Abstract
Purpose:
To study the corneal epithelial thickness with 9-mm scans of optical coherence tomography in normal Indians with appropriate representation of all age groups.
Methods:
This was a cross-sectional observational study. 263 patients were divided into the age groups 5–20 years, 21–35 years, 36–50 years and more than 51 years were recruited for the study. All patients underwent a detailed ophthalmic examination. Patients found to have any ocular surface or intraocular disease condition (except cataract and refractive error), or who had undergone any ophthalmic surgery in the past, or had corneal topography changes suggestive of corneal ectasias (screened in patients with astigmatism more than 3 diopters) or had been continuously using any topical medication in either eye for a period of 3 months or more with the last instillation being within 1 month of inclusion in the study were excluded. All subjects underwent corneal epithelial thickness measurement with anterior segment optical coherence tomography (AS-OCT) on the Avanti OCT (Model RTVueXR1002, Optovue, USA). The corneal epithelial thickness (CET) data from 25 sectors in each eye were analyzed.
Results:
263 right and left eyes of 263 patients were analyzed in the study. Mean CETs in the central 2 mm zone were 54.13 ± 4.51 μm and 54.37 ± 3.75 μm for the right and left eyes, respectively. The superior peripheral sectors and inferior paracentral sectors were the thinnest and the thickest sectors, respectively, in both eyes.
Conclusion:
CET parameters for Indian eyes are comparable to those reported from racially distinct and geographically distant study subjects.
Keywords: Epithelium thickness, corneal epithelium, optical coherence tomogrpahy, normative data, Indian
Corneal epithelial thickness (CET) parameters and the changes thereof are being studied with a renewed interest vis-à-vis ectasia diagnosis and treatment, orthokeratology lenses, and advanced surface ablations for correction of refractive errors.[1,2] However, a knowledge of normal CET is essential prior to understanding and analyzing abnormalities or changes secondary to diseases or treatment modalities.
In the past, few studies have assessed the corneal epithelial thickness in normal individuals using optical coherence tomography (OCT). However, initial studies had maximum scan diameter of only 6 mm which analyzed a very thin 1 mm (between 5 mm and 6 mm) wide outer rim.[3,5,6] This leads to poor assessment of extreme peripheral corneal epithelial thickness which may have a bearing on the assessment of CET changes in peripheral ectasias, wider ablation zones in keratorefractive surgery, and orthokeratology lenses. Studies with wide measurement zones (9 mm) either had too few subjects in the normal group or had poor representation of the pediatric age group.[7,8]
We aim to study the corneal epithelial thickness in normal Indians with appropriate representation of all age groups.
Methods
This was a prospective, cross-sectional observational study carried out in a tertiary care eye hospital in western India over an 18-month period from August 2017 to February 2019. Institutional Review Board and Ethics committee clearance was obtained prior to the commencement of the study. The adult subjects provided a written informed consent to participate in the study. Informed consents were obtained from the parents/guardians of the children and minor subjects.
A convenient sample of at least 200 subjects was predetermined for the study. A stratified sampling technique was employed by dividing the subjects into four age groups to have comparable representation. The aim was to recruit at least 50 subjects in each of the following age groups: 5–20 years, 21–35 years, 36–50 years, and more than 51 years. The age completed at last birthday was considered while including the subject in the study.
Patients presenting to the tertiary care eye hospital seeking consultation for refractive errors and cataracts were included in the study. All patients underwent a detailed refraction, slit lamp and biomicroscopic examination prior to inclusion in the study. Patients who were found to have any ocular surface or intraocular disease condition (except cataract and refractive error), or who had undergone any ophthalmic surgery in the past, or had corneal topography changes suggestive of corneal ectasias (screened in patients with astigmatism more than 3 diopters) or had been continuously using any topical medication in either eye for a period of 3 months or more with the last instillation being within 1 month of inclusion in the study were excluded.
The subjects, who fulfilled all the criteria, underwent corneal epithelial thickness measurement with anterior segment optical coherence tomography (AS-OCT) on the Avanti OCT (Model RTVueXR1002, Optovue, USA) using the Cam-L (low magnification corneal lens adapter). A 735-nm infra-red LED on gooseneck cable was used to externally illuminate the cornea and pupil and the subjects were asked to look at the internal fixation target. Scans were obtained when bright, well centered video images of the cornea were displayed real time on the console screen. The single best of 3 consecutive scans with good demarcation of corneal boundaries and good measurement reliability rating with signal strength index (SSI) > 60 was included in the study for analysis.
The OCT corneal epithelial thickness (CET) output map comprises 4 concentric zones. The innermost or the central zone is a circle of 2 mm diameter. The paracentral, midperipheral, and peripheral zones are concentric rings created by circles of the diameters 5 mm, 7 mm, and 9 mm, respectively. The outer three zones are further divided into eight pie-segments (PS) by eight radiating lines. Thus, each PS viz. superior, supero-temporal, temporal, infero-temporal, inferior, infero-nasal, nasal, and supero-nasal, has a paracentral, mid-peripheral, and peripheral zone. We chose to call each of this area, a sector. Thus, the machines present the CET, in microns, for a total of 25 sectors including the central circle.
The CET data from each of these sectors were analyzed separately using IBM SPSS Statistical Software version 23. The demographic data and refraction data were also captured and analyzed. The Paired t-test was performed for inter-eye comparison of the mean CET of each sector. The one-way ANOVA test was done to assess the variance of the mean CETs of the sectors within each pie-segment.
The CET values of each sector in the superior, supero-nasal, and supero-temporal pie segments were compared to the corresponding sector in the inferior, infero-nasal, and infero-temporal pie segments, respectively, for both eyes. The sectors in the nasal pie segments were compared with the corresponding sectors in the temporal pie-segments for both eyes.
An unweighted statistical mean of the CET values of all 3 sectors in each PS was calculated to represent the cumulative mean epithelial thickness (CuMET) for that particular PS. This was done to generate a simplified CET value representative of that particular PS.
All data are being presented with tables and figures.
Results
263 right and left eyes of 263 patients were analyzed as a part of the study. The mean (± SD) age of the whole study population was 34.42 ± 18.31 years. The male: female ratio was 123: 140. The median spherical refractive error was 0.00 D in both right and left eyes (minimum, maximum: right eye -8.50 D, + 4.75D; left eye -9.00 D, + 6.00 D).
There were 71 subjects (mean age 14.04 ± 5.10 years) in 5–20 years age group, 76 subjects (mean age 26.63 ± 4.71 years) in 21–35 years age group, 59 subjects (mean age 42.66 ± 3.92 years) in 36–50 years age group, and 57 subjects (mean age 61.65 ± 7.47 years) in the age group of > 51 years.
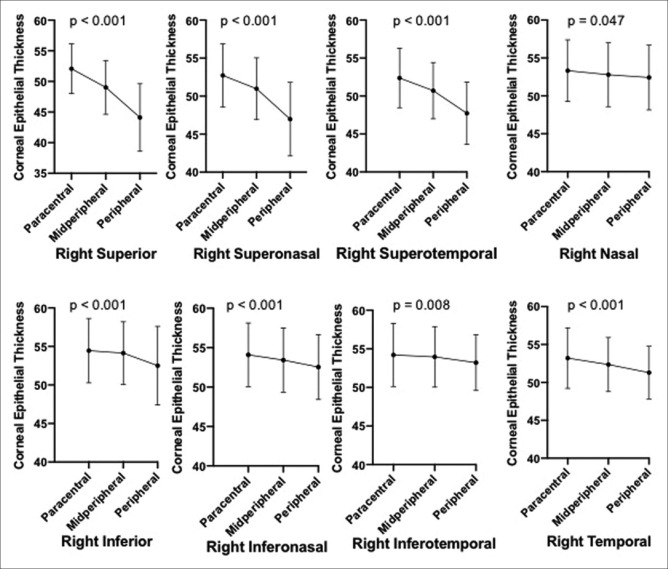
Fig. 1a shows the mean and standard deviation of the CET values in each sector for the right and left eye of the whole study population. Table 1 shows the inter-eye comparison of these mean CET values of each sector. The P values depicted in the last column are derived by comparing the means for right and left eyes using the T-test.
Figure 1.
(a) Mean CET values of the 25 sectors in the right and left eye. (b) Cumulative mean epithelial thickness (CuMET) values of the 8 pie segments in the right and left eye. (values in parenthesis depict the Standard Deviation)
Table 1.
Sector wise comparison of Mean±SD corneal epithelial thickness between the right eye and left eye of all subjects (n=263) in the study
| Corneal Sectors | Right eye | Left eye | P |
|---|---|---|---|
| Central Corneal Thickness | 54.13±4.51 | 54.37±3.75 | 0.337 |
| Superior | |||
| Paracentral | 52.08±4.06 | 52.26±3.75 | 0.418 |
| Mid-Peripheral | 49.03±4.39 | 49.32±3.73 | 0.239 |
| Peripheral | 44.12±5.52 | 44.24±5.15 | 0.731 |
| Supero-temporal | |||
| Paracentral | 52.37±3.92 | 52.66±3.77 | 0.192 |
| Mid-Peripheral | 50.70±3.70 | 50.34±3.76 | 0.097 |
| Peripheral | 47.73±4.10 | 46.61±4.15 | <0.001 |
| Temporal | |||
| Paracentral | 53.21±4.01 | 53.51±3.73 | 0.184 |
| Mid-Peripheral | 52.35±3.57 | 52.23±3.81 | 0.579 |
| Peripheral | 51.29±3.46 | 50.81±3.87 | 0.026 |
| Infero-temporal | |||
| Paracentral | 54.21±4.08 | 54.41±3.74 | 0.388 |
| Mid-Peripheral | 53.96±3.92 | 53.88±3.58 | 0.719 |
| Peripheral | 53.20±3.60 | 53.00±3.57 | 0.299 |
| Inferior | |||
| Paracentral | 54.46±4.17 | 55.03±3.85 | 0.019 |
| Mid-Peripheral | 54.14±4.07 | 54.32±4.83 | 0.548 |
| Peripheral | 52.51±5.10 | 53.02±3.88 | 0.086 |
| Infero-nasal | |||
| Paracentral | 54.09±4.04 | 54.40±3.68 | 0.183 |
| Mid-Peripheral | 53.42±4.07 | 54.06±3.64 | 0.008 |
| Peripheral | 52.55±4.13 | 53.16±3.63 | 0.010 |
| Nasal Sector | |||
| Paracentral | 53.33±4.07 | 53.62±3.62 | 0.222 |
| Mid-Peripheral | 52.79±4.22 | 53.28±3.73 | 0.057 |
| Peripheral | 52.43±4.27 | 53.24±3.69 | 0.002 |
| Supero-nasal | |||
| Paracentral | 52.73±4.16 | 52.89±3.64 | 0.487 |
| Mid-Peripheral | 50.97±4.08 | 51.79±3.70 | 0.001 |
| Peripheral | 46.98±4.85 | 48.51±4.07 | <0.001 |
SD=standard deviation
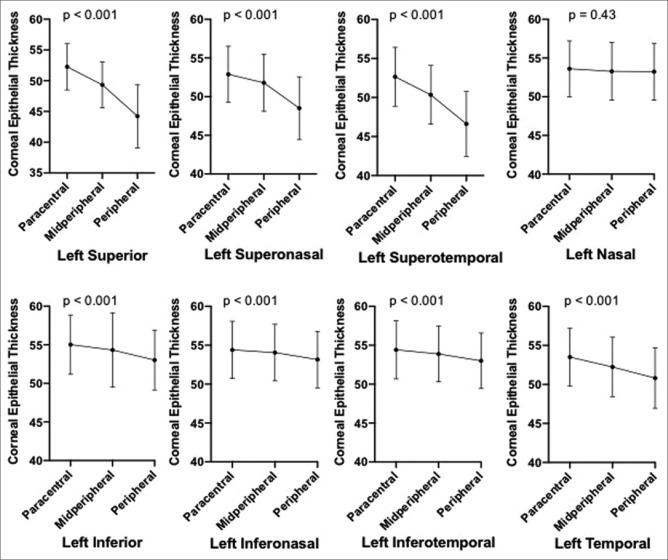
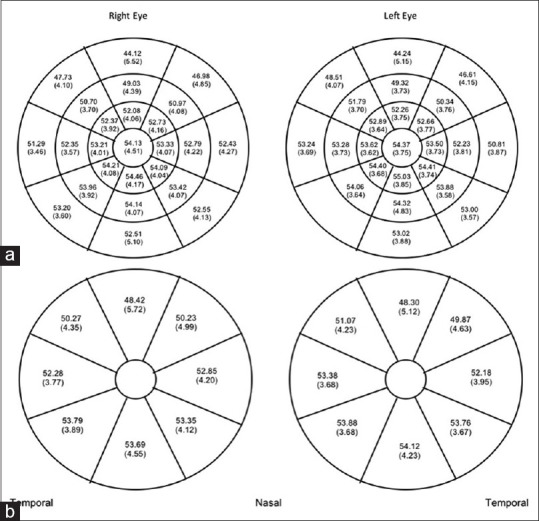
Fig. 2 shows the trend in the mean (with standard deviation) CET values from the paracentral to peripheral sector for each pie segment for the right eye. The P value depicted above each trend graph is obtained from a one-way ANOVA test which tested the variance in the CET values of the three sectors in each pie-segment. Fig. 3 shows the same analysis for the left eye.
Figure 2.
Dot and Whisker plot depicting the trends in the mean CET values from the paracentral to peripheral sector in each pie segment in the right eye. (Whisker depicts the standard deviation. P value above every plot is computed for the one-way ANOVA comparing the three mean CET values for each pie segment)
Figure 3.
Dot and whisker plot depicting the trends in the mean CET values from the paracentral to peripheral sector in each pie segment in the left eye. (Whisker depicts the standard deviation. P value above every plot is computed for the one-way ANOVA comparing the three mean CET values for each pie segment)
In both eyes, there was a statistically significant difference between the mean CET values of all the sectors in the superior pie segments and the corresponding sectors of the inferior pie-segments. The mean CET values of nasal sectors, except the paracentral sector, were found to be significantly different for the corresponding temporal sectors in both eyes [Table 2].
Table 2.
Comparison of mean±SD corneal epithelial thickness of each sector in the corresponding superior and inferior pie segments for the right and left eyes
| Sector | Pie Segment | Right Eye | P | Left Eye | P |
|---|---|---|---|---|---|
| Paracentral | Superior | 52.08±4.06 | <0.001 | 52.26±3.75 | <0.001 |
| Inferior | 54.44±4.17 | 55.03±3.85 | |||
| Superonasal | 52.73±4.16 | <0.001 | 52.89±3.64 | <0.001 | |
| Inferonasal | 54.09±4.04 | 54.40±3.68 | |||
| Superotemporal | 52.37±3.92 | <0.001 | 52.66±3.77 | <0.001 | |
| Inferotemporal | 54.21±4.08 | 54.41±3.74 | |||
| Nasal | 53.33±4.07 | 0.242 | 53.62±3.62 | 0.324 | |
| Temporal | 53.21±4.01 | 53.51±3.73 | |||
| Midperipheral | Superior | 49.03±4.39 | <0.001 | 49.32±3.73 | <0.001 |
| Inferior | 54.14±4.07 | 54.32±4.83 | |||
| Superonasal | 50.97±4.08 | <0.001 | 51.79±3.70 | <0.001 | |
| Inferonasal | 53.42±4.07 | 54.06±3.64 | |||
| Superotemporal | 50.70±3.70 | <0.001 | 50.34±3.76 | <0.001 | |
| Inferotemporal | 53.96±3.92 | 53.88±3.58 | |||
| Nasal | 52.79±4.22 | 0.002 | 53.28±3.73 | <0.001 | |
| Temporal | 52.35±3.57 | 52.23±3.81 | |||
| Peripheral | Superior | 44.12±5.52 | <0.001 | 44.24±5.15 | <0.001 |
| Inferior | 52.53±5.11 | 53.02±3.88 | |||
| Superonasal | 46.98±4.85 | <0.001 | 48.51±4.07 | <0.001 | |
| Inferonasal | 52.55±4.13 | 53.16±3.63 | |||
| Superotemporal | 47.73±4.10 | <0.001 | 46.61±4.15 | <0.001 | |
| Inferotemporal | 53.20±3.60 | 53.00±3.57 | |||
| Nasal | 52.43±4.27 | <0.001 | 53.24±3.69 | <0.001 | |
| Temporal | 51.29±3.46 | 50.81±3.87 |
n=263; SD=standard deviation
Fig. 1b depicts the cumulative mean epithelial thickness (CuMET) in each pie segment for the right and the left eye.
Discussion
In our study, the CETs in the central 2-mm zone were 54.13 ± 4.51 mm and 54.37 ± 3.75 mm for the right and left eyes, respectively. These values compare well to the average corneal vertex epithelial thickness of 53.9 ± 3.7 mm observed by Hashmani et al.[8] in their study. The mean CET in the central zone was 54.5 ± 5.9 mm in the study by Ma et al.[7] Furthermore, the mean central CET values observed in our study also compare well with those reported in other OCT-based studies but with a 6-mm scan zone.[3,5,6]
In our study, there was no statistically significant difference between the central CET values for the right and left eye.
As evident from Fig. 1a and Table 1, the superior peripheral sectors and inferior paracentral sectors were the thinnest and the thickest sectors, respectively, in both eyes. Overall, the superior pie-segments, in both eyes, had thinner mean CET values in all sectors as compared to corresponding sectors in other pie-segments. The thinner CET values in the superior pie-segments are attributed to the upper eyelid dynamics. The constant excursion of the upper eyelid, during blinking, causes friction leading to desquamation of the epithelium in the superior cornea.[9]
A trend of reduction in CET from the paracentral to peripheral sector was noted in each pie segment in our study. This trend was the most pronounced in the three superior pie segments of both eyes. A similar trend was reported by Du et al.[10] using custom made ultra-high resolution spectral domain OCT which showed lower CET values in the periphery as compared to center in the vertical meridian. This difference was more prominent in the superior cornea similar to our study. However, in the horizontal meridian (nasal-temporal), the peripheral CET values were found to be higher as compared to the central cornea. This is in direct contradiction to the findings in our study and we do not have a hypothesis to explain the same.
Our study has a significant representation of the pediatric age group which was lacking in the past studies. Assessing the CET of children not only makes our sample more inclusive but also is important because children form a significant proportion of the population benefitting from orthokeratology lenses. Furthermore, ectatic disorders like keratoconus may start manifesting and progressing in teenagers and thus knowledge of their normal CET profiles is essential to make CET-based early diagnostic algorithms.
The age groups formed in our study cross over from one decade of life to other and therefore are not representative of a particular age group decade. This is one of the limitations of our study. This distribution of the age groups was created because of our endeavor to include even the youngest children while maintaining a regular class interval of the age group. We do not believe that reclassifying the children according to chronological age group decades of life will have any major effect on the outcome of the study.
Conclusion
Our study accomplishes its objective of generating a normative database of CET values in normal Indian subjects. The values correlate well with data published by other studies from other parts of the world. Therefore, any future guidelines pertaining to diagnostic algorithms and treatment protocols, which are based on CET parameters, could be extrapolated to Indian subjects too.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Salomão MQ, Hofling-Lima AL, Lopes BT, Canedo ALC, Dawson DG, Carneiro-Freitas R, et al. Role of the corneal epithelium measurements in keratorefractive surgery. Curr Opin Ophthalmol. 2017;28:326–36. doi: 10.1097/ICU.0000000000000379. [DOI] [PubMed] [Google Scholar]
- 2.Kim WK, Kim BJ, Ryu I-H, Kim JK, Kim SW. Corneal epithelial and stromal thickness changes in myopic orthokeratology and their relationship with refractive change. PLoS ONE. 2018;13:e0203652. doi: 10.1371/journal.pone.0203652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kanellopoulos AJ, Asimellis G. In vivo three-dimensional corneal epithelium imaging in normal eyes by anterior-segment optical coherence tomography:A clinical reference study. Cornea. 2013;32:1493–8. doi: 10.1097/ICO.0b013e3182a15cee. [DOI] [PubMed] [Google Scholar]
- 4.Wu Y, Wang Y. Detailed distribution of corneal epithelial thickness and correlated characteristics measured with SD-OCT in myopic eyes. J Ophthalmol. 2017;2017:1018321. doi: 10.1155/2017/1018321. doi:10.1155/2017/1018321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Y, Tan O, Brass R, Weiss JL, Huang D. Corneal epithelial thickness mapping by Fourier-domain optical coherence tomography in normal and keratoconic eyes. Ophthalmology. 2012;119:2425–33. doi: 10.1016/j.ophtha.2012.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma Y, He X, Zhu X, Lu L, Zhu J, Zou H. Corneal epithelium thickness profile in 614 normal chinese children aged 7-15 years old. Sci Rep. 2016;6:23482. doi: 10.1038/srep23482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ma JX, Wang L, Weikert MP, Montes de Oca I, Koch DD. Evaluation of the repeatability and reproducibility of corneal epithelial thickness mapping for a 9-mm zone using optical coherence tomography. Cornea. 2019;38:67–73. doi: 10.1097/ICO.0000000000001806. [DOI] [PubMed] [Google Scholar]
- 8.Hashmani N, Hashmani S, Saad CM. Wide corneal epithelial mapping using an optical coherence tomography. Invest Ophthalmol Vis Sci. 2018;59:1652–8. doi: 10.1167/iovs.17-23717. [DOI] [PubMed] [Google Scholar]
- 9.Wang J, Aquavella J, Palakuru J, Chung S. Repeated measurements of dynamic tear distribution on the ocular surface after instillation of artificial tears. Invest Ophthalmol Vis Sci. 2006;47:3325–9. doi: 10.1167/iovs.06-0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Du C, Wang J, Cui L, Shen M, Yuan Y. Vertical and horizontal corneal epithelial thickness profiles determined by ultrahigh resolution optical coherence tomography. Cornea. 2012;31:1036–43. doi: 10.1097/ICO.0b013e31823f8d56. [DOI] [PMC free article] [PubMed] [Google Scholar]