Abstract
Rural-urban health disparities in life expectancy are large and increasing, with the rural-urban disparity stroke mortality serving as a potential contributor. Data from Vital Statistics (referenced through the CDC WONDER system) shows an unexplained temporal pattern in the rural-urban disparity in stroke-specific mortality, with the magnitude of the disparity increasing from 15% to 25% between 1999 and 2010, but subsequently decreasing to 8% by 2019. This recent decrease in the magnitude of the rural-urban disparity in stroke mortality appears to be driven by a previously unreported plateauing of stroke mortality in urban areas and a continued decline of stroke mortality in rural areas. There is also a need to better understand the contributors to the higher stroke mortality in rural areas; however, a general lack of temporal data implies that this can only be examined cross-sectionally. A higher stroke incidence in rural areas appears to be a contributor to the higher rural stroke mortality, and there is clear evidence of a higher prevalence of stroke risk factors in rural areas potentially contributing to this higher incidence. Conversely, studies of rural-urban disparities in stroke case fatality show smaller and inconsistent associations. To the extent that disparities in case fatality do exist, there are many studies showing rural-urban disparities in stroke care could be contributing. While these data offer insights to the overall rural-urban disparities in stroke mortality, additional data are needed to help understand temporal changes in the magnitude of the rural-urban stroke mortality disparity.
Keywords: stroke, rural, urban, mortality, incidence, case fatality, review
Introduction
A rural-urban disparity in the United States in life expectancy has been long recognized, and these mortality disparities appear to be increasing. In 1969–1971, life expectancy was 0.4 years longer in metropolitan areas relative to non-metropolitan areas, a difference that increased to 2.0 years by 2005–2009,1 and then to over 3 years by 2014.2 These increases arise from larger gains in life expectancy in the metropolitan areas relative to non-metropolitan areas.1 The rural-urban difference in life expectancy is reflected in the temporal changes in the rural-urban differences in all-cause mortality calculated from Vital Statistics data available from the CDC WONDER3 system (Figure 1A and Supplemental Table 1), where increasing rural-urban risk differences are shown by the National Center for Health Statistics (NCHS) Urban-Rural Classification for Counties (see definitions in Supplemental Table 2) to extend beyond the 2005–2009 period through 2019. Specifically, in 1999, all-cause mortality was 880.4/100,000 in the most urban counties compared to 933.4/100,000 in the most rural counties, a 53.0/100,000 difference or a 6% ((933.4 – 880.4)/880.4 = 0.06) higher rate in rural areas (Figure 1B). The temporal decline in mortality was substantially greater in urban than rural counties (Figure 1A), where by 2019 the most-urban all-cause mortality rate had fallen to 658.1/100,000 compared to a rate 842.2/100,000 in the most rural counties. This resulted in an increase in the absolute difference in rural-urban all-cause mortality to 184.1/100,000, with the relative difference increasing to 28%. Hence, while mortality is decreasing in counties across the entire rural-urban spectrum, the magnitude of rural-urban disparity in the most objective health outcome is increasing.
Figure 1:
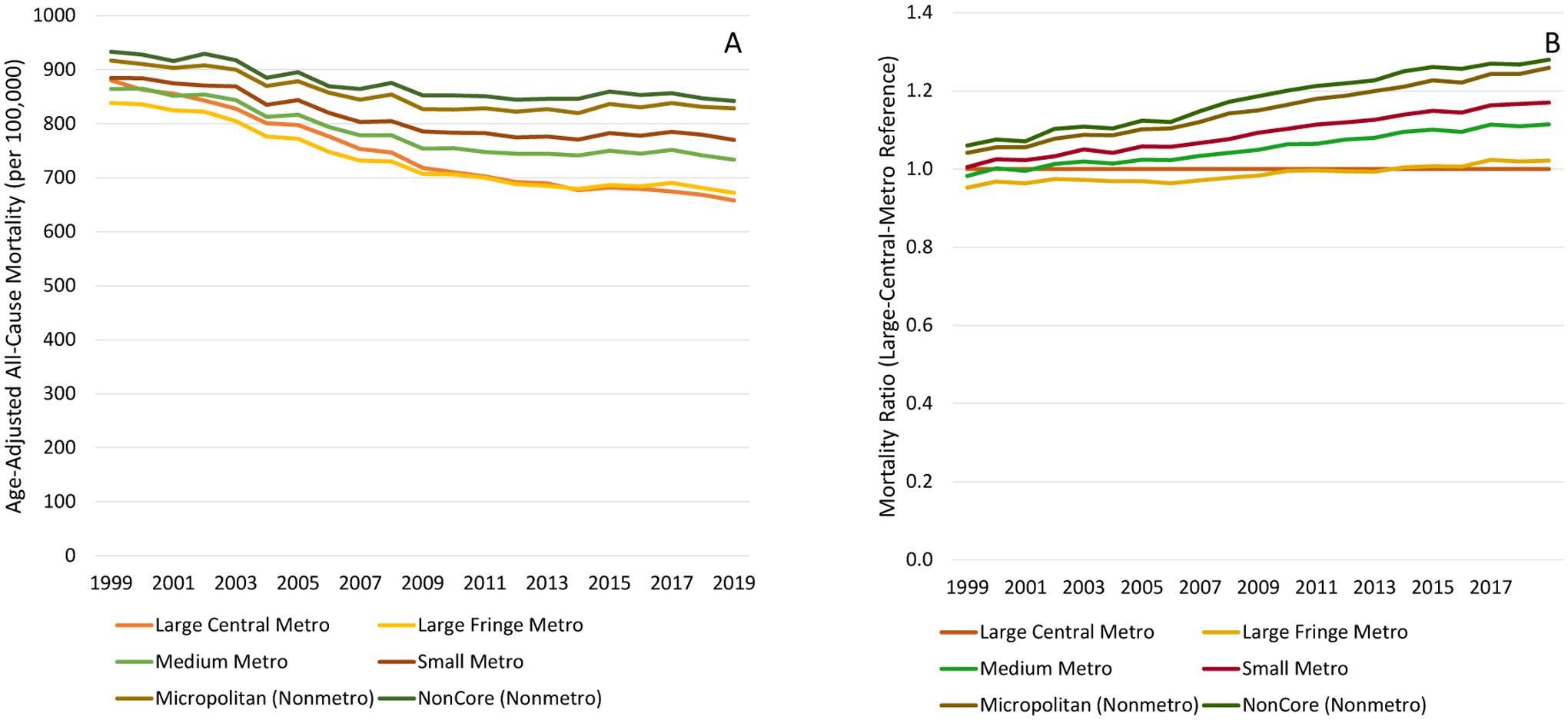
Temporal changes in age-adjusted all-cause mortality for all ages between 1999 and 2019 shown by 2013 NCHS Urban-Rural Classification Scheme (panel A), and mortality ratio relative to residents of in large-central-metro counties (panel B). Source CDC WONDER.
In response to these substantial disparities in life expectancy and mortality, and in compliance with Public Law 106–525 (Minority Health and Health Disparities Research and Education Act) in 2000,4 the National Institutes of Health (NIH) has included a focus on rural disparities as one of the three target populations for heath disparities research (along with racial/ethnic minorities and those with low socioeconomic status - SES).5 These same rural-urban disparities motivated a “Call to Action” by the American Heart Association in 2020 to develop active interventions to reduce rural-urban disparities.6
With stroke as a major contributor to death and disability, one would presume there to be a rich literature describing descriptions of the magnitude of the rural-urban disparity in: 1) stroke mortality, 2) the relative contribution of disparities in stroke incidence versus stroke case-fatality as the underlying contributor to rural-urban disparities in mortality, and 3) factors that are the primary contributors to any observed disparities in either stroke incidence or case-fatality. Herein we review a surprisingly sparse and relatively weak literature on the contributors to the rural-urban disparity in the burden of stroke.
Rural-Urban Differences in Stroke Mortality
In 2013, we reported temporal changes in age-adjusted stroke mortality rates between 1999 and 2010 (again, from US Vital Statistics available from CDC WONDER3), noting that while stroke mortality is decreasing across the spectrum of rurality, there was an alarming increase in magnitude of the relative rural-urban disparity on stroke-specific mortality that increased from 15% (189.7/164.3 = 1.15) in 1999 to 25% (126.9/101.8 = 1.26) in 2010.7 This report proved to be at an inflection point in the temporal change in mortality, where in this updated analysis shows that after 2010 the magnitude of the rural-urban disparity has decreased from 25% to 8% (108.0/100.2 = 1.08) between 2010 and 2019 (age-adjusted rates in Figure 2A and Supplemental Table 3, with mortality ratios provided in Figure 2B). This decrease appears to be driven by a plateauing of stroke mortality in urban areas, but a continued decline in stroke mortality in rural areas (Figure 2A). Specifically, in large urban metro counties, stroke mortality declined from 101.8/100,000 in 2010, to a low of 94.6/100,000 in 2013, but has subsequently rebounded to 100.2/100,000 in 2019. In contrast, stroke mortality in non-core regions has nearly monotonically declined from 126.9/100,000 in 2010, to 108.0/100,000 in 2019. An overall national trend for potentially increasing stroke mortality has been previously noted, along with documentation of a substantial heterogeneity in county-level changes in stroke mortality.8 However, to our knowledge, this is the first report noting that the heterogeneity between counties may be associated with rurality, with the recent increasing stroke mortality apparently concentrated in urban areas, but with a continued decline in more rural regions.
Figure 2:
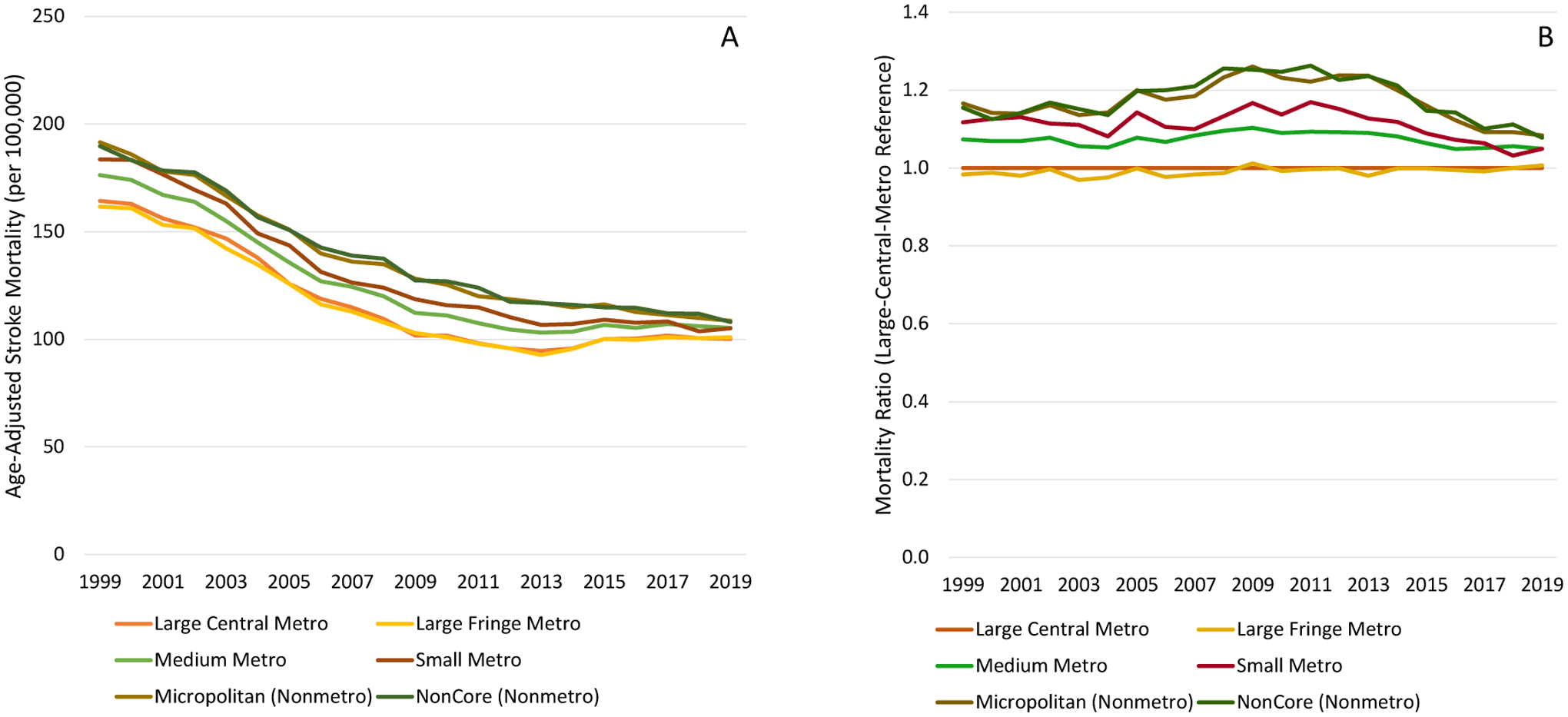
Temporal changes in age-adjusted stroke mortality (ICD-10 I60 to I69) for ages 45 and over between 1999 and 2019, shown by the 2013 NCHS Urban-Rural Classification Scheme (panel C), and mortality ratio relative to residents of in large-central-metro counties (panel D). Source CDC WONDER.
Potential Contributors to the Overall Urban-Rural Differences in Stroke Mortality
Unfortunately (as will be subsequently discussed), there are not data that can contribute directly to the understanding of the temporal changes in stroke mortality, and as such the remainder of the report will focus on factor contributing to the overall rural-urban disparity in stroke. Mortality from a disease can be higher for a subgroup (such as rural residents relative to urban residents) because of higher incidence (more people in the subgroup are having the disease) or because of a higher case-fatality (more people in the subgroup who have the disease are dying), or both. The implications of which pathway is the major contributor is immense. If the higher mortality in the subgroup is attributable to a higher incidence, then the primary effort to reduce disparity should focus on population or community interventions to reduce the excess risk of disease development in the higher risk group. Alternatively, if the higher morality in the subgroup is attributable to a higher case-fatality in the subgroup, then the primary effort to reduce the disparity should focus on acute and hospital-post-stroke care to improve the outcome of those with the disease.
In this section we review the evidence for rural-urban disparities in stroke incidence, and then a review the rural-urban disparities in risk factors potentially contributing to the potential disparities in incidence. This is followed by a review of the evidence for rural-urban differences in stroke case fatality, followed by the evidence for rural-urban disparities in stroke care contributing to the potential case-fatality differences.
Rural-Urban Disparities in Stroke Incidence
The status of the literature describing urban-rural differences in stroke incidence is not strong. While reports on urban-rural disparities in stroke prevalence had been published,9 as recently as 8 years ago (specifically at the time of our 2013 report7) there were no reports describing urban-rural differences in stroke incidence. This relative dearth of reports on the disparity in incidence is potentially attributable to the majority of research being conducted at tertiary medical centers located in urban areas, and to the relatively smaller population size in rural areas where reliable estimation of incidence from longitudinal observational studies requires a substantial sample size. To our knowledge, since 2013 there have been only three reports describing rural-urban disparities in stroke incidence: one in the US, Canada and France.
In the US, the REasons for Geographic And Racial Differences in Stroke (REGARDS), a longitudinal population-based cohort study, study assessed rural-urban differences in stroke incidence using the Rural-Urban Commuting Areas (RUCA) classifications (for definitions see Supplemental Table 3). Relative to participants who were stroke-free at baseline and who were from urban areas (n = 18,705), the hazard for those in large rural cities or town (n = 2,645) was 1.23-times higher (95% CI: 1.01 – 1.51), while those from small rural cities and towns or from isolated areas (n = 1,930) had a hazard 1.30-times higher (95% CI: 1.03 – 1.62).10 Adjustment for traditional stroke risk factors modestly mediated these associations (1.21; 95% CI: 0.99 – 1.48 and 1.26; 95% CI: 1.01 – 1.58, respectively), and further adjustment for socioeconomic factors additionally attenuated the associations (1.18; 95% CI: 0.96 – 1.44 and 1.19; 95% CI: 0.95 – 1.50), suggesting that some, but not all, of the higher stroke incidence in rural areas may be attributable a more detrimental risk factor and SES profile in rural areas.10
Administrative data from the Cardiovascular Health in Ambulatory Care Research Team (CANHEART) Study were used to describe rural-urban stroke incidence disparities in Ontario (Canada), where residents were classified as rural if they were not in a commuting area of a metropolitan area and resided in a community of less than 10,000 persons. Among stroke-free persons at baseline, the hazard for incident stroke was 1.11-times higher (95% CI: 1.04 – 1.09) in persons from rural areas than for those from more urban areas. This difference was substantially mediated to 1.06-times higher (95% CI: 1.04 – 1.09) by adjustment for stroke risk factors, again suggesting that differences in risk factors could be a contributor to the higher stroke incidence in rural areas.11
Urban areas in France were defined as towns of 2,000+ persons where no building was more than 200 meters from its nearest neighbor. With this somewhat more “liberal” definition of an urban area, age-adjusted stroke incidence was higher with rurality in men, but was lower in women. The paper provided no adjustment for rural-urban differences in the prevalence of risk factor.12
Hence, to our knowledge, there is one US longitudinal cohort study,10 and one Canadian study using administrative data,11 showing higher stroke incidence in rural relative to urban areas. In addition, there is one French study using a rather “low bar” criteria to define urban areas that found an association with higher risk in rural areas for men (but not for women).12 In both of the North American studies, adjustment for traditional stroke risk factors modestly or substantially attenuated the association of stroke risk and rurality suggesting that the disparities are partially (but not completely) attributable to a higher prevalence of stroke risk factors in rural areas.
Rural-Urban Disparities in Stroke Risk Factors
In contrast to the sparse literature describing rural-urban differences in stroke incidence, there are more reports documenting an adverse stroke risk factor profile among residents of rural areas. For brevity, we will focus on hypertension, diabetes and smoking, the factors with the largest population attributable risk for incident stroke;13 a secondary focus will be on indices of SES and other “non-traditional” risk factors.
Numerous studies have shown a higher prevalence hypertension among residents of rural areas. The REGARDS Study has documented a higher prevalence of hypertension in more rural areas using defined both by county-level NCHS classification of rurality,14 and by Census Tracts using the RUCA classification.10 Specifically, for the NCHS classification and relative to residents of large central metro counties, after adjustment for age, race, sex, state and neighborhood SES levels the prevalence of hypertension is monotonically higher from the most urban to the most rural non-core areas, where the odds of hypertension is 1.25-times higher (95% CI: 1.11 – 1.42).14 Using the RUCA Census tract definition and relative to residents of an Urban tract, the odds of hypertension were 1.23-times higher (95% CI: 1.13 – 1.34) for rural large cities or towns, and 1.25-times higher (95% CI: 1.13 – 1.38) in small rural cities or isolated areas.10 The National Health and Nutrition Examination Survey (NHANES) showed a higher prevalence of hypertension in rural whites (28.5%) and blacks (36.0%) than in urban regions (23.3% and 28.8% respectively).15 Although based on self-reported hypertension, the National Health Interview Survey (NHIS) has reported that 29.0% of rural residents are hypertensive, compared to 26.1% in suburban and 22.8% in urban areas.16
REGARDS has also reported a higher prevalence of diabetes in rural regions, where: 1) on the NCHS classification the prevalence increased with rurality (ptrend = 0.003) with those in non-core counties having an odds of diabetes 1.15-times higher (95% CI: 0.99–1.33) than those in the large central metro counties,14 and 2) using the RUCA classification, those in small rural towns or isolated regions had an adjusted odds ratio 1.26-times higher (95% CI: 1.12 – 1.42) than in urban Census tracts.10 NHANES has also shown a higher prevalence of diabetes in rural whites (6.5%) and blacks (9.5%) than for those in urban areas (4.5% and 6.0%, respectively).15 Although self-reported, the Behavioral Risk Factor Surveillance System (BRFSS) has also reported a higher prevalence of diabetes in rural (9.9%) compared to urban (9.0%) areas.17
Unlike hypertension and diabetes where direct blood pressure and glucose assessments adds confidence, prevalence of smoking is more dependent on self-report. With this, the large sample size of BRFSS increases the importance of estimates from this source, where the prevalence of smoking increased monotonically across the NCHS categories of rurality from 16.1% in the large metro centers to 25.1% in the non-core regions.18
It is tempting to “look under the streetlamp” to find the contributors to the higher stroke incidence in rural areas, and clearly rural-urban differences in stroke risk factors seem to be the most obvious contributor. However, it is also important to have a broad view of potential contributors to the higher rural stroke incidence, and this reveals a wide spectrum of other factors known to be related to the risk of incident stroke where rural residents are at a disadvantage. As detailed in the AHA Call to Action: Rural Health,6 relative to urban residents, rural residents have lower socioeconomic status, with concomitant lower median income (median income $10,000 less than urban areas), with a lower tax base for local governments, lower educational achievement, greater transportation challenges, and greater food insecurity. Rural residents have more adverse levels of psychosocial factors known to be related to incident stroke risk, for example the 1999 NHIS showed age-race-sex adjusted prevalence of depression is 1.19-times higher (95% CI: 1.03 – 1.38) for rural than urban participants.19 There are also structural factors working to the disadvantage of rural residents. For example, among employed individuals, differences in the type of employer is associated with access to health insurance, with 68% of employed urban residents having health insurance compared to only 57% of those living in small rural counties not adjacent to urban centers.20 Additionally, there are rural-urban differences in exposure to environmental contaminates. For example, not only are rural residents more reliant on the less-processed well water, but also 10.0% of water systems in non-core regions have concentrations of contaminates greater than the maximum allowable level, compared to 5.4% of water systems in large central metro areas.21 Each of these factors (depression, access to care, and environmental contaminative exposures) are well-recognized risk factors for stroke,22 and are offered as examples of the the broad array of factors potentially contributing to higher stroke risk in rural areas. In summary, not only must we consider the disparities in traditional stroke risk factors as potential drivers of the higher stroke incidence in rural areas, but we also need to keep an open mind to the wide range of other exposure differences for rural residents.
Rural-Urban Disparities in Stroke Case Fatality
The reports on rural-urban disparities in case fatality following stroke show an inconsistent relationship with rurality, and with potentially smaller than rural-urban differences than for stroke incidence. In the REGARDS study, there was a non-significant and inconsistent pattern across the RUCA classifications, with an odds of death within 30-days of a stroke 1.22-times higher (95% CI: 0.70 – 2.15) for those in a large rural city/town relative to those in an urban area, but with the odds 0.73-times smaller (95% CI: 0.36 – 1.48) in small rural towns or isolated areas.10 Adjustment for traditional stroke risk factors and indices of SES had little impact on these estimates.10 Based on administrative data, the rural-urban differences in 30-day case fatality in Ontario (CA) were also not significantly associated with rurality, with death in 9.2% of those from a large urban area, 9.4% in those from a medium urban area, and 9.4% for those from a rural area. There were also no differences in death or disability at discharge with 42.3%, 42.1% and 39.8%, respectively.23 However, data from the National Inpatient Sample did show an association between rurality and in-hospital mortality, where relative to those in an urban area, the odds of death in the hospital increased nearly monotonically across the NHCS classifications to be 1.21-times higher (95% CI: 1.15 – 1.27) in rural areas.24 This finding is somewhat offset by the observation of lower 30-day case fatality in French residents of rural areas (relative risk = 0.76; 95% CI: 0.60 – 0.96) compared to those from the town centers.12
Rural-Urban Differences in Stroke Care
There is a richer literature documenting a lower level of stroke care for patients from rural areas. A 2019 systematic review of 28 studies concluded there is “convincing, albeit not unanimous, evidence to suggest that stroke patients in rural areas receive less acute care than their urban counterparts.”25 After adjustment for demographic factors, among strokes occurring in the REGARDS study, those living in a rural area (defined as being in a Census tract that is < 75% urban by the US Census Bureau) were substantially less likely to be evaluated at a primary stroke center (aOR = 0.39; 95% CI: 0.22 – 0.67).26 These rural-urban differences in treatment at primary stroke centers is likely a product of access, where 70% of urban US citizens are within a 30-minute drive time to a center, while only 26% of rural residents are within this travel time.27 However, differences in the relationship of rurality with case fatality could also be attributable to differences in the type of person with access, where the populations without access to a primary stroke center (defined as within a 60-minute drive) have a lower median household income ($43,250 vs. $52,436), a higher proportion living in poverty (8.0% vs. 5.6%), a higher proportion of those over 25 without a high school degree (14.6% vs. 11.8%).28 Using administrative data, relative to urban Ontario residents, rural residents of Ontario were less like to receive stroke unit care (36% vs. 51%), less likely to have a neurology consult (36% vs. 65%), and less likely to have carotid imaging (62% vs. 73%).23 There are also substantial rural-urban differences in acute stroke care, where in the National Inpatient Sample and relative to urban residents, rural residents had dramatically lower use of both intravenous thrombolysis therapy (adjusted odds ratio = 0.55; 95% CI: 0.51 – 0.59) and endovascular therapy (aOR = 0.64; 95% CI: 0.57 – 0.73)24
Discussion and Conclusions
It appears that rural-urban disparities in stroke incidence is a likely contributor to the observed rural-urban disparities in stroke mortality, and that a higher prevalence of major stroke risk factors in rural areas could also be contributing to this higher stroke incidence. The risk factors that are more prevalent in rural areas offer a promising target for interventions to reduce the disparity in stroke incidence (and subsequently stroke mortality) in rural areas. Importantly, individuals with even well-managed stroke risk factors are at higher stroke risk. For example individuals with prevalent hypertension with systolic blood pressure controlled to below 120 mmHg are at a 60% increased stroke risk relative to those below 120 mmHg without medications.29 As such, the efforts to reduce stroke risk must not only focus on primary risk factor control among rural residents with prevalent risk factors, but also on primordial risk factor prevention of risk factors themselves, i.e., preventing the development of risk factors for people living in rural areas.
While it seems clear that there are substantial rural-urban disparities in stroke care, the evidence is mixed as to whether these disparities in care translate to rural-urban disparities in stroke case fatality. There are many ethical and moral reasons to reduce the disparity in stroke care, and this should also be a priority; however, it is less clear that success in reducing rural-urban disparities in care will reduce the rural-urban disparity in stroke mortality.
It remains a mystery why the relative rural-urban stroke mortality disparity increased between 1999 and 2010, and then subsequently decreased over the period up to 2019. A hint to understanding this is offered by the observation that it seems to be a product of the stagnation of the stroke mortality decline in urban areas, where the decline in stroke mortality has continued to decline in more rural areas. At this point, suggestions of factors that would contribute to this differential pattern would be only speculation; however, the stroke burden could be lessened by investigations of factors that would differentially slow the decline in mortality in more urban areas. There are currently few studies examining rural-urban disparities in incidence and only marginally more examining rural-urban disparities in case fatality. Understanding these temporal changes in the rural-urban stroke mortality disparity will require substantially more complex studies that would permit the assessment of temporal changes in the rural-urban disparity in both incidence and case fatality, where adding the new dimension of time to an already challenging investigation will be complex.
Supplementary Material
There is a persistent rural-urban disparity in stroke mortality that increased between 1999 to 2010, then decreased to 2018
A higher stroke incidence in rural areas seems a likely contributor to the rural-urban stroke mortality disparity
A higher prevalence of stroke risk factors in rural areas is likely contributing to the higher incidence in the regions
Inconsistent rural-urban disparities in stroke case-fatality likely contribute less to rural-urban stroke disparity
However, to the extent that case-fatality could be contributing, rural health care delivery lags that in urban areas
Funding
This development of this manuscript was supported by cooperative agreement U01-NS041588 from the National Institute of Neurological Disorders and Stroke, NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
George Howard is one of the principal investigators of the REasons for Geographic and Racial Differences in Stroke (REGARDS) study
References
- 1.Singh GK, Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969–2009. Am J Prev Med. 2014;46(2):e19–29. [DOI] [PubMed] [Google Scholar]
- 2.Singh GK, Daus GP, Allender M, et al. Social Determinants of Health in the United States: Addressing Major Health Inequality Trends for the Nation, 1935–2016. Int J MCH AIDS. 2017;6(2):139–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Underlying cause of death file: 1999–2019. CDC WONDER Online Database, compiled from Underlying Cause of Death Mortality File 1968–2019. Centers for Disease Control and Prevention. Accessed January 21, 2021. https://wonder.cdc.gov/Deaths-by-Underlying-Cause.html. Accessed. [Google Scholar]
- 4.S. 1880 -- 106th Congress: Minority Health and Health Disparities Research and Education Act of 2000. In: 106th Congress -, ed. Vol 106–5252000:2498. [Google Scholar]
- 5.Dankwa-Mullan I, Rhee KB, Williams K, et al. The science of eliminating health disparities: summary and analysis of the NIH summit recommendations. American journal of public health. 2010;100 Suppl 1:S12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harrington RA, Califf RM, Balamurugan A, et al. Call to Action: Rural Health: A Presidential Advisory From the American Heart Association and American Stroke Association. Circulation. 2020;141(10):e615–e644. [DOI] [PubMed] [Google Scholar]
- 7.Howard G Ancel Keys Lecture: Adventures (and Misadventures) in Understanding (and Reducing) Disparities in Stroke Mortality. Stroke; a journal of cerebral circulation. 2013;44(11):3254–3259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall EW, Vaughan AS, Ritchey MD, Schieb L, Casper M. Stagnating National Declines in Stroke Mortality Mask Widespread County-Level Increases, 2010–2016. Stroke; a journal of cerebral circulation. 2019;50(12):3355–3359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adams PF, Hendershot GE, Marano MA, Centers for Disease C, Prevention/National Center for Health S. Current estimates from the National Health Interview Survey, 1996. Vital and health statistics Series 10, Data from the National Health Survey. 1999(200):1–203. [PubMed] [Google Scholar]
- 10.Howard G, Kleindorfer DO, Cushman M, et al. Contributors to the Excess Stroke Mortality in Rural Areas in the United States. Stroke; a journal of cerebral circulation. 2017;48(7):1773–1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kapral MK, Austin PC, Jeyakumar G, et al. Rural-Urban Differences in Stroke Risk Factors, Incidence, and Mortality in People With and Without Prior Stroke. Circulation Cardiovascular quality and outcomes. 2019;12(2):e004973. [DOI] [PubMed] [Google Scholar]
- 12.Grimaud O, Lachkhem Y, Gao F, et al. Stroke Incidence and Case Fatality According to Rural or Urban Residence: Results From the French Brest Stroke Registry. Stroke; a journal of cerebral circulation. 2019;50(10):2661–2667. [DOI] [PubMed] [Google Scholar]
- 13.Ohira T, Shahar E, Chambless LE, Rosamond WD, Mosley TH Jr., Folsom AR. Risk factors for ischemic stroke subtypes: the Atherosclerosis Risk in Communities study. Stroke; a journal of cerebral circulation. 2006;37(10):2493–2498. [DOI] [PubMed] [Google Scholar]
- 14.Kamin-Mukaz D, Dawson E, Howard VJ, et al. Rural/Urban differences in the prevalence of stroke risk factors. Journal of Rural Health. 2021;(in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mainous AG 3rd, King DE, Garr DR, Pearson WS. Race, rural residence, and control of diabetes and hypertension. Annals of family medicine. 2004;2(6):563–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Summary Health Statistics: National Health Interview Survey, 2018. In. Rockville, MD: Centers for Disease Control and Prevention, National Center for Health Statistics; 2018. [Google Scholar]
- 17.O’Connor A, Wellenius G. Rural-urban disparities in the prevalence of diabetes and coronary heart disease. Public health. 2012;126(10):813–820. [DOI] [PubMed] [Google Scholar]
- 18.Matthews KA, Croft JB, Liu Y, et al. Health-Related Behaviors by Urban-Rural County Classification - United States, 2013. Morbidity and mortality weekly report Surveillance summaries. 2017;66(5):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Probst JC, Laditka SB, Moore CG, Harun N, Powell MP, Baxley EG. Rural-urban differences in depression prevalence: implications for family medicine. Fam Med. 2006;38(9):653–660. [PubMed] [Google Scholar]
- 20.Larson SL, Hill SC. Rural-urban differences in employment-related health insurance. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association. 2005;21(1):21–30. [DOI] [PubMed] [Google Scholar]
- 21.Strosnider H, Kennedy C, Monti M, Yip F. Rural and Urban Differences in Air Quality, 2008–2012, and Community Drinking Water Quality, 2010–2015 - United States. Morbidity and mortality weekly report Surveillance summaries. 2017;66(13):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meschia JF, Bushnell C, Boden-Albala B, et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke; a journal of cerebral circulation. 2014;45(12):3754–3832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koifman J, Hall R, Li S, et al. The association between rural residence and stroke care and outcomes. J Neurol Sci. 2016;363:16–20. [DOI] [PubMed] [Google Scholar]
- 24.Hammond G, Luke AA, Elson L, Towfighi A, Joynt Maddox KE. Urban-Rural Inequities in Acute Stroke Care and In-Hospital Mortality. Stroke; a journal of cerebral circulation. 2020;51(7):2131–2138. [DOI] [PubMed] [Google Scholar]
- 25.Dwyer M, Rehman S, Ottavi T, et al. Urban-rural differences in the care and outcomes of acute stroke patients: Systematic review. J Neurol Sci. 2019;397:63–74. [DOI] [PubMed] [Google Scholar]
- 26.Mullen MT, Judd S, Howard VJ, et al. Disparities in evaluation at certified primary stroke centers: reasons for geographic and racial differences in stroke. Stroke; a journal of cerebral circulation. 2013;44(7):1930–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khan JA, Casper M, Asimos AW, et al. Geographic and sociodemographic disparities in drive times to Joint Commission-certified primary stroke centers in North Carolina, South Carolina, and Georgia. Preventing chronic disease. 2011;8(4):A79. [PMC free article] [PubMed] [Google Scholar]
- 28.Mullen MT, Wiebe DJ, Bowman A, et al. Disparities in accessibility of certified primary stroke centers. Stroke; a journal of cerebral circulation. 2014;45(11):3381–3388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Howard G, Banach M, Cushman M, et al. Is blood pressure control for stroke prevention the correct goal? The lost opportunity of preventing hypertension. Stroke; a journal of cerebral circulation. 2015;46(6):1595–1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


