Abstract
BACKGROUND:
Health disparities affect cancer incidence, treatment decisions, and adverse effects. Oncology providers may hold biases in the decision-making process, which can perpetuate health disparities.
OBJECTIVES:
The purpose of this article is to describe health disparities across treatment decisions and adverse effects, describe decision-making biases, and provide suggestions for nurses to mitigate adverse outcomes.
METHODS:
A scoping review of the literature was conducted.
FINDINGS:
Factors affecting health disparities stem, in part, from structural racism and decision-making biases, such as implicit bias, which occurs when individuals have unconscious negative thoughts or feelings toward a particular group. Other decision-making biases, seemingly unrelated to race, include default bias, delay discounting bias, and availability bias. Nurses and nurse navigators can mitigate health disparities by providing culturally appropriate care, assessing health literacy, providing education regarding adverse effects, serving as patient advocates, empowering patients, evaluating personal level of disease knowledge, and monitoring and managing cancer treatment adverse effects.
Keywords: decision-making, decision bias, treatment adverse effects, cancer survivorship
THERE ARE ROUGHLY 16.9 MILLION CANCER SURVIVORS living in the United States, and advances in cancer treatment have contributed to longer survival (American Cancer Society, 2021). Living longer, cancer survivors are experiencing adverse effects of cancer treatment, such as cancer pain and infertility, persisting years after treatment completion (National Comprehensive Cancer Network, 2020). However, cancer and its treatment have historically led to disparate outcomes for Black patients with cancer relative to White patients across cancer incidence, mortality, and adverse effects (American Cancer Society, 2019b). Health disparities are differences in cancer measures—such as incidence, treatment, and mortality—among cancer survivors from certain population groups (National Cancer Institute, 2015). The causes of health disparities are varied and occur at multiple levels of influence; however, when considering the patient–provider interaction, treatment decision-making can differ for Black patients compared to White patients (Nocon et al., 2020; Patel et al., 2015; Savitch et al., 2021), which, subsequently, may lead to disparities in which Black patients are more likely to suffer from adverse effects of cancer and its treatment (e.g., mortality and cancer-related morbidities) (Berkman et al., 2014; Collin et al., 2020; Connor et al., 2021; Pallok et al., 2019; Stein et al., 2016; Troeschel et al., 2019).
Despite increasing concerns about the adverse effects of cancer treatment, patients and oncology providers may hold biases in the decision-making process, such that the risk and/or management of adverse effects, toxicities, and late effects are not always appropriately or thoroughly considered in treatment decisions (Forman et al., 2010; Gillman et al., 2021; Henry et al., 2018; Koop et al., 2021; Peng et al., 2019; Shields et al., 2019). Decision-making biases combined with structural racism (i.e., embedded racial hierarchies in societal norms and institutional practices [Pallok et al., 2019]) may disproportionately affect Black patients with cancer and perpetuate health disparities.
This scoping review of the literature does the following:
Outlines how health disparities exist for treatment decisions and adverse effects of cancer treatment among Black patients with cancer
Describes how biases within treatment decision-making (such as implicit bias, default bias, delay discounting bias, availability bias) that are well-established in the psychological and decision science literature can perpetuate health disparities
Discusses implications of decision-making biases in oncology practice and the potential negative impact on Black patients with cancer
Clarifies the role of oncology nurses to mitigate consequences of decision-making biases
The following examples will focus broadly on cancer pain and infertility as adverse effects to provide context, but the authors acknowledge that the presented case scenarios are applicable to other adverse effects of cancer treatment.
Health Disparities in Cancer Survivorship
Cancer Incidence and Mortality
Health disparities and inequities affect cancer outcomes, from diagnosis and treatment to adverse effects of treatment. Overall, Black men and women have the highest mortality rate and shortest survival rate across all racial groups by most cancers (American Cancer Society, 2019b). For breast cancer, incidence rates for the non-Hispanic White population are relatively similar to the non-Hispanic Black population (131 per 100,000 versus 127 per 100,000); however, Black women have the highest breast cancer mortality rate across all racial and ethnic groups. Compared to White women, Black women are more likely to be diagnosed at a younger age, have nearly double the prevalence of triple-negative breast cancer, and are more likely to die of breast cancer within every age group (American Cancer Society, 2019a). Black men have higher incidence and mortality rates compared to White men for prostate cancer, stomach cancer, and colorectal cancer (American Cancer Society, 2019b). These health disparities in cancer incidence and mortality suggest that cancer treatment and screening advancements are not shared equally across all sociodemographic populations. High mortality rates among Black breast cancer survivors are largely attributable to differences in high-quality health care, unequal access to high-quality treatment, and poor access to prompt or timely treatment (American Cancer Society, 2019a; Cho et al., 2021; Green et al., 2018; Penner et al., 2012), which partially result from structural racism.
Cancer Treatment Decision-Making
Health disparities affect treatment decision-making for patients with cancer. Compared to White patients, Black survivors of acute myeloid leukemia are less likely to receive chemotherapy (Patel et al., 2015), Black prostate cancer survivors are less likely to receive cancer pelvic lymph node dissection (Hayn et al., 2011), and Black survivors of esophageal cancer and head and neck cancers are less likely to undergo surgery (Nocon et al., 2020; Savitch et al., 2021). Among women who should have received guideline-concordant adjuvant surgery for breast cancer, non-White patients were more likely than White patients to experience a system failure, defined as the treatment that was recommended but did not ensue (Bickell et al., 2007). Black patients also report receiving less information from their doctors about the rationale for treatment recommendations (Dovidio & Fiske, 2012; Lin & Kressin, 2015).
Cancer Adverse Effects
In addition to affecting treatment decisions, health disparities affect treatment-related adverse effects. More than one-third of patients with cancer experience pain after completion of cancer treatment, including neuropathic pain, chronic pain, skeletal pain, or post-radiation pain (National Comprehensive Cancer Network, 2020; Paice et al., 2016). However, Black patients are less likely to have pain assessed or managed, resulting in delays in pain treatment compared to White patients (Hoffman et al., 2016; Shavers et al., 2010; Stein et al., 2016). Some oncologists under-prescribe opioids for cancer pain and are less likely to prescribe opioids for Black patients with advanced cancer (Shields et al., 2019). Health disparities in cancer pain among cancer survivors are driven by both systemic issues (e.g., cost of pain medication, underinsured/uninsured, living in areas where pharmacies do not stock opioid pain medications) and provider-level barriers, including lack of formal training in pain management, communication, addiction/tolerance, and inadequate pain assessment (Anderson et al., 2009; Shavers et al., 2010; Stein et al., 2016). Clinical guidelines provide recommendations for treating pain among cancer survivors (National Comprehensive Cancer Network, 2020; Paice et al., 2016); however, inadequate pain management can lead to long-term consequences, including psychological distress and poor quality of life (National Comprehensive Cancer Network, 2020; Pachman et al., 2012). Other aspects of health disparities across adverse effects of cancer treatment include higher mortality from cardiovascular disease among Black breast cancer survivors (Troeschel et al., 2019) and less referrals and counseling for fertility preservation for Black women (Letourneau et al., 2012; Voigt et al., 2020) compared to White women.
Decision-Making Biases
Although decision-making is a shared process between patients and providers, it is important to acknowledge the role that oncologists and oncology healthcare providers have in facilitating the decisions, including providing sufficient information for treatment adverse effects, assessment and treatment of symptoms, and alternative cancer treatment options. It is evident that Black patients are more likely than White patients to experience negative consequences in cancer incidence, mortality, and adverse effects. These effects may be attributable, in part, to differences in provider treatment decision-making for Black patients.
Although multiple factors affect the decision-making process for patients’ cancer treatment selection (e.g., availability of treatment, drug costs, insurance coverage, clinical guidelines, patient preferences), discussions between oncology providers and patients are one important factor to consider. Of note, providers may rely on cognitive heuristics (or mental shortcuts) to simplify their decision-making. This is a natural human tendency; however, when heuristics are used improperly, they can lead to systematic biases in decision-making (Klein, Bloch, et al., 2014; O’Sullivan & Schofield, 2018). Decision-making biases, which are well-established in psychological and decision science literature, can occur among clinical medicine providers (O’Sullivan & Schofield, 2018) and affect treatment decision-making, with potential to contribute to disparities in the burden of adverse effects for Black patients with cancer. Table 1 summarizes decision-making biases, their definitions, and clinical examples.
TABLE 1.
DECISION-MAKING BIASES, DEFINITIONS, AND CLINICAL EXAMPLES
| CLINICAL EXAMPLE | ||
|---|---|---|
| Implicit | When individuals have nonconscious negative thoughts or feelings toward someone in a particular group (FitzGerald & Hurst, 2017) | Providers may unconsciously assume that certain patients cannot afford fertility preservation and may not discuss the option of fertility counseling prior to cancer treatment administration. |
| Default | When individuals make decisions that involve a default option or deciding to maintain the status quo (Jachimowicz et al., 2019) | Oncology providers may select non-opioid pain management as a default option, even if it is not the most effective for all patients. |
| Delay discounting | When providers or patients tend to favor immediate over delayed rewards, when given such an intertemporal choice (Chapman & Elstein, 1995) | This could occur when oncologists decide to use cancer treatments known to have adverse effects, such as infertility, without appropriate fertility preservation prior to treatment. |
| Availability | When individuals judge outcomes as more likely if they can retrieve greater instances of that outcome from memory (Tversky & Kahneman, 1973) | Oncologists and oncology nurses, who are exposed daily to the reality of a cancer diagnosis, may think of other diseases or late-occurring adverse effects comparatively less often, which could exacerbate availability biases related to cancer and reduce risk perceptions for other diseases (Klein, Ferrer, et al., 2014). |
Implicit Bias
Implicit bias may occur when individuals have unconscious negative thoughts or feelings toward someone in a particular group (e.g., of certain race or socioeconomic status) (FitzGerald & Hurst, 2017). For example, studies confirm that many individuals, including healthcare providers, unconsciously believe that Black patients can tolerate more pain than White patients and that these biases influence providers’ decision-making surrounding the treatment of pain (Hirsh et al., 2010; Hoffman et al., 2016; Mende-Siedlecki et al., 2019, 2021). In addition, previous studies demonstrated that implicit biases and stereotypical beliefs can affect the way that providers interact with patients—for example, one study found that non-Black providers use more anxiety-related words (e.g., worry, nervous, tense) when they interact with Black patients (Hagiwara et al., 2017), and another study reported that non-Black oncologists had shorter interactions with Black patients (Penner et al, 2016).
In the context of shared treatment decision-making, shorter or more negative interactions may mean that providers are not taking adequate time to explain the risks of treatment to their Black patients and can lead patients to be less informed about the treatment decision at hand—an assertion which is supported by the finding that Black patients report receiving less information about the reasoning behind treatment recommendations from their doctors (Lin & Kressin, 2015). In addition, implicit bias among healthcare providers is associated with negative patient outcomes (FitzGerald & Hurst, 2017; Hall et al., 2015; Meints et al., 2019; Zestcott et al., 2016), and a recent meta-analysis reported that 6 of 14 studies examining the role of implicit bias in healthcare outcomes identified a relationship between provider implicit bias and disparities in their treatment recommendations (Maina et al., 2018). In summation, the literature demonstrates that unconscious thoughts or implicit bias affect clinical interactions between oncology healthcare providers and Black patients, as well as the treatment decisions and health outcomes resulting from these interactions. Although the degree to which racial bias in clinical interactions specifically contributes to disparities in the burden of adverse effects of cancer treatment between Black and White patients has not been studied specifically, the extensive literature on racial bias in clinical interactions for other medical decisions supports the notion that bias in doctor–patient interactions may influence treatment decision-making in this context.
Other forms of cognitive bias and heuristics, seemingly unrelated to patient race, may impact treatment decision-making about cancer treatments with adverse effects. Potential decision-making biases and clinical tradeoffs regarding cardiotoxic cancer treatments were previously described (Gillman et al., 2021).
Default Bias
Default bias occurs when individuals make decisions that involve a default option or decide to maintain the status quo (Jachimowicz et al., 2019; Redelmeier & Shafir, 1995). If providers select non-opioid medications for cancer pain management, they may be responding to a default option for management of cancer pain (i.e., one that may be put in place in response to a desire to reduce prescription of opioids due to the opioid epidemic [Moo et al., 2020], even if it may not be the most effective for all patients).
Delay Discounting Bias
Delay discounting bias may occur when providers or patients tend to favor immediate over delayed outcomes, when given such an intertemporal choice (Chapman & Elstein, 1995). An example of an intertemporal choice that may be influenced by delay discounting bias is when oncologists decide whether to use cancer treatments known to have adverse effects, such as infertility after treatment completion; delay discounting bias would influence oncologists to place greater importance on the immediate outcome of aggressively treating cancer now versus the delayed reward of preventing adverse effects in the future.
Availability Bias
Availability bias may occur when providers judge outcomes as more likely if they are able to retrieve greater instances of that outcome from memory (Tversky & Kahneman, 1973).
Although these cognitive biases are not directly related to race, some research suggests that people may be more likely to use cognitive heuristics when making decisions about outgroup (e.g., those outside one’s racial, ethnic, gender, or nationality group) compared to ingroup members (Rothman & Hardin, 1997). Therefore, oncology providers may rely on these decision-making shortcuts to a greater extent when treating patients who are outside their own racial group (Hagiwara et al., 2017; Penner et al., 2016)—potentially exacerbating disparities in the burden of adverse effects. Presence of oncology provider biases can influence patient–provider communication regarding available treatment options, potential treatment-related toxicities, and late or long-term adverse effects, ultimately influencing the patient’s decision-making. Patients with cancer can experience uncertainty with treatment decisions, and insufficient communication can lead to decision conflict, decision regret, and poor decisional quality (Gustafson, 2017). In addition, research demonstrates that many members of the healthcare team, including physicians and nurses, use the same approach of addressing cultural beliefs regardless of race, ethnicity, and culture (Mott-Coles, 2014).
Implications for Nursing
Causes of health disparities across treatment decisions and adverse effects are multifactorial, with decision-making biases and racism serving as components of the cause; however, nurses can act toward reducing health disparities. To mitigate decision-making biases, oncology providers need continuing education to improve knowledge of default bias, delayed discounting bias, and availability bias, as well as implicit bias training to help with recognizing and preventing negative consequences for cancer survivors. Oncology nurses can also have decision-making biases, and a key focus of this article is to help educate nurses to acknowledge their own risk for decision-making biases and facilitate nurses’ ability to recognize when their colleagues may have biased decisions when caring for Black cancer survivors. In addition, nurses can play a role in reducing health disparities for cancer treatment-related adverse effects. Table 2 describes the role of nursing to recognize and mitigate health disparities.
TABLE 2.
MITIGATING HEALTH DISPARITIES: ADVERSE CANCER TREATMENT EFFECTS
| EXAMPLES TO REDUCE HEALTH DISPARITIES | |
|---|---|
| Culturally appropriate care | Nurses can provide culturally appropriate care and interventions by providing a welcoming and inclusive environment and using the cultural practices and behaviors to help improve the health of Black patients. In addition, community members who are familiar with pain management can act as advocates for patients or educate providers on culturally appropriate pain assessment (Anderson et al., 2009; Andrews & Boyle, 2002). |
| Assess health literacy | Nurses can assess patients’ health literacy and ensure patient comprehension of adverse effects to drive informed decision-making. Specifically, a teach-back method can help with ensuring patient understanding (Callaway et al., 2018; Scott et al., 2019). |
| Education, advocacy, and empowerment | Oncology nurses can facilitate patients’ desires to voice their preferences for cancer treatments and values in their care. For example, oncology nurses can help patients with cancer voice their desires for fertility preservation prior to chemotherapy initiation or embolden patients to contribute to shared decision-making regarding cancer treatments. |
| Knowledge of, monitoring, and management of cancer treatment adverse effects | Oncology nurse roles include monitoring and assessing adverse effects during cancer treatment and providing an additional layer of protection for medication and medication reconciliation. Oncology nurse practitioners should be aware of clinical guidelines related to major adverse effects, including management of cancer pain (National Comprehensive Cancer Network, 2020; Paice et al., 2016), cardiotoxicity (Armenian et al., 2017; Mehta et al., 2018), fertility preservation (Oktay et al., 2018), and other cancer survivorship–related issues as described in the National Comprehensive Cancer Network (2020) Survivorship Guidelines. |
| Oncology nurse navigators | Oncology nurse navigators are specialized nurses who can offer individualized assistance to patients with cancer and their families. In addition, they provide education and resources to facilitate informed decision-making and improve quality of care (Oncology Nursing Society, 2017). |
Culturally Appropriate Care
Providing culturally appropriate nursing care is crucial to mitigate health disparities. Cultural leverage is a focused strategy to provide culturally appropriate care and interventions by using cultural practices and behaviors to help improve the health of Black patients. Individuals from the community who are familiar with pain management can act as advocates for patients or educate providers on culturally appropriate pain assessment (Anderson et al., 2009; Andrews & Boyle, 2002). Nurses are well positioned to implement culturally appropriate nursing care to reduce health disparities and implicit bias for Black patients.
Education, Advocacy, and Empowerment
Nurses play a major role in patient education, advocacy, and empowerment to strengthen patients’ decision-making. Nurses can provide supporting information regarding cancer treatment and adverse effects, as well as signs and symptoms to monitor. Nurses can also assess patients’ health literacy, use the teach-back method, and ensure patient comprehension of adverse effects to drive informed decision-making (Callaway et al., 2018; Scott et al., 2019). By doing this, nurses act as patient advocates to help facilitate the patients’ autonomy during the cancer treatment decision-making process. In addition, nurses can help provide a voice to the patient’s needs and communicate wishes to the oncology team (Tariman & Szubski, 2015). Communication between the healthcare team and patient to increase informational and support needs can lead to patient empowerment and improve quality of life (Knobf, 2013). Patient education and advocacy, awareness of the potential decision-making biases, and the incorporation of cultural beliefs, can provide opportunities for nurses to conduct culturally tailored care and reduce disparities in adverse effects for Black patients with cancer. For patients with chronic cancer pain, oncology nurses should learn culturally appropriate methods for assessing pain among racially diverse patients and understand that patients may express pain differently than their own culture (Peacock & Patel, 2008). Figure 1 provides a case study example of how implicit bias may present itself regarding Black patients with cancer, as well as how nurses can help facilitate a welcoming and inclusive environment for appropriate pain assessment and pain management.
FIGURE 1.
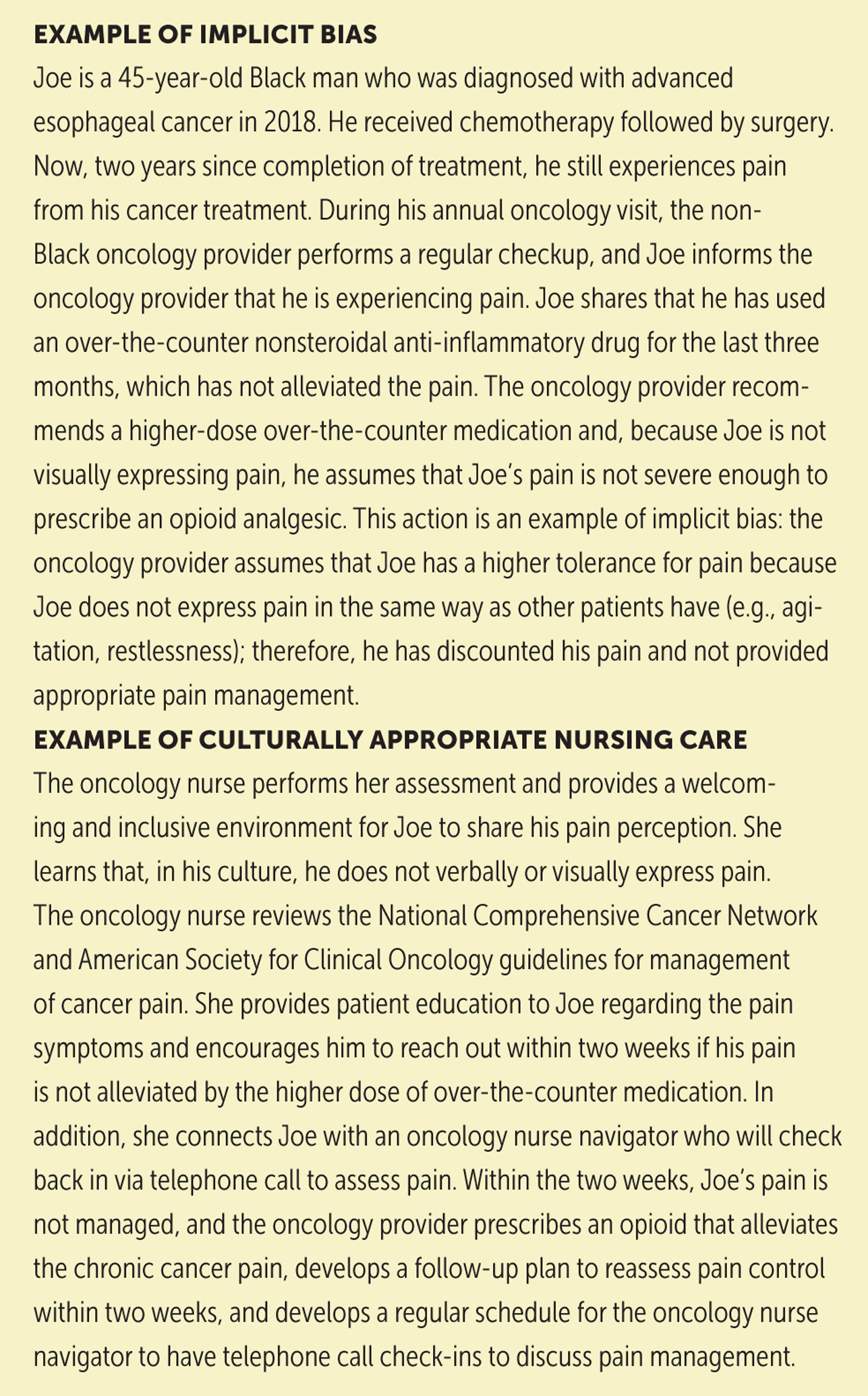
CASE STUDY
Monitoring and Management of Cancer Treatment Adverse Effects
Another important aspect of oncology nursing is the importance of monitoring and management of cancer treatment adverse effects (Tariman & Szubski, 2015). This is particularly important during the administration of chemotherapy. Nurses collect information and share with other team members, including adverse effects of the chemotherapy. However, nurses’ level of disease knowledge influences the degree of participation in cancer shared decision-making and monitoring and management of treatment adverse effects. Therefore, it is important for oncology nurses to be familiar with common treatment-related adverse effects and symptoms associated with cancer. Oncology nurse practitioners should be aware of clinical guidelines related to major adverse effects, including management of cancer pain (National Comprehensive Cancer Network, 2020; Paice et al., 2016), cardiotoxicity (Armenian et al., 2017; Mehta et al., 2018), fertility preservation (Oktay et al., 2018), and other cancer survivorship-related adverse effects as described in the National Comprehensive Cancer Network (2020) Survivorship Guidelines.
Role of Oncology Nurse Navigators
Oncology nurse navigators (ONNs) are specialized nurses who offer individualized assistance to patients with cancer and their families, provide education and resources to facilitate informed decision-making, and improve quality of care (Oncology Nursing Society, 2017). They help through collaboration with various members of the oncology team (oncologists, advanced practitioners, and clinical oncology nurses) by using patient-reported outcomes tools to screen patients before starting treatment to better understand their knowledge of their disease, provide education prior to their initial treatment, and follow patients closely from diagnosis into survivorship. The ONN brings an added layer of coordination and support, which is invaluable for the patients’ informed decision-making in treatment and beyond, and potentially alleviates health disparities within adverse effects from cancer treatment (Oncology Nursing Society, 2017).
Finally, as structural racism has begotten health disparities, including among cancer populations (Ellis et al., 2018), nurses should be educated on the impact of structural racism, ways in which to mitigate its effects, and the role of research and implementation to reduce implicit bias (i.e., developing effective implicit bias training or testing other training tools that can change practice). As the authors presented in this article, there are a multitude of structural racism effects on cancer outcomes. Ongoing training is warranted to address such effects in a culturally sensitive manner. Nurses can apply principles of cultural humility in each patient encounter, acknowledging that patients identifying as Black are individuals with unique needs and concerns that must be addressed. In addition, there is a need for significant emphasis on identifying provider best practices that yield optimal patient results and reduce cancer health disparities.
Conclusion
Nurses should be aware of decision-making biases, their own or others, that may present during shared decision-making, intervene when appropriate, and be an active participant in shared decision-making to help mitigate health disparities across adverse treatment effects. Oncology nurses can ensure that patients understand the major adverse effects and that the patients’ wishes, particularly Black patients who are disproportionately affected by cancer, are heard and met. Importantly, oncology nurses, ONNs, and nurse practitioners should be patient advocates, ensuring that patients obtain the appropriate care and facilitate screening measures, assessing risk factors and symptoms, providing culturally appropriate care, and empowering patients to make informed decisions, which ultimately transform care delivery toward equitable healthcare.
IMPLICATIONS FOR PRACTICE.
Understand that health disparities exist related to cancer and its treatment, which have historically led to disparate outcomes for Black patients. This is a crucial step toward equitable care.
Acknowledge that treatment decision-making biases may perpetuate health disparities among cancer survivors, and these biases include implicit bias, default bias, delay discounting bias, and availability bias.
Learn about the potential for decision-making biases, develop an understanding of adverse effects, actively participate in shared decision-making, and conduct culturally appropriate care to mitigate health disparities across adverse treatment effects.
Acknowledgments
The authors take full responsibility for this content. Funding was provided by the National Cancer Institute (K08CA245208 [Nolan]). The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias.
Contributor Information
Jacqueline B. Vo, Cancer Prevention Fellowship Program and the Radiation Epidemiology Branch in the Division of Cancer Epidemiology and Genetics, both at the National Cancer Institute in Bethesda, MD;.
Arielle Gillman, Cancer Prevention Fellowship Program and the Basic Biobehavioral and Psychological Sciences Branch in the Behavioral Research Program in the Division of Cancer Control and Population Sciences, both at the National Cancer Institute;.
Kelsey Mitchell, University of Alabama at Birmingham Hospital;.
Timiya S. Nolan, College of Nursing at the Ohio State University in Columbus..
REFERENCES
- American Cancer Society. (2019a). Breast cancer facts and figures 2019–2020. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf
- American Cancer Society. (2019b). Cancer facts and figures for African Americans 2019–2021. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-african-americans/cancer-facts-and-figures-for-african-americans-2019-2021.pdf
- American Cancer Society. (2021). Cancer facts and figures 2021. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2021/cancer-facts-and-figures-2021.pdf
- Anderson KO, Green CR, & Payne R (2009). Racial and ethnic disparities in pain: Causes and consequences of unequal care. Journal of Pain, 10(12), 1187–1204. [DOI] [PubMed] [Google Scholar]
- Andrews MM, & Boyle JS (2002). Transcultural concepts in nursing care. Journal of Transcultural Nursing, 13(3), 178–180. [DOI] [PubMed] [Google Scholar]
- Armenian SH, Lacchetti C, Barac A, Carver J, Constine LS, Denduluri N, … Lenihan D (2017). Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. Journal of Clinical Oncology, 35(8), 893–911. 10.1200/JCO.2016.70.5400 [DOI] [PubMed] [Google Scholar]
- Berkman AF, Cole B, Ades PA, Dickey S, Higgins ST, Trentham-Dietz A, … Lakoski SG (2014). Racial differences in breast cancer, cardiovascular disease, and all-cause mortality among women with ductal carcinoma in situ of the breast. Breast Cancer Research and Treatment, 148(2), 407–413. 10.1007/s10549-014-3168-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickell NA, LePar F, Wang JJ, & Leventhal H (2007). Lost opportunities: Physicians’ reasons and disparities in breast cancer treatment. Journal of Clinical Oncology, 25(18), 2516–2521. [DOI] [PubMed] [Google Scholar]
- Callaway C, Cunningham C, Grover S, Steele K, McGlynn A, & Sribanditmongkol V (2018). Patient handoff processes: Implementation and effects of bedside handoffs, the teach-back method, and discharge bundles on an inpatient oncology unit. Clinical Journal of Oncology Nursing, 22(4), 421–428. 10.1188/18.CJON.421-428 [DOI] [PubMed] [Google Scholar]
- Chapman GB, & Elstein AS (1995). Valuing the future: Temporal discounting of health and money. Medical Decision Making, 15(4), 373–386. [DOI] [PubMed] [Google Scholar]
- Cho B, Han Y, Lian M, Colditz GA, Weber JD, Ma C, & Liu Y (2021). Evaluation of racial/ethnic differences in treatment and mortality among women with triple-negative breast cancer. JAMA Oncology, 7(7), 1016. 10.1001/jamaoncol.2021.1254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collin LJ, Troeschel AN, Liu Y, Gogineni K, Borger K, Ward KC, & McCullough LE (2020). A balancing act: Racial disparities in cardiovascular disease mortality among women diagnosed with breast cancer. Annals of Cancer Epidemiology, 4, 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor AE, Schmaltz CL, Jackson-Thompson J, & Visvanathan K (2021). Comorbidities and the risk of cardiovascular disease mortality among racially diverse patients with breast cancer. Cancer, 127(15), 2614–2622. 10.1002/cncr.33530 [DOI] [PubMed] [Google Scholar]
- Dovidio JF, & Fiske ST (2012). Under the radar: How unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. American Journal of Public Health, 102(5), 945–952. 10.2105/AJPH.2011.300601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis L, Canchola AJ, Spiegel D, Ladabaum U, Haile R, & Gomez SL (2018). Racial and ethnic disparities in cancer survival: The contribution of tumor, sociodemographic, institutional, and neighborhood characteristics. Journal of Clinical Oncology, 36(1), 25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FitzGerald C, & Hurst S (2017). Implicit bias in healthcare professionals: A systematic review. BMC Medical Ethics, 18(1), 19. 10.1186/s12910-017-0179-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman EJ, Anders CK, & Behera MA (2010). A nationwide survey of oncologists regarding treatment-related infertility and fertility preservation in female cancer patients. Fertility and Sterility, 94(5), 1652–1656. 10.1016/j.fertnstert.2009.10.008 [DOI] [PubMed] [Google Scholar]
- Gillman AS, Vo JB, Nohria A, & Ferrer RA (2021). Decision science can inform clinical trade-offs regarding cardiotoxic cancer treatments. JNCI Cancer Spectrum, pkab053. 10.1093/jncics/pkab053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green AK, Aviki EM, Matsoukas K, Patil S, Korenstein D, & Blinder V (2018). Racial disparities in chemotherapy administration for early-stage breast cancer: A systematic review and meta-analysis. Breast Cancer Research and Treatment, 172, 247–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson A (2017). Reducing patient uncertainty: Implementation of a shared decision-making process enhances treatment quality and provider communication. Clinical Journal of Oncology Nursing, 21(1), 113–115. 10.1188/17.CJON.113-115 [DOI] [PubMed] [Google Scholar]
- Hagiwara N, Slatcher RB, Eggly S, & Penner LA (2017). Physician racial bias and word use during racially discordant medical interactions. Health Communication, 32(4), 401–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, … Coyne-Beasley T (2015). Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: A systematic review. American Journal of Public Health, 105(12), e60–e76. 10.2105/AJPH.2015.302903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayn MH, Orom H, Shavers VL, Sanda MG, Glasgow M, Mohler JL, & Underwood W (2011). Racial/ethnic differences in receipt of pelvic lymph node dissection among men with localized/regional prostate cancer: Race differences in PLND Receipt. Cancer, 117(20), 4651–4658. 10.1002/cncr.26103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry ML, Niu J, Zhang N, Giordano SH, & Chavez-MacGregor M (2018). Cardiotoxicity and cardiac monitoring among chemotherapy-treated breast cancer patients. JACC: Cardiovascular Imaging, 11(8), 1084–1093. 10.1016/j.jcmg.2018.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsh AT, Jensen MP, & Robinson ME (2010). Evaluation of nurses’ self-insight into their pain assessment and treatment decisions. Journal of Pain, 11(5), 454–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman KM, Trawalter S, Axt JR, & Oliver MN (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proceedings of the National Academy of Sciences, 113(16), 4296–4301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jachimowicz JM, Duncan S, Weber EU, & Johnson EJ (2019). When and why defaults influence decisions: A meta-analysis of default effects. Behavioural Public Policy, 3(2), 159–186. 10.1017/bpp.2018.43 [DOI] [Google Scholar]
- Klein WMP, Bloch M, Hesse BW, McDonald PG, Nebeling L, O’Connell ME, … Tesauro G (2014). Behavioral research in cancer prevention and control. American Journal of Preventive Medicine, 46(3), 303–311. 10.1016/j.amepre.2013.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein WMP, Ferrer RA, Graff KA, Kaufman AR, & Han PKJ (2014). Perceived ambiguity, fatalism, and believing cancer is more prevalent than heart disease. American Journal of Preventive Medicine, 46(4), e45–e47. 10.1016/j.amepre.2014.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knobf MT (2013). Being prepared: Essential to self-care and quality of life for the person with cancer. Clinical Journal of Oncology Nursing, 17(3), 255–261. [DOI] [PubMed] [Google Scholar]
- Koop Y, Dobbe L, Maas AHEM, van Spronsen DJ, Atsma F, El Messaoudi S, & Vermeulen H (2021). Oncology professionals’ perspectives towards cardiac surveillance in breast cancer patients with high cardiotoxicity risk: A qualitative study. PLOS ONE, 16(3), e0249067. 10.1371/journal.pone.0249067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letourneau JM, Smith JF, Ebbel EE, Craig A, Katz PP, Cedars MI, & Rosen MP (2012). Racial, socioeconomic, and demographic disparities in access to fertility preservation in young women diagnosed with cancer: Fertility preservation disparities. Cancer, 118(18), 4579–4588. 10.1002/cncr.26649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin MY, & Kressin NR (2015). Race/ethnicity and Americans’ experiences with treatment decision making. Patient Education and Counseling, 98(12), 1636–1642. 10.1016/j.pec.2015.07.017 [DOI] [PubMed] [Google Scholar]
- Maina IW, Belton TD, Ginzberg S, Singh A, & Johnson TJ (2018). A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Social Science and Medicine, 199, 219–229. 10.1016/j.socscimed.2017.05.009 [DOI] [PubMed] [Google Scholar]
- Mehta LS, Watson KE, Barac A, Beckie TM, Bittner V, Cruz-Flores S, … Santos Volgman A (2018). Cardiovascular disease and breast cancer: Where these entities intersect: A scientific statement from the American Heart Association. Circulation, 137(8), 30–66. 10.1161/CIR.0000000000000556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meints SM, Cortes A, Morais CA, & Edwards RR (2019). Racial and ethnic differences in the experience and treatment of noncancer pain. Pain Management, 9(3), 317–334. 10.2217/pmt-2018-0030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mende-Siedlecki P, Lin J, Ferron S, Gibbons C, Drain A, & Goharzad A (2021). Seeing no pain: Assessing the generalizability of racial bias in pain perception. Emotion. Advance online publication. 10.1037/emo0000953 [DOI] [PubMed] [Google Scholar]
- Mende-Siedlecki P, Qu-Lee J, Backer R, & Van Bavel JJ (2019). Perceptual contributions to racial bias in pain recognition. Journal of Experimental Psychology: General, 148(5), 863–889. 10.1037/xge0000600 [DOI] [PubMed] [Google Scholar]
- Moo TA, Pawloski KR, Sevilimedu V, Charyn J, Simon BA, Sclafani LM, … Morrow M (2020). Changing the default: A prospective study of reducing discharge opioid prescription after lumpectomy and sentinel node biopsy. Annals of Surgical Oncology, 27(12), 4637–4642. 10.1245/s10434-020-08886-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mott-Coles S (2014). Patients’ cultural beliefs in patient-provider communication with African American women and Latinas diagnosed with breast cancer. Clinical Journal of Oncology Nursing, 18(4), 443–448. 10.1188/14.CJON.443-448 [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. (2015). Cancer health disparities definitions and examples. U.S. Department of Health and Human Services, National Institutes of Health. https://www.cancer.gov/about-nci/organization/crchd/about-health-disparities/definitions [Google Scholar]
- National Comprehensive Cancer Network. (2020). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Survivorship [v.2.2020]. https://www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf
- Nocon CC, Ajmani GS, & Bhayani MK (2020). A contemporary analysis of racial disparities in recommended and received treatment for head and neck cancer. Cancer, 126(2), 381–389. 10.1002/cncr.32342 [DOI] [PubMed] [Google Scholar]
- Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, … Loren AW (2018). Fertility preservation in patients with cancer: ASCO clinical practice guideline update. Journal of Clinical Oncology, 36(19), 1994–2001. [DOI] [PubMed] [Google Scholar]
- Oncology Nursing Society. (2017). 2017 oncology nurse navigator core competencies. https://www.ons.org/sites/default/files/2017-05/2017_Oncology_Nurse_Navigator_Competencies.pdf
- O’Sullivan E, & Schofield SJ (2018). Cognitive bias in clinical medicine. Journal of the Royal College of Physicians of Edinburgh, 48(3), 225–232. 10.4997/JRCPE.2018.306 [DOI] [PubMed] [Google Scholar]
- Pachman DR, Barton DL, Swetz KM, & Loprinzi CL (2012). Troublesome symptoms in cancer survivors: Fatigue, insomnia, neuropathy, and pain. Journal of Clinical Oncology, 30(30), 3687–3696. 10.1200/JCO.2012.41.7238 [DOI] [PubMed] [Google Scholar]
- Paice JA, Portenoy R, Lacchetti C, Campbell T, Cheville A, Citron M, … Bruera E (2016). Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. Journal of Clinical Oncology, 34(27), 3325–3345. 10.1200/JCO.2016.68.5206 [DOI] [PubMed] [Google Scholar]
- Pallok K, De Maio F, & Ansell DA (2019). Structural racism—A 60-year-old Black woman with breast cancer. New England Journal of Medicine, 380(16), 1489–1493. [DOI] [PubMed] [Google Scholar]
- Patel MI, Ma Y, Mitchell B, & Rhoads KF (2015). How do differences in treatment impact racial and ethnic disparities in acute myeloid leukemia? Cancer Epidemiology Biomarkers and Prevention, 24(2), 344–349. 10.1158/1055-9965.EPI-14-0963 [DOI] [PubMed] [Google Scholar]
- Peacock S, & Patel S (2008). Cultural influences on pain. Reviews in Pain, 1(2), 6–9. 10.1177/204946370800100203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng J, Rushton M, Johnson C, Brezden-Masley C, Sulpher J, Chiu MG, … Dent S (2019). An international survey of healthcare providers’ knowledge of cardiac complications of cancer treatments. Cardio-Oncology, 5, 12. 10.1186/s40959-019-0049-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Dovidio JF, Gonzalez R, Albrecht TL, Chapman R, Foster T, … Eggly S (2016). The effects of oncologist implicit racial bias in racially discordant oncology interactions. Journal of Clinical Oncology, 34(24), 2874–2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Eggly S, Griggs JJ, Underwood W, Orom H, & Albrecht TL (2012). Life-threatening disparities: The treatment of Black and White cancer patients. Journal of Social Issues, 68(2), 328–357. 10.1111/j.1540-4560.2012.01751.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redelmeier DA, & Shafir E (1995). Medical decision making in situations that offer multiple alternatives. JAMA, 273(4), 302–305. 10.1001/jama.1995.03520280048038 [DOI] [PubMed] [Google Scholar]
- Rothman AJ, & Hardin CD (1997). Differential use of the availability heuristic in social judgment. Personality and Social Psychology Bulletin, 23(2), 123–138. [Google Scholar]
- Savitch SL, Grenda TR, Scott W, Cowan SW, Posey J, Mitchell EP, … Evans NR (2021). Racial disparities in rates of surgery for esophageal cancer: A study from the National Cancer Database. Journal of Gastrointestinal Surgery, 25(3), 581–592. [DOI] [PubMed] [Google Scholar]
- Scott C, Andrews D, Bulla S, & Loerzel V (2019). Teach-back method: Using a nursing education intervention to improve discharge instructions on an adult oncology unit. Clinical Journal of Oncology Nursing, 23(3), 288–294. 10.1188/19.CJON.288-294 [DOI] [PubMed] [Google Scholar]
- Shavers VL, Bakos A, & Sheppard VB (2010). Race, ethnicity, and pain among the U.S. adult population. Journal of Health Care for the Poor and Underserved, 21(1), 177–220. [DOI] [PubMed] [Google Scholar]
- Shields CG, Griggs JJ, Fiscella K, Elias CM, Christ SL, Colbert J, … Epstein RM (2019). The influence of patient race and activation on pain management in advanced lung cancer: A randomized field experiment. Journal of General Internal Medicine, 34(3), 435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein KD, Alcaraz KI, Kamson C, Fallon EA, & Smith TG (2016). Sociodemographic inequalities in barriers to cancer pain management: A report from the American Cancer Society’s Study of Cancer Survivors-II (SCS-II): Inequalities in cancer pain management. Psycho-Oncology, 25(10), 1212–1221. 10.1002/pon.4218 [DOI] [PubMed] [Google Scholar]
- Tariman J, & Szubski K (2015). The evolving role of the nurse during the cancer treatment decision-making process: A literature review. Clinical Journal of Oncology Nursing, 19(5), 548–556. 10.1188/15.CJON.548-556 [DOI] [PubMed] [Google Scholar]
- Troeschel AN, Liu Y, Collin LJ, Bradshaw PT, Ward KC, Gogineni K, & McCullough LE (2019). Race differences in cardiovascular disease and breast cancer mortality among US women diagnosed with invasive breast cancer. International Journal of Epidemiology, 48(6), 1897–1905. 10.1093/ije/dyz108 [DOI] [PubMed] [Google Scholar]
- Tversky A, & Kahneman D (1973). Availability: A heuristic for judging frequency and probability, 5(2), 207–232. 10.1016/0010-0285(73)90033-9 [DOI] [Google Scholar]
- Voigt PE, Blakemore JK, McCulloh D, & Fino ME (2020). Equal opportunity for all? An analysis of race and ethnicity in fertility preservation in New York City. Journal of Assisted Reproduction and Genetics, 37(12), 3095–3102. 10.1007/s10815-020-01980-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zestcott CA, Blair IV, & Stone J (2016). Examining the presence, consequences, and reduction of implicit bias in health care: A narrative review. Group Processes and Intergroup Relations, 19(4), 528–542. 10.1177/1368430216642029 [DOI] [PMC free article] [PubMed] [Google Scholar]


