ABSTRACT
This study investigates the short-term effects of the coronavirus disease 2019 (COVID-19) pandemic lockdown on tracing and detection of tuberculosis (TB) patients in Tehran, Iran. Results of this study have demonstrated that due to the significant decrease in the identification of patients with suspected TB during the COVID-19 outbreak in Tehran, it is imperative that patients with suspected TB be tracked and diagnosed more quickly to make up for some of the decline in TB diagnosis in recent months and to recover lost cases.
KEYWORDS: tuberculosis, COVID-19, lockdowns, Iran
PERSPECTIVE
Tuberculosis (TB) remains the top cause of global mortality from infectious diseases with an estimated 1.4 million deaths in 2018 (1). In January 2020, the emergence of SARS-CoV-2 as a pandemic attracted global attention and was seen as a priority for all governments. This situation along with strict lockdowns imposed to control the pandemic has had disruptive effects on the regional routine TB services and the national program for TB elimination (2–4). Accordingly, in this study, we sought to investigate the short-term effects of the coronavirus disease 2019 (COVID-19) pandemic lockdown on tracing and detection of TB patients in Tehran, Iran.
STATISTICAL METHODS
Categorical variables are presented as n (%). Time trend curves were tested by linear trend test (Z-test statistic). Also, linear slopes and 95% confidence intervals (95% CIs) were estimated based on the nonparametric trend tests done by “sens.slope” function in the “trend” R package. Moreover, polynomial slopes and R2 for nonlinear trend curves were calculated using a robust local polynomial trend model. The patterns of data were identified using LOWESS smoother. A two-sided P value of less than 0.05 was considered statistical significance.
Biomedical and socioeconomic impacts of the COVID-19 lockdowns on tuberculosis.
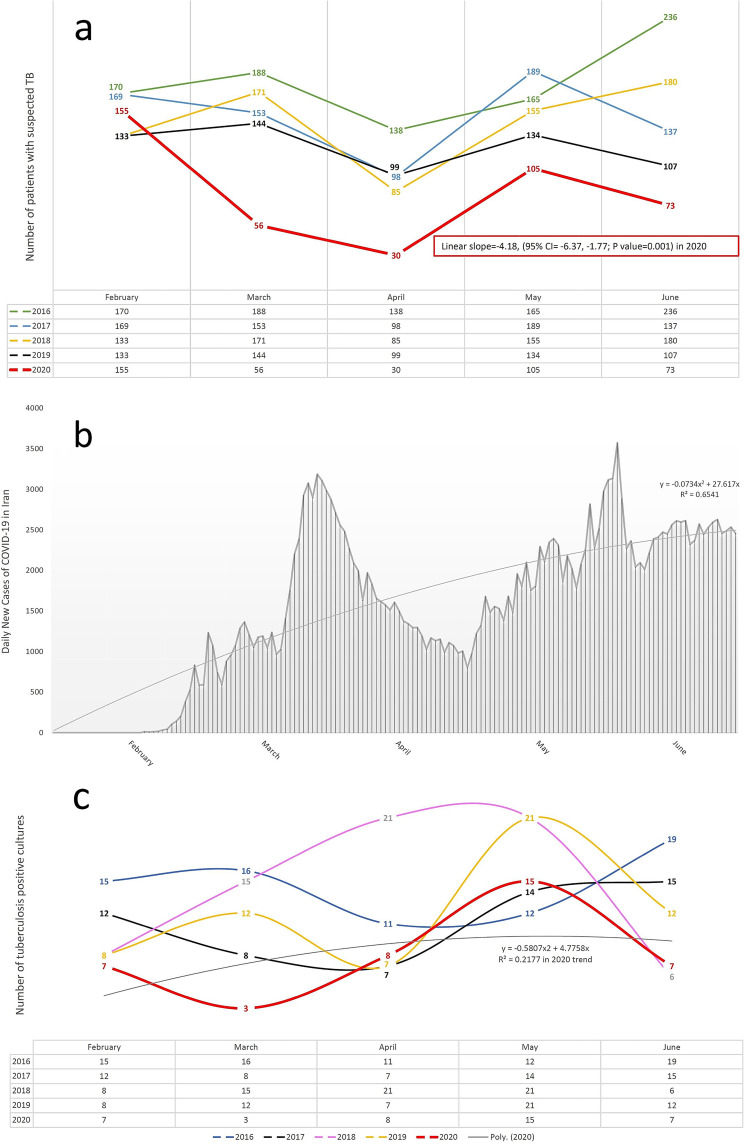
The occurrence of COVID-19 adversely affected TB incidence and deaths. The consequences of lockdowns, impaired detection of new cases of TB, and dormant TB reactivation as a result of the viral pandemic can be reasons for this situation to occur (2, 5). India has recently shown a 59% decline in the diagnosis of TB in 8 weeks of lockdown (6). It was also predicted worldwide that due to a 25% reduction in the diagnosis of TB in a 3-month period of lockdown, 190,000 additional deaths due to TB would occur in 2020 (3). Interestingly, the decline in multidrug resistance (MDR) TB screening in China occurred at the time of the COVID-19 outbreak (7). Another report also predicted that due to lockdown, 4% of surplus deaths in the world and 5.7% of surplus deaths in India will happen due to TB between 2020 and 2025 (4). Also, a recent study in Italy showed that despite efforts to maintain TB services, these services were significantly disrupted during the COVID-19 outbreak (8). Our short-term study of the statistics of patients with suspected TB during the COVID-19 outbreak and the resulting lockdown in Iran also confirms these results and predictions. Our review shows that the number of patients with suspected TB in March and April 2020 (simultaneously with the outbreak of the COVID-19 epidemic in Iran) had a sharp decrease compared to previous years (65.9% and 71.4% decrease, respectively). In other words, the linear slope of the suspected TB patient trend curve in 2020 was −4.18 (95% CI = −6.37, −1.77; P value = 0.001). Also, in 2016, 2018, and 2019, there was an increase in the number of patients with suspected TB in March compared to February, but in 2020, we saw a sharp decrease in the number of patients with suspected TB in March compared to February. In all months of the outbreak of COVID-19 in Iran (from March to June 2020), the lowest number of patients with suspected TB was recorded (55.6% decrease) compared to previous years (2016 to 2020) (Fig. 1a).
FIG 1.
Changes in frequency of suspected TB patients, TB-positive cultures, and COVID-19 patients. (a) Frequency of suspected TB patients who were registered at the Department of Mycobacteriology and Pulmonary Research, Pasteur Institute of Iran, between 2016 and 2020 (February to June in each year). (b) Daily number of COVID-19 patients in Iran. (c) Number of TB-positive cultures between February and June, 2016 to 2020. Poly. (2020), polynomial trend curve (2020).
These results were obtained in a situation where March and April were part of the period of lockdown and closure of jobs in Iran, because the number of patients with COVID-19 peaked in March and April (9), many businesses closed in those 2 months, and most people tried to lock themselves down. At the end of April, the number of COVID-19 patients per day decreased. But most of the jobs in Iran resumed in May and lockdowns were lifted, which led to a reincrease in the number of people with COVID-19 in Iran from May onwards. The polynomial slope of the COVID-19 time trend curve was (−0.073 × time2 + 27.61 × time, R2 = 0.65) (Fig. 1b).
Also, the number of TB-positive cultures in March 2020 was the lowest compared to the same month in all previous years (76.5% decrease). The polynomial slope of the TB-positive culture time trend curve was (−0.58 × time2 + 4.77 × time, R2 = 0.217) in 2020 (Fig. 1c).
All of these statistics reflect the fact that lockdowns due to COVID-19 had a significant impact on the identification of TB patients in this short period.
Decreased diagnosis of TB can be due to the lockdown and the fear of visiting health centers (to diagnose TB) during COVID-19 lockdown (2). On the other hand, our data show that in all months (even after the lockdown was lifted in May) of the outbreak of the COVID-19 epidemic in Iran (from March to June 2020), the lowest number of patients with suspected TB (55.6% decrease) was recorded compared to previous years (2016 to 2020). This can be caused by the fear of going to health centers (to diagnose TB) throughout the COVID-19 outbreak.
Perhaps another reason for the decrease in patients with suspected TB in Iran (simultaneously with the outbreak of the COVID-19 epidemic) is the similarity of the symptoms of COVID-19 and TB. People with these two diseases show similar clinical manifestations such as fever, cough, and respiratory problems, and both diseases initially affect the lungs (10). Thus, perhaps in this pandemic period most people focus only on COVID-19, and after such symptoms occur, they suspect only COVID-19 and seek home treatment or visit COVID-19 diagnostic centers. This can be even more frustrating when a person has the two diseases simultaneously, because predictions show that people with both TB and COVID-19 can have poorer treatment outcomes, especially if TB treatment is disrupted (10). Furthermore, people who have a current TB infection or a history of TB are more likely to have more severe consequences after a COVID-19 infection due to lung damage (4, 11, 12). Therefore, TB should not be overlooked during the outbreak of COVID-19.
Another problem that has arisen during the COVID-19 lockdown has been the increase in unemployment and poverty in a significant part of Iranian society. In this regard, the Iranian Ministry of Labor has announced that 783,000 people have complained of unemployment since 13 March 2020. A government spokesman also said that 4 million jobs are at risk of being lost as a result of the COVID-19 outbreak and that 10 business groups were closed as soon as the virus was confirmed (13). These will cause poverty in Iranian society, and poverty is directly related to malnutrition. Malnutrition causes TB to progress to active TB because poor nutrition impairs innate and adaptive immunity (14). It has also been recently shown that about half of people with TB were poor (15). Other studies have also shown that reduced protein intake in poor people increases their risk of developing TB (16, 17). Thus, lockdowns due to COVID-19 can increase TB in the long term by increasing poverty, unemployment, and malnutrition.
CONCLUSION
Due to the significant decrease in the identification of patients with suspected TB during the COVID-19 outbreak in Tehran, it is imperative that patients with suspected TB be tracked and diagnosed more quickly to make up for some of the decline in TB diagnosis in recent months, to recover lost cases, and also to mitigate the impact of COVID-19 on routine TB services and TB incidence and mortality. Lockdowns should also be managed in such a way that a dangerous infectious disease such as TB is not ignored.
ACKNOWLEDGMENT
No acknowledgments to disclose.
Contributor Information
Farzam Vaziri, Email: f_vaziri@pasteur.ac.ir.
Michael J. Imperiale, University of Michigan-Ann Arbor
REFERENCES
- 1.WHO. 2019. WHO global report, global tuberculosis report 2019. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 2.Bhargava A, Shewade HD. 2020. The potential impact of the COVID-19 response related lockdown on TB incidence and mortality in India. Indian J Tuberc 67:S139–S146. doi: 10.1016/j.ijtb.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glaziou P. 2020. Predicted impact of the COVID-19 pandemic on global tuberculosis deaths in 2020. medRxiv doi: 10.1101/2020.04.28.20079582. [DOI] [Google Scholar]
- 4.Stop TB Partnership. 2020. The potential impact of the COVID-19 response on tuberculosis in high-burden countries: a modelling analysis. http://www.stoptb.org/assets/documents/news/Modeling%20Report_1%20May%202020_FINAL.pdf.
- 5.Pathak L, Gayan S, Pal B, Talukdar J, Bhuyan S, Sandhya S, Yeger H, Baishya D, Das B. 2020. Corona virus activates a stem cell mediated defense mechanism that accelerates activation of dormant tuberculosis: implications for the COVID-19 pandemic. bioRxiv doi: 10.1101/2020.05.06.077883. [DOI] [PMC free article] [PubMed]
- 6.National Tuberculosis Elimination Programme. 2020. Nikshay reports. TB notification. National Tuberculosis Elimination Programme, Ministry of Health and Family Welfare, Government of India, New Delhi, India. https://reports.nikshay.in/Reports/TBNotification. Accessed 11 June 2020.
- 7.Liu Q, Lu P, Shen Y, Li C, Wang J, Zhu L, Lu W, Martinez L. 2020. Collateral impact of the coronavirus disease 2019 (COVID-19) pandemic on tuberculosis control in Jiangsu Province, China. Clin Infect Dis doi: 10.1093/cid/ciaa1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Magro P, Formenti B, Marchese V, Gulletta M, Tomasoni LR, Caligaris S, Castelli F, Matteelli A. 2020. Impact of the SARS-CoV-2 epidemic on tuberculosis treatment outcome in Northern Italy. Eur Respir J 56:2002665. doi: 10.1183/13993003.02665-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Worldometer. 30 June 2020. COVID-19 coronavirus pandemic. https://www.worldometers.info/coronavirus/#countries.
- 10.WHO. 11 May 2020. World Health Organization (WHO) information note. Tuberculosis and COVID-19. https://www.who.int/docs/default-source/documents/tuberculosis/infonote-tb-covid-19.pdf.
- 11.Ravimohan S, Kornfeld H, Weissman D, Bisson GP. 2018. Tuberculosis and lung damage: from epidemiology to pathophysiology. Eur Respir Rev 27:170077. doi: 10.1183/16000617.0077-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stop TB Partnership. 2019. Global plan to end TB: 2018–2022. The paradigm shift. http://www.stoptb.org/assets/documents/global/plan/GPR_2018-2022_Digital.pdf.
- 13.EghtesadOnline. 11 May 2020. Unemployment filing amid coronavirus. https://www.en.eghtesadonline.com/Section-economy-4/32399-labor-force-participation-rate-at-in-fiscal.
- 14.Bhargava A. 2016. Undernutrition, nutritionally acquired immunodeficiency, and tuberculosis control. BMJ 355:i5407. doi: 10.1136/bmj.i5407. [DOI] [PubMed] [Google Scholar]
- 15.Shewade HD, Gupta V, Satyanarayana S, Kharate A, Sahai KN, Murali L, Kamble S, Deshpande M, Kumar N, Kumar S, Pandey P, Bajpai UN, Tripathy JP, Kathirvel S, Pandurangan S, Mohanty S, Ghule VH, Sagili KD, Prasad BM, Nath S, Singh P, Singh K, Singh R, Jayaraman G, Rajeswaran P, Srivastava BK, Biswas M, Mallick G, Bera OP, Jaisingh AJJ, Naqvi AJ, Verma P, Ansari MS, Mishra PC, Sumesh G, Barik S, Mathew V, Lohar MRS, Gaurkhede CS, Parate G, Bale SY, Koli I, Bharadwaj AK, Venkatraman G, Sathiyanarayanan K, Lal J, Sharma AK, Rao R, Kumar AMV, Chadha SS. 2018. Active case finding among marginalised and vulnerable populations reduces catastrophic costs due to tuberculosis diagnosis. Glob Health Action 11:1494897. doi: 10.1080/16549716.2018.1494897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cegielski JP, Arab L, Cornoni-Huntley J. 2012. Nutritional risk factors for tuberculosis among adults in the United States, 1971–1992. Am J Epidemiol 176:409–422. doi: 10.1093/aje/kws007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boccia D, Hargreaves J, De Stavola BL, Fielding K, Schaap A, Godfrey-Faussett P, Ayles H. 2011. The association between household socioeconomic position and prevalent tuberculosis in Zambia: a case-control study. PLoS One 6:e20824. doi: 10.1371/journal.pone.0020824. [DOI] [PMC free article] [PubMed] [Google Scholar]