Abstract
Early diagnosis is critical for the prevention and control of the coronavirus disease 2019 (COVID-19). We attempted to apply a protocol using teleultrasound, which is supported by the 5G network, to explore the feasibility of solving the problem of early imaging assessment of COVID-19. Four male patients with confirmed or suspected COVID-19 were hospitalized in isolation wards in two different cities. Ultrasound specialists, located in two other different cities, carried out the robot-assisted teleultrasound and remote consultation in order to settle the problem of early cardiopulmonary evaluation. Lung ultrasound, brief echocardiography, and blood volume assessment were performed. Whenever difficulties of remote manipulation and diagnosis occurred, the alternative examination was repeated by a specialist from another city, and in sequence, remote consultation was conducted immediately to meet the consensus. The ultrasound specialists successfully completed the telerobotic ultrasound. Lung ultrasound indicated signs of pneumonia with varying degrees in all cases and mild pleural effusion in one case. No abnormalities of cardiac structure and function and blood volume were detected. Remote consultation on the issue of manipulation practice, and the diagnosis in one case was conducted. The cardiopulmonary information was delivered to the frontline clinicians immediately for further treatment. The practice of teleultrasound protocol makes early diagnosis and repeated assessment available in the isolation ward. Ultrasound specialists can be protected from infection, and personal protective equipment can be spared. Quality control can be ensured by remote consultations among doctors. This protocol is worth consideration as a feasible strategy for early imaging assessment in the COVID-19 pandemic.
Keywords: 5G network, coronavirus disease 2019 (COVID-19), infectious disease, telerobotics, ultrasound
I. Introduction
There is a new public health crisis threatening the world with the emergence and spread of 2019 novel coronavirus or the severe acute respiratory syndrome coronavirus 2 [1]–[3]. Since November 2019, the coronavirus disease 2019 (COVID-19) has been spreading in China, and now it is prevailing worldwide. According to the World Health Organization (WHO) situation report of March 30, 2020, a total of 638 146 confirmed cases globally, 82 356 confirmed in China, with 30 039 deaths (4.7%) and 555 790 cases confirmed outside of China in 202 different countries, areas or territories [4], [5]. In China, the epidemic was effectively controlled in late March, 2020 after great efforts.
In the severely affected cities, such as Wuhan, Hubei Province, China, during the early epidemic period, medical resources are severely insufficient because there are extensive suspicious cases waiting for test and abundant confirmed cases needing treatment. To cope with this situation, early diagnosis is critical. The major diagnostic measures include chest CT scan and laboratory examinations. In terms of timely diagnosis, reverse transcription-polymerase chain reaction (RT-PCR) test, as a reference standard to make a definite diagnosis, is initially only 30%–70% sensitive for acute infection [6], [7], while CT examination is difficult to carry out timely in the patient-gathering primary hospitals and is hardly completed in instrument-insufficient cabin hospitals. More feasible methods for early diagnosis are needed especially in the current pandemic.
Ultrasound can be used at the patient’s bedside [8] to detect the occurrence and development of lung inflammation and to evaluate the therapeutic effect on time [9]–[12]. On March 4, the Chinese government released the Pneumonia Treatment Program for COVID-19 (Trial 7th Edition) to increase COVID-19’s concerns for children and pregnancy, highlighting early warning of severe and critical illness [13]. CT examination is not routinely performed for children and pregnant women, while bedside imaging assessment of critically ill patients relies heavily on ultrasound examination [14]–[17].
In this outbreak, the critical illness morbidity is high in Wuhan. In one single-center case series of 138 hospitalized patients with confirmed COVID-19 in Wuhan, 26% of patients received ICU care, and mortality was 4.3% [18]. Making the situation worse, many inspection instruments, such as a stethoscope, can hardly be used in the isolation ward because the healthcare workers are wearing personal protective equipment (PPE) clothing. Furthermore, without medical imaging, many key problems are difficult to solve, such as monitoring of pneumonia development, assessment of blood volume, detection of myocardial injury, deep venous thrombosis and pulmonary embolism, intestinal paralysis, and toxic organ damage. Fortunately, these problems can be solved by bedside ultrasound. In the epidemic area, the number of patients increased dramatically, and thus, the problems of lacking medical resources and ultrasound specialists arose. More specifically, many frontline doctors were not familiar with lung ultrasound. PPE and portable ultrasound equipment were also insufficient. They were hard to meet the clinical requirements. In spite of the highlighted advantages of bedside ultrasound in daily intensive care, the ultrasound clinicians working in the affected areas should be in close contact with patients, increasing the risk of exposure to the coronavirus and consuming more medical resources.
The powerful artificial intelligence and telemedicine technologies have emerged, which could potentially make a major contribution to the current outbreak. Teleultrasound, both in synchronous mode and asynchronous mode, can be used across remote distance. Robot-assisted teleultrasound, which is controlled by a skilled sonographer in the remote area, can act as the synchronous mode under a 5G network. Asynchronous mode usually needs on-site operation by a sonographer. Considering the risk of infection suffered by medical staffs during bedside ultrasound examination, the synchronous mode by robot-assisted teleultrasound is more applicable to the current context than the asynchronous mode. With the help of the robot-assisted teleultrasound under 5G network, we have successfully carried out remote consultation and remote manipulation for ultrasonic diagnosis and treatment between a continental city and an oceanic island, across a long distance of 2606 kilometers. We also carried out robot-assisted teleultrasound examination in a routine manner for the diagnosis of acute abdominal diseases, including calculous cholecystitis, appendicitis, pancreatitis, and urolithiasis. In addition, teleultrasound has been applied in many other fields, such as focused assessment with sonography for trauma (FAST) and extended FAST, musculoskeletal injuries, thyroid gland diseases, and subcutaneous soft tissue lesions.
Considering the merits of bedside ultrasound and teleultrasound, we believed that the problems of timely imaging assessment of COVID-19 could be settled. Therefore, we proposed a bedside ultrasound protocol using 5G network-based robotic teleultrasound and remote consultation to examine the suspected and confirmed COVID-19 patients in the epidemic areas. To validate the protocol, we conducted a pilot study using teleultrasound among multiple cities to timely deliver professional sonographic skills and diagnosis from specialists into isolation ward. We are aiming to seek a feasible strategy for early diagnostic imaging during such a current infectious public health event.
II. Subjects and Methods
A. Subjects
Four male patients involved in this study were all suffered from cough and fever for 3–5 days. Two of them were residents of the city of Wuhan, aged 45 (case 1) and 61 (case 2). They were confirmed COVID-19 by positive PCR test of throat swabs and clinical manifestations and were hospitalized for treatment in a mobile cabin hospital in Wuhan, which was temporarily reconstructed from a stadium. Chest CT examination was not completed because of the inaccessible instrument, resulting in an urgent demand of cardiopulmonary evaluation.
The other two patients were residents of the city of Tongxiang, Zhejiang Province, China, and were sent to an isolation ward of a primary hospital in Tongxiang because of suspicious COVID-19. Neither of them had recent travel history to Wuhan and the PCR tests were negative. One patient aged 70 (case 3) had completed chest CT examination, showing a pneumonia which was difficult to be differentiated from COVID-19. Another patient aged 75 (Case 4) had not gone through CT examination yet, but urgently needed a cardiopulmonary evaluation because of a sudden deterioration. Hence, requests for teleultrasound were sent out from clinicians.
B. Problem Solving Protocol
As medical imaging for cardiopulmonary evaluation was urgently demanded in all cases, we arranged a protocol to settle this problem, involving multiple teleultrasound via 5G network.
Demonstration of the protocol for cases 1–4 is indicated as follows and also shown in Fig. 1.
-
1)
Each patient received a single robot-assisted teleultrasound examination executed by a specialist either from Sanya or from Hangzhou.
-
2)
In terms of the doctor’s side, each specialist would carry out multiple teleultrasound on several different patients from different cities.
-
3)
Whenever difficulties in the remote manipulation or differential diagnosis appeared, a repeated examination on the same patient was carried out by a specialist from another city.
-
4)
Group teleconsultation was conducted between the two doctor sides. After consensus was agreed, the detailed ultrasonic information was instantly delivered to the clinicians on the patient side for further diagnosis and management.
Fig. 1.
Working schematic of robot assisted teleultrasound protocol. Each ultrasound specialist from Sanya (DS1) or from Hangzhou (DS2) carries out robot-assisted teleultrasound on several patients in different cities, which is one-to-many mode. Each patient is able to receive repeated teleultrasound examination executed by different specialists from DS1 and DS2, which is many-to-one mode. Group remote consultation is conducted between the doctors in DS1 and DS2 to meet the consensus whenever difficulties of manipulation and diagnosis appear. All the procedure is supported by 5G network through a cloud server.
C. Teleultrasound System
An MGIUS-R3 robotic ultrasound system (MGI Tech Co., Ltd., Shenzhen, China) was adopted in the teleultrasound examination. It consists of a doctor-side subsystem and a patient-side subsystem, and a high-definition audio–video communication system as well. The patient-side subsystem consists of a pressure sensor, a robotic arm that can achieve 6 degrees of freedom (DOF) movement, and a 64-channel portable ultrasound system. The ultrasound instrument was specially designed by Wisonic Co., Ltd., Shenzhen, and was equipped with multiple replaceable probes, including a linear probe with the frequency ranging 4–15 MHz, a curved probe with the frequency ranging 1–5 MHz, and a sector probe with the frequency ranging 1–4 MHz. In this study, the curved probe was adopted for lung ultrasound and blood volume assessment, while the sector probe was adopted for brief echocardiography. The linear probe was also adopted for lung ultrasound. The probe was handled firmly and controlled directly by the robotic arm, and could be taken down and replaced by a medical assistant. The doctor-side subsystem mainly includes a duplicate control panel of the ultrasound instrument, a handheld controller which can control the robotic arm though sensors, and a screen to display ultrasonic images. The handheld controller has six DOFs, including three DOFs for rotation of a gesture sensor, two DOFs for the movement on horizontal plane of a position sensor, and one DOF for the up and down movement of a pressure sensor. The duplicate control panel enables sonographer to adjust all the settings on the panel such as gain, depth, and focus [Fig. 2(a)], (Media-Movie 1). The robotic arm in patient side can perform the remote ultrasound scanning with a contact force ranging 3–40 N [Fig. 2(b)], (Media-Movie 2). The safety measures, including the working space limit of 600 mm
 mm
mm
 mm and impact force limit of 120 N also provide a viable solution to carry out the teleultrasound examination. The original images were acquired from the ultrasound instrument in the patient side and instantly transmitted to the doctor side through 5G network. In order to ensure the transmission efficiency under a certain bandwidth of the network condition, they were compressed before transmission. The quality of the images had been previously quantified by the instrument supplier. According to the supplier, the peak signal-to-noise ratio and visual multimethod assessment fusion of the transmitted image and original image were 46.88 and 98.85, respectively, which demonstrated that the image loss after compression was relatively low and the quality meet the demand of clinical diagnosis. The system had got European Conformity (CE) and National Medical Products Administration of China approved after 90 clinical trials, which also validated the image quality. The communication system allows real-time consultation among the patients and assistants at the patient site and doctors at a single or multiple doctor site.
mm and impact force limit of 120 N also provide a viable solution to carry out the teleultrasound examination. The original images were acquired from the ultrasound instrument in the patient side and instantly transmitted to the doctor side through 5G network. In order to ensure the transmission efficiency under a certain bandwidth of the network condition, they were compressed before transmission. The quality of the images had been previously quantified by the instrument supplier. According to the supplier, the peak signal-to-noise ratio and visual multimethod assessment fusion of the transmitted image and original image were 46.88 and 98.85, respectively, which demonstrated that the image loss after compression was relatively low and the quality meet the demand of clinical diagnosis. The system had got European Conformity (CE) and National Medical Products Administration of China approved after 90 clinical trials, which also validated the image quality. The communication system allows real-time consultation among the patients and assistants at the patient site and doctors at a single or multiple doctor site.
Fig. 2.
Performance of robot-assisted teleultrasound based on the 5G network. (a) Doctors on the doctor side are manipulating a handheld controller, which can control the robotic arm. The duplicate control panel is used to adjust all the settings such as gain, depth, focus, and so on, as is performed on a real-ultrasound instrument. The screen is displaying ultrasonic images, and is monitoring the activities of the robotic arm and the probe. (b) Patient is receiving robotic lung ultrasound in the isolation ward, where there is no ultrasound specialist.
D. 5G Network
All the teleultrasound procedures and communications were based on a 5G network, which was supported by China Mobile Communications Group Co., Ltd., Beijing, China, and China Telecom Co., Ltd., Beijing. Customer premise equipment (5G CPE Pro, Huawei Device Co., Ltd., Shenzhen) was applied to provide the wireless gateway for 5G network that exchanged data between wireless WANs and wired or wireless local area networks. It was able to customize the network with desirable characteristics, such as low latency for smooth controlling of the robotic system and high bandwidth for live communication between the doctor side and the patient side. The upload rate, download rate, network latency, and package loss were recorded during all the procedures.
E. Robot-Assisted Teleultrasound Procedure
The patient-side subsystem was placed bedside, and the essential preparations were done with the help of a medical assistant. These preparations included the booting of the subsystem, the application of an ultrasonic coupling agent after the exposure of the patient’s chest and back, and the adjustment to a suitable position so that the robotic arm could reach the body. The patients were placed initially at a supine position and changed to left or right lateral position and a prone position when needed.
Acquisition of medical history and clinical demand was carried out through a high-definition audio–video communication system before scanning. Once teleultrasound examination began, the ultrasound specialist in the doctor side manipulated the handheld controller to control the robotic arm, holding the probe for scanning, and operated the duplicate control panel simultaneously, adjusting imaging parameter to obtain satisfactory ultrasonic images displayed in the screen, similar to a standard ultrasound examination. Real-time consultation between the patient and the doctor was carried out whenever needed.
Considering that the critically ill patients might not cooperate well, e.g., adjusting a proper examination position and that medical workers were occupied by overloaded healthcare tasks in the isolation ward, fast and brief lung ultrasonography was performed using a 12-zone method examination [19]. Brief echocardiography was performed to obtain the parasternal long-axis view and apical four-chamber view for fast assessment of the cardiac structure and function. For blood volume assessment, inferior vena cava (IVC) measurement in a longitudinal section under xiphoid process was achieved by M-mode ultrasound [20].
Because the imaging protocol was crucial for lung ultrasound [21], [22], the imaging parameters were strictly restricted. When using the curved probe, the frequency was 4.5 MHz, and the mechanical index was 0.8–1.1. When using the linear probe, the frequency was 10.0 MHz and the mechanical index was 0.5–0.7. During all the lung ultrasound, a single-focal point was adopted. To visualize the artifacts, such as A-lines (horizontal artifacts) and B-lines (vertical artifacts) [23], [24], and to clearly confirm the pleural lesion or the subpleural lesion, the focal point was set at the level of pleural line or deeper, not exceeding the first A-line in depth. The scanning depth varied from 4 to 10 cm, according to different imaging purposes and different patients. To detect the pleural lesion, the depth was set two folds of the distance between chest surface and pleural line. To observe the artifacts, the depth was set 3–4 folds of the distance where the second or the third A-line might be observed.
Protective measures were carried out by a medical assistant after the performance of teleultrasound on each patient, including the disinfection of the robotic arm and the probe.
F. Remote Consultation
When the difficulty of remote manipulation in one city occurred, another specialist in another city would repeat the manipulation on the same patient, in order to acquire satisfying images. Once there was a doubt in diagnosis or differential diagnosis, a group consultation would be held through the online communication system, which bridged the two doctor sites. The doubted issues concerning diagnosis were discussed until consensus was achieved, and in sequence, the detailed ultrasound information was instantly delivered to the clinicians on the patient side for further clinical diagnosis and management.
III. Results
The ultrasound specialists from the cities of Sanya, China, and Hangzhou, China, completed the robot-assisted teleultrasound with the aids of 5G network, timely providing essential imaging information for clinical usage.
Ultrasound specialists in Sanya completed the robotic teleultrasound on case 1, while specialists in Hangzhou examined case 2. Each patient accepted a single examination because no difficulties occurred in the remote operation and diagnosis. The remote examination was performed on cases 3 and 4 by specialists in Sanya and Hangzhou, respectively, and repeated alternatively due to the difficulties in scanning and differential diagnosis of pneumonia. Each teleultrasound procedure took about 10–20 min.
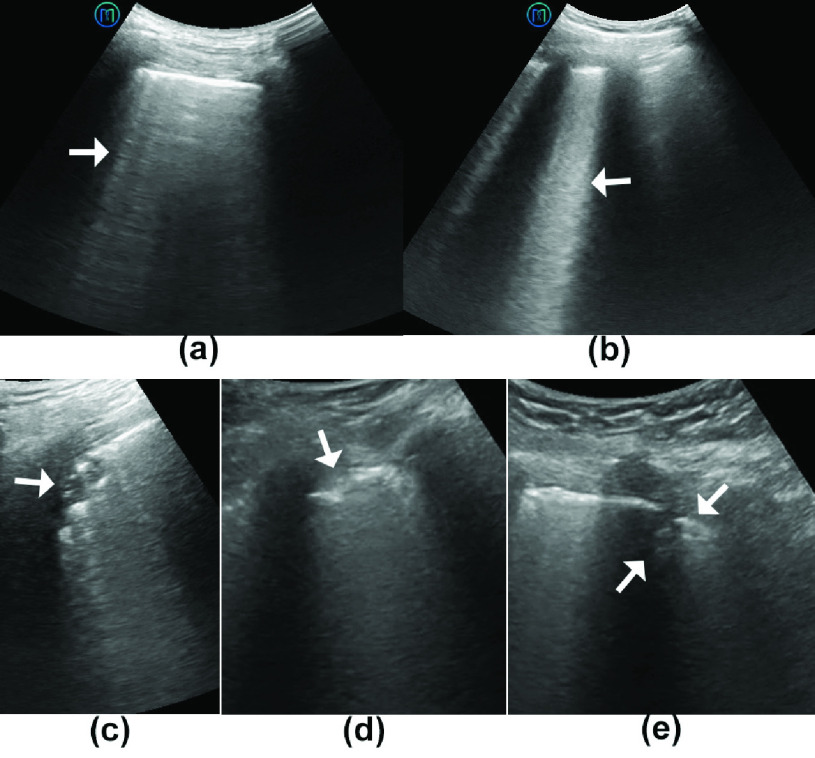
In terms of ultrasound manifestations, all the above confirmed and suspected COVID-19 cases showed varying lung abnormalities in bilateral lungs (Table I). Common findings in all the four cases included irregularity of pleural lines (from indented to thickened or broken), disappearance of A-lines, and presence of B-lines. Dense and largely extended white lung existed in the two confirmed cases (Fig. 3) (Media-Movie 3). Large lung consolidation below the pleural line was found in two confirmed cases, and small lung consolidation was found in one suspected case (case 4). Lung sliding remained in all cases. No pleural effusion was found except bilateral mild effusion in case 4 (suspected case). According to the scoring system developed by Soldati et al. [25], two confirmed cases were scored 3, while two suspected cases were scored 1 (case 3) and 2 (case 4), respectively. The manifestations were consistent with pneumonia, confirmed by chest CT examination. Ejection fractions of left ventricle measured on the M-mode echocardiogram at parasternal long axis view were all greater than 60%, indicating a well systolic cardiac function. Neither abnormalities of atrioventricular size and morphology nor pericardial effusion was found. The ultrasound findings of the heart indicated no special feature of novel coronavirus infection in the four cases. No blood volume abnormalities by IVC measurements were found (Table I).
TABLE I. Brief Summary of Cardiopulmonary Manifestation.
| Confirmed COVID-19 | Suspected COVID-19 | |||
|---|---|---|---|---|
| Case 1 | Case 2 | Case 3 | Case 4 | |
| Lung ultrasound | ||||
| Disappearance of A-lines | + | + | + | + |
| Presence of B-lines | + | + | + | + |
| Irregularity of pleural line | broken | broken | indented | thickened |
| Subpleural consolidation | small | large | – | small |
| White lung | + | + | – | – |
| Pleural effusion | – | – | – | Mild |
| Score | 3 | 3 | 1 | 2 |
| Brief Echocardiography | ||||
| Atrioventricular size and morphology | – | – | – | – |
| Cardiac function (LVEF %) | 65 | 59 | 60 | 63 |
| Volume assessment | – | – | – | – |
Score 0: The pleura line is continuous and regular. A-lines (horizontal artifacts) are present.
Score 1: The pleura line is indented. B-lines (vertical artifacts) are visible.
Score 2: The pleura line is broken. Small to large consolidated areas appear with white lung.
Score 3: Dense and largely extended white lung with or without larger consolidations.
LVEF: ejection fraction of left ventricle, measured by M-mode ultrasonography.
Fig. 3.
Lung ultrasound manifestations of confirmed and suspected COVID-19 patients. (a) B-lines (vertical artifacts) appear (arrow), while the A-lines (horizontal artifacts) disappear. (b) White lung (arrow) exists in a confirmed COVID-19 patient. (c) Ultrasound findings from a confirmed COVID-19 patient show a local consolidation (arrow) beneath the broken pleural line. (d) Irregularity of the pleural line is found in all the confirmed and suspected COVID-19 patients. The pleural line is indented and thickened (arrow). (e) Small consolidation area (arrow) is found in a suspected COVID-19 patient.
The practice of remote manipulation on case 3 and case 4 was discussed among the specialists in the two doctor sides. Remote consultation on the issue of the relationship between pleural effusion and COVID-19 in case 4 was conducted after the repeated examination. After twice of remote examination and timely consultation, the diagnostic information concerning cardiopulmonary function, which was advantageous for further diagnosis and management, was delivered to the clinicians on the patient side immediately.
During the teleultrasound procedures and communications, the download rate of the network was 930 Mbps and the upload rate of 130 Mbps, approximately remaining at a stable level. No package loss was detected during all the procedures. The network latency was 23–30 ms and the network jitter was 1–2 ms. This network condition contributed to the smooth scanning by the robotic arm and the time delay was almost unaware.
Despite the previous image compression before transmission, the quality of the images transmitted to the doctor’s side has no visual reduction compared with those obtained by traditional on-site examination and did not affect the clinical diagnosis.
IV. Discussion
With the rapid increase of COVID-19 patients, medical resources are increasingly lacking, especially in severely affected areas. As a reliable imaging tool in the diagnosis and follow-up assessment of the cardiopulmonary function of critically ill patients, ultrasound was urgently demanded in the isolation ward [26]. Concerning the high contagious coronavirus and insufficient medical resources, the on-site examination would increase the risk of cross infection. We carried out the protocol of teleultrasound and remote consultation among multiple cities in this pilot practice and had partially overcome the difficulties. This novel method combines one-to-many examination mode, many-to-one examination mode, and cloud discussion, which can not only protect doctors from being infected but also save protective equipment (isolation gowns, medical masks, goggles, and so on) which is in short supply in frontline. This protocol integrated top medical resources, especially ultrasound, and thus, improved diagnostic accuracy. In addition, although the epidemic is effectively controlled in Wuhan and other most affected areas in China, the follow-up of confirmed patients, especially those in sever conditions, can also be accomplished by teleultrasound via this protocol, which is critical to further study.
In the above-mentioned cases, the doctor site, which was located in the cities of Sanya and Hangzhou, is about 1756 and 55 km away from the patient site in the city of Tongxiang, respectively, and about 1479 and 560 km away from the patient site in the city of Wuhan, respectively. Despite such remote distances among multiple cities, the practice of teleultrasound was acceptable, in terms of scanning experience and image quality. Thanks to 5G network, robot-assisted teleultrasound succeeded in the assessment of cardiopulmonary function and blood volume. Teleultrasound provided plenty of diagnostic information for helping further treatment, with the absence of chest CT examination. Although ultrasound lacked the diagnostic specificity of COVID-19 and could not be served as the confirming standard, lung ultrasound was a useful tool for the evaluation of many different lung conditions. Pleural or subpleural abnormalities were easy to be detected. Several distinct artifacts, such as A-lines, B-lines, and white lung, were observed during the lung ultrasound examination of the confirmed and suspected COVID-19 patients. Interpretation of these ultrasound artifacts made differential diagnosis between a normally aerated lung and a lung with interstitial pathology possible. They were useful to recognize and evaluate several pathological conditions [27], [28]. The lung ultrasound scoring system was useful in the evaluation of the patients, supporting the diagnosis of COVID-19 pneumonia [25]. Cardiac structure, function, and blood volume assessment could be evaluated for further clinical management of patients with confirmed or suspected COVID-19. All the procedures were successfully and timely completed, making the application available in isolation ward of either cabin hospital or primary hospital during COVID-19 outbreak.
5G network bridges the gaps between specialists and patients from remote cities, breaking the temporal and spatial limitations. Teleultrasound shares professional skills and ameliorates the medical resource-scarce situation. This protocol is a novel and efficient solution for the current severe COVID-19 outbreak. One specialist can provide medical service for multiple remote patients and obtain reliable imaging data. As ultrasound is highly operator dependent, unqualified images acquired by the unskilled operator may result in misdiagnosis or neglect of important information. Meanwhile, one patient can receive different professional services. Once difficulties of diagnosis or scanning occurred, interhospital consultation among specialists can be instantly conducted through 5G network.
This protocol has several advantages [29]: 1) high-quality ultrasound diagnosis and professional sonographic skills can be delivered seamlessly into the COVID-19 outbreak area where most medical instruments are inaccessible. 2) Early diagnosis and repeated assessment can be achieved in confirmed or suspected patients, with the absence of other important diagnostic methods. 3) Protective medical materials, which is scarce during the pandemic, can be spared since fewer medical staffs are involved. 4) Infectious exposure to the coronavirus can be minimized, and ultrasound specialists can be protected from being infected without close contact with infected patients. 5) Quality control can be ensured by remote consultations. The ultrasound training can also be conducted through real time manipulation and instruction. 6) Experts can gather large numbers of cases during a very short period of time and share the experience after professional analysis and review. This is prior to the work from a single-medical agency with relatively small number of cases, where healthcare workers were occupied by overload works in the frontline combating COVID-19. 7) 5G network enables a rapid response to the clinical request for remote scanning and consultation, compared with the commonly used 4G or 3G network currently.
Despite the advantages of this protocol, there are still some issues to be concerned about. As the basis of teleultrasound, a 5G network should be set up on both the doctor side and patient side, and the stability should be guaranteed through the whole procedure. The disinfection of the instrument, especially the robotic arm and the probe, should be concerned in order to avoid cross infection. Of note, this is a pilot study with a limited number of patients, and thus, lacks quantitative analysis. Larger number of patients should be involved in further studies to further validate the protocol and the teleultrasound system.
V. Conclusion
The clinical practice of the four cases of robot-assisted teleultrasound provides the possibility in solving the problem of early imaging of patients with confirmed or suspected COVID-19 in isolation ward. With the aids of 5G network, the protocol of teleultrasound is applicable and is worth consideration as a feasible strategy during such a current infectious public health event.
Biographies
Shengzheng Wu was born in Shantou, China. He received the bachelor’s degree in medical imaging from First Military Medical University, Guangzhou, China, in 2005, and the master’s and Ph.D. degrees in medical imaging from Third Military Medical University, Chongqing, China, in 2015.
She is currently with the Department of Ultrasound, Hainan Hospital of Chinese People’s Liberation Army General Hospital, Sanya, China. His research interests include teleultrasound and contrast-enhanced ultrasound.
Dr. Wu is a member of the Chinese Medical Equipment Technology Association.

Dudu Wu was born in Xianyang, Shannxi, China, in 1995. She received the bachelor’s degree in clinical medicine from the Military Medical University of Air Force, Xi’an, China, in 2018, where she majors in abdominal ultrasound, vascular ultrasound, and cardiac ultrasound.
Since 2018, she has been a Junior Resident with the Department of Ultrasound, Hainan Hospital of Chinese People’s Liberation Army General Hospital, Sanya, China.
Dr. Wu was a recipient of the Young Investigator Scholarship (English) of 2019 WIFUMB and the Young Investigator Scholarship (English) of 2019 ACUCI.

Ruizhong Ye was born in Wenzhou, China, in 1980. He received the bachelor’s degree in clinical medicine from Tongji University, Shanghai, China, in 2003, and the master’s degree in clinical medicine from Zhejiang University, Hangzhou, China, in 2008.
He is currently with the Department of Ultrasound Medicine, Zhejiang Provincial People’s Hospital & People’s Hospital of Hangzhou Medical College, Hangzhou. His current research interests include ultrasound diagnosis, interventional ultrasound therapy, and point-of-care ultrasound.
Dr. Ye is a member of WINFOUCS.

Keyan Li was born in Xi’an, China, in 1995. He received the bachelor’s degree in clinical medicine from the Military Medical University of Air Force, Xi’an, in 2018, where he majors in abdominal ultrasound and teleultrasound.
He is currently with the Department of Ultrasound, Hainan Hospital of Chinese People’s Liberation Army General Hospital, Sanya, China.
Dr. Li is a member of the Chinese Medical Equipment Technology Association.

Yuehua Lu was born in Tongxiang, China, in 1972. He received the bachelor’s degree in clinical medicine from Wenzhou Medical University, Wenzhou, China, in 2008.
He is currently with the Department of Ultrasound Medicine, The First People’s Hospital of Tongxiang City, Jiaxing, China, where she specializes in the ultrasound diagnosis.
Dr. Lu is a member of the Ultrasound Branch of the Zhejiang Medical Doctor Association and the Jiaxing Medical Association, and the Director of the Zhejiang Society of Ultrasound Medical Engineering.

Jufen Xu was born in Tongxiang, China, in 1968. She received the bachelor’s degree in clinical medicine from Wenzhou Medical University, Wenzhou, China, in 2007.
She is currently with the Department of Infectious Diseases, The First People’s Hospital of Tongxiang City, Jiaxing, Zhejiang, China, where she specializes in the diagnosis and treatment of chronic liver disease and infectious diseases.
Dr. Xu is a member of the Infection Branch of the Zhejiang Medical Association, the Tropical and Parasitic Diseases Professional Committee of the Zhejiang Integrative Medicine Association, and the Jiaxing Infectious Diseases Professional Committee.

Linfei Xiong received the B.Eng. degree from the Huazhong University of Science and Technology, Wuhan, China, in 2008, and the Ph.D. degree in mechanical engineering from the National University of Singapore, Singapore, in 2014.
He is currently a Senior Research and Development Manager with MGI Tech Company Ltd. His research interests include medical robotics integration, human machine interaction, and medical image processing.

Yuanyuan Zhao was born in Xinjiang, China, in 1995. She received the bachelor’s degree in clinical medicine from the Military Medical University of Air Force, Xi’an, China, in 2018, where she majors in abdominal ultrasound and teleultrasound.
She is currently with the Department of Ultrasound, Hainan Hospital of Chinese People’s Liberation Army General Hospital, Sanya, China.
Dr. Zhao is a member of the Chinese Medical Equipment Technology Association.

Ailin Cui received the bachelor’s degree in medical imageology from Kunming Medical University, Kunming, China, in 2015, and the master’s degree in imaging and nuclear medicine from Lanzhou University, Lanzhou, China, in 2018.
She is currently a Resident with the Department of Ultrasound, Zhejiang Provincial People’s Hospital & People’s Hospital of Hangzhou Medical College, Hangzhou, China. Her research focuses on the ultrasonic diagnosis of common diseases, especially gynecological, and fetal fields.

Yaqing Li was born in Xiaogan, Hubei, China. He received the Ph.D. degree in respiratory medicine from the Tongji Medical College of HUST, Wuhan, China, in 2006.
He is currently with the Department of Internal Medicine, Zhejiang Cancer Hospital & Cancer Hospital of the University of Chinese Academy of Sciences, Hangzhou, China, where he specializes in the diagnosis and treatment of airway inflammatory diseases, lung cancer, central airway stenosis, pleural diseases, and critical respiratory diseases. His main research interests include early diagnosis and clinical treatment of lung cancer, chronic obstructive pulmonary disease, and clinical application of respiratory endoscopy.
Dr. Li is a member of the Chronic Obstructive Pulmonary Disease Committee of the Chinese Medical Association and the Respiratory Endoscopy Association of world Endoscopy Association, a Standing Member of the Interventional Minimally Invasive Breathing Branch, China Medical Education Association, and the Respiratory Physician Branch, Zhejiang Medical Doctor Association.

Chengzhong Peng was born in Wenzhou, China, in 1974. He received the bachelor’s degree in clinical medicine and the master’s degree in imaging and nuclear medicine from Zhejiang University, Hangzhou, China, in 2004 and 2010, respectively.
He is currently with the Department of Ultrasound Medicine, Zhejiang Provincial People’s Hospital & People’s Hospital of Hangzhou Medical College, Hangzhou. His main research interests include contrast-enhanced ultrasound diagnosis, interventional ultrasound therapy, remote ultrasound, and ultrasound education.
Dr. Peng is a Young Member of the Ultrasonic Medical Branch, Chinese Medical Association; the Vice Chairman of the Ultrasonic Committee on Reproductive Health and Eugenics, Chinese Society of Ultrasonic Engineering; a member of the Ultrasonic Intervention Committee, Ultrasonic Medical Committee, Medical Association of China; a member of the Standing Committee, Ultrasonic Medical Branch, Zhejiang Medical Association; the Leader of the Abdominal Ultrasound Group; the Deputy Director Member of the Special Ultrasonic Committee, Zhejiang Mathematical Medical Association; and Leader of the Severe Ultrasound Group.

Faqin Lv was born in Shandong, China. She received the bachelor’s degree in medical engineering, in 2001, and the master’s and Ph.D. degrees in medical imaging from Fourth Military Medical University, Xi’an, China, in 2004.
She is currently with the Department of Ultrasound, Hainan Hospital of Chinese People’s Liberation Army General Hospital, Sanya, China. She specializes in interventional ultrasound and contrast-enhanced ultrasound.
Dr. Lv is a Committee Member of the Ultrasound Branch, Chinese Imaging Technology Institute; Vice Chairman of the Ultrasound Committee, Hainan Medical Association; and Vice Chairman of the Ultrasound Committee, Medical Imaging Quality Research Association.
Funding Statement
This work was supported in part by the Natural Science Foundation of Hainan Province under Grant 819QN376, in part by the Major Science and Technology Project of Hainan Province under Grant ZDKJ2019012, in part by theMilitaryMedicalResearch Programof PLA General Hospital under Grant CX19025 and Grant QNC19050, and in part by the National MOST “13.5” Key Projects under Grant 2016YFC0105006. The work of Faqin Lv was supported by the Talents Development Project of Sanya City.
Contributor Information
Shengzheng Wu, Email: emailwsz@126.com.
Dudu Wu, Email: 13649104190@163.com.
Ruizhong Ye, Email: yee981120@139.com.
Keyan Li, Email: kelianx@qq.com.
Yuehua Lu, Email: txlyh1@126.com.
Jufen Xu, Email: logabcd6789@163.com.
Linfei Xiong, Email: xionglinfei@genomics.cn.
Yuanyuan Zhao, Email: 15692537619@163.com.
Ailin Cui, Email: cuiailin_1991@163.com.
Yaqing Li, Email: lidoctor03@126.com.
Chengzhong Peng, Email: pcz001@126.com.
Faqin Lv, Email: lvjin8912@163.com.
References
- [1].Zhu N.et al. , “A novel coronavirus from patients with pneumonia in China, 2019,” New England J. Med., vol. 382, pp. 727–733, Feb. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Huang C.et al. , “Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China,” Lancet, vol. 395, no. 10223 pp. 497–506, Jan. 2020, doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Tanu S., “A review of coronavirus sisease-2019 (COVID-19),” Indian J. Pediatrics, vol. 87, no. 4, pp. 281–286, Apr. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Guo Y. R.et al. , “The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—An update on the status,” Mil. Med. Res., vol. 7, no. 1, p. 11, Mar. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].WHO Situation Report, World Health Org., Geneva, Switzerland, Mar. 2020. [Google Scholar]
- [6].Wang C., Horby P. W., Hayden F. G., and Gao G. F., “A novel coronavirus outbreak of global health concern,” Lancet, vol. 395, no. 10223, pp. 470–473, Feb. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Lake M. A., “What we know so far: COVID-19 current clinical knowledge and research,” Clin. Med., vol. 20, no. 2, pp. 124–127, Mar. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Shrestha G. S., Weeratunga D., and Baker K., “Point-of-care lung ultrasound in critically ill patients,” Rev. Recent Clin. Trials, vol. 13, no. 1, pp. 15–26, Jan. 2018. [DOI] [PubMed] [Google Scholar]
- [9].Lichtenstein D. A., “Lung ultrasound in the critically ill,” in Ann Intensive Care, 1st ed. Cham, Switzerland: Springer, 2014, p. 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bélaïd B., Zhang M., Lu Q., and Rouby J.-J., “Clinical review: Bedside lung ultrasound in critical care practice,” Crit. Care, vol. 11, no. 1, p. 205, Feb. 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Shrestha G., “Point-of-care ultrasonography in critically ill patients,” Kathmandu Univ. Med. J., vol. 13, no. 1, pp. 83–87, Oct. 2015. [DOI] [PubMed] [Google Scholar]
- [12].Lichtenstein D. A., “Ultrasound examination of the lungs in the intensive care unit,” Pediatric Crit. Care Med., vol. 10, no. 6, pp. 693–698, Nov. 2009. [DOI] [PubMed] [Google Scholar]
- [13].Guidelines for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infection by the National Health Commission (Trial Version 7), Nat. Health Commission People’s Republic China, Beijing, CHN, Mar. 2020. [Google Scholar]
- [14].Vaishali P. S., Michael G. T., and James W. T., “Prospective evaluation of point-of-care ultrasonography for the diagnosis of pneumonia in children and young adults,” JAMA Pediatrics, vol. 167, no. 2, pp. 119–125, Feb. 2013. [DOI] [PubMed] [Google Scholar]
- [15].Musolino A. M.et al. , “Lung ultrasound in children with COVID-19: Preliminary findings,” Ultrasound Med. Biol., vol. 46, no. 8, pp. 2094–2098, Aug. 2020, doi: 10.1016/j.ultrasmedbio.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Moro F.et al. , “How to perform lung ultrasound in pregnant women with suspected COVID-19,” Ultrasound Obstetrics Gynecol., vol. 55, no. 5, pp. 593–598, May 2020. [DOI] [PubMed] [Google Scholar]
- [17].Buonsenso D.et al. , “Clinical role of lung ultrasound for diagnosis and monitoring of COVID-19 pneumonia in pregnant women,” Ultrasound Obstetrics Gynecol., vol. 56, no. 1, pp. 106–109, Jul. 2020, doi: 10.1002/uog.22055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Wang D.et al. , “Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China,” J. Amer. Med. Assoc., vol. 323, no. 11, p. 1061, Mar. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Soummer A.et al. , “Ultrasound assessment of lung aeration loss during a successful weaning trial predicts postextubation distress,” Crit. Care Med., vol. 40, no. 7, pp. 2064–2072, Jul. 2012. [DOI] [PubMed] [Google Scholar]
- [20].Dexheimer N. F. L., Dalcin P. T., Teixeira C., and Beltrami F. G., “Lung ultrasound in critically ill patients: A new diagnostic tool,” J. Bras. Pneumol., vol. 38, no. 2, pp. 246–256, Apr. 2012. [DOI] [PubMed] [Google Scholar]
- [21].Demi M., Prediletto R., Soldati G., and Demi L., “Physical mechanisms providing clinical information from ultrasound lung images: Hypotheses and early confirmations,” IEEE Trans. Ultrason., Ferroelectr., Freq. Control, vol. 67, no. 3, pp. 612–623, Mar. 2020. [DOI] [PubMed] [Google Scholar]
- [22].Demi L., van Hoeve W., van Sloun R. J. G., Soldati G., and Demi M., “Determination of a potential quantitative measure of the state of the lung using lung ultrasound spectroscopy,” Sci. Rep., vol. 7, no. 1, Oct. 2017, Art. no. 12746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Lichtenstein D. A., Mezière G. A., Lagoueyte J. F., Biderman P., Goldstein I., and Gepner A., “A-lines and b-lines lung ultrasound as a bedside tool for predicting pulmonary artery occlusion pressure in the critically ill,” Chest, vol. 136, no. 4, pp. 1014–1020, 2009. [DOI] [PubMed] [Google Scholar]
- [24].Soldati G., Demi M., Smargiassi A., Inchingolo R., and Demi L., “The role of ultrasound lung artifacts in the diagnosis of respiratory diseases,” Expert Rev. Respiratory Med., vol. 13, no. 2, pp. 163–172, Feb. 2019. [DOI] [PubMed] [Google Scholar]
- [25].Soldati G.et al. , “Proposal for international standardization of the use of lung ultrasound for COVID-19 patients: A simple, quantitative, reproducible method,” J. Ultrasound Med., vol. 39, no. 7, pp. 1413–1419, Jul. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Marchetti G.et al. , “New insights in the use of pleural ultrasonography for diagnosis and treatment of pleural disease,” Clin. Respiratory J., vol. 12, no. 6, pp. 1993–2005, Jun. 2018. [DOI] [PubMed] [Google Scholar]
- [27].Soldati G., Smargiassi A., Demi L., and Inchingolo R., “Artifactual lung ultrasonography: It is a matter of traps, order, and disorder,” Appl. Sci., vol. 10, no. 5, p. 1570, Feb. 2020. [Google Scholar]
- [28].Soldati G., Demi M., Inchingolo R., Smargiassi A., and Demi L., “On the physical basis of pulmonary sonographic interstitial syndrome,” J. Ultrasound Med., vol. 35, no. 10, pp. 2075–2086, Oct. 2016. [DOI] [PubMed] [Google Scholar]
- [29].Lv F. Q.et al. , “Chinese expert consensus on critical care ultrasound applications at COVID-19 pandemic,” Adv. Ultrasound Diagnosis Therapy, vol. 4, no. 2, pp. 27–42, Apr. 2020. [Google Scholar]