Abstract
Objective:
To evaluate whether hospital entry into the 340B Drug Pricing Program - which entitles eligible hospitals to discounts on drug purchases and intends for hospitals to use associated savings to devote more resources to the care of low-income populations - is associated with changes in hospital provision of uncompensated care.
Study design:
We analyzed secondary data on 340B participation and uncompensated care provision among general acute care hospitals and critical access hospitals from 2003–2015. We constructed an annual, hospital-level dataset on hospital 340B participation from the Office of Pharmacy Information Systems and on uncompensated care provision from the Hospital Cost Reporting Information System.
Methods:
Focusing on two periods of Program expansion, we separately analyzed trends in uncompensated care costs for 340B-eligible general acute-care hospitals and critical access hospitals, stratified by year of 340B Program entry, including a stratum of eligible hospitals that never participated. We used a differences-in-differences approach to quantify whether there were differential changes in provision of uncompensated care after hospitals enter the 340B Program relative to hospitals that did not participate or had not yet entered.
Results:
We do not find evidence that hospitals increased provision of uncompensated care after entry into the 340B Program differentially more than hospitals that never entered or had not yet entered the Program.
Conclusions:
Relying on hospitals to invest surplus into care for the underserved without marginal incentives to do so or strong oversight may not be an effective strategy to expand safety net care.
Precis:
Participation in the 340B Drug Pricing Program by general acute care hospitals and critical access hospitals has not been associated with increased provision of uncompensated care.
INTRODUCTION
The 340B Drug Pricing Program is a federal program that entitles eligible hospitals to manufacturer discounts on purchases of drugs administered or prescribed in an outpatient setting. The discounted drugs can be provided to patients regardless of their ability to pay or their insurance coverage status or provider. The 1992 statute under which the Program was established states that Program savings are intended to “stretch scarce federal resources as far as possible, reaching more eligible patients and providing more comprehensive services.” The Program does not provide a direct incentive for hospitals to invest surplus in any specific way.
While the Program statute does not explicitly articulate how revenue from the 340B Program should be used,1 federal agencies have since clarified that Program resources should be used to better serve underserved patient populations.2 Uncompensated care, which includes charity care and other unreimbursed care provided to uninsured or underinsured patients is one key mechanism by which hospitals devote resources to the care of vulnerable populations.3 Therefore, increases in hospital provision of uncompensated care following entry into the 340B Program would be consistent with hospitals passing through discounts to patients in a manner intended by the Program.
Program growth and evidence that 340B Program incentives have increased hospital provision of drugs4,5 has led to increased scrutiny of whether 340B discounts benefit the underserved as intended. We examined trends in hospital-reported provision of uncompensated care during periods of 340B Program expansion. We test whether hospital provision of uncompensated care increased following hospital entry into the 340B Program for general acute-care hospitals and critical access hospitals separately.
METHODS
We focused on two periods during which 340B participation by hospitals grew rapidly. The first period occurred after passage of the 2003 Medicare Modernization Act (MMA). The MMA expanded 340B eligibility to rural and small urban general acute-care hospitals with sufficient shares of inpatient admissions for low-income patients as measured by the disproportionate share (DSH) adjustment percentage; following the MMA, participation increased among the newly eligible hospitals as well as previously eligible hospitals. (While the reason for the increase in participation among already-eligible hospitals is unclear, it may be due to greater awareness about the Program and organized industry efforts to support provider participation. For example, the first 340B Coalition Winter Conference which aims to provide 340B entities with support and information on topics ranging from Program implementation, operations, compliance, contract pharmacy relationships, inventory management, among other practical issues was held in 2004.6) The second period followed the 2010 Affordable Care Act (ACA), which expanded eligibility to all critical access hospitals.5,7 We estimated changes in hospital-reported uncompensated care costs associated with Program participation during these two periods of 340B growth for general acute-care hospitals and critical access hospitals.
Study Data and Population
We used annual data for years 2003–2015 from the Office of Pharmacy Affairs Information System,8 which identifies hospitals that participated in the 340B Program by year, and the Hospital Cost Reporting Information System (HCRIS). Our study outcome was uncompensated care costs reported by hospitals in HCRIS, which is a measure of hospital costs associated with charity care, care provided to patients in means-tested government programs with low reimbursement rates (including Medicaid, the Children’s Health Insurance Program, and state and local indigent programs), and other unreimbursed care.
We analyzed two groups of hospitals. The first included general acute-care hospitals in years 2003–2009, a period of rapid growth in participation among general acute-care hospitals specifically; in fact, 78% of all general acute-care hospitals in the 340B Program in 2016 had entered by 2010. To be 340B eligible, general acute-care hospitals were required to be non-profit or publicly owned and had to have a disproportionate share hospital (DSH) percentage exceeding 11.75% in the previous year. The DSH percentage is a function of several factors, including the proportion of a hospital’s admissions that are for Medicaid or low-income Medicare patients. We required general acute-care hospitals to be 340B eligible in at least one year during the study period to be included in the main analysis, but results were similar when we controlled for eligibility or limited the analysis to hospitals eligible in every year.
Second, we examined critical access hospitals during years 2011–2015; all critical access hospitals became 340B eligible under the ACA in 2010. We excluded 2010 from the analysis because of inconsistent reporting resulting from a transition to a new HCRIS formula for calculating uncompensated care costs adopted by most hospitals in 2011.
We excluded the small number of hospitals that started and subsequently stopped 340B participation during the study period; our results were not substantively altered by their inclusion. To ensure at least one year of pre-participation data to estimate changes in uncompensated care costs from before to after Program entry, we excluded general acute-care hospitals participating before 2004 and critical access hospitals participating before 2012 from regression analyses.
We also excluded hospitals with missing uncompensated care data. Because reporting of uncompensated care was not mandatory during 2003–2009, 251 (18.7%) general acute-care hospitals were excluded due to missing uncompensated care data. We did not find substantial differences in 340B participation, other hospital characteristics, or subsequent uncompensated care costs in 2011–2015 (when reporting was mandatory) between hospitals with missing and non-missing data on uncompensated care costs in the 2003–2009 period (Table A1). These findings suggest missingness in the earlier period was unrelated to provision of uncompensated care and thus mitigates concerns that it was a source of bias in our analysis. For further details of the exclusion criteria and analysis of hospitals with and without missing outcomes data, see the online appendix.
Statistical Analysis
We separately analyzed trends in uncompensated care costs for general acute-care hospitals and critical access hospitals, stratified by year of 340B Program entry, including a stratum of eligible hospitals that never participated. We used a differences-in-differences approach to quantify the extent to which hospitals differentially changed provision of uncompensated care after entering the 340B Program relative to hospitals that did not participate or had not yet started participating. We estimated the following linear model:
where Log(UCist) denotes the logged uncompensated care costs for hospital i in state s and year t, 340Bit) is a time-varying annual indicator for hospital i’s participation status, αi denotes a vector of hospital fixed effects to control for time-invariant differences between hospitals, αt denotes a vector of year fixed effects, αs * αt denotes a vector of fixed effects for every state-year combination in the data to control for state-specific time trends that might vary because of policy changes at the state level (e.g., Medicaid expansion), and αist is a random error term. We log-transformed uncompensated care costs to estimate relative differences between cohorts. The coefficient for the time-varying 340B participation indicator approximated the quantity of interest: the percentage change in uncompensated care costs from before to after 340B participation for hospitals participating in a given year divided by the percentage change for hospitals not participating through that year, averaged over all years. In robustness tests, we specified the outcome in absolute dollars. We estimated robust standard errors clustered at the state level.9
In additional robustness tests, we weighted the regression by the number of hospital beds and specified the outcome as the log-transformed uncompensated care costs per hospital bed. One concern in analyses of general acute-care hospitals is that our results could be biased by hospitals losing eligibility during the study period since our sanalysis requires hospitals to be eligible for one year during the study period at a minimum (this is not an issue in the analysis of CAHs since all CAHs became 340B eligible under the ACA). To test whether potential changes in hospital eligibility status in subsequent years could be a source of endogeneity, we conducted two tests. First, we estimated the main model after limiting the analysis to hospitals that were eligible in every year of the study period starting in 2004. In a separate test, we controlled for whether a hospital was eligible in each year.
Analyses of selection in 340B participation and 340B eligibility
An assumption necessary to interpret our results as causal effects of the 340B Program is that time-varying, omitted variables do not affect changes in both participation status and levels of uncompensated care. We test for evidence on this assumption by comparing trends in the outcome between hospital cohorts during pre-participation years. Specifically, we tested for differences in uncompensated care cost trends during pre-participation years between entry-year cohorts of hospitals (including non-participants) by estimating the following model:
where denotes an interaction term between a categorical variable assigned to each entry-year cohort including non-participants and a continuous year trend. Entry Cohorti * 1(Yeart=n) is a vector of interaction terms between an indicator for hospital i’s 340B entry year and an indicator for each post-entry year t, estimating a differential change in uncompensated care spending associated with each year of participation by entry-year cohort after adjusting for any pre-participation differences in trends. Because effects in post-entry years will be absorbed by the vector of interactions Entry Cohorti * 1(Yeart=n), the estimates δ describe the difference in the annual change in uncompensated care for each entry cohort during pre-entry years relative to the omitted cohort of hospitals that never participated. To assess differences in pre-entry trends between hospital cohorts, we calculate and report each cohort’s pre-entry trend from the coefficients in the vector δ and conduct a test of joint significance of the trend differences.
Another key assumption of our analysis, and prior work using a similar approach,10 is that changes in uncompensated care do not cause changes in participation by affecting hospital eligibility for the Program. General acute care hospitals, for example, might increase the number of Medicaid patients served to increase their DSH payment percentage above the threshold for Program eligibility, potentially resulting in an increase in uncompensated care spending associated with Program entry. Because we defined our comparison groups based on observed changes in participation, random fluctuations or secular trends in uncompensated care that cause eligibility changes could also contribute to increases in uncompensated care spending that are associated with, but not caused by, Program entry. This source of potential endogeneity bias is addressed in our sensitivity analysis restricting the analysis to hospitals eligible for the Program in all years of the relevant expansion period, thereby eliminating changes in uncompensated care that caused changes in eligibility from estimates.
In prior work,11 we also tested extensively for evidence of hospital manipulation of DSH percentages to gain entry into the Program and did not find evidence of this behavior. Specifically, we found minimal bunching of hospital DSH percentages just above the 11.75% DSH percentage threshold, at least in data through 2012. Emergence of such bunching in later years would not be consistent with strategic manipulation to enter the Program since 78% of hospitals had already entered the Program by 2010. We also found no evidence that general acute care hospitals with DSH percentages just above 11.75% in 2010 had exhibited greater increases in DSH percentages over preceding years, or that characteristics of hospitals or their patients changed discontinuously at the threshold.
RESULTS
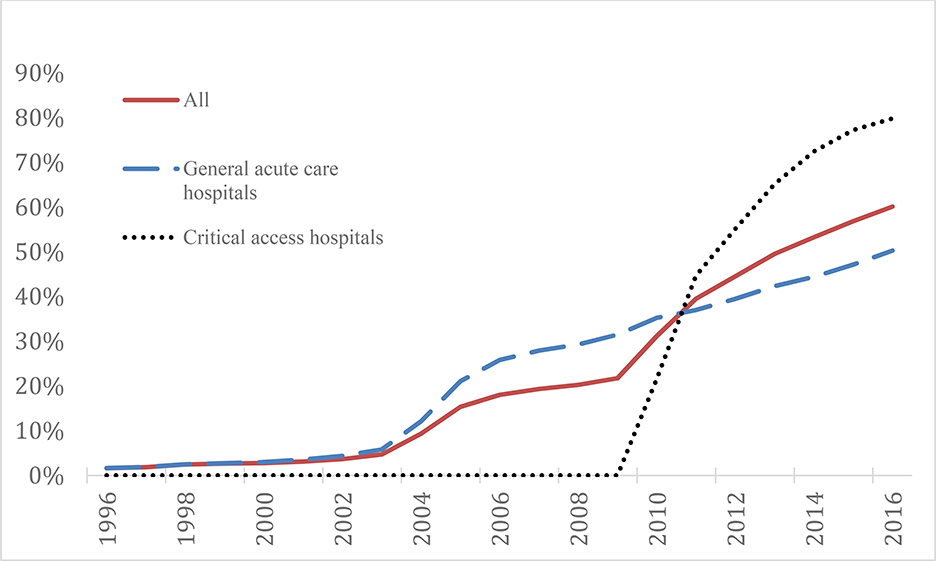
The study population consisted of 873 general acute-care hospitals and 632 critical access hospitals. Figure 1 shows the percent of all hospitals, general acute-care hospitals, and critical access hospitals participating in the 340B Program by year from 1996 to 2016, including the inflections in participation rates at the outset of the two expansion periods starting in 2004 and 2010. Following exclusions, among general acute-care hospitals, the participation rate increased from 17% to 65% from 2004 to 2009. Among critical access hospitals in our study population, the participation rate increased from 45% to 79% from 2011 to 2015.
Figure 1. Rate of hospital participation in the 340B Program among public and non-profit hospitals, 1996–2016.
Notes. The figure plots the percent of all hospitals, (non-critical access) general acute care hospitals, and critical access hospitals that participated in the 340B Program in each year from 1996–2016. The study hospitals are limited to public and not-for-profit hospitals, since for-profit hospitals are not 340B eligible. However, this figure includes hospitals excluded in our analysis. Increases in hospital participation following the MMA and ACA can be observed.
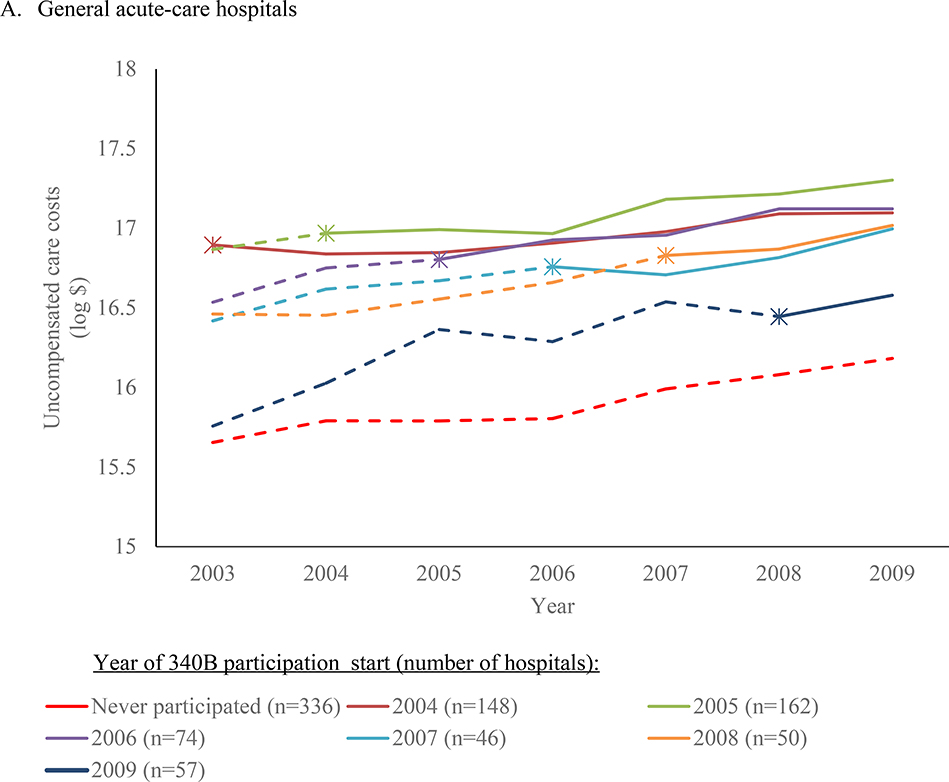
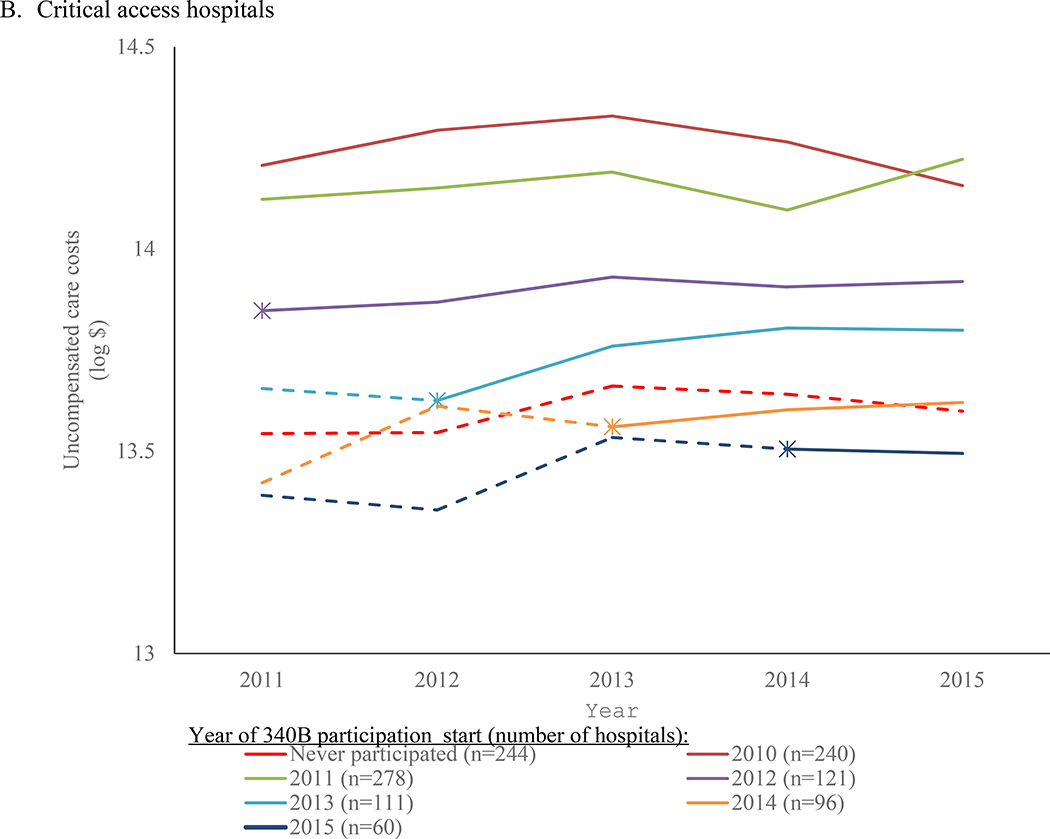
In their respective baseline years, general acute-care hospitals reported average uncompensated care costs of $26.1 million and critical access hospitals had average uncompensated care costs of $1.6 million. (Note that these two measures are not directly comparable because of the change in the uncompensated care cost formula between the two study periods.) We do not find evidence that hospitals increased provision of uncompensated care in the years following entry into the 340B Program differentially more than hospitals that never entered the Program or had not yet entered the Program. When stratified by year of 340B Program entry, trends in log uncompensated care costs were similar across entry cohorts in non-participation years and did not systematically change following entry (Figure 2). On average, increases in uncompensated care costs from years before participation to years after Program entry did not differ significantly from concurrent increases among hospitals not yet or never participating, both among general acute-care hospitals (differential change: −4.6% [95% CI:−9.7,0.7]; P=0.09) and critical access hospitals (2.3% [−4.3,9.4]; P=0.49) (Table 1). For comparison, average annual changes in uncompensated care costs in non-participation years were 6% for general acute-care hospitals and 3% for critical access hospitals. Hospitals that participated in the 340B Program reported higher levels of uncompensated care compared to non-participating hospitals even prior to participation, demonstrating that cross-sectional differences between hospitals cannot be attributed to the 340B Program.
Figure 2. Hospital uncompensated care costs by year of 340B participation start.
Notes. This figure plots hospital log-transformed uncompensated care costs by year for general acute-care hospitals (A) and critical access hospitals (B). Hospitals are categorized by the year in which they began participation or as never participating during the study period. The dotted line portion indicates pre-participation years and solid line indicates participation years, with the transition point depicted at the last pre-participation year so that changes from the last pre-participation year to the first participation year are reflected by the (solid) participation phase of the time trend.
Table 1.
Differential changes in uncompensated care costs for 340B participating hospitals relative to eligible hospitals not yet or never participating
| Hospital-reported uncompensated care costsa |
|||||
| Average in first year of study period ($, millions)b | Annual change during non-participation years, %c | Differential change after participation relative to concurrent change among non-participating hospitals, %d | |||
|
|
|
|
|||
| Hospital-type (# of unique hospitals) | Mean [Stand. dev.] | Estimate [95% CI] | P value | Estimate [95% CI] | P value |
|
| |||||
| General acute-care hospitalse (n=873) | 26.1 [41.4] | 6 [3.8,8.3] | <0.001 | −4.6 [−9.7,0.7] | 0.09 |
| Critical access hospitalsf (n=632) | 1.6 [1.7] | 3 [0.2,5.9] | 0.03 | 2.3 [−4.3,9.4] | 0.49 |
Uncompensated care cost is defined as costs associated with charity care, Medicaid, Children’s Health Insurance Program, state and local indigent care programs, as well as bad debt expenses which are write-offs from other care that was not reimbursed (2003–2009: worksheet S-10, sum of lines 32 and 31; critical access hospitals: worksheet S-10, line 30). Due to a reporting change, the measurement of uncompensated care costs during the 2003–2009 study period differed from that in the 2011–2015 study period. In the 2003–2009 analysis, the costs reflect charges multiplied by the hospital’s cost-to-charge ratio. In the 2011–2015 analyses, the outcome reflects the unreimbursed costs which are calculated as the charges multiplied by the cost-to-charge ratio less net revenues from each component. As a result, the two measures cannot be directly compared to each other. From 2009–2015, hospitals could report negative uncompensated care costs if recovery of previous year’s bad debt exceeded uncompensated care costs in that year. The 69 hospital-year observations (1.2%) reporting negative uncompensated care were excluded from the analysis.
2003 for general acute-care hospitals and 2011 for critical access hospitals.
Estimated during years prior to participation among hospitals that participated and during all years among hospitals that never participated. Adjusted for hospital fixed effects. Outcome specified as log-transformed uncompensated care costs. Percentage effects derived from the coefficient estimates are reported.
Linear regression controlling for an interaction between a continuous year variable and an indicator for whether the hospital ever participated in the 340B Program during the study period, hospital fixed effects, year fixed effects, and state-year fixed effects. Outcome specified as log-transformed uncompensated care costs. Percentage effects derived from the coefficient estimates are reported.
General acute-care hospitals were identified as those reporting as short-term acute-care hospitals but not critical access hopsitals in HCRIS.
Hospitals that reported as critical access hospitals in HCRIS.
Conclusions were similar when we specified the outcome as uncompensated care costs in absolute dollars (Table A2). The differences-in-differences estimate of the increase in absolute uncompensated care costs associated with hospital 340B participation represents 3% of uncompensated care costs in the first year of the study period among general acute-care hospitals (beta=$791,400; p=0.61) and 4% of uncompensated care costs in the first year of the study period for critical access hospitals (beta=$66,200; p=0.19). Analyses limiting the general acute care hospitals to those that were eligible in every year of the study period starting in 2004 as well analyses using all hospitals from our main analysis but controlling for eligibility status in each year yielded results consistent with the main findings. Additional robustness tests, including controlling for changes in hospital 340B eligibility status and weighting by the number of beds, produced similar results (Tables A3-A5).
Pre-participation trends differed minimally between hospital cohorts and were not systematically related to entry year or participation status, suggesting that 340B participation was not related to pre-existing growth rates of uncompensated care and supporting our assumption that differences between cohorts would have remained constant in the absence of Program participation (Table A6). On average during non-participation years, trends in uncompensated care costs differed between cohorts of hospitals with different years of program entry by only 1.8% for acute-care hospitals and by 0.6% for critical access hospitals. For 17 of 21 pairwise comparisons of acute-care hospital cohorts and 10 of 10 pairwise comparisons of critical access hospital cohorts, trend differences were not statistically significant.
DISCUSSION
Our results indicate that participation in the 340B Program has not been associated with increases in hospital-reported uncompensated care provision. Our analyses also highlight that cross-sectional differences between 340B and non-340B hospitals do not support inferences about the causal effects of the 340B Program. We found that hospitals entering the 340B Program earlier provided more uncompensated care, but these differences were present at baseline, before Program participation and before Program expansion, and did not widen between earlier and later entrants (or non-participants) after up to 6 more years of 340B discounts for the earlier entrants.
Our analyses add to evidence that questions whether the Program is achieving its stated goal of freeing up resources to devote to the care of low-income populations. Our conclusions are consistent with prior work finding that the 340B Program has not been associated with net increases in community benefit spending or outcomes for low-income populations.4,10 Our analysis extends this and other previous work by examining impacts of 340B entry on uncompensated care costs for both general acute-care hospitals and critical access hospitals, the latter of which constitute a large proportion of new entrants following the Affordable Care Act’s eligibility expansion.
Our study had several limitations. We could not assess the response of critical access hospitals entering the 340B Program in the first two years of expanded eligibility because we lacked their pre-participation uncompensated care data. Moreover, hospital surplus from 340B discounts may have affected care for low-income patients in ways not reflected by the uncompensated care measure. In particular, we could not assess Program effects on hospital closures. Next, our estimates would be biased if timing of hospital entry into the 340B Program was associated with financial hardship and helped maintain uncompensated care provision that would have otherwise declined. However, such selection into participation would also be expected to be accompanied by differential trends in uncompensated care provision in the years prior to Program entry, but we do not find evidence that pre-participation trends systematically differed between hospitals entering the program earlier versus later versus never. Because hospitals benefit from participation only if they administer discounted drugs, some eligible hospitals may not participate if they provide low volumes of outpatient drugs.12 Our analysis of pre-participation trends would suggest that hospital outpatient drug volume is not systematically related to trends in uncompensated care provision.
Relatedly, our research design does not control for confounding by time-varying predictors of uncompensated care that differentially changed after Program entry. For example, if 340B participation was associated with displacement of subsidies from state and local governments, our estimates may underestimate the effects of participation. However, such displacement has not been documented to our knowledge and such a regulatory mechanism at the hospital level would need to be relatively sophisticated since hospital eligibility can fluctuate over time and also seems unlikely given reports of limited Program oversight.13 Finally, Medicare reimburses critical access hospitals for Part B (parenteral) drugs at 101% of costs, which limits savings accrued in the 340B Program from administering Part B drugs to Medicare patients.14 While these hospitals may still generate savings from the Program via dispensing prescription drugs and administering parenteral drugs to commercially insured patients, the resulting surplus may be more limited than for acute-care hospitals and insufficient to finance substantive increases in uncompensated care spending. Moreover, the high participation rate among critical access hospitals suggests they benefit from Program participation.
Our findings contribute to evidence that hospitals may not use 340B Program surplus to expand or enhance care for safety net populations. A growing body of evidence that the Program is not benefiting safety net populations combined with evidence that it is contributing to hospital-physician consolidation and increases in hospital-based drug provision suggest the need for Program reform. Reforms could include requiring that drugs purchased under the 340B Program are provided to safety net populations, establishing mechanisms for hospitals to pass on discounts to patients in the form of cost sharing assistance, and increasing oversight and enforcement of how hospital surplus is used. More broadly, evidence to date on the Program suggests that policies to finance safety net care should more transparently and directly target resources to patient populations of interest, rather than indirectly by altering the profitability of some services, and include greater oversight and enforcement over how providers receiving resources use them. Recently, the Centers for Medicare and Medicaid Services proposed reducing Part B drug reimbursements for 340B hospitals to 22.5% less than Average Sales Price.15 This reimbursement cut substantially reduces Program funding for hospitals by reducing the profitability of administering 340B drugs, particularly for hospitals with a heavier Medicare payor mix. Instead, optimal policy might involve ending the 340B Program and expanding or developing other programs to help low-income populations.
CONCLUSION
Our study sheds light on whether policies that direct unrestricted funds to hospitals for the purpose of expanding safety net care in fact increase the provision of safety net care. Prior research on whether hospitals cross-subsidize care for low-income populations is mixed and much of it predates our study period.16–18 Our findings suggest that relying on hospitals to invest surplus in care for the underserved without incentives to do so or strong oversight is not a consistently effective strategy. Policies that target resources directly to the intended populations (for example, through health insurance coverage expansions) may more reliably improve care and access compared to policies that encourage but do not require cross-subsidization by health care providers.
Supplementary Material
Take-Away Points:
Participation in the 340B Program has not been associated with increases in hospital-reported uncompensated care provision, questioning whether the Program is achieving its stated goal of freeing up resources that are devoted to the care of low-income populations.
Our results add to a body of work that questions the extent to which Program discounts are being used by general acute-care and critical access hospitals to invest in care for low-income patients.
Our findings suggest that relying on hospitals to invest surplus in care for the underserved without marginal incentives to do so or strong oversight is not a consistently effective strategy.
Acknowledgments
Grant Support: This work was supported by grants from the Agency for Healthcare Research and Quality (U19HS024072). Sunita Desai was supported by grant number K01HS026980 from the Agency for Healthcare Research and Quality. Sunita Desai also thanks the Becker Friedman Institute Health Economics Fellowship for generous financial support. The funding sources did not play a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, and approval of the manuscript.
Footnotes
Disclosures: The authors have no conflicts to disclose.
References
- 1.Public Health Service. Federal Register: Notice Regarding Section 602 of the Veterans Health Care Act of 1992 Outpatient Hospital Facilities, Final Notice. 1994:47884–47886. https://www.340bpvp.com/resource-center/faqs/eligibility-requirements/#. Accessed April 13, 2017.
- 2.Medicaid and CHIP Payment and Access Commission. Report to Congress on Medicaid and CHIP. https://www.macpac.gov/wp-content/uploads/2016/03/March-2016-Report-to-Congress-on-Medicaid-and-CHIP.pdf. Published 2016. Accessed January 1, 2021.
- 3.Young GJ, Flaherty S, Zepeda ED, Singh SR, Cramer GR. Community benefit spending by tax-exempt hospitals changed little after ACA. Health Aff. 2018;37(1):121–124. doi: 10.1377/hlthaff.2017.1028 [DOI] [PubMed] [Google Scholar]
- 4.Desai S, McWilliams JM. Consequences of the 340B Drug Pricing Program. N Engl J Med. 2018;378:NEJMsa1706475. doi: 10.1056/NEJMsa1706475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jung J, Xu WY, Kalidindi Y. Impact of the 340B Drug Pricing Program on Cancer Care Site and Spending in Medicare. Health Serv Res. 2018:1–21. doi: 10.1111/1475-6773.12823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.340B Coalition Winter Conference. https://www.340bwinterconference.org/wc21/Overview/Wc21/Overview.aspx?hkey=38eb8c31-d3c9-46b9-b2a3-68fa60a87cbb. Accessed January 7, 2021.
- 7.Alpert A, Hsi H, Jacobson M. Evaluating the role of payment policy in driving vertical integration in the oncology market. Health Aff. 2017;36(4):680–688. doi: 10.1377/hlthaff.2016.0830 [DOI] [PubMed] [Google Scholar]
- 8.HRSA. HRSA Office of Pharmacy Affairs. 340B Database. https://opanet.hrsa.gov/340B/Views/CoveredEntity/CESearch. Published 2015. Accessed October 27, 2015.
- 9.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Vol 58. MIT Press; 2010. doi: 10.1515/humr.2003.021 [DOI] [Google Scholar]
- 10.Nikpay SS, Buntin MB, Conti RM. Relationship between initiation of 340B participation and hospital safety-net engagement. Health Serv Res. 2020;55(2):157–169. doi: 10.1111/1475-6773.13278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Desai S, McWilliams JM. Supplementary Appendix to Consequences of the 340B Drug Pricing Program. N Engl J Med. 2018;378:1–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Conti RM, Nikpay SS, Buntin MB. Revenues and Profits From Medicare Patients in Hospitals Participating in the 340B Drug Discount Program, 2013–2016. JAMA Netw Open. 2019;2(10):1–10. doi: 10.1001/jamanetworkopen.2019.14141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Office USGA. 340B Drug Discount Program: Increased Oversight Needed to Ensure Nongovernmental Hospitals Meet Eligibility Requirements; 2019. https://www.gao.gov/assets/710/703128.pdf.
- 14.Medicare Learning Network: Critical Access Hospital. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/CritAccessHospfctsht.pdf. Published 2019. Accessed January 9, 2021.
- 15.Centers for Medicare and Medicaid Services. CY 2021 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (CMS-1736-P). https://www.cms.gov/newsroom/fact-sheets/cy-2021-medicare-hospital-outpatient-prospective-payment-system-and-ambulatory-surgical-center. Published 2020. Accessed January 7, 2021.
- 16.David G, Lindrooth RC, Helmchen LA, Burns LR. Do hospitals cross-subsidize? J Health Econ. 2014. doi: 10.1016/j.jhealeco.2014.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baicker K, Staiger D. Fiscal Shenanigans, Targeted Federal Health Care Funds, and Patient Mortality. Q J Econ. 2005;120(1):345–386. doi: 10.1162/0033553053327461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Norton EC, Staiger DO. How Hospital Ownership Affects Access to Care for the Uninsured. RAND J Econ. 1994;25(1):171–185. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.