16 | ab(placebo) | 732 |
| 17 | ab(randomized) | 5528 |
| 18 | ti(trial) | 3301 |
| 19 | S14 OR S15 OR S16 OR S17 OR S18 | 8276 |
| 20 | S13 AND S19 | 12 |
Appendix 5. SportsDISCUS search strategy
| Line | Search Term | Results |
| S1 | DE "CHILDREN" OR DE "AIDS & children" OR DE "BOYS" OR DE "CHILD acrobats" OR DE "CHILD circus performers" OR DE "CHILD dancers" OR DE "CHILD development" OR DE "DANCE for children" OR DE "DEAFBLIND children" OR DE "GIRLS" OR DE "OUTDOOR recreation for children" OR DE "OVERWEIGHT children" OR DE "SCHOOL children" OR DE "SELF‐defense for children" OR DE "VIDEO games & children" | 50,291 |
| S2 | DE “TEACHERS” | 5763 |
| S3 | child* or preschool* or preschool* or "pre school*" or "school age*" or schoolage* or schoolboy* or schoolgirl* or boy# or girl# or teacher# or facilitator# or educator# or instructor# | 192,394 |
| S4 | S1 OR S2 OR S3 | 192,394 |
| S5 | DE "EXERCISE" OR DE "ABDOMINAL exercises" OR DE "AEROBIC exercises" OR DE "ANAEROBIC exercises" OR DE "AQUATIC exercises" OR DE "ARM exercises" OR DE "BACK exercises" OR DE "BREATHING exercises" OR DE "BREEMA" OR DE "BUTTOCKS exercises" OR DE "CALISTHENICS" OR DE "CHAIR exercises" OR DE "CHEST exercises" OR DE "CIRCUIT training" OR DE "COMPOUND exercises" OR DE "COOLDOWN" OR DE "DO‐in" OR DE "EXERCISE adherence" OR DE "EXERCISE for children" OR DE "EXERCISE for girls" OR DE "EXERCISE for men" OR DE "EXERCISE for middle‐aged persons" OR DE "EXERCISE for older people" OR DE "EXERCISE for people with disabilities" OR DE "EXERCISE for women" OR DE "EXERCISE for youth" OR DE "EXERCISE therapy" OR DE "EXERCISE video games" OR DE "FACIAL exercises" OR DE "FALUN gong exercises" OR DE "FOOT exercises" OR DE "GYMNASTICS" OR DE "HAND exercises" OR DE "HATHA yoga" OR DE "HIP exercises" OR DE "ISOKINETIC exercise" OR DE "ISOLATION exercises" OR DE "ISOMETRIC exercise" OR DE "ISOTONIC exercise" OR DE "KNEE exercises" OR DE "LEG exercises" OR DE "LIANGONG" OR DE "METABOLIC equivalent" OR DE "MULAN quan" OR DE "MUSCLE strength" OR DE "PILATES method" OR DE "PLYOMETRICS" OR DE "QI gong" OR DE "REDUCING exercises" OR DE "RUNNING" OR DE "RUNNING ‐‐ Social aspects" OR DE "SCHOOL exercises & recreations" OR DE "SEXUAL exercises" OR DE "SHOULDER exercises" OR DE "STRENGTH training" OR DE "STRESS management exercises" OR DE "TAI chi" OR DE "TREADMILL exercise" OR DE "WHEELCHAIR workouts" OR DE "YOGA" | 168,258 |
| S6 | DE "PHYSICAL activity" | 19,849 |
| S7 | DE "PHYSICAL fitness" OR DE "ANAEROBIC exercises" OR DE "ASTROLOGY & physical fitness" OR DE "BODYBUILDING" OR DE "CARDIOPULMONARY fitness" OR DE "CARDIOVASCULAR fitness" OR DE "CIRCUIT training" OR DE "COMPOUND exercises" OR DE "EXERCISE tolerance" OR DE "ISOLATION exercises" OR DE "LIANGONG" OR DE "MUSCLE strength" OR DE "PERIODIZATION training" OR DE "PHYSICAL fitness for children" OR DE "PHYSICAL fitness for girls" OR DE "PHYSICAL fitness for men" OR DE "PHYSICAL fitness for older people" OR DE "PHYSICAL fitness for people with disabilities" OR DE "PHYSICAL fitness for women" OR DE "PHYSICAL fitness for youth" OR DE "SPORT for all" | 116,298 |
| S8 | DE "WALKING" | 10,433 |
| S9 | DE "STAIR climbing" | 522 |
| S10 | DE "SPORTS" OR DE "AERODYNAMICS in sports" OR DE "AERONAUTICAL sports" OR DE "AGE & sports" OR DE "AMATEUR sports" OR DE "ANIMAL sports" OR DE "ANTISEMITISM in sports" OR DE "AQUATIC sports" OR DE "BALL games" OR DE "BALLISTICS in sports" OR DE "BASEBALL" OR DE "BIOMECHANICS in sports" OR DE "COLLEGE sports" OR DE "COMMUNICATION in sports" OR DE "CONTACT sports" OR DE "CROSS‐training (Sports)" OR DE "DISC golf" OR DE "DISCRIMINATION in sports" OR DE "DOG sports" OR DE "DOPING in sports" OR DE "ENDURANCE sports" OR DE "EXTREME sports" OR DE "FANTASY sports" OR DE "FASCISM & sports" OR DE "FEMINISM & sports" OR DE "GAELIC games" OR DE "GAY Games" OR DE "GOODWILL Games" OR DE"GYMNASTICS" OR DE "HOCKEY" OR DE "HOMOPHOBIA in sports" OR DE "HYDRODYNAMICS in sports" OR DE "INDIVIDUAL sports" OR DE "KINEMATICS in sports" OR DE "KNIFE throwing" OR DE "LGBT people & sports" OR DE "LOG‐chopping (Sports)" OR DE "MASCULINITY in sports" OR DE "MASS media & sports" OR DE "MILITARY sports" OR DE "MINORITIES in sports" OR DE "MOTION pictures in sports" OR DE "MOTORSPORTS" OR DE "NATIONAL socialism & sports" OR DE "NATIONALISM & sports" OR DE "NONVERBAL communication in sports" OR DE "OLYMPIC Games" OR DE "PARKOUR" OR DE "PHYSICS in sports" OR DE "PRESIDENTS ‐‐ Sports" OR DE "PROFESSIONAL sports" OR DE "PROFESSIONALISM in sports" OR DE "RACING" OR DE "RACISM in sports" OR DE "RACKET games" OR DE "RADAR in sports" OR DE "RECREATIONAL sports" OR DE "REGIONALISM & sports" OR DE "ROBOTICS in sports" OR DE "RODEOS" OR DE "ROLLER skating" OR DE "SCHOOL sports" OR DE "SENIOR Olympics" OR DE "SEXUAL harassment in sports" OR DE "SHOOTING (Sports)" OR DE "SHUTOUTS (Sports)" OR DE "SOCIALISM & sports" OR DE "SOFTBALL" OR DE "SPORT for all" OR DE "SPORTS & state" OR DE "SPORTS & technology" OR DE "SPORTS & theater" OR DE "SPORTS & tourism" OR DE "SPORTS competitions" OR DE "SPORTS for children" OR DE "SPORTS for girls" OR DE "SPORTS for older people" OR DE "SPORTS for people with disabilities" OR DE "SPORTS for women" OR DE "SPORTS for youth" OR DE "SPORTS forecasting" OR DE "SPORTS in antiquity" OR DE "SPORTS penalties" OR DE "SPORTS photography" OR DE "SPORTS rivalries" OR DE "SPORTS teams" OR DE "SPORTS tourism" OR DE "STEREOTYPES in sports" OR DE "TARGETS (Sports)" OR DE "TEAM sports" OR DE "TEAMWORK (Sports)" OR DE "TELEVISION & sports" OR DE "TRACEURS" OR DE "VIDEO tapes in sports" OR DE "VIOLENCE in sports" OR DE "WINTER sports" | 277,215 |
| S11 | DE "DANCE" | 5537 |
| S12 | DE "EXERCISE therapy" OR DE "EXERCISE therapy for children" OR DE "EXERCISE therapy for older people" OR DE "MENSENDIECK system" OR DE "ORTHOPTICS" OR DE "SWEDISH gymnastics" OR DE "THERAPEUTIC use of breathing exercises" | 6374 |
| S13 | exercis* or physical* activ* or physical education or physical training or motor activity or fitness or aerobic? or walk* or stair climb* or climb* stair? or sport* or athletics or athletic performance or physical endurance or baseball or basketball or bicycling or cycling or boxing or football or golf or gymnastics or hockey or martial arts or tai ji or tai chi or mountaineering or tennis or badminton or run or running or ran or track and field or jog or jogging or jogged or cross country or orienteering or skating or skiing or volleyball or swim or swimming or swam or weight lifting or wrestling or dance or dancing or danced or yoga or active lifestyle | 1,774,663 |
| S14 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 | 1,782,660 |
| S15 | after school* or afterschool* or before school* or out of school* or vacation or holiday or outside school hours or OOSH or OSHC or ASP | 13,356 |
| S16 | S4 AND S14 AND S15 | 2300 |
| S17 | "randomized controlled trial" | 6864 |
| S18 | "controlled clinical trial" | 772 |
| S19 | AB randomized | 25,763 |
| S20 | AB placebo | 11,910 |
| S21 | "clinical trials as topic" | 10 |
| S22 | AB randomly | 18,964 |
| S23 | TI trial | 13,932 |
| S24 | S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 | 54,804 |
| S25 | S16 AND S24 | 103 |
Appendix 6. TROVE search strategy
(“physical activity” OR sport*) AND ("outside school hours" OR "out of school" OR "after‐school") AND intervention* AND child*
Search limited to thesis
Total 356 thesis
Appendix 7. ProQuest Dissertations and Theses search strategy
| Line | Search Term | Results |
| S1 | mainsubject(child) | 4838 |
| S2 | mainsubject(teacher) | 41,906 |
| S3 | ab, ti (child*or preschool* OR "school age*" OR schoolage* OR schoolboy* OR schoolgirl* OR boy? OR girl? OR teacher? OR facilitator? OR educator? OR instructor?) | 114,589 |
| S4 | S1 OR S2 OR S3 | 160,003 |
| S5 | ab, ti(Physical activity) | 614 |
| S6 | ab, ti(physical fitness) | 91 |
| S7 | ab, ti(exercis* or "physical* activ*" or "physical education" or "physical training" or "motor activity" or fitness or aerobic? or walk* or "stair climb*" or "climb* stair?" or sport* or athletics or "athletic performance" or "physical endurance" or baseball or basketball or bicycling or cycling or boxing or football or golf or gymnastics or hockey or "martial arts" or "tai ji" or "tai chi" or mountaineering or tennis or badminton or run or running or ran or "track and field" or jog or jogging or jogged or "cross country" or orienteering or skating or skiing or volleyball or swim or swimming or swam or "weight lifting" or wrestling or dance or dancing or danced or yoga or "active lifestyle") | 5634 |
| S8 | S5 OR S6 OR S7 | 5663 |
| S9 | ab, ti("after school*" or afterschool* or "before school*" or "out of school*" or "outside school hours" or OOSH or vacation or holiday or OSHC or ASP) | 120 |
| S10 | S4 AND S8 AND S9 | 2 |
| S11 | noft("randomi?ed controlled trial") | 3861 |
| S12 | noft("controlled clinical trials") | 158 |
| S13 | ab(randomized) | 22,214 |
| S14 | ab(placebo) | 6304 |
| S15 | noft("clinical trials") | 8012 |
| S16 | ab(randomly) | 55,363 |
| S17 | ti(trial) | 6369 |
| S18 | S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 | 88,807 |
| S19 | S10 AND S18 | 0 |
Appendix 8. Data extraction form
Data extraction form – Cochrane Review
Form Version/Date: Version 1.0; 19 February 2019
Review Title:Interventions in outside‐school hours settings for promoting physical activity amongst schoolchildren aged 4 to 12 years
| Study: First author and year of publication: | |
| Name of review author completing this form: | |
| Date form completed: |
| Notes: Unpublished ‐ for own use e.g. references to be followed up, source of information (especially if multiple reports of the same trial, or unpublished data/personal communication included) |
Methods:
| Notes/comments | Paper/ page | |
| Details of Study | ||
| Aim of intervention (As stated in the trial report/s. What was the problem that this intervention was designed to address?) | ||
| Aim of study (As stated in the trial report/s. What was the trial designed to assess?) | ||
| Study design / i.e. CRCT or RCT; number of experimental conditions | ||
| Unit of randomisation (i.e. individual or group for cluster trials) | ||
| Method of randomisation | ||
| Methods of recruitment of participants (How were potential participants approached and invited to participate? ADDED: Brief description only here: e.g. Convenience. No need to contact authors if missing). | ||
| Inclusion/exclusion criteria for participation in study (ADDED: Include explicit criteria only, not only post‐hoc exclusions). | ||
| Informed consent obtained? (Yes/No/Unclear) | ||
| Ethical approval (Yes/No/Unclear –no details required) | ||
| Funding (including source, amount, if stated). | ||
| Study Date/Recruitment date | ||
| Consumer involvement (e.g. In design of study and/or intervention; in delivery of intervention; in evaluation of intervention; in interpretation of study findings) |
Participants:
| Notes/comments | Paper/ page | |
| Description (e.g. children; carers; parents of children; educators; policy makers) ADDED: Choose from these categories only | ||
| Age: range, mean (SD) | ||
| Gender: % Male, % Female | ||
| SES: (disadvantaged population (yes/no/unclear) e.g. mean income, maternal education | ||
| Geographic location (e.g. City/State/Country) | ||
| Setting (e.g. school based outside school hours care, community based outside school hours care | ||
| Presence of baseline imbalance |
Intervention and Comparison:
| Intervention A | Control | Paper/ page | |
| Overview / content: | |||
|
Number: Assessed for eligibility: Eligible: Excluded: Refused to take part: Randomised: Allocated: Received allocated intervention/control: Did not receive allocated intervention / control: Lost to follow up: Withdrawn/discontinued intv/control: Analysed: Excluded from analysis: |
|||
|
Theoretical basis (e.g. sociocognitive theory) |
|||
|
Delivery format / modality |
|||
|
Setting (e.g. School based OSHC, community based, church/private third party/government run) |
|||
| Delivery information: | |||
| Number of sessions: | |||
| Duration of intervention | |||
| Intervention period | |||
| Details of providers: | |||
| Who delivers the intervention | |||
| Number of providers | |||
| Training received in intervention delivery | |||
| Qualifications of intervention providers | |||
| Process measures: | |||
| Was the intervention delivered as intended(Record any assessment of this). | |||
| Details of co‐interventions |
Outcomes:
| Notes/comments | Paper/ page | |
| Principal and secondary outcome measures (as identified by the study authors). Only include if relevant to the review. Note if NOT primary outcome). |
||
| Methods of assessing outcome measures (e.g. accelerometry, pedometers, self‐report questionnaire) | ||
| Validity and reliability of outcome measures reported? If so, paste quote from paper in here | ||
| Methods of follow‐up for non‐respondents | ||
| Timing of outcome assessment (including frequency, length of follow up (for each outcome)) | ||
| Adverse events (e.g. complaints, levels of dissatisfaction, adverse incidents, side effects)) if presence or absence of events not clearly stated = 'unclear' | ||
| Statistical analysis (include method and any assumptions made for intention to treat analyses and for CRCT any accounting for clustering effects | ||
| Unit of analysis |
Results
These data will be used in the 'Comparisons and data' section in Review Manager 5 (not the 'Characteristics of included studies' table) and as the basis for the Results section of your review text.
All data are numbers (of participants), not percentages.
Dichotomous outcomes
| Outcome | Timing of outcome assessment (days/months) | Intervention group* | Control group | Notes | ||
| Observed (n) | Total (N) | Observed (n) | Total (N) | |||
*Note: add additional columns if there is more than one intervention group, e.g. Intervention Group A, Intervention Group B…
| Any other reported results (i.e. effect estimates, P values) |
Continuous outcomes
| Outcome | Timing of outcome assessment (days/months) | Intervention group |
Control group | Notes | ||||
| *Mean (pre‐post) / Mean change | Standard deviation | N | *Mean (pre‐post) / Mean change | Standard deviation | N | |||
| Any other reported results (i.e. effect estimates, P values) |
*Delete as appropriate
Data and analyses
Comparison 1. Measures of physical activity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 MVPA (daily minutes), longest follow‐up | 6 | 3036 | Mean Difference (IV, Random, 95% CI) | 1.70 [‐0.42, 3.82] |
| 1.2 MVPA (daily minutes) – sensitivity high risk of bias removed | 5 | 2971 | Mean Difference (IV, Random, 95% CI) | 1.68 [‐0.54, 3.91] |
Comparison 2. Cardiovascular measures.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Body mass index (BMI) + BMI z‐score | 4 | 1684 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.44, 0.10] |
| 2.2 BMI + BMI z score – sensitivity high risk of bias removed | 2 | 268 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐1.13, 0.45] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Annesi 2017.
| Study characteristics | ||
| Methods |
Study design: cluster randomised control trial. Study aim: to test a new theory‐based protocol for its effects on measures of fitness and BMI, and its proposed psychosocial mediators, during elementary after‐school (out‐of‐school hours) care. Study length: 9‐month school year. Differences in baseline characteristics: reported as baseline difference in sample size, did not report differences in age, gender, racial makeup or SES. No data provided in published results. Unit of allocation: after‐school service. Unit of analysis: participant‐ and treatment‐group level. |
|
| Participants |
Demographic/socioeconomic characteristics: children aged 10–13 years; 86 intervention sites, 55 control sites; mean age 10.0 (SD 0.9) years; 55% boys; 31% white, 65% black, 4% other; median family income USD 74,000 (quote: "those characteristics approximated that of the region where this research was conducted" p 366). Geographic location: South‐East US, in YMCA after‐school sites. Inclusion criteria: children enrolled in after‐school care, no further details. Exclusion criteria: not reported. Recruitment method: participants recruited from YMCA after‐school sites across South‐East US, details on recruitment/uptake not mentioned. Number of services randomised: not provided. Setting: YMCA sites, not specified if school‐based or community‐based. |
|
| Interventions |
Intervention group Youth Fit 4 Life curricular: 45‐minute sessions, 4 days/week for 24 weeks (96 lessons in total); 5‐minute warm‐up of light movement and stretching; 30‐minute MVPA games (e.g. tag and ball games); 10 minutes of education on self‐management/nutrition skills every second day. Theoretical basis: social cognitive theory. Delivery format: face‐to‐face sessions with trainer, consisted of 6 hours of training attended by existing after‐school care staff. After‐school care staff:researcher ratio was 18:1, goal was to dedicate 45 minutes per day of PA. Training received: 6 hours plus manual detailing each structured lesson and education materials. Control group Typical after‐school care (sporadic organised activities, e.g. running and ball games) at the discretion of the after‐school care staff and based on children's interests. Theoretical basis: none. Delivery format: usual after‐school care format. Training received: not stated. |
|
| Outcomes |
Primary
Secondary
Timing of outcome assessments: baseline (0), 3 months, 9 months. Adverse events: not reported. Statistical analysis: assumed missing data (14%) was missing at random, and, therefore, used imputation. Set P < 0.05, used series of mixed model repeated measures ANOVA, if significant followed 1‐way ANOVAs. Multiple mediation analyses were used to determine simultaneous entry of changes in self‐regulation, mood and self‐efficacy, linear bivariate analyses between gender, age, race and BMI. |
|
| Notes | ||
Beets 2015.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT. Study aim: to assist children to achieve 30 minutes of MVPA during after‐school care sessions. Study length: 12 months. Differences at baseline: baseline imbalance in programme scheduled time for PA opportunities and race. No difference in number of enrolments, PA space, poverty, programme duration or age. Unit of allocation: group (after‐school service site level). Unit of analysis: service level. Funding: National Heart, Lung, and Blood Institute of the NIH under award number R01HL112787. Amount not stated. |
|
| Participants |
Demographic/socioeconomic details: children and educators in after‐school services. Control group: 1018 children; age: mean 8.1 (SD 1.8) years; 52.4% boys; race: 48.4% white non‐Hispanic, 44.7% African American, 6.9% other; % of population in poverty according to 2010 census: 17.5%. Intervention group: 972 children; age: mean 7.9 (SD 1.8) years; 53.3% boys; race: 64.4% white non‐Hispanic, 29.7% African American, 5.7% other; % of population in poverty according to 2010 census: 13.3%. Geographic location: Columbia, South Carolina, US. All services involved in the study were within a 1.5‐hour drive of the University of South Carolina. Inclusion criteria: after‐school providers operating in a south‐eastern state, representing 12 after‐school provider organisations, randomly selected from a pre‐existing list of 533 programme providers within a 1.5‐hour drive of the University of South Carolina. The list was provided by a state level organisation responsible for policy and resources for after‐school care providers. After‐school care providers were defined as childcare programmes operating immediately after the school day, every day of the school year for a minimum of 2 hours, serving a minimum of 30 elementary‐aged (6–12 years) children; operating in a school, community, or faith setting; and providing a snack, homework assistance/completion time, enrichment (e.g. arts and crafts), and opportunities for PA. Exclusion criteria: programmes that were singularly focused (e.g. dance, tutoring) or PA‐focused (e.g. sports, activity clubs) were not eligible for participation. Recruitment method: after‐school providers from 553 programme providers within a 1.5‐hour drive of the University of South Carolina were invited to participate in the study. 376 eligible for study, of those 76 did not operate Monday to Friday, 53 had < 30 children enrolled, 28 did not have sufficient information to evaluate eligibility; 20 chosen at random from the remaining 219. Number of services randomised: 20 services: 10 to control, 10 to intervention. Setting: 9 school settings, 4 faith/church settings, 7 community settings. |
|
| Interventions |
Intervention group Theoretical basis: systems change theory. Delivery format: face‐to‐face training. Focussed on professional development training targeting ASP directors and educators, to develop high‐quality schedules. Consisted of 1–2 week rotating schedule total of 3 hours. This occurred prior to beginning of school year, then 4 booster sessions occurred over an entire afternoon service (3 p.m. to 6 p.m.). At end of day, site leaders and research personnel met to discuss areas consistent and inconsistent with meeting PA standards and strategies to address this for the following day. STEPs programme. Based on systems change theory. Focussed primarily on ASP leaders, helping them to develop high‐quality schedule that included PA opportunities every day, and clearly articulated the roles and responsibilities of staff during scheduled activity opportunities. Also "LET US Play" principle (removal of lines, elimination of elimination, reduction in team size, getting uninvolved staff and children involved in the games, creative use of space, equipment and rules), which puts the focus on skill development and enjoyment. This was delivered via 1 × 3‐hour workshop with after‐school care directors, plus 4 × "walk throughs" at each ASP where study personnel and after‐school care staff discussed feedback/strategies. Training received: 1 × 3‐hour training prior to intervention commencing, then 4 × "booster" sessions by the after‐school care staff trained by research personnel. Control group Theoretical basis: none. Delivery format: usual after‐school care. Training received: none. |
|
| Outcomes |
Primary
Secondary
Timing of outcome assessments: baseline (spring 2013), follow‐up (spring 2014). Adverse events: none reported. Statistical analysis: random‐effects logic models. Divided analysis into intention‐to‐treat and cohort analysis. Cohort analysis considered a more complete analysis, accounted for clustering. |
|
| Notes | ||
Branscum 2013.
| Study characteristics | ||
| Methods |
Study design: RCT. Study aim: to help children learn and engage in behaviours to reduce obesity, through pilot test of the "Comics for Health" intervention. Study length: 6 weeks. Differences at baseline: none. Unit of allocation: site level. Unit of analysis: site level. Funding: United Health HEROES grant by Youth Services America and an internal faculty‐mentoring grant, provided by the College of Education, Criminal Justice, and Human Services at the University of Cincinnati. |
|
| Participants |
Demographic/socioeconomic details: children aged 8–11 years. Intervention group: 37 children; mean age 8.86 (SD 0.86) years; 47% boys; 73% white, 14% African American, 5% Asian. Control group: 34 children; mean age 9.12 (SD 1.01) years; 57% boys; 82% white, 6% African American, 12% Asian. Geographic location: Ohio, US. Inclusion criteria: not reported. Exclusion criteria: not reported. Recruitment method: children from 12 mid‐western YMCA ASPs. Number of services randomised: 12. |
|
| Interventions |
Intervention group Theoretical basis: social cognitive theory: version of comics for health, focus on 4 health behaviours: engaging in ≤ 2 hours of screen time per day (lesson 1), consuming water and sugar‐free drinks instead of sugar‐sweetened beverages (lesson 2), participating in ≥ 60 minutes of PA per day (lesson 3) and consuming 5 servings of fruits and vegetables per day (lesson 4). Also provided education around self‐efficacy and self‐control. Delivery format: 4 × 30‐minute lessons from corresponding author of study to children. Training received: n/a. Control group Theoretical basis: knowledge‐based version of comics for health, focussing on the 4 health behaviours engaging in ≤ 2 hours of screen time per day (lesson 1), consuming water and sugar‐free drinks instead of sugar‐sweetened beverages (lesson 2), participating in ≥ 60 minutes of PA per day (lesson 3), and consuming 5 servings of fruits and vegetables per day (lesson 4). Delivery format: 4 × 30‐minute lessons from corresponding author of study to children. Training received: n/a. |
|
| Outcomes |
Primary
Secondary
Timing of outcome assessments: baseline, 6 weeks (post‐test), 3 months (follow‐up). Process evaluation: recorded and published in Health Promotion and Practice 2012. Adverse events: none reported. Statistical analysis: to ensure that both groups were similar at pretest, a comparison of demographic and study variables between both groups was first done, using either a Chi2 test (for discrete variables) or univariate ANOVA (for continuous variables). To evaluate (quote) "the efficacy of the programme, univariate repeated‐measures ANOVAs with a partial nested design were used. The primary independent variable for this study was the intervention (group). This was a fixed, categorical variable with 2 levels: 1. theory‐based group and 2. knowledge‐based group. The second independent variable was ASP, which was nested within levels of group variable (the nested). This was a random quantitative variable with 12 levels (six programmes were randomly assigned to receive the experimental intervention and six programmes were randomly assigned to receive the comparison intervention). The third independent variable was a within‐group variable of time, with 3 levels of measurement. Therefore, the design used for testing the experimental and comparison interventions was a hierarchical one between and one within repeated‐measures design. In calculating the required sample size of children for this study, G*Power was used with the following criteria: an α level of significance (α = .05), statistical power (β = .80), an estimated medium effect size (f = 0.30), the number of groups (n = 2), the number of measurements (n = 3), and an attrition rate of 20%" p 68. |
|
| Notes | ||
Brown 2018.
| Study characteristics | ||
| Methods |
Study design: RCT – pretest/post‐test feasibility study. Study aim: to assess the feasibility and behavioural and health‐related outcomes of the Generations Health Program intervention an outside‐school childcare programme and home‐based obesity prevention intervention for rural native American and non‐native American children. Study length: 11 weeks. Differences at baseline: no. Unit of allocation: individual. Unit of analysis: group. |
|
| Participants |
Demographic/socioeconomic details: 23 (52%) children were Native America, with mean age 8 years; 48% had a BMI classification of normal weight and the remainder were classified as overweight (13%) or obese (39%); all parents reported having a high school degree and 74% had completed some tertiary education. 26% of parents were male included in the study. 82.6% of participants qualified for free and reduced‐price school lunch programme, 35% were at risk of food insecurity. Geographic location: the study took place at an existing Boys and Girls Club (an outside‐school hours childcare) site in a small, rural town on an American Indian reservation (population 29,000) comprised of 33% Native American and 66% non‐Native American people in Montana, US. Inclusion criteria: Native American and non‐Native American children aged 6–9 years, who attend the outside‐school hours childcare ≥ 3 times per week and planned to attend throughout the study period. Children living with a physical disability were not excluded. Exclusion criteria: not reported. Recruitment method: obtained a list of eligible children from after‐school care programme directors then trained research staff recruited children. Number of services randomised: 1 outside‐school hours programme. |
|
| Interventions |
Intervention group Theoretical basis: ecological model of PA. Delivery format and description of intervention: project staff delivered in‐person sessions to children, telephone messages and resource kits. Consisted of 3 × 1‐hour lesson, followed by 1 text message to parents per week, 3 tool kits given to parents per week, 2‐hours per month family night and 1 hour one‐off information night about the study. Children were taken off site from the regular OSHC service to participate in physical activities. Details of providers: project staff. Number of providers: 5. Training received: 1‐day training session 3 weeks before study began. Control group Theoretical basis: none. Delivery format and description of intervention: usual after‐school care programming. Children in the comparison group received the usual activities at the OSHC site, which routinely included opportunities for PA. There were no activities for parents in the comparison group, except to complete pre‐ and post‐test measures. Details of providers: usual after‐school staff. Number of providers: not specified. Training received: none. |
|
| Outcomes |
Primary Intervention feasibility
Secondary Behavioural and health outcomes
Timing of outcome assessments: pre‐ and post‐test measures (11 weeks between measures). Adverse events: none reported. Statistical analysis: no formal sample size calculation, as the study aimed to recruit sufficient participants to generate estimates of variability for our outcome measures and to generate preliminary estimates of effect for the intervention. Behavioural and health outcome variables used 2 tailed paired t tests to detect changes with 95% confidence interval using SPSS. Multi‐variate ANOVA for PA, sleep efficiency and wake after sleep onset data. Significance was set at P = 0.05. |
|
| Notes | ||
Cradock 2016.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT. Study aim: to test the effectiveness of the OSNAP initiative in increasing children's PA levels in existing ASPs. The OSNAP initiative works with ASPs to improve nutrition and PA‐related practices, environments and policies using a socioecological model and a community‐based participatory research approach. The OSNAP initiative resources and links to research evidence are available online. The 2 PA goals were to include 30 minutes of moderate, fun PA for every child every day (including outdoor activity, if possible) and to offer 20 minutes of vigorous PA 3 times per week. Study length: 6 months. Differences at baseline: none reported. Unit of allocation: service level. Unit of analysis: individual level. |
|
| Participants |
Demographic/socioeconomic details: 402 children (182 in intervention group, 220 in control group); aged 5–12 years, mean 7.7 (SD 1.7) years; 48.8% boys; race: 7.5% white non‐Hispanic, 30.6% black non‐Hispanic, 34.8% Hispanic/Latino, 3.2% Asian, 21.5% other; SES not collected. Geographic location: Boston, Massachusetts, US. Inclusion criteria: ASPs were eligible if they served children aged 5–12 years, enrolled ≥ 40 children and ran continuously from mid‐October through the end of May (2010–2011). Exclusion criteria: not reported. Recruitment method: eligible ASPs were identified and recruited to participate in the study through collaboration between study staff and local community programme providers. Number of services randomised: 20: 10 to control, 10 to intervention. |
|
| Interventions |
Intervention group Theoretical basis: socioecological model and community‐based participatory research approach. Delivery format and description of intervention: professional development session provided to teams of staff from intervention sites including staff and programme directors. 3 × 3 hour OSNAP initiative LC sessions that helped the after‐school service personnel identify areas for improvement against OSNAP initiative, develop relevant policies and communicate changes to parents and other partners. At these sessions, after‐school service personnel shared progress with other teams and participated in skill development sessions. Study staff provided additional PA skill building sessions (including Food & Fun After School curriculum, recess‐focused training by Playworks and SPARK training). Between LC sessions, study staff provided intervention programmes, with technical assistance and reminders via telephone, newsletter and email. Intervention sites were invited to apply for up to USD 200 to support implementation. Details of providers: study staff. Number of providers: not reported. Training received: not reported. Control group Theoretical basis: none. Delivery format and description of intervention: usual after‐school programming. Details of providers: after‐school personnel. Number of providers: not reported. Training received: not reported. |
|
| Outcomes |
Primary Child level outcomes
Secondary Programme level outcomes
Timing of outcome assessments: baseline (27 September to 12 November 2010); follow‐up (25 April to 27 May 2011). Adverse events: none reported. Statistical analysis: power calculation: based on previous data with 30 participants clustered within 10 matched intervention and control programmes, assuming an intraclass correlation coefficient of children's PA minutes within programmes of 0.01 and a correlation of 0.6 between baseline and follow‐up PA minutes, researchers would have 80% power to detect a mean difference of 4.6 (SD 19.7) minutes of MVPA as a primary outcome. SDs were based on data collected in 4 pilot sites. PA measures: linear mixed‐effects models used to investigate whether students at participating OSNAP initiative programmes experienced greater increases in accelerometer‐derived PA levels during the programme period compared with those at control programmes. The intervention effect was estimated by an interaction term of period (follow‐up was 1, and baseline was 0) by intervention (intervention was 1, and control was 0), in addition to period and intervention status main effects. Models were adjusted at the child level for daily minutes monitored; child sex, race/ethnicity and grade; matched pair indicators at the programme level; model of accelerometer worn (to account for potential differences in output between models); and percentage deviation from the mean annual temperature and the presence of precipitation at the observation day level. Programme‐level random intercepts were used to account for the correlation due to clustering of students within programmes. A compound symmetry within‐person error covariance structure was used to account for nesting of successive daily observations within students. The degrees of freedom for significance tests were calculated using the between‐within method. Adjusted means for each outcome at baseline and follow‐up were estimated from models adjusting for clustering, monitored minutes and monitor model only. Post‐hoc analyses using stratified mixed models examined whether intervention effects differed by sex or grade (kindergarten to grade 2 (UK age about 5–8 years) vs grades 3–6 (UK age about 8–12 years)). Accelerometer counts were collected at 1‐minute epochs, MVPA minutes were estimated using age‐specific cut points used in national surveillance with thresholds of 4 METs for MVPA and 6 METs for vigorous PA. < 100 counts per minute was considered sedentary. Non‐wear = 60 consecutive minutes of 0 counts. Implausibly high counts were replaced with previous minutes and next minutes' mean. |
|
| Notes | ||
Dzewaltowski 2010a.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT. Study aim: to evaluate the effectiveness of the HOP'N ASP for preventing obesity in children attending ASPs to promote PA and healthy eating by building the capacity of existing ASPs. Study length: 2 years (baseline 2005–2006; follow‐up 2006–2007 and 2007–2008). Differences at baseline: none: stratified into 2 groups of high SES/low diversity, low SES/high diversity and matched based on the percentage of students who qualified for free and reduced‐price lunch, and the percentage of students who were non‐Hispanic white or of diverse race/ethnicity. Unit of allocation: service level. Unit of analysis: child level. |
|
| Participants |
Demographic/socioeconomic details: intervention group baseline characteristics: 29 children; mean age 9.34 (SD 0.65) years; 47% boys; 56% not eligible for free/reduced‐price lunch; ethnicity: 7% American Indian/Native Alaskan, 1% Asian, 11% black/African American, 8% Hispanic/Latino, 1% Native Hawaiian/Pacific Islander, 71% white, 1% other. Control group baseline characteristics: 43 children; mean age 9.19 (SD 0.66) years; 54% boys; 42% not eligible for free/reduced‐price lunch; ethnicity: 10% American Indian/Native Alaskan, 1% Asian, 28% black/African American, 5% Hispanic/Latino, 1% Native Hawaiian/Pacific Islander, 53% white, 2% other. Geographic location: Kansas, Missouri US. Setting: schools with onsite after‐school care programme. Inclusion criteria: ASP on elementary school grounds, children in 4th grade (aged 9–10 years) elementary school. Exclusion criteria: not reported. Recruitment method: all 8 schools involved in the ASP alliance of the Lawrence Public School District, Douglas County Co‐Op extension service, Lawrence Boys and Girls Club and community partners were considered for inclusion, of those, 7/8 sites were invited and included in the study. The 8th site was excluded as it was not on the elementary school grounds. Number of services randomised: 7; 3 to control sites, 4 to intervention site. |
|
| Interventions |
Intervention group Theoretical basis: social cognitive theory and an ecological developmental systems approach. Delivery format and intervention: the HOP'N intervention targeted the development of the skills and efficacy of ASP staff and children to build healthy after‐school environments. It included 3 levels of training.
Duration: ASPs lasted 2.5 hours per day, elements incorporated into programme. Weekly sociocognitive theory‐based curriculum delivered to each after‐school site for 60 minutes once a week for 29 sessions in total. Details of Providers: study staff. Number of providers: 4 after‐school care services; number of staff at each service not reported. Training received: not reported. Control group Theoretical basis: none. Delivery format and intervention: usual after‐school care. Details of providers: usual after‐school care staff. Number of providers: 3 after‐school care services; number of staff at each service not reported. Training received: none. |
|
| Outcomes |
Primary Child level outcomes
Secondary After‐school and HEPA opportunities
Timing of outcome assessments: all outcomes measured at baseline, year 1 and year 2. Adverse events: none reported. Statistical analysis: power calculation: study was powered to detect a 0.5 kg/m2 difference in BMI between a sample size of 4 intervention and 4 control schools with a reduction in the detectable difference adjusting for age, ethnicity and gender using 20 students per group. To adjust for the clustered data structure, a mixed model 3‐level design structure (school, year, child) was used to analyse the after‐school participant outcomes (autumn to spring academic year change in BMI z‐score, autumn to spring academic year change in BMI, and accelerometer measured PA across the year) and fourth grade student outcomes (spring BMI z‐score, spring BMI). The impact of the intervention on the after‐school site PA session opportunities and fruit and vegetable snack offerings was analysed using a non‐parametric Mann‐Whitney U test for each group comparison. |
|
| Notes | ||
Economos 2020.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT. Study aims: to increase the bone quality and muscular strength of children participating in the intervention and to improve knowledge and level of bone health and behaviours (e.g. level of bone‐strengthening PA and calcium intake). Study length: 2‐year intervention period. Differences in baseline characteristics: yes; small but statistically significant difference in mean of both height and weight between intervention and control groups. The control group boys were shorter and lighter than 2 intervention groups (BONES‐only group and BONES + parent group); the control group girls were lighter than one intervention group (BONES‐only group). No statistically significant difference between BMI z‐score for all groups, or children who completed measurements at all 3 time points vs 1 or 2 time points. Unit of allocation: group level. Unit of analysis: participant level. Funding: National Institute of Child Health and Human Development and the National Institutes of Health (R01 HD037752), with product support from The Minute Maid Company, The Almond Board of California, Cabot Creamery of Vermont, Stonyfield Farm, Hood Inc., and SPORTime International. |
|
| Participants |
Demographic/socioeconomic characteristics: mean age 7.18 years, 64.5% white, 10.5% black, 9% Hispanic, 16% other. Geographic location: Massachusetts and Rhode Island, US. Inclusion criteria: lower‐income communities (based on % children eligible for free or reduced‐price meals) that had multiple after‐school services (≥ 3 per community) with > 40 eligible children per programme. For an after‐school service to be eligible for inclusion, the after‐school service had to recruit ≥ 8 children, randomised in a 2:1 ratio into 1 of the 2 intervention groups (BONES‐only or BONES + parent) or control group. Used a blocked design to consider the size of the ASP and community SES were balanced so that the final 3 groups had a similar number of programmes, similar number of participants per programme and a similar SES distribution. Exclusion criteria: not reported. Recruitment method: within 33 eligible communities, 384 ASPs were invited to participate in the study. 181 did not respond, a further 60 were excluded based on lack of interest, programme structure or administrative turn over. 143 programmes were then approached for formal consent to participation in the project, with 83 recruited to the study. Number of services randomised: 25 programmes randomised to BONES group (459 children), 33 programmes to the BONES + parent group (611 children) and 25 programmes to control group (354 children). Setting: after‐school care programmes: 42% in schools, 18% in YMCAs, 18% in community agencies, 15% in boys and girls clubs, and 7% in other private agencies. |
|
| Interventions |
Intervention group 1 BONES: consisted of 3 components 1. Let's eat: focus on eating calcium rich foods with calcium 380 mg, 2. Let's play: focus on active games that provided 20 minutes of vigorous PA 3 × week, with a 5‐minute jumping component 5 × week and 3. Let's explore: nutrition education lessons delivered as a fun hands‐on activity 2 × week. Was designed to fit in with current after‐school care programming (which typically offered homework and academic assistance and recreational activities and snacks, rather than formal PA programming). Theoretical basis: 3 models combined: expectancy model of motivation, health belief model and theory of reasoned action social cognitive theory. Delivery format: in‐person. Training received: ASP staff received attended a comprehensive training programme at start of each intervention year and ongoing support from study research staff with newsletters, site visits and telephone calls. Intervention group 2 BONES + parent. Same 3 components as BONES, but also incorporated a parent/caretaker component which involved receiving material (e.g. newsletters to complement lessons, educational worksheets, coupons, and a detailed community directory/resource guide for family‐friendly active living and healthy eating) to complement work in the ASP. Theoretical basis: 3 models combined: expectancy model of motivation, health belief model and theory of reasoned action social cognitive theory. Delivery format: in‐person. Training received: ASP staff received attended comprehensive training programme at start of each intervention year and ongoing support from study research staff with newsletters, site visits and telephone calls. Control group Usual care. Theoretical basis: n/a. Delivery format: n/a. Training received: n/a. |
|
| Outcomes |
Primary
Secondary
Timing of outcome assessments: baseline, end of year 1, end of year 2. Adverse events: not reported. |
|
| Notes | ||
Lee 2019.
| Study characteristics | ||
| Methods |
Study design: group RCT. Study aim: to assess the cost and effectiveness of 2 existing models of delivery (online and face‐to‐face) of the OSNAP initiative in after‐school care programmes in YMCA services in the US. Study length: 6 months (autumn 2016 to spring 2017). Differences in baseline characteristics: no. Unit of allocation: group. Unit of analysis: group. Funding: National Cancer Institute Award (R21CA201567‐ 01A1) and The JPB Foundation. |
|
| Participants |
Demographic/socioeconomic characteristics: mean age 8.1 years, provided mean child enrolment at each site; in‐person site mean 35.4 (SD 21.5) years, online site mean 43.8 (SD 27.2) years, control site mean 40.8 (SD 29.4) years. Overall, participants across sites were 47% white, 24% black/African American, 16% Hispanic/Latino, 3% Asian children and 2.5% other. Geographic location: South, Mid‐West and North‐East communities in US. Inclusion criteria: eligible services had to be located in 1 of 3 US regions (South, Mid‐West, North‐East) in communities with < 75% of residents identified as white in 2010 census. The YMCAs included had to have ≥ 15 after‐school sites and demonstrated readiness for implementation and potential to benefit. This was assessed by services having pledged to a commitment to promote nutrition and PA as part of the campaign 'Partnership for Healthy America 2016'. Services that self‐reported to YMCA as having ≥ 1 site that met 25–75% (i.e. those with ≥ 25% standards met readiness criteria, while those with ≤ 75% standards were likely to benefit) of the Health Eating and Physical Activity standards in 2016 were included in the sample. Only 12/450 YMCA associations met the inclusion criteria for service size (15 sites per association) and demographic criteria (< 75% of residents identified as white). Exclusion criteria: not reported. Recruitment method: YMCA staff help to select 3 YMCA associations with limited competing demands and strong leadership. All 3 eligible associations agreed to participation, with 70 after‐school care services recruited. 2/3 YMCA staff were recruited at each association to lead the in‐person train‐the‐trainer arm. 1–3 adult staff members from each study site were enrolled and participated in human research. Number of services randomised: 70, 24 to in‐person intervention (South 8, Mid‐West 11, North‐West 5), 23 to online intervention (South 8, Mid‐West 10, North‐West 5), 23 to control (South 7, Mid‐West 11, North‐West 5). |
|
| Interventions |
Intervention group 1 In‐person – train the trainer model. Theoretical basis: Proctors conceptual model for implementation research used to understand the study intervention, implementation and outcomes. Delivery format: in‐person. Training received: 1. initial 6‐hour training session delivered by principal investigator at each YMCA site in autumn 2016; 2. 2–3 YMCA staff in each region were trained as facilitators to deliver OSNAP in their local YMCA; 3. research staff trained as facilitators delivered 3 × 3‐hour in‐person learning sessions to after‐school care staff at YMCAs in their association and 1 × 1 hour Food and Fun training session. After‐school site staff received ongoing assistance via site visits, email, text and telephone. In addition, the principal investigator conducted 2 × 1‐hour group telephone calls to the after‐school care staff between learning sessions. Intervention group 2 Online training for train the trainer. Theoretical basis: Proctors conceptual model for implementation research used to understand the study intervention, implementation and outcomes. Delivery format: online. Training received: 7 × short, self‐paced learning modules of 1–1.5 hours' durations via online platform (Canvas) between November 2016 and May 2017. Used online discussion boards, facilitated by research team member for questions and connect after‐school site staff. Local facilitators and research staff provided reminders and logistical support for the platform. 2–3 staff members per site were encouraged to participate in training. Control group Theoretical basis: n/a. Delivery format: n/a. Training received: n/a; did not receive any OSNAP training materials until the following school year (autumn 2017 to spring 2018). |
|
| Outcomes |
Primary
Secondary
Timing of outcome assessments: baseline, 6 months. Adverse events: not reported. |
|
| Notes | ||
Riiser 2020.
| Study characteristics | ||
| Methods |
Study design: cluster‐RCT. Study aim: to evaluate the effectiveness of active play in ASPs. Consisted of a course for ASP staff aimed at supporting PA play and PA among first‐graders. Study length: 7 months. Differences in baseline characteristics: none. Unit of allocation: group level. Unit of analysis: individual participant level accounting for clustering. Funding: Norwegian Fund for Postgraduate Training in Physiotherapy and OsloMet – Oslo Metropolitan University as part of the first author's postdoctoral fellowship. The funding body had no impact on the design of the study, or the data collection, analysis, interpretation or in writing of the manuscript. Open access was funded by OsloMet. |
|
| Participants |
Demographic/socioeconomic characteristics: children aged 5–6 years, in first grade. Mean and SD of age not provided. 426 at baseline, 383 at follow‐up 1, 313 at follow‐up 2. At baseline, 52.2% were boys and 14.9% were overweight or obese. Geographic location: school health services in municipalities of 3 counties in eastern Norway. Inclusion criteria: all students attending ASPs were eligible. Exclusion criteria: none. Recruitment method: step 1: engage school physiotherapists to be involved in the study as the physiotherapists assisted with implementation and assessment of the intervention; step 2: school administrators of invited schools provided written consent to participation in study; step 3: parents of school students attending ASPs were required to provide written consent. Number of services randomised: 14 to either intervention or control arm. Setting: existing ASP attached to school. |
|
| Interventions |
Intervention group Theoretical basis: self‐determination theory. Delivery format: short course delivered to ASP staff to increase their knowledge of and skills in creating PA supportive environments by accommodating and encouraging activities, rather than directing them in a controlled manner. Training received: prior to commencing in the ASP, the local school physiotherapists who were involved in the intervention groups, attended an 8‐hour training course with study aims and intervention explained along with their role and responsibility throughout the trial; and they received intervention materials (workbook). ASP staff received 2 × training sessions led by the study researchers and school physiotherapists. Session 1 focussed on children's PA play, the importance of friends and the activity play space. Session 2 focussed on ASP staff's interaction styles, the children's motivation for PA and the ways in which the staff could support the children's engagement in PA. Control group Theoretical basis: n/a. Delivery format: usual care provided during ASP. Training received: n/a. |
|
| Outcomes |
Primary
Secondary
Timing of outcome assessments: baseline, 7 months, 19 months. Adverse events: not reported. Statistical analysis: random‐effects models used to account for clustering of pupils within schools; using mixed‐effects models and longitudinal data analysis method to adjust baseline values. Controlled for daily outdoor mean temperature at each school and used unstructured covariance pattern for level 1 residuals and identity covariance structure for random effects. |
|
| Notes | ||
Weaver 2015.
| Study characteristics | ||
| Methods |
Study design: process evaluation of Beets 2015 RCT. Study aim: 3 aims: 1. describe the level of implementation, 2. assess the level of STEPs implementation to the main outcomes (i.e. children's engagement in MVPA and snacks served) and 3. explore differences in services defined as 'high' and 'low' implementers. Study length: 12 months. Differences at baseline: baseline imbalance in programme scheduled time for PA opportunities and race. No difference in number of enrolments, PA space, poverty, programme duration or age. Unit of allocation: group (after‐school service site level). Unit of analysis: service level. Funding: National Heart, Lung, and Blood Institute of the NIH under award number R01HL112787. Amount not stated. |
|
| Participants |
Demographic/socioeconomic details: children and educators in after‐school services. Intervention group: 972 children; age: mean 7.9 (SD 1.8) years; 53.3% boys; 64.4% white non‐Hispanic, 29.7% African American, 5.7% other; % of population in poverty according to 2010 census: 13.3%. Control group: 1018 children; age: mean 8.1 (SD 1.8) years; 52.4% boys; 48.4% white non‐Hispanic, 44.7% African American, 6.9% other; % of population in poverty according to 2010 census: 17.5%. Geographic location: Columbia, South Carolina, US. All services involved in the study were within a 1.5‐hour drive of the University of South Carolina. Inclusion criteria: 20 after‐school providers operating in a south‐eastern state, representing 12 after‐school provider organisations, were randomly selected from a pre‐existing list of 533 programme providers within a 1.5‐hour drive of the University of South Carolina. The list was provided by a state‐level organisation responsible for policy and resources for after‐school care providers. For this study, after‐school care providers were defined as child care programmes operating immediately after the school day, every day of the school year for a minimum of 2 hours, serving a minimum of 30 elementary‐aged (6–12‐year‐old) children; operating in a school, community or faith setting; and providing a snack, homework assistance/completion time, enrichment (e.g. arts and crafts) and opportunities for PA. 22 programmes that were singularly focused (e.g. dance, tutoring) or PA focused (e.g. sports, activity clubs) were not eligible for participation. Exclusion criteria: none. Recruitment method: after‐school providers from a list of 553 programme providers within a 1.5‐hour drive of the University of South Carolina were invited to participate in the study. 376 eligible for study; of these, 76 did not operate Monday to Friday, 53 had < 30 children enrolled, 28 did not have sufficient information to evaluate eligibility; 20 chosen at random from the remaining 219. Number of services randomised: 20; 10 to control, 10 to intervention. Setting: 9 school setting, 4 faith/church setting, 7 community setting. |
|
| Interventions |
Intervention group Theoretical basis: systems change theory. Delivery format: face‐to‐face training. Focussed on professional development training targeting ASP leaders, educators, to develop high quality schedules. Consisted of 1–2 week rotating schedule total of 3 hours. This occurred prior to beginning of school year, then 4 booster sessions occurred over an entire afternoon service (3 p.m. to 6 p.m.). Following end of day site leaders and research personnel met to discuss areas consistent and inconsistent with meeting PA standards and strategies to address this for the following day. STEPs programme. Based on systems change theory. Focuses primarily on ASP leaders, helping them to develop high‐quality schedule that include PA opportunities every day, and clearly articulating the roles and responsibilities of staff during scheduled activity opportunities. Also, 'LET US Play' principle (removal of lines, elimination of elimination, reduction in team size, getting uninvolved staff and children involved in the games, creative use of space, equipment and rules), which puts the focus on skill development and enjoyment. This was delivered via 1 × 3‐hour workshop with ASP leaders, plus 4 × 'walk throughs' at each ASP where study personnel and ASP staff discussed feedback/strategies. Training received: 1 × 3‐hour training prior to intervention commencing, then 4 × 'booster' sessions; after‐school staff trained by research personnel. Control group Theoretical basis: none. Delivery format: usual after‐school care. Training received: none. |
|
| Outcomes | Process evaluation measures
Analysis
|
|
| Notes | ||
ANOVA: analysis of variance; ASP: after‐school programme; BMI: body mass index; CATCH: Co‐ordinated Approach To Child Health; HAAND: Healthy After school Activity and Nutrition Documentation; HEPA: healthy eating and physical activity; HOP'N: Healthy Opportunities for Physical Activity and Nutrition; LC: learning collaborative; METs: metabolic equivalents; MVPA: moderate‐to‐vigorous physical activity; n/a: not applicable ; OPAT: Out‐of‐school Nutrition and Physical Activity Observation Practice Assessment Tool; OSNAP: Out of School Hours Nutrition and Physical Activity; PA: physical activity; RCT: randomised controlled trial; SD: standard deviation; SES: socioeconomic status; SOFIT: System of Observing Fitness Instruction Time; SOSPAN: System for Observing Staff Promotion of Physical Activity and Nutrition; STEPs: Strategies To Enhance Practice; VO2max: maximum rate of oxygen consumption.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Beets 2014 | Protocol of paper included in review. |
| Beets 2016a | Wrong intervention; not a physical activity intervention rather a healthy‐eating intervention focussed on improving snacks offered in after‐school care programmes. |
| Beets 2016b | Wrong study design; used a delayed cross‐over RCT; not a cluster‐RCT or RCT. |
| Beets 2018 | Wrong study design; published results of process evaluation of Beets 2016b, which used a cross‐over RCT design. |
| Connor 1986 | Wrong study design; quasi‐experimental design stated in methods, not an RCT or cluster‐RCT. |
| Dzewaltowski 2010b | Duplicate. |
| Gutin 2008 | Wrong setting; intervention was a programme set up specifically for the research and not in a regular outside‐school hours childcare service that was provided on a regular, ongoing basis. |
| Iversen 2011 | Wrong study setting and study design; intervention programme set up specifically for the intervention and not conducted in an ongoing, regular outside‐school hours childcare service. In addition, unclear from methods described in published paper of study design, stated schools were randomised using random number table but no information on the groups. |
| Jago 2014 | Wrong setting; intervention programme set up specifically for intervention during the after‐school period, not in an ongoing, regular outside‐school hours childcare service. |
| Jago 2019 | Wrong setting; intervention programme set up specifically for intervention during the after‐school time period, not in an ongoing, regular outside‐school hours childcare service. |
| Kelder 2005 | Wrong study design; pilot study using a pre–post quasi‐experimental design, not a cluster‐RCT or RCT. |
| Kenney 2014 | Wrong outcomes; assessed the psychometric properties of a tool to assess physical activity and nutrition policies in outside‐school hours childcare programmes, and improvement on policy. Did not have data on primary or secondary outcomes of interest. |
| Madsen 2013 | Wrong setting; intervention programme set up specifically for intervention during the after‐school period as part of outside‐school hours care but available as a separate programme in after‐school care not as a physical activity programme in an ongoing, regular outside‐school hours childcare service. |
| NCT04213014 | Wrong setting; intervention programme set up specifically for intervention during the after‐school period, not in an ongoing, regular outside‐school hours childcare service. |
| Nigg 2004 | Wrong study design; not an RCT. |
| Salcedo Aguilar 2010 | Wrong setting; intervention programme set up specifically for intervention during the after‐school period, not in an ongoing, regular outside‐school hours childcare service. |
| Sharpe 2011 | Wrong study design; used pre–post test quasi‐experimental design. |
| Tibbitts 2019 | Wrong setting; intervention programme set up specifically for intervention during the after‐school period, not in an ongoing, regular outside‐school hours childcare service. |
| Weaver 2016 | Wrong study aims; designed to assess implementation of STEPs programmes in after‐school care programmes not interventions to increase physical activity. |
| Wiecha 2012 | Wrong outcomes; study reported on the development of the Healthy Eating and Physical Activity quality standards, not on the outcomes of interest to this review. |
| Yin 2005 | Wrong setting; intervention programme set up specifically for intervention during the after‐school time period, not in an ongoing, regular outside‐school hours childcare service. |
| Yin 2012 | Wrong setting; intervention programme set up specifically for intervention during the after‐school time period, not in an ongoing, regular outside‐school hours childcare service. |
RCT: randomised controlled trial; STEPs: Strategies To Enhance Practice.
Differences between protocol and review
Eligibility criteria
There was an error in the terminology of the published protocol (Virgara 2019), in eligibility criteria under 'types of interventions'. It read "We will include interventions that involve strategies targeting physical activity in other contexts, such as the home or school, only if two review authors (RV and CM/LL/AP) judge the majority of the intervention to have occurred in the outside‐school hours setting." This sentence should have read "We will include interventions that involve strategies targeting physical activity in other contexts, such as the home or school, only if two review authors (RV and CM/AP) judge the majority of the intervention (>75%) to have occurred in the outside‐school hours childcare setting". The previously published statement would have allowed interventions that occurred outside school hours to be included, when, in fact, these may have been set up temporarily for research.
Types of outcomes
We reclassified the four primary outcomes of the protocol (duration of MVPA, number of steps, proportion of care session spent in MVPA and proportion of children categorised as being sufficiently active; Virgara 2019) into one primary outcome (total daily MVPA) and one secondary outcome (proportion of the care session spent in MVPA).
In the protocol, the outcomes for the summary of findings table were (Virgara 2019):
intensity of physical activity (e.g. Light, MVPA;
overall physical activity (duration of activity as minutes or % time);
cardiovascular health;
quality of life;
adverse outcomes.
Outcomes 1 and 2 have been edited to now be:
Total daily MVPA (minutes per day): assessed by direct observation (using a standardised, validated direct‐observation tool), accelerometry, self‐report (i.e. from children or childcare staff or both, reported using a validated questionnaire), heart rate monitor or wrist‐worn activity monitor (including pedometers and consumer‐level devices where results were extrapolated to minutes in MVPA). It was anticipated data would be expressed in terms of baseline and postintervention mean values (and SDs) or change scores;
proportion of the care session spent in MVPA (e.g. through direct observation, self‐report or accelerometry).
Search strategy
Changes to search strategy after academic librarian review from University of Newcastle; terms added were: pre school*, school student*, OOSH, "outside school hours". These items were added to all databases. We added the term 'physical activity' to the Embase, ERIC and SportsDISCUS database searches, which is a subject heading unavailable in MEDLINE.
Assessment of risk of bias
We used RoB 2 to assess the risk of bias, rather than the original tool referred to in the protocol (Virgara 2019).
Assessment of reporting biases
There was an insufficient number of studies (fewer than 10) for both the primary and secondary outcomes of interest to assess reporting biases with funnel plots. Therefore, there are no funnel plots in this review, and we addressed reporting bias with the RoB 2 tool.
Analysis
We used the longest term of follow‐up for data.
Software
We used RevMan Web for writing the review, rather than Review Manager 5 as specified in the protocol (Virgara 2019).
Summary of findings table
We added cost‐effectiveness to the summary of findings table.
We removed process evaluation from the summary of findings table. This was due to the descriptive nature of this measure, which meant that they could not be assessed using the GRADE tool and, therefore, were unsuitable for inclusion in table.
The outcomes in the summary of findings table are now:
total daily MVPA (primary outcome);
proportion of care session spent in MVPA (secondary outcome);
cardiovascular health: BMI (secondary outcome);
cardiovascular health: cardiovascular fitness (secondary outcome);
evaluation outcomes: cost‐effectiveness (secondary outcome);
adverse outcomes (secondary outcome);
quality of life (secondary outcome).
Contributions of authors
RV, CM, LL, AP and MR conceptualised the review question.
All authors contributed to the writing of the review.
RV and CM focused on the background section, while RV and LW focused on the methods section.
RV developed the search strategy with input from CM, LW, AP, LL and academic librarians from the University of South Australia and University of New South Wales.
RV, AP, TF, LL, KB and CM completed all searches, screening, data extraction and risk of bias assessments. MB was not involved in the study selection, data extraction or risk of bias assessment of any of the included studies.
KB and RV completed all data analyses.
RV and LW completed GRADE assessments and the summary of findings table.
All authors contributed to the discussion section.
RV and CM have overall responsibility for the review.
Sources of support
Internal sources
-
University of South Australia, Other
Associate Professor Carol Maher, Dr Anna Phillips, Dr Katherine Baldock and Ms Carole Gibbs are supported by the University of South Australia employment.
-
Flinders University, Other
Dr Lucy Lewis is supported through employment at Flinders University.
-
University of Wollongong, Other
Professor Anthony Okely is supported through employment at the University of Wollongong.
-
University of South Carolina, Other
Professor Michael Beets is supported through employment at University of South Carolina.
-
St Pius X School, Other
Ms Mandy Richardson is supported by employment at St Pius X School.
-
Hunter New England Health and University of Newcastle, Other
Associate Professor Luke Wolfenden is supported through employment at Hunter New England Health and University of Newcastle.
External sources
-
NHMRC, Australia
Associate Professor Carol Maher is supported by an NHMRC Career Development Position (2017–2020).
-
University of South Australia – Research Training Program domestic (RTPd) Stipend. Health Development Adelaide, University of Adelaide – PhD Top Up Scholarship, Australia
Ms Rosa Virgara is a PhD Candidate with the University of South Australia and is supported by a RTPd Stipend. In addition, she is supported by a Top Up Scholarship from Health Development Adelaide, University of Adelaide.
-
NHMRC, Australia
Associate Professor Luke Wolfenden is an NHMRC Career Development Fellow (2013 to present) CDF II and Brawn Career Development Fellow at School of Medicine and Public Health, University of Newcastle. He is also Hunter New England Clinical Research Fellow for Hunter New England Population Health.
Declarations of interest
RV: No interests to declare.
AP: No interests to declare.
LL: No interests to declare.
KB: No interests to declare.
LW is a Co‐ordinating Editor for Cochrane Public Health Group. He has not been involved in the editorial process of this review. He also declares that he is a health promotion manager that is responsible for providing preventive health services to a community in Australia. His team is considering outside of school hours care as a setting for health promotion.
TF: No interests to declare.
MR: MR is an Out of School Hours Care Director for St Pius X School, Windsor Gardens SA, Australia. In addition, she is the South Australian Chairperson for the Out of School Hours Care Association and the South Australian Representative for the National Out of School Hours Care Services Alliance and a member of the Education Standards Board of South Australia.
AO: No interests to declare.
MB: MB is an author on a study (Beets 2015), funded by the National Institutes of Health, included in this review. He was not involved in the study selection, data extraction or risk of bias assessment of any of the included studies.
CM: No interests to declare.
New
References
References to studies included in this review
Annesi 2017 {published data only}
- Annesi JJ, Walsh SM, Greenwood BL, Mareno N, Unruh-Rewkowski JL. Effects of the Youth Fit 4 Life physical activity/nutrition protocolon body mass index, fitness and targeted social cognitive theory variables in 9- to 12-year-olds during after-school care. Journal of Paediatrics and Child Health 2017;53:365-73. [DOI: 10.1111/jpc.13447] [DOI] [PubMed] [Google Scholar]
Beets 2015 {published data only}
- Beets MW, Weaver RG, Turner-McGreivy G, Huberty J, Ward DS, Pate RR, et al. Making policy practice in afterschool programs: a randomized controlled trial on physical activity changes. American Journal of Preventive Medicine 2015;48(6):694-706. [DOI] [PMC free article] [PubMed] [Google Scholar]
Branscum 2013 {published data only}
- Branscum P, Sharma M, Leigh Wang L, Wilson B, Rojas-Guyler L. A true challenge for any superhero: an evaluation of a comic book obesity prevention program. Family and Community Health 2013;36(1):63-76. [DOI] [PubMed] [Google Scholar]
Brown 2018 {published data only}24274245
- Brown B, Harris KJ, Heil D, Tryon M, Cooksley A, Semmens E, et al. Feasibility and outcomes of an out-of-school and home-based obesity prevention pilot study for rural children on an American Indian reservation. Pilot and Feasibility Studies 2018;4:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cradock 2016 {published data only}
- Cradock AL, Barrett JL, Giles CM, Lee RM, Kenney EL, deBlois ME, et al. Promoting physical activity with the out of school nutrition and physical activity initiative – a cluster-randomized controlled trial. Journal of American Medical Association Pediatrics 2016;170(2):155-62. [DOI] [PubMed] [Google Scholar]
Dzewaltowski 2010a {published data only}
- Dzewaltowski DA, Rosenkranz RR, Geller KS, Coleman KJ, Welk GJ, Hastmann TJ, et al. HOP'N after-school project: an obesity prevention randomized controlled trial. International Journal of Behavioural Nutrition and Physical Activity 2010;7:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Economos 2020 {published data only}
- Economos CD, Hennessy E, Chui K, Dwyer J, Marcotte L, Must A, et al. Beat Osteoporosis – Nourish and Exercise Skeletons (BONES): a group randomized controlled trial in children. BMC Pediatrics 2020;20:83. [CLINICAL TRIALS: NCT00065247.] [DOI: 10.1186/s12887-020-1964-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2019 {published data only}
- Lee RM, Barrett JL, Daly JG, Mozaffarian RS, Giles CM, Cradock AL, et al. Assessing the effectiveness of training models for national scale-up of an evidence-based nutrition and physical activity intervention: a group randomized trial. BMC Public Health 2019;19:1587. [CLINICAL TRIALS: NCT04009304] [DOI: 10.1186/s12889-019-7902-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
Riiser 2020 {published data only}
- Riiser K, Richardsen KR, Haugen AL, Lund S, Løndal K. Active play in ASP – a matched-pair cluster-randomized trial investigating the effectiveness of an intervention in after-school programs for supporting children's physical activity. BMC Public Health 2020;20:500. [CLINICAL TRIALS: NCT02954614,] [DOI: 10.1186/s12889-020-08645-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Weaver 2015 {published data only}
- Weaver RG, Beet MW, Hutto B, Saunders RP, Moore JB, Turner-McGreivy G, et al. Making healthy eating and physical activity policy practice: process evaluation of a group randomized controlled intervention in afterschool programs. Health Education Research 2015;30(6):849-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Beets 2014 {published data only}
- Beets MW, Weaver GR, Turner-McGrievy G, Huberty J, Ward DS, Freedman DA, et al. Making healthy eating and physical activity policy practice: the design and overview of a group randomized controlled trial in afterschool programs. Contemporary Clinical Trials 2014;38:291-303. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beets 2016a {published data only}
- Beets MW, Turner-McGrievy B, Weaver RG, Huberty J, Moore JB, Ward DS, et al. Intervention leads to improvements in the nutrient profile of snacks served in afterschool programs: a group randomized controlled trial. Translational Behavioural Medicine 2016;6(3):329-38. [DOI: 10.1007/s13142-015-0342-z.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beets 2016b {published data only}
- Beets MW, Weaver RG, Turner-McGrievy G, Huberty J, Ward DS, Pate RR. Physical activity outcomes in afterschool programs: a group randomized controlled trial. Preventive medicine 2016;90:207-15. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beets 2018 {published data only}
- Beets MW, Brazendale K, Weaver RG, Turner-McGrievy GM, Huberty J, Moore JB, et al. Economic evaluation of a group randomized controlled trial on healthy eating and physical activity in afterschool programs. Preventive Medicine 2018;106:60-5. [DOI: 10.1016/j.ypmed.2017.10.003] [DOI] [PMC free article] [PubMed] [Google Scholar]
Connor 1986 {published data only}
- Connor MK, Smith LG, Fryer A, Erikson S, Fryer S, Drake J. Future fit: a cardiovascular health education and fitness project in an after-school setting. Journal of School Health 1986;56:329-33. [DOI] [PubMed] [Google Scholar]
Dzewaltowski 2010b {published data only}
- Dzewaltowski DA, Rosenkranz RR, Geller KS, Coleman KJ, Welk GJ, Hastmann TJ, et al. HOP'N after-school project: an obesity prevention randomized controlled trial. International Journal of Behavioural Nutrition and Physical Activity 2010;7:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gutin 2008 {published data only}
- Gutin B, Yin Z, Johnson M, Barbeau P. Preliminary findings of the effect of a 3-year after-school physical activity intervention on fitness and body fat: the Medical College of Georgia Fitkid Project. International Journal of Pediatric Obesity 2008;3(Suppl 1):3-9. [DOI: 10.1080/17477160801896457] [DOI] [PubMed] [Google Scholar]
Iversen 2011 {published data only}
- Iversen CS, Nigg C, Titchenal CA. The impact of an elementary after-school nutrition and physical activity program on children's fruit and vegetable intake, physical activity, and body mass index: Fun 5. Hawaii Medical Journal 2011;70(17 Suppl):37-41. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Jago 2014 {published data only}
- Jago R, Sebire SJ, Davies B, Wood L, Edwards MJ, Banfield K, et al. Randomised feasibility trial of a teaching assistant led extracurricular physical activity intervention for 9 to 11 year olds: Action 3:30. International Journal of Behavioral Nutrition and Physical Activity 2014;11(1):114. [DOI: 10.1186/s12966-014-0114-z.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jago 2019 {published data only}
- Jago R, Tibbitts B, Sanderson E, Bird EL, Porter A, Metcalfe C, et al. Action 3:30R: results of a cluster randomised feasibility study of a revised teaching assistant-led extracurricular physical activity intervention for 8 to 10 year olds. International Journal of Environmental Research & Public Health 2019;16(1):6. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kelder 2005 {published data only}
- Kelder S, Hoelscher DM, Barroso CS, Walker JL, Cribb P, Hu S. The CATCH Kids Club: a pilot after-school study for improving elementary students' nutrition and physical activity. Public Health Nutrition 2005;8(2):133-40. [DOI: 10.1079/PHN2004678] [DOI] [PubMed] [Google Scholar]
Kenney 2014 {published data only}
- Kenney EL, Giles CM, deBlois ME, Gortmaker SL, Chinfatt S, Cradock AL. Improving nutrition and physical activity policies in afterschool programs: results from a group-randomized controlled trial. Preventive Medicine 2014;66:159-66. [DOI: 10.1016/j.ypmed.2014.06.011] [DOI] [PMC free article] [PubMed] [Google Scholar]
Madsen 2013 {published data only}
- Madsen K, Thompson H, Adkins A, Crawford Y. School-community partnerships: a cluster-randomized trial of an after-school soccer program. JAMA Pediatrics 2013;167(4):321-6. [DOI: 10.1001/jamapediatrics.2013.1071] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT04213014 {unpublished data only}
- NCT04213014. Guys/Girls Opt for Activities for Life Trial (GOAL) to increase young adolescents' physical activity and healthy eating (GOAL). clinicaltrials.gov/ct2/show/NCT04213014 (first received 30 December 2019). [NCT: 04213014]
Nigg 2004 {published and unpublished data}
- Nigg C, Battista J, Chang JA, Yamashita M, Chung R. Physical activity outcomes of a pilot intervention using SPARK active recreation in elementary after-school programs. Journal of Sport & Exercise Psychology 2004;26:S144-5. [Google Scholar]
Salcedo Aguilar 2010 {published data only}
- Salcedo Aguilar F, Martinez-Vizcaino V, Sanchez Lopez M, Solera Martinez M, Franquelo Gutierrez R, Serrano Martinez S, et al. Impact of an after-school physical activity program on obesity in children. Journal of Pediatrics 2010;157(1):36-42. [DOI: 10.1016/j.jpeds.2009.12.046] [DOI] [PubMed] [Google Scholar]
Sharpe 2011 {published data only}
- Sharpe EK, Forrester S, Mandigo J. Engaging community providers to create more active after-school environments: results from the Ontario CATCH kids club implementation project. Journal of Physical Activity and Health 2011;8(Suppl 1):S26-31. [PMID: ] [DOI] [PubMed] [Google Scholar]
Tibbitts 2019 {published data only}
- Tibbitts B, Porter A, Sebire SJ, Bird EL, Sanderson E, Metcalfe C, et al. Action 3: 30R: process evaluation of a cluster randomised feasibility study of a revised teaching assistant-led extracurricular physical activity intervention for 8 to 10 year olds. BMC Pediatrics 2019;19(1):1111. [DOI: 10.1186/s12889-019-7347-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Weaver 2016 {published data only}
- Weaver RG, Moore JB, Huberty J, Freedman D, Turner-McGrievy B, Beighle A, et al. Process evaluation of making HEPA policy practice: a group randomized trial. Health Promotion Practice 2016;17(5):631-47. [DOI: 10.1177/1524839916647331] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiecha 2012 {published data only}
- Wiecha JL, Hall G, Gannett E, Roth B. Development of healthy eating and physical activity quality standards for out-of-school time programs. Childhood Obesity 2012;8(6):572-6. [DOI: 10.1089/chi.2012.0030] [DOI] [PubMed] [Google Scholar]
Yin 2005 {published data only}
- Yin Z, Moore JB, Johnson MH, Barbeau P, Cavnar M, Thornburg J, et al. The Medical College of Georgia Fitkid project: the relations between program attendance and changes in outcomes in year 1. International Journal of Obesity 2005;29(Suppl 2):S40-5. [DOI: ] [DOI] [PubMed] [Google Scholar]
Yin 2012 {published data only}
- Yin Z, Moore JB, Johnson MH, Vernon MM, Gutin B. The impact of a 3-year after-school obesity prevention program in elementary school children. Childhood Obesity 2012;8(1):60-70. [DOI: 10.1089/chi.2011.0085] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
ABS 2017
- Australian Bureau of Statistics. Childhood education and care Australia. Canberra (ACT): Australian Bureau of Statistics; 2017 June. Report No.:44020DO001_201706.
Afterschool Alliance 2014
- Afterschool Alliance. America after 3pm: afterschool programs in demand. Washington (DC): Afterschool Alliance; 2014.
Atkin 2011
- Atkin AJ, Gorely T, Biddle SJ, Cavill N, Foster C. Interventions to promote physical activity in young people conducted in the hours immediately after school: a systematic review. International Journal of Behavioural Medicine 2011;18(3):176-87. [DOI] [PubMed] [Google Scholar]
Aubert 2018
- Aubert S, Barnes JD, Abdeta C, Abi Nader P, Adeniyi AF, Aguilar-Farias N, et al. Global matrix 3.0 physical activity report card grades for children and youth: results and analysis from 49 countries. Journal of Physical Activity and Health 2018;15(Suppl 2):251-73. [DOI] [PubMed] [Google Scholar]
Baranowski 2003
- Baranowski T, Baranowski JC, Cullen KW, Thompson DI, Nicklas T, Zakeri IF, et al. The fun, food, and fitness project (FFFP): the Baylor GEMS pilot study. Ethnicity and Disease 2003;13(Suppl 1):1-30. [PubMed] [Google Scholar]
Barbeau 2007
- Barbeau P, Johnson MH, Howe CA, Allison J, Davis CL, Gutin B, et al. Ten months of exercise improved general and visceral adiposity, bone and fitness in black girls. Obesity 2007;15(8):2077-85. [DOI] [PubMed] [Google Scholar]
Bassett 2015
- Bassett DR, John D, Conger SA, Fitzhugh EC, Coe DP. Trends in physical activity and sedentary behaviours of United States youth. Journal of Physical Activity and Health 2015;12(8):1102-11. [DOI: 10.1123/jpah.2014-0050] [DOI] [PubMed] [Google Scholar]
Beets 2009
- Beets MW, Beighle A, Erwin HE, Huberty JL. After-school program impact on physical activity and fitness: a meta-analysis. American Journal of Preventive Medicine 2009;36(6):527-37. [DOI] [PubMed] [Google Scholar]
Beets 2018
- Beets MW, Weaver GR, Brazendale K, Turner-McGrievy G, Saunders RP, Moore JB, et al. Statewide dissemination and implementation of physical activity standards in afterschool programs: two-year results. BMC Public Health 2018;18(1):819-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Booth 2015
- Booth VM, Rowlands AV, Dollman J. Physical activity temporal trends among children and adolescents. Journal of Science and Medicine in Sport 2015;18(4):418-25. [DOI] [PubMed] [Google Scholar]
Brazendale 2015
- Brazendale K, Beets MW, Weaver RG, Huberty J, Beighle AE, Pate RR. Wasting our time? Allocated versus accumulated physical activity in afterschool programs. Journal of Physical Activity and Health 2015;12(8):1061-5. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2020
- Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 2020;368:l6890. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 2015
- Cooper AR, Goodman A, Page AS, Sherar LB, Esliger DW, Sluijs EM, et al. Objectively measured physical activity and sedentary time in youth: the International Children's Accelerometry Database (ICAD). International Journal of Behavioural Nutrition and Physical Activity 2015;12(1):113. [DOI] [PMC free article] [PubMed] [Google Scholar]
Covidence 2018 [Computer program]
- Veritas Health Innovation Covidence. Version accessed January 2018. Melbourne, Australia: Veritas Health Innovation, 2018. Available at covidence.org.
D'Souza 2020
- D'Souza NJ, Kuswara K, Zheng M, Leech R, Downing KL, Lioret S, et al. A systematic review of lifestyle patterns and their association with adiposity in children aged 5–12 years. Obesity Reviews 2020;21(e13029):1-12. [DOI: ] [DOI] [PubMed] [Google Scholar]
Dalene 2018
- Dalene KE, Anderssen SA, Andersen LB, Steene‐Johannessen J, Ekelund U, Hansen BH, et al. Secular and longitudinal physical activity changes in population‐based samples of children and adolescents. Scandinavian Journal of Medicine and Science in Sports 2018;28(1):161-71. [DOI] [PubMed] [Google Scholar]
Ding 2016
- Ding D, Lawson KD, Kolbe-Akexader TL, Finkelstein EA, Katzmarzyk PT, Mechelen W, et al. The economic burden of physical inactivity: a global analysis of major non-communicable diseases. Lancet 2016;388(10051):1311-24. [DOI] [PubMed] [Google Scholar]
Dollman 2005
- Dollman J, Norton K, Norton L. Evidence for secular trends in children's physical activity behaviour. British Journal of Sports Medicine 2005;39(12):892-7. [DOI: 10.1136/bjsm.2004.016675] [DOI] [PMC free article] [PubMed] [Google Scholar]
Drenowatz 2010
- Drenowatz C, Eisenmann JC, Pfeiffer KA, Welk G, Heelan K, Gentile D, et al. Influence of socio-economic status on habitual physical activity and sedentary behaviour in 8 to 11 year old children. BMC Public Health 2010;10(1):214. [DOI: 10.1186/1471-2458-10-214] [DOI] [PMC free article] [PubMed] [Google Scholar]
EndNote [Computer program]
- EndNote X9. Boston (MA): Clarivate Analytics, 2018. Available at endnote.com.
GRADEpro GDT 2015 [Computer program]
- McMaster University (developed by Evidence Prime) GRADEpro GDT. Version accessed January 2019. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015. Available at gradepro.org.
Guyatt 2013
- Guyatt G, Oxman AD, Sultan S, Brozek J, Glasziou P, Alonso-Coello P, et al. GRADE guidelines: 11: making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. Journal of Clinical Epidemiology 2013;66(2):151-7. [DOI] [PubMed] [Google Scholar]
Harris 2009
- Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. Canadian Medical Association Journal 2009;180(7):719-26. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2020
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Available from training.cochrane.org/handbook/archive/v6.1.
Higgins 2020b
- Higgins JP, Li T, Deeks JJ. Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. 6.1 edition. Chichester (UK): John Wiley & Sons, 2020. [URL: training.cochrane.org/handbook/current/chapter-06#section-6-5] [Google Scholar]
Jones 2013
- Jones RA, Hinkley T, Okely AD, Salmon J. Tracking physical activity and sedentary behavior in childhood: a systematic review. American Journal of Preventive Medicine 2013;44(6):651-8. [DOI] [PubMed] [Google Scholar]
Mears 2016
- Mears R, Jago R. Effectiveness of after-school interventions at increasing moderate-to-vigorous physical activity levels in 5- to 18-year olds: a systematic review and meta-analysis. British Journal of Sports Medicine 2016;50(21):1315-24. [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Medicine 2009;6:7. [DOI: 10.1371/journal.pmed1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
OECD 2016
- Organisation for Economic Co-operation and Development – Social policy division. LMF 2.2: Patterns of employment and the distribution of working hours for couples with children. Paris (IDF): Organisation for Economic Co-operation and Development (OECD); OECD Database; 2016. www.oecd.org/els/family/LMF-2-2-Distribution-working-hours-couple-households.pdf (accessed 10 February 2019).
OECD 2018
- Organisation for Economic Co-operation and Development – Social Policy division. PF4.3: Out-of-school-hours care services. www.oecd.org/els/family/PF4-3-Out-of-school-hours-care.pdf (accessed 10 February 2019).
Ontario Ministry of Education 2017
- Ontario Ministry of Education. Before-and-after school programs (kindergarten to grade 6) policies and guidelines for school boards. Toronto (ON): Ontario Ministry of Education; 2017 January.
Pate 2009
- Pate RR, O'Neill JR. After-school interventions to increase physical activity among youth. British Journal of Sports Medicine 2009;43:14-8. [DOI: ] [DOI] [PubMed] [Google Scholar]
Reiner 2013
- Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity – a systematic review of longitudinal studies. BMC Public Health 2013;13(1):813. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan Web [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager Web (RevMan Web). Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2019.
Schünemann 2020
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Eakl EA, Skoetz N, Guyatt GH. Chapter 14: Completing 'Summary of findings' tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. 6.1 edition. Chichester (UK): John Wiley & Sons, 2020. [URL: https://training.cochrane.org/handbook/current/chapter-14] [Google Scholar]
Sterdt 2014
- Sterdt E, Liersch S, Walter U. Correlates of physical activity of children and adolescents: a systematic review of reviews. Health Education Journal 2014;73(1):72-89. [Google Scholar]
Sterne 2019
- Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. [DOI: 10.1136/bmj.l4898] [DOI] [PubMed] [Google Scholar]
Tammelin 2014
- Tammelin R, Yang X, Leskinen E, Kankaanpaa A, Hirvensalo M, Tammeline T, et al. Tracking of physical activity from early childhood through youth into adulthood. Medicine and Science in Sports and Exercise 2014;46:955-62. [DOI] [PubMed] [Google Scholar]
Weintraub 2008
- Weintraub DL, Tirumalai EC, Haydel KF, Fujimoto M, Fulton JE, Robinson TN. Team sports for overweight children: the Stanford Sports to Prevent Obesity Randomized Trial (SPORT). Archives of Pediatric and Adolescent Medicine 2008;162(3):232-7. [DOI] [PubMed] [Google Scholar]
WHO 2018a
- World Health Organization. Noncommunicable diseases and their risk factors, 2018. www.who.int/ncds/en/ (accessed prior to 9 September 2021).
WHO 2018b
- World Health Organization. Non communicable diseases and their risk factors – WHO launches ACTIVE: a toolkit for countries to increase physical activity and reduce non communicable disease, 2018. www.who.int/ncds/prevention/physical-activity/active-toolkit/en/ (accessed prior to 9 September 2021).
WHO 2020
- World Health Organization. Physical activity and young people: recommended levels of physical activity for children aged 5–17 years. www.who.int/teams/health-promotion/physical-activity/physical-activity-and-young-people (accessed prior to 9 September 2021).
References to other published versions of this review
Virgara 2019
- Virgara R, Maher C, Lewis LK, Phillips A, Wolfenden L, Okely A, et al. Interventions in outside‐school hours childcare settings for promoting physical activity amongst schoolchildren aged 4 to 12 years. Cochrane Database of Systematic Reviews 2019, Issue 7. Art. No: CD013380. [DOI: 10.1002/14651858.CD013380] [DOI] [PMC free article] [PubMed] [Google Scholar]


