Abstract
In the early months of the COVID-19 pandemic with no designated cure or vaccine, the only way to break the infection chain is self-isolation and maintaining the physical distancing. In this article, we present a potential application of the Internet of Things (IoT) in healthcare and physical distance monitoring for pandemic situations. The proposed framework consists of three parts: a lightweight and low-cost IoT node, a smartphone application (app), and fog-based Machine Learning (ML) tools for data analysis and diagnosis. The IoT node tracks health parameters, including body temperature, cough rate, respiratory rate, and blood oxygen saturation, then updates the smartphone app to display the user health conditions. The app notifies the user to maintain a physical distance of 2 m (or 6 ft), which is a key factor in controlling virus spread. In addition, a Fuzzy Mamdani system (running at the fog server) considers the environmental risk and user health conditions to predict the risk of spreading infection in real time. The environmental risk conveys from the virtual zone concept and provides updated information for different places. Two scenarios are considered for the communication between the IoT node and fog server, 4G/5G/WiFi, or LoRa, which can be selected based on environmental constraints. The required energy usage and bandwidth (BW) are compared for various event scenarios. The COVID-SAFE framework can assist in minimizing the coronavirus exposure risk.
Keywords: IoT, health monitoring, smart healthcare, pandemic, COVID-19
I. Introduction
Internet of Things (IoT) development brings new opportunities in many applications, including smart cities and smart healthcare. Currently, the primary usage of the IoT in healthcare can be categorized as remote monitoring and real-time health systems. Controlling and managing dire situations, such as the one in 2020 when the coronavirus disease (COVID-19) took over the world, can be achieved with the help of IoT systems, without imposing severe restrictions on people and industries. COVID-19 causes respiratory symptoms and appears to be more contagious in comparison to SARS in 2003 [1]. One way to control the spread of viruses, until a vaccine is available, is to observe physical (or social) distancing [2]. By implementing better systems for surveillance, healthcare, and transportation, contagious diseases will have less chance of spreading [3], [4]. An IoT system, combined with Artificial Intelligence (AI), may offer the following contributions when considering a pandemic [5]: 1) improving public security using surveillance and image recognition systems, 2) utilizing drones for supply, delivery, or disinfection, 3) contact tracing and limiting people’s access to public places through apps and platforms empowered with AI. An IoT system for healthcare is typically composed of many sensors connected to a server; it gives real-time monitoring of an environment or users. In a pandemic, AI-assisted sensors can be used to help predict whether or not people are infected with the virus, based on signs such as body temperature, coughing patterns, and blood oxygen levels. Tracking people’s geolocation can be another useful feature. During the outbreak of a contagious disease, tracking the distance between people can provide valuable information. Using technologies, such as Bluetooth, we can get a reasonable estimate of how much distance people maintain when walking in public places. This data can be used to warn people who are not physically distanced within a specific range, 2 m for example [6], of a person, and thereby, potentially prevent further transmission of the virus. During the development of such platforms, it is also crucial to consider security and data management thoroughly to prevent abuse of personal information [7], [8]. Governments may try to use these platforms and information for permanent surveillance after a pandemic to control and track people’s behaviors.
II. Related Works
During the last several years, different IoT applications have been proposed to improve healthcare systems. The IoT can be used for remote patient monitoring, e.g., connecting seniors who have chronic diseases to doctors and medical resources [9]. IoT applications have been implemented to aid people with Parkinson’s [10] and Alzheimer’s disease [11]. It offers disaster management for seniors who are living alone and need special care [12] and can also be applied to manage equipment and patients in hospitals [13]. In a smart healthcare setting, the IoT can help to provide a remote diagnosis prior to hospitals for more efficient treatment [14]. For diabetic patients, it is vital to monitor their blood glucose continuously [15]; blood glucose data can be sent from wearable sensors to doctors or smartphones for continuous monitoring of patients’ state of health. Castillejo et al. [16] develop an IoT e-health system based on Wireless Sensor Networks (WSN) for firefighters.
Geolocation of people gives important information about a potential outbreak during a pandemic. This process can be performed in many ways, each having its pros and cons although providing accurate estimations. A global positioning system (GPS) uses large power consumption. However, GPS accuracy can be severely degraded based on the position of a receiver and satellites, especially indoors [17]. The work in [18] has demonstrated the feasibility of using the Received Signal Strength Indicator (RSSI) to locate the user in an indoor environment. The user carries a mobile which is connected to the Wireless Local Area Network (WLAN). The mobile sends a signal to several fixed position access points (APs), which are then fused using a Center of Gravity algorithm to locate the user. Chawathe [19] conveys the usage of Bluetooth beacons for geolocation tracking. Bluetooth is used everywhere from smartwatches to phones, but one problem of using this technology is the reflection of its signals, which makes it difficult to acquire accurate distance estimations. In [20], a low-power tracking method for IoT systems is proposed. It uses an orientation sensor and accelerometer for geolocation tracking to reduce the use of GPS, which requires less power consumption. Recently, Apple and Google announced that they would be using Bluetooth for contact tracing of iOS and Android users [21]. Users can turn it on or off, and the data would only be given to trusted health authorities that follow specified privacy policies.
Audio signal processing is another area that can be helpful for the diagnosis of many respiratory diseases. For COVID-19, the patients with advanced cases often suffer from coughing in, but it can also be a symptom of influenza and many other medical conditions [22]. Currently, many research groups are working on this idea to battle COVID-19 [23], including Coughvid from Ecole Polytechnique Federale de Lausanne (EPFL) [24], Breath for Science from NYU [25], CoughAgainstCovid from Wadhwani AI group in collaboration with Stanford University [26], and COVID Voice Detector from Carnegie Mellon University [27]. Imran et al. [22] have made an AI model to distinguish between coughs related to COVID-19 and coughs coused by other respiratory conditions. Their model has achieved promising results; however, their dataset is not large enough. Providing more data about the coughing of COVID-19 patients will make such AI models much more effective.
FluPhone [28] is one of the first projects that utilized users’ phones to study how fast an infectious disease spreads. Mobile phones were used to collect some data, such as the presence of nearby Bluetooth devices, GPS coordination, and flu symptoms. Then, the data were sent to a server via 3G/GPRS [29]. EpiMap [30] was another project done followed FluPhone. The proposed framework could be used for rural areas or developing countries, where opportunistic networks and satellite communications were employed for the transmission of data. Another recent study [30] evaluates how much active contact tracing and surveillance can reduce the spread of infectious diseases. The results show that mobile phone contact tracing has significant social and economic benefits.
In this article, the proposed COVID-SAFE framework offers: 1) a low-cost and lightweight IoT node to monitor continually a person’s body temperature, heart rate, and blood oxygen saturation, and periodically monitor coughing patterns; 2) a smartphone app to display the parameters and individual risk factors; 3) a physical distance tracking mechanism using Bluetooth 4.0 technology to alert the user in case of violation of safe physical distance; and 4) a fog server that collects data from the IoT nodes and applies a machine-learning algorithm to send the necessary information to users.
III. Proposed Framework
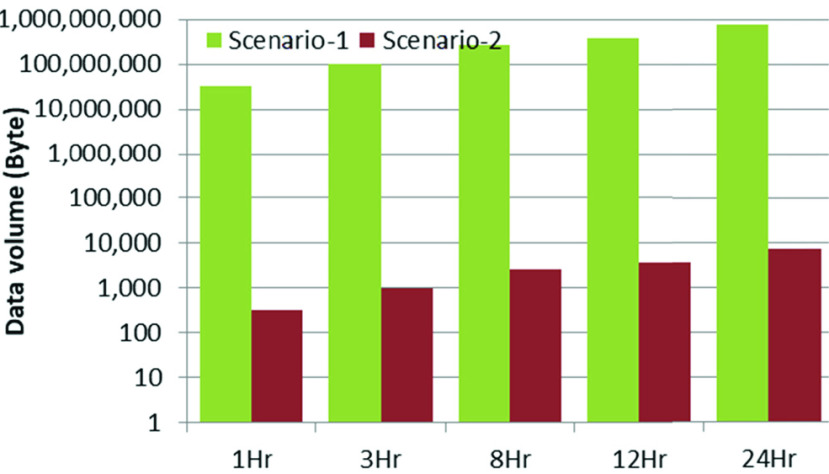
The development of the COVID-SAFE platform relies on three parts, including a wearable IoT device, smartphone app, and fog (or cloud) server. The hardware contains nodes that were developed on the Raspberry Pi Zero (RPIZ). The software parts include an application program interface (API) for interacting with users on a smartphone, and a fuzzy decision-making system on the fog server. Nodes collect specific vital data from participations and upgrade their decision-making regulations to aid users in various scenarios, such as the need to refer to a doctor, maintaining physical distance from others, and alerts regarding high-risk areas. Fig. 1 illustrates the high-level architecture of the COVID-SAFE framework. A detailed description of each part is given in the next sections.
FIGURE 1.
High-level architecture of COVID-SAFE framework, in which COVID-SAFE-1 is carried by the user and COVID-SAFE-2 - N belong to adjacent people.
A. Wearable IoT Device
This IoT node works in association with the user’s smartphone to collect proximity data using Bluetooth and to communicate with the server through the cellular data network. It consists of a RPIZ as the central processor, temperature and photoplethysmogram sensors, and a LoRa module for data communication in the absence of a cellular data network and WiFi. The system then is synchronized with the software to monitor the user’s behavior during daily activities. In Scenario-1, the IoT node sends the sensor data to the smartphone app via Bluetooth connection. The smartphone then sends the data stream to the server via 4G/5G or WiFi. The server feeds the app with the latest updates. The app can notify users of new restrictions and provide useful tips given by the health service and governments. Meanwhile, the app sends the participations’ body parameters for further processing. The cloud server receives all the information and applies a fuzzy inference system on the data, and finally sends back the risk score to the phone for the user. The second mode of operation (Scenario-2) is a LoRa-based network. The IoT node enters this mode when a 4G/5G/WiFi connection is not available. A possible situation is in rural areas with limited Global System for Mobile Communications (GSM) coverage.
The RPIZ has a 1 GHz single Central Processing Unit (CPU) core with 512 MB of Random Access Memory (RAM), several Global Purpose Input/Outputs (GPIOs), wireless LAN, and Bluetooth connectivity, all in one platform. These features make the RPIZ a suitable choice for implementing many IoT-based systems. The COVID-SAFE framework is equipped with a temperature sensor and a photoplethysmogram (PPG) sensor. The PPG sensor is a noninvasive tool that attaches painlessly to the user’s fingertip, sending two wavelengths of light through the finger, and captures the reflected light using a pin diode. The output of this sensor is a PPG signal. The PPG recording is based on an analog sensor and needs a converter before connecting to the digital part; hence, an analog-to-digital converter (ADC) is used. The RPIZ is equipped with an internal Bluetooth and WiFi module, which makes it easy to interface with a smartphone app. The IoT node is battery operated and is designed with a 3D printer as a finger clip to encapsulate the necessary hardware and to be friendly for the user during daily activities.
In order to measure the power consumption of the system, the wearable IoT device is connected to a digital wattmeter. The data is logged in a computer that produces the wattage measurements.
B. Smartphone App
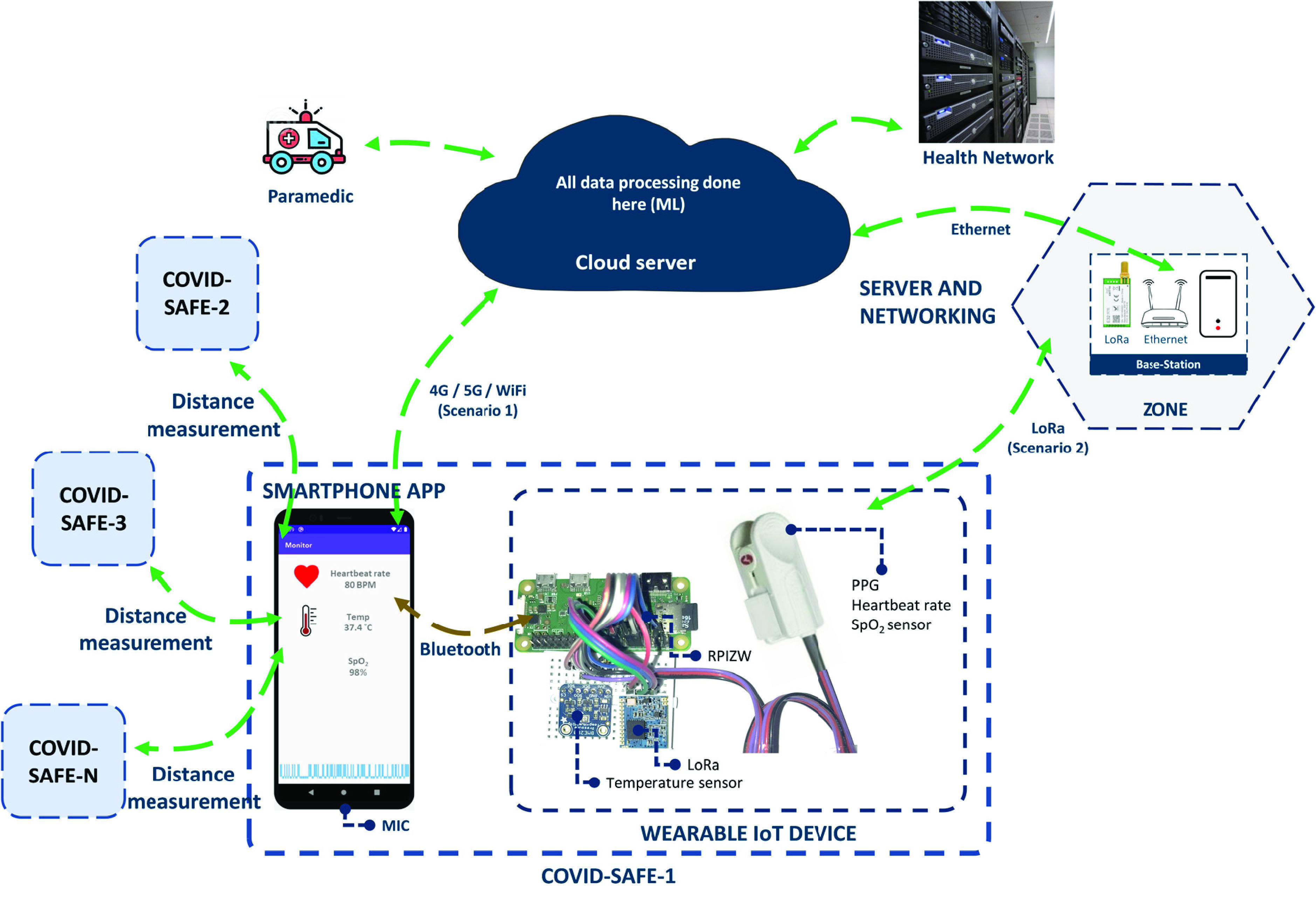
Fig. 2 shows the COVID-SAFE smartphone app, which is built to interact easily with users. First, the user has to create an account and answer general background questions such as gender, age, weight, height, and history of diseases. Fig. 2(b) shows the general information page. By accumulating this information, the system can provide an individual risk factor for the user. Fig. 2(c) shows the radar dashboard; in this menu, all adjacent nodes in the range of 3 m are shown on the screen. The red dots illustrate nodes in the range of 2 m or less, the yellow dots indicate nodes between 2 to 3 m, and green dots are nodes placed at 3 m or further. The app notifies the user as soon as the second node comes closer than the specified range. The position of nodes on the radar screen are separated for better visualization purposes. The app can display the heart rate, body temperature, blood oxygen saturation, and individual risk factor in real-time mode as Fig. 2(d) shows. The output of the decision-making system is depicted in Fig. 2(e). In this fragment, the app asks for symptoms following the body parameters, and it provides the risk evaluation, and sends some useful tips.
FIGURE 2.
COVID-SAFE application which is connected to fog server based on predefined API, a) login menu b) general information page c) radar dashboard d) health monitoring menu and e) individual risk factor.
C. Decision-Making System
A fuzzy inference system called the decision-making system, is used for predicting the risk of spreading the virus. The model estimates a risk factor containing three linguistic values (low, moderate, and high), which can help users to find out if they are in a safe position or if they might spread a disease. There has been significant evolving activities in this domain that are changing our understanding of symptoms and significant features in diagnosis. For instance, government quarantine strategies and risk tolerance may be changed because of various factors, such as economic circumstances, or factors in different regions of a country. In this regard, a fuzzy decision seems more suitable for predicting the risk factor of a person since it conveys uncertainties. Moreover, all predefined rules in a fuzzy system can be updated regularly based on expert definitions from the cloud. A similar model were developed by other researchers with slightly different input variables [32].
A subset of samples from the Khorshid COVID Cohort (KCC) study [33] was used to design the rules of the proposed decision-making system. Thirty samples from COVID-19 patients (the case group) and thirty other samples from hospitalized pneumonia patients (or patients with similar breathing problems) with negative Polymerase Chain Reaction (PCR) and CT-scan results (the control group) were used in our study. The following baseline patient parameters were considered in the clinical study: gender (female, male), age, body temperature, oxygen saturation (SpO2), shortness of breath (yes, no), cough severity (high, increasing-moderate, low), and the presence of chronic respiratory disease (yes, no) (Table 1).
TABLE 1. Characteristics of the Participants in the COVID-19 and Non-COVID-19 Groups.
| Non-COVID | COVID |
 -value -value |
|
|---|---|---|---|
| Gender | 13 (female) | 15 (female) | 0.873 |
| Age (years) | 59.9±19.8 | 59.5±14.4 | 0.919 |
| Body temperature | 37±1 | 39±9 | 0.328 |
| Oxygen saturation (%) | 86±8 | 84±10 | 0.426 |
| Shortness of breath | 9 (no) | 9 (no) | 0.804 |
| Cough severity | 2 (low) 4 (high) |
7 (low) 16 (high) |
< 0.001 |
| Chronic respiratory disease | 18 (no) | 27 (no) | 0.079 |
| N | 30 | 30 | - |
MEAN±SD and frequency were provided for continuous and categorical variables, respectively.
In this research, Sugeno architecture [34] is utilized, and an Adaptive-Network-Based Fuzzy Inference System (ANFIS) is used for training memberships and defining rules [35] for simplicity. All membership function types are selected based on a Gaussian function, which is more conventional for training ANFIS. A similar model [36] was developed by other researchers, wherein they selected rules and membership properties manually without using ANFIS. In addition to the ANFIS model, a support vector machine (SVM) [37] and decision tree [38] are trained to be compared with the proposed method. The advantages of a fuzzy system are that it can handle uncertainty and its linguistic rules can be better realized.
The cellphone fetches the rules from the cloud, which is updated regularly. Inputs of the fuzzy system are defined based on health features, and region-based information. Health-related features include respiratory rate, cough rate, temperature, Body Mass Index (BMI), and blood oxygen saturation level. The region-based risk value can be calculated on the server using parameters such as the last time an exposed case was detected and the number of cases in the region.
D. Data Acquisition
Two different sensors are used in the IoT node. At the startup, the RPIZ initializes all sensors and makes them ready to capture the data. The digital temperature sensor has a 4-byte output resolution. The body temperature usually does not change rapidly; hence, the sensor captures data every 15 or 30 min. In order to have consistency in values, at each iteration, 10 samples are taken, and their average is stored into internal memory storage and also is sent to the server.
The output of the photoplethysmogram sensor is a PPG signal. Due to the nature of the signal, it should be sampled continuously for at least 10 seconds to see the patterns and extract necessary features. The IoT node is responsible to reads the output of the sensor, using an external 8-bit ADC at a 50 Hz sampling rate. By applying the signal processing algorithms on the PPG signal, the heart rate, blood oxygen saturation (SpO2), and respiratory rhythm can be extracted [39]. For measuring the SpO2 from the signal, first, an average of five subsequent samples of the signals ( and
and  ) and offsets (
) and offsets ( and
and  ) for red and infrared waveforms (indexed as 1 and 2, respectively) are measured. Then, SpO2 is measured using a formula given by Maxim Integrated™.
) for red and infrared waveforms (indexed as 1 and 2, respectively) are measured. Then, SpO2 is measured using a formula given by Maxim Integrated™.
 |
where,  / (
/ ( and
and  is the SpO2 value. According to the literature [40], there is substantial evidence that can increasing respiratory rate is a contributing factor in determining COVID-19. For predicting the respiratory rate from the PPG signal, an adaptive lattice notch filter is utilized based on Park and Lee [41]; the results can achieve 0.78% R-square on the MIMIC II dataset.
is the SpO2 value. According to the literature [40], there is substantial evidence that can increasing respiratory rate is a contributing factor in determining COVID-19. For predicting the respiratory rate from the PPG signal, an adaptive lattice notch filter is utilized based on Park and Lee [41]; the results can achieve 0.78% R-square on the MIMIC II dataset.
This database contains physiological signals and a time series of vital signs captured from patient monitors, as well as comprehensive clinical information obtained from hospital information systems. Furthermore, an average of 10 seconds of an estimated respiratory rate and SpO2 are used for reducing prediction error.
The proposed framework can record the surrounding voice using the phone’s microphone to detect the user’s coughing patterns. To save battery power consumption, this feature is activated based on the user’s request. For cough detection, a pre-trained model for acoustic activity prediction is used [42]. For extracting a cough from the environment sounds, a pre-trained model is utilized [43]. After activation, the input microphone is sampled at 5 KHz and an 8-bit resolution for a duration of 10 seconds at each iteration. The reason for choosing 5 KHz is that cough frequency usually accuse between 200–900 Hz [44]. All the sensors’ data are stored in internal memory for further processing.
E. Proximity Detection
Most of the present smartphones have Bluetooth Low Energy (BLE) V4.0 or above, along with another short-range wireless interface like Near Field Communication (NFC). Table 2 presents the comparison among related wireless technologies. It shows that NFC cannot be used for distance measurement due to its short range, and Bluetooth cannot be used due to its higher power consumption and lack of broadcast capability. On the other hand, using the beacon feature implemented in BLE, a connectionless RSSI monitoring can be used to detect the proximity of the devices or to calculate or measure the relative distance between the smartphones.
TABLE 2. Comparison of Smartphone-Based Wireless Interface.
| NFC | Bluetooth | Bluetooth Low Energy | |
|---|---|---|---|
| RFID compatible | ISO 1 8000-3 | Active | Active |
| Standardization body | ISO/IEC | Bluetooth SIG | Bluetooth SIG |
| Network Standard | ISO 13157 etc. | IEEE 802.15.1 | IEEE 802.15.1 |
| Network Type | Point-to-point | WPAN | WPAN |
| Cryptography | Not with RFID | available | available |
| Range | < 0.2 m | ~ 10 m (class 2) | ~ 100 m |
| Frequency | 13.56 MHz | 2.4– 2.5 GHz | 2.4– 2.5 GHz |
| Bit rate | 424 Kbit/s | 2.1 Mbit/s | ~1.0 Mbit/s |
| Setup time | < 0.1 s | < 6 s | < 0.006 s |
| Power consumption | < 15 mA (read) | Varies with class | < 15 mA (Tx or Rx) |
The proposed method makes it possible to indicate whether another person is located at an adjacent area or not. As soon as the second IoT node (along with the associated phone) comes within range, a flag is raised and the user is notified. The relationship between the transmitted signal strength and received signal power level can be mathematically expressed by equation (2):
 |
where,  stands for the distance,
stands for the distance,  is the transmit power,
is the transmit power,  is the received RSSI values, and
is the received RSSI values, and  is the environmental coefficient.
is the environmental coefficient.
Two experiments were performed to validate the distance estimation using the RSSI. In the first experiment, two phones are placed at different orientation (face to face and side by side). One phone is placed at a fixed position to record the signal strength, while the second one can move around. In this experiment, the transmit power was set at 4 different levels (−16 dBm, −26 dBm, −35 dBm, and −59 dBm), and the position of the moving phone was changed from 30 to 240 cm with a 30 cm step size. The same experiment was performed again with a 12 cm wooden wall between the scanner phone and broadcasters to consider various orientation and other ambient conditions, such as reflection and absorption.
In experiment 2, multiple smartphones of different models were used, and Fig. 3 shows a graphical representation of the experimental setup. The RSSI data is acquired in the phone at the center using “Beacon Scanner” with an acquisition frequency of 1 Hz, while other phones are traveling toward and away from the center phone at different angles and orientations. All phones are configured to broadcast the BLE beacon signal (using Google’s Eddystone protocol) at the same interval (3 Hz) with the same transmit power level (−59 dBm). Various angular positions or orientations are defined for the moving phones, and they change their states while the fixed center phone records the received signals.
FIGURE 3.
BLE test setup.
F. Server and Networking
All the sensors’ data are sent from the IoT node to the smartphone using WiFi (IEEE 802.11.x standard protocol) as a physical layer for real-time data visualization. Meanwhile, data are transferred to the fog server for further processing. Any transmission of information through the network utilizing IPv4 or IPv6 and the Representational State Transfer (REST) API is given for each participant to access his or her information.
The main advantage of having REST API is that small devices can use the API even if they have certain limitations such as limited computational capacity and low physical memory. A user can use a designed web page or a smartphone app to link to the services and see his or her status. User data are saved as a user history in the database for potential future development. Connecting to the server can be established either through a 4G/5G infrastructure or LoRa network. Fig. 4 shows a map with different zones; each zone indicates the risk of infection. The database can be updated based on the recent status of regions reported by governments, with parameters such as the number of residences and history of infected people. The map is divided into three colors: green for low risk of infection, yellow for moderate, and red for high.
FIGURE 4.
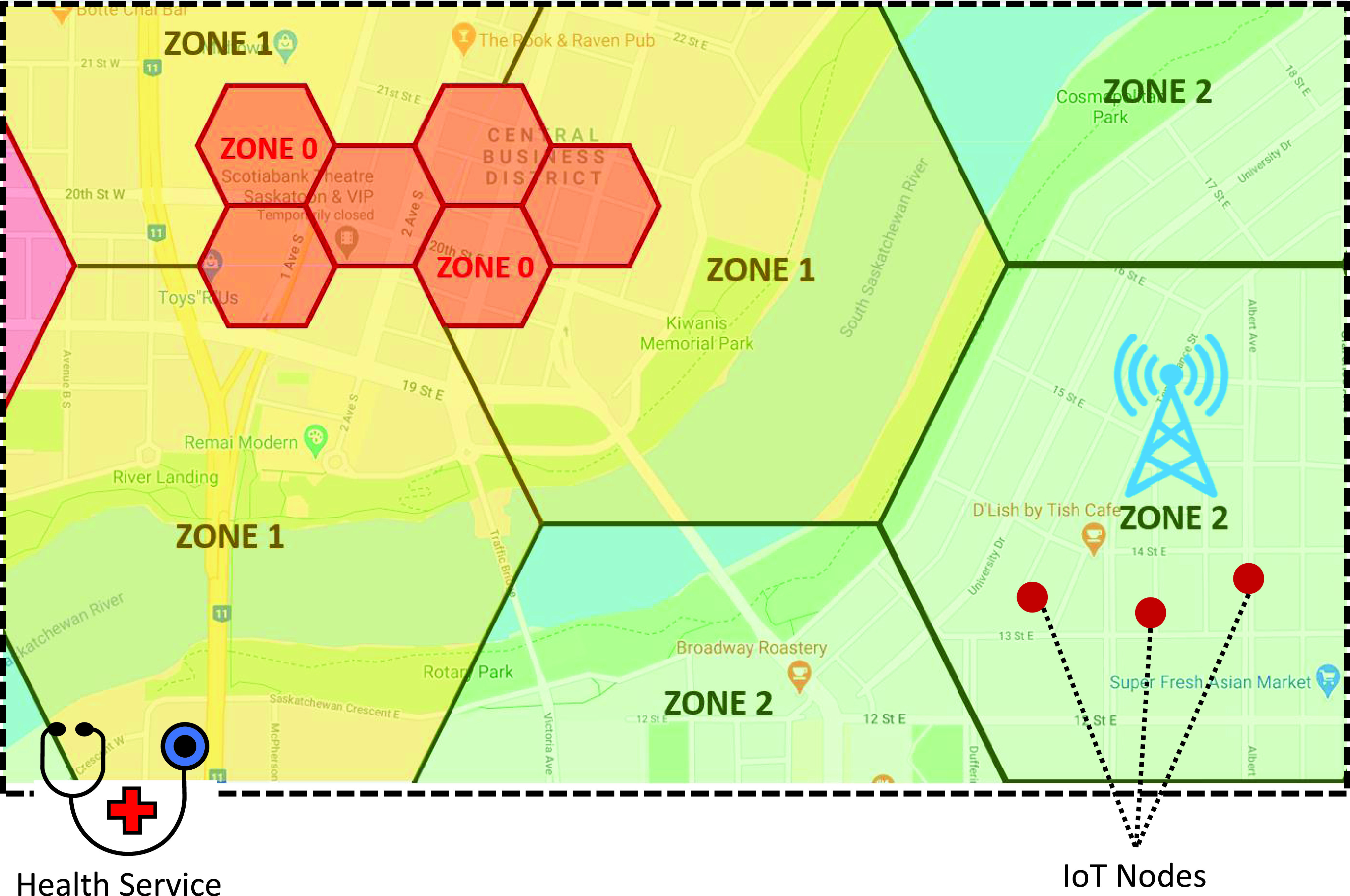
Zone definition (displayed on the smartphone app showing real-time geolocation of hotspots; zone 0 being the most critical with the highest risk of spread; zone 1 has medium risk; zone 2 has low risk).
Zone segmentation has several benefits. First, using the information that each zone provides, users can manage their social activities with the necessary precautions. In addition, governments can send notification to users or limit their access in case of emergency. Thus, the decision-making process is enhanced, and reaction time to a situation is significantly reduced. Information on the zones is then used in risk assessment by the software. The zones should cover the whole map; however, for visualization, only parts of the zones are depicted in Fig. 4.
IV. Results and Discussion
A. Distance Measuring
According to our experiment, Fig. 5 shows the RSSI values at different distances from 30 to 240 cm, where phones are placed face-to-face, side-by-side, and face to face separated by a wooden wall. The results show that the relative orientation between two IoT nodes could change the RSSI by a maximum value of −10 dBm when phones are placed in side-by-side position. The same experiments were conducted while separating the transmitter and receiver by a wooden wall with a thickness of 10 cm to examine the effect of signal blockage by the wooden wall, and the result is shown in Fig. 5(c). Comparing Fig. 5(a) and 5(b) shows that the RSSI levels depend on the relative positions of the phones. Fig. 5(c) also shows significant changes in the RSSI levels with the presence of a wall in between. As expected, a decrease of RSSI with an increase of distance was observed.
FIGURE 5.
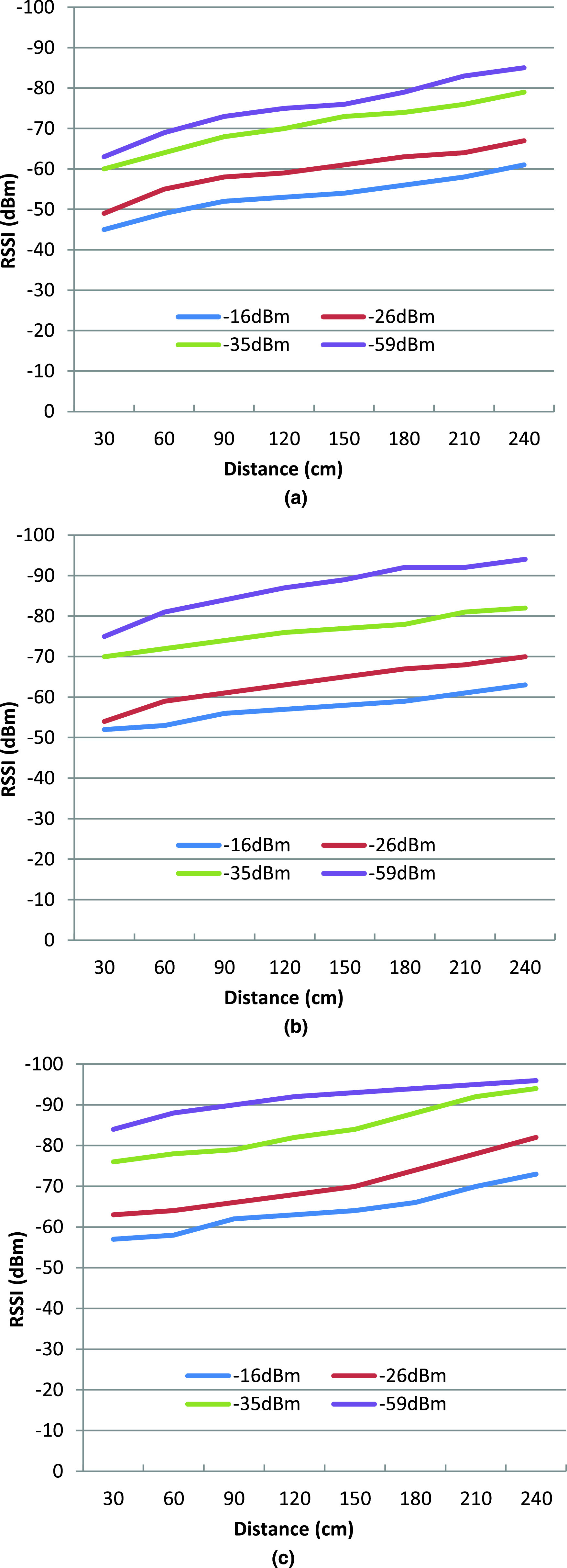
RSSI of BLE for different distances at different Tx power gain (dBm), keeping two smartphones in a) face-to-face, b) side-by-side position, and c) two smartphones in the face-to-face position separated by a wooden wall.
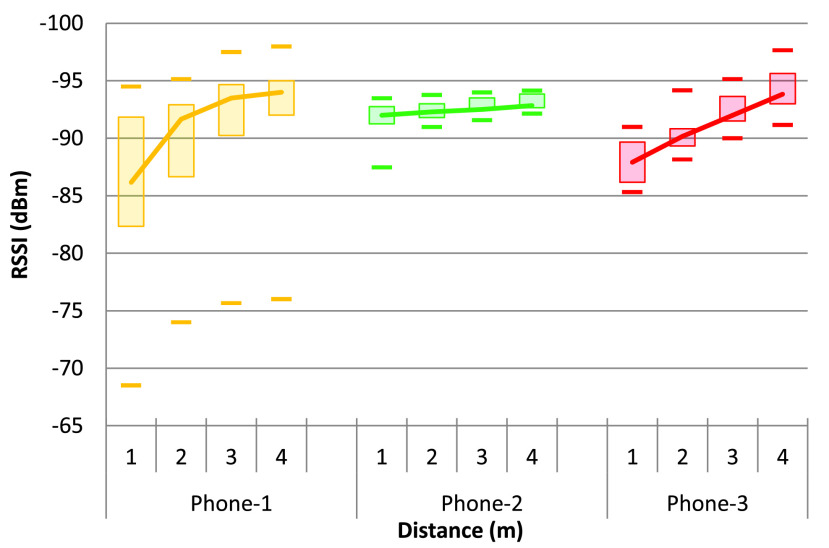
This result is further justified by experiment 2 (as shown in Fig. 3), and the results are shown in Fig. 6. The data are processed separately for every phone used, and there is a noticeable relationship with the distance from the receiving phone. Although this relationship between RSSI and distance is highly dependent on the device itself (model or hardware construction), this can still be used to calculate the distance between two devices by using Bayesian filters (such as a Kalman filter or particle filter) to reduce the noise in the RSSI data [45].
FIGURE 6.
RSSI of BLE at four different distances with various orientation and fixed transmit power for three different types of cellphones.
Equation (2) can be presented in a more straightforward format, as shown in (3), where the environmental coefficient  is replaced by a and
is replaced by a and  . Parameter
. Parameter  is used as a threshold for the initial alarm or to trigger the calculation function locally in the IoT node. Parameter
is used as a threshold for the initial alarm or to trigger the calculation function locally in the IoT node. Parameter  , along with the reference RSSI (RSSI at 1 m distance, denoted as
, along with the reference RSSI (RSSI at 1 m distance, denoted as  ), is used to calculate the distance from the RSSI measured (denoted as
), is used to calculate the distance from the RSSI measured (denoted as  ).
).
 |
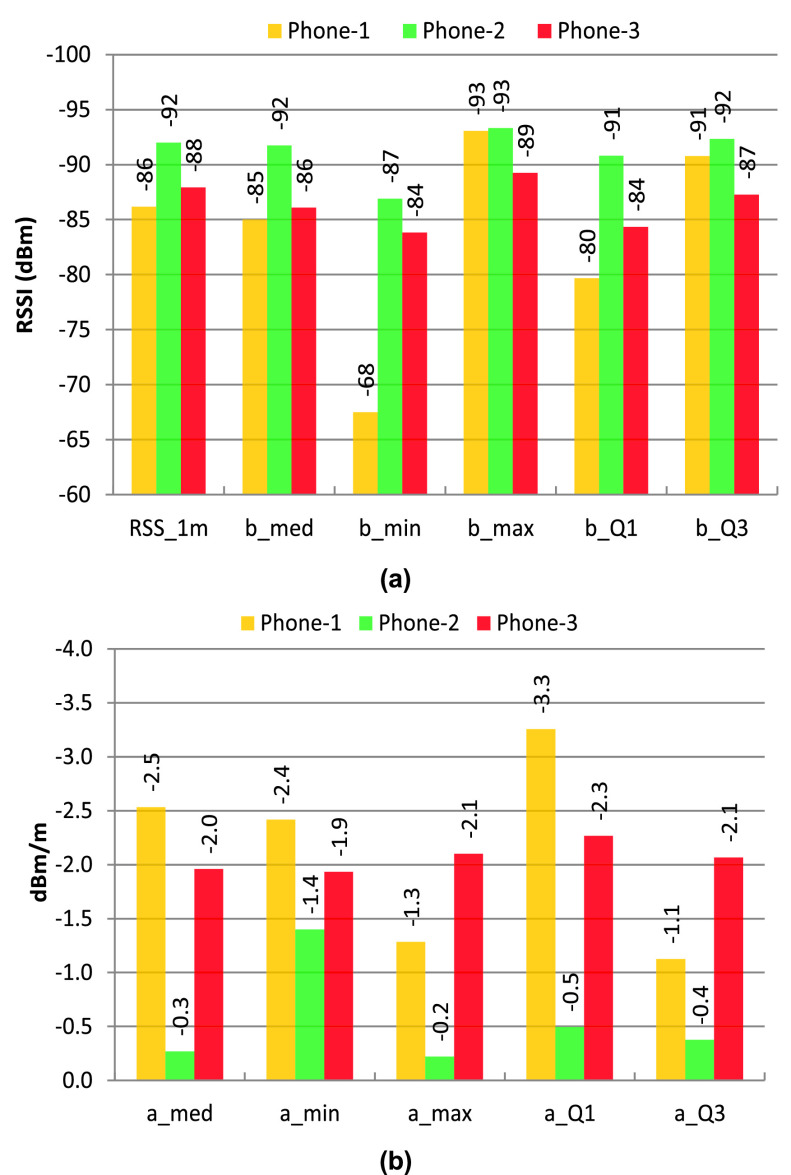
Fig. 7(a) shows the phone-specific values of the reference RSSI (at 1 m distance) and the parameter  for different RSSI levels like maximum, minimum, Q1 (lower limit of the 75% quartile), Q3 (upper limit of the 75% quartile); and Fig. 7(b) shows the phone-specific values of the parameter a for different RSSI levels. For this experiment, a threshold of −93 dBm (taken from the value of parameter
for different RSSI levels like maximum, minimum, Q1 (lower limit of the 75% quartile), Q3 (upper limit of the 75% quartile); and Fig. 7(b) shows the phone-specific values of the parameter a for different RSSI levels. For this experiment, a threshold of −93 dBm (taken from the value of parameter  for the maximum RSSI level above 2 m distance) can be used to trigger the proximity aware alarm and the distance calculation function in the smartphone app. However,
for the maximum RSSI level above 2 m distance) can be used to trigger the proximity aware alarm and the distance calculation function in the smartphone app. However,  ,
,  , and the reference RSSI are dependent on the smartphone used and the real-life environment. There are several algorithms, such as SVM and Machine Learning (ML) [46], with the device or environment-specific training parameterization [47] that can be used to calculate the distance between the devices. In addition, AltBeacon can be used to get device-specific information (manufacturer identification number and 1 m reference RSSI) along with the beacon signal [48] which can be used to improve the distance accuracy for different types of devices used.
, and the reference RSSI are dependent on the smartphone used and the real-life environment. There are several algorithms, such as SVM and Machine Learning (ML) [46], with the device or environment-specific training parameterization [47] that can be used to calculate the distance between the devices. In addition, AltBeacon can be used to get device-specific information (manufacturer identification number and 1 m reference RSSI) along with the beacon signal [48] which can be used to improve the distance accuracy for different types of devices used.
FIGURE 7.
(a) Phone specific RSSI values for the 1 m reference and the RSSI threshold of  for different levels of RSSI data (maximum, minimum, median, Q1 of 75%, and Q3 of 75% RSSI values), (b) phone specific values of a for different levels of RSSI data (maximum, minimum, median, Q1 of 75%, and Q3 of 75%.
for different levels of RSSI data (maximum, minimum, median, Q1 of 75%, and Q3 of 75% RSSI values), (b) phone specific values of a for different levels of RSSI data (maximum, minimum, median, Q1 of 75%, and Q3 of 75%.
In order to notify the user to maintain physical distancing, three threshold values are indicated. The software checks the RSSI values then maps them to the distance according to equation (3). If the distance is less than 200 cm a red flag is raised, if the transmitter is in the range of 200 to 300 cm the flag is yellow, and if the distance is longer than 300 cm it is green.
B. Decision-Making Results
Table 3 shows the parameters acquired for training the model using ANFIS.
TABLE 3. Inputs and Outputs Membership Functions in Proposed Fuzzy System.
| Feature Name | Description ([ , ,  ]) ]) |
|---|---|
| Shortness of breath | Has: [.2,1] Has not: [.2,2] |
| Cough rate | Normal: [0.35 2.00] Not normal: [0.35 3.00] |
| Temperature | Cluster 1: [0.70 36.67] Cluster 2: [0.70 37.33] Cluster 3: [0.70 38.00] Cluster 4: [0.70 38.67] Cluster 5: [0.70 39.33] |
| Age | 15 Clusters evenly distributed between 10 and 90 with 
|
| SpO2 | 15 clusters unevenly distributed between 60 and 100 with 
|
| Gender | Male: [.2,1] Female: [.2,2] |
| Predicted risk | 15 clusters with Sugeno type |
The performance of the proposed method is compared with two ML methods, decision tree and SVM classifiers. The results are provided for five times a training algorithm with shuffling data based on hold-out validation (70% train-30% test) in Table 4.
TABLE 4. Accuracy and F1-Score Indices for Test Set According to Different Methods.
| Method | Accuracy (%) | F1-score (%) |
|---|---|---|
| Proposed Method | 74.7 ± 4.2 | 75.3 ± 3.7 |
| Decision tree | 72.9 ± 4.0 | 73.5 ± 3.8 |
| SVM | 72.6 ± 4.2 | 74.1 ± 4.0 |
Fig. 8 illustrates two examples of fuzzy rules and shows a risk of 0.79 and 0.07 for two people aged 45, with different genders, and similar shortness of breath. The first person has a low fever, and his cough rate is higher than the other persons. It is worth noting that the estimated rules in the fuzzy interference system may not be ideal and can be extended and modified over time based on received feedback. The closed-loop system requires more data and could be addressed in future work.
FIGURE 8.
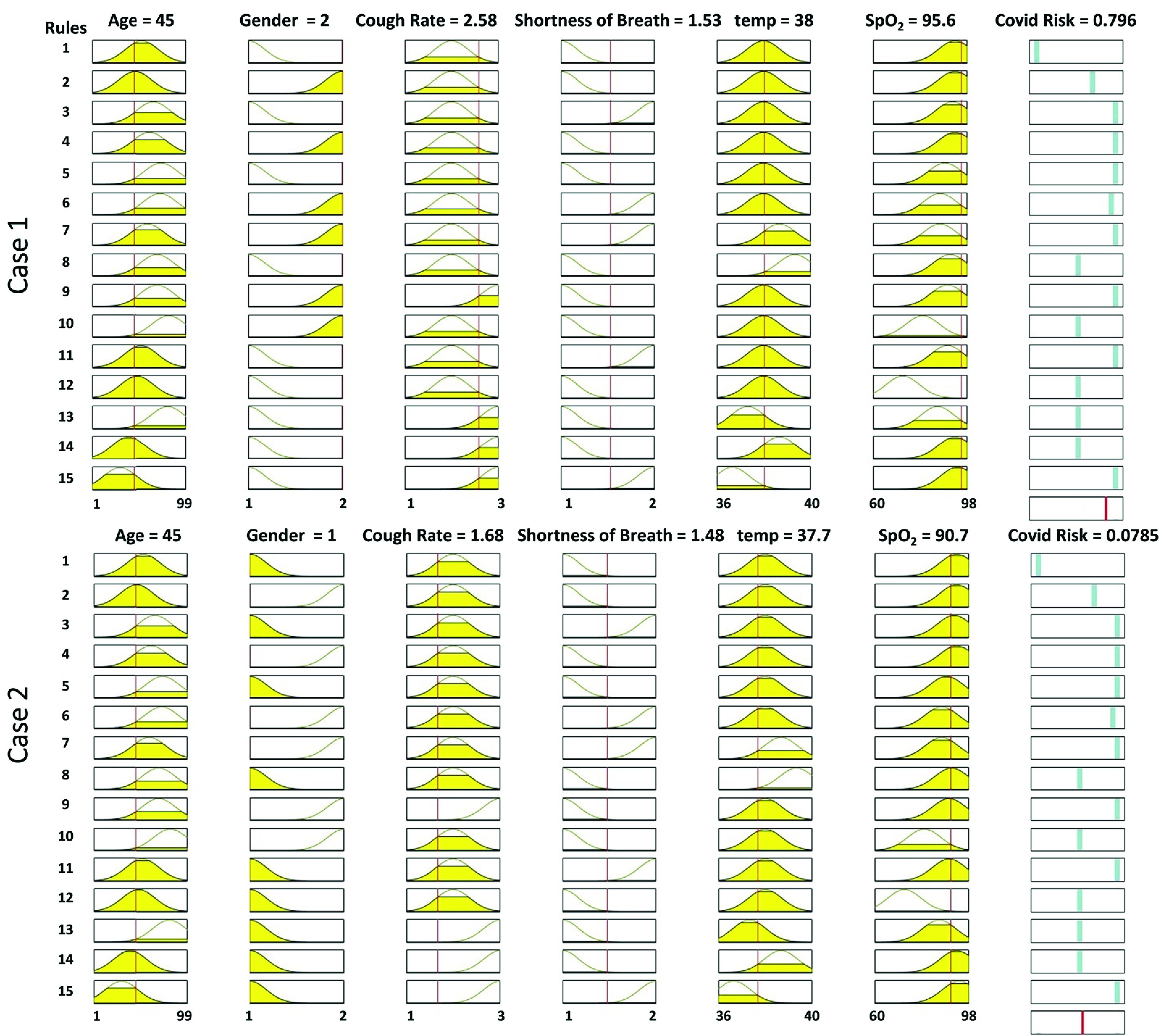
The designed fuzzy inference system based on rules defined in the cloud. Two examples of rules for showing how a person’s risk is generated, based on input features.
C. System Performance
Table. 5 shows scenario-specific activities with power requirements for the various activities measured at the laboratory. According to the measured power, we can quantify the overall energy demand based on scenario-specific activities. Smartphone app power analysis shows that 25 mA is used for all processing in the cellphone. The bandwidth requirement is based on a one-second volume of data generated by the PPG sensors and voice data at the specified sampling rate.
TABLE 5. Scenario Specific Activities and Power Requirement.
| Scenario | No Network | S1 | S2 | Power consumption (mW) |
|---|---|---|---|---|
| Data acquisition | Yes | Yes | Yes | 678 |
| Data post-processing | Yes | No | Yes | 770 |
| LoRa Transfer | No | No | Yes | 1040 |
| Cellular network | No | Yes | No | 970 |
| BW requirement (bps) | 147 K | 80 | ||
| Data Burst time (sec) | 1 | 0.02 |
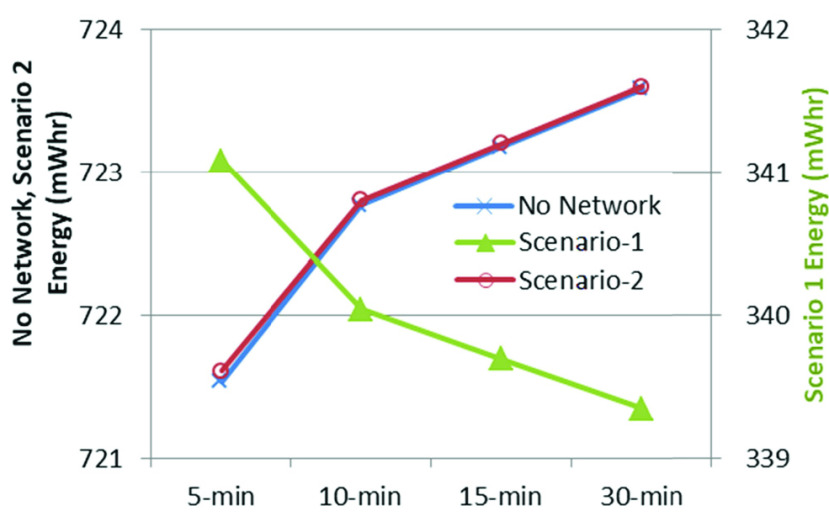
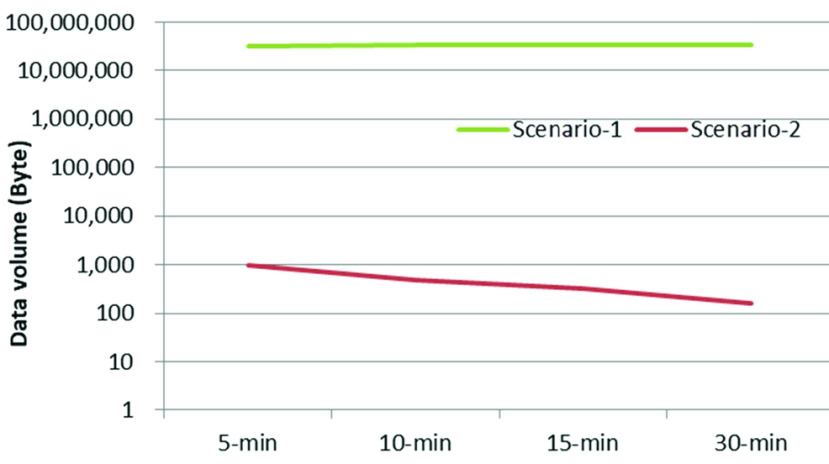
Time ranges, spanning 5 to 30 minutes, were used for data transfer using LoRa or Bluetooth. Scenario-specific energy demand was distinct, depending on time span. Fig. 9 shows the hourly energy requirement for different transmission intervals; No Network and Scenario-2 require almost the same amount of energy, while Scenario-1 requires less than half of that as there is no offline processing in the IoT node itself. Since the node may need to be carried during only part of the day, the daily energy requirement will also vary depending on the duration of the operation. Scenario-1 is shown on a different scale for better visualization of the changes with transmission intervals.
FIGURE 9.
Scenario-specific hourly energy requirement for different transmission intervals.
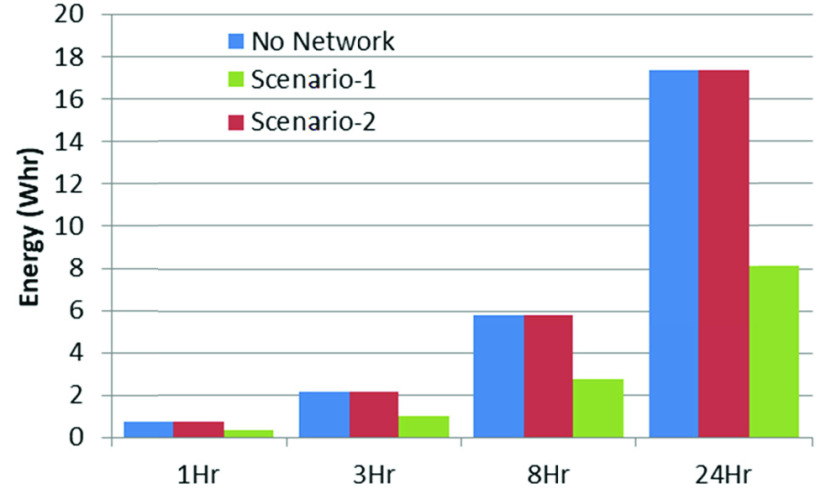
Fig. 10 shows the energy requirement for various durations of daily operation using 15-minute transmission intervals. It also shows that local processing requires more than double the energy, compared with that required to send the unprocessed data over the wireless link.
FIGURE 10.
Scenario-specific hourly energy requirement.
Since data acquisition and processing were carried out continuously, and the unprocessed data was sent to the network, hourly data volume remained the same for Scenario-1. However, it varied in Scenario-2 as only the processed data was sent. Fig. 11 shows the hourly data volume sent over the wireless links (both LoRa and Bluetooth) for different transmission intervals. Scenario-1 generated much higher data volume compared with Scenario-2 due to the transmission of unprocessed sensor data over the wireless link. Fig. 12 shows the data volume to be transferred over the wireless links at a transmission interval of 15 minutes for different durations of operation of the portable node.
FIGURE 11.
Scenario-specific hourly data volume for different transmission intervals.
FIGURE 12.
Scenario-specific data volume for different operation durations at 15-minute transmission intervals.
After comparing both scenarios in terms of energy and bandwidth requirement, it can be seen that Scenario-1 is better fit for outdoor use, where the energy requirement could be a constraint and there is good quality wireless data connectivity, mainly in an urban area. On the other hand, Scenario-2 might be a better choice for rural areas with a lack of cellular network coverage. Therefore, the energy requirement can be reduced by increasing the data-transmission interval mainly for outdoor operation of the node.
Table 6 provides a summary of recent similar systems available to fight COVID-19 with the help of digital technology. As shown the proposed COVID-SAFE system presents a more complete IoT framework than others and can be used to control the infection after the pandemic. Many countries have implemented contact tracing apps, which are similar to the one shown in [21]. However, these apps merely trace a patient’s history and location, and notify users if anyone has contracted COVID-19 in the places they have recently visited. On the other hand, the proposed system provides hardware, sensors, and software (ML and mobile apps), which offer many other benefits, as shown in the table.
TABLE 6. Available Technologies for COVID-19 Pandemic.
| Ref | Description / Scope | Service offered | |||||
|---|---|---|---|---|---|---|---|
| COVID symptoms | Hardware offered? | Diagnosis | Notification to person/ HA | Update real-time? | Remote monitoring | ||
| [1] | Overview of digital technology and COVID-19 | No | No | No | No | No | No |
| [21] | Contact tracing, exposure notifications system by Apple and Google | No | Use smartphone | No | Yes, Yes | Yes | Yes |
| [22] | AI4COVID-19 – cough sample via an app | Yes (cough) | Use smartphone | Yes (cough samples) | Yes, No | Yes | No |
| [49] | AI-enabled CT for fast diagnosis of patients | No | No | Yes (CT scan) | No, Yes | No | No |
| [50] | nCapp diagnosis and treatment system | Yes (based on questionnaire only) | No (caregivers wear VR glass) | Yes (based on questionnaire only) | Yes, Yes | No | Yes |
| [51] | Smart-city network and AI-based universal data sharing standards | No | No | No | No | No | No |
| [52] | A plasmonic biosensor for COVID diagnosis | No | Yes | Yes (plasmon resonance) | No, Yes | No | No |
| [53] | Small wearables for social distancing | No | Developing kit | No | Yes | Yes | Yes |
| Our | COVID-SAFE – a complete IoT system | Yes (fever, cough, SpO2, HR, BMI, hotspots) | Yes (both smartphone and sensors to collect real-time data) | Yes (personal and regional data) | Yes, Yes | Yes | Yes |
V. Conclusion
In this article, an IoT framework is presented to monitor participants’ health conditions and notify them to maintain physical distancing. The proposed system integrates a wearable IoT node with a smartphone app, by which the IoT sensor node can collect a user’s health parameters, such as temperature and blood oxygen saturation, and the smartphone connects to the network to send the data to the server. The paper proposed a Radio Frequency (RF) distance-monitoring method which operates both for indoor and outdoor environments to notify users to maintain the physical distancing. Applying ML algorithms on body parameters makes it possible to monitor participant’s’ health conditions and to notify individuals in real time. A voice coughing-detector continually monitors the user’s voice and records the number and severity of coughing. The fog-based server is implemented to process received data from an IoT node using a cellular network or LoRa connection. In addition, locally processing the data makes it possible to use the IoT node in the environments without internet connectivity or fog-based networks. The system can assist participants in monitoring their daily activities and minimize the risk of exposure to the Coronavirus.
Biographies
Seyed Shahim Vedaei received the B.S. degree in electrical and electronic engineering from IAUCTB University, Tehran, Iran, in 2015, and the M.S. degree in electrical and electronic engineering from KNTU University, Tehran, in 2018. He is currently pursuing the Ph.D. degree in electrical engineering with the University of Saskatchewan, Saskatoon, SK, Canada. He has been a Research Assistant with the Multimedia Processing and Prototyping Laboratory (MPP Lab), since January 2019. His current research interests include, but not limited to, hardware design, the Internet of Things (IoT)-based smart systems, embedded software develop, machine learning, and biomedical systems.
Amir Fotovvat received the B.Sc. degree in a major in electrical engineering, telecommunications, and a minor in computer software engineering from the K. N. Toosi University of Technology, Tehran, Iran, in 2019. He is currently pursuing the M.Sc. degree in electrical and computer engineering with the University of Saskatchewan, SK, Canada.
Since September 2019, he has been working as a Research Assistant at the Multimedia Processing and Prototyping Laboratory (MPP Lab). His research interests mainly include computer networks, Internet security, the Internet of Things (IoT), machine learning, and image processing.

Mohammad Reza Mohebbian received the B.Sc. and M.Sc. degrees in biomedical engineering from the University of Isfahan. He is currently pursuing the degree in electrical and computer engineering with the University of Saskatchewan, Canada. He ranked in the top 2 of the B.Sc. and M.Sc. students. He won the Devolved Scholarship from the University of Saskatchewan, in 2019, and conducted a research for Philips, Canada, during his Ph.D. program.
Gazi M. E. Rahman (Graduate Student Member, IEEE) received the B.Sc. and M.Sc. degrees in electrical and electronic engineering from the Bangladesh University of Engineering and Technology (BUET), Dhaka, Bangladesh, in 1999 and 2008, respectively. He is currently pursuing the Ph.D. degree in electrical and computer engineering with the University of Saskatchewan, Canada.
He started his career with cellular communication service provider and continued for ten years, contributed to automate some system management, planning, and reporting system over there. He also worked as an Assistant Professor at the Electrical and Electronic Engineering Department, United International University, Bangladesh. He has been working as a Research Assistant at the Multimedia Processing and Prototyping Laboratory (MPP Lab), University of Saskatchewan, since May 2018. He contributed to the commercial product development based on embedded systems and the Internet of Things (IoT) for various industries. His main research interests include the IoT-based WSN, embedded system design, and machine learning.
Khan A. Wahid (Senior Member, IEEE) received the B.Sc. degree from the Bangladesh University of Engineering and Technology, in 2000, and the M.Sc. and Ph.D. degrees from the University of Calgary, in 2003 and 2007, respectively. He is currently a Professor with the Department of Electrical and Computer Engineering, University of Saskatchewan. He has coauthored three book chapters and over 180 peer-reviewed journal and international conference papers in the field of health informatics, wireless capsule endoscopy, wearable health monitoring, smart-health, the Internet-of-Things, and smart-city. He has three patents. His research on capsule endoscopy was featured in local and Canadian national media (CBC, CTV, and Global). His work attracted funding from major Canadian and international agencies (NSERC, CFI, WED Canada, Grand Challenges, Government of Saskatchewan). He has been serving on the multidisciplinary review panel of several national funding programs, including NSERC Discovery, I2I, New Frontiers in Research Fund, and MITACS. He has served on the technical program and advisory committee of numerous IEEE sponsored international conferences. Along with the Award of Innovation in 2016, he received many prestigious awards and scholarships, including the Most Distinguished Killam Scholarship and the NSERC Canada Graduate Scholarship for his doctoral research. He is a registered Professional Engineer in the Province of Saskatchewan.
Paul Babyn received the degrees in biology and electrical engineering from the Massachusetts Institute of Technology and the Medical degree from McGill University.
He completed his residency in diagnostic imaging at the Pennsylvania Hospital, Philadelphia, and fellowships in general radiology and neuroradiology/special procedures at The Hospital for Sick Children. He is a member of the Radiological Society of North America, the Canadian Association of Radiology, and the Society for Pediatric Radiology.

Hamid Reza Marateb received the B.S. degree from the Shahid Beheshti University of Medical Science, in 2000, the M.S. degree from the Amirkabir University of Technology, Tehran, Iran, in 2003, and the Ph.D. degree from the Laboratory of Engineering of Neuromuscular Systems, Politecnico di Torino, Turin, Italy, in 2011. He received the Postdoctoral Fellowship from the Laboratory of Engineering of Neuromuscular Systems, Politecnico di Torino, in 2012. He was a Visiting Researcher with Stanford University, in 2009, and Aalborg University, in 2010. He was a Visiting Professor with the Universitat Politècnica de Catalunya, BarcelonaTech (UPC), Barcelona, Spain, in 2012 and 2017. He is currently with the Department of Biomedical Engineering, Faculty of Engineering, University of Isfahan, Iran, and the Biomedical Engineering Research Center, BIOsignal Analysis for Rehabilitation and Therapy Research Group (BIOART), Department of Automatic Control, UPC. His research interests include cognitive informatics in health and biomedicine, mainly focusing on clinical neurophysiology, computational neurosciences, and medical data mining. He also received European Union/Spanish grants (e.g., Marie Curie Fellowship and MYOSLEEVE). He is a Reviewer in more than 30 international ISI journals and is in the editorial board of international journals, including Frontiers in Integrative Physiology and Frontiers in Cognitive Neuroscience.

Marjan Mansourian received the B.S. and M.S. degrees from the University of Isfahan and Isfahan University of Medical Sciences, Isfahan, Iran, in 2003 and 2007, respectively, and the Ph.D. degree in biostatistics from Tarbiat Modares University, Tehran, Iran, in 2004. She is currently affiliated to the BIOART Research Group (UPC) with the Marie Curie Fellowship and the Biostatistics and Epidemiology Department, Faculty of Health, Isfahan University of Medical Sciences, Iran, as a Professor and also the Head of the Burden of Disease Department, Isfahan Cardiovascular Research Center, a WHO-collaborating center. She has authored numerous publications in indexed journals in the field of data modeling and medical data mining. Her research interests include longitudinal data mining/modeling and survival analysis.

Ramin Sami is currently a Pulmonologist and Intensivist. He has been a Faculty Member of the Isfahan University of Medical Sciences for nine years. He also had an observership in interventional pulmonology at the Thoraxklinik Heidelberg, Germany, under Univ.-Prof. Dr. med. Felix Herth’s supervision. He is the Head of the Khorshid Hospital (the COVID-19 referral hospital in Isfahan). He has published six national books in the field of pulmonary diseases and the author/coauthor of 12 articles in international journals. He is also working on ICT-based medical student teaching. His research interests include multidisciplinary management of invasive pulmonology, chronic respiratory diseases, ICU, and respiratory infections. He is an Executive Member of the Iranian Respiratory Society.
Funding Statement
This work was supported by the Natural Sciences and Engineering Research Council of Canada (NSERC).
References
- [1].Ting D. S. W., Carin L., Dzau V., and Wong T. Y., “Digital technology and COVID-19,” Nature Med., vol. 26, no. 4, pp. 459–461, Apr. 2020, doi: 10.1038/s41591-020-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lewnard J. A. and Lo N. C., “Scientific and ethical basis for social-distancing interventions against COVID-19,” Lancet Infect. Dis., vol. 20, no. 6, pp. 631–633, 2020, doi: 10.1016/S1473-3099(20)30190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Woolhandler S. and Himmelstein D. U., “Intersecting U.S. epidemics: COVID-19 and lack of health insurance,” Ann. Internal Med., vol. 173, no. 1, pp. 63–64, Jul. 2020, doi: 10.7326/M20-1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Christaki E., “New technologies in predicting, preventing and controlling emerging infectious diseases,” Virulence, vol. 6, no. 6, pp. 558–565, Aug. 2015, doi: 10.1080/21505594.2015.1040975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Penang Institude. (2020). Smart City Technologies Take on COVID-19. Accessed: Aug. 2, 2020. [Online]. Available: https://penanginstitute.org/publications/issues/smart-city-technologies-take-on-covid-19/
- [6].Setti L., Passarini F., De Gennaro G., Barbieri P., Perrone M. G., Borelli M., Palmisani J., Di Gilio A., Piscitelli P., and Miani A., “Airborne transmission route of COVID-19: Why 2 meters/6 feet of inter-personal distance could not be enough,” Int. J. Environ. Res. Public Health, vol. 17, no. 8, pp. 2932–2937, 2020, doi: 10.3390/ijerph17082932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Calvo R. A., Deterding S., and Ryan R. M., “Health surveillance during covid-19 pandemic,” BMJ, vol. 2020, p. m1373, Apr. 2020, doi: 10.1136/bmj.m1373. [DOI] [PubMed] [Google Scholar]
- [8].Sharon T., “Blind-sided by privacy? Digital contact tracing, the Apple/Google API and big tech’s newfound role as global health policy makers,” Ethics Inf. Technol., Jul. 2020, doi: 10.1007/s10676-020-09547-x. [DOI] [PMC free article] [PubMed]
- [9].Yin Y., Zeng Y., Chen X., and Fan Y., “The Internet of Things in healthcare: An overview,” J. Ind. Inf. Integr., vol. 1, pp. 3–13, Mar. 2016, doi: 10.1016/j.jii.2016.03.004. [DOI] [Google Scholar]
- [10].Pasluosta C. F., Gassner H., Winkler J., Klucken J., and Eskofier B. M., “An emerging era in the management of Parkinson’s disease: Wearable technologies and the Internet of Things,” IEEE J. Biomed. Health Informat., vol. 19, no. 6, pp. 1873–1881, Nov. 2015, doi: 10.1109/JBHI.2015.2461555. [DOI] [PubMed] [Google Scholar]
- [11].Laplante P. A. and Laplante N., “The Internet of Things in healthcare: Potential applications and challenges,” IT Prof., vol. 18, no. 3, pp. 2–4, May 2016, doi: 10.1109/MITP.2016.42. [DOI] [Google Scholar]
- [12].Pandey P. and Litoriya R., “Elderly Care through Unusual Behavior Detection: A Disaster Management Approach using IoT and Intelligence,” IBM. J. Res. Dev., vol. 64, nos. 1–2, pp. 1–11, 2019, doi: 10.1147/JRD.2019.2947018. [DOI] [Google Scholar]
- [13].Kang S., Baek H., Jung E., Hwang H., and Yoo S., “Survey on the demand for adoption of Internet of Things (IoT)-based services in hospitals: Investigation of nurses’ perception in a tertiary university hospital,” Appl. Nursing Res., vol. 47, pp. 18–23, Jun. 2019, doi: 10.1016/j.apnr.2019.03.005. [DOI] [PubMed] [Google Scholar]
- [14].Kotronis C., Minou G., Dimitrakopoulos G., Nikolaidou M., Anagnostopoulos D., Amira A., Bensaali F., Baali H., and Djelouat H., “Managing Criticalities of e-Health IoT systems,” Proc. IEEE 17th Int. Conf. Ubiquitous Wireless Broadband (ICUWB), Salamanca, Spain, 2017, pp. 1–5, doi: 10.1109/ICUWB.2017.8251004. [DOI] [Google Scholar]
- [15].Chang S.-H., Chiang R.-D., Wu S.-J., and Chang W.-T., “A context-aware, interactive M-health system for diabetics,” IT Prof., vol. 18, no. 3, pp. 14–22, May 2016, doi: 10.1109/MITP.2016.48. [DOI] [Google Scholar]
- [16].Castillejo P., Martinez J.-F., Rodriguez-Molina J., and Cuerva A., “Integration of wearable devices in a wireless sensor network for an E-health application,” IEEE Wireless Commun., vol. 20, no. 4, pp. 38–49, Aug. 2013, doi: 10.1109/MWC.2013.6590049. [DOI] [Google Scholar]
- [17].Aly H., Basalamah A., and Youssef M., “Accurate and energy-efficient GPS-less outdoor localization,” ACM Trans. Spatial Algorithms Syst., vol. 3, no. 2, pp. 1–31, Aug. 2017, doi: 10.1145/3085575. [DOI] [Google Scholar]
- [18].Ng J. K.-Y., Lam K.-Y., Cheng Q. J., and Shum K. C. Y., “An effective signal strength-based wireless location estimation system for tracking indoor mobile users,” J. Comput. Syst. Sci., vol. 79, no. 7, pp. 1005–1016, Nov. 2013, doi: 10.1016/j.jcss.2013.01.016. [DOI] [Google Scholar]
- [19].Chawathe S. S., “Indoor Localization Using Bluetooth-LE Beacons,” in Proc. 9th IEEE Annu. Ubiquitous Comput., Electron. Mobile Commun. Conf. (UEMCON), New York, NY, USA, 2018, pp. 262–268, doi: 10.1109/UEMCON.2018.8796600. [DOI] [Google Scholar]
- [20].Zhang L., Liu J., and Jiang H., “Energy-efficient location tracking with smartphones for IoT,” in Proc. Sensors, Taipei, Japan, 2012, pp. 1–4, doi: 10.1109/ICSENS.2012.6411521. [DOI] [Google Scholar]
- [21].Exposure Notifications: Helping fight COVID-19. Accessed: Jul. 20, 2020. [Online]. Available: https://www.google.com/covid19/exposurenotifications/
- [22].Imran A., Posokhova I., Qureshi H. N., Masood U., Riaz M. S., Ali K., John C. N., Hussain M. I., and Nabeel M., “AI4COVID-19: AI enabled preliminary diagnosis for COVID-19 from cough samples via an app,” Informat. Med. Unlocked, vol. 20, 2020, Art. no. 100378, doi: 10.1016/j.imu.2020.100378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Deshpande G. and Schuller B., “An overview on audio, signal, speech, language processing for COVID-19,” 2020, arXiv:2005.08579. [Online]. Available: http://arxiv.org/abs/2005.08579 [Google Scholar]
- [24].Coughvid. Accessed: Aug. 2, 2020. [Online]. Available: https://coughvid.epfl.ch/about/
- [25].Breath for Science. Accessed: Aug. 2, 2020. [Online]. Available: https://www.breatheforscience.com
- [26].Cough Against Covid. Accessed: Aug. 2, 2020. [Online]. Available: https://www.coughagainstcovid.org
- [27].COVID Voice Detector. Accessed: Aug. 2, 2020. [Online]. Available: https://cvd.lti.cmu.edu/
- [28].FluPhone Project: Understanding Spread of Infectious Disease and Behavioural Responses. Accessed: Aug. 2, 2020. [Online]. Available: https://www.cl.cam.ac.uk/research/srg/netos/projects/archive/fluphone2
- [29].Yoneki E., “FluPhone study: Virtual disease spread using haggle,” in Proc. 6th ACM workshop Challenged Netw., 2011, pp. 65–66, doi: 10.1145/2030652.2030672. [DOI] [Google Scholar]
- [30].Yoneki E. and Crowcroft J., “EpiMap: Towards quantifying contact networks and modelling the spread of infections in developing countries,” in Proc. 1st Int. Conf. Wireless Technol. Hum. Relief, 2011, pp. 233–240, doi: 10.1145/2185216.2185282. [DOI] [Google Scholar]
- [31].Hernandez-Orallo E., Manzoni P., Calafate C. T., and Cano J.-C., “Evaluating how smartphone contact tracing technology can reduce the spread of infectious diseases: The case of COVID-19,” IEEE Access, vol. 8, pp. 99083–99097, 2020, doi: 10.1109/ACCESS.2020.2998042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Painuli D., Mishra D., Bhardwaj S., and Aggarwal M., “Fuzzy rule based system to predict COVID19—A deadly virus,” Int. J. Manage. Hum., vol. 4, no. 8, pp. 78–82, 2020, doi: 10.35940/ijmh.H0781.044820. [DOI] [Google Scholar]
- [33].Sami R., Soltaninejad F., Amra B., Naderi Z., Haghjooy Javanmard S., Iraj B., Haji Ahmadi S., Shayganfar A., Dehghan M., Khademi N., Hosseini N. S., Mortazavi M., Mansourian M., Mananas M. A., Marateb H. R., and Adibi P.. (2020). A One-Year Hospital-Based Prospective Covid-19 Open-Cohort in the Eastern Mediterranean Region: The Khorshid Covid Cohort (KCC) Study. [Online]. Available: https://www.medrxiv.org/content/10.1101/2020.05.11.20096727v2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Mamdani E. H. and Assilian S., “An experiment in linguistic synthesis with a fuzzy logic controller,” Int. J. Hum.-Comput. Stud., vol. 51, no. 2, pp. 135–147, Aug. 1999, doi: 10.1006/ijhc.1973.0303. [DOI] [Google Scholar]
- [35].Karaboga D. and Kaya E., “Adaptive network based fuzzy inference system (ANFIS) training approaches: A comprehensive survey,” Artif. Intell. Rev., vol. 52, no. 4, pp. 2263–2293, 2019, doi: 10.1007/s10462-017-9610-2. [DOI] [Google Scholar]
- [36].Painuli D., Mishra D., Bhardwaj S., and Aggarwal M., “Fuzzy rule based system to predict COVID19-A deadly virus,” Int. J. Manage. Humanities, vol. 3, no. 4, pp. 78–82, 2020, doi: 10.35940/ijmh.H0781.044820. [DOI] [Google Scholar]
- [37].Burges C. J. C., “A tutorial on support vector machines for pattern recognition,” Data Mining Knowl. Discovery, vol. 2, no. 2, pp. 121–167, 1998, doi: 10.1023/A:1009715923555. [DOI] [Google Scholar]
- [38].Farid D. M., Zhang L., Rahman C. M., Hossain M. A., and Strachan R., “Hybrid decision tree and naïve bayes classifiers for multi-class classification tasks,” Expert Syst. Appl., vol. 41, no. 4, pp. 1937–1946, Mar. 2014, doi: 10.1016/j.eswa.2013.08.089. [DOI] [Google Scholar]
- [39].Yoon G., Lee J. Y., Jeon K. J., Park K.-K., Yeo H. S., Hwang H. T., Kim H. S., and Hwang I.-D., “Multiple diagnosis based on photoplethysmography: Hematocrit, SpO₂, pulse, and respiration,” in Proc. Opt. Health Care Biomed. Opt., Diag. Treatment, vol. 4916, 2002, pp. 185–188, doi: 10.1117/12.482947. [DOI] [Google Scholar]
- [40].Sartini C., Tresoldi M., Scarpellini P., Tettamanti A., Carcá F., Landoni G., and Zangrillo A., “Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit,” JAMA, vol. 232, no. 22, 2020, pp. 2338–2340, doi: 10.1001/jama.2020.7861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Park C. and Lee B., “Real-time estimation of respiratory rate from a photoplethysmogram using an adaptive lattice notch filter,” BioMed. Eng. Online, vol. 13, no. 1, pp. 170–186, 2014, doi: 10.1186/1475-925X-13-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Laput G., Ahuja K., Goel M., and Harrison C., “Ubicoustics: Plug-and-play acoustic recognition,” in Proc. 31st Annu. ACM Symp. User Interface Softw. Technol., Berlin, Germany, vol. 18, 2018, pp. 213–224, doi: 10.1145/3242587.3242609. [DOI] [Google Scholar]
- [43].Matos S., Birring S. S., Pavord I. D., and Evans D. H., “Detection of cough signals in continuous audio recordings using hidden Markov models,” IEEE Trans. Biomed. Eng., vol. 53, no. 6, pp. 1078–1083, Jun. 2006, doi: 10.1109/TBME.2006.873548. [DOI] [PubMed] [Google Scholar]
- [44].Korpas J., Vrabec M., Sadlonova J., Salat D., and Debreczeni L. A., “Analysis of the cough sound frequency in adults and children with bronchial asthma,” Acta Phys. Hungarica, vol. 90, no. 1, pp. 27–34, 2003, doi: 10.1556/APhysiol.90.2003.1.4. [DOI] [PubMed] [Google Scholar]
- [45].Mackey A., Spachos P., Song L., and Plataniotis K. N., “Improving BLE beacon proximity estimation accuracy through Bayesian filtering,” IEEE Internet Things J., vol. 7, no. 4, pp. 3160–3169, Apr. 2020, doi: 10.1109/JIOT.2020.2965583. [DOI] [Google Scholar]
- [46].Al Qathrady M. and Helmy A., “Improving BLE distance estimation and classification using TX power and machine learning: A comparative analysis,” in Proc. 20th ACM Int. Conf. Model., Anal. Simul. Wireless Mobile Syst., Nov. 2017, pp. 79–83, doi: 10.1145/3127540.3127577. [DOI] [Google Scholar]
- [47].Lam C. H., Ng P. C., and She J., “Improved distance estimation with BLE beacon using Kalman filter and SVM,” in Proc. IEEE Int. Conf. Commun. (ICC), Kansas City, MO, USA, 2018, pp. 1–5, doi: 10.1109/ICC.2018.8423010. [DOI] [Google Scholar]
- [48].AltBeacon Protocol Specification v1.0. Accessed: Aug. 2, 2020. [Online]. Available: https://github.com/AltBeacon/spec
- [49].Mei X., “Artificial intelligence–enabled rapid diagnosis of patients with COVID-19,” Nature Med., vol. 26, no. 8, pp. 1224–1228, Aug. 2020, doi: 10.1038/s41591-020-0931-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Bai L., “Chinese experts’ consensus on the Internet of Things-aided diagnosis and treatment of coronavirus disease 2019 (COVID-19),” Clin. eHealth, vol. 3, pp. 7–15, 2020, doi: 10.1016/j.ceh.2020.03.001. [DOI] [Google Scholar]
- [51].Allam Z. and Jones D. S., “On the coronavirus (COVID-19) outbreak and the smart city network: Universal data sharing standards coupled with artificial intelligence (AI) to benefit urban health monitoring and management,” Healthcare, vol. 8, no. 1, p. 46, Feb. 2020, doi: 10.3390/healthcare8010046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Qiu G., Gai Z., Tao Y., Schmitt J., Kullak-Ublick G. A., and Wang J., “Dual-functional plasmonic photothermal biosensors for highly accurate severe acute respiratory syndrome coronavirus 2 detection,” ACS Nano, vol. 14, no. 5, pp. 5268–5277, May 2020, doi: 10.1021/acsnano.0c02439. [DOI] [PubMed] [Google Scholar]
- [53].Winning A.. Reference Design for Small Wearables for Social-Distancing. Accessed: Aug. 2, 2020. [Online]. Available: https://www.eenewsembedded.com/news/reference-design-small-wearables-social-distancing [Google Scholar]