Abstract
Actinomycosis is an uncommon, chronic granulomatous disease caused by the filamentous, gram-positive bacterium Actinomyces israelii. It causes indolent, painful wound infections commonly presenting with oral-cervicofacial manifestations, but other infections of the chest wall and gastrointestinal and genital tract are also seen. A high level of suspicion is required for diagnosis, as it may be missed or mistaken for malignancy. Severe cases may involve the central nervous system and require surgical intervention. We present a case report of actinomycosis causing a brain abscess.
Keywords: Actinomyces, actinomycosis, brain abscess, central nervous system
Actinomyces is a human commensal organism of the oral, gastrointestinal, and pelvic mucosa; it affects mostly middle-aged men.1,2 The disease is sporadic and is not transmitted from person to person. Disruption of the mucosal surface is the initiating factor for infection, with subsequent invasion of breached or necrotic tissue.1 Individuals of all ages and any host may be infected. Actinomycosis is classically associated with intrauterine devices and use of bisphosphonates causing osteonecrosis of the jaw.3 Pathognomonic “sulfur granules” can be seen on histopathology. The most common presentation is a painless mass at the angle of the jaw; however, any organ can be involved.4 In rare cases, the infection may spread hematogenously, causing distant metastatic disease. We present an interesting case of actinomycosis involving the central nervous system (CNS).
CASE REPORT
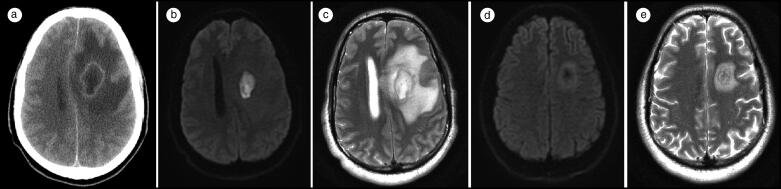
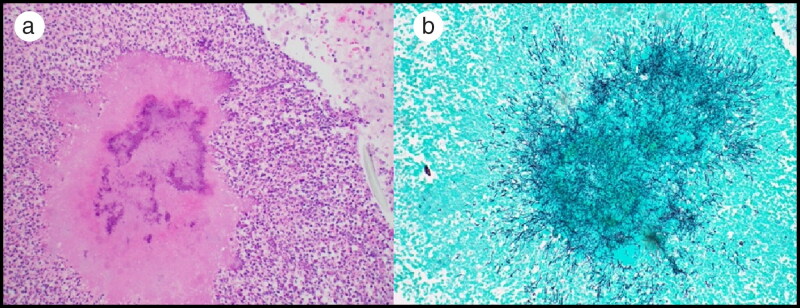
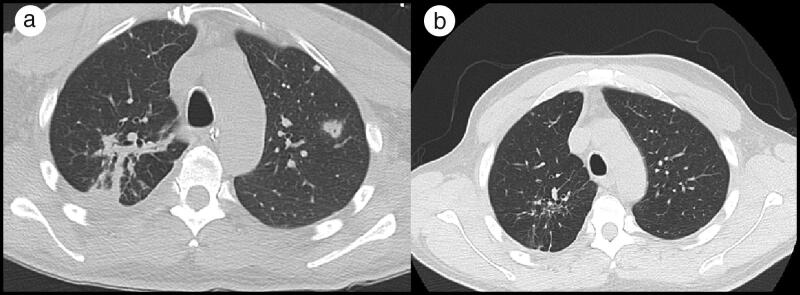
A 48-year old black man who was an everyday smoker was brought to the emergency room following a witnessed seizure. He had developed progressive confusion, short-term memory loss, and right-sided weakness days before presentation. He was intubated for airway protection. He was hypertensive, did not have fever, and had right-sided weakness. His white blood cell count was 23.5 k/μL. Computed tomography (CT) of his head showed a 3.5 cm mass in the left frontal lobe (Figure 1a). A transthoracic echocardiogram showed no vegetations, and blood cultures did not show any growth. Magnetic resonance imaging (MRI) of his brain showed a left frontal abscess (Figure 1b, 1c). Stereotactic biopsy and drainage was performed and tissue sections showed a cluster of filamentous gram-positive branching rods, consistent with Actinomyces (Figure 2). CT of his chest showed multifocal pneumonia with a cavitary lesion in the left upper lobe (Figure 3a). Bronchoscopy with bronchoalveolar lavage was performed but cytology, stains, and microbiology were unremarkable. He was started on ceftriaxone 2 g every 12 h, which continued throughout the hospitalization. After the patient was successfully extubated, a thorough oral exam revealed multiple caries and broken and missing teeth, which were thought to be the source of infection.
Figure 1.
Brain imaging. (a) CT without contrast showing a 3.5 × 2.1 cm peripherally hyperdense mass within the left frontal lobe with extensive associated vasogenic edema and a 10 mm left-to-right subfalcine herniation. (b) Diffusion-weighted and (c) T2-weighted MRI showing a 3.5 × 2.4 cm mass within the left frontal lobe compatible with a cerebral abscess. The vasogenic edema involves the left frontal lobe and anterior parietal lobe with diffuse sulcal effacement and left-to-right midline shift. (d) Diffusion-weighted and (e) T2-weighted MRI showing interval improvement in the left frontal lobe abscess cavity with decreased surrounding edema and improvement in the mass effect without midline shift.
Figure 2.
(a) Hematoxylin and eosin–stained slide showing a cluster of filamentous-appearing bacteria. (b) Grocott’s methenamine silver–stained slide highlighting the filamentous appearance of Actinomycetes.
Figure 3.
(a) CT of the chest without contrast showing irregular small areas of nodular consolidation within the right upper lobe as well as within the right lower lobe superior segment. Irregular reticulonodular opacities are scattered throughout. A partially cavitary nodule is present in the left upper lobe apex measuring 8 mm in greatest dimension, and a small right pleural effusion is present. (b) Near resolution of right upper and lower lobe infiltrates and of right pleural effusion, with resolution of the left lung nodule and no evidence of a cavitary lesion.
The patient was discharged from the hospital on intravenous ceftriaxone 2 g twice a day, which he received for 4 months (due to adherence and reluctance to have a 24-h penicillin G infusion at home). Four months later, repeat MRI of his brain showed improvement in the left frontal lobe abscess cavity (Figure 1d, 1e). Repeat CT of his chest showed near resolution of the pulmonary infiltrates and resolution of the left lung nodule (Figure 3b). At that time, he was transitioned to oral doxycycline 100 mg twice a day to complete at least 1 year of outpatient treatment. The patient was since lost to follow-up.
DISCUSSION
Diagnosis of actinomycosis is challenging due to its nonspecific symptoms and physical findings, unless the classic “lumpy jaw” is seen on clinical exam.2,5 CNS involvement is rare and usually results from hematogenous spread from distant sites such as lung, abdomen, or pelvis (infected intrauterine device) or contiguous foci like ear, sinus, and cervicofacial region.4,6 Our patient had evidence of poor dentition, which could have been the inciting event leading to aspiration and formation of a lung abscess with subsequent hematogenous spread to the CNS. Although bronchoalveolar cultures were obtained, it is not unusual to yield negative results given that they are usually not obtained under proper anaerobic conditions.7 Tissue biopsy would be more appropriate, but we did not feel it would be necessary in this case.
Diagnosis of actinomycosis requires the recovery of Actinomyces species from an abscess, fistula, or sinus tract; histologically, they appear as colonies of filamentous bacteria with a zone of granulation tissue known as sulfur granules.1,8 Due to the slow-growing nature of the organism, cultures should be held for at least 14 days in an anaerobic environment.9 The microbiology laboratory should be informed about suspected actinomycosis.6 Branching gram-positive bacilli may indicate either aerobic Nocardia, Actinomyces, or sometimes Rhodococcus species. Actinomyces species is indistinguishable from Nocardia on Gram stain,1 but can be differentiated by special cultures and by modified acid-fast stain: Nocardia stains partially acid-fast, while Actinomyces does not.2 Differentiation of actinomycosis from nocardiosis is crucial for the selection of appropriate antimicrobial therapy.4
Actinomycotic brain abscess mainly involves the temporal and frontal lobes and appears on MRI as single or multiple peripherally enhancing lesions that may be encapsulated or less frequently unencapsulated and exhibit a hyperintense rim on T1 noncontrast imaging and a grape-like cluster pattern with a T2 hypointense wall.6,10 Surgery is reserved for refractory disease and critical sites such as the CNS.11 Medical therapy is usually curative, even with extensive disease. Recommended treatment involves 2 to 6 weeks of high-dose penicillin G or ceftriaxone followed by 6- to 12-month oral doxycycline.12,13
In conclusion, actinomycosis is an infrequent but potentially severe disease that requires a high index of suspicion and may ultimately need an invasive approach for diagnosis. Surgical resection and prolonged antimicrobial therapy are the cornerstones of management.
References
- 1.Wong V, Turmezei T, Weston C.. Actinomycosis. BMJ. 2011;343:d6099. doi: 10.1136/bmj.d6099. [DOI] [PubMed] [Google Scholar]
- 2.Cintron J, Pino A, Duarte B, Wood D.. Abdominal actinomycosis. Dis Colon Rectum. 1996;39(1):105–108. doi: 10.1007/BF02048278. [DOI] [PubMed] [Google Scholar]
- 3.Yegüez J, Martinez S, Sands L, Hellinger M.. Pelvic actinomycosis presenting as malignant large bowel obstruction: a case report and a review of the literature. Am Surg. 2000;66(1):85–90. [PubMed] [Google Scholar]
- 4.Smego R. Actinomycosis of the central nervous system. Rev Infect Dis. 1987;9(5):855–865. doi: 10.1093/clinids/9.5.855. [DOI] [PubMed] [Google Scholar]
- 5.Harris L, DeCosse J, Dannenberg A.. Abdominal actinomycosis: evaluation by computed tomography. Am J Gastroenterol. 1989;84(2):198–200. [PubMed] [Google Scholar]
- 6.Rahiminejad M, Hasegawa H, Papadopoulos M, MacKinnon A.. Actinomycotic brain abscess. BJR Case Rep. 2016;2(4):20150370. doi: 10.1259/bjrcr.20150370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mabeza G, Macfarlane J.. Pulmonary actinomycosis. Eur Respir J. 2003;21(3):545–551. doi: 10.1183/09031936.03.00089103. [DOI] [PubMed] [Google Scholar]
- 8.Ha HK, Lee HJ, Kim H, et al. Abdominal actinomycosis: CT findings in 10 patients. AJR Am J Roentgenol. 1993;161(4):791–794. doi: 10.2214/ajr.161.4.8372760. [DOI] [PubMed] [Google Scholar]
- 9.Ferrari TC, Couto CA, Murta-Oliveira C, Conceição SA, Silva RG.. Actinomycosis of the colon: a rare form of presentation. Scand J Gastroenterol. 2000;35(1):108–109. doi: 10.1080/003655200750024623. [DOI] [PubMed] [Google Scholar]
- 10.Ham H, Jung S, Jung T, Heo S.. Cerebral actinomycosis: unusual clinical and radiological findings of an abscess. J Korean Neurosurg Soc. 2011;50(2):147–150. doi: 10.3340/jkns.2011.50.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Song JU, Park HY, Jeon K, Um SW, Kwon OJ, Koh WJ.. Treatment of thoracic actinomycosis: a retrospective analysis of 40 patients. Ann Thorac Med. 2010;5(2):80–85. doi: 10.4103/1817-1737.62470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilbert DN, Moellering RC, Jr, Sande MA.. The Sanford Guide to Antimicrobial Therapy. Antimicrobial Therapy. 2001;31:70. [Google Scholar]
- 13.Valour F, Sénéchal A, Dupieux C, et al. . Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 2014;7:183–197. doi: 10.2147/IDR.S39601. [DOI] [PMC free article] [PubMed] [Google Scholar]