Abstract
The epidemiology and organ-specific sequelae following acute illness due to COVID-19 and prompting patients to seek COVID recovery care are not yet well characterized. This cross-sectional study reviewed data on 200 adult patients with prolonged symptoms of COVID-19 (>14 days after symptom onset) not resolved by usual primary care or specialist care who were referred for COVID-specific follow-up. Most patients sought COVID recovery clinic visits within the first 2 months of initial onset of symptoms (median 37 days), with some seeking care for sequelae persisting up to 10 months (median 82 days). At the time of telehealth evaluation, 13% of patients were using home oxygen, and 10% of patients had been unable to return to work due to persistent fatigue and/or subjective cognitive dysfunction (“brain fog”). The prominent specific symptom sequelae prompting patients to seek COVID-specific evaluation beyond usual primary care and specialist referrals were dyspnea, fatigue/weakness, and subjective cognitive dysfunction, irrespective of whether patients had required hospitalization or time since COVID-19 symptom onset.
Keywords: Care coordination, neuropsychiatric symptoms, post-acute sequelae of COVID-19, PASC, primary care
Target audience: All physicians
Learning objectives: After completing the article, the learner should be able to
1. Describe the sequelae of COVID-19 in patients referred to COVID recovery clinic services.
2. Examine the similarities of COVID-19 sequelae in the context of initial onset and severity of acute illness in patients seeking COVID recovery care.
Faculty credentials/disclosure: Dr. Danesh is a research investigator at Baylor Scott & White Research Institute and a faculty affiliate at the University of Texas at Austin. Dr. Arroliga is the chief medical officer of Baylor Scott & White Health and a clinical professor of medicine at Texas A&M University. Dr. Bourgeois is the chair of psychiatry at Baylor Scott & White Medical Center at Temple and a clinical professor of medicine at Texas A&M University College of Medicine. Dr. Widmer, Dr. Michael McNeal, and Dr. Tresa McNeal are internal medicine physicians at Baylor Scott & White Health in Temple and clinical faculty members at Texas A&M University College of Medicine. None of the planners/authors for this educational activity have relevant financial relationship(s) to disclose with ineligible companies whose primary business is producing, marketing, selling, re-selling, or distributing health care products used by or on patients.
>Accreditation: The A. Webb Roberts Center for Continuing Medical Education of Baylor Scott & White Health is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Designation: The A. Webb Roberts Center for Continuing Medical Education of Baylor Scott & White Health designates this journal CME activity for a maximum of 1.0 AMA PRA Category 1 CreditTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
ABIM MOC: The successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 1.0 Medical Knowledge MOC points in the American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
The A. Webb Roberts Center for Continuing Medical Education of Baylor Scott & White Health will submit participant completion information to the ACCME, which will be transferred to the ABIM for MOC credits claimed. By entering your ABIM Diplomate number into your profile and completing the credit claim process for this activity, you are giving permission for the transfer of your information to take place.
Process: To complete this CME activity, read the entire article and then go to https://ce.bswhealth.com/Proceedings2020. You will register for the course, pay any relevant fee, take the quiz, complete the evaluation, and claim your CME credit. For more information about CME credit, email ce@bswhealth.org.
Expiration date: November 1, 2023.
The complications associated with post-acute sequelae of COVID-19 include dyspnea, fatigue, and neuropsychiatric symptoms, among other syndromic features.1 Although persistent sequelae of acute illness are commonly associated with severe disease requiring hospitalization, the epidemiology and organ-specific sequelae following mild acute illness due to COVID-19 are not yet well characterized. Patients with mild disease are defined as those who were not hospitalized, patients with moderate disease as those who were hospitalized, and patients with severe disease as hospitalized patients receiving care in intensive care units. Specifically, persistent multiple neuropsychiatric complications occur across the continuum of COVID-19 severity. We report on an integrated health system multispecialty telemedicine-based consultation service for post-COVID patients to monitor and facilitate management of persistent post-COVID symptoms.
METHODS
This was a cross-sectional study of adult patients with prolonged symptoms of COVID-19 (>14 days after symptom onset) not resolved following usual primary or specialist care who were referred for COVID-specific follow-up through the COVID recovery clinic at Baylor Scott & White Health. To accelerate shared learning, provide comprehensive care, and support primary care physicians, patients with prolonged recoveries from mild, moderate, or severe COVID-19 referred by primary care physicians were evaluated via telehealth by internal medicine physicians for symptom management recommendations and/or specialist referral. COVID recovery clinic visits were available on weekends, weekdays, and after hours to facilitate patient access in an integrated medical group practice setting. Telehealth evaluations via physician referral accommodated access to patients in rural, urban, and suburban regions of a 34,000-square-mile service area in Central and North Texas.
A semistructured interview guide was used to incorporate common data elements into evolving standard of care documentation. Consulting specialists—from cardiology, gastroenterology, physical medicine and rehabilitation, pulmonology, infectious disease, geriatrics, hematology/oncology, neurology, and psychiatry—reviewed case narratives written by the internal medicine physicians conducting the post-COVID telemedicine assessments. Consultants offered specialty-specific reviews (without billing) to advise on care plan decisions. Subsequent assessments and/or official consults were recommended for a subset of case reviews. COVID recovery clinic assessments and findings were then shared with the patients’ primary care team. For example, recommendations from the consultation-liaison psychiatrist included advice for psychopharmacological management in primary care and referrals to psychiatry and/or neurology when more detailed assessment, ongoing specialty care, and multicomponent interventions were indicated.
Data from a 4-month period (November 2020–February 2021) were extracted to characterize comorbidities, illness onset, and the time course of persistent symptoms in a consecutive sample of 200 COVID recovery clinic patient visits. Descriptive statistics were used for clinical parameters. Comparisons among groups and predictors were not assessed because of the sample size. This report adheres to STROBE and SQUIRE reporting standards,2 with approval by the Baylor Scott & White Research Institute institutional review board.
RESULTS
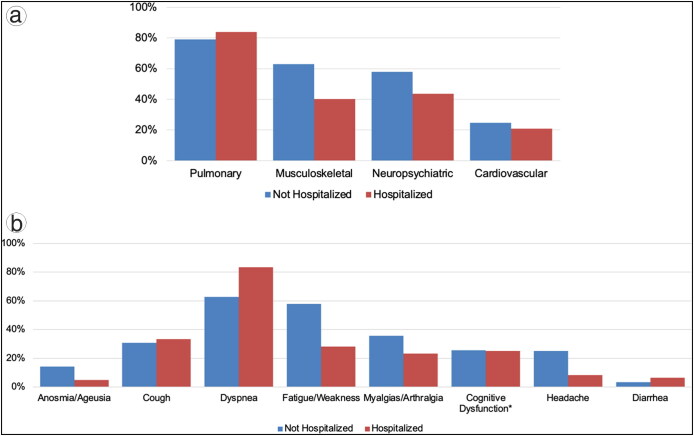
Clinic notes were reviewed for 200 adults seeking care for COVID-19 sequelae (median age 52; 71% women) following mild, moderate, or severe disease (Table 1). Most patients had visits within the first 2 months of initial onset of symptoms (median 37 days), with some seeking care for sequelae persisting up to 10 months (median 82 days). During acute illness, the most commonly reported symptoms were cough (53%), dyspnea (48%), and fatigue (39%). At the time of evaluation, 13% of patients were using home oxygen, and 10% had been unable to return to work due to persistent weakness and/or cognitive dysfunction. Cognitive dysfunction was defined as subjective complaints of “brain fog,” including patient reports of confusion, poor concentration, memory loss, and/or trouble with word-finding. The most prominent sequelae by organ system were pulmonary (81%), musculoskeletal (56%), and neuropsychiatric (54%). Specific sequelae most commonly endorsed during the telehealth assessment were dyspnea (69%), fatigue (48%), and subjective cognitive dysfunction (i.e., “brain fog”; 26%). Subjective cognitive dysfunction was endorsed by 1 in 4 patients seeking care who were hospitalized for moderate to severe acute disease and also by 1 in 4 patients with mild disease not requiring hospitalization (Figure 1).
Table 1.
Demographic and clinical characteristics of 200 patients evaluated in a COVID-19 recovery clinic
| Variable | 2–8 weeks since onset (n = 138) | 2–10 months since onset (n = 62) | All (n = 200) |
|---|---|---|---|
| Age, median (Q1–Q3), years | 53 (28–45) | 51 (40–61) | 52 (41–61) |
| 18–40 | 29 (21%) | 17 (27%) | 46 (23%) |
| 41–64 | 79 (57%) | 36 (58%) | 115 (58%) |
| ≥65 | 30 (22%) | 9 (15%) | 39 (20%) |
| Female | 93 (67%) | 48 (77%) | 141 (71%) |
| Race | |||
| Black | 15 (13%) | 6 (11%) | 21 (12%) |
| White | 93 (78%) | 45 (83%) | 138 (79%) |
| Other | 12 (10%) | 3 (6%) | 15 (9%) |
| Hispanic/Latino | 29 (23%) | 13 (23%) | 42 (23%) |
| Comorbidities | |||
| Hypertension | 44 (32%) | 15 (24%) | 59 (30%) |
| Diabetes mellitus | 26 (19%) | 8 (13%) | 34 (17%) |
| Obesity | 40 (29%) | 20 (32%) | 60 (30%) |
| Hospitalization for acute illness | 46 (33%) | 14 (23%) | 60 (30%) |
| COVID onset, median (Q1–Q3), days | 37 (28–45) | 82 (66–134) | 44 (33–66) |
| Sequelae | |||
| Cough | 53 (38%) | 10 (16%) | 63 (32%) |
| Dyspnea | 93 (67%) | 45 (73%) | 138 (69%) |
| Home oxygen | 21 (15%) | 5 (8%) | 26 (13%) |
| Fatigue | 64 (46%) | 32 (52%) | 96 (48%) |
| Myalgias/arthralgia | 11 (8%) | 8 (13%) | 19 (10%) |
| Cognitive dysfunctiona | 34 (25%) | 17 (27%) | 51 (26%) |
| Headache | 25 (18%) | 15 (24%) | 40 (20%) |
| Diarrhea | 7 (5%) | 2 (3%) | 9 (5%) |
| Unable to work | 14 (10%) | 6 (10%) | 20 (10%) |
aCognitive dysfunction is defined as subjective complaints of “brain fog,” including self-report of confusion, poor concentration, memory loss, and/or trouble word-finding. Q1 indicates quartile 1; Q3, quartile 3.
Figure 1.
Sequelae category by (a) organ system and (b) specific symptomatic sequelae present when seeking COVID-19 recovery clinic assessments. *Cognitive dysfunction is defined as subjective complaints of “brain fog,” including self-report of confusion, poor concentration, memory loss, and/or trouble in word-finding.
DISCUSSION
The prominent specific symptom sequelae prompting patients to seek COVID-specific evaluation via physician referral beyond routine primary care and specialists were dyspnea, fatigue, and subjective cognitive dysfunction, irrespective of whether patients had required hospitalization or time since COVID-19 symptom onset. In our sample of 200 consecutive patients referred to COVID recovery clinic services, almost 1 in 4 were under 40 years old, and 1 in 10 were seeking COVID-specific recovery care while unable to return to work due to the severity and persistence of sequelae. Persistent sequelae for a subset of patients continued for months after the onset of initial symptoms, irrespective of the initial severity of disease. Furthermore, the proportions of patients reporting musculoskeletal, neuropsychiatric, and cardiovascular symptoms at the time of telehealth evaluation were higher in patients with mild disease (defined as not having been hospitalized) than in those with moderate/severe disease (who were hospitalized).
Patients referred by primary care providers to COVID recovery clinic services self-report new-onset cognitive symptoms. When patients self-report new-onset cognitive symptoms such as poor concentration or memory loss when seeking care, it is in the context of daily activities. The presence of perceived cognitive decline is important and relevant, irrespective of subsequent formal clinical ascertainment such as neuropsychological testing, because self-reported cognitive function is a patient-reported outcome tied to well-being.3,4 Furthermore, the presence of self-reported cognitive dysfunction in adults may be a risk factor for dementia later in life,5 with self-reported cognitive decline discernible as a patient-reported outcome in advance of formal neuropsychological testing results.6,7
The comorbidities, illness onset, and time course of persistent symptoms presented in this report are representative of adults seeking care beyond routine primary care in a 52-hospital integrated health system and thus reflect the characterization of concerning sequelae from the perspective of primary care clinicians and patients. Cross-sectional epidemiologic assessments of post-acute sequelae of COVID-19 describe similar sequelae of dyspnea and fatigue.1,8–10 In contrast to self-report epidemiologic surveys, our use of expert clinician interviews contributes comprehensive assessments of the depth and breadth of post-acute sequelae of COVID, including assessment for neurocognitive and other neuropsychiatric sequelae. Additionally, this report contributes insights regarding the sequelae prompting physician referral beyond routine primary care: inability to return to work, use of home oxygen, neurocognitive function, and other neuropsychiatric symptoms in the context of sequelae duration and COVID-19-related hospitalization status. Characteristics of troubling sequelae of COVID-19 reported by patients without a primary care referral with insurance coverage for recovery clinic services are not represented.
Patients seeking COVID recovery clinic services are experiencing subjective cognitive dysfunction, fatigue, and dyspnea. The proportions of patients reporting cognitive dysfunction and pulmonary sequelae are similar in care seekers who experienced mild disease (nonhospitalized) and moderate/severe disease (hospitalized). This report distills comprehensive telehealth evaluations by COVID-focused internal medicine physicians to offer preliminary profiles and durations of sequelae presentations stratified by duration of sequelae and severity of disease.
References
- 1.Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27:601–615. doi: 10.1038/s41591-021-01283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.International Committee of Medical Journal Editors . Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals. International Committee of Medical Journal Editors ; 2019. [PubMed] [Google Scholar]
- 3.Rabin LA, Smart CM, Crane PK, et al. Subjective cognitive decline in older adults: an overview of self-report measures used across 19 international research studies. J Alzheimers Dis. 2015;48(Suppl 1):S63–S86. doi: 10.3233/JAD-150154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Comijs HC, Dik MG, Aartsen MJ, Deeg DJ, Jonker C.. The impact of change in cognitive functioning and cognitive decline on disability, well-being, and the use of healthcare services in older persons: results of a longitudinal aging study. Dement Geriatr Cogn Disord. 2005;19:316–323. doi: 10.1159/000084557. [DOI] [PubMed] [Google Scholar]
- 5.Liew TM. Subjective cognitive decline, anxiety symptoms, and the risk of mild cognitive impairment and dementia. Alzheimers Res Ther. 2020;12:107. doi: 10.1186/s13195-020-00673-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hess C, Levy B, Hashmi AZ, et al. Subjective versus objective assessment of cognitive functioning in primary care. J Am Board Fam Med. 2020;33:417–425. doi: 10.3122/jabfm.2020.03.190265. [DOI] [PubMed] [Google Scholar]
- 7.Hill NL, Mogle J, Whitaker EB, et al. Sources of response bias in cognitive self-report items: “which memory are you talking about?” Gerontologist. 2019;59:912–924. doi: 10.1093/geront/gny087. [DOI] [PubMed] [Google Scholar]
- 8.Logue JK, Franko NM, McCulloch DJ, et al. Sequelae in adults at 6 months after COVID-19 infection. JAMA Netw Open. 2021;4:e210830. doi: 10.1001/jamanetworkopen.2021.0830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carfi A, Bernabei R, Landi F, Gemelli Against COVID-19 Post-Acute Care Study Group . Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garrigues E, Janvier P, Kherabi Y, et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect. 2020;81:e4–e6. doi: 10.1016/j.jinf.2020.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]