Abstract
Objective
Oral intake after aspiration prevention surgery (APS) is influenced by postoperative pharyngeal pressure and the dynamics of the upper esophageal sphincter (UES). We examined the effects of less invasive APS combined with UES relaxation techniques (laryngeal closure with cricopharyngeal myotomy [LC-CPM] and central-part laryngectomy [CPL]) on pharyngeal pressure and UES dynamics.
Study Design
Retrospective, observational study.
Setting
Single center.
Methods
We assessed the high-resolution pharyngeal manometric parameters of patients who underwent APS from 2018 to 2020. Then, we compared the effects of bilateral cricopharyngeal myotomy (combined with LC: LC-CPM group) and total cricoidectomy (CPL group) on both pharyngeal pressure and UES dynamics pre- and postoperatively.
Results
Eighteen patients (median age, 68 years; 17 men [94%]) were enrolled. Primary diseases associated with severe aspiration were neuromuscular disorders in 13, stroke in 3, and others in 2 patients. Pharyngeal swallowing pressure did not significantly change before and after APS. UES resting pressure and UES relaxation duration were significantly reduced (P < .001) and prolonged (P < .001), respectively, after APS. Only the CPL group (8 patients: median 62 years, all men) showed an increase in the velopharyngeal closure integral after APS (P < .05). More prolonged UES relaxation duration was recognized postoperatively in the CPL group (P < .01) than in the LC-CPM group.
Conclusion
Less invasive APS minimally affects pharyngeal swallowing pressure, decreases UES resting pressure, and prolongs UES relaxation duration. CPL may be more effective for postoperative UES relaxation in patients with a short UES relaxation time.
Keywords: aspiration prevention surgery, cricopharyngeal myotomy, total cricoidectomy, high-resolution pharyngeal manometry, pharyngeal pressure, UES dynamics
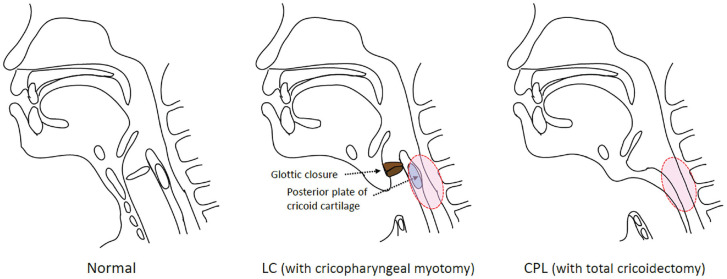
Aspiration prevention surgery (APS) is a treatment option for intractable aspiration.1-3 It has been reported that surgery can improve the quality of life of patients with severe dysphagia and help them regain oral intake.3-6 Various surgical techniques are available for aspiration prevention, such as total laryngectomy, tracheoesophageal diversion, and laryngotracheal separation. Considering the area of tissue removal and suturing, the most invasive of these techniques is total laryngectomy, and the least invasive is laryngotracheal separation. In recent years, other less invasive techniques, such as laryngeal closure (LC)4-7 and central-part laryngectomy (CPL),5,7 have become more common in Japan. In our institute, LC is performed using a glottic closure procedure, removing the anterior third of the cricoid cartilage and laryngeal cartilage under local or general anesthesia. 6 CPL was first reported in 2014. 5 In CPL, the glottis area, including the midpart of the thyroid cartilage and the entire cricoid cartilage, is removed. In both LC and CPL, the lateral part of the thyroid cartilage, the entire hypopharyngeal mucosa, and epiglottis are preserved.
Although APS can completely prevent aspiration into the airway, oral food intake after APS is not guaranteed in patients with preoperative swallowing dysfunction, including velopharyngeal insufficiency, diminished pharyngeal swallowing pressure, and upper esophageal sphincter (UES) dysfunction. It was suggested that surgical techniques facilitating bolus passage through the UES should be performed simultaneously with APS for patients with severe dysphagia who have diminished UES opening (relaxation during swallowing) or the potential for its development, as APS alone is considered insufficient to improve UES passage. 7 These techniques include bilateral cricopharyngeal myotomy (CPM), which induces relaxation of the cricopharyngeal muscles during swallowing, and total cricoidectomy, which improves physical passage obstruction by the cricoid cartilage and relaxes the cricopharyngeal muscle during swallowing. In our institution, we perform less invasive APS (L-APS) simultaneously with techniques to facilitate UES relaxation, that is, less invasive APS with a UES relaxation effect including LC (glottic closure, subglottic closure) with CPM (LC-CPM) and CPL as a technique involving total cricoidectomy ( Figure 1 ).
Figure 1.
Schemas of less invasive aspiration prevention surgery. CPL, central-part laryngectomy; LC, laryngeal closure.
Increased velopharyngeal pressure and total swallow durations and decreased UES pressure were reported for swallowing pressure after total laryngectomy for laryngeal cancer using high-resolution manometry. 8 However, to the best of our knowledge, the characteristics of swallowing pressure after L-APS have not been reported. To predict oral intake after L-APS, it is necessary to determine the impact of surgery on swallowing function. In this study, we evaluated the effects of L-APS on postoperative pharyngeal pressure and the dynamics of the UES using high-resolution pharyngeal manometry (HRPM). In addition, we investigated the status of oral intake before and after surgery.
Methods
Patients and Ethics
We included patients who underwent L-APS and swallowing-function evaluation with HRPM at the University of Tokyo Hospital between 2018 and 2020. Patients with a history of severe dementia, who could not hold liquid in their mouth, who had undergone laryngectomy, and who were not able to sit in a wheelchair or stand upright were excluded. This study was approved by the Human Ethics Committee of the University of Tokyo (No. 2487). Written informed consent was obtained from every patient, and patient anonymity was preserved.
Methodology
We conducted a retrospective, single-center study using medical charts from the hospital database and a videofluoroscopic swallow study recording database of our institute. Clinical and demographic profiles, including age, sex, and primary diseases, were reviewed. HRPM parameters of patients who underwent L-APS were evaluated pre- and postoperatively, and preoperative HRPM parameters were compared with those of previously reported healthy participants. 9 Then, pre- and postoperative HRPM parameters were compared. Subsequently, the patients were divided into 2 groups (LC-CPM and CPL groups), and the effects of LC-CPM and CPL on both pharyngeal pressure and UES dynamics were compared pre- and postoperatively. To investigate the status of oral intake, the Functional Oral Intake Scale (FOIS) 10 was adopted. FOIS scores were assigned as levels 1-7 (normal level: 7). FOIS scores of the patients were evaluated preoperatively and at 3 months postoperatively. The Glasgow Coma Scale (GCS) 11 was assessed at the time of the postoperative FOIS evaluation.
High-Resolution Pharyngeal Manometric Study and Measures
HRPM was performed in the upright sitting position. The high-resolution manometry catheter (Unisensor) was lubricated with 2% viscous lidocaine, inserted transnasally, and positioned to record from the oropharynx to the upper esophagus. The protocol consisted of a 5-minute baseline recording, followed by 3 dry swallows and 3 wet swallows of a 3-mL thickened contrast agent (iohexol, Omnipaque; Daiichi-Sankyo). A solid-state high-resolution manometer (Starlet; Star Medical) was used for data acquisition. The manometric catheter has an outer diameter of 4 mm and 20 circumferential pressure sensors spaced 1 cm apart. Pharyngeal and proximal esophageal measures were obtained from all patients according to a previously reported method. 12
The following parameters were obtained from the manometric output: maximum swallowing pressure (velopharynx, meso-hypopharynx), integrals (velopharyngeal closure integral, meso-hypopharynx contractile integral), UES resting pressure, UES relaxation duration, and UES relaxation pressure (nadir).
Statistical Analysis
Paired-group comparisons were performed with the Wilcoxon signed-rank test, and independent-group comparisons were performed with the Mann-Whitney U test implemented in BellCurve for Excel (version 3.20; Social Survey Research Information Co.). Data are presented as medians with interquartile ranges (IQRs) or numbers with percentages as appropriate. P < .05 was considered statistically significant.
Results
Demographic Data
Table 1 lists the demographic data of the enrolled patients. Eighteen patients were included in this study. The median age at the time of surgery was 68 years (IQR, 61-75 years), with a male predominance (94.4%). Primary diseases associated with severe aspiration were neuromuscular disorders in 13 patients, stroke in 3 patients, and others in 2 patients. Except for 1 patient, these patients were different from those receiving total laryngectomy for laryngeal cancer. The patients in the LC-CPM group (10 patients; median age, 73 years) were older than those in the CPL group (8 patients; median age, 62 years).
Table 1.
Patient Demographics.
| Demographics | All | LC-CPM | CPL |
|---|---|---|---|
| No. of patients | 18 | 10 | 8 |
| Age, median [IQR], y | 68 [61-75] | 73 [66-77] | 62 [59-68] |
| Male, No. (%) | 17 (94.4) | 9 (90) | 8 (100) |
| Primary diseases, No. | |||
| Multiple system atrophy | 4 | 2 | 2 |
| Stroke | 3 | 2 | 1 |
| Amyotrophic lateral sclerosis | 3 | 0 | 3 |
| Parkinson’s disease | 2 | 2 | 0 |
| Progressive supranuclear palsy | 1 | 1 | 0 |
| Neuromyelitis optica | 1 | 0 | 1 |
| Myopathy | 1 | 1 | 0 |
| Alexander disease type II | 1 | 1 | 0 |
| Traumatic brain injury | 1 | 0 | 1 |
| Postradiotherapy for laryngeal cancer | 1 | 1 | 0 |
Abbreviations: CPL, central-part laryngectomy; LC-CPM, laryngeal closure with cricopharyngeal myotomy; IQR, interquartile range.
Postoperative Change in Pharyngeal Swallowing Pressure and Integrals after Aspiration Prevention Surgery
Table 2 shows the pre- and postoperative HRPM parameters. Comparing preoperative HRPM metrics with normal HRPM data, 9 maximum meso-hypopharyngeal pressure and UES relaxation duration of the patients in this study showed a tendency to be lower than those of healthy individuals. The pharyngeal swallowing pressure did not significantly change before and after L-APS. UES resting pressure and UES relaxation duration were significantly reduced (P < .001) and prolonged (P < .001), respectively, after L-APS.
Table 2.
Comparison of HRPM Values Before and After Aspiration Prevention Surgery.
| Characteristic | Preoperatively | Postoperatively | P value |
|---|---|---|---|
| Maximum velopharyngeal pressure (mm Hg), median [IQR] | 181.5 [126.6 to 232.2] | 177.6 [138.9 to 213.4] | .31 |
| Velopharyngeal closure integral (mm Hg/s/cm), median [IQR] | 63.6 [33.4 to 105.5] | 92.8 [41.0 to 130.0] | .25 |
| Maximum meso-hypopharyngeal pressure (mm Hg), median [IQR] | 246.4 [198.9 to 273.6] | 209.1 [182.9 to 282.1] | .47 |
| Meso-hypopharyngeal contractile integral (mm Hg/s/cm), median [IQR] | 313.5 [190.6 to 394.8] | 299.4 [217.9 to 366.3] | .74 |
| UES resting pressure (mm Hg), median [IQR] | 59.9 [36.4 to 93.2] | 16.6 [5.98 to 26.1] | .0004 a |
| UES relaxation duration (s), median [IQR] | 250.0 [93.8 to 525.0] | 525.0 [300.0 to 612.5] | .0006 a |
| UES relaxation pressure-nadir (mm Hg), median [IQR] | 9.2 [–10.5 to 53.1] | –2.8 [–6.4 to 5.3] | .18 |
Abbreviations: IQR, interquartile range; UES, upper esophageal sphincter.
P < .001.
Postoperative Change in the Status of Oral Intake After Aspiration Prevention Surgery
Table 3 shows the pre- and postoperative FOIS scores and the GCS scores at 3 months postoperatively. In all patients, postoperative FOIS scores were higher than preoperative FOIS scores, and the oral intake status improved to varying degrees after APS. Moreover, the lower the patient’s overall GCS was, the worse the postoperative oral intake tended to be. Postoperatively, oral nutrition only (FOIS >3) was achieved in 3 (30%) of the 10 patients in the LC-CPM group and in 5 (63%) of the 8 patients in the CPL group.
Table 3.
FOIS Scores Before and After Aspiration Prevention Surgery and the Level of Consciousness 3 Months After Surgery.
| FOIS, No. | ||||
|---|---|---|---|---|
| Type of surgery | GCS | Primary disease | Preoperative | Post 3M |
| LC-CPM | E4VtM6 | Multiple system atrophy | 2 | 6 |
| E4VtM5 | Multiple system atrophy | 1 | 3 | |
| E4VtM6 | Myopathy | 1 | 3 | |
| E4VtM6 | Postradiotherapy for laryngeal cancer | 4 | 6 | |
| E2VtM4 | Progressive supranuclear palsy | 1 | 2 | |
| E4VtM6 | Parkinson’s disease | 1 | 3 | |
| E4VtM5 | Stroke | 1 | 2 | |
| E4VtM6 | Stroke | 1 | 5 | |
| E4VtM6 | Parkinson’s disease | 1 | 3 | |
| E4VtM1 | Alexander disease type II | 1 | 2 | |
| CPL | E4VtM6 | Multiple system atrophy | 1 | 6 |
| E3VtM5 | Stroke | 1 | 3 | |
| E4VtM1 | Amyotrophic lateral sclerosis | 1 | 2 | |
| E3VtM1 | Traumatic brain injury | 1 | 2 | |
| E4VtM6 | Multiple system atrophy | 1 | 5 | |
| E4VtM6 | Amyotrophic lateral sclerosis | 1 | 4 | |
| E4VtM6 | Neuromyelitis optica | 2 | 6 | |
| E4VtM6 | Amyotrophic lateral sclerosis | 1 | 4 | |
Abbreviations: CPL, central-part laryngectomy; E, eye opening; FOIS, Functional Oral Intake Scale; GCS, Glasgow Coma Scale; LC-CPM, laryngeal closure with cricopharyngeal myotomy; M, motor response; Post 3M, 3 months after surgery; t, tracheostomy; V, verbal response.
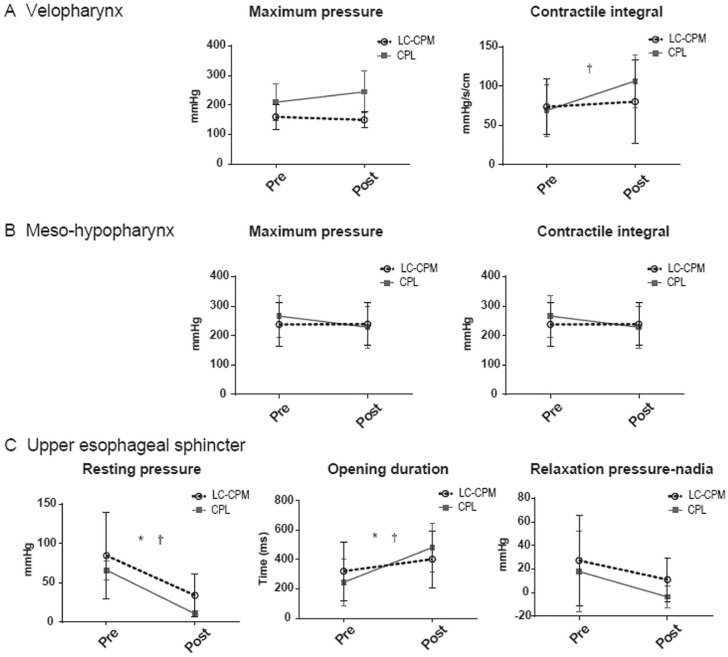
Comparison of Pre- and Postoperative HRPM Parameters in Each Surgery
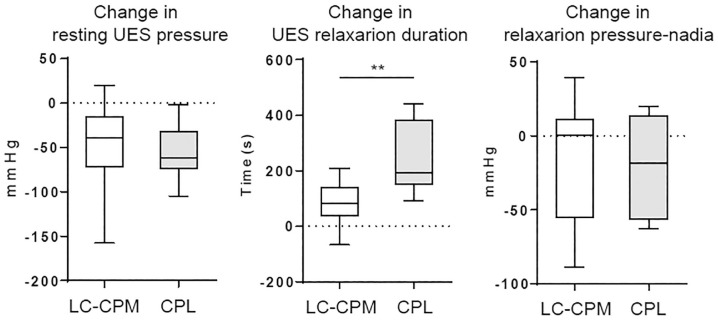
We compared the pre- and postoperative HRPM parameters in LC-CPM and CPL ( Figure 2 ; see Supplemental Table S1 in the online version of the article). In the LC-CPM group, no significant differences were recognized in velopharyngeal/meso-hypopharyngeal parameters, while the CPL group showed an increase in the velopharyngeal closure integral after surgery (P < .05). Regarding UES-related parameters, UES resting pressure and UES relaxation duration during swallowing were significantly reduced and prolonged, respectively, after surgery in both the LC-CPM and CPL groups (P < .05). Furthermore, more prolonged UES relaxation duration was recognized postoperatively in the CPL group (P < .01) than in the LC-CPM group ( Figure 3 ; see Supplemental Table 2 in the online version of the article).
Figure 2.
Changes in the high-resolution pharyngeal manometry values before and after aspiration prevention surgery. Bars show the mean with 95% confidence intervals. *P < .05 (LC-CPM group). †P < .05 (CPL group). CPL, central-part laryngectomy; LC-CPM, laryngeal closure with cricopharyngeal myotomy.
Figure 3.
Postoperative changes in high-resolution pharyngeal manometry measurements for each surgery. Bars show the mean with 95% confidence intervals. CPL, central-part laryngectomy; LC-CPM, laryngeal closure with cricopharyngeal myotomy; UES, upper esophageal sphincter. **P < .01.
Discussion
In the present study, we investigated the effects of L-APS on postoperative pharyngeal pressure and the dynamics of the UES using HRPM and arrived at the following 2 major results. First, UES resting pressure and UES relaxation duration were significantly reduced and prolonged, respectively, after L-APS, although no significant difference was observed in pharyngeal swallowing pressure before and after L-APS. Second, more prolonged UES relaxation duration was present postoperatively in the CPL group than in the LC-CPM group.
Total laryngectomy for laryngeal cancer reportedly has an effect on postoperative pharyngeal pressure and UES dynamics and induces reduced UES pressure,8,13,14 prolonged UES relaxation duration, 13 and increased velopharyngeal pressure duration. 8 Cricopharyngeal myotomy can also affect the postoperative swallowing dynamics and result in reduced UES resting pressure15,16 and improved UES relaxation duration during swallowing.17,18 Some studies have reported that no significant change in pharyngeal pressure was observed as a result of cricopharyngeal myotomy for patients with neuromuscular diseases,15,16,19 whereas other studies have reported statistically significant increases in peak pharyngeal pressure.20,21 In this study, the decreased UES pressure in the CPL and LC-CPM groups was consistent with that observed in previous reports, although the patient population was different from those usually receiving total laryngectomy for laryngeal cancer. In addition, we found an increased velopharyngeal closure integral without an increase in velopharyngeal maximum pressure in the CPL group. This could be attributed to an increase in velopharyngeal pressure duration after surgery 8 due to longer UES transit time compared with preoperative time. Regarding the finding of no remarkable change in meso- and hypopharyngeal pressure after LC-CPM and CPL, these procedures might not affect pharyngeal pressure because both lateral parts of the thyroid cartilage remained intact and the inferior pharyngeal constrictor itself was not surgically damaged.
The present study showed that either LC-CPM or CPL, as L-APS, can be effective in reducing resting UES pressure and opening the UES during swallowing. Accordingly, the functional effects of LC-CPM and CPL on UES relaxation are likely to be comparable. This is supported by the fact that the oral intake status improved postoperatively in all patients who underwent APS. Conversely, a greater effect of prolonged UES relaxation time during swallowing was observed in the CPL group than in the LC-CPM group, which may be a physical effect due to removal of the posterior plate of the cricoid cartilage. The higher rate of oral nutrition only in the CPL group compared with the LC-CPM group might be because the CPL had a greater effect on UES relaxation than the LC-CPM. For patients with high resting UES pressure and poor UES relaxation during swallowing, CPL can be more effective than LC-CPM in opening the UES. Furthermore, in patients with decreased pharyngeal pressure, which comprises the ejection force during swallowing, CPL may be more advantageous for postoperative oral intake because it is a highly effective technique for prolonging the UES relaxation time.
Notably, both UES dynamics and velopharyngeal closure function are important for regaining oral intake after APS. For patients with velopharyngeal insufficiency, improving the UES passage status during swallowing alone may not provide sufficient pharyngeal pressure, and oral feeding may not proceed smoothly. Therefore, concomitant pharyngeal valvuloplasty with APS or the use of palatal lift prosthesis should be considered in patients with velopharyngeal insufficiency.
This study has several limitations, including diverse disease backgrounds (primary diseases, level of consciousness, state of movement, etc), subjects’ age difference, and the small number of included patients. The retrospective nature of the study contributed to selection bias. In case the patient was in poor general condition, the surgeon might choose LC under local anesthesia. Future investigation is required to compare the HRPM values between LC-CPM and CPL groups with similar disease backgrounds and swallowing functions.
Conclusion
Our results indicate that L-APS minimally affects pharyngeal swallowing pressure, decreases UES resting pressure, and prolongs UES relaxation duration. CPL may be more effective for postoperative UES relaxation in patients with a short UES relaxation time.
Author Contributions
Rumi Ueha, developed the concept, designed the study, collected and analyzed the data, and wrote the draft of the manuscript; Taku Sato, designed the study, collected the data, and reviewed the manuscript; Takao Goto, designed the study, collected the data, and reviewed the manuscript; Misaki Koyama, designed the study, collected the data, and reviewed the manuscript; Akihito Yamauchi, collected the data and reviewed the manuscript; Aiko Mizukami, collected the data and reviewed the manuscript; Tatsuya Yamasoba, developed the concept and reviewed the manuscript.
Disclosures
Competing interests: None.
Sponsorships: None.
Funding source: This work was supported by the Japanese Foundation for Research and Promotion of Endoscopy.
Supplemental Material
Supplemental material, sj-docx-1-opn-10.1177_2473974X211048505 for Effects of Aspiration Prevention Surgery on the Dynamics of the Pharynx and Upper Esophageal Sphincter by Rumi Ueha, Taku Sato, Takao Goto, Misaki Koyama, Akihito Yamauchi, Aiko Mizukami and Tatsuya Yamasoba in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Footnotes
ORCID iDs: Rumi Ueha  https://orcid.org/0000-0002-0608-7237
https://orcid.org/0000-0002-0608-7237
Taku Sato  https://orcid.org/0000-0002-5871-1425
https://orcid.org/0000-0002-5871-1425
Supplemental Material: Additional supporting information is available at http://journals.sagepub.com/doi/suppl/10.1177/2473974X211048505
Availability of Data and Materials: The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1. Montgomery WW. Surgery to prevent aspiration. Arch Otolaryngol. 1975;101(11):679-682. [DOI] [PubMed] [Google Scholar]
- 2. Lindeman RC. Diverting the paralyzed larynx: a reversible procedure for intractable aspiration. Laryngoscope. 1975;85(1):157-180. [DOI] [PubMed] [Google Scholar]
- 3. Shima H, Kitagawa H, Wakisaka M, Furuta S, Hamano S, Aoba T. The usefulness of laryngotracheal separation in the treatment of severe motor and intellectual disabilities. Pediatr Surg Int. 2010;26(10):1041-1044. [DOI] [PubMed] [Google Scholar]
- 4. Sekiguchi Koyama M, Ueha R, Goto T, et al. Aspiration prevention surgery under local anesthesia for palliative care in patients with head and neck cancer: a report of two cases. ORL J Otorhinolaryngol Relat Spec. 2021;83(1):52-58. [DOI] [PubMed] [Google Scholar]
- 5. Kawamoto A, Katori Y, Honkura Y, et al. Central-part laryngectomy is a useful and less invasive surgical procedure for resolution of intractable aspiration. Eur Arch Otorhinolaryngol. 2014;271(5):1149-1155. [DOI] [PubMed] [Google Scholar]
- 6. Ueha R, Nito T, Sakamoto T, Yamauchi A, Tsunoda K, Yamasoba T. Post-operative swallowing in multiple system atrophy. Eur J Neurol. 2016;23(2):393-400. [DOI] [PubMed] [Google Scholar]
- 7. Katoh M, Ueha R, Sato T, et al. Choice of aspiration prevention surgery for patients with neuromuscular disorders: report of three cases. Front Surg. 2019;6:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lippert D, Hoffman MR, Britt CJ, et al. Preliminary evaluation of functional swallow after total laryngectomy using high-resolution manometry. Ann Otol Rhinol Laryngol. 2016;125(7):541-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Aoyagi Y, Ohashi M, Ando S, et al. Effect of tongue-hold swallow on pharyngeal contractile properties in healthy individuals [published online January 1, 2021]. Dysphagia. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86(8):1516-1520. [DOI] [PubMed] [Google Scholar]
- 11. Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;2(7872):81-84. [DOI] [PubMed] [Google Scholar]
- 12. Ueha R, Goto T, Sato T, et al. High resolution manofluorographic study in patients with multiple system atrophy: possible early detection of upper esophageal sphincter and proximal esophageal abnormality. Front Med. 2018;5:286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Choi EC, Hong WP, Kim CB, et al. Changes of esophageal motility after total laryngectomy. Otolaryngol Head Neck Surg. 2003;128(5):691-699. [DOI] [PubMed] [Google Scholar]
- 14. Dantas RO, Aguiar-Ricz LN, Oliveira EC, Mello-Filho FV, Mamede RC. Influence of esophageal motility on esophageal speech of laryngectomized patients. Dysphagia. 2002;17(2):121-125. [DOI] [PubMed] [Google Scholar]
- 15. Takasaki K, Umeki H, Enatsu K, Kumagami H, Takahashi H. Evaluation of swallowing pressure in a patient with amyotrophic lateral sclerosis before and after cricopharyngeal myotomy using high-resolution manometry system. Auris Nasus Larynx. 2010;37(5):644-647. [DOI] [PubMed] [Google Scholar]
- 16. Poirier NC, Bonavina L, Taillefer R, Nosadini A, Peracchia A, Duranceau A. Cricopharyngeal myotomy for neurogenic oropharyngeal dysphagia. J Thorac Cardiovasc Surg. 1997;113(2):233-240. [DOI] [PubMed] [Google Scholar]
- 17. Lawson G, Remacle M, Jamart J, Keghian J. Endoscopic CO2 laser-assisted surgery for cricopharyngeal dysfunction. Eur Arch Otorhinolaryngol. 2003;260(9):475-480. [DOI] [PubMed] [Google Scholar]
- 18. Kos MP, David EF, Klinkenberg-Knol EC, Mahieu HF. Long-term results of external upper esophageal sphincter myotomy for oropharyngeal dysphagia. Dysphagia. 2010;25(3):169-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ozgursoy OB, Salassa JR. Manofluorographic and functional outcomes after endoscopic laser cricopharyngeal myotomy for cricopharyngeal bar. Otolaryngol Head Neck Surg. 2010;142(5):735-740. [DOI] [PubMed] [Google Scholar]
- 20. Arenaz Bua B, Olsson R, Westin U, Rydell R, Ekberg O. Treatment of cricopharyngeal dysfunction: a comparative pilot study. BMC Res Notes. 2015;8:301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mason RJ, Bremner CG, DeMeester TR, et al. Pharyngeal swallowing disorders: selection for and outcome after myotomy. Ann Surg. 1998;228(4):598-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-opn-10.1177_2473974X211048505 for Effects of Aspiration Prevention Surgery on the Dynamics of the Pharynx and Upper Esophageal Sphincter by Rumi Ueha, Taku Sato, Takao Goto, Misaki Koyama, Akihito Yamauchi, Aiko Mizukami and Tatsuya Yamasoba in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation