Abstract
Background:
The present study assessed how the adaptation to American culture by United States (U.S.)-born and foreign-born Hispanics living in the U.S. may influence stress-related physiological aspects that may impair health.
Methods:
Data on 8,360 Hispanics living in the U.S. categorized as U.S.-born (n=3,347) and foreign-born (n=5,013) from NHANES 1999–2010 (ages 18–85) were used. Stress-related physiological impact was measured by the allostatic load index (ALoad). Adaptation to American culture was evaluated through three acculturation-related measures.
Results:
The average age was 39.39 years in a sample where 51% were males. ALoad was classified as no load (15.41%), low load (55.33%), and high load (29.24%). The U.S.-born Hispanics showed higher ALoad compared to foreign-born Hispanics (p<0.001). Among foreign-born Hispanics, length of residence (LOR) and age of arrival in the U.S. (AOA) were associated with higher ALoad scores (p<0.05), and in U.S.-born Hispanics, age and sex were positively associated and education was negatively associated with ALoad scores (p<0.05).
Discussion:
Adaptation to American culture in foreign-born Hispanics living in the U.S. appears to influence levels of ALoad in this population.
Keywords: Stress, Acculturation, Hispanics
Introduction
In 2016, Hispanic/Latino immigrants contributed to the 44 million foreign-born members of the United States (U.S.) population [1]. After migrating to the U.S., people often adopt the health behaviors, beliefs, values, and languages of the host country, a process known as acculturation [2]. In Hispanic/Latino immigrants, the process of acculturation has been related to both positive and negative health outcomes, some of which result from changes in health-related behaviors, including dietary practices and physical activity [3]. Although the influence of acculturation on health is complex, length of residence, linguistic isolation, education, socioeconomic factors, origin, and stress have been described as risk factors for mental and physical health deterioration, morbidity, and mortality among Hispanics/Latinos [3–6].
Exposure to the aforementioned risk factors appears to contribute to both psychosocial and physiological stresses that make it challenging for individuals to maintain the normal functioning of the physiological systems through a process known as allostasis [7]. The hypothalamic–pituitary–adrenal (HPA) axis and sympathetic–adrenal–medullary systems have been identified as the basis of the allostasis process [8]. Indeed, many past studies have consistently found that individuals with higher stress have higher ALoad scores [9–11]. When the process of allostasis increases as a result of increased stress accumulation, the same physiological systems designed to preserve normal functioning become dysregulated, a phenomenon commonly referred to as allostatic load (ALoad) [10]. Such dysregulation is quantified by the allostatic load index, which estimates ALoad using a composite of biomarkers representing neuroendocrine, cardiovascular, metabolic, and immune system functions [8]. The multisystem ALoad index has been used in many studies assessing related health outcomes; however, there is lack of congruency about the specific markers that define the ALoad measures. For example, some studies have limited the measures to those that include only cardiometabolic and immunologic function [9, 12]. This research will include the cardiometabolic and inflammatory measures; ALoad is defined using the method by Doamekpor et al. [13], which has been used to examine differences in ALoad in non-Hispanic Blacks. However, it has not been used among Hispanics or to examine how acculturation impacts ALoad among Hispanics.
Past research has documented disparities in ALoad by race/ethnicity [9, 14, 15]. For example, Non-Hispanic Blacks have shown higher ALoad scores compared to non-Hispanic Whites and Hispanics, even after controlling for the potential confounders of poverty, socioeconomic factors, physical activity, and smoking status [16–18]. When the interaction of race/ethnicity and sex has been evaluated, non-Hispanic Black women appear to be especially disadvantaged and have higher ALoad scores than non-Hispanic White and Mexican-American women [19].
Given that the acculturation process has been described as a stressful experience for first- (referring to those who were foreign-born) and second-generation (referring to those who were U.S.-born from immigrant parents) immigrants, it is not surprising that there are differences in levels of stress among Hispanics by place of birth. For example, Peek et al. [18] used a sample of residents in Texas City, which has a large community of Hispanics, and found that U.S.-born Mexican Americans have been shown to have higher ALoad scores compared to Mexican-born Hispanics [18]. The reasons for such disparity, and whether the stress differences extend to a national sample of Hispanics, are not clearly understood. The purpose of the present study was to examine, first, the differences in ALoad by place of birth (U.S.-born vs. foreign-born). The second aim was to examine the relationship between ALoad and acculturation-related measures (language use [LU], length of residence [LOR], and age of arrival [AOA]) in foreign-born Hispanics controlling for age, sex, education, income, and marital status. This study attempts to fill in the gap in the knowledge of adaptation to American culture, stress, and differences among Hispanics in the U.S.
Methodology
Data
Data from six waves of the public data of the National Health and Nutrition Examination Survey (NHANES) collected from 1999 to 2010 were included for this study (n=8,360). NHANES Institutional Review Board (IRB) approval and documented consent were obtained from the participants. This study was exempt from Institutional Review Board (IRB) review. This exemption complied with the policy of the University of Alabama at Birmingham IRB related to the use of publically available data for research and publication.
For this research, the analyses included those participants who self-identified as Mexican American or Hispanic. Most research on immigrant health compares Hispanics to non-Hispanic Whites and non-Hispanic Blacks without exploring the heterogeneity that exists among Hispanics. The six NHANES waves were pooled and adjusted for person weights, four-year sample weights from NHANES 1999–2002 (WTMEC4YR) and two-year sample weights from NHANES 2003–2010 (WTMEC2YR), to create 12-year subset weights, as is recommended by NCHS. Excluded were participants who were pregnant and those younger than 18 years old. Included were questions from the demographics, examination, laboratory, and questionnaire data of NHANES. The classification of place of birth among Hispanics (U.S.-born and foreign-born) was evaluated with the question: “In what country were you born?” Those born in Alaska, Hawaii, or the continental U.S. were classified as U.S.-born, and those born in Mexico or elsewhere were classified as foreign-born.
Measures
Allostatic load
The use of ALoad as a measure of chronic stress and its association with health outcomes has been highly described in the literature [8–10]. ALoad represents the cumulative, multisystem physiological dysregulation resulting from repeated activation and deactivation of allostasis in response to stress throughout the lifespan. Although there are no universally accepted biomarkers that quantify ALoad, it has been suggested that ALoad candidate variables among adults should include biomarkers from three systems (cardiovascular, metabolic, and immune/inflammatory) [10, 11, 20]. For the purpose of this study, the ALoad biomarkers were the same as those used by Doamekpor et al. [13].
The ALoad index included eight biomarkers. The cardiovascular biomarkers were systolic blood pressure, diastolic blood pressure, total cholesterol, 60-second pulse, and HDL cholesterol; the metabolic biomarkers were creatinine clearance and serum albumin; and the inflammatory biomarker was C-reactive protein. The sample-based cutoff values were set in the top quartile for systolic blood pressure, diastolic blood pressure, total cholesterol, 60-second pulse, and creatinine clearance and in the lower quartile for HDL cholesterol and albumin. For each biomarker, a dichotomous variable was created in which “1” reflected values in the high-risk and “0” reflected values in the lowest-risk range. A total ALoad score (0–8) reflects the number of these eight singular indicators for which each participant scored in the upper or lower quartile of risk; higher scores indicated higher ALoad. Further, high allostatic load was evaluated in three groups by a number of high-risk indicators: 1) 0 biomarkers, which is referred to as “no load,” 2) 1–2 biomarkers, referred to as “low load,” and 3) ≥3 biomarkers, referred to as “high load.” The cutoff point of “high load” with a total score of three or above was based on previous evidence, which suggests that a score of at least three is associated with higher morbidity and mortality [13, 17].
Acculturation-related measurements
A number of scales and models have been developed to understand the complex process of acculturation [3]. Each has inherent strengths and limitations, and it is therefore common to find in the scientific literature the use of multiple instruments to assess acculturation. Further, individual characteristics, such as age of migration, generational status, place of birth, and length of residence, have been used as a proxy for the process of acculturation and to evaluate associations with health outcomes [3]. For the purpose of this research, we included three measures to evaluate acculturation [21]: 1) language use (LU), 2) length of residence (LOR), and 3) age of arrival in the U.S. (AOA). Language use was assessed with the question “What language is usually spoken at home?” included in the acculturation questionnaire. The answers include: 1) Only Spanish, 2) More Spanish than English, 3) Both equally, 4) More English than Spanish, or 5) Only English. Those who answered “Speak both equally,” “More English than Spanish,” and “Only English” were considered to be more acculturated. The LOR was evaluated with the question “Length of time has been in the U.S.?” included in the demographic section. For the purpose of this research, LOR were collapsed into five categories (<1 year, 1–5 years, 6–10 years, 11–15 years, >15 years) due to previous research suggesting that after 10–15 years of LOR in the U.S., the risk of some health outcomes increases [22, 23]. AOA was calculated using the LOR and age at interview and was categorized into four groups (<6 years, 6–18 years, 18–24 years, and >25 years of age). The classification of AOA was based on studies that suggest that generations of immigrants who arrive at an early age are exposed to different socialization during childhood, which leads to lifelong changes in preferences, beliefs, and modifications of their native culture compared to those who arrive during adulthood [6, 24, 25].
Acculturation and exposure to different social environments and experiences have been associated with different biological systems activity, and neuroendocrine responses according to sex [3, 26, 27]. The effects of social environment on biological parameters seem to be sensitive by sex due to diverse aspects such as social status, stability, and quality of social relations within the environment [26]. Regarding social experiences and differences in ALoad by sex appears to be associated with parental bonding, adult bonding, relationship histories, social ties, and social support [27]. Therefore, for this manuscript, acculturation measures were also explored by sex.
Covariates
Consistent with previous research, marital status, income, sex, education, and age were included as factors that could influence health outcomes [13, 18]. Annual income was collapsed into three categories (<$25,000, $25,000–$54,999, and $≥55,000). Marital status was classified in six categories (married, widowed, divorced, separated, never married, and living with a partner).
Statistical analysis
Descriptive statistics (mean, standard deviation, and frequencies) were calculated to summarize age, sex, education, marital status, annual income, and acculturation-related measures (LU, LOR, and AOA) by place of birth (U.S.-born vs. foreign-born). Independent-sample t-tests and chi-squared tests were performed to detect differences in sociodemographic characteristics and acculturation measures by place of birth.
Differences among ALoad groups were analyzed using analysis of variance (ANOVA) and chi-squared tests. The Rao-Scott x2 p-values were reported in the results as recommended by NHANES. The cut-off points used to calculate ALoad scores and to group Hispanics by a number of high-risk indicators were systolic blood pressure, 127.14 mmHg; diastolic blood pressure, 75.84 mmHg; total cholesterol, 218.02 mg/dL; 60-second pulse, 78.96; C-reactive protein, 0.46 mg/dL; HDL cholesterol, 39.51 mg/dL; creatinine clearance, 172.62 mg/dL; and serum albumin, 4.05 mg/dL. We tested separate multiple regression models for U.S.-born and foreign-born Hispanics to compare factors associated with ALoad scores and by each ALoad biomarker. For all models, the dependent variable was ALoad, and acculturation measures (LU, LOR, and AOA) were added to the model when only foreign-born Hispanics were considered. As covariates, sex, age, education, marital status, and income were included. The analyses included two statistical models: 1) the U.S.-born Hispanics model included the covariates only, and 2) the foreign-born Hispanics model included the covariates and the acculturation-related measures (LU, LOR, and AOA).
To avoid the multicollinearity of age with AOA, in the foreign-born Hispanics model, only the AOA variable was included. The VIF values were calculated for both models. In both statistical models, sex, education, marital status, and origin were included in the class statement. The LU was considered as an ordinal variable 1 (Only Spanish) to 5 (Only English), in which more English use is associated with higher acculturation. All residuals were tested for normality, and significance level was considered α=0.05 for all statistical analyses. All analyses were performed with SAS statistical software (version 9.4, 2002–2012 by SAS Institute Inc., Cary, NC).
Results
Demographic characteristics are summarized in Table 1 of the total sample and by Hispanic place of birth. From the total sample, 40.03% (n=3,347) of Hispanics were born in the U.S., and 59.96% (n=5,013) were foreign-born (born in Mexico or elsewhere). The average age was 39.39 years, and a total of 51.28% were males. Significant differences were observed for age, sex, education, marital status, and income by place of birth. Foreign-born Hispanics were older, more were married, and more had less education and lower income compared to U.S.-born (p<0.0001).
Table 1.
Descriptive characteristics of Hispanics by place of birth, NHANES (1999-2010)
| Variable | All Hispanics Weighted (n=8,360) |
Hispanics US–Born Weighted (n=3,347) |
Hispanics Foreign–Born Weighted (n=5,013) |
p |
|---|---|---|---|---|
| Percentage (n) | ||||
| Sex | <0.0001 | |||
| Male | 51.28 (n=4,145) | 17.22 (n=1,528) | 34.05 (n=2,617) | |
| Female | 48.71 (n=4,215) | 20.51 (n=1,819) | 28.20 (n=2,396) | |
| Education | ||||
| 18-19 years of age | <0.0001 | |||
| 9th grade | 40.99 (n=213) | 19.50 (n=87) | 21.49 (n=126) | |
| 10th–12th grade | 25.60 (n=374) | 16.41 (n=241) | 9.19 (n=133) | |
| High school graduate | 17.34 (n=266) | 10.88 (n=175) | 6.46 (n=91) | |
| GED or equivalent | 1.98 (n=22) | 1.69 (n=17) | 0.29 (n=5) | |
| More than high school | 14.06 (n=174) | 11.92 (n=139) | 2.13 (n=35) | |
| 20+ years of age | ||||
| Less than 9th grade | 26.33 (n=2,666) | 2.83 (n=455) | 23.50 (n=2,211) | |
| 9th–11th grade (Includes 12th grade with no diploma) | 20.83 (n=1,449) | 6.83 (n=541) | 13.99 (n=908) | |
| High school graduate/GED or equivalent | 20.25 (n=1,302) | 9.59 (n=653) | 10.66 (n=649) | |
| Some college or AA degree | 22.52 (n=1,354) | 12.44 (n=789) | 10.07 (n=565) | |
| College graduate or above | 10.05 (n=580) | 4.72 (n=302) | 5.32 (n=278) | |
| Marital Status | <0.0001 | |||
| Married | 52.49 (n=4,205) | 16.09 (n=1,426) | 36.39 (n=2,779) | |
| Widowed | 3.62 (n=532) | 1.31 (n=208) | 2.30 (n=324) | |
| Divorced | 7.01 (n=545) | 3.75 (n=292) | 3.25 (n=253) | |
| Separated | 4.76 (n=341) | 1.41 (n=79) | 3.35 (n=262) | |
| Never married | 23.43 (n=1,822) | 11.17 (n=918) | 12.25 (n=904) | |
| Living with partner | 8.66 (n=583) | 3.38 (n=221) | 5.27 (n=362) | |
| Annual income | <0.0001 | |||
| <$25,000 | 39.42 (n=2,878) | 14.32 (n=1,058) | 25.10 (n=1,820) | |
| $25,000–$54,999 | 40.05 (n=2,652) | 13.52 (n=1,005) | 26.52 (n=1,647) | |
| $≥55,000 | 20.51 (n=1,235) | 9.75 (n=665) | 10.75 (n=570) | |
| Acculturation-related measurements | ||||
| Language spoken at home | <0.0001 | |||
| Only Spanish | 41.80 (n=3,632) | 2.10 (n=243) | 39.70 (n=3,389) | |
| More Spanish than English | 12.20 (n=1,039) | 2.46 (n=271) | 9.73 (n=768) | |
| Both equally | 15.16 (n=1,230) | 8.26 (n=767) | 6.90 (n=463) | |
| More English than Spanish | 12.90 (n=1,036) | 9.28 (n=806) | 3.62 (n=230) | |
| Only English | 17.91 (n=1,365) | 15.41 (n=1,222) | 2.49 (n=143) | |
| Length of residence | ||||
| < 1 year | NA | NA | 5.05 (n=204) | |
| 1–5 years | NA | NA | 14.41 (n=662) | ` |
| 6–10 years | NA | NA | 18.16 (n=776) | |
| 11–15 years | NA | NA | 14.25 (n=574) | |
| >15 years | NA | NA | 48.10 (n=2,577) | |
| Age of arrival | ||||
| <6 years of age | NA | NA | 3.97 (n=155) | |
| 6–18 years of age | NA | NA | 19.42 (n=935) | |
| 18–24 years of age | NA | NA | 31.15 (n=1,287) | |
| >25 years of age | NA | NA | 45.44 (n=2,401) | |
| Mean (95% CI) | ||||
| Age | 39.39 (38.75-40.04) | 37.92 (36.99-38.85) | 40.28 (39.31-41.26) | <0.0001 |
| Allostatic Load | 2.00 (1.94-2.06) | 2.03 (1.95-2.11) | 1.98 (1.91-2.06) | <0.0001 |
NA, not applicable. Significant differences were denoted at p <0.05. The cut-off points used to calculate ALoad scores, and to group the Hispanics by a number of high-risk indicators were systolic blood pressure, 127.14 mmHg; diastolic blood pressure, 75.84 mmHg; total cholesterol, 218.02 mg/dL; 60-second pulse, 78.96; C-reactive protein, 0.46 mg/dL; HDL cholesterol, 39.51 mg/dL; creatinine clearance, 172.62 mg/dL; serum albumin, 4.05 mg/dL.
Allostatic load by place of birth and by load group
Regarding the first research aim, which was to examine differences in ALoad by place of birth, we found significant differences among Hispanics (Table 1). Overall, the mean ALoad was significantly higher among U.S.-born Hispanics as compared to their foreign-born counterparts (p<0.0001), a trend that extended to both sexes. The ALoad mean in U.S.-born Hispanic females was higher than the ALoad mean in foreign-born Hispanic females (1.94 CI 1.84–2.05 and 1.83 CI 1.74–1.92, respectively). In males, the ALoad also showed differences. Among U.S.-born Hispanics, the ALoad showed a higher mean compared to foreign-born Hispanic males (2.14 CI 2.06–2.22, and 2.11 CI 2.03–2.20, respectively). Regarding ALoad by group (Table 2), from the total sample, 15.41% of Hispanics showed no load, 55.33% showed low load, and 29.24% showed high load. There were significant differences in sex (p<0.0001) and place of birth (p=0.0017) by ALoad group. Among Hispanics classified in the high-load group (≥3 high-risk biomarkers), 55.86% were male, and 59.91% were foreign-born. There were no differences among ALoad groups by Hispanic identity for foreign-born Hispanics who were born in Mexico or elsewhere.
Table 2.
Characteristics of Hispanics based on allostatic load (ALoad) group and biomarkers, NHANES (1999-2010)
| Variables | All Hispanics Weighted (n=8,360) |
No load Weighted (n=1,289) |
Low load Weighted (n=4,626) |
High load Weighted (n=2,445) |
p |
|---|---|---|---|---|---|
| Percentage (n) | |||||
| Sex | <0.0001 | ||||
| Male | 51.27 (n=4,144) | 7.02 (n=569) | 27.61 (n=2,209) | 16.63 (n=1,366) | |
| Female | 48.72 (n=4,216) | 9.06 (n=720) | 27.71 (n= 2,417) | 11.40 (n=1,079) | |
| Place of birth | 0.0017 | ||||
| US-born Hispanics | 37.74 (n=3,347) | 5.42 (n=460) | 21.89 (n=1,907) | 10.42 (n=980) | |
| Foreign-born Hispanics | 62.25 (n=5,013) | 11.20 (n=830) | 33.43 (n=2,718) | 17.62 (n=1,465) | |
| Hispanic identity (country of origin) | 0.1410 | ||||
| Mexican American | 59.93 (n=6,452) | 10.49 (n=1,034) | 33.00 (n=3,559) | 16.42 (n=1,859) | |
| Other Hispanics | 40.06 (n=1,909) | 6.12 (n=256) | 22.32 (n=1,067) | 11.61 (n=586) | |
| Mean (95% CI) | |||||
| ALoad score | 2.00 (1.94-2.06) | NA | 1.68 (1.66-1.71) | 3.76 (3.70-3.82) | NA |
| Biomarkers (cut-off points used to calculate allostatic load scores) | |||||
| Systolic blood pressure (127.14 mmHg) | 121.00 (120.08-121.92) | 110.31 (109.65-110.97) | 118.08 (117.18-118.97) | 131.69 (130.22-133.15) | <0.0001 |
| Diastolic blood pressure (75.84 mmHg) | 70.17 (69.75-70.59) | 63.53 (62.94-64.11) | 67.75 (67.23-68.28) | 77.91 (77.38-78.44) | <0.0001 |
| Pulse (78.96 pulse) | 72.37 (71.97-72.77) | 67.29 (66.75-67.83) | 71.22 (70.63-71.81) | 77.34 (76.42-78.26) | <0.0001 |
| Total cholesterol (218.02 mg/dL) | 196.66 (195.33-198.00) | 176.01 (174.31-177.70) | 194.41 (192.71-196.11) | 215.35 (212.55-218.15) | <0.0001 |
| HDL cholesterol (39.51 mg/dL) | 49.12 (48.65-49.58) | 54.61 (53.81-55.41) | 49.79 (49.27-50.32) | 43.99 (43.12-44.86) | <0.0001 |
| Creatinine clearance (172.62 mg/dL) | 134.28 (131.47-137.10) | 95.49 (92.35-98.62) | 136.67 (132.59-140.75) | 152.89 (148.11-157.66) | <0.0001 |
| Serum albumin (4.05 g/dL) | 4.33 (4.31-4.35) | 4.44 (4.42-4.45) | 4.33 (4.32-4.35) | 4.25 (4.22-4.28) | <0.0001 |
| C-reactive protein (0.46 mg/dL) | 0.41 (0.38-0.44) | 0.22 (0.20-025) | 0.40 (0.35-0.44) | 0.56 (0.516-0.622) | <0.0001 |
NA, not applicable. Significant differences were denoted at p<0.05. Allostatic load group: no load= not high-risk biomarkers, low load = 1–2 high-risk biomarkers, and high load= ≥3 high-risk biomarkers.
Acculturation-related measures and allostatic load in U.S.-born Hispanics and foreign-born Hispanics
Evaluating the second aim, which was to examine the relationship between ALoad and acculturation-related measures, we found that acculturation influenced the ALoad scores among Hispanics. The ALoad variance yielded a main effect for the LOR [F(4,792)=151.84, p<0.001], such that the average ALoad was significantly lower for those with LOR <1 year (males 1.72±0.098, and females 1.49±0.242). ALoad increased significantly among those with 10 years of LOR and greater (p=0.001) (Figure 1). In addition, ALoad scores showed differences based on AOA; higher scores were seen in the group who arrived between six and 18 years of age and >25 years of age (Figure 2).
Figure 1. ALoad mean by length of residence group and sex in foreign-born Hispanics, NHANES (1999-2010).
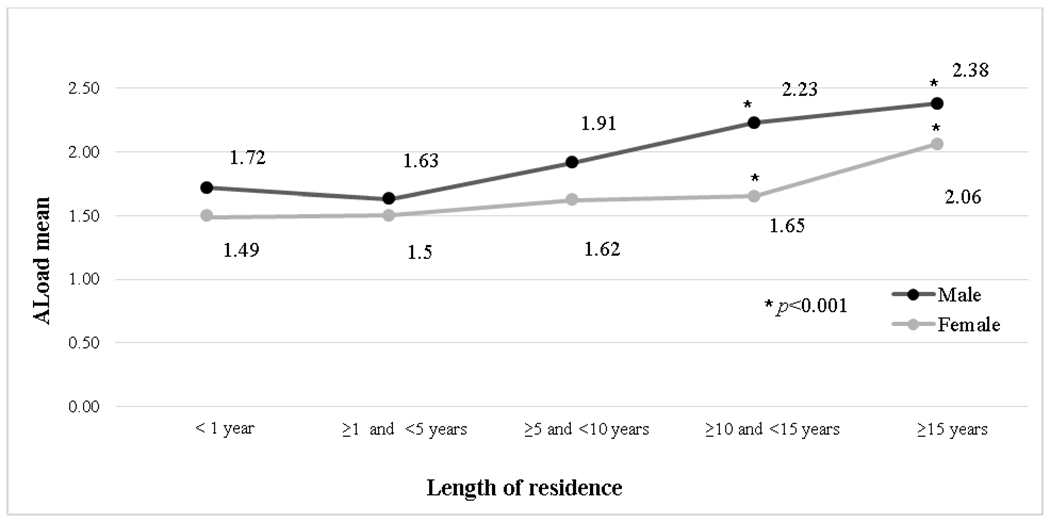
ALoad, allostatic load. One-way ANOVA test was performed to assess mean differences in ALoad by length of residence in the U.S. Significant differences among groups were denoted at p<0.05.
Figure 2. ALoad mean by age of arrival and sex in foreign-born Hispanics, NHANES (1999-2010).
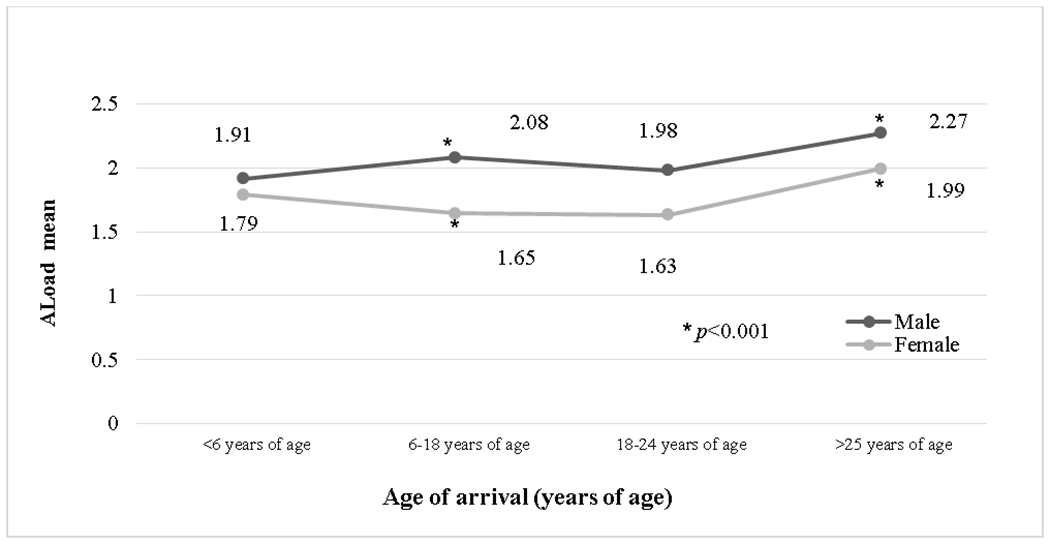
ALoad, allostatic load. One-way ANOVA test was performed to assess mean differences in ALoad by age of arrival in the U.S. Significant differences among groups were denoted at p<0.05.
Results for the multiple regression models assessing the contribution of variables on ALoad scores controlled by age, sex, education, income, and marital status are shown in Table 3. The multiple regression analysis yielded statistically significant models [Model 1: F(5,90)=13.13; p<0.0001; R2=0.03861 and Model 2: F(7,89)=48.54; p<0.0001; R2=0.08826]. In foreign-born Hispanics, LOR, AOA, sex, and income were associated with higher ALoad scores (p<0.0001, p<0.0001, p<0.0001, and p=0.0354, respectively). Among U.S.-born Hispanics, age, sex, and education were associated with higher ALoad scores (p<0.0001, p<0.0001, and p=0.0267 respectively). While there were significant differences in LU (spoken at home) by place of birth (Table 1), LU was not associated with ALoad levels among foreign-born Hispanics. Regarding the influence on each ALoad biomarker from LOR and AOA, we found similar results; the majority of the biomarkers were influenced by LOR and AOA, except for CRP (Table 4).
Table 3.
Multiple regression analyses exploring the relation between acculturation measures and ALoad scores, NHANES (1999-2010)
| Models | ALoad Load | |||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | |||||||
| Hispanics US–Born (n=2,550) | Hispanics Foreign–Born (n=3,749) | |||||||
| β | p | Standard error | Variance inflation | β | p | Standard error | Variance inflation | |
| Independent variables | ||||||||
| Age | 0.011431 | <0.0001 | 0.002695 | 1.35 | NA | NA | NA | NA |
| Sex | 0.147026 | <0.0001 | 0.074798 | 1.00 | 0.3882170 | <0.0001 | 0.029832 | 1.02 |
| Education | −0.034064 | 0.0267 | 0.015123 | 1.20 | −0.0025473 | 0.7851 | 0.009314 | 1.22 |
| Income | −0.001489 | 0.9131 | 0.013608 | 1.08 | −0.0234173 | 0.0354 | 0.010960 | 1.07 |
| Marital status | −0.017098 | 0.4228 | 0.131171 | 1.27 | −0.0161760 | 0.1197 | 0.065643 | 1.09 |
| Acculturation measures | ||||||||
| Length of residence | NA | NA | NA | NA | 0.1915815 | <0.0001 | 0.007715 | 1.23 |
| Age at arrival | NA | NA | NA | NA | 0.0217027 | <0.0001 | 0.001176 | 1.29 |
| Language | NA | NA | NA | NA | 0.0107280 | 0.6803 | 0.025949 | 1.37 |
NA, not applicable. Model 1: US-born Hispanics; Model 2: foreign-born Hispanics. Significant differences were denoted at p <0.05
Table 4.
Multiple regression analyses exploring the relation between allostatic load biomarkers by length of residence and year of arrival among foreign-born Hispanics, NHANES (1999-2010)
| Model | ||||||
|---|---|---|---|---|---|---|
| Length of residence | Age of arrival | |||||
| Biomarkers | β | p | Standard error | β | p | Standard error |
| Systolic blood pressure | 3.609193 | <0.0001 | 0.173968 | 0.637481 | <0.0001 | 0.031011 |
| Diastolic blood pressure | 1.245956 | <0.0001 | 0.071472 | 0.184733 | <0.0001 | 0.013102 |
| Pulse | −0.256463 | 0.0098 | 0.097160 | −0.085161 | <0.0001 | 0.008138 |
| Total cholesterol | 4.635606 | <0.0001 | 0.238444 | 0.739272 | <0.0001 | 0.051796 |
| HDL cholesterol | 0.202768 | 0.0640 | 0.010374 | 0.027727 | 0.0090 | 0.010374 |
| Creatinine clearance | −1.935945 | 0.0096 | 0.730975 | −0.917325 | <0.0001 | 0.091004 |
| Serum albumin | −0.037655 | <0.0001 | 0.003458 | −0.005466 | <0.0001 | 0.000316 |
| C-reactive protein | 0.019692 | <0.0001 | 0.003453 | 0.000555 | 0.0887 | 0.000321 |
All models were adjusted by sex, education, and income. Significant differences were denoted at p <0.05.
Discussion
This study investigated the differences in ALoad by place of birth among Hispanics and the influence of acculturation-related measures as factors that may increase stress, captured by a physiological measure of ALoad in Hispanics. Our results showed that U.S.-born Hispanics have higher ALoad scores compared to foreign-born Hispanics. In addition, our results showed that the ALoad increases in foreign-born Hispanics with increased LOR and in those who arrived at an early age. Among U.S.-born Hispanics, ALoad increased with age, decreased with higher levels of education, and tended to be higher in men.
Differences in allostatic load levels among Hispanics previously have been seen among U.S.-born Mexicans vs. foreign-born Hispanics [18]. Also, among Hispanics from different countries of birth, ALoad levels appear to be different, with South Americans showing the lowest ALoad levels and Puerto Ricans (whose immersion into American culture may be more evident, due to Puerto Rico’s political relationship with the U.S.) showing the highest mean of ALoad scores [28]. Disparities in ALoad have been associated mainly with the healthy immigrant hypothesis, in which newer immigrants are healthier on arrival, and the longer the length of residence in the U.S., the greater the likelihood of losing culture-related health-protective effects [18]. However, exposure to stressors associated with acculturation might not be the only factor that drives our associations. Some of the factors that may be associated with the increase and disparities in ALoad levels may be related to a lifetime of exposure to discrimination [29].
Our results demonstrate that almost half of the sample speak English at home, according to the classification of LU. Hispanics’ adaptation of the host country’s language represents, in part, their acculturation to the U.S. The increase in English use at home may be influenced by an increase in the Hispanic population and the LOR; about 50% of the foreign-born individuals in our sample have been in the U.S. for 15 years or more, and most arrived in the U.S. during early adulthood.
The ALoad calculation was derived using quartile distribution (75th for upper or 25th for lower) of eight biomarkers. Among these biomarkers, it is possible that some may confer high-risk status for disease outcomes that are not stress related. Concerned about the possibility that the cutoff points of the biomarkers included in the ALoad were associated with a medical condition, we performed additional analyses (n=6,631), excluding participants who self-reported a medical condition related to the ALoad biomarkers. These conditions included asthma, high blood pressure, arthritis, congestive heart failure, coronary heart disease, angina, heart attack, stroke, emphysema, goiter, thyroid, bronchitis, liver condition, cancer, and diabetes. These statistical analyses (data not shown) produced similar results and supported the described association of ALoad with age, sex, and education in U.S.-born Hispanics and LOR and AOA in foreign-born Hispanics. Even though ALoad served as a basis for measuring cumulative physical and social demands (stressors) throughout life, some calculations defining ALoad use similar biomarkers as those considered for the definition of metabolic syndrome (MetS). As previously indicated, the cutoff definition of each biomarker defining ALoad is different, resulting in two unique and independent constructs. Hence, it is not surprising that participants with high levels of ALoad in our sample were not necessarily classified as having MetS (data not shown).
While most Hispanics had at least one high-risk biomarker independent of birth origin, ALoad was significantly higher in U.S.-born Hispanics. This observation may support previously documented health advantages for immigrants in the U.S., as proposed by the healthy immigrant hypothesis.[18, 28, 30].
Biological factors, in combination with sociocultural determinants, appear to influence the stress pathways among males and females in different ways throughout the lifespan [31, 32]. In our results, differences of ALoad by sex were similar to previous research [28, 33], with men showing a higher mean ALoad independent of place of birth. Given that ALoad has been associated with a variety of environmental, social, and interpersonal stressors, it is plausible that these stressors may differentially influence the physiological responses of male and female Hispanics [12, 33, 34]. These different responses may be modulated also by poor neighborhood conditions, environmental health risks (such as residential proximity to petrochemical plants) [35] and sociocultural gender-roles that have been seen modulate the differences in ALoad by sex [31]. Regarding AOA, previous research has suggested that those who migrate when young (<24 years of age) show lower ALoad scores [28]; however, we found differences between those who arrived at <6 years of age compared to those who arrived between six and 18 years of age. The differences in load may relate to the exposure to different environmental stressors in early ages [6, 24, 25].
Some limitations in the present study deserve consideration. For example, we did not identify differences in ALoad by Hispanic country of origin because the NHANES ethnicity variable classifies Hispanics only as Mexican American or “other.” In addition, developmental trajectories of ALoad could not be examined in our study given the cross-sectional design of NHANES. Regarding ALoad, even though the biomarkers used to calculate ALoad in this study were previously evaluated, in future studies it could be beneficial to include additional biomarkers in the calculation of ALoad and compare this measurement with scales of perceived stress. Nonetheless, and despite its limitations, our study supports the belief that adaptation to American culture plays a role in ALoad scores.
Our results showed lower ALoad among foreign-born Hispanics compared to U.S.-born Hispanics, that their ALoad increases with increased LOR, and that this increase exacerbates with age at the time of migration to the U.S. As we continue to work toward improving the health of the population, the effects of stressful environments on disease and mortality risk cannot be ignored [36, 37].
Given the impact of the political migration crisis faced in today’s world, further research is needed to alleviate the detrimental consequences of acculturation stress on the health of migrant populations. The inclusion of stress in the study of the impact of the environment is intended to help enhance individuals’ adaptive behaviors and to promote well-being among the Hispanic community. In addition, the inclusion of ALoad as a measurement of stress provides multifaceted mind-body (psychopathological and pathophysiological) research to connect measures from the dynamic process of acculturation. The findings of this study could help researchers, public health practitioners, and policymakers consider the stress influence on intervention strategies during the acculturation process of immigrants and decrease the health risk associated with chronic stress exposure. Hence, considering the interactions of acculturation and ALoad is essential for developing prevention programs and intervention strategies to attenuate the burden of health risk among Hispanics and their descendants.
Study Importance.
What is already known about this subject?
There are differences in allostatic load based on race/ethnicity
Allostatic load has been associated with health outcomes
What does your study add?
Acculturation influence allostatic load among Hispanics
Comparison of allostatic load scores based on place of birth
Acknowledgments:
We thank Rebecca F Lipscomb, MA, MPPM, Manager Department Research Grants and Training, Nutrition Obesity Research Center, University of Alabama at Birmingham for her assistance with the edits in this manuscript.
References
- 1.Radford J, Budiman A. Facts on U.S. Immigrants, 2016. Statistical portrait of the foreign-born population in the United States. Pew Research Center. http://www.pewhispanic.org/2018/09/14/facts-on-u-s-immigrants/#fb-key-charts-population2018. [Google Scholar]
- 2.Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: implications for theory and research. Am Psychol. 2010;65(4):237–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goel MS, McCarthy EP, Phillips RS, Wee CC. Obesity among US immigrant subgroups by duration of residence. JAMA. 2004;292(23):2860–7. [DOI] [PubMed] [Google Scholar]
- 5.van Rompay MI, McKeown NM, Castaneda-Sceppa C, et al. Acculturation and sociocultural influences on dietary intake and health status among Puerto Rican adults in Massachusetts. J Acad Nutr Diet. 2012;112(1):64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arevalo SP, Tucker KL, Falcon LM. Life events trajectories, allostatic load, and the moderating role of age at arrival from Puerto Rico to the US mainland. Soc Sci Med. 2014;120:301–10. Epub 2014/09/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Arch Intern Med. 1993;153(18):2093–101. [PubMed] [Google Scholar]
- 8.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–9. [DOI] [PubMed] [Google Scholar]
- 9.Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev. 2010;35(1):2–16. [DOI] [PubMed] [Google Scholar]
- 10.Beckie TM. A systematic review of allostatic load, health, and health disparities. Biol Res Nurs. 2012;14(4):311–46. [DOI] [PubMed] [Google Scholar]
- 11.McEwen BS, Seeman T. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci. 1999;896:30–47. [DOI] [PubMed] [Google Scholar]
- 12.McClure HH, Josh Snodgrass J, Martinez CR Jr., et al. Stress, Place, and Allostatic Load Among Mexican Immigrant Farmworkers in Oregon. J Immigr Minor Health. 2015;17(5):1518–25. [DOI] [PubMed] [Google Scholar]
- 13.Doamekpor LA, Dinwiddie GY. Allostatic load in foreign-born and US-born blacks: evidence from the 2001–2010 National Health and Nutrition Examination Survey. Am J Public Health. 2015;105(3):591–7. Epub 2015/01/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carlson ED, Chamberlain RM. Allostatic load and health disparities: a theoretical orientation. Res Nurs Health. 2005;28(4):306–15. [DOI] [PubMed] [Google Scholar]
- 15.Graves KY, Nowakowski ACH. Childhood Socioeconomic Status and Stress in Late Adulthood: A Longitudinal Approach to Measuring Allostatic Load. Glob Pediatr Health. 2017;4:2333794X17744950. Epub 2017/12/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96(5):826–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97(7):1305–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peek MK, Cutchin MP, Salinas JJ, et al. Allostatic load among non-Hispanic Whites, non-Hispanic Blacks, and people of Mexican origin: effects of ethnicity, nativity, and acculturation. Am J Public Health. 2010;100(5):940–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chyu L, Upchurch DM. Racial and ethnic patterns of allostatic load among adult women in the United States: findings from the National Health and Nutrition Examination Survey 1999–2004. J Womens Health (Larchmt). 2011;20(4):575–83. Epub 2011/03/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duong MT, Bingham BA, Aldana PC, Chung ST, Sumner AE. Variation in the Calculation of Allostatic Load Score: 21 Examples from NHANES. J Racial Ethn Health Disparities. 2017;4(3):455–61. Epub 2016/06/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deyo RA, Diehl AK, Hazuda H, Stern MP. A simple language-based acculturation scale for Mexican Americans: validation and application to health care research. Am J Public Health. 1985;75(1):51–5. Epub 1985/01/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Himmelgreen DA, Perez-Escamilla R, Martinez D, et al. The longer you stay, the bigger you get: length of time and language use in the U.S. are associated with obesity in Puerto Rican women. Am J Phys Anthropol. 2004;125(1):90–6. [DOI] [PubMed] [Google Scholar]
- 23.Commodore-Mensah Y, Ukonu N, Obisesan O, et al. Length of Residence in the United States is Associated With a Higher Prevalence of Cardiometabolic Risk Factors in Immigrants: A Contemporary Analysis of the National Health Interview Survey. J Am Heart Assoc. 2016;5(11). Epub 2016/11/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baker EH, Rendall MS, Weden MM. Epidemiological Paradox or Immigrant Vulnerability? Obesity Among Young Children of Immigrants. Demography. 2015;52(4):1295–320. Epub 2015/06/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rumbaut RG. Assimilation and its discontents: between rhetoric and reality. Int Migr Rev. 1997;31(4):923–60. Epub 1997/01/01. [PubMed] [Google Scholar]
- 26.Seeman TE, McEwen BS. Impact of social environment characteristics on neuroendocrine regulation. Psychosom Med. 1996;58(5):459–71. Epub 1996/09/01. [DOI] [PubMed] [Google Scholar]
- 27.Seeman TE, Singer BH, Ryff CD, Dienberg Love G, Levy-Storms L. Social relationships, gender, and allostatic load across two age cohorts. Psychosom Med. 2002;64(3):395–406. Epub 2002/05/22. [DOI] [PubMed] [Google Scholar]
- 28.Salazar CR, Strizich G, Seeman TE, et al. Nativity differences in allostatic load by age, sex, and Hispanic background from the Hispanic Community Health Study/Study of Latinos. SSM Popul Health. 2016;2:416–24. Epub 2016/08/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cuevas AG, Wang K, Williams DR, et al. The Association Between Perceived Discrimination and Allostatic Load in the Boston Puerto Rican Health Study. Psychosom Med. 2019;81(7):659–67. Epub 2019/05/31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Argeseanu Cunningham S, Ruben JD, Narayan KM. Health of foreign-born people in the United States: a review. Health Place. 2008;14(4):623–35. Epub 2008/02/05. [DOI] [PubMed] [Google Scholar]
- 31.Juster RP, Lupien S. A sex- and gender-based analysis of allostatic load and physical complaints. Gend Med. 2012;9(6):511–23. Epub 2012/11/20. [DOI] [PubMed] [Google Scholar]
- 32.Phillips SP. Measuring the health effects of gender. J Epidemiol Community Health. 2008;62(4):368–71. Epub 2008/03/15. [DOI] [PubMed] [Google Scholar]
- 33.Arbona C, Olvera N, Rodriguez N, et al. Acculturative Stress Among Documented and Undocumented Latino Immigrants in the United States. Hisp J Behav Sci. 2010;32(3):362–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Latinos Caplan S., acculturation, and acculturative stress: a dimensional concept analysis. Policy Polit Nurs Pract. 2007;8(2):93–106. [DOI] [PubMed] [Google Scholar]
- 35.Mair CA, Cutchin MP, Kristen Peek M. Allostatic load in an environmental riskscape: the role of stressors and gender. Health Place. 2011;17(4):978–87. Epub 2011/05/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Borrell LN, Dallo FJ, Nguyen N. Racial/ethnic disparities in all-cause mortality in U.S. adults: the effect of allostatic load. Public Health Rep. 2010;125(6):810–6. Epub 2010/12/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Robertson T, Beveridge G, Bromley C. Allostatic load as a predictor of all-cause and cause-specific mortality in the general population: Evidence from the Scottish Health Survey. PLoS One. 2017;12(8):e0183297. Epub 2017/08/17. [DOI] [PMC free article] [PubMed] [Google Scholar]


