Abstract
The COVID-19 pandemic caused by the novel coronavirus SARS-CoV-2 (2019-nCoV) has devastated global healthcare and economies. Despite the stabilization of infectivity rates in some developed nations, several countries are still under the grip of the pathogenic viral mutants that are causing a significant increase in infections and hospitalization. Given this urgency, targeting of key host factors regulating SARS-CoV-2 life cycle is postulated as a novel strategy to counter the virus and its associated pathological outcomes. In this regard, Poly (ADP)-ribose polymerase-1 (PARP-1) is being increasingly recognized as a possible target. PARP-1 is well studied in human diseases such as cancer, central nervous system (CNS) disorders and pathology of RNA viruses. Emerging evidence indicates that regulation of PARP-1 by non-coding RNAs such as microRNAs is integral to cell survival, redox balance, DNA damage response, energy homeostasis, and several other cellular processes. In this short perspective, we summarize the recent findings on the microRNA/PARP-1 axis and its therapeutic potential for COVID-19 pathologies.
Keywords: COVID-19, PARP-1, miRNA, therapeutics, drug repurposing, neuropathology, RNA viruses, SARS-CoV-2
1. Introduction
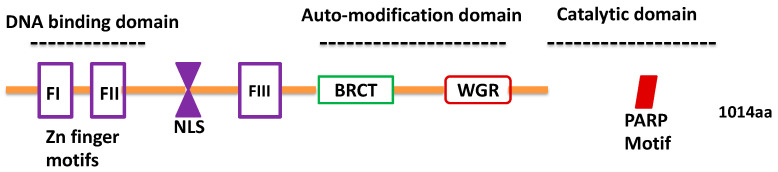
The rapidly evolving coronavirus disease (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), presents an urgent and unmet clinical need for novel therapeutics [1,2]. This effort requires a clear understanding of the role of host cell factors that aid in the viral life cycle. This knowledge will pave the way for efficient drug repurposing and novel therapeutic strategies. One such host factor that has caught considerable attention is Poly (ADP)-ribose polymerase-1 (PARP-1) [3,4,5,6]. PARP-1 is a multi-domain enzyme that utilizes cellular NAD+ to catalyze the synthesis of poly (ADP) ribose (PAR) residues following its transfer onto target proteins by a mechanism known as PARylation [7,8,9]. PARP-1 belongs to the PARP/ARTD family of enzymes that constitutes 17 isoforms in humans (PARP-1–PARP-17) [10]. It is a highly conserved enzyme with a molecular mass of 116 kDa [7] that predominantly localizes in the nucleus. PARP-1 multi-domain unit comprises the amino (N) terminal DNA binding domain (DBD), a central auto-modification domain (AMD), Zn binding domain (FIII/Zn3), and a carboxyl (C) terminal catalytic domain [11], as illustrated in Figure 1 [12,13,14]. Among the different isoforms, PARP-1 is predominantly responsible for 85–90% of cellular PARP activity; PARP-2 is responsible for 10–15%; and the remainder of the enzymes contribute to the remainder of PARP activity [8,15]. Like the PARP-1 function, recent studies have highlighted the role of PARP-2 in response to DNA damage, genome maintenance, metabolic regulation, and oxidative stress [16,17]. Alteration in PARP-1 activity has been reported in several diseases including viral pathogenesis [9,18]. For instance, interferon-stimulated genes (ISGs), which are members of the PARP superfamily, have been implicated in the restriction of viral replication. However, the exact mechanisms underlying the antiviral response of the PARP superfamily of proteins are not clearly understood [19,20]. This is because several viruses harbor the machinery to modulate PARP function, implying that PARP-mediated signaling can be both anti- and pro-viral in a context-dependent manner [20,21]. However, with regards to coronavirus species, a recent study reported that SARS-CoV-2 infection strikingly induced activity of PARPs, along with expression of genes encoding enzymes for salvage NAD synthesis from nicotinamide and nicotinamide riboside, while simultaneously downregulating other NAD utilizing biosynthetic pathways [4,10,13,22].
Figure 1.
Structure of Poly (ADP)-ribose polymerase-1 (PARP-1). The N terminus of PARP-1 contains the DNA-binding domain (DBD) constituting two zinc-finger motifs and a bipartite nuclear localization signal (NLS). The auto-modification domain constitutes a breast cancer (BRCA) C-terminus-like (BRCT) interaction domain and the Tryptophan-Glycine-Arginine (WGR) domain that mediates interactions with self or protein partners. PARP-1 has a catalytic domain at its C’ terminus, within which is contained its Poly (ADP)-ribosylation polymerase (PARP) signature motif that catalyzes Poly (ADP)-ribosylation (i.e., PARylation) reactions using intracellular nicotinamide adenine dinucleotide (NAD+) as a donor of ADP-ribose.
PARP-1 is a multi-functional enzyme, which depends on specific interactions with DNA, nucleosomes, or chromatin-associated proteins [11,22,23,24]. PARP-1-mediated PARylation of proteins is a key post-translational modification that leads to a series of molecular signaling cascades involving ATP and co-factor NAD+ [25]. In addition, PARP-1 undergoes auto-modification, i.e., auto-PARylation, marked by the addition of ADP-ribose chains ranging from 20 to more than 200 units in length, that inhibit its DNA binding ability and regulate its catalytic activity [7]. Thus, PARylation is a critical determinant for direct (autocrine) and indirect (paracrine) molecular signaling that is dependent on PARP-1 function. In this perspective, we summarize and discuss two important questions pertaining to the miRNA-mediated regulation of PARP-1 in the context of COVID-19 pathogenesis. First, how relevant is PARP-1’s activity across cell/tissue types in SARS-CoV-2 pathogenesis and second, can miRNA-mediated regulation of PARP-1 be exploited as a therapeutic target to prevent SARS-CoV-2 infection to mitigate COVID-19 pathological outcomes?
2. PARP-1 in Viral Pathology
Emerging evidence highlights the role of the PARP family of proteins, and specifically PARP-1, as a potential therapeutic target for COVID-19 [3,4,5,6]. Various small molecule inhibitors targeting PARP-1′s enzymatic activity are available and have been extensively studied. Currently, these inhibitors are under investigation in clinical trials for several cancer types and associated disorders [26,27]. Unfortunately, only a limited number of studies have discussed the repurposing of PARP1 inhibitors in other disease models (e.g., inflammatory or viral diseases). Given the ability of PARP proteins to bind nucleic acids, several members of the PARP family have been shown to impact host–virus interactions. In particular, these proteins affect a number of steps of the viral life cycle (integration, recombination, and transcription) suggesting potential pro- and antiviral properties of PARP proteins [20,28,29]. Although these findings are primarily reported for other RNA viruses, such as influenza and porcine reproductive and respiratory syndrome viruses (PRSSV), the effect of PARP-1 and other PARP proteins on coronavirus species cannot be ignored. In general, studies have highlighted that PARP-1 inhibitors may be useful therapeutic targets for viral infections [5,6]. However, the drug doses optimized for treating cancers may be insufficient to treat viral infection and pathogenesis. Hence, there is an urgent need for research to understand the impact of drugs targeting PARP1 on viral pathogenesis, specifically investigation of the direct role of PARP-1 and SARS-CoV-2 life cycle and pathology.
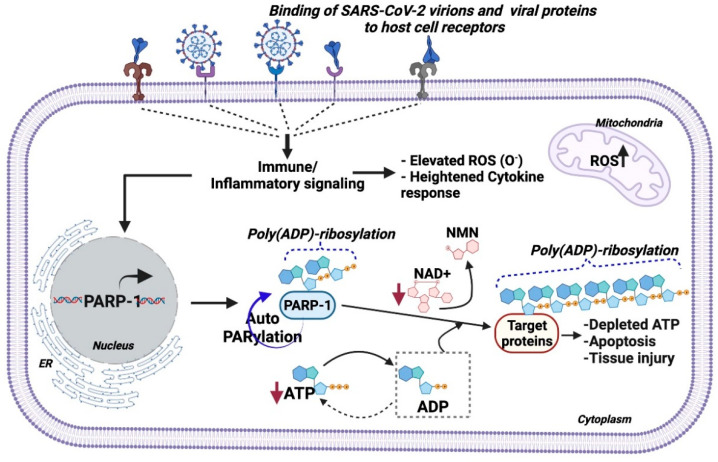
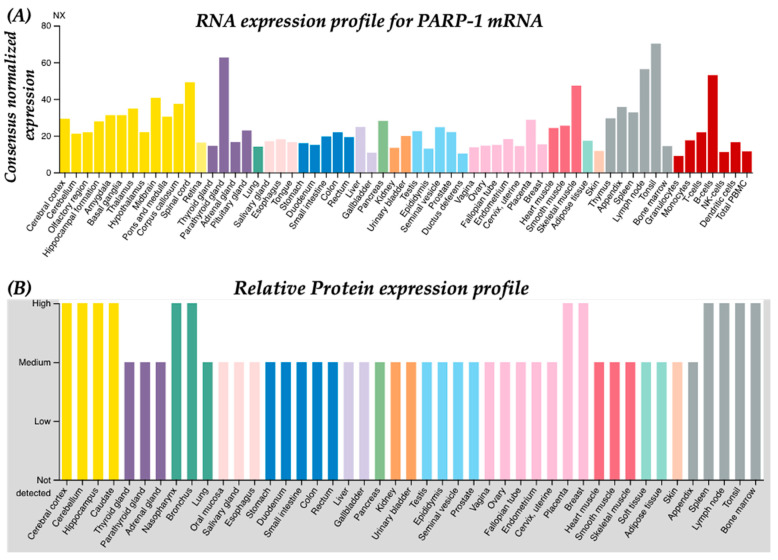
As illustrated in Figure 2, in SARS-CoV-2 infection, both viral proteins and virions in circulation bind to cell surface receptors (e.g., ACE2 and TLRs) and activate immune response cascades (e.g., pro-inflammatory cytokines such as IL6), in addition to increasing mitochondrial reactive oxygen species (ROS) and impairing redox balance, followed by PARP-1-induced PARylation of downstream targets, which results in depletion of intracellular ATP levels causing cellular apoptosis and tissue injury [30,31,32]. Viruses require an intracellular ATP pool to maintain their life cycle in the host cell [33,34]. Viral replication is dependent on nicotinamide adenine dinucleotide (NAD) coenzymes and redox factors such as NAD+, NADH, NADP+, and NADPH, which are central to cellular metabolism [35]. Primarily, these coenzymes regulate electron (e−) exchange in essential metabolic processes and scavenging of intracellular ROS generated during the infectivity cycle. It is well established that metabolic stresses, including obesity, type 2 diabetes [36], smoking [37], heart failure [38], hypertension [39], nerve damage [40], and brain injury [41], deplete intracellular ATP and NAD+ in affected tissues with a dramatic induction of ROS and PARP-1 expression. Induced ROS levels also result in depleted NAD+ levels and an impaired antioxidant system, following inflammatory triggers (cytokine response and cellular activation/adhesion markers) that are hallmarks of aging, hypertension, diabetes, and obesity [42,43,44,45]. Despite this importance, the direct roles of these coenzymes in viral replication and antiviral defenses remain largely unexplored. Strikingly, PARP-1 is recognized as a master regulator of intracellular NAD+ and ATP pools. In this context, we showed that PARP-1-mediated PARylation of nuclear p53 maintains the intracellular ATP pool via transactivation of Proline oxidase (POX) mRNA [46]. With regards to diseases, studies have shown that increased age-associated lower NAD+ and increased ROS levels serve as strong predictors of SARS-CoV-2-associated in-hospital mortality [47,48]. A recent laboratory investigation revealed that non-canonical PARP isozyme (PARP-10) having an affinity for NAD+ was consistently upregulated by SARS-CoV infection [4]. Moreover, the abundant expression of PARP-1 across tissue types (Figure 3) implies functional significance in diseased conditions. Based on these observations, we postulate that deficiency of NAD+ due to increased PARP activation may be a key factor related to the SARS-CoV-2 associated disease spectrum. Oxidative stress induces PARP1, whose hyper activation depletes NAD+ and ATP levels, culminating in energy loss and subsequent cell death [49,50,51]. Overall, these processes enhance pro-inflammatory signaling. Hence, regulating the levels/activity of PARP-1 may serve as an important factor to maintain basal intracellular NAD+ levels and restore redox balance without inducing immune dysfunction. The supplementation of NAD+ or precursors is hypothesized to minimize disease severity in COVID-19 patients. Nevertheless, the significance of this hypothesis needs experimental and clinical validation.
Figure 2.
Model for PARP-1 activation in SARS-CoV-2 pathogenesis. Systemic inflammation in SARS-CoV-2 pathogenesis induces immune signaling in cells causing elevated mitochondrial ROS and cytokine response, which triggers PARP-1 transcription and activity. Thereafter, PARP-1 activation PARylates self (autoPARylation) or downstream protein targets by adding Poly (ADP)-ribose residues in a NAD+ dependent manner. Sustained PARylation events under diseased and inflammatory conditions cause declines in intracellular ATP and NAD+ pools, which leads to metabolic dysfunction and cell death, followed by tissue injury, as reported in COVID-19 pathology.
Figure 3.
PARP-1 is expressed in all tissue types. (A) Normalized RNA expression profile for PARP-1 mRNA across human tissues. (B) Relative protein expression profile for PARP-1 across human tissues. These figures are obtained from the publicly available human protein and cell type atlas at proteinatlas.org. Details of data analysis, annotation, and normalization can be obtained at https://www.proteinatlas.org/ENSG00000143799-PARP1/tissue (accessed on 17 September 2021).
Interferon signaling induces the PARP family of proteins (e.g., PARP-9, PARP-10, PARP-12, and PARP-14) causing inhibition of ADP-ribosylation, a mechanism that is presumed to impact viral translation [28,29]. In parallel, it should be noted that the conserved macro domain of SARS-CoV species suppresses host interferon and immune response to facilitate viral replication [28,29]. Regulation of PARP-1 expression and activity is shown to be important in cancer, cell metabolism, stress response, DNA damage, and neuronal differentiation and signaling, in addition to drug abuse [18,52,53,54]. Similarly, other studies have also established the regulation of PARP-1 in several disease conditions, including hypertension, obesity, and inflammation [50,55,56,57].
We have also reported the in vivo and in vitro implications of post-transcriptional mechanisms regulating PARP-1 in the context of neuronal function [52,53]. Employing molecular and biochemical approaches, we established the role of cellular microRNAs miR-124 and miR-125b in the regulation of PARP-1 mRNA in neurons [52,53]. miRNAs are small non-coding RNAs that post-transcriptionally regulate gene expression by binding to 3′-UTR of mRNAs. Although several pieces of evidence exist for the binding of miRNAs to 5′-UTR, and the open reading frame (ORF) of mRNAs to induce post-transcriptional events [57,58,59,60], miRNAs have been shown to be important in the regulation of PARP-1 in various physiological and pathological conditions (Table 1). As presented in Table 1, several of these diseases involving regulation of PARP-1 have been well documented as risk factors for COVID-19-associated mortality and hospitalizations, thus highlighting the plausible role of miRNA-regulated PARP-1 in COVID-19.
Table 1.
List of functionally validated cellular microRNAs that regulate PARP-1mRNA in the context of human diseases.
| miRNA | Functional Assay | Region | Disease Relevance/Context | Ref. |
|---|---|---|---|---|
| miR-181a | Gof/Lof | 3′-UTR | Acute Myeloid Leukemia | [61] |
| miR-7-5p | Gof/Lof; Reporter assay | 3′-UTR | Small cell lung cancer | [62] |
| miR-379-5p | Luciferase Reporter assay | 3′-UTR | Premature ovarian insufficiency | [63] |
| miR-103a-2-5 pmiR-585-5p |
Luciferase Reporter assay | ORF | Oxidative stress, Hypertension | [64] |
| miR-335 | Luciferase Reporter assay | 3′-UTR | Small cell lung cancer | [65] |
| miR-520 | Luciferase Reporter assay | 3′-UTR | Recurrent spontaneous abortion | [66] |
| miR-223 | Gof/Lof; Reporter assay | 3′-UTR | Pulmonary arterial hypertension | [67] |
| miR-489 | Luciferase Reporter assay | 3′-UTR | Ischemic kidney injury | [68] |
| Let-7a | Luciferase Reporter assay | 3′-UTR | HER2-overexpressing Breast cancer | [69] |
| miR-149 | Luciferase Reporter assay | 3′-UTR | Skeletal muscle metabolism | [16] |
| miR-577 | Luciferase Reporter assay | 3′-UTR | Myocardial infarction | [70] |
| miR-221-3p | Luciferase Reporter assay | 3′-UTR | Triple negative Breast cancer | [61] |
| miR-124 | Gof/Lof; Reporter assay, RNA-pulldown |
3′-UTR | Drug (cocaine) abuse | [52] |
| miR-125b | Gof/Lof; Reporter assay, RNA-pull-down |
3′-UTR | Drug (cocaine) abuse; Regulation of HIV integration |
[53,71] |
Abbreviations used: Gof/Lof, gain-of-function/loss-of-function; 3′-UTR, 3′-untranslated region; ORF, open reading frame.
One of the long-term effects of COVID-19 is a broad spectrum of neurological disorders [72,73,74]. Cerebrovascular complications featuring peripheral nervous system damage (olfactory disorder), and ischemic and acute hemorrhagic encephalopathies with neurological features, are some of the profound observations made in COVID-19 patients [75,76,77]. The neurological features include ischemic stroke and cerebral hemorrhage, reduced consciousness, and nerve pain with abnormal levels of blood pressure. Additionally, multifocal lesions in the thalamus with signs of hemorrhage were observed in COVID-19 patients [75,78,79]. It is widely postulated that SARS-CoV-2 may employ the “Trojan horse model” of viral pathogenesis in the CNS [80,81]. The viral particles traverse through the blood brain barrier (BBB) via transcytosis and paracellular mechanisms, predominantly via the destabilization of endothelial tight junctions [82,83,84]. The hijacking of integral transport mechanisms by viral particles from the blood stream to the brain parenchyma is exacerbated as a result of induced matrix metalloproteinase (MMP) activity, causing severe BBB dysfunction and a productive infection cycle in the cellular constituents of brain parenchyma [83,84]. Given that PARP-1 is ubiquitously expressed across all tissue types with higher expression in the brain (Figure 3), it is plausible that PARP-1 may be exploited as a useful therapeutic target.
Specifically, regarding the neurological and related pathologies observed in COVID-19 patients, it is critical to understand whether:
-
(a)
SARS-CoV-2 infection affects PARP-1expression across cell types of the brain;
-
(b)
SARS-CoV-2 infection in the brain alters intracellular ATP and NAD+ levels;
-
(c)
Alteration occurs in the expression levels of miRNAs that are known to regulate PARP-1 expression in the brain and whether there is a cell-type specific effect.
Answering these broadly significant questions may provide key insights into the role of PARP-1 in the replication features of SARS-CoV-2 in the brain.
The regulation of PARP-1, particularly by miRNAs in the context of COVID-19 pathogenesis, may be of therapeutic relevance. miRNAs have been proposed as novel therapeutic molecules for several diseases, including cardiovascular dysfunction, cancer, and viral infections [85]. More recently, studies have reported alterations in host cell miRNAs in COVID-19 infection and have proposed computational modeling to predict miRNAs that can target the viral genome [86,87,88]. It will be interesting and worth validating to identify if any of the PARP-1 regulatory miRNAs are altered in COVID-19 and whether there is any tissue/cell-type specificity in such alterations. Such studies are anticipated to advance our understanding of the role of miRNAs, and to establish the relevance of miRNAs for RNA-based therapeutics for COVID-19. Given that levels of miRNA can regulate gene expression, miRNA-replacement therapy is postulated as one of the viable and emerging therapeutic options. Nonetheless, limitations such as tissue specific delivery strategies and therapeutic feasibility of miRNAs need to be thoroughly investigated.
miRNA and small RNA-based drugs are anticipated to be the next generation drugs for the cure and prevention of complex human diseases [89,90,91]. In contrast, there are currently four approved small molecule inhibitors of PARP-1, namely, Olaparib, rucaparib, talazoparib, and niraparib, which target PARP-1′s function and activity at the protein level and are used for several forms of cancer [92]. However, these inhibitors are non-selective inhibitors of PARP-1 [92]. Additionally, challenges including off-target effects, tissue distribution, dose optimization, and toxicity have resulted in a low success rate of small molecule inhibitors in clinical trials [93,94]. Nonetheless, the pleiotropic nature of miRNAs presents a major challenge in its therapeutic approach. However, miRNAs can be engineered with chemical modifications to enhance stability and target specificity; details are provided in these cited studies [90,95,96]. Importantly, the small RNA-based therapeutic approach is highly specific, and its off-target effects can be controlled and can bypass the secondary effects of targeting other mRNAs or protein function [97,98]. Although most oligonucleotide/nucleic acid-based drugs are antisense oligos or siRNA-based, the miRNA-based approach has yet to be proved to be successful. Nevertheless, a well-validated repertoire of miRNAs that regulate PARP-1 must be investigated in pre-clinical models. Therefore, targeting PARP-1 at the mRNA level by modulating the expression of tissue-specific microRNAs can be a path forward to examine the relevance of this idea. In conclusion, gaining insight into the effect of SARS-CoV-2 on miRNAs that regulate PARP-1 expression in tissue types will be an important step to understand the relevance of the “miRNA-PARP-1” axis in COVID-19 disease pathology.
Author Contributions
S.D. conceived the idea and wrote the original draft.; C.D., J.P. reviewed and edited the draft; S.D. prepared the figures and summarized the table. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.V’Kovski P., Kratzel A., Steiner S., Stalder H., Thiel V. Coronavirus biology and replication: Implications for SARS-CoV-2. Nat. Rev. Microbiol. 2021;19:155–170. doi: 10.1038/s41579-020-00468-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Coronavirus. 2021. [(accessed on 20 September 2021)]. Available online: https://www.who.int/health-topics/coronavirus#tab=tab_1.
- 3.Badawy A.A.B. Immunotherapy of COVID-19 with poly (ADP-ribose) polymerase inhibitors: Starting with nicotinamide. Biosci. Rep. 2020;40:BSR20202856. doi: 10.1042/BSR20202856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heer C.D., Sanderson D.J., Voth L.S., Alhammad Y.M.O., Schmidt M.S., Trammell S.A.J., Perlman S., Cohen M.S., Fehr A.R., Brenner C. Coronavirus and PARP expression dysregulate the NAD Metabolome: A potentially actionable component of innate immunity. bioRxiv Prepr. Serv. Biol. 2020 doi: 10.1074/jbc.RA120.015138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Curtin N., Banyai K., Thaventhiran J., Le Quesne J., Helyes Z., Bai P. Repositioning PARP inhibitors for SARS-CoV-2 infection(COVID-19): A new multi-pronged therapy for acute respiratory distress syndrome? Br. J. Pharmacol. 2020;177:3635–3645. doi: 10.1111/bph.15137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ge Y., Tian T., Huang S., Wan F., Li J., Li S., Wang X., Yang H., Hong L., Wu N., et al. An integrative drug repositioning framework discovered a potential therapeutic agent targeting COVID-19. Signal. Transduct. Target. Ther. 2021;6:165. doi: 10.1038/s41392-021-00568-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D’Amours D., Desnoyers S., D’Silva I., Poirier G.G. Poly(ADP-ribosyl)ation reactions in the regulation of nuclear functions. Pt 2Biochem. J. 1999;342:249–268. doi: 10.1042/bj3420249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krishnakumar R., Kraus W.L. PARP-1 regulates chromatin structure and transcription through a KDM5B-dependent pathway. Mol. Cell. 2010;39:736–749. doi: 10.1016/j.molcel.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luo X., Kraus W.L. On PAR with PARP: Cellular stress signaling through poly(ADP-ribose) and PARP-1. Genes Dev. 2012;26:417–432. doi: 10.1101/gad.183509.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amé J.C., Spenlehauer C., de Murcia G. The PARP superfamily. Bioessays. 2004;26:882–893. doi: 10.1002/bies.20085. [DOI] [PubMed] [Google Scholar]
- 11.Haince J.F., McDonald D., Rodrigue A., Déry U., Masson J.Y., Hendzel M.J., Poirier G.G. PARP1-dependent kinetics of recruitment of MRE11 and NBS1 proteins to multiple DNA damage sites. J. Biol. Chem. 2008;283:1197–1208. doi: 10.1074/jbc.M706734200. [DOI] [PubMed] [Google Scholar]
- 12.Hakmé A., Wong H.K., Dantzer F., Schreiber V. The expanding field of poly(ADP-ribosyl)ation reactions. “Protein Modifications: Beyond the Usual Suspects” Review Series. EMBO Rep. 2008;9:1094–1100. doi: 10.1038/embor.2008.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schreiber V., Dantzer F., Ame J.C., de Murcia G. Poly(ADP-ribose): Novel functions for an old molecule. Nat. Rev. Mol. Cell Biol. 2006;7:517–528. doi: 10.1038/nrm1963. [DOI] [PubMed] [Google Scholar]
- 14.Steffen J.D., McCauley M.M., Pascal J.M. Fluorescent sensors of PARP-1 structural dynamics and allosteric regulation in response to DNA damage. Nucleic Acids Res. 2016;44:9771–9783. doi: 10.1093/nar/gkw710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schreiber V., Amé J.C., Dollé P., Schultz I., Rinaldi B., Fraulob V., Ménissier-de Murcia J., de Murcia G. Poly(ADP-ribose) polymerase-2 (PARP-2) is required for efficient base excision DNA repair in association with PARP-1 and XRCC1. J. Biol. Chem. 2002;277:23028–23036. doi: 10.1074/jbc.M202390200. [DOI] [PubMed] [Google Scholar]
- 16.Mohamed J.S., Hajira A., Pardo P.S., Boriek A.M. MicroRNA-149 Inhibits PARP-2 and Promotes Mitochondrial Biogenesis via SIRT-1/PGC-1α Network in Skeletal Muscle. Diabetes. 2014;63:1546–1559. doi: 10.2337/db13-1364. [DOI] [PubMed] [Google Scholar]
- 17.Yélamos J., Schreiber V., Dantzer F. Toward specific functions of poly (ADP-ribose) polymerase-2. Trends Mol. Med. 2008;14:169–178. doi: 10.1016/j.molmed.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 18.Pazzaglia S., Pioli C. Multifaceted Role of PARP-1 in DNA Repair and Inflammation: Pathological and Therapeutic Implications in Cancer and Non-Cancer Diseases. Cells. 2019;9:41. doi: 10.3390/cells9010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alhammad Y.M.O., Fehr A.R. The Viral Macrodomain Counters Host Antiviral ADP-Ribosylation. Viruses. 2020;12:384. doi: 10.3390/v12040384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fehr A.R., Singh S.A., Kerr C.M., Mukai S., Higashi H., Aikawa M. The impact of PARPs and ADP-ribosylation on inflammation and host-pathogen interactions. Genes Dev. 2020;34:341–359. doi: 10.1101/gad.334425.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ha H.C., Juluri K., Zhou Y., Leung S., Hermankova M., Snyder S.H. Poly (ADP-ribose) polymerase-1 is required for efficient HIV-1 integration. Proc. Natl. Acad. Sci. USA. 2001;98:3364–3368. doi: 10.1073/pnas.051633498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mortusewicz O., Amé J.-C., Schreiber V., Leonhardt H. Feedback-regulated poly(ADP-ribosyl)ation by PARP-1 is required for rapid response to DNA damage in living cells. Nucleic Acids Res. 2007;35:7665–7675. doi: 10.1093/nar/gkm933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kraus W.L. Transcriptional control by PARP-1: Chromatin modulation, enhancer-binding, coregulation, and insulation. Curr. Opin. Cell Biol. 2008;20:294–302. doi: 10.1016/j.ceb.2008.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kraus W.L., Lis J.T. PARP goes transcription. Cell. 2003;113:677–683. doi: 10.1016/S0092-8674(03)00433-1. [DOI] [PubMed] [Google Scholar]
- 25.Alemasova E.E., Lavrik O.I. Poly(ADP-ribosyl)ation by PARP1: Reaction mechanism and regulatory proteins. Nucleic Acids Res. 2019;47:3811–3827. doi: 10.1093/nar/gkz120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rose M., Burgess J.T., O’Byrne K., Richard D.J., Bolderson E. PARP Inhibitors: Clinical Relevance, Mechanisms of Action and Tumor Resistance. Front. Cell Dev. Biol. 2020;8:564601. doi: 10.3389/fcell.2020.564601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Slade D. PARP and PARG inhibitors in cancer treatment. Genes Dev. 2020;34:360–394. doi: 10.1101/gad.334516.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grunewald M.E., Chen Y., Kuny C., Maejima T., Lease R., Ferraris D., Aikawa M., Sullivan C.S., Perlman S., Fehr A.R. The coronavirus macrodomain is required to prevent PARP-mediated inhibition of virus replication and enhancement of IFN expression. PLoS Pathog. 2019;15:e1007756. doi: 10.1371/journal.ppat.1007756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grunewald M.E., Shaban M.G., Mackin S.R., Fehr A.R., Perlman S. Murine Coronavirus Infection Activates the Aryl Hydrocarbon Receptor in an Indoleamine 2,3-Dioxygenase-Independent Manner, Contributing to Cytokine Modulation and Proviral TCDD-Inducible-PARP Expression. J. Virol. 2020;94 doi: 10.1128/JVI.01743-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sawalha A.H., Zhao M., Coit P., Lu Q. Epigenetic dysregulation of ACE2 and interferon-regulated genes might suggest increased COVID-19 susceptibility and severity in lupus patients. Clin. Immunol. 2020;215:108410. doi: 10.1016/j.clim.2020.108410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Y.X., Ma J.R., Wang S.Q., Zeng Y.Q., Zhou C.Y., Ru Y.H., Zhang L., Lu Z.G., Wu M.H., Li H. Utilizing integrating network pharmacological approaches to investigate the potential mechanism of Ma Xing Shi Gan Decoction in treating COVID-19. Eur. Rev. Med. Pharmacol. Sci. 2020;24:3360–3384. doi: 10.26355/eurrev_202003_20704. [DOI] [PubMed] [Google Scholar]
- 32.Chernyak B.V., Popova E.N., Prikhodko A.S., Grebenchikov O.A., Zinovkina L.A., Zinovkin R.A. COVID-19 and Oxidative Stress. Biochemistry. 2020;85:1543–1553. doi: 10.1134/S0006297920120068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nagy P.D., Lin W. Taking over Cellular Energy-Metabolism for TBSV Replication: The High ATP Requirement of an RNA Virus within the Viral Replication Organelle. Viruses. 2020;12:56. doi: 10.3390/v12010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sanchez E.L., Lagunoff M. Viral activation of cellular metabolism. Virology. 2015;479–480:609–618. doi: 10.1016/j.virol.2015.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Belenky P., Bogan K.L., Brenner C. NAD+ metabolism in health and disease. Trends Biochem. Sci. 2007;32:12–19. doi: 10.1016/j.tibs.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 36.Trammell S.A., Weidemann B.J., Chadda A., Yorek M.S., Holmes A., Coppey L.J., Obrosov A., Kardon R.H., Yorek M.A., Brenner C. Nicotinamide Riboside Opposes Type 2 Diabetes and Neuropathy in Mice. Sci. Rep. 2016;6:26933. doi: 10.1038/srep26933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Künzi L., Holt G.E. Cigarette smoke activates the parthanatos pathway of cell death in human bronchial epithelial cells. Cell Death Discov. 2019;5:127. doi: 10.1038/s41420-019-0205-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Diguet N., Trammell S.A.J., Tannous C., Deloux R., Piquereau J., Mougenot N., Gouge A., Gressette M., Manoury B., Blanc J., et al. Nicotinamide Riboside Preserves Cardiac Function in a Mouse Model of Dilated Cardiomyopathy. Circulation. 2018;137:2256–2273. doi: 10.1161/CIRCULATIONAHA.116.026099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chakraborty S., Mandal J., Yang T., Cheng X., Yeo J.-Y., McCarthy C.G., Wenceslau C.F., Koch L.G., Hill J.W., Vijay-Kumar M., et al. Metabolites and Hypertension: Insights into Hypertension as a Metabolic Disorder. Hypertension. 2020;75:1386–1396. doi: 10.1161/HYPERTENSIONAHA.120.13896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu H.W., Smith C.B., Schmidt M.S., Cambronne X.A., Cohen M.S., Migaud M.E., Brenner C., Goodman R.H. Pharmacological bypass of NAD(+) salvage pathway protects neurons from chemotherapy-induced degeneration. Proc. Natl. Acad. Sci. USA. 2018;115:10654–10659. doi: 10.1073/pnas.1809392115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vaur P., Brugg B., Mericskay M., Li Z., Schmidt M.S., Vivien D., Orset C., Jacotot E., Brenner C., Duplus E. Nicotinamide riboside, a form of vitamin B(3), protects against excitotoxicity-induced axonal degeneration. FASEB J. 2017;31:5440–5452. doi: 10.1096/fj.201700221RR. [DOI] [PubMed] [Google Scholar]
- 42.Ying W. NAD+/NADH and NADP+/NADPH in cellular functions and cell death: Regulation and biological consequences. Antioxid. Redox Signal. 2008;10:179–206. doi: 10.1089/ars.2007.1672. [DOI] [PubMed] [Google Scholar]
- 43.Lee H.J., Yang S.J. Aging-Related Correlation between Serum Sirtuin 1 Activities and Basal Metabolic Rate in Women, but not in Men. Clin. Nutr. Res. 2017;6:18–26. doi: 10.7762/cnr.2017.6.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Blacker T.S., Duchen M.R. Investigating mitochondrial redox state using NADH and NADPH autofluorescence. Free. Radic. Biol. Med. 2016;100:53–65. doi: 10.1016/j.freeradbiomed.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Massudi H., Grant R., Braidy N., Guest J., Farnsworth B., Guillemin G.J. Age-associated changes in oxidative stress and NAD+ metabolism in human tissue. PLoS ONE. 2012;7:e42357. doi: 10.1371/journal.pone.0042357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dash S., Dash C., Pandhare J. Activation of proline metabolism maintains ATP levels during cocaine-induced polyADP-ribosylation. Amino Acids. 2021 doi: 10.1007/s00726-021-03065-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Miller R., Wentzel A.R., Richards G.A. COVID-19: NAD(+) deficiency may predispose the aged, obese and type2 diabetics to mortality through its effect on SIRT1 activity. Med. Hypotheses. 2020;144:110044. doi: 10.1016/j.mehy.2020.110044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mueller A.L., McNamara M.S., Sinclair D.A. Why does COVID-19 disproportionately affect older people? Aging. 2020;12:9959–9981. doi: 10.18632/aging.103344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hu L., Wang Z., Carmone C., Keijer J., Zhang D. Role of Oxidative DNA Damage and Repair in Atrial Fibrillation and Ischemic Heart Disease. Int. J. Mol. Sci. 2021;22:3838. doi: 10.3390/ijms22083838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ke Y., Wang C., Zhang J., Zhong X., Wang R., Zeng X., Ba X. The Role of PARPs in Inflammation—And Metabolic—Related Diseases: Molecular Mechanisms and Beyond. Cells. 2019;8:1047. doi: 10.3390/cells8091047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Petriti B., Williams P.A., Lascaratos G., Chau K.-Y., Garway-Heath D.F. Neuroprotection in Glaucoma: NAD+/NADH Redox State as a Potential Biomarker and Therapeutic Target. Cells. 2021;10:1402. doi: 10.3390/cells10061402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dash S., Balasubramaniam M., Rana T., Godino A., Peck E.G., Goodwin J.S., Villalta F., Calipari E.S., Nestler E.J., Dash C., et al. Poly (ADP-Ribose) Polymerase-1 (PARP-1) Induction by Cocaine Is Post-Transcriptionally Regulated by miR-125b. eneuro. 2017;4:ENEURO.0089-17.2017. doi: 10.1523/ENEURO.0089-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dash S., Balasubramaniam M., Martínez-Rivera F.J., Godino A., Peck E.G., Patnaik S., Suar M., Calipari E.S., Nestler E.J., Villalta F., et al. Cocaine-regulated microRNA miR-124 controls poly (ADP-ribose) polymerase-1 expression in neuronal cells. Sci. Rep. 2020;10:11197. doi: 10.1038/s41598-020-68144-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Scobie K.N., Damez-Werno D., Sun H., Shao N., Gancarz A., Panganiban C.H., Dias C., Koo J., Caiafa P., Kaufman L., et al. Essential role of poly(ADP-ribosyl)ation in cocaine action. Proc. Natl. Acad. Sci. USA. 2014;111:2005–2010. doi: 10.1073/pnas.1319703111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang C., Xu W., An J., Liang M., Li Y., Zhang F., Tong Q., Huang K. Poly(ADP-ribose) polymerase 1 accelerates vascular calcification by upregulating Runx2. Nat. Commun. 2019;10:1203. doi: 10.1038/s41467-019-09174-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kaur G., Singh N., Lingeshwar P., Siddiqui H.H., Hanif K. Poly (ADP-ribose) polymerase-1: An emerging target in right ventricle dysfunction associated with pulmonary hypertension. Pulm. Pharmacol. Ther. 2015;30:66–79. doi: 10.1016/j.pupt.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 57.Margulies C.E., Ladurner A.G. PARP-1 Flips the Epigenetic Switch on Obesity. Mol. Cell. 2020;79:874–875. doi: 10.1016/j.molcel.2020.08.019. [DOI] [PubMed] [Google Scholar]
- 58.Schnall-Levin M., Rissland O.S., Johnston W.K., Perrimon N., Bartel D.P., Berger B. Unusually effective microRNA targeting within repeat-rich coding regions of mammalian mRNAs. Genome Res. 2011;21:1395–1403. doi: 10.1101/gr.121210.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lytle J.R., Yario T.A., Steitz J.A. Target mRNAs are repressed as efficiently by microRNA-binding sites in the 5’ UTR as in the 3’ UTR. Proc. Natl. Acad. Sci. USA. 2007;104:9667–9672. doi: 10.1073/pnas.0703820104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Iwakawa H., Tomari Y. Molecular Insights into microRNA-Mediated Translational Repression in Plants. Mol. Cell. 2013;52:591–601. doi: 10.1016/j.molcel.2013.10.033. [DOI] [PubMed] [Google Scholar]
- 61.Deng L., Lei Q., Wang Y., Wang Z., Xie G., Zhong X., Wang Y., Chen N., Qiu Y., Pu T., et al. Downregulation of miR-221-3p and upregulation of its target gene PARP1 are prognostic biomarkers for triple negative breast cancer patients and associated with poor prognosis. Oncotarget. 2017;8:108712–108725. doi: 10.18632/oncotarget.21561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lai J., Yang H., Zhu Y., Ruan M., Huang Y., Zhang Q. MiR-7-5p-mediated downregulation of PARP1 impacts DNA homologous recombination repair and resistance to doxorubicin in small cell lung cancer. BMC Cancer. 2019;19:602. doi: 10.1186/s12885-019-5798-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dang Y., Wang X., Hao Y., Zhang X., Zhao S., Ma J., Qin Y., Chen Z.-J. MicroRNA-379-5p is associated with biochemical premature ovarian insufficiency through PARP1 and XRCC6. Cell Death Dis. 2018;9:106. doi: 10.1038/s41419-017-0163-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dluzen D.F., Kim Y., Bastian P., Zhang Y., Lehrmann E., Becker K.G., Hooten N.N., Evans M.K. MicroRNAs Modulate Oxidative Stress in Hypertension through PARP-1 Regulation. Oxid. Med. Cell. Longev. 2017;2017:1–12. doi: 10.1155/2017/3984280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Luo Y., Tong L., Meng H., Zhu W., Guo L., Wei T., Zhang J. MiR-335 regulates the chemo-radioresistance of small cell lung cancer cells by targeting PARP-1. Gene. 2017;600:9–15. doi: 10.1016/j.gene.2016.11.031. [DOI] [PubMed] [Google Scholar]
- 66.Dong X., Yang L., Wang H. miR-520 promotes DNA-damage-induced trophoblast cell apoptosis by targeting PARP1 in recurrent spontaneous abortion (RSA) Gynecol. Endocrinol. 2017;33:274–278. doi: 10.1080/09513590.2016.1266476. [DOI] [PubMed] [Google Scholar]
- 67.Meloche J., Le Guen M., Potus F., Vinck J., Ranchoux B., Johnson I., Antigny F., Tremblay E., Breuils-Bonnet S., Perros F., et al. miR-223 reverses experimental pulmonary arterial hypertension. Am. J. Physiol. Physiol. 2015;309:C363–C372. doi: 10.1152/ajpcell.00149.2015. [DOI] [PubMed] [Google Scholar]
- 68.Wei Q., Liu Y., Liu P., Hao J., Liang M., Mi Q., Chen J.-K., Dong Z. MicroRNA-489 Induction by Hypoxia–Inducible Factor–1 Protects against Ischemic Kidney Injury. J. Am. Soc. Nephrol. 2016;27:2784–2796. doi: 10.1681/ASN.2015080870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wielgos M.E., Rajbhandari R., Cooper T.S., Wei S., Nozell S., Yang E.S. Let-7 Status Is Crucial for PARP1 Expression in HER2-Overexpressing Breast Tumors. Mol. Cancer Res. 2017;15:340–347. doi: 10.1158/1541-7786.MCR-16-0287-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang Y.-H., Zhang X.-Y., Han Y.-Q., Yan F., Wu R. MicroRNA-577 inhibits cardiomyocyte apoptosis induced by myocardial infarction via targeting PARP1. Eur. Rev. Med. Pharmacol. Sci. 2019;23:9566–9573. doi: 10.26355/eurrev_201911_19451. [DOI] [PubMed] [Google Scholar]
- 71.Chaudhuri E., Dash S., Balasubramaniam M., Padron A., Holland J., Sowd G.A., Villalta F., Engelman A.N., Pandhare J., Dash C. The HIV-1 capsid-binding host factor CPSF6 is post-transcriptionally regulated by the cellular microRNA miR-125b. J. Biol. Chem. 2020;295:5081–5094. doi: 10.1074/jbc.RA119.010534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kubota T., Kuroda N. Exacerbation of neurological symptoms and COVID-19 severity in patients with preexisting neurological disorders and COVID-19: A systematic review. Clin. Neurol. Neurosurg. 2021;200:106349. doi: 10.1016/j.clineuro.2020.106349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Taquet M., Geddes J.R., Husain M., Luciano S., Harrison P.J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: A retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8:416–427. doi: 10.1016/S2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zubair A.S., McAlpine L.S., Gardin T., Farhadian S., Kuruvilla D.E., Spudich S. Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019: A Review. JAMA Neurol. 2020;77:1018–1027. doi: 10.1001/jamaneurol.2020.2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Beyrouti R., Adams M.E., Benjamin L., Cohen H., Farmer S.F., Goh Y.Y., Humphries F., Jäger H.R., Losseff N.A., Perry R.J., et al. Characteristics of ischaemic stroke associated with COVID-19. J. Neurol. Neurosurg. Psychiatry. 2020;91:889–891. doi: 10.1136/jnnp-2020-323586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mao L., Jin H., Wang M., Hu Y., Chen S., He Q., Chang J., Hong C., Zhou Y., Wang D., et al. Neurologic Manifestations of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pleasure S.J., Green A.J., Josephson S.A. The Spectrum of Neurologic Disease in the Severe Acute Respiratory Syndrome Coronavirus 2 Pandemic Infection: Neurologists Move to the Frontlines. JAMA Neurol. 2020;77:679–680. doi: 10.1001/jamaneurol.2020.1065. [DOI] [PubMed] [Google Scholar]
- 78.Oxley T.J., Mocco J., Majidi S., Kellner C.P., Shoirah H., Singh I.P., De Leacy R.A., Shigematsu T., Ladner T.R., Yaeger K.A., et al. Large-Vessel Stroke as a Presenting Feature of COVID-19 in the Young. N. Engl. J. Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B. COVID-19–associated Acute Hemorrhagic Necrotizing Encephalopathy: Imaging Features. Radiology. 2020;296:E119–E120. doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Erickson M.A., Rhea E.M., Knopp R.C., Banks W.A. Interactions of SARS-CoV-2 with the Blood—Brain Barrier. Int. J. Mol. Sci. 2021;22:2681. doi: 10.3390/ijms22052681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pennisi M., Lanza G., Falzone L., Fisicaro F., Ferri R., Bella R. SARS-CoV-2 and the Nervous System: From Clinical Features to Molecular Mechanisms. Int. J. Mol. Sci. 2020;21:5475. doi: 10.3390/ijms21155475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dash S., Balasubramaniam M., Villalta F., Dash C., Pandhare J. Impact of cocaine abuse on HIV pathogenesis. Front. Microbiol. 2015;6:1111. doi: 10.3389/fmicb.2015.01111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Meyding-Lamadé U., Craemer E., Schnitzler P. Emerging and re-emerging viruses affecting the nervous system. Neurol. Res. Pract. 2019;1:20. doi: 10.1186/s42466-019-0020-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Miner J.J., Diamond M.S. Mechanisms of restriction of viral neuroinvasion at the blood—Brain barrier. Curr. Opin. Immunol. 2016;38:18–23. doi: 10.1016/j.coi.2015.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Broderick J.A., Zamore P.D. MicroRNA therapeutics. Gene Ther. 2011;18:1104–1110. doi: 10.1038/gt.2011.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhang S., Amahong K., Sun X., Lian X., Liu J., Sun H., Lou Y., Zhu F., Qiu Y. The miRNA: A small but powerful RNA for COVID-19. Brief. Bioinform. 2021;22:1137–1149. doi: 10.1093/bib/bbab062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Alam T., Lipovich L. miRCOVID-19: Potential Targets of Human miRNAs in SARS-CoV-2 for RNA-Based Drug Discovery. Non-Coding RNA. 2021;7:18. doi: 10.3390/ncrna7010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Farr R.J., Rootes C.L., Rowntree L.C., Nguyen T.H.O., Hensen L., Kedzierski L., Cheng A.C., Kedzierska K., Au G.G., Marsh G.A., et al. Altered microRNA expression in COVID-19 patients enables identification of SARS-CoV-2 infection. PLoS Pathog. 2021;17:e1009759. doi: 10.1371/journal.ppat.1009759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bajan S., Hutvagner G. RNA-Based Therapeutics: From Antisense Oligonucleotides to miRNAs. Cells. 2020;9:137. doi: 10.3390/cells9010137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rupaimoole R., Slack F.J. MicroRNA therapeutics: Towards a new era for the management of cancer and other diseases. Nat. Rev. Drug Discov. 2017;16:203–222. doi: 10.1038/nrd.2016.246. [DOI] [PubMed] [Google Scholar]
- 91.Hanna J., Hossain G.S., Kocerha J. The Potential for microRNA Therapeutics and Clinical Research. Front. Genet. 2019;10:478. doi: 10.3389/fgene.2019.00478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sahin K., Durdagi S. Identifying new piperazine-based PARP1 inhibitors using text mining and integrated molecular modeling approaches. J. Biomol. Struct. Dyn. 2021;39:681–690. doi: 10.1080/07391102.2020.1715262. [DOI] [PubMed] [Google Scholar]
- 93.Ricks T.K., Chiu H.J., Ison G., Kim G., McKee A.E., Kluetz P., Pazdur R. Successes and Challenges of PARP Inhibitors in Cancer Therapy. Front. Oncol. 2015;5:222. doi: 10.3389/fonc.2015.00222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang Y.-Q., Wang P.-Y., Wang Y.-T., Yang G.-F., Zhang A., Miao Z.-H. An Update on Poly (ADP-ribose)polymerase-1 (PARP-1) Inhibitors: Opportunities and Challenges in Cancer Therapy. J. Med. Chem. 2016;59:9575–9598. doi: 10.1021/acs.jmedchem.6b00055. [DOI] [PubMed] [Google Scholar]
- 95.Baumann V., Winkler J. miRNA-based therapies: Strategies and delivery platforms for oligonucleotide and non-oligonucleotide agents. Futur. Med. Chem. 2014;6:1967–1984. doi: 10.4155/fmc.14.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lockhart J., Canfield J., Mong E.F., VanWye J., Totary-Jain H. Nucleotide Modification Alters MicroRNA-Dependent Silencing of MicroRNA Switches. Mol. Ther.-Nucleic Acids. 2019;14:339–350. doi: 10.1016/j.omtn.2018.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Damase T.R., Sukhovershin R., Boada C., Taraballi F., Pettigrew R.I., Cooke J.P. The Limitless Future of RNA Therapeutics. Front. Bioeng. Biotechnol. 2021;9:628137. doi: 10.3389/fbioe.2021.628137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yu A.-M., Choi Y.H., Tu M.-J. RNA Drugs and RNA Targets for Small Molecules: Principles, Progress, and Challenges. Pharmacol. Rev. 2020;72:862–898. doi: 10.1124/pr.120.019554. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.