Abstract
In stroke patients, a high neutrophil-to-lymphocyte ratio (NLR) has been associated with poor functional outcome at 3 months, higher mortality, and a higher hemorrhagic transformation. We assessed the role of NLR in patients with acute ischemic stroke who received thrombolysis. The charts of 98 patients treated between 2015 and 2019 were retrospectively reviewed. The mean NLR was compared using an independent Student’s t test. At 3 months, a good functional outcome was seen in 31 patients (32%) and a poor functional outcome was seen in 67 patients (68%). Patients with NLR >2.39 had a poor functional outcome (odds ratio 2.7; 95% confidence interval 1.11–6.39; P < 0.02). Our study revealed that patients who present with acute ischemic stroke and have an increased NLR at the time of administration of thrombolysis have a poor functional outcome at 3 months.
Keywords: Acute ischemic stroke, developing country, functional outcome, neutrophil-to-lymphocyte ratio, thrombolysis
Stroke is the second most common cause of death and the leading cause of disability in the world.1,2 Ischemic stroke accounts for 80% of strokes,3 and alteplase (recombinant tissue plasminogen activator [TPA]) is an effective treatment.4 Inflammation plays an important role in the ischemic stroke cascade, involving a complex mix of innate and adaptive immunity.5 Previous studies have reported a positive association between a high neutrophil-to-lymphocyte ratio (NLR) and poor functional outcome at 3 months in patients with acute ischemic stroke (AIS). In one study, NLR predicted poor functional outcome at 3 months, stroke severity, and stroke recurrence in patients with AIS.6 Previous metaanalyses also confirmed poor functional outcome at 3 months and a higher mortality rate in patients with a high NLR and AIS.7–9 Liu et al found a higher risk of hemorrhagic transformation in patients with AIS who received TPA.10 Cheng et al reported a poor outcome with high NLR and glucose levels in patients with AIS who received TPA,11 but Pektezel et al found no relationship between admission NLR and outcome.12 Shi et al found that a high NLR at 24 hours, but not a high NLR at baseline, was predictive of poor functional outcome.13 Duan et al found a high risk of symptomatic intracranial hemorrhage, 3-month mortality, and poor functional outcome in patients with a high NLR and AIS who underwent endovascular thrombectomy.14 Further studies may predict functional outcome in patients with AIS after TPA with high NLR. We present retrospective data from our stroke registry evaluating the association of NLR with outcomes in patients with AIS who received TPA.
METHODS
This retrospective chart review involved patients presenting to the Shifa International Hospital, Islamabad, Pakistan, between 2015 and 2019 with AIS who received thrombolytic therapy. All patients arrived at the emergency department within 4.5 hours of last being seen well. They were diagnosed with AIS based on clinical and radiological findings. All patients were screened for contraindications to thrombolysis with alteplase, and patients with any contraindications did not receive it, thereby being excluded from the study. Patients with a history of fever or clinical suspicion of infection were excluded from the analysis. This study was approved by the institutional review board and ethics committee of Shifa International Hospital.
The data collected as part of this study included the patients’ age, gender, comorbid conditions (including atrial fibrillation, diabetes, and hypertension), location of infarct, National Institutes of Health Stroke Scale (NIHSS) score at admission and discharge, modified Rankin scale (mRS) score before the stroke, mRS at 3 months, ASPECTS score at the first brain imaging, the presence of hemorrhagic transformation of the infarct, neutrophil count at admission, and lymphocyte count at admission. Blood samples for the NLR were obtained in the emergency department on the first day of presentation to the hospital. The NLR was calculated. We divided our patients into two groups: group 1 had an NLR of <2.39, and group 2 had an NLR of >2.39.
Stroke severity was assessed using the NIHSS, which grades ischemic strokes based on the neurologic deficits.15 The highest score on the NIHSS is 42, with a higher score correlating with larger deficits. A minor stroke was defined as an NIHSS score of <4; moderate, a score of 5 to 15; moderately severe, a score of 16 to 20; and severe, a score of 21 to 42. A good functional outcome was defined as an mRS of 0 to 2, and a poor functional outcome was defined as an mRS of 3 to 6. The ASPECTS, NIHSS, and mRS scores were recorded by a neurology team.
SPSS 21.0 software was used to perform statistical analysis. Quantitative variables were presented as mean with standard deviation. The NLR was calculated for all patients at admission, and the mean values with standard deviation were calculated. The mean NLR between patients with good and poor functional outcomes was compared using an independent Student’s t test. The mean NLR was also compared between different categories of stroke severity, based on the NIHSS.
RESULTS
A total of 98 patients were included in the analysis. The mean age of patients was 58 ± 6.4 years, with 60 male participants (61.2%) (Table 1). Of the 98 patients, 44 (44.9%) had an NLR of <2.39 and were included in group 1, whereas the remaining 54 patients (55.1%) had an NLR of >2.39 and were included in group 2. Group 1 had 25 men and 19 women (male-to-female ratio of 1.3), and group 2 had 35 men and 19 women (male-to-female ratio of 1.8). Patients in group 2 had a higher mean NIHSS (18.6 ± 7.9) than those in group 1 (12.8 ± 6.3; P = 0.01). Hemorrhagic transformation was seen in 11 patients (11.2%), with 7 patients in group 2 and 4 patients in group 1 (P = 0.04). The stroke occurred in the middle cerebral artery in 70 patients (71.4%), in the anterior cerebral artery in 14 (14.3%), in the posterior cerebral artery in 8 (8.2%), and in the cerebellar or brainstem in 6 (6.1%).
Table 1.
Baseline characteristics of patients
| Variable | Value |
|---|---|
| Mean age ± standard deviation (years) | 58 ± 6.4 |
| Males | 60 (61%) |
| Females | 38 (39%) |
| Diabetes | 45 (46%) |
| Hypertension | 53 (54%) |
| Chronic kidney disease | 18 (18%) |
| Old stroke | 21 (21%) |
| Smoking | 18 (18%) |
| Atrial fibrillation | 13 (13%) |
| Heart failure | 11 (11%) |
| Previous antiplatelet use | 37 (38%) |
| TOAST classificationa | |
| 1. Large artery atherosclerosis | 27 (28%) |
| 2. Cardio embolism | 46 (47%) |
| 3. Small vessel occlusion | 16 (16%) |
| 4. Stroke of other determined etiology | 4 (4%) |
| 5. Stroke of undetermined etiology | 5 (5%) |
Trial of Org 10172 in Acute Stroke Treatment (TOAST). Using this rating system, interphysician agreement was very high.
Of the 70 patients with middle cerebral artery infarct, the initial computed tomography (CT) of the brain was available for 63 patients (90%). For the remaining patients, magnetic resonance imaging of the brain was done initially or a CT was done in another hospital and was not available for analysis. Of the 63 scans available for calculation of the ASPECTS score, 58 (92.1%) had a score of ≥6. There were 5 CT scans (7.9%) with an ASPECTS score of <6, and all were from patients in group 2 (P < 0.01).
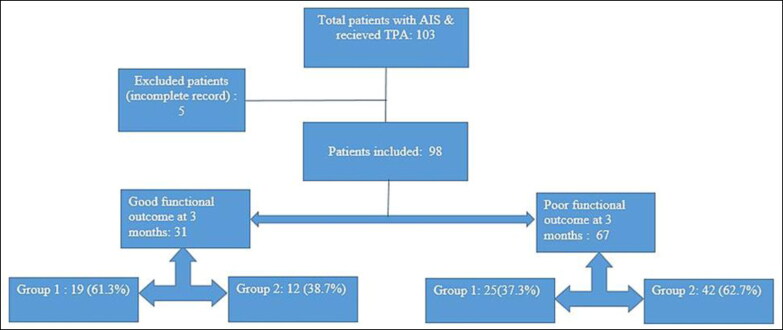
At 3 months, a good functional outcome was seen in 31 patients (31.6%), and a poor functional outcome was seen in 67 patients (68.4%) (Figure 1). Of the patients with a poor functional outcome, 25 (37.3%) were in group 1 and 42 (62.7%) were in group 2. Patients in group 2 were more likely to have a poor functional outcome (odds ratio [OR] 2.7; 95% confidence interval [CI] 1.11–6.39; P < 0.02).
Figure 1.
Flow chart of study participants. In group 1, the neutrophil-to-lymphocyte ratio was <2.39; in group 2, >2.39. AIS indicates acute ischemic stroke; TPA, tissue plasminogen activator.
DISCUSSION
This study is the first to evaluate the role of NLR at the time of receiving thrombolysis in predicting the 3-month functional outcome of patients with AIS. Numerous studies have revealed a positive association between high NLR and poor functional outcome in patients with AIS, but none of these studies evaluated the role of NLR with AIS in patients who received thrombolysis.6–9,11,12 Our study revealed that patients with AIS who had a high NLR at the time of thrombolysis had higher NIHSS scores, a higher rate of hemorrhagic transformation, and a lower ASPECT score and were more likely to have a poor functional outcome at 3 months (OR 2.7; 95% CI 1.11–6.39; P < 0.02).
Shi et al13 revealed no significant association between NLR and functional outcome in patients with AIS who received thrombolysis. At 24 hours postthrombolysis, NLR was significantly higher in patients with death or major disability. Our study did not evaluate dynamic NLR. The poor functional outcome (OR 1.58; 95% CI 1.02–2.45; P = 0.039) revealed by Duan et al14 was seen in patients presenting with AIS who underwent endovascular treatment; however, thrombolysis outcome was not assessed.
Higher white cell counts have a significant role in stroke severity, disability, and 30-day mortality.16 Raised neutrophils on admission are known to be related to poor functional outcomes in patients with AIS.17 The inflammatory cascade is activated by stagnant blood flow. The subsequent release of proinflammatory cytokines such as tumor necrosis factor-α, interleukin-1, interleukin-6, and matrix metalloproteinase-9 (MMP-9) from endothelium/brain parenchyma and damaged neuronal release of danger-/damage-associated molecular patterns (DAMP) target the disruption of the blood-brain barrier. Neutrophils are the first to arrive in the resultant systemic inflammatory response, leading to further oxidative stress and consequent brain edema and hemorrhagic transformation.9
Our study showed a 12.9% rate of hemorrhagic transformation in patients with high NLR compared to 9.0% (P < 0.04) in patients with lower NLR, which was similar to a previous study that showed hemorrhagic transformation (37.5% vs. 20.7%, P < 0.004).10 Overall, although the decision for thrombolysis remains the same, NLR has a role in prediction of functional outcome in patients with AIS undergoing thrombolysis.
NLR in AIS was assessed at the time of administration of thrombolysis but was not followed up after thrombolysis. Our study did not evaluate the association of other variables, including endovascular thrombectomy, that may impact the functional outcome. As it is a retrospective study, we had to rely on the data available in the medical record.
In conclusion, our study revealed that patients who presented with AIS and a raised NLR at the time of administration of thrombolysis have a worse functional outcome at 3 months.
References
- 1.World Health Organization . The top 10 causes of death. 2020. Accessed April 3, 2021. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
- 2.Goldstein LB, Bushnell CD, Adams RJ, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(2):517–584. doi: 10.1161/STR.0b013e3181fcb238. [DOI] [PubMed] [Google Scholar]
- 3.Ikram MA, Wieberdink RG, Koudstaal PJ.. International epidemiology of intracerebral hemorrhage. Curr Atheroscler Rep. 2012;14(4):300–306. doi: 10.1007/s11883-012-0252-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384(9958):1929–1935. doi: 10.1016/S0140-6736(14)60584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iadecola C, Anrather J.. The immunology of stroke: from mechanisms to translation. Nat Med. 2011;17(7):796–808. doi: 10.1038/nm.2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xue J, Huang W, Chen X, et al. Neutrophil-to-lymphocyte ratio is a prognostic marker in acute ischemic stroke. J Stroke Cerebrovasc Dis. 2017;26(3):650–657. doi: 10.1016/j.jstrokecerebrovasdis.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 7.Zhang J, Ren Q, Song Y, et al. Prognostic role of neutrophil-lymphocyte ratio in patients with acute ischemic stroke. Medicine (Baltimore). 2017;96(45):e8624. doi: 10.1097/MD.0000000000008624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wan J, Wang X, Zhen Y, et al. The predictive role of the neutrophil-lymphocyte ratio in the prognosis of adult patients with stroke. Chin Neurosurg J. 2020;6:1–10. doi: 10.1186/s41016-020-00201-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song SY, Zhao XX, Rajah G, et al. Clinical significance of baseline neutrophil-to-lymphocyte ratio in patients with ischemic stroke or hemorrhagic stroke: an updated meta-analysis. Front Neurol. 2019;1032. doi: 10.3389/fneur.2019.01032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu YL, Lu JK, Yin HP, et al. High neutrophil-to-lymphocyte ratio predicts hemorrhagic transformation in acute ischemic stroke patients treated with intravenous thrombolysis. Int J Hypertens. 2020;1–6. doi: 10.1155/2020/5980261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng Y, Ying A, Lin Y, et al. Neutrophil-to-lymphocyte ratio, hyperglycemia, and outcomes in ischemic stroke patients treated with intravenous thrombolysis. Brain Behav. 2020;10(9):01741. doi: 10.1002/brb3.1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pektezel MY, Yilmaz E, Arsava EM, Topcuoglu MA.. Neutrophil-to-lymphocyte ratio and response to intravenous thrombolysis in patients with acute ischemic stroke. J Stroke Cerebrovasc Dis. 2019;28(7):1853–1859. doi: 10.1016/j.jstrokecerebrovasdis.2019.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Shi J, Peng H, You S, et al. Increase in neutrophils after recombinant tissue plasminogen activator thrombolysis predicts poor functional outcome of ischaemic stroke: a longitudinal study. Eur J Neurol. 2018;25(4):687-e45. doi: 10.1111/ene.13575. [DOI] [PubMed] [Google Scholar]
- 14.Duan Z, Wang H, Wang Z, et al. Neutrophil-lymphocyte ratio predicts functional and safety outcomes after endovascular treatment for acute ischemic stroke. Cerebrovasc Dis. 2018;45(5-6):221–227. doi: 10.1159/000489401. [DOI] [PubMed] [Google Scholar]
- 15.Lyden P. Using the National Institutes of Health Stroke Scale: a cautionary tale. Stroke. 2017;48(2):513–519. doi: 10.1161/STROKEAHA.116.015434. [DOI] [PubMed] [Google Scholar]
- 16.Furlan JC, Vergouwen MD, Fang J, Silver FL.. White blood cell count is an independent predictor of outcomes after acute ischaemic stroke. Eur J Neurol. 2014;21(2):215–222. doi: 10.1111/ene.12233. [DOI] [PubMed] [Google Scholar]
- 17.Kim J, Song TJ, Park JH, et al. Different prognostic value of white blood cell subtypes in patients with acute cerebral infarction. Atherosclerosis. 2012;222(2):464–467. doi: 10.1016/j.atherosclerosis.2012.02.042. [DOI] [PubMed] [Google Scholar]