Abstract
As the COVID-19 pandemic has ravaged the United States, healthcare teams are on the frontlines of this global crisis, often navigating harrowing conditions at work, such as a lack of personal protective equipment and staffing shortages, and distractions at home, including worries about elderly relatives or making childcare arrangements. While the nature and severity of stressors impacting healthcare teams are in many ways unprecedented, decades of psychological research exploring teamwork in extreme contexts can provide insights to understand and improve outcomes for teams in a crisis. This review highlights the psychological principles that apply to teams in a crisis and illustrates how psychologists can use this knowledge to improve teamwork for medical teams in the midst of the COVID-19 pandemic., The review also provides a glimpse toward the future, noting both how psychologists can help healthcare teams recover and rebound, as well as how additional research can improve psychologists’ understanding of teamwork in times of crisis.
Keywords: teamwork, team stress, healthcare, COVID-19
As the COVID-19 pandemic has strained healthcare systems around the world, medical teams have faced unprecedented working conditions. Teams of physicians, nurses, respiratory therapists, and pharmacists have experienced shortages not only in personal protective equipment, but also in staff, as those on the frontlines have fallen ill while the numbers of cases have risen (Gan et al., 2020). In the midst of a medical crisis, understanding how teams can improve patient outcomes with scarce resources is paramount. Psychologists have amassed a large body of research over several decades that captures and characterizes the types of stressors work teams face in a crisis, the effects of these stressors on team processes and performance, and the behavioral interventions that can be implemented to mitigate stress and help teams recover (Driskell et al., 2018; Razinskas & Hoegl, 2020). Moreover, extensive research on teams in healthcare contexts demonstrates the importance of improving teamwork for patient and provider outcomes (Ervin et al., 2018; Fiscella & McDaniel, 2018; Rosen et al., 2018).
Accordingly, this review serves three purposes. First, it illustrates the psychological dynamics that can influence team effectiveness in times of crisis, with a focus on healthcare teams in the COVID-19 pandemic. Second, it demonstrates how psychologists can use this information to enable frontline medical teams to maintain their effectiveness. Finally, it highlights future implications, outlining how these findings can apply to future crises and offering a research agenda to address new questions brought to light by the pandemic.
To achieve these aims, the manuscript is organized into four sections. The first section focuses on team stressors, illustrating sources of stress that are either unique to or heightened under current conditions. This section also provides a brief review of existing empirical work and frameworks (e.g., Razinkas & Hoegl, 2020), highlighting the impact these stressors can have on team functioning. Second, the paper focuses on the aspects of teamwork that are most likely to be negatively impacted by the stressors relevant to healthcare teams, clarifying key constructs such as psychological safety, collective efficacy, and shared mental models (Edmondson, 1999; Stajkovic et al., 2009; DeChurch & Mesmer-Magnus, 2010). Third, it provides recommendations for countermeasures—actions that can be employed quickly and at little or no cost, aimed at buffering the effects of stress on team performance and outcomes for patients and providers.
The final section focuses on the aftermath of the pandemic, both for healthcare teams and for the psychologists who study them, by discussing how teams can recover and learn from the current crisis to prepare for the next challenge and suggesting avenues for research that can improve how teams respond to stressful events in the future. Although the scale of COVID-19 is perhaps unprecedented, the lessons learned can be carried forward as medical teams are strained by future natural disasters or epidemics. Recommendations are targeted at recovery, learning, and preparation in the months and years after the worst of this pandemic has waned.
In sum, the contribution here is to provide psychologists from a wide range of disciplines with the know-how to understand how findings about stress and teamwork can be used to manage and improve teamwork for healthcare teams in the midst of the COVID-19 pandemic. By translating team science to practice, illustrating concepts in the current context, and providing applicable recommendations, the manuscript catalyzes some of the potential the research has to improve the lives of those working on the front lines during a crisis.
Stressors Impacting Teams
For decades, researchers have studied team stress across a number of contexts. Although much of the early research in this domain was conducted in military teams (Cannon-Bowers & Salas, 1998), a growing body of work has investigated or extended findings to other high-stakes environments including aviation, oil refineries, and healthcare (e.g., Drach-Zahavy & Freund, 2007; Schippers et al., 2015). The stressors experienced by healthcare teams facing the COVID-19 pandemic are unprecedented in many ways: documented cases of the disease are in the millions, hospitalization and mortality rates are higher than seen during a typical influenza season, and resources to protect workers are scarce (CDC, 2020a; WHO, 2020). Although the specific nature and extent of these stressors are unprecedented, psychologists studying teams in extreme environments have provided a number of relevant insights (Driskell et al., 2018).
In their multilevel review of team stressor research, Razinskas and Hoegl (2020) illustrate several potential sources of stress on teams. Of these sources, the most relevant in the current context are stressors intrinsic to a job (e.g., workload, time pressure), stressors due to roles in the organization (e.g., team unfamiliarity, role ambiguity), and stressors at the work-home interface (e.g., work-family conflict), and these sources can be conceptualized as impacting teams from multiple hierarchical levels (i.e., individual, team, organizational). All types and levels of stressors are salient for healthcare teams in the COVID-19 context.
For healthcare teams at the frontlines of the pandemic, staffing issues are one prominent stressor intrinsic to workers’ jobs, generating increased workload and time pressure. Though many hospitals were facing staffing issues prior to the pandemic, an increased number of patients and absences due to healthcare workers falling ill have increased the stress-related demands impacting teams (Gohar et al., 2020). Staffing issues impact teams from multiple levels—increased absences at the organizational level create a ripple-down effect as managers and leaders work to shift staffing at the team level. Teams that are short-staffed or tasked with increased caseloads are likely to experience higher workload and time pressure, and working longer hours may impact team members at the individual level.
Relatedly, shifts in staffing may generate stressors due to increased role ambiguity or team unfamiliarity, both of which can undermine team performance (Rodríguez-Escudero et al., 2010). Although role ambiguity is often conceptualized as team-level source of stress (Razinkas & Hoegl, 2020), team members who are assigned to a new unit or expected to communicate with patients’ family members outside of hospital may experience stress at the individual level as they attempt to identify and adapt to their new roles. Sources of situational ambiguity, like the uncertainty surrounding COVID-19 symptoms and treatment, may also contribute to role ambiguity as teams struggle to determine who is best equipped to treat the patient.
Finally, teams may be impacted by stressors at the work-home interface. Team members may experience increased home demands (ten Brummelhaus & Bakker, 2012) stemming from feelings of concern about the health and well-being of family and friends or needing to find childcare while they are at work, or they may experience social isolation as they avoid transmitting the virus to their families. While much of the research regarding stressors at the work-home interface has focused on the individual level (ten Brummelhuis & Bakker, 2012), initial research indicates that a team’s additive work-life conflict can impact team member interactions by, for example, reducing helping behavior (ten Brummelhuis et al., 2012).
The Impact of Stressors on Teamwork
Team scientists typically conceptualize the role that stressors and other contextual variables play on team functioning through an IMOI (input-mediator-output-input) model of teamwork. The IMOI model describes how team inputs (i.e., conditions for teamwork, context, and composition) influence a set of mediators (i.e., team processes and emergent states), which in turn generate team outcomes (i.e., performance and affective outcomes) and create the conditions under which teams engage in subsequent performance episodes (Ilgen et al., 2005).
The IMOI model of teamwork is helpful in conceptualizing stressors as an input but does not explicate how they work. Stress theories, such as job demands-resources and conservation of resources theories, help illustrate how stressors intrinsic to a job, related to roles in an organization, and at the work-home interface influence team processes and emergent states, providing insights about how behavioral countermeasures can buffer the effects of stressors on teamwork. Broadly, job demands-resources (JD-R) theory guides the structure of the theoretical model. Although originally conceptualized at the individual level, in teams, JD-R theory demonstrates how job demands require teams to exert sustained effort over time whereas job resources can buffer teams from the deleterious effects of demands on outcomes (Bakker & Demerouti, 2007; Ellis & Pearsall, 2011). For example, cross-training can buffer teams from the negative impact of job demands on team processes and emergent states (Ellis & Pearsall, 2011).
While JD-R theory illustrates the impact of job demands on teams, in the current context, healthcare teams are also experiencing increased demands at the work-home interface. The impact of these and other non-work stressors on teams can be understood via conservation of resources theory. Conservation of resources theory explains how stress, originating from the actual or potential loss of one’s physical or psychological resources, influences individuals’ well-being and stress (Hobfoll, 1989). Importantly, when individuals experience heightened levels of stress, the risk of a downward spiral increases, wherein continuous resource loss occurs and individuals are less effective in managing demands (ten Brummelhuis et al., 2011). In teams, threatened resources on the home front—stemming from work-life conflict—impact team task completion, as team members experiencing stress perform sub-optimally or impede others from doing their jobs, and impact teamwork as individuals have less time and energy to attend to their relationships with other team members (ten Brummelhuis et al., 2012). In a positive cycle, resources at the team level (i.e., social support; ten Brummelhuis et al., 2012) can also buffer teams from members’ experiences of stress from the work-home interface.
Figure 1 depicts the IMOI model of teamwork, incorporating salient stressors. Work and home demands shape a team’s existing resources and can adversely affect team processes and emergent states. The countermeasures teams implement in the midst of the pandemic buffer the impact of team demands on processes and emergent states, and those implemented in the pandemic’s aftermath help teams rebuild resources, strengthening inputs for the next crisis. Notably, this review focuses on the IMOI model in the context of teamwork processes and emergent states, rather than on team taskwork (i.e., actions and interactions involving the accomplishment of team tasks; Marks et al., 2001), given the highly variable taskwork demands on healthcare teams. The recommendations provided here are intended to apply broadly to healthcare teams impacted by COVID-19, regardless of taskwork demands. Research in healthcare contexts broadly supports the importance of team processes and emergent states in improving patient outcomes (Manser, 2009), as well as the importance of interventions in maintaining and improving processes, emergent states, and performance (Weller et al., 2014).
Figure 1.
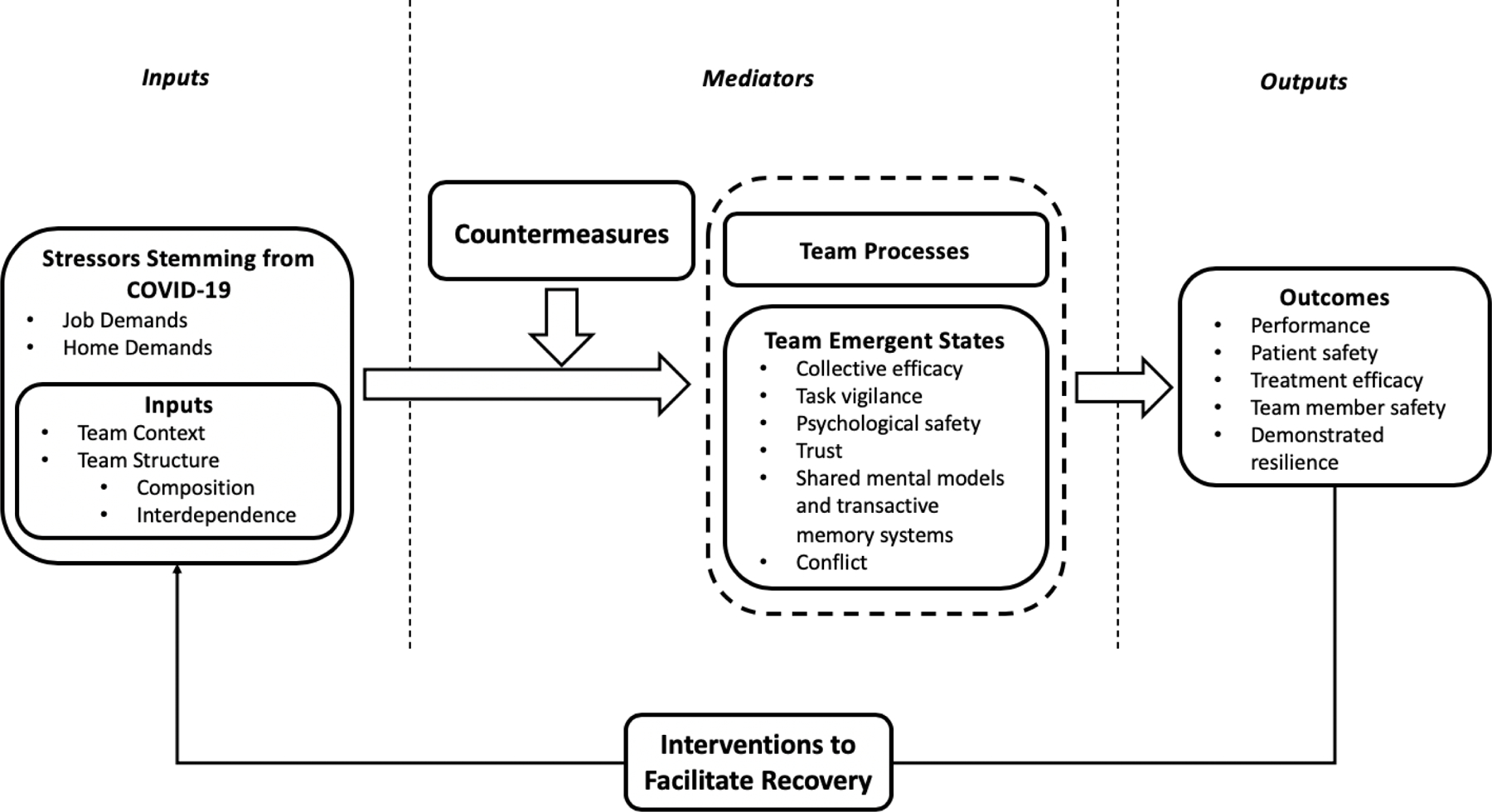
IMOI Model of Teamwork in the Context of COVID-19
Team Inputs
For frontline teams in healthcare and beyond, COVID-19 has generated new stressors that directly alter team inputs, including context and structure.
Context.
The organizational context in which a team is performing can be thought of in terms of discrete phenomena characterizing the team’s environment (Johns, 2006). For frontline medical teams, it is useful to think of how pandemic-related stressors have influenced the team’s task and physical context. In this case, teams are working with much higher levels of uncertainty than in their typical day and are doing so with far fewer resources (Lazzerini & Putoto, 2020). Heightened uncertainty may impact how teams communicate or make decisions—it may be unclear who on the team has expertise in a given area, and new research about the presentation of the coronavirus and best courses of treatment may create additional uncertainty. Teams also face uncertainty about the days, weeks, and months ahead—both within and outside of work—which may make it more difficult to maintain optimism that the team can keep going successfully.
Structure.
The stressors facing frontline teams also impact team structure (i.e., composition and interdependence). Whereas team composition describes the specific configuration of individuals’ characteristics on a team, interdependence broadly describes how and to what extent team members rely on each other for resources, interaction, and desired outcomes (Mathieu et al., 2014). Staffing issues may impact team composition by increasing the frequency with which team composition changes, and/or by altering the characteristics of teammates. While some teams working in the context of the COVID-19 pandemic may maintain stable membership, but experience increased stress, others may have rotating membership, requiring teams to re-establish norms and build trust frequently. While healthcare teams’ shared experiences working together can improve the can improve the synchronization of behavior, having numerous shared experiences can also lead to complacency (Luciano et al., 2018). However, teams with rotating membership may have more difficulty maintaining processes and emergent states due to increased unfamiliarity and role ambiguity.
Changes in the composition of a team in terms of expertise, professional roles, and demographics can also impact team functioning. For example, working with a team where expertise is scattered or members are not clear who they can count on can undermine early trust (Webber, 2008). In contrast, increased diversity on the basis of academic rank and demographic characteristics may improve team outcomes. For example, science team composition with regard to academic rank and funding sources can impact production of breakthrough publications, and mixed-gender teams’ publications tend to yield more citations (Hall et al., 2018). In medicine, where compositional research has focused primarily on professional roles, multidisciplinary and interprofessional diversity can improve teamwork and patient outcomes (Rosen et al., 2018).
In healthcare, team task interdependence tends to be high (Rosen et al., 2018), and the collaboration across specialties and professional backgrounds required to care for COVID-19 patients in hospitals and clinics may exacerbate team interdependence. In general, team interdependence tends to strengthen the importance of team processes and emergent states on performance (LePine et al., 2008; DeChurch & Mesmer-Magnus, 2010). Accordingly, managing the impact of stressors on team processes and emergent states is especially pertinent for highly interdependent healthcare teams.
Team Mediators
The impact of stressors and changes to team conditions on team processes and emergent states are well-documented. The following emergent states represent those most likely to be impacted by the increased stress facing COVID-19 teams.
Collective efficacy.
Stressors including role ambiguity and workload can impact a team’s collective efficacy, or a shared sense that a team can accomplish its goals (Jex & Gudanowski, 1992; Stajkovic et al., 2009; Taggar & Seijts, 2003). Prior successes can help frontline teams build and sustain collective efficacy, but medical teams without a reliable treatment for their patients may feel like they are experiencing one failure after another, and this sequence of events can have the opposite effect (Watson et al., 2001). Moreover, when teams are composed of many members who lack experience treating COVID, it can be difficult for members to believe their team will be successful in treating patients.
Task vigilance.
A team’s ability to maintain vigilance, or sustained focus over a long period of time, is a key component of the teamwork behaviors necessary to improve patient outcomes in healthcare settings (Mazzocco et al., 2009). While the urgency of fighting a pandemic may boost vigilance at first, increased home demands and sustained high workload can distract or drain teams, making it difficult for team members to maintain high levels of vigilance (Smallwood & Schooler, 2006). Moreover, increased workload and time pressure can cause teams to narrow their focus, losing sight of the “bigger picture” and focusing on the self instead of the team (Driskell et al., 1999). In the current context, managing home demands ranging from childcare issues to concern about an elderly parent contracting the disease, combined with increased workload stemming from a rapidly rising number of COVID-19 positive patients can make it difficult for teams to sustain focus, especially on a broader picture of their team’s goals.
Psychological safety.
In addition to struggling to maintain focus, team members may feel lower levels of psychological safety than they would under normal conditions. Psychological safety describes the shared sense that a team is safe for interpersonal risk taking (Edmondson, 1999). On teams with high psychological safety, members speak up when they see a problem and are not afraid to ask questions if they are uncertain about how to proceed with a task. As a result, teams learn from their mistakes and improve outcomes for patients (Carmeli & Gittell, 2009). In healthcare contexts, psychological safety is already somewhat difficult to develop due to inherent power gradients (Nembhard & Edmondson, 2006). When staff members are working on new units and experiencing heightened role ambiguity, it is especially important that team members feel they can ask questions or provide critical feedback, as psychological safety helps prevent medical errors and improves the team’s ability to develop creative workarounds for problems (Kessel et al., 2012; Nembhard & Edmondson, 2006).
Team trust.
A team’s sense of trust is related to, but distinct from psychological safety. Team trust is captured by both affective and cognitive components—the affective component of trust, centered on interpersonal care and concern, precedes a sense of psychological safety (Edmondson, 1999). In contrast, cognitive trust centers on beliefs about peer reliability, dependability, and competence (McAllister, 1995). Lack of familiarity with team members and role ambiguity are likely to impede trust initially, leading to increased difficulty developing cognitive and affective trust down the road (Webber, 2008). For healthcare teams, role stressors can differentially impact affective and cognitive trust. Though unfamiliarity may impede affect-based trust, members’ lack of expertise is more likely to impede cognitive-based trust.
Shared mental models and transactive memory systems.
Teams working with new members may also struggle to form and maintain shared mental models or transactive memory systems, two forms of team cognition that help teams process information. Shared mental models describe a team’s shared understanding of their situation, roles, and responsibilities, and help teams interpret information upon receipt, whereas transactive memory systems help teams distribute and retrieve knowledge by understanding which team member possesses certain knowledge and expertise (DeChurch et al., 2010). Acute stress can weaken shared mental models and transactive memory systems (Ellis, 2006). Medical teams on the frontlines may be asked to quickly adapt to changing circumstances, working on new units or with new colleagues, leading to difficulty developing shared mental models.
Team conflict.
Finally, the stressors impacting COVID-19 teams may generate additional team conflict. There are three common types of team conflict—task, interpersonal, and process conflict (Jehn, 1997). In the current context, process conflict, which concerns disagreements about task delegation and role assignment, is particularly pertinent. Role conflict stemming from team unfamiliarity can get personal, leading team members to feel frustrated and less open to cooperation. Teams may also experience increased task conflict surrounding new tasks and processes that have emerged in response to the pandemic, as well as increased interpersonal conflict given the levels of home-related stressors.
Team processes.
Team processes describe a team’s interdependent behaviors directed toward achieving a goal and are distinct from emergent states in they are behavior-based, rather than affect- or cognition-based (Marks et al., 2001). Though this review focuses primarily on team emergent states, team processes including action (e.g., coordination), transition (e.g., strategy formulation), and interpersonal (e.g., conflict management) processes as well as leadership, planning, and conflict management are integral to healthcare team performance (Manser, 2009; Rosen et al., 2018). Team processes are depicted alongside emergent states in the theoretical model, as they are also negatively impacted by stressors (e.g., communication, Urban et al., 1996), and positively impact performance (LePine et al., 2008). Moreover, as discussed in the following section on countermeasures, teams that effectively bolster behavioral processes should be better able to buffer the negative effects of stressors.
Team Outcomes
Numerous studies have linked the aforementioned emergent states to a wide range of team outcomes. First and foremost, effective engagement in team processes and maintenance of emergent states elicits better team performance. Indeed, there is robust evidence to support the link between collective efficacy (Stajkovic et al., 2009), task vigilance (Hollenbeck et al., 1995), psychological safety (Frazier et al., 2017), team trust (De Jong et al., 2016), shared mental models and transactive memory systems (DeChurch & Mesmer-Magnus, 2010), and team behavioral processes (LePine et al., 2008) with team performance.
The aforementioned emergent states and behavioral processes have also been linked to outcomes specific to healthcare, including patient safety and treatment efficacy (Baker et al., 2003). For example, surgical team task vigilance can improve patient outcomes (Mazzocco et al., 2009), whereas increased conflict may worsen these outcomes (Rogers et al., 2011). Psychological safety, commonly studied in medical teams, has been shown to increase team quality improvement behavior and error reporting (Applebaum et al., 2016; Nembhard & Edmondson, 2006). Emergent states may also improve outcomes for healthcare team members. For example, teams characterized by psychological safety, trust, collective efficacy, and accurate shared mental models are more likely to adhere to the safety protocols that enable members to maintain their personal health in crisis (Salas et al., 2019).
Finally, effectively managing stressors to buffer their effects on team processes and emergent states demonstrates a component of team resilience (Alliger et al., 2015). Demonstrating resilience can help teams to recover and maintain psychological resources, preparing teams to manage future setbacks and additional stressors after a long shift or in the weeks and months after the peak of COVID cases wanes.
Countermeasures to Mitigate the Effects of Stress
Although the circumstances under which frontline COVID teams are performing are intense, decades of psychological research on team development interventions (Lacerenza et al., 2018) can inform how the effects of stress can be mitigated. The deleterious effects of stress highlighted above are not inevitable. While a full arsenal of team development interventions might include more formalized approaches, this paper focuses on efforts that can be implemented quickly and at a low cost. This section focuses on countermeasures aimed at team functioning in the day-to-day, whereas the following section takes a broadened perspective, focusing on interventions that can help teams in the aftermath of crisis. A summary of countermeasures with relevant emergent states and stressors is provided in Table 1.
Table 1.
Summary of stressors, emergent states, and countermeasures impacting COVID-19 response teams
| Countermeasure | Associated Psychological Construct(s) | Associated Stressor(s) |
|---|---|---|
| Preparing to perform | ||
| Engage team in pre-briefs to introduce members, clarify roles, and bring new or returning team members up to speed about current priorities, emergent challenges, and performance expectations | Shared mental models and transactive memory systems | Team unfamiliarity, role ambiguity |
| Ensure team members know who possesses deep expertise in key and emergent areas | Transactive memory systems, cognitive trust | Team unfamiliarity, role ambiguity |
| Provide team with instrumental support and resources to reduce concerns at home (e.g., childcare) | Task vigilance | Home demands |
|
| ||
| During Performance Episode | ||
| Note when team members may be drained or distracted, and offer to provide support and backup | Task vigilance, affect-based trust | Workload, team unfamiliarity, home demands |
| Respond to questions and concerns openly, ensuring that team members speak up, ask questions, and admit when they need help | Psychological safety, cognitive-based trust | Role ambiguity, team unfamiliarity |
| When disagreements emerge, focus on identifying what is right, not who is right | Team conflict | Role ambiguity |
|
| ||
| After Performance Episode | ||
| Engage in team de-briefing to discuss what is going right and what is going wrong, discussing recent “wins (e.g., a success, an obstacle overcome, progress made) | Psychological safety, collective efficacy | Role ambiguity, team unfamiliarity, workload |
| Take time to regularly check in with coworkers | Task vigilance | Home demands |
Preparing to perform.
A number of countermeasures can be introduced as a team prepares for a performance episode—for example, at the beginning of a shift or between each patient’s room on rounds. High performing teams engage in pre-briefing to strategize together and coordinate actions (Salas et al., 2007). Pre-briefing is especially important for teams with rotating membership, as it allows teams a time to clarify roles and responsibilities and to help build a shared mental model even if team members have never worked together before (Fiore et al., 2003). However, even teams with stable membership can benefit from pre-briefing—instead of focusing on role clarity, these teams may focus on developing a shared mental model of the team environment, improving team adaptability (Christian et al., 2017). Pre-briefs can be informal and need not take much time, but teams should focus on communicating information that will provide role clarity and improve situation awareness. For example, a team might designate a point person for questions about a new type of treatment, or even simply introduce teammates and provide a bit of background so everyone knows who is a hospital veteran or has deep expertise in a particular area versus who has been called in to help with the crisis. To further bolster these pre-briefs and help teams reduce cognitive load, hospitals might provide name tags for newly formed teams with team members’ organizational role and sub-specialty.
While pre-briefing can be conducted by team members, the organization or a team leader should try to provide instrumental support and resources to team members to help reduce their “home-related” concerns prior to beginning a shift. The benefits of perceived organization support are numerous (Rhoades & Eisenberger, 2002), but under times of stress, support plays an even more important role. Where possible, organizations might consider providing additional support to the families of healthcare workers. If financial resources are too limited to offer direct support, simply maintaining a website with community resources for families may at least reduce some of the concerns that would otherwise distract them from maintaining task vigilance (Tannenbaum et al., 2020). Team leaders can provide similar support by providing time for people to check in with family members or friends, which can both reduce stress on the home front, and afford brief moments of recovery to build resiliency (Alliger et al., 2015).
During a performance episode.
Teams that engage in backup behavior can improve both performance and affective outcomes for teams. Backup behavior involves any assistance provided to a team member to perform their work—for example, providing coaching, helping a team member complete a task, or assuming and completing a teammate’s task on their behalf (Marks et al., 2001). Team members and leaders can, by observing and talking with team members, maintain a sense of who may be struggling or fatigued in a given shift. Providing backup to these team members by, for example, offering to take on a team member’s responsibilities for half an hour to provide the team member an opportunity to decompress or call a family member, can help team members cope with workload and home demands and can also help the team build affect-based trust (Webber, 2008).
When teams are in the midst of a performance episode, but also before and after, team members (and especially leaders) should take care to respond to questions and concerns openly. This is especially important when others are admitting mistakes or a lack of knowledge—responding positively when others speak up directly boosts psychological safety and cognitive-based trust (Nembhard & Edmondson, 2006; Webber, 2008). While longer term teams may have established psychological safety, responding with openness is especially pertinent in rotating and newly formed teams, where norms for communication have not been established.
After a performance episode.
Just as pre-briefing is a vitally important behavior before a shift or patient interaction, de-briefing can help teams learn after a performance episode (Salas et al., 2007). De-briefing provides team members an opportunity to share what’s working despite insufficient resources, and brainstorm creative workarounds to problems they confront—meta-analytic findings indicate that de-briefing can improve team performance by 20–25% (Tannenbaum & Cerasoli, 2013). Debriefs can also improve team reflexivity (i.e., the extent to which teams reflect upon and modify their performance), as debriefing provides an opportunity for reflection and planning (Widmer et al., 2009). Importantly, teams should use debriefs as an opportunity to build and maintain psychological safety—when team members, and especially leaders, show a willingness to admit something they didn’t know or a mistake they made, others are more likely to speak up. The more individuals share about what isn’t working or what they would do differently, the more teams learn from each performance episode (Edmondson, 1999).
In the current context, teams de-briefing should take special care to also discuss what is working. In the midst of a pandemic, a team’s “wins” may feel infrequent and out of a team’s control. Directing teams to also reflect on what is working can boost a team’s collective efficacy by reminding them of their successes. Some team members may be unaware of a recent win or indication of progress, like the recovery of long-term patients or a reduction in newly admitted patients, so it is important to communicate those wins to the entire team. Taking a moment to celebrate can provide teams with a sign of their efficacy, boosting their morale.
Finally, teams should take time to regularly check-in with coworkers. Check-ins can be particularly important after a stressful performance episode. These check-ins should be distinct from a de-brief—instead of focusing on team behaviors and performance, checking in with a teammate about how they are doing psychologically is an opportunity to demonstrate team care, ensuring that teammates remain physically and psychologically healthy (Landon et al., 2018). To provide further psychological support, organizations may consider sharing stories of how the community is recognizing the contributions of healthcare workers. Such acts demonstrate social support, helping team members maintain vigilance and avoid burnout (Etzion, 1984).
Recommendations for Recovery
Although the earliest peak of COVID-19 cases has seemed to wane, additional outbreaks have occurred and will continue until a vaccine has proven safe and efficacious (Anderson et al., 2020). Regardless, there is a need to understand how teams in healthcare and beyond can recover from the current pandemic and prepare for the next disaster. While the recommendations provided so far are aimed at helping teams in the midst of a crisis, additional actions can be implemented in the aftermath. The recommendations for post-crisis recovery involve many of the same psychological constructs most salient in the midst of a crisis (e.g., collective efficacy and psychological safety), but with more time and resources, organizations can broaden the scope of team development interventions included in a strategic recovery (Shuffler et al., 2018).
Boost team resilience.
While some efforts to improve team resilience can help lessen the impact of stressors within days or weeks, additional measures to help teams bounce back can aid recovery over months and help prepare teams to tackle the next crisis that comes their way. Team resilience involves three phases: minimizing, managing, and mending (Alliger et al., 2015; Stoverink et al., 2020). While behaviors associated with “managing” help teams during a disaster, mending and minimizing behaviors help teams recover and prepare for the future, respectively. Mending behaviors involve reflecting on and learning from the team’s experiences, making necessary changes to team structures and processes (Alliger et al., 2015). Minimizing behaviors focus on preparing for the future by enhancing a team’s ability to detect adversity and formulating strategies for bouncing back (Stoverink et al., 2020).
Reflect on the challenges that emerged and how response could improve.
Perhaps the most effective tool for teams “mending” in the aftermath of the pandemic is debriefing. Recall that debriefing activities can be used between performance episodes for teams currently experiencing stressors—similar principles apply on a broader scale for recovery to debrief at both the team and organizational level (Allen et al., 2018). For example, teams should focus their discussion on team processes, rather than outcomes; discuss specific events rather than general performance; and identify new roles, norms, and processes that emerged and should continue (Salas et al., 2008; Tannenbaum & Cerasoli, 2013; Reyes et al., 2018). Debriefing about new processes and emergent adaptations helps surface where the team has developed new or strengthened capabilities that they can carry forward (Salas et al., 2008), and this feedback can help teams recall their successes to boost collective efficacy (Baker, 2001). Lessons learned can then be shared across teams.
While discussing things that did not go well is also pertinent to the debrief process, the discussion should frame “mistakes” as learning opportunities. Such an approach can buffer teams from losing collective efficacy and can also boost psychological safety—a key component of debriefing (Allen et al., 2018). Instead of fearing judgment for contributing, people are more likely to share “failures” that the team can build on to improve outcomes in the future. Table 2 provides a debriefing guide, summarizing recommendations for healthcare teams in COVID-19.
Table 2.
Periodic Team Debriefs During COVID-19: Leader’s Guide (adapted from Reyes et al., 2018)
|
1. Set the stage (30 to 60 seconds) • Explain why you are conducting a debrief and what the team will be discussing. • “This is a quick opportunity to learn from our experience. We’ll do these periodically.” “Let’s consider how we worked as a team, in addition to any technical issues.” • If there are any boundaries or “non-negotiables,” let the team know what’s off limits. Basic assumption: “We’re all competent and well-intentioned people who want to do our best. But these are not normal times; we’ll need to continually make small adjustments to be effective.” | ||
|
| ||
|
2. Ask the team for their observations (5–20 minutes) • Where have we had a success, made progress, or overcome a challenge? What are we doing well under the circumstances? • What new or additional challenges have emerged? • What should we do differently or focus more attention on going forward? Why? • Is there anything we need to help us treat our patients and help us stay healthy? | ||
|
| ||
|
3. Add your observations/recommendations and confirm you understanding (5–10 minutes) • Reinforce their observations, or if you noticed something different, share your view. • Be sure any feedback is clear, actionable, and focuses on the work, not personal traits. | ||
|
| ||
|
4. Summarize any agreed upon actions or focus for the future (5 minutes) • Be clear about who will do what, when…and how this will help the team. • Specify when and how you will follow up to assess progress (e.g., next debrief?). • If you will be seeking resources, do not make commitments that you aren’t sure you can keep. Tell them what you will request, but not that you are “getting” this for them. Tip: Ask the team for their perceptions first. Then if possible, acknowledge something you could have done differently or will focus on in the future. This will make it easier for team members to voice their own observations or concerns. | ||
|
| ||
| Tip : If the team doesn’t naturally discuss teamwork, ask “ how have we been working as a team ?” Perhaps ask one or two specific questions such as: | ||
|
| ||
| How well did we…? | How clear were our…? | |
|
| ||
| • Share information • Anticipate challenges • Handle conflict • Coordinate with “outsiders” |
• Ask for/offer help • Monitor/provide backup • Share/allocate resources • Speak up/challenge |
• Roles/assignments • Priorities • Sources of expertise (who knows what) |
Implement team training to reiterate best practices.
Using debriefs helps teams and leaders catalyze new insights from the crisis. These findings can be used as part of a needs analysis to identify where team training might help to strengthen a teams’ existing skills or build new skills that became increasingly important during the pandemic (Hughes et al., 2018). Although it may not be practical to conduct team training while combatting a pandemic, the same behaviors that lead to effective teamwork under normal circumstances are even more important for teams under stress. After a crisis wanes, organizations can continue to build employee teamwork skills through team training programs focused on a broad range of team best practices. The same teamwork behaviors instilled in widely available training programs (e.g., TeamSTEPPS for healthcare teams; King et al., 2008) are paramount in times of crisis.
Promote team well-being.
While the first three recommendations are focused on improving team learning and performance, it is also important to attend to team members’ psychological needs. Given the psychological stress and trauma employees across contexts are expected to face in the aftermath of the pandemic (CDC, 2020b), it is important that teams instill behaviors to continue to promote the well-being of their members. Initial research has explored the role that socially supportive behaviors (e.g., checking in on teammates) can have on teams working in high stress environments (Landon et al., 2018). Interventions at the organizational level that improve social support can also have ripple effects to teams, improving both teamwork climate and team member mental health (Heaney et al., 1995).
Recognize those working “behind the scenes.”
Physicians and nurses have rightly been declared heroes in this pandemic. However, hospital staff members include individuals in a wide range of roles, many of which are receiving less recognition in the media. Such a dynamic allows for the development of faultlines, or schisms dividing a team along the lines of two or more demographic or occupational characteristics (Rico et al., 2007). In healthcare, faultlines might occur on a team of ICU physicians and respiratory therapists, who differ in both role (physician vs. ancillary care) and specialty (intensive care vs. respiratory care). This example can be extrapolated across contexts on the basis of any number of demographic characteristics (e.g., age, race, educational background, or organizational department). While external threat helps mitigate the risk of fautlines while teams are in duress (Spoelma & Ellis, 2017), as the pandemic wanes, the lack of external threat might provide fodder for divisions to grow. To avoid such faultlines, leaders and team members should demonstrate gratitude toward all contributors and include them in debriefs and reflections about the crisis. Efforts to appreciate the role that every worker has played creates a sense that everyone played a part in getting through the crisis.
Work to improve conditions for teams in crisis.
Although some stressors in any crisis are unpredictable or unavoidable, the aforementioned recommendations serve as a foundation for improving conditions for teams in the future. As Figure 1 illustrates, the outcomes of the current pandemic—including team learning, performance, and resilience—inform the inputs for the next crisis. Beyond preparing teams, organizations should also prepare their leaders to continue promoting team learning. Leaders who foster inclusiveness by demonstrating openness to new ideas and being accessible to their team members help build psychological safety and improve team learning (Hirak et al., 2012).
Organizations can also use the experiences shared in the aftermath of COVID-19 to prepare interventions that will serve as countermeasures in the next crisis. For example, in organizations where staffing was in flux, team members may have had difficulty forming trust with their new teammates. Although some of the aforementioned countermeasures can help teams boost trust in the midst of a crisis, interventions can also be prepared ahead of time to help future teams build swift trust, or trust that develops rapidly in temporary or swift-starting action teams where members do not have time to perceive deep-level trust cues—instead, they may use surface-level cues (e.g., demographic characteristics) to indicate whether team members are trustworthy (Meyerson et al., 1996; Wildman et al., 2012). For example, organizations might develop a “launch protocol” to help leaders guide team members through their initial emotional reactions to their new team members in order to promote swift trust (Wildman et al., 2012).
The Research Road Ahead
This review demonstrates a robust body of research exploring how teams coordinate, cooperate, and communicate in turbulent times. However, the nature of the current pandemic (i.e., the length of the crisis and strains on healthcare team resources) has shed light on several avenues for future research in understanding healthcare teams under stress. First, a better understanding of team dynamics, or the moment-to-moment affect, behavior, and cognition of healthcare teams over time and under stress, would provide greater insight into how countermeasures can be designed and implemented to have the greatest impact on team process and outcomes. For example, an understanding of how emergent processes (e.g., psychological safety) evolve, change, and mature over long periods of time, particularly in healthcare, is lacking. Though research to this point has provided a robust understanding of the conditions that promote psychological safety, less is known about how these conditions impact psychological safety over weeks and months in healthcare teams working in adverse and shifting conditions.
Second, emergent, multi-level phenomena related to the psychological health of healthcare teams and their members warrant additional research and further thought. For example, while some work has investigated how individual member stress can additively impact team outcomes (ten Brummelhuis et al., 2012), additional research might investigate the conditions that facilitate stress contagion in teams, or whether teams experience a “tipping point” wherein a certain proportion of a team must experience stress for contagion to occur. Some organizations, including NASA, have studied concepts like “team well-being” and “team care” within their contexts, noting the importance of behaviors that promote behavioral health as critically important for team success (Landon et al., 2018). Moreover, behavioral health is paramount to healthcare teams’ viability and success. Accordingly, more work is needed to elucidate the definitions of these terms, their relationship to emergent states and to develop a better understanding of how they influence other team-level constructs.
Third, team member fluidity is a common characteristic of healthcare teams, even outside of this pandemic. Additional research is needed to better understand how teamwork unfolds in teams with dynamic rather than more stable membership (Tannenbaum et al., 2012), as well as on teams with members who are asked to fulfill unfamiliar roles. As is the case currently, teams with rotating membership are especially prevalent during a crisis, and the dynamics of these teams are likely to differ from those typically studied.
Fourth, not all team training is created equal. Under stressful conditions, the design and delivery of medically-focused team training may require alterations, and future research might identify new design, delivery, and implementation methods to train healthcare teams facing stressors. In addition, new approaches to creating robust countermeasures, including simulation and “learning teamwork as-you-go” require additional exploration.
Finally, as outlined above, further exploration of team resilience in healthcare teams is warranted. The ability to bounce back in the face of adversity is key to sustaining effective teamwork under stressful conditions. However, team scientists are just beginning to unpack what team resilience looks like and how it can be boosted. To date, most work on team resilience is theoretical in nature (Alliger et al., 2015; Stoverink et al., 2020). Additional empirical work could help identify the precise behavioral markers that characterize and promote team resilience. Moreover, an understanding of these behavioral markers is necessary for developing metrics and assessment tools to better understand team resilience in healthcare contexts.
Final Thoughts
The conditions frontline healthcare workers are facing during the current crisis are unprecedented on many metrics. However, many of the stressors stemming from the pandemic resemble those well-documented in the psychological literature (Razinskas & Hoegl, 2020). Other events, like natural disasters or smaller-scale epidemics, trigger similar stressors and thus, the same principles for remediation and recovery apply. In addition, though many of the countermeasures described in this review can be implemented by team members and team leaders, organizations can play a vital role in promoting effective teamwork by standardizing and supporting the implementation of countermeasures.
Thus, the recommendations provided in this review are intended to serve several purposes. Primarily, they provide insights and countermeasures for those positions in medical settings (e.g., quality improvement, human factors, patient safety, performance improvement, team science) that can help healthcare teams persist through the ebb and flow of COVID-19 stressors. In the weeks and months that follow resolution, psychologists can use these recommendations to help teams catalyze what they have learned from these harrowing circumstances and learn lessons for the future. The science of teamwork has generated important understandings about team performance under stress, and this review can help translate the science to practice, improving team effectiveness and outcomes for healthcare workers at the frontlines of this pandemic.
Public Significance Statement.
In the wake of the COVID-19 pandemic, medical teams have been central to community and healthcare center response efforts. However, increased stressors from both within and outside of the hospital have generated unprecedented challenges for healthcare teams and their members. This review highlights how psychological research can inform our understanding of stress in healthcare teams, focusing on evidence-based countermeasures that can improve teamwork during and in the aftermath of the pandemic.
Acknowledgments
This work was partially supported by the Center for Clinical and Translational Sciences (UT Health Science Center, Houston, TX), which is funded by National Institutes of Health Clinical and Translational Award UL1 TR003167 from the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health. Rice University and University of Texas Health Sciences Center Houston are partners in this grant. This work was also partially supported by National Science Foundation grants #1853528 and #1842894 to Rice University as well as NASA grants NNX16AP96G and NNX17AB55G to Rice University.
References
- Allen JA, Reiter-Palmon R, Crowe J, & Scott C (2018). Debriefs: Teams learning from doing in context. American Psychologist, 73(4), 504–516. [DOI] [PubMed] [Google Scholar]
- Alliger GM, Cerasoli CP, Tannenbaum SI, & Vessey WB (2015). Team resilience: How teams flourish under pressure. Organizational Dynamics, 44(3), 176–184. [Google Scholar]
- Anderson RM, Heesterbeek H, Klinkenberg D, & Hollingsworth TD (2020). How will country-based mitigation measures influence the course of the COVID-19 epidemic?. The Lancet, 395(10228), 931–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appelbaum NP, Dow A, Mazmanian PE, Jundt DK, & Appelbaum EN (2016). The effects of power, leadership and psychological safety on resident event reporting. Medical Education, 50(3), 343–350. [DOI] [PubMed] [Google Scholar]
- Baker DF (2001). The Development of Collective Efficacy in Small Task Groups. Small Group Research, 32(4), 451–474. [Google Scholar]
- Baker DP, Gustafson S, Beaubien J, Salas E, & Barach P (2003). Medical teamwork and patient safety: The evidence-based relation (Report No05–0053). Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- Bakker AB, & Demerouti E (2007). The job demands-resources model: State of the art. Journal of Managerial Psychology, 22(3), 309–328. [Google Scholar]
- Cannon‐Bowers JA, & Salas E (1998). Making decisions under stress: Implications for individual and team training. Washington, DC, U.S.: American Psychological Association. [Google Scholar]
- Carmeli A, & Gittell JH (2009). High‐quality relationships, psychological safety, and learning from failures in work organizations. Journal of Organizational Behavior, 30(6), 709–729. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2020a). CDC COVID data tracker. Retrieved May 12, 2020, from https://www.cdc.gov/covid-data-tracker/
- Centers for Disease Control and Prevention (CDC). (2020b). Employees: How to cope with job stress and build resilience during the COVID-19 pandemic. Retrieved May 28, 2020, from https://www.cdc.gov/coronavirus/2019-ncov/community/mental-health-non-healthcare.html
- Christan JS, Christian MS, Pearsall MJ, & Long EC (2017). Team adaptation in context: An integrated conceptual model and meta-analytic review. Organizational Behavior and Human Decision Processes, 140, 62–89. [Google Scholar]
- DeChurch LA, & Mesmer-Magnus JR (2010). Measuring shared team mental models: A meta-analysis. Group Dynamics: Theory, Research, and Practice, 14(1), 1–14. [Google Scholar]
- De Jong BA, Dirks KT, & Gillespie N (2016). Trust and team performance: A meta-analysis of main effects, moderators, and covariates. Journal of Applied Psychology, 101(8), 1134–1150. [DOI] [PubMed] [Google Scholar]
- Drach‐Zahavy A, & Freund A (2007). Team effectiveness under stress: A structural contingency approach. Journal of Organizational Behavior, 28(4), 423–450. [Google Scholar]
- Driskell T, Salas E, & Driskell JE (2018). Teams in extreme environments: Alterations in team development and teamwork. Human Resource Management Review, 28(4), 434–449. [Google Scholar]
- Driskell JE, Salas E, & Johnston J (1999). Does stress lead to a loss of team perspective? Group Dynamics: Theory, Research, and Practice, 3(4), 291–302. [Google Scholar]
- Edmondson A (1999). Psychological safety and learning behavior in work teams. Administrative Science Quarterly, 44(2), 350–383. [Google Scholar]
- Ellis APJ (2006). System breakdown: The role of mental models and transactive memory in the relationship between acute stress and team performance. Academy of Management Journal, 49(3), 576–589. [Google Scholar]
- Ellis APJ, & Pearsall MJ (2011). Reducing the negative effects of stress in teams through cross-training: A job demands-resources model. Group Dynamics: Theory, Research, and Practice, 15(1), 16–31. [Google Scholar]
- Ervin JN, Kahn JM, Cohen TR, & Weingart LR (2018). Teamwork in the intensive care unit. American Psychologist, 73(4), 468–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etzion D (1984). Moderating effect of social support on the stress–burnout relationship. Journal of Applied Psychology, 69(4), 615–622. [PubMed] [Google Scholar]
- Fiore SM, Salas E, Cuevas HM, & Bowers CA (2003). Distributed coordination space: toward a theory of distributed team process and performance. Theoretical Issues in Ergonomics Science, 4(3–4), 340–364. [Google Scholar]
- Fiscella K, & McDaniel SH (2018). The complexity, diversity, and science of primary care teams. American Psychologist, 73(4), 451–467. [DOI] [PubMed] [Google Scholar]
- Frazier ML, Fainshmidt S, Klinger RL, Pezeshkan A, & Vracheva V (2017). Psychological safety: A meta-analytic review and extension. Personnel Psychology, 70(1), 113–165. [Google Scholar]
- Gan WH, Lim JW, & David KOH (2020). Preventing intra-hospital infection and transmission of COVID-19 in healthcare workers. Safety and Health at Work, 11(2), 241–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goha B, Larivière M, & Nowrouzi-Kia B (2020). Sickness absence in healthcare workers during the COVID-19 pandemic. Occupational Medicine. [DOI] [PMC free article] [PubMed]
- Hall KL, Vogel AL, Huang GC, Serrano KJ, Rice EL, Tsakraklides SP, & Fiore SM (2018). The science of team science: A review of the empirical evidence and research gaps on collaboration in science. American Psychologist, 73(4), 532–548. [DOI] [PubMed] [Google Scholar]
- Heaney CA, Price RH, & Rafferty J (1995). Increasing coping resources at work: A field experiment to increase social support, improve work team functioning, and enhance employee mental health. Journal of Organizational Behavior, 16(4), 335–352. [Google Scholar]
- Hirak R, Peng AC, Carmeli A, & Schaubroeck JM (2012). Linking leader inclusiveness to work unit performance: The importance of psychological safety and learning from failures. The Leadership Quarterly, 23(1), 107–117. [Google Scholar]
- Hobfoll SE (1989). Conservation of resources: A new attempt at conceptualizing stress. American Psychologist, 44(3), 513–524. [DOI] [PubMed] [Google Scholar]
- Hollenbeck JR, Ilgen DR, Tuttle DB, & Sego DJ (1995). Team performance on monitoring tasks: An examination of decision errors in contexts requiring sustained attention. Journal of Applied Psychology, 80(6), 685–696. [Google Scholar]
- Hughes AM, Gregory ME, Joseph DL, Sonesh SC, Marlow SL, Lacerenza CN, Benishek LE, King HB, & Salas E (2016). Saving lives: A meta-analysis of team training in healthcare. Journal of Applied Psychology, 101(9), 1266–1304. [DOI] [PubMed] [Google Scholar]
- Ilgen DR, Hollenbeck JR, Johnson M, & Jundt D (2005). Teams in Organizations: From Input-Process-Output Models to IMOI Models. Annual Review of Psychology, 56, 517–543. [DOI] [PubMed] [Google Scholar]
- Jehn KA (1997). A qualitative analysis of conflict types and dimensions in organizational groups. Administrative Science Quarterly, 42(3), 530–557. [Google Scholar]
- Jex SM, & Gudanowski DM (1992). Efficacy beliefs and work stress: An exploratory study. Journal of Organizational Behavior, 13(5), 509–517. [Google Scholar]
- Johns G (2006). The essential impact of context on organizational behavior. Academy of Management Review, 31(2), 386–408. [Google Scholar]
- Kessel M, Kratzer J, & Schultz C (2012). Psychological safety, knowledge sharing, and creative performance in healthcare teams. Creativity and Innovation Management, 21(2), 147–157. [Google Scholar]
- King HB, Battles J, Baker DP, Alonso A, Salas E, Webster J, Toomey L, Salisbury M (2008). TeamSTEPPS: Team strategies and tools to enhance performance and patient safety. In Henriksen K, Battles JB, Keyes MA, & Grady ML (Eds.), Advances in patient safety: New directions and alternative approaches (3rd ed., Vol. 3, pp. 5–20: Performance and Tools). Rockville, MD: Agency for Healthcare Research and Quality. [PubMed] [Google Scholar]
- Lacerenza CN, Marlow SL, Tannenbaum SI, & Salas E (2018). Team development interventions: Evidence-based approaches for improving teamwork. American Psychologist, 73(4), 517–531. [DOI] [PubMed] [Google Scholar]
- Landon LB, Slack KJ, & Barrett JD (2018). Teamwork and collaboration in long-duration space missions: Going to extremes. American Psychologist, 73(4), 563–575. [DOI] [PubMed] [Google Scholar]
- Lazzerini M, & Putoto G (2020). COVID-19 in Italy: momentous decisions and many uncertainties. The Lancet Global Health, 8(5), e641–e642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LePine JA, Piccolo RF, Jackson CL, Mathieu JE, & Saul JR (2008). A meta-analysis of teamwork processes: tests of a multidimensional model and relationships with team effectiveness criteria. Personnel Psychology, 61(2), 273–307. [Google Scholar]
- Luciano MM, Bartels AL, D’Innocenzo L, Maynard MT, & Mathieu JE (2018). Shared team experiences and team effectiveness: Unpacking the contingent effects of entrained rhythms and task characteristics. Academy of Management Journal, 61(4), 1403–1430. [Google Scholar]
- Manser T (2009). Teamwork and patient safety in dynamic domains of healthcare: A review of the literature. Acta Anaesthesiologica Scandinavica, 53(2), 143–151. [DOI] [PubMed] [Google Scholar]
- Marks MA, Mathieu JE, & Zaccaro SJ (2001). A temporally based framework and taxonomy of team processes. Academy of Management Review, 26(3), 356–376. [Google Scholar]
- Mathieu JE, Tannenbaum SI, Donsbach JS, & Alliger GM (2014). A review and integration of team composition models: Moving toward a dynamic and temporal framework. Journal of Management, 40, 126–156. [Google Scholar]
- Mazzocco K, Petitti DB, Fong KT, Bonacum D, Brookey J, Graham S, … & Thomas EJ (2009). Surgical team behaviors and patient outcomes. The American Journal of Surgery, 197(5), 678–685. [DOI] [PubMed] [Google Scholar]
- McAllister DJ (1995). Affect- and cognitive-based trust as foundations for interpersonal cooperation in organizations. Academy of Management Journal, 38(1), 24–59. [Google Scholar]
- Meyerson D, Weick K, & Kramer R (1996). Swift trust and temporary groups. Trust in organizations: Frontiers of theory and research (pp. 166–195). SAGE. [Google Scholar]
- Nembhard IM, & Edmondson AC (2006). Making it safe: The effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. Journal of Organizational Behavior, 27(7), 941–966. [Google Scholar]
- Razinskas S & Hoegl M (2020). A multilevel review of stressor research in teams. Journal of Organizational Behavior, 41(2), 185–209. [Google Scholar]
- Reyes DL, Tannenbaum SI, & Salas E (2018). Team development: the power of debriefing. People & Strategy, 41(2), 46–52. [Google Scholar]
- Rhoades L, & Eisenberger R (2002). Perceived organizational support: a review of the literature. Journal of Applied Psychology, 87(4), 698–714. [DOI] [PubMed] [Google Scholar]
- Rico R, Molleman E, Sánchez-Manzanares M, & Van der Vegt GS (2007). The effects of diversity faultlines and team task autonomy on decision quality and social integration. Journal of Management, 33(1), 111–132. [Google Scholar]
- Rodríguez‐Escudero AI, Carbonell P, & Munuera‐Aleman JL (2010). Positive and negative effects of team stressors on job satisfaction and new product performance. Journal of Product Innovation Management, 27(6), 856–868. [Google Scholar]
- Rogers D, Lingard L, Boehler ML, Espin S, Klingensmith M, Mellinger JD, & Schindler N (2011). Teaching operating room conflict management to surgeons: clarifying the optimal approach. Medical Education, 45(9), 939–945. [DOI] [PubMed] [Google Scholar]
- Rosen MA, DiazGranados D, Dietz AS, Benishek LE, Thompson D, Pronovost PJ, & Weaver SJ (2018). Teamwork in healthcare: Key discoveries enabling safer, high-quality care. American Psychologist, 73(4), 433–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas E, Bisbey TM, Traylor AM, & Rosen MA (2019). Can teamwork promote safety in organizations?. Annual Review of Organizational Psychology and Organizational Behavior, 7, 283–313. [Google Scholar]
- Salas E, Rosen MA, & King H (2007). Managing teams managing crises: principles of teamwork to improve patient safety in the emergency room and beyond. Theoretical Issues in Ergonomics Science, 8(5), 381–394. [Google Scholar]
- Salas E, Klein C, King H, Salisbury M, Augenstein JS, Birnbach DJ, … & Upshaw C (2008). Debriefing medical teams: 12 evidence-based best practices and tips. The Joint Commission Journal on Quality and Patient Safety, 34(9), 518–527. [DOI] [PubMed] [Google Scholar]
- Schippers MC, West MA, & Dawson JF (2015). Team reflexivity and innovation: The moderating role of team context. Journal of Management, 41(3), 769–788. [Google Scholar]
- Shuffler ML, Diazgranados D, Maynard MT, & Salas E (2018). Developing, sustaining, and maximizing team effectiveness: An integrative, dynamic perspective of team development interventions. Academy of Management Annals, 12(2), 688–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smallwood J, & Schooler JW (2006). The restless mind. Psychological Bulletin, 132(6), 946–958. [DOI] [PubMed] [Google Scholar]
- Spoelma TM, & Ellis APJ (2017). Fuse or fracture? Threat as a moderator of the effects of diversity faultlines in teams. Journal of Applied Psychology, 102(9), 1344–1359. [DOI] [PubMed] [Google Scholar]
- Stajkovic AD, Lee D, & Nyberg AJ (2009). Collective efficacy, group potency, and group performance: Meta-analyses of their relationships, and test of a mediation model. Journal of Applied Psychology, 94(3), 814–828. [DOI] [PubMed] [Google Scholar]
- Stoverink AC, Kirkman BL, Mistry S, & Rosen B (2020). Bouncing back together: Toward a theoretical model of work team resilience. Academy of Management Review, 45(2), 395–422. [Google Scholar]
- Tannenbaum SI, & Cerasoli CP (2013). Do team and individual debriefs enhance performance? A meta-analysis. Human Factors, 55(1), 231–245. [DOI] [PubMed] [Google Scholar]
- Tannenbaum SI, Mathieu JE, Salas E & Cohen D (2012). Teams are changing – Are research and practice evolving fast enough? Industrial and Organizational Psychology: Perspectives on Science and Practice, 5, 2–24. [Google Scholar]
- Tannenbaum SI, Traylor AM, Thomas EJ, & Salas E (2020). Managing teamwork in the face of pandemic: Evidence-based tips. BMJ Quality & Safety, 0, 1–5. [DOI] [PubMed] [Google Scholar]
- ten Brummelhuis LL, Ter Hoeven CL, Bakker AB, & Peper B (2011). Breaking through the loss cycle of burnout: The role of motivation. Journal of Occupational and Organizational Psychology, 84(2), 268–287. [Google Scholar]
- ten Brummelhuis LL, & Bakker AB (2012). A resource perspective on the work–home interface: The work–home resources model. American Psychologist, 67(7), 545–556. [DOI] [PubMed] [Google Scholar]
- ten Brummelhuis LL, Oosterwaal A, & Bakker AB (2012). Managing family demands in teams: The role of social support at work. Group & Organization Management, 37(3), 376–403. [Google Scholar]
- Urban JM, Weaver JL, Bowers CA, & Rhodenizer L (1996). Effects of workload and structure on team processes and performance: Implications for complex team decision making. Human Factors, 38(2), 300–310. [Google Scholar]
- Watson CB, Chemers MM, & Preiser N (2001). Collective efficacy: A multilevel analysis. Personality and Social Psychology Bulletin, 27(8), 1057–1068. [Google Scholar]
- Webber SS (2008). Development of cognitive and affective trust in teams: A longitudinal study. Small Group Research, 39(6), 746–769. [Google Scholar]
- Weller J, Boyd M, & Cumin D (2014). Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgraduate Medical Journal, 90(1061), 149–154. [DOI] [PubMed] [Google Scholar]
- Wildman JL, Shuffler ML, Lazzara EH, Fiore SM, Burke CS, Salas E, & Garven S (2012). Trust development in swift starting action teams: A multilevel framework. Group & Organization Management, 37(2), 137–170. [Google Scholar]


