Abstract
Background
Patients affected by poverty-related infectious diseases (PRDs) are disproportionally affected by malnutrition. To optimize treatment of patients affected by PRDs, we aimed to assess the influence of malnutrition associated with PRDs on drug pharmacokinetics, by way of a systematic review.
Methods
A systematic review was performed on the effects of malnourishment on the pharmacokinetics of drugs to treat PRDs, including HIV, tuberculosis, malaria, and neglected tropical diseases.
Results
In 21/29 PRD drugs included in this review, pharmacokinetics were affected by malnutrition. Effects were heterogeneous, but trends were observed for specific classes of drugs and different types and degrees of malnutrition. Bioavailability of lumefantrine, sulfadoxine, pyrimethamine, lopinavir, and efavirenz was decreased in severely malnourished patients, but increased for the P-glycoprotein substrates abacavir, saquinavir, nevirapine, and ivermectin. Distribution volume was decreased for the lipophilic drugs isoniazid, chloroquine, and nevirapine, and the α1-acid glycoprotein-bound drugs quinine, rifabutin, and saquinavir. Distribution volume was increased for the hydrophilic drug streptomycin and the albumin-bound drugs rifampicin, lopinavir, and efavirenz. Drug elimination was decreased for isoniazid, chloroquine, quinine, zidovudine, saquinavir, and streptomycin, but increased for the albumin-bound drugs quinine, chloroquine, rifampicin, lopinavir, efavirenz, and ethambutol. Clinically relevant effects were mainly observed in severely malnourished and kwashiorkor patients.
Conclusions
Malnutrition-related effects on pharmacokinetics potentially affect treatment response, particularly for severe malnutrition or kwashiorkor. However, pharmacokinetic knowledge is lacking for specific populations, especially patients with neglected tropical diseases and severe malnutrition. To optimize treatment in these neglected subpopulations, adequate pharmacokinetic studies are needed, including severely malnourished or kwashiorkor patients.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40262-021-01031-z.
Key Points
| Malnutrition leads to physiological alterations that affect drug pharmacokinetics. |
| Patients affected by poverty-related diseases are a highly vulnerable population, requiring optimal and individualized drug treatment. |
| This systematic review highlights the key findings of pharmacokinetic drug alterations by malnutrition, for specific drug classes and patient populations. |
| This overview can be used as a basis to predict the effects of malnutrition on the drug pharmacokinetics of poverty-related infectious diseases. |
Introduction
Malnutrition, defined here as lack of protein and/or calorie intake, is a major public health problem, especially in low-income countries where malnutrition is associated with about 50% of the 10.8 million deaths per year in children under 5 years of age [1–4]. Because of poor hygienic conditions and a lack of access to healthcare, a large proportion of this population is affected by poverty-related infectious diseases (PRDs), including HIV, tuberculosis (TB), malaria, and neglected tropical diseases (NTDs) as defined by the World Health Organization (WHO) [5]. To illustrate, 42% of African children [6] and 43% of Ethiopian adults [7] with HIV were affected by malnutrition. Similarly, 57% of Ethiopian TB patients [8] and 75% of Sudanese children affected by malaria [9] were malnourished. The association between malnutrition and PRDs is bidirectional, where on the one hand malnutrition increases the susceptibility to infections as a result of secondary immune deficiency, and on the other hand, infections can add to the development of malnutrition because of the increased need for anabolic energy by the prolonged activated immune system, and because of complications such as chronic diarrhoea, cachexia, and anaemia [10–12]. An association between NTDs and underweight was found in African children under 5 years of age [13], and, similarly, a negative correlation between malaria parasite density and malnutrition was found in Cameroonian children [14].
Malnutrition can manifest in various forms, depending on the type and severity of protein and calorie deficiency. Kwashiorkor is predominantly characterized by protein deficiency and comes with different clinical signs, including oedema, fatty liver, and anaemia. Marasmus reflects an overall deficiency of energy, mainly characterized by muscular wasting and loss of subcutaneous fat. Although there is still no consensus about the clinical definition of these phenotypes, the differences in biological features have been well described [15]. In children, stunting is usually a result of long-term nutritional deprivation, causing gut mucosal changes and altered levels of drug-metabolizing enzymes, whereas wasting is an acute condition, characterized by insufficient food intake or a high incidence of infectious diseases, and is associated with not only fatty liver but also impaired functioning of the immune system [16, 17].
The different pathophysiological conditions in malnutrition can alter the pharmacokinetics of drugs. Gastrointestinal changes include hypochlorhydria, delayed gastrointestinal emptying time, increased or decreased intestinal transit time, gastric and mucosal atrophy and dysfunction, gastrointestinal inflammation, and pancreatic insufficiency [18–20]. Moreover, in the enterocytes, P-glycoprotein activity is decreased and tight junctions are enlarged, influencing the uptake of nutrients and drugs [21]. Total body water is increased, and adipose mass and lean body mass is reduced, especially in children with marasmus and marasmic-kwashiorkor [20], and kwashiorkor is associated with the presence of oedema [22]. Furthermore, hypoproteinaemia is a common feature of malnutrition [20]. Hypoalbuminaemia is more severe in kwashiorkor than marasmus, and is associated with malnutrition combined with infectious or non-infectious inflammation, likely caused by the increased capillary permeability in inflammation, and a higher albumin degradation rate in the liver [23]. The synthesis of acute-phase proteins such as α1-acid glycoprotein is often increased in malnutrition, although this is related to the inflammation caused by infections, which often accompanies malnutrition [24–26]. In the liver, the basal metabolic rate is reduced with impaired synthesis of protein, and fat accumulation occurs, particularly in kwashiorkor [19]. In severe protein energy malnutrition or kwashiorkor, glomerular filtration rate (GFR) and renal blood flow are diminished, particularly in the presence of dehydration [20], and tubular excretion and reabsorption may be impaired [18]. These physiological alterations can alter the pharmacokinetics of drugs in different ways, which can lead to either reduced treatment efficacy in case of subtherapeutic drug levels, or toxicity in case of overdosing.
An understanding of the effect of different types of malnutrition on pharmacokinetic processes is needed to characterize drug exposure in all patients affected by PRDs, and to improve treatment and dosing guidelines in this vulnerable population. A previous general review found heterogeneous effects of protein-energy malnutrition (PEM) on pharmacokinetics in children and concluded that studies should take into account the differential effects of different forms of malnutrition on drug pharmacokinetics [27]. To provide a complete and systematic overview of the influence of malnutrition on PRD drug pharmacokinetics, we performed a systematic review of published literature on this topic. We aimed to characterize the effects of different types of malnutrition on different pharmacokinetic processes, and if mentioned by the included studies, the potential clinical relevance and whether dose recommendations are necessary for malnourished PRD patients. Furthermore we aimed to identify gaps of knowledge in specific populations.
Methods
Search Strategy
A systematic literature review was performed by a medical information specialist, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [28]. A full literature search was performed on 19 October 2020 in the MEDLINE (PubMed), Embase (OVID), and SCOPUS databases. Publications were searched on a combination of three following free-text words and related standardized keywords (Medical Subject Heading [MeSH] and Emtree terms): malnutrition, PRDs, and pharmacokinetics. Malnutrition is defined as PEM, including kwashiorkor and marasmus. PRDs include HIV, TB, malaria, and NTDs, as defined by the WHO [5]. NTDs include Buruli ulcer, Chagas disease, Dengue and Chikungunya, Dracunculiasis (guinea-worm disease), Echinococcosis, Foodborne trematodiases, Human African trypanosomiasis (sleeping sickness), Leishmaniasis, Leprosy (Hansen’s disease), Lymphatic filariasis, Mycetoma, chromoblastomycosis and other deep mycoses, Onchocerciasis (river blindness), Rabies, Scabies and other ectoparasites, Schistosomiasis, Soil-transmitted helminthiases, Snakebite envenoming, Taeniasis/Cysticercosis, Trachoma, Yaws (Endemic treponematoses), and Zika. Pharmacokinetics include any parameters describing drug exposure, bioavailability, absorption, distribution, protein binding, clearance, or elimination half-life. No limits were applied for date, study design or language. The full search strategy is shown in Table S1 in the electronic supplementary material. Duplicate articles were removed according to the method of Bramer et al. [29].
Study Selection
Studies were screened and included by two independent reviewers (LV and TD) through each phase of the review. Rayyan QCRI [30] was used to screen references on title and abstract. Studies were included when the studied population included malnourished patients at risk for or affected by one or more PRDs, as well as nonmalnourished patients or healthy volunteers. Although the scope of this review was to compare pharmacokinetics between malnourished and well-nourished infected patients, studies including non-infected patients or healthy individuals as controls were also included due to the overall scarcity of studies with infected patients as controls. Second, studies were included when the pharmacokinetics of drugs intended to treat PRDs in both populations was reported. Studies were excluded when one or more of these criteria were not met. Other exclusion criteria were missing abstract or full-text, nonclinical research, and wrong publication type (i.e. case reports, reviews, or any article not reporting original research). The reviewers resolved discrepancies by consensus. Secondary sources were identified through the reference lists of the included studies.
Data Extraction
Information from the included studies was extracted and summarized, including PRDs, PRD drugs used for pharmacokinetic analysis, route of administration of these drugs, number of patients, type of malnourished patients, classification of malnutrition as defined by the original study, definition of the control group, patient age range, and country. The methodology of pharmacokinetic analysis was reported, including (1) noncompartmental analysis when concentration time points were compared, maximum concentration (Cmax) and time to reach Cmax (Tmax) were derived by visual inspection of the data, area under the curve (AUC) was calculated by the trapezoidal rule, and/or half-life (T½) was derived by linear regression of the last data points; and (2) compartmental analysis, including a standard two-stage approach or population approach. Collected pharmacokinetic parameters for exposure included AUC, concentration on different time points after treatment (Ct), Cmax, and trough concentration (Ctrough); drug absorption was characterized by bioavailability; drug absorption rate was characterized by Tmax, absorption rate constant, and absorption lag time; drug distribution was characterized by apparent central or peripheral volume of distribution and apparent intercompartmental clearance; drug clearance was characterized by apparent clearance, elimination half-life, and elimination rate constant; drug metabolism was characterized by drug/metabolite ratio; and protein binding was characterized by free fraction in plasma, maximum enzyme binding rate, and drug concentration where enzyme achieves half maximum velocity (Vmax). Results were summarized as the change in any of the pharmacokinetic parameters in the malnourished population compared with those of a nonmalnourished control population.
Summary and Interpretation of the Results
In order to summarize the findings and interpret the results of the heterogeneous studies, a selection of the main findings was summarized by the reviewers according to the different pharmacokinetic processes (absorption, distribution, metabolism, and elimination). The main findings were summarized per studied drug, and the effects on pharmacokinetics were attempted to relate to mechanistic explanations based on explanations by the original studies or based on other relevant literature. This includes the type and severity of malnutrition, as well as specific drug characteristics (e.g. lipophilicity, P-glycoprotein binding, plasma protein binding, route of elimination). Malnutrition was considered severe when the original study defined patients as severely malnourished or severely wasted, or when patients had a Z-score for any of the used body size/mass descriptors of less than or equal to − 3. Other definitions of malnutrition were considered as moderate malnutrition. The different pathophysiological processes in malnutrition associated with pharmacokinetic changes observed for specific drugs were summarized, and when observed for a specific type of malnutrition, this was specified. In the summarizing figure, the effects on pharmacokinetics were categorized as weak or strong by the reviewers, based on the level of evidence. The evidence for the effect was considered strong when identified by multiple studies, or when the quality of the results of the original study was high (i.e. when the difference between patients and controls was adequately assessed, when pharmacokinetic parameters were adequately and precisely identified). The evidence for the effect was considered weak when the study design to identify an effect was considered poor, when the definition of the malnourished patient and control group was unclear, when the effect was statistically nonsignificant, when contradicting effects were found by different studies, or when other studies could not replicate the results.
Results and Discussion
Publications
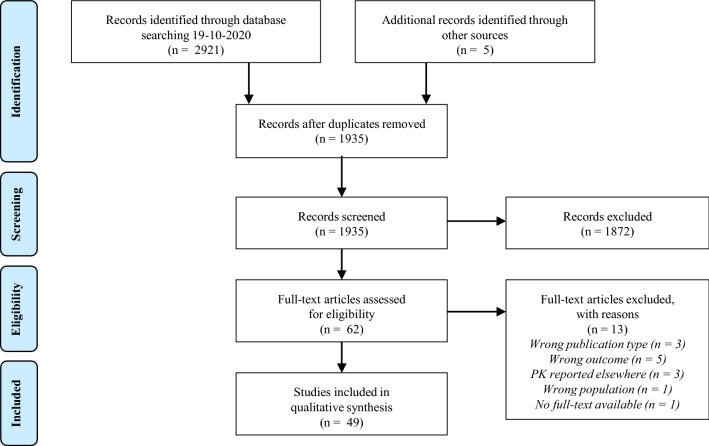
The systematic search yielded 1929 abstracts after deduplication (Fig. 1). Screening of the abstracts left 44 publications for inclusion. Five additional publications were identified through reference screening of the included publications. In total, 49 publications were included in this review. The studies were mainly conducted in TB patients (24), HIV patients (12), and malaria patients (11). Only two studies were conducted in patients with an NTD, i.e. helminthiasis caused by Trichuris trichiura and visceral leishmaniasis.
Fig. 1.
PRISMA flow diagram. PRISMA Preferred Reporting Items for Systematic Reviews and Meta-Analyses, PK pharmacokinetics
Study Population and Methodology
Overall, the majority of studies were conducted in children (19/24 in TB, 8/12 in HIV, 9/11 in malaria, and 2/2 in NTDs) (Tables 1, 2, 3 and 4). All studies were performed in malnourished patients, with well-nourished patients or well-nourished noninfected volunteers as control subjects. In 2/24 TB studies [31, 32] and 2/12 HIV studies [33, 34], the same patients served as control after nutritional rehabilitation. Malnourished patients had different degrees and forms of malnutrition (moderately or severely malnourished, underweight, wasted, stunted, marasmus, or kwashiorkor), measured by different metrics (see Sect. 3.3). Pharmacokinetic analysis was mostly performed by noncompartmental analysis (20/24 studies in TB, 6/12 studies in HIV, 7/11 studies in malaria, and 1/2 studies in NTDs) (Tables 5, 6, 7 and 8).
Table 1.
Overview of the included studies in TB patients
| Author (year) [Ref] | Drug | Route of administration | Total no. of patients | Malnourished patients (n) | Control group (n)a | Classification malnutrition | Age, yearsb | Country |
|---|---|---|---|---|---|---|---|---|
| Buchanan et al. (1979) [31] | Isoniazid | IV | 7 | Kwashiorkor (7) | Same patients after 21 days (7) | Wellcome classification | 1.53 ± 0.79 | Pakistan |
| Polasa et al. (1984) [59] | Rifampicin | PO | 28 | Uninfected volunteers (8) | Well-nourished uninfected volunteers (10) | AI < 0.18 | 49 | India |
| Rifampicin | PO | Patients receiving rifampicin therapy (10) | ||||||
| Prasad and Krishnaswamy (1978) [75] | Streptomycin | IM | 34 | (15) | (6) | AI < 0.18 | (25–35) | India |
| Bolme et al. (1988) [54] | Streptomycin | IM | 56 | Underweight (6); marasmic (6); kwashiorkor (3) | (4) | Wellcome classification | 4.9 (0.5–12) | Ethiopia |
| Streptomycin | IM | Underweight (11); marasmic (12); kwashiorkor (5) | (9) | |||||
| Eriksson et al. (1988)c [67] | Isoniazid | PO | 41 | Underweight (9); marasmic (15); kwashiorkor (6) | (11) | Wellcome classification | (0.5–12) | Ethiopia |
| Garg et al. (1988) [65] | Isoniazid | PO | 63 | Malnourished (10) | (13) | AI < 0.18 | 45 ± 5.2 (40–50) | India |
| Rifampicin | PO | Malnourished (10) | (11) | |||||
| Isoniazid and rifampicin | PO | Malnourished (10) | (9) | |||||
| Seth et al. (1992)d [18] | Rifampicin | PO | 115 | Undernourished (30); malnourished (10) | (15) | Grade I and II: undernourished; grade III and IV: malnourished | Children | India |
| Isoniazid | PO | Undernourished (30); malnourished (10) | (20) | |||||
| Seifart et al. (1995) [32] | Isoniazid | PO | 13 | PEM [no marasmus or kwashiorkor] (13), mean MUAC 135 mm | Same patients after 6 months (13), mean MUAC 150 mm | Weight, weight-for-age, and MUAC scores | 2.3 (0.8–7.6) | South Africa |
| Graham et al. (2006) [88] | Pyrazinamide | PO | 34 | Undernourished (12); marasmic (9) | (6) | Wellcome classification | 5.6 | Malawi |
| Ethambutol | PO | Undernourished (3); marasmic (1) | (3) | |||||
| McIlleron et al. (2009) [82] | Isoniazid | PO | 56 | Kwashiorkor (NA) | (NA) | Clinical diagnosis and presence of edema | 3.22 (0.25–13) | South Africa |
| Roy et al. (2010) [66] | Isoniazid | PO | 20 | Moderately malnourished (NA) | (NA) | WAZ less than −2 and greater than −3 | (5–12) | India |
| Verhagen et al. (2012) [78] | Isoniazid, rifampicin, and pyrazinamide | PO | 30 | Malnourished patients (4) | (26) | <5 years of age: WAZ or HAZ less than −2; >5 years of age: BAZ less than −2 | (1–15) | Venezuela |
| Ramachandran et al. (2013) [77] | Isoniazid, rifampicin, and pyrazinamide | PO | 84 | Stunting (22); underweight (31); wasting (16) | (NA) | WAZ, HAZ, or WHZ less than −2 | (1–12) | India |
| Garcia-Prats et al. (2015) [89] | Ofloxacin | PO | 85 | Underweight (14) | (71) | WAZ less than −2 | 3.4 (IQR 1.9–5.2) | South Africa |
| Mukherjee et al. (2015) [90] | Isoniazid, rifampicin, pyrazinamide, and ethambutol | PO | 127 | Severely malnourished (32) | (32) | <5 years of age: weight for height <70%; > 5 years of age: BMI for age <5th percentile | (0.5–15) | India |
| Isoniazid, rifampicin, pyrazinamide, and ethambutol | PO | Severely malnourished (26) | (37) | |||||
| te Brake et al. (2015) [80] | Rifampicin | PO | 36 | Severely malnourished (7); malnourished (4) | (25) | Severely malnourished: BMI < 16.0 kg/m2; malnourished: BMI < 18.5 kg/m2 | 35 (18–55) | Indonesia |
| Thee et al. (2015) [87] | Moxifloxacin | PO | 23 | Underweight for age (3) | (20) | WAZ less than − 2 | Median 11.1 (7–15) | South Africa |
| Antwi et al. (2017) [55] | Isoniazid, rifampicin, pyrazinamide, and ethambutol | PO | 113 | HIV co-infected patients (59), median WAZ − 2.7, median HAZ − 2.8 | HIV uninfected patients (54), median WAZ − 2.1, median HAZ − 1.6 | WAZ, HAZ, BAZ, MUAC and head circumference scores | Median 5.0 (IQR 2.2–8.3) | Ghana |
| Ramachandran et al. (2016) [83] | Isoniazid, rifampicin, and pyrazinamide | PO | 161 | NA | (NA) | NAe | (1–5) | India |
| Rogers et al. (2016) [79] | Isoniazid | PO | 30 | Underweight (7); stunted (4); wasted (9) | (NA) | WAZ, HAZ, or WHZ less than − 2 | (0–10) | South Africa |
| Ramachandran et al. (2017) [84] | Isoniazid, rifampicin, and pyrazinamide | PO | 1912 | Patients (961) | (951) | Body weight < 48 | Median 38 (IQR 27–50) | India |
| Dayal et al. (2018) [86] | Isoniazid and pyrazinamide | PO | 37 | Severely wasted (11); underweight (19); stunted (15); severely malnourished (14) | (NA) | According to WHO growth standards | (1–15) | India |
| Justine et al. (2020) [76] | Isoniazid, rifampicin, pyrazinamide, and ethambutol | PO | 51 | Malnourished (39) | (12) | WAZ, HAZ, or BAZ less than − 2 | (0.75–14) | Tanzania |
| Kumar et al. (2018) [91] | Levofloxacin, pyrazinamide, ethionamide, cyclosporine | PO | 25 | Underweight (10); stunted (14) | Not underweight (11); not stunted (7) | WAZ or HAZ less than − 2 | 16 (5–18) | India |
AI anthropometric index, BAZ BMI-for-age Z-score, BMI body mass index, HAZ height-for-age Z-score, IM intramuscularly, IQR interquartile range, IV intravenously, MUAC mid-upper arm circumference, NA not available, PEM protein-energy malnutrition, PO orally, SD standard deviation, TB tuberculosis, WAZ weight-for-age Z-score, WHO World Health Organization, WHZ weight-for-height Z-score
aWell-nourished patients, unless stated otherwise
bMean ± SD (range), unless stated otherwise
cStreptomycin results reported by Bolme et al. (1988)
dOriginal publication not traceable
e HAZ, WAZ and WHZ scores were tested as factors influencing drug concentration
Table 2.
Overview of the included studies in HIV patients
| Author (year) [Ref] | Drug | Route of administration | Total no. of patients | Malnourished patients (n) | Control group (n)a | Classification malnutrition | Age, yearsb | Country |
|---|---|---|---|---|---|---|---|---|
| Gatti et al. (1999) [60] | Rifabutin | PO | 20 | Wasting syndrome (10) | (10) | Weight loss > 10% in the last year | Wasting syndrome: 35.3 ± 6.0; controls: 37 ± 7 | Italy |
| Brantley et al. (2003) [44] | Stavudine, zidovudine, didanosine, and/or lamivudine | PO | 19 | Wasting and diarrhoea (12) | (7) | Weight loss > 10% in the last 2 months | 32.8 (21–54) | Brazil |
| Trout et al. (2004) [49] | Saquinavir | PO | 100 | AIDS symptomatic patients with severe body weight loss and/or diarrhoea (33) | Asymptomatic patients (30); AIDS symptomatic patients (37) | Weight loss > 10% in the last month | 40 ± 10 | France |
| Ellis et al. (2007) [50] | Nevirapine | PO | 127 | Stunting and wasting (NA) | (NA) | Stunting based on height-for-age, wasting based on BMI-for-age | (0.67–18) | Malawi and Zambia |
| Pollock et al. (2009) [92] | Nevirapine | PO | 37 | Mild to moderate malnutrition (12) | (25) | Weight-for-height 75–85% of the median | 4.4 (0.7–16.0) | Malawi |
| Swaminathan et al. (2011) [17] | Nevirapine | PO | 88 | Underweight (51), stunted (55) | Not underweight (37), not stunted (33) | Underweight: WAZ less than − 2; stunting: HAZ less than − 2 | 6.5 (0.5–12) | India |
| Bartelink et al. (2014) [81] | Lopinavir and ritonavir | PO | 116 | Underweight (42) | (160) | BMI < 18.5c | 30.5 (18–49) | Uganda |
| Efavirenz | PO | 105 | ||||||
| Fillekes et al. (2014) [68] | Zidovudine | PO | 45 | Moderate wasting (NA) and stunting (NA) | (NA) | NAd | 3.4 (IQR 2.6–6.2) | Uganda |
| Vreeman et al. (2014) [53] | Nevirapine | PO | 21 | Malnourished (NA) | (NA) | NAe | 5.4 (3–13) | Kenya |
| Bartelink et al. (2015) [48] | Efavirenz | PO | 163 | Ugandan children (32) [44% malnourished] | Dutch children (52) [10% underweight] | WAZ, HAZ, or BAZ less than − 2 | (0.7–7) | Uganda |
| Lopinavir | PO | Ugandan children (83) [47% malnourished] | French children (56) [14% underweight] | |||||
| Nevirapine | PO | Ugandan children (48) [50% malnourished] | American children (96) [14% malnourished] | |||||
| Archary et al. (2018) [33] | Lopinavir | PO | 63 | Severe acute malnutrition (34) | Patients after nutritional recovery (29) [WHZ greater than or equal to −2, >15% weight gain, or resolution of oedema and return of appetite] | WHZ less than −3, MUAC < 115 mm, or peripheral oedema | 0.9 (0.1–3.9) | South Africa |
| Archary et al. (2019) [34] | Abacavir and lamivudine | PO | 75 | Severe acute malnutrition (36) | Patients after nutritional recovery (39) [WHZ greater than or equal to − 2, > 15% weight gain, or resolution of oedema and return of appetite] | WHZ less than − 3, MUAC < 115 mm, or peripheral oedema | (0.08–12) | South Africa |
BAZ BMI-for-age Z-score, BMI body mass index, GWG gestational weight gain, HAZ height-for-age Z-score, HFIAS household food insecurity access scale, HHS household hunger scale, MUAC mid-upper arm circumference, NA not available, PO orally, SD standard deviation, TBW% total body water percentage, WAZ weight-for-age Z-score, WHZ weight-for-height Z-score
aWell-nourished patients, unless stated otherwise
bMean ± SD (range), unless stated otherwise
cBMI, GWG, MUAC, HFIAS and HHS scores were tested as factors influencing drug concentration
dWeight-for-age and height-for-age scores were tested as factors influencing drug concentration
eMUAC, WAZ scores and TBW% were tested as factors influencing pharmacokinetic parameters
Table 3.
Overview of the included studies in malaria patients
| Author (year) [Ref] | Drug | Route of administration | Total no. of patients | Malnourished patients (n) | Control group (n)a | Classification malnutrition | Age, yearsb | Country |
|---|---|---|---|---|---|---|---|---|
| Wharton et al. (1970) [69] | Chloroquine | PO | 13 | Kwashiorkor uninfected children (10) | Well-nourished uninfected children (3); Kwashiorkor children after 2–3 weeks recovery (7) | NA | Children | Uganda |
| Tulpule and Krishnaswamy (1983) [74] | Chloroquine | PO | 15 | Undernourished uninfected subjects (8) | Well-nourished uninfected subjects (7) | AI <0.18 | (25–40) | India |
| Walker et al. (1987) [70] | Chloroquine | PO | 11 | Kwashiorkor uninfected subjects (5) | Well-nourished uninfected subjects (6) | Wellcome classification | 2.5 (2–3.5) | Nigeria |
| Salako et al. (1989) [72] | Quinine | PO | 13 | Kwashiorkor uninfected subjects (6) | Well-nourished uninfected subjects (7) | Universally accepted clinical grounds | 2.2 ± 0.6 (1.5–3) | Nigeria |
| Treluyer et al. (1996) [26] | Quinine | IM | 15 | Undernourished patients (8) | Well-nourished patients (7) | MUAC/head circumference ratio < 0.28 | (0.75–5) | Gabon |
| Pussard et al. (1999) [58] | Quinine | IV | 40 | Malnourished uninfected subjects (10); malnourished patients (10) | Well-nourished uninfected subjects (10) | At least 2/3 measures (WAZ, HAZ and WHZ) less than − 2 | (2–6) | Niger |
| Dua et al. (2002) [71] | Chloroquine | PO | 22 | Malnourished tribal uninfected volunteers (6) | Healthy volunteers [AI > 0.2] (5) | AI < 0.18 | Mean 29–34 | India |
| Malnourished tribal patients (6) | Nontribal patients [AI > 0.2] (5) | |||||||
| WWARN (2015) [93] | Artemether-lumefantrine | PO | 567 | Underweight patients < 3 years of age (28) | Well-nourished patients < 3 years of age (262) | WAZ less than − 2 | 3 (1–4) | Africa and Asia |
| Underweight patients 3–4 years of age (48) | Well-nourished patients 3–4 years of age (229) | |||||||
| Kadam et al. (2016) [52] | Chloroquine | PO | 25 | PEM (13) | (12) | IAP classification | (5–12) | India |
| de Kock et al. (2018) [46] | Sulfadoxine and pyrimethamine | PO | 383 | Malnourished (41) | (326) | − 3 ≤ WAZ < − 2 | (0.25–4.9) | Africa |
| Severely malnourished (16) | WAZ less than − 3 | |||||||
| Chotsiri et al. (2019) [47] | Artemether-lumefantrine | PO | 263 | SAM (131) | Non-SAM (160) | WHZ less than −3 or MUAC < 115 cm | (0.5–4.9) | Mali and Niger |
AI anthropometric index, IAP Indian Academy of Pediatrics, IM intramuscularly, IV intravenously, MUAC mid-upper arm circumference, HAZ height-for-age Z-score, NA not available, PEM protein-energy malnutrition, PO orally, SAM severe acute malnutrition, SD standard deviation, WAZ weight-for-age Z-score, WHZ weight-for-height Z-score
aWell-nourished patients, unless stated otherwise
bMean ± SD (range), unless stated otherwise
Table 4.
Overview of the included studies in NTD patients
| Author (year) [Ref] | Disease | Drug | Route of administration | Total no. of patients | Malnourished patients (n) | Control group (n) | Classification malnutrition | Age, yearsa | Country |
|---|---|---|---|---|---|---|---|---|---|
| Schulz et al. (2019) [51] | Helminthiasis | Ivermectin | PO | 80 | (NA) | Well-nourished patients (NA) | NAb [total BMI: mean 15 (range 12–24)] | (2–5) | Ivory Coast |
| Helminthiasis | Ivermectin | PO | 120 | (NA) | Well-nourished patients (NA) | NAb [total BMI: mean 16 (range 12–25)] | (6–12) | Ivory Coast | |
| Palić et al. (2020) [94] | Visceral leishmaniasis | Miltefosine | PO | 51 | (NA) | Well-nourished patients (NA) | BAZ, WHZ or HAZ less than −2 | (4–12) | Kenya, Sudan, Uganda |
BAZ BMI-for-age Z-score, BMI body mass index, HAZ height-for-age Z-score, NA not available, NTD neglected tropical diseases, PO orally, WHZ weight-for-height Z-score
aRange
bThe correlation between BMI and pharmacokinetic parameters was investigated
Table 5.
Pharmacokinetic results of TB studies
| Drug | Absorption | Exposure | Distribution | Elimination | PK methodology | References |
|---|---|---|---|---|---|---|
| Isoniazid | Vd/F decreased | CL/F decreased*; T½ increased* | NCA | Buchanan et al. (1979) [31] | ||
| AUC and Cmax unchanged | T½ increased | NCA | Eriksson et al. (1988) [67] | |||
| AUC∞ unchanged | T½ increased | NCA | Garg et al. (1988) [65] | |||
| Tmax unchanged | AUC and Cmax increased | T½ increased; ke decreased | NA | Seth et al. (1992) [18] | ||
| C2h unchanged | T½ and ke unchanged | NCA | Seifart et al. (1995) [32] | |||
| Cmax unchanged | NCA | McIlleron et al. (2009) [82] | ||||
| Tmax unchanged | AUC24 and AUC increased; Cmax unchanged | Vd/F unchanged | CL/F decreased; T½ and ke unchanged | CA | Roy et al. (2010) [66] | |
| AUC24 unchanged | NCA | Verhagen et al. (2012) [78] | ||||
| AUC8 and Cmax decreased in stunting* | NCA | Ramachandran et al. (2013) [77] | ||||
| Tmax unchanged | AUC4, C2h, and Cmax unchanged | NCA | Mukherjee et al. (2015) [90] | |||
| Tmax decreased* | AUC8 and Cmax unchanged | Normalized Vd/F unchanged | Normalized CL/F unchanged | NCA | Antwi et al. (2017) [55] | |
| AUC8 decreased with low WAZ; Cmax decreased with low HAZ | NCA | Ramachandran et al. (2016) [83] | ||||
| Vmax and Km unchanged | ke unchanged | CA | Rogers et al. (2016) [79] | |||
| C2h decreased* | NCA | Ramachandran et al. (2017) [84] | ||||
| AUC8 and Cmax unchanged | NCA | Dayal et al. (2018) [86] | ||||
| C2h decreased* | NCA | Justine et al. (2020) [76] | ||||
| Rifampicin | AUC∞ and Cmax decreased* | Plasma protein binding decreased* | CL/F and CLR increased*; T½ unchanged | NCA | Polasa et al. (1984) [59] | |
| AUC∞ increased | T½ unchanged | NCA | Garg et al. (1988) [65] | |||
| Tmax unchanged | AUC and Cmax increased | T½ and ke unchanged | NA | Seth et al. (1992) [18] | ||
| AUC24 unchanged | NCA | Verhagen et al. (2012) [78] | ||||
| AUC8 and Cmax decreased in stunting* and underweight* | NCA | Ramachandran et al. (2013) [77] | ||||
| Tmax unchanged | AUC4, C2h, and Cmax unchanged | NCA | Mukherjee et al. (2015) [90] | |||
| Tmax unchanged | AUC24 and Cmax unchanged | Vd/F and ffree unchanged | CL/F and T½ unchanged | NCA | te Brake et al. (2015) [80] | |
| Tmax unchanged | AUC8 and Cmax decreased* | Normalized Vd/F unchanged | Normalized CL/F increased* | NCA | Antwi et al. (2017) [55] | |
| AUC8 and Cmax unchanged | NCA | Ramachandran et al. (2016) [83] | ||||
| C2h unchanged | NCA | Ramachandran et al. (2017) [84] | ||||
| C2h decreased* | NCA | Justine et al. (2020) [76] | ||||
| Pyrazinamide | Tmax unchanged | AUC24 and Cmax decreased; AUC24/dose and Cmax/dose unchanged | NCA | Graham et al. (2006) [88] | ||
| AUC24 decreased | NCA | Verhagen et al. (2012) [78] | ||||
| AUC8 and Cmax decreased in stunting* and underweight* | NCA | Ramachandran et al. (2013) [77] | ||||
| Tmax unchanged | AUC4, C2h, and Cmax unchanged | NCA | Mukherjee et al. (2015) [90] | |||
| Tmax decreased* | AUC8 decreased*; Cmax unchanged | Normalized Vd/F unchanged | Normalized CL/F increased* | NCA | Antwi et al. (2017) [55] | |
| AUC8 and Cmax unchanged | NCA | Ramachandran et al. (2016) [83] | ||||
| C2h decreased* | NCA | Ramachandran et al. (2017) [84] | ||||
| AUC8 decreased in severe wasting*, stunting*, and severe malnutrition*; Cmax decreased in severe malnutrition* | NCA | Dayal et al. (2018) [86] | ||||
| C2h unchanged | NCA | Justine et al. (2020) [76] | ||||
| AUC8 unchanged; Cmax decreased in underweight* | NCA | Kumar et al. (2018) [91] | ||||
| Ethambutol | Tmax decreased | AUC24 and AUC24/dose unchanged; Cmax and Cmax/dose increased | NCA | Graham et al. (2006) [88] | ||
| Tmax unchanged | AUC4, C2h, and Cmax unchanged | NCA | Mukherjee et al. (2015) [90] | |||
| Tmax unchanged | AUC8 and Cmax decreased* | Normalized Vd/F increased* | Normalized CL/F increased* | NCA | Antwi et al. (2017) [55] | |
| C2h unchanged | NCA | Justine et al. (2020) [76] | ||||
| Streptomycin | T½,abs unchanged | Vd/F increased in kwashiorkor* | CL/F unchanged; T½,el increased in kwashiorkor* | CA | Bolme et al., (1988) [54] | |
| Tmax increased | Concentrations unchanged | Vd/F and plasma protein binding unchanged | T½ unchanged | NCA | Prasad and Krishnaswamy (1978) [75] | |
| Ofloxacin | Tmax unchanged | AUC8, AUC24, and Cmax unchanged | Vd/F unchanged | CL/F and T½ unchanged | NCA | Garcia-Prats et al. (2015) [89] |
| Moxifloxacin | Tmax unchanged | AUC8 decreased*; Cmax unchanged | NCA | Thee et al. (2015) [87] | ||
| Levofloxacin | AUC8 and Cmax unchanged | NCA | Kumar et al. (2018) [91] | |||
| Ethionamide | AUC8 and Cmax unchanged | NCA | Kumar et al. (2018) [91] | |||
| Cyclosporine | AUC8 and Cmax unchanged | NCA | Kumar et al. (2018) [91] |
AUC area under the curve, AUC4 AUC from time zero to 4 h, AUC8 AUC from time zero to 8 h, AUC24 AUC from time zero to 24 h, AUC∞ AUC from time zero to infinity, C2h concentration at 2 h, CA compartmental analysis, CL/F apparent oral clearance, CLR renal clearance, Cmax peak concentration, ffree unbound fraction, HAZ height-for-age Z-score, ka absorption rate constant, ke elimination rate constant, Km drug concentration where enzyme achieves half Vmax, NA not available, NCA noncompartmental analysis, PK pharmacokinetic, T½,abs absorption half-life, T½,el elimination half-life, T½ terminal half-life, TB tuberculosis, Tmax time to maximum plasma concentration, Vd/F apparent volume of distribution, Vmax maximum enzyme binding rate, WAZ weight-for-age Z-score
*Significant difference
Table 6.
Pharmacokinetic results of HIV studies
| Drug | Absorption | Exposure | Distribution | Elimination | PK methodology | References |
|---|---|---|---|---|---|---|
| Rifabutin | Tmax decreased | AUC unchanged; Cmax increased*; C24h increased* | Vd/F decreased; Vd/F/kg decreased | CL/F unchanged; CL/F/kg unchanged; T½ decreased | NCA | Gatti et al. (1999) [60] |
| Stavudine | Cmax decreased* | NCA | Brantley et al. (2003) [44] | |||
| Didanosine | Cmax decreased | NCA | Brantley et al. (2003) [44] | |||
| Lamivudine | Cmax unchanged | NCA | Brantley et al. (2003) [44] | |||
| ka unchanged | Vd/F unchanged | CL/F unchanged | CA | Archary et al. (2019) [34] | ||
| Abacavir | ka unchanged, F increased* | Vc/F unchanged; Q/F unchanged; Vp/F unchanged | CL/F unchanged | CA | Archary et al. (2019) [34] | |
| Saquinavir | Tlag decreased*; ka decreased*; Tmax unchanged | AUC increased*; Cmax increased* | Vd/F decreased* | CL/F decreased*; ke decreased* | CA | Trout et al. (2004) [49] |
| Nevirapine | Cmax increased in wasting*; Cmax decreased in stunting* | NCA | Ellis et al. (2007) [50] | |||
| AUC12, Cmax, and Ctrough unchanged | NCA | Pollock et al. (2009) [92] | ||||
| C2h decreased in stunting*; Ctrough unchanged | NCA | Swaminathan et al. (2011) [17] | ||||
| ka unchanged | Vd/F decreased with increasing TBW% | CL/F unchanged | CA | Vreeman et al. (2014) [53] | ||
| F increased* | Vd/F decreased* | CL/F decreased* | CA | Bartelink et al. (2015) [48] | ||
| Lopinavir | F unchanged | CL/F unchanged | CA | Bartelink et al. (2014) [81] | ||
| F decreased* | Vd/F increased* | CL/F increased* | CA | Bartelink et al. (2015) [48] | ||
| ka unchanged | Cmax decreased | Vd/F unchanged | CL/F unchanged | CA | Archary et al. (2018) [33] | |
| Efavirenz | F unchanged | CL/F unchanged | CA | Bartelink et al. (2014) [81] | ||
| F decreased* | Vd/F increased* | CL/F increased* | CA | Bartelink et al. (2015) [48] | ||
| Ritonavir | F unchanged | CL/F unchanged | CA | Bartelink et al. (2014) [81] | ||
| Zidovudine | Cmax unchanged | NCA | Brantley et al. (2003) [44] | |||
| AUC12 increased in wasting*, Cmax and C12h unchanged | CL/F decreased in wasting*, T½ unchanged | NCA | Fillekes et al. (2014) [68] |
AUC area under the curve, AUC12 area under the curve from time zero to 12 h, C2h concentration at 2 h, C12h concentration at 12 h, C24h concentration at 24 h; CA compartmental analysis, CL/F apparent oral clearance, Cmax peak concentration, Ctrough trough concentration, F apparent bioavailability, ka absorption rate constant, ke elimination rate constant, NCA noncompartmental analysis, PK pharmacokinetic, Q/F apparent intercompartmental clearance, T½ terminal half-life, TBW% total body water percentage, Tlag absorption lag time, Tmax time to reach Cmax, Vc/F central volume of distribution, Vd/F volume of distribution, Vp/F peripheral volume of distribution
*Significant difference
Table 7.
Pharmacokinetic results of malaria studies
| Drug | Absorption | Exposure | Distribution | Metabolism | Elimination | PK methodology | References |
|---|---|---|---|---|---|---|---|
| Chloroquine | Drug/metabolite ratio increased* | NCA | Wharton and McChesney (1970) [69] | ||||
| AUC unchanged | CL/F increased*; T½ unchanged | NCA | Tulpule and Krishnaswamy (1983) [74] | ||||
| AUC decreased* | Drug/metabolite ratio increased | T½ unchanged | NCA | Walker et al. (1987) [70] | |||
| Tmax increased | AUC168, AUC∞, and Cmax unchanged | Drug/metabolite ratio increased | CL/F unchanged; T½ unchanged | NCA | Dua et al. (2002) [71] | ||
| AUC∞ increased; Cmax unchanged | Vd/F decreased | Drug/metabolite ratio unchanged | CL/F decreased; T½ unchanged | NCA | Kadam et al. (2016) [52] | ||
| Quinine | T½,abs increased* | AUC increased*; Cmax decreased* | CL/F decreased*; T½ increased* | CA | Salako et al. (1989) [72] | ||
| Tmax decreased* | Cmax unchanged; C12h decreased | Vd/F and plasma protein binding unchanged | Drug/metabolite ratio decreased* | CL/F increased*; T½ decreased* | NCA | Treluyer et al. (1996) [26] | |
| AUC8 and Cmax increased* | Vd/F decreased*; plasma protein binding increased*; erythrocyte binding unchanged | CL/F decreased*; T½ increased* | CA | Pussard et al. (1999) [58] | |||
| Lumefantrine | Ca decreased in children < 3 years of age | NCA | WWARN (2015) [93] | ||||
| F decreased* | CA | Chotsiri et al. (2019) [47] | |||||
| Sulfadoxine | F decreased* | CA | de Kock et al. (2018) [46] | ||||
| Pyrimethamine | F decreased* | CA | de Kock et al. (2018) [46] |
AUC area under the curve, AUC8 AUC from time zero to 8 h, AUC168 AUC from time zero to 168 h, AUC∞ AUC from time zero to infinity, C12h concentration at 12 h, CA compartmental analysis, CL/F apparent oral clearance, Cmax peak concentration, F apparent bioavailability, NCA noncompartmental analysis, PK pharmacokinetic, T½,abs apparent absorption half-life, T½ terminal half-life, Tmax time to reach Cmax, Vd/F volume of distribution
*Significant difference
aDay 7 concentrations at different time points
Table 8.
Pharmacokinetic results of NTD studies
| Drug | Absorption | Exposure | Distribution | Excretion | PK methodology | References |
|---|---|---|---|---|---|---|
| Ivermectin | AUC increased* | NCA | Schulz et al. (2019) [51] | |||
| Miltefosine | F and ka unchanged | Vc/F, Q/F, and Vp/F unchanged | CL/F unchanged | CA | Palić et al. (2020) [94] |
AUC area under the curve, CA compartmental analysis, CL/F apparent oral clearance, F apparent bioavailability, ka absorption rate constant, NCA noncompartmental analysis, NTD neglected tropical diseases, PK pharmacokinetic, Q/F apparent intercompartmental clearance, Vc/F apparent central volume of distribution, Vp/F apparent peripheral volume of distribution
*Significant difference
Classification of Malnutrition
The classification of malnutrition in the included studies was very heterogeneous. In the majority of studies, Z-score was used to classify the degree of malnutrition (Tables 1, 2, 3 and 4), i.e. the difference in terms of standard deviations from a median nutritional status reference value as defined, for example, by the National Center for Health Statistics (NCHS)/WHO Growth Standards [35–38]. A Z-score of less than or equal to − 2 and greater than − 3 was considered as moderate malnutrition, while a score of less than or equal to −3 was considered as severe malnutrition. In children, the weight-for-age Z-score (WAZ), height-for-age Z-score (HAZ), and weight-for-height Z-score (WHZ) were used to define the degree of underweight, stunting, or wasting, respectively. In children over 5 years of age, adolescents, and adults, the HAZ, body mass index (BMI)-for-age Z-score (BAZ), and BMI were generally used as a nutritional status metric [37]. Severe malnutrition in children was further categorized as marasmus (absence of oedema) or kwashiorkor (presence of oedema) [39]. Other metrics used for classification in children were (1) the Wellcome Classification [40], based on the percentage of expected weight for age (WFA): > 80% WFA was graded as normal, 60–80% WFA was graded as undernutrition, < 60% WFA was graded as marasmus, and low WFA in combination with oedema and low serum protein was graded as kwashiorkor; (2) The Indian Academy of Pediatrics classification of PEM based on Khadilkar’s growth charts [41]: measurements included height, weight, head circumference, and penile length (≤ 3 years of age); weight, height, BMI, penile length, and standard metabolic rate (4–8 years of age); weight, BMI, and standard metabolic rate (9–18 years of age); or (3) the left mid-upper arm circumference (MUAC) [42]. For adults, the anthropometric index (AI) [43] was used, defined as (weight[kg]/height[cm]2) × 100, where an AI < 0.18 was considered as malnutrition.
Effect of Malnutrition on Pharmacokinetics
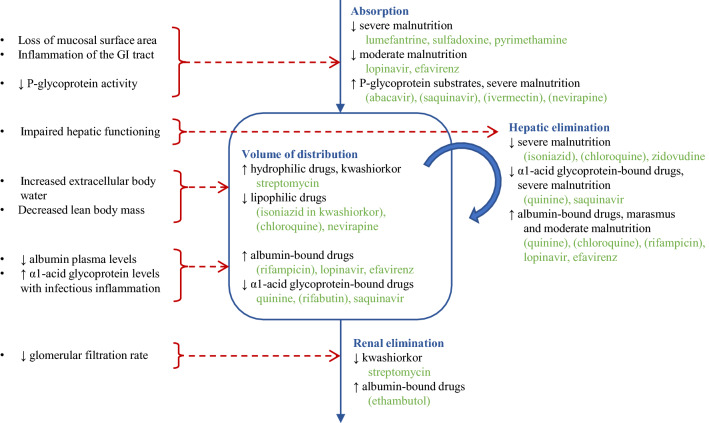
A complete overview of the effects of malnutrition on the various pharmacokinetic processes is presented in Tables 5, 6, 7 and 8. If possible, the effects were related to the type and severity of malnutrition or specific drug characteristics in the subsections below. The main findings with mechanistic explanations are summarized in Fig. 2.
Fig. 2.
Alterations in drug pharmacokinetics by malnutrition. Figure summarizes the main pathophysiological changes (left) and the associated effects on drug pharmacokinetics in different pharmacokinetic stages, illustrated by the effects found for drugs against poverty-related infectious diseases (right). Drug names are mentioned when the evidence for the effect was considered strong, or mentioned in brackets when the evidence for the effect was considered weak
Absorption
Drug absorption might be impaired because of loss of mucosal surface area and inflammation of the gastrointestinal tract, often observed in patients with severe wasting and diarrhoea (Fig. 2) [20, 44, 45]. Whereas a change in absorption rate might not be clinically relevant, an altered extent of absorption (bioavailability) might impact drug exposure and, consequently, drug effect. According to the studies included in this review, apparent bioavailability of lumefantrine, sulfadoxine, pyrimethamine, lopinavir, and efavirenz was decreased in severely malnourished patients [46–48]. On the other hand, apparent bioavailability of abacavir was increased in severe acute malnutrition [34], and increased exposure for saquinavir [49], nevirapine [50], and ivermectin [51] in severely wasted [49, 50]/malnourished [51] patients was potentially caused by increased absorption. As suggested by the literature, the increased absorption of these drugs is likely due to decreased P-glycoprotein activity in the enterocytes or the enlargement of their tight junctions, enhancing paracellular passive uptake of the drug [21, 49].
Distribution and Protein Binding
Severe malnutrition is associated with changes in body composition, such as increased extracellular body water and decreased lean body mass, and the presence of oedema in kwashiorkor, leading to decreased drug distribution of lipophilic drugs and increased distribution of hydrophilic drugs (Fig. 2) [19, 20]. This was demonstrated by various identified studies: volume of distribution was decreased for the lipophilic drug isoniazid in kwashiorkor [31], and for chloroquine [52] and nevirapine [48, 53] in malnutrition. Volume of distribution was increased for the hydrophilic drug streptomycin in kwashiorkor [54]. These effects seem to exhibit mainly in kwashiorkor, as the effects could not be demonstrated for isoniazid and streptomycin in moderate malnutrition [19, 52, 55].
Nonetheless, distribution of highly protein-bound drugs with a high extraction ratio may be changed because of altered plasma protein levels (Fig. 2) [19, 20, 56]. Basic drugs mainly bind to albumin, whereas acidic drugs mainly bind to α1-acid glycoprotein. Binding of drugs to α1-acid glycoprotein becomes pharmacologically relevant when the dissociation constant for α1-acid glycoprotein is <0.1 times lower compared with albumin [25]. Malnutrition in combination with infectious inflammation is associated with low serum albumin levels [23] but with increased inflammatory proteins such as α1-acid glycoprotein [57, 58]. This was supported by some of the studies: protein binding for rifampicin was decreased [59] and volume of distribution for lopinavir and efavirenz was increased in malnourished patients [48], potentially causing increased drug elimination and resulting decreased drug exposure. The increased levels of α1-acid glycoprotein in malnutrition resulted in higher quinine plasma protein binding and increased exposure in malnourished patients [58]. For the weak bases rifabutin [60] and saquinavir [49], the decreased volume of distribution and resulting increased Cmax in wasting [49, 60] might also be the result of elevated α1-acid glycoprotein binding [61]. However, it should be noted that the increased levels of α1-acid glycoprotein in malnourished patients are a result of infections, often accompanied by malnutrition. The effect of malnutrition itself on α1-acid glycoprotein levels has not been well-investigated. Although it is believed that the humoral immune response is well preserved in malnourished patients during infection, some studies demonstrated an impaired acute-phase protein response in children with severe PEM, especially in kwashiorkor [62]. This complicates the evaluation of α1-acid glycoprotein binding in relation to malnutrition.
Metabolism and Excretion
Metabolism of hepatically cleared drugs may be altered in severe malnutrition due to impaired hepatic functioning by fat infiltration of the liver and decreased synthesis and activity of certain phase I and II metabolizing enzymes [19, 20, 45, 63, 64]. Impaired GFR in severe malnutrition may impact the excretion of renally cleared drugs (Fig. 2) [19, 20]. Decreased elimination was observed for the hepatically cleared drug isoniazid in kwashiorkor or different degrees of malnutrition [18, 31, 65–67], for saquinavir and zidovudine in wasting [49, 68], for chloroquine in kwashiorkor [69, 70] and malnutrition [52, 71], and for quinine in kwashiorkor [72] and severely malnourished patients [58]. An increased AUC and slower clearance of isoniazid in malnutrition is likely caused by reduced metabolism by acetylation, although the effect of malnutrition on the process of acetylation could not be clearly determined [73]. Saquinavir, zidovudine, chloroquine, and quinine metabolism is mainly driven by cytochrome P450 enzymes, whose activity is reduced in malnutrition [64]. Another reason for the decreased metabolism of, for example, quinine and saquinavir could be the increase of α1-acid glycoprotein levels in kwashiorkor and severe malnutrition, leading to a decrease in the unbound fraction and, consequently, lower hepatic uptake [26, 58]. Likewise, the increased excretion of chloroquine [74], quinine [26], ethambutol [55], rifampicin [55, 59], lopinavir [48], and efavirenz [48] in (moderate) malnutrition might be caused by the increased free fraction of these highly albumin-bound drugs. For the renally cleared drug streptomycin, excretion was decreased in kwashiorkor [54], but unchanged in malnutrition [75].
Type of Malnutrition
The alterations in drug exposure likely depend on the patient population, as for some drugs relationships could be identified between the type or severity of malnutrition and the effect on drug exposure in these studies. For example, isoniazid and rifampicin exposure was decreased in moderately malnourished patients [59, 76, 77], potentially due to either reduced absorption or decreased protein binding and, consequently, an increased volume of distribution or elevated drug clearance [59]. On the other hand, isoniazid and rifampicin exposure was increased in severe malnutrition [18, 65, 66], potentially caused by a more pronounced suppression of enzyme activity in severe malnutrition [65]. On the other hand, chloroquine exposure was decreased in kwashiorkor, potentially caused by decreased bioavailability [70]. Nevirapine concentrations were decreased in stunted children but increased in wasted children [50]. This might be explained by the different pathophysiological conditions: the decreased absorption and enhanced clearance of protein-bound drugs associated with stunting might lead to decreased serum concentrations, whereas reduced metabolism in wasting might cause an increase in plasma concentration [17].
Study Design and Data Analysis
The effects of malnutrition on PRD drug pharmacokinetics were not always replicable, which might be due to the underpowered study designs. The sample size was small (< 50 participants) in the majority of studies, which can be the reason why a potentially expected effect could not be demonstrated in some of the studies [32, 67, 78–81]. The effect might not be traceable because of the small difference in malnutrition status between patient groups [32, 55, 76, 78, 79, 81]. In other studies, the number of malnourished patients was unknown [82, 83] or malnutrition was poorly diagnosed [84].
The studies included in this review include a heterogeneous patient population with a wide variety in the source and severity of malnutrition, as well as different metrics used to define and score malnourished patients. In order to identify the effects of malnutrition on pharmacokinetics, a standard and generic definition of the different types of malnutrition is needed to compare different studies. Moreover, the studied populations included patients of different age ranges and patients infected by different PRDs, different severity of disease, as well as non-infected subjects. Disease activity with increased inflammatory cytokine levels, local disease activity in the gastrointestinal tract, and comedications can all impact pharmacokinetics. Malnutrition may impact physiological processes differently in patients of different ages. All these sources of heterogeneity complicate the extraction of the effects of malnutrition on pharmacokinetics. Moreover, the dosing guidelines might impact drug exposure in the different populations. When fixed dosing is applied, the dose per kilogram of body weight will be higher in malnourished patients after fixed dosing, but even when using a linear weight-based dosing, exposure differences might be expected.
Conclusions and Recommendations
Forty-nine studies were included in this review, with most of the studies conducted in TB, HIV, and malaria patients. For most of the NTDs, no studies were identified at all. In 21/29 of the PRD drugs included in this review, pharmacokinetics were affected by malnutrition. A complete overview of the literature is summarized in Tables 1, 2, 34, 5, 6, 7, and 8. The included studies were relatively small and heterogeneous. However, trends were observed for specific classes of drugs and types of malnutrition. An interpretation of the results by the reviewers is summarized in Fig. 2, where the effects are categorized as strong or weak effects based on the level of evidence. The bioavailability of lumefantrine, sulfadoxine, pyrimethamine, lopinavir, and efavirenz was decreased in severely malnourished patients, but increased for the P-glycoprotein substrates abacavir, saquinavir, nevirapine, and ivermectin. Volume of distribution was decreased for the lipophilic drugs isoniazid, chloroquine, and nevirapine, and for the α1-acid glycoprotein-bound drugs quinine, rifabutin, and saquinavir. Volume of distribution was increased for the hydrophilic drug streptomycin, and for the albumin-bound drugs rifampicin, lopinavir, and efavirenz. Drug elimination was decreased in severe malnutrition for the hepatically cleared drugs isoniazid, chloroquine, quinine, zidovudine, and saquinavir, and for the renally cleared drug streptomycin. On the other hand, elimination was increased for the albumin-bound drugs quinine, chloroquine, rifampicin, lopinavir, efavirenz, and ethambutol.
The alterations in pharmacokinetics in malnourished patients might impact clinical efficacy and/or toxicity and therefore may require dose adjustments in the malnourished population. A systematic review on antibiotics suggested that normal doses of penicillins, cotrimoxazole and gentamicin are well-tolerated in malnourished children, while the dose or frequency of chloramphenicol requires adjustment, although evidence was not sufficiently strong to establish dosing recommendations [85]. These studies suggested a clinically relevant impact of malnutrition on the pharmacokinetics of certain PRD drugs. Various studies included in this systematic review addressed the need for dose adjustments in the malnourished population for isoniazid [18, 67, 76, 77, 83, 84], rifampicin [55, 76, 77], pyrazinamide [55, 77, 84, 86], ethionamide [55], moxifloxacin [87], stavudine [44], nevirapine [17], chloramphenicol [70], and ivermectin [51]. A specifically adapted treatment regimen in malnourished patients was only suggested for nevirapine [50] and quinine [26]. Other studies concluded that the identified effect on pharmacokinetics was of no clinical relevance, and no dose adjustment might be needed for rifampicin [59, 65], rifabutin [60], chloramphenicol [52], quinine [58], and pyrimethamine [46]. These results imply a trend between the degree of malnutrition and the pharmacokinetic effect size: a clinically relevant effect was observed in severe malnutrition and kwashiorkor [18, 50, 67, 70, 86], except for quinine [58], whereas no dose adjustment was needed in mainly moderately malnourished patients. The clinical impact of these pharmacokinetic effects in severely malnourished patients is highly relevant as these patients are mostly excluded in clinical trials, whereas, in reality, these patients constitute a sizeable proportion of the PRD patient populations. This highlights the importance to include severely malnourished patients in pharmacokinetic studies for PRD drugs.
This systematic review summarizes the main effects of malnutrition on PRD drug pharmacokinetics, with potentially clinically relevant effects on treatment response. This overview can be used as a basis to predict the effects of malnutrition on PRD drug pharmacokinetics. This might be relevant for the study design of clinical studies, to account for the possible clinically relevant effects of malnutrition on pharmacokinetics, based on the drug characteristics and types of malnutrition in the studied population.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Funding
This study is part of the EDCTP2 programme supported by the European Union (grant number RIA2016S1635-AfriKADIA). TPCD was also supported by a ZonMw/Dutch Research Council (NWO) Veni grant (project number 91617140).
Conflicts of interest
Luka Verrest, Erica A. Wilthagen, Jos H. Beijnen, Alwin D.R. Huitema and Thomas P.C. Dorlo have no conflicts of interest to declare.
Author contributions
LV and TPCD were responsible for the collection and summary of the study data, as well as the draft of the first version of the manuscript. EW was responsible for the systematic literature search and summary of the search in the manuscript. All authors participated in the interpretation of the study results and in the drafting, critical revision and approval of the final version of the manuscript.
Availability of data, material and code
Not applicable.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
The original online version of this article was revised: The Open Access funding information was published incorrectly in the original version.
Change history
9/8/2022
Correct Open Access funding information has been updated in the Funding Note.
Change history
10/25/2021
A Correction to this paper has been published: 10.1007/s40262-021-01080-4
References
- 1.Rice AL, Sacco L, Hyder A, Black RE. Malnutrition as an underlying cause of childhood deaths associated with infectious diseases in developing countries. Bull World Health Organ. 2000;78:1207–1221. [PMC free article] [PubMed] [Google Scholar]
- 2.Pelletier DL, Frongillo EA. Changes in child survival are strongly associated with changes in malnutrition in developing countries. J Nutr. 2003;133:107–119. doi: 10.1093/jn/133.1.107. [DOI] [PubMed] [Google Scholar]
- 3.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–451. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 4.Bryce J, Boschi-Pinto C, Shibuya K, Black RE. WHO estimates of the causes of death in children. Lancet. 2005;365:1147–1152. doi: 10.1016/S0140-6736(05)71877-8. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Neglected Tropical Diseases. 2020 [cited 25 Mar 2020]. https://www.who.int/neglected_diseases/diseases/en/. Accessed 10 Nov 2020.
- 6.Jesson J, Masson D, Adonon A, Tran C, Habarugira C, Zio R, et al. Prevalence of malnutrition among HIV-infected children in Central and West-African HIV-care programmes supported by the Growing Up Programme in 2011: a cross-sectional study. BMC Infect Dis. 2015;15:216. doi: 10.1186/s12879-015-0952-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gizaw A, Eshetu A, Birhanu D. Malnutrition and associated factors among adult people living with HIV/AIDS receiving antiretroviral therapy at Organization for Social Service Health Development in Jimma Town Oromia Region South West Ethiopia. Gen Med Open Access. 2018;06:4–11. [Google Scholar]
- 8.Feleke BE, Feleke TE, Biadglegne F. Nutritional status of tuberculosis patients, a comparative cross-sectional study. BMC Pulm Med. 2019;19:1–9. doi: 10.1186/s12890-019-0953-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Charchuk R, Houston S, Hawkes MT. Elevated prevalence of malnutrition and malaria among school-aged children and adolescents in war-ravaged South Sudan. Pathog Glob Health. 2015;109:395–400. doi: 10.1080/20477724.2015.1126033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schaible UE, Kaufmann SHE. Malnutrition and infection: Complex mechanisms and global impacts. PLoS Med. 2007;4:0806–812. doi: 10.1371/journal.pmed.0040115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walson JL, Berkley JA. The impact of malnutrition on childhood infections. Curr Opin Infect Dis. 2018;31:231–236. doi: 10.1097/QCO.0000000000000448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katona P, Katona-Apte J. The interaction between nutrition and infection. Clin Infect Dis. 2008;46:1582–1588. doi: 10.1086/587658. [DOI] [PubMed] [Google Scholar]
- 13.Hall A, Zhang Y, MacArthur C, Baker S. The role of nutrition in integrated programs to control neglected tropical diseases. BMC Med. 2012;10:41. doi: 10.1186/1741-7015-10-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nkuo- Akenji T, Sumbele I, Mankah E, Njunda A, Samje M, Kamga L. The burden of malaria and malnutrition among children less than 14 years of age in a rural village of Cameroon. Afr J Food Agric Nutr Dev. 2008;8:252–264. [Google Scholar]
- 15.Pham TPT, Alou MT, Golden MH, Million M, Raoult D. Difference between kwashiorkor and marasmus: Comparative meta-analysis of pathogenic characteristics and implications for treatment. Microb Pathog. 2021;150:104702. doi: 10.1016/j.micpath.2020.104702. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Nutrition Landscape Information System (NLIS) country profile indicators: interpretation guide. 2010. pp. 1–51. https://apps.who.int/iris/bitstream/handle/10665/44397/9789241599955_eng.pdf?sequence=1&isAllowed=y. Accessed 10 Nov 2020.
- 17.Swaminathan S, Ramachandran G, Kupparam HKA, Mahalingam V, Soundararajan L, Kannabiran BP, et al. Factors influencing plasma nevirapine levels: a study in HIV-infected children on generic antiretroviral treatment in India. J Antimicrob Chemother. 2011;66:1354–1359. doi: 10.1093/jac/dkr075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seth V, Beotra A, Bagga A, Seth S. Drug therapy in malnutrition. Indian Pediatr. 1992;29:1341–1346. [PubMed] [Google Scholar]
- 19.Krishnaswamy K. Drug metabolism and pharmacokinetics in malnourished children. Clin Pharmacokinet. 1989;17:68–88. doi: 10.2165/00003088-198900171-00006. [DOI] [PubMed] [Google Scholar]
- 20.Oshikoya KA, Senbanjo IO. Pathophysiological changes that affect drug disposition in protein-energy malnourished children. Nutr Metab. 2009;6:1–7. doi: 10.1186/1743-7075-6-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Washington CB, Duran GE, Man MC, Sikic BI, Blaschke TF. Interaction of anti-HIV protease inhibitors with the multidrug transporter P-glycoprotein (P-gp) in human cultured cells. J Acquir immune Defic Syndr Hum retrovirology. 1998;19:203–209. doi: 10.1097/00042560-199811010-00001. [DOI] [PubMed] [Google Scholar]
- 22.Coulthard MG. Oedema in kwashiorkor is caused by hypoalbuminaemia. Paediatr Int Child Health. 2015;35:83–89. doi: 10.1179/2046905514Y.0000000154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soeters PB, Wolfe RR, Shenkin A. Hypoalbuminemia: pathogenesis and clinical significance. J Parenter Enter Nutr. 2019;43:181–193. doi: 10.1002/jpen.1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morlese JF, Forrester T, Jahoor F. Acute-phase protein response to infection in severe malnutrition. Am J Physiol - Endocrinol Metab. 1998;275:3–8. doi: 10.1152/ajpendo.1998.275.1.E112. [DOI] [PubMed] [Google Scholar]
- 25.Smith SA, Waters NJ. Pharmacokinetic and pharmacodynamic considerations for drugs binding to alpha-1-acid glycoprotein. Pharm Res. 2018;36(2):30. doi: 10.1007/s11095-018-2551-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Treluyer J, Roux A, Mugnier C, Flouvat B, Lagardere B. Metabolism of quinine in children with global malnutrition. Pediatr Res. 1996;40:558–563. doi: 10.1203/00006450-199610000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Oshikoya KA, Sammons HM, Choonara I. A systematic review of pharmacokinetics studies in children with protein-energy malnutrition. Eur J Clin Pharmacol. 2010;66:1025–1035. doi: 10.1007/s00228-010-0851-0. [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1–9. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bramer WM, Giustini D, De JGB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016;104:240–243. doi: 10.3163/1536-5050.104.3.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:1–10. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Buchanan N, Eyberg C, Davis MD. Isoniazid pharmacokinetics in kwashiorkor. South African Med J. 1979;56:299–300. [PubMed] [Google Scholar]
- 32.Seifart HI, Donald PR, De Villiers JN, Parkin DP, Jaarsveld PPHIS, et al. Isoniazid elimination kinetics in children with protein-energy malnutrition treated for tuberculous meningitis with a four-component antimicrobial regimen. Ann Trop Paediatr. 1995;15:249–254. doi: 10.1080/02724936.1995.11747780. [DOI] [PubMed] [Google Scholar]
- 33.Archary M, McLlleron H, Bobat R, La RP, Sibaya T, Wiesner L, et al. Population pharmacokinetics of lopinavir in severely malnourished HIV-infected children and the effect on treatment outcomes. Pediatr Infect Dis J. 2018;37:349–355. doi: 10.1097/INF.0000000000001867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Archary M, Mcllleron H, Bobat R, LaRussa P, Sibaya T, Wiesner L, et al. Population pharmacokinetics of abacavir and lamivudine in severely malnourished human immunodeficiency virus-infected children in relation to treatment outcomes. Br J Clin Pharmacol. 2019;85:2066–2075. doi: 10.1111/bcp.13998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization. Management of severe malnutrition: a manual for physicians and other senior health workers. 1999. https://apps.who.int/iris/bitstream/handle/10665/41999/a57361.pdf?sequence=1&isAllowed=y. Accessed 10 Nov 2020.
- 36.World Health Organization. Department of Nutrition for Health and Development. WHO Child Growth Standards. 2006. https://www.who.int/childgrowth/standards/Technical_report.pdf. Accessed 10 Nov 2020.
- 37.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Org. 2007;85:660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. Growth Charts - 2000 CDC Growth Charts. CDC.gov. 2017. https://www.cdc.gov/growthcharts/clinical_charts.htm. Accessed 10 Nov 2020.
- 39.Gernaat HBPE, Voorhoeve HWA. A new classification of acute protein-energy malnutrition. J Trop Pediatr. 2000;46:97–106. doi: 10.1093/tropej/46.2.97. [DOI] [PubMed] [Google Scholar]
- 40.Party WTW. Classification of infantile malnutrition. Lancet. 1970;2:302–303. [PubMed] [Google Scholar]
- 41.Khadilkar V, Khadilkar A, Choudhury P, Agarwal K, Ugra D, Shah NK. IAP growth monitoring guidelines for children from birth to 18 years. Indian Pediatr. 2007;44:187–197. [PubMed] [Google Scholar]
- 42.Voorhoeve H. A new reference for the mid-upper arm circumference? J Trop Pediatr. 1990;36:256–262. doi: 10.1093/tropej/36.5.256. [DOI] [PubMed] [Google Scholar]
- 43.Rao KS, Mukherjee NR, Rao KV. A survey of diabetes mellitus in a rural population of India. Diabetes. 1972;21:1192–1196. doi: 10.2337/diab.21.12.1192. [DOI] [PubMed] [Google Scholar]
- 44.Brantley RK, Williams KR, Silva TMJ, Sistrom M, Thielman NM, Ward H, et al. AIDS-associated diarrhea and wasting in Northeast Brazil is associated with subtherapeutic plasma levels of antiretroviral medications and with both bovine and human subtypes of Cryptosporidium parvum. Brazilian J Infect Dis. 2003;7:16–22. doi: 10.1590/s1413-86702003000100003. [DOI] [PubMed] [Google Scholar]
- 45.Mehta S. Malnutrition and drugs: clinical implications. Dev Pharmacol Ther. 1990;15:159–165. doi: 10.1159/000457640. [DOI] [PubMed] [Google Scholar]
- 46.de Kock M, Tarning J, Workman L, Allen EN, Tekete MM, Djimde AA, et al. Population pharmacokinetic properties of sulfadoxine and pyrimethamine: a pooled analysis to inform optimal dosing in african children with uncomplicated malaria. Antimicrob Agents Chemother. 2018;62:1–16. doi: 10.1128/AAC.01732-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chotsiri P, Denoeud-Ndam L, Baudin E, Guindo O, Diawara H, Attaher O, et al. Severe acute malnutrition results in lower lumefantrine exposure in children treated with artemether-lumefantrine for uncomplicated malaria. Clin Pharmacol Ther. 2019;106:1299–1309. doi: 10.1002/cpt.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bartelink IH, Savic RM, Dorsey G, Ruel T, Gingrich D, Scherpbier HJ, et al. The effect of malnutrition on the pharmacokinetics and virologic outcomes of lopinavir, efavirenz and nevirapine in food insecure HIV-infected children in Tororo. Uganda. Pediatr Infect Dis J. 2015;34:e63–70. doi: 10.1097/INF.0000000000000603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Trout H, Mentré F, Panhard X, Kodjo A, Escaut L, Pernet P, et al. Enhanced saquinavir exposure in human immunodeficiency virus type 1-infected patients with diarrhea and/or wasting syndrome. Antimicrob Agents Chemother. 2004;48:538–545. doi: 10.1128/AAC.48.2.538-545.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ellis JC, L’homme RFA, Ewings FM, Mulenga V, Bell F, Chileshe R, et al. Nevirapine concentrations in HIV-infected children treated with divided fixed-dose combination antiretroviral tablets in Malawi and Zambia. Antivir Ther. 2007;12:253–260. doi: 10.1177/135965350701200205. [DOI] [PubMed] [Google Scholar]
- 51.Schulz JD, Coulibaly JT, Schindler C, Wimmersberger D, Keiser J. Pharmacokinetics of ascending doses of ivermectin in Trichuris trichiura-infected children aged 2–12 years. J Antimicrob Chemother. 2019;74:1642–1647. doi: 10.1093/jac/dkz083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kadam P, Gogtay N, Karande S, Shah V, Thatte U. Evaluation of pharmacokinetics of single-dose chloroquine in malnourished children with malaria—a comparative study with normally nourished children. Indian J Pharmacol. 2016;48:498–502. doi: 10.4103/0253-7613.190720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vreeman RC, Nyandiko WM, Liechty EA, Busakhala N, Bartelink IH, Savic RM, et al. Impact of adherence and anthropometric characteristics on nevirapine pharmacokinetics and exposure among HIV-infected Kenyan children. J Acquir Immune Defic Syndr. 2014;67:277–286. doi: 10.1097/QAI.0000000000000300. [DOI] [PubMed] [Google Scholar]
- 54.Bolme R, Eriksson M, Habte D, Paalzow L. Pharmacokinetics of streptomycin in Ethiopian children with tuberculosis and of different nutritional status. J Clin Pharmacol. 1988;33:647–649. doi: 10.1007/BF00542504. [DOI] [PubMed] [Google Scholar]
- 55.Antwi S, Yang H, Enimil A, Sarfo AM, Gillani FS, Ansong D, et al. Pharmacokinetics of the first-line antituberculosis drugs in Ghanaian children with tuberculosis with or without HIV coinfection. Antimicrob Agents Chemother. 2017;61:1–8. doi: 10.1128/AAC.01701-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Heuberger J, Schmidt S, Derendorf H. When is protein binding important? J Pharm Sci. 2013;102:3458–3467. doi: 10.1002/jps.23559. [DOI] [PubMed] [Google Scholar]
- 57.Jagadeesan V, Krishnaswamy K. Drug binding in the undernourished: a study of the binding of propranolol to α1-acid glycoprotein. Eur J Clin Pharmacol. 1985;27:657–659. doi: 10.1007/BF00547044. [DOI] [PubMed] [Google Scholar]
- 58.Pussard E, Barennes H, Daouda H, Clavier F, Sani AM, Osse M, et al. Quinine disposition in globally malnourished children with cerebral malaria. Clin Pharmacol Ther. 1999;65:500–510. doi: 10.1016/S0009-9236(99)70069-X. [DOI] [PubMed] [Google Scholar]
- 59.Polasa K, Murthy K, Krishnaswamy K. Rifampicin kinetics in undernutrition. Br J Clin Pharmacol. 1984;17:481–484. doi: 10.1111/j.1365-2125.1984.tb02377.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gatti G, Di Biagio A, De Pascalis CR, Guerra M, Bassetti M, Bassetti D. Pharmacokinetics of rifabutin in HIV-infected patients with or without wasting syndrome. Br J Clin Pharmacol. 1999;48:704–711. doi: 10.1046/j.1365-2125.1999.00069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Holladay JW, Dewey MJ, Michniak BB, Wiltshire H, Halberg DL, Weigl P, et al. Elevated alpha-1-acid glycoprotein reduces the volume of distribution and systemic clearance of saquinavir. Drug Metab Dispos. 2001;29:299–303. [PubMed] [Google Scholar]
- 62.Bresnahan KA, Tanumihardjo SA. Undernutrition, the acute phase response to infection, and its effects on micronutrient status indicators. Adv Nutr. 2014;5:702–711. doi: 10.3945/an.114.006361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Oshikoya KA, Senbanjo IO. Caution when treating tuberculosis in malnourished children. Arch Dis Child. 2018;103:1101–1103. doi: 10.1136/archdischild-2018-314972. [DOI] [PubMed] [Google Scholar]
- 64.Zhang W, Parentau H, Greenly RL, Metz CA, Aggarwal S, Wainer IW, et al. Effect of protein-calorie malnutrition on cytochromes P450 and glutathione S-transferase. Eur J Drug Metab Pharmacokinet. 1999;24:141–147. doi: 10.1007/BF03190359. [DOI] [PubMed] [Google Scholar]
- 65.Garg S, Dhand R, Malik S, Kalra S, Gupta P, Jha V, et al. Single dose kinetics of rifampicin and isoniazid in well-nourished and malnourished patients of tuberculosis. J Clin Pharmacol Ther Toxicol. 1988;26:417–420. [PubMed] [Google Scholar]
- 66.Roy V, Gupta D, Gupta P, Sethi GR, Mishra TKVR, et al. Pharmacokinetics of isoniazid in moderately malnourished children with tuberculosis. Int J Tuberc Lung Dis. 2010;14:374–376. [PubMed] [Google Scholar]
- 67.Eriksson M, Bolme P, Habte D, Paalzow L. INH and streptomycin in Ethiopian children with tuberculosis and different nutritional status. Acta Paediatr Scand. 1988;77:890–894. doi: 10.1111/j.1651-2227.1988.tb10774.x. [DOI] [PubMed] [Google Scholar]
- 68.Fillekes Q, Kendall L, Kitaka S, Mugyenyi P, Musoke P, Ndigendawani M, et al. Pharmacokinetics of zidovudine dosed twice daily according to world health organization weight bands in Ugandan HIV-infected children. Pediatr Infect Dis J. 2014;33:495–498. doi: 10.1097/INF.0000000000000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wharton BA, McChesney EW. Chloroquine metabolism in kwashiorkor. J Trop Pediatr. 1970;16:130–32. [DOI] [PubMed]
- 70.Walker O, Dawodu A, Salako L, Alvan G, Johnson A. Single dose disposition of chloroquine in kwashiorkor and normal children-evidence for decreased absorption in kwashiorkor. Br J Clin Pharmacol. 1987;23:467–472. doi: 10.1111/j.1365-2125.1987.tb03077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dua VK, Gupta NC, Kar PK, Edwards G, Singh N, Sharma VP. Pharmacokinetics of chloroquine in Indian tribal and non-tribal healthy volunteers and patients with Plasmodium falciparum malaria. Curr Sci. 2002;83:1128–1131. [Google Scholar]
- 72.Salako L, Sowunmi A, Akinbami F. Pharmacokinetics of quinine in African children suffering from kwashiorkor. Br J Clin Pharmacol. 1989;28:197–201. doi: 10.1111/j.1365-2125.1989.tb05417.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mehta S. Drug Metabolism in the Malnourished Child. In: Suskind RM, Lewinter-Suskind MSS, editors. Malnourished child. Nestle nutrition workshop series. New York: Raven Press; 1990. pp. 329–338. [Google Scholar]
- 74.Tulpule A, Krishnaswamy K. Chloroquine kinetics in the undernourished. Eur J Clin Pharmacol. 1983;24:273–276. doi: 10.1007/BF00613831. [DOI] [PubMed] [Google Scholar]
- 75.Prasad J, Krishnaswamy K. Streptomycin pharmacokinetics in malnutrition. Chemotherapy. 1978;24:333–337. doi: 10.1159/000237803. [DOI] [PubMed] [Google Scholar]
- 76.Justine M, Yeconia A, Nicodemu I, Augustino D, Gratz J, Mduma E, et al. Pharmacokinetics of first-line drugs among children with tuberculosis in Rural Tanzania. J Pediatric Infect Dis Soc. 2020;9(1):14–20. doi: 10.1093/jpids/piy106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ramachandran G, Hemanth Kumar AK, Bhavani PK, Poorana Gangadevi N, Sekar L, Vijayasekaran D, et al. Age, nutritional status and INH acetylator status affect pharmacokinetics of anti-tuberculosis drugs in children. Int J Tuberc Lung Dis. 2013;17:800–806. doi: 10.5588/ijtld.12.0628. [DOI] [PubMed] [Google Scholar]
- 78.Verhagen LM, López D, Hermans PWM, Warris A, de Groot R, García JF, et al. Pharmacokinetics of anti-tuberculosis drugs in Venezuelan children younger than 16 years of age: Supportive evidence for the implementation of revised WHO dosing recommendations. Trop Med Int Health. 2012;17:1449–1456. doi: 10.1111/tmi.12003. [DOI] [PubMed] [Google Scholar]
- 79.Rogers Z, Hiruy H, Pasipanodya JG, Mbowane C, Adamson J, Ngotho L, et al. The non-linear child: ontogeny, isoniazid concentration, and NAT2 genotype modulate enzyme reaction kinetics and metabolism. EBioMedicine. 2016;11:118–126. doi: 10.1016/j.ebiom.2016.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.te Brake LHM, Ruslami R, Later-Nijland H, Mooren F, Teulen M, Apriani L, et al. Exposure to total and protein-unbound rifampin is not affected by malnutrition in Indonesian tuberculosis patients. Antimicrob Agents Chemother. 2015;59:3233–3239. doi: 10.1128/AAC.03485-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bartelink IH, Savic RM, Mwesigwa J, Achan J, Clark T, Plenty A, et al. Pharmacokinetics of lopinavir/ritonavir and efavirenz in food insecure HIV-infected pregnant and breastfeeding women in Tororo. Uganda. J Clin Pharmacol. 2014;54:121–132. doi: 10.1002/jcph.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.McIlleron H, Willemse M, Werely CJ, Hussey GD, Schaaf HS, Smith PJ, et al. Isoniazid plasma concentrations in a cohort of south african children with tuberculosis: implications for international pediatric dosing guidelines. Clin Infect Dis. 2009;48:1547–1553. doi: 10.1086/598192. [DOI] [PubMed] [Google Scholar]
- 83.Ramachandran G, Kumar AKH, Kannan T, Bhavani PK, Kumar SR, Gangadevi NP, et al. Low Serum concentrations of rifampicin and pyrazinamide associated with poor treatment outcomes in children with tuberculosis related to HIV status. Pediatr Infect Dis J. 2016;35:530–534. doi: 10.1097/INF.0000000000001069. [DOI] [PubMed] [Google Scholar]
- 84.Ramachandran G, Kupparam HKA, Vedhachalam C, Thiruvengadam K, Rajagandhi V, Dusthackeer A, et al. Factors influencing tuberculosis treatment outcome in adult patients treated with thrice-weekly regimens in India. Antimicrob Agents Chemother. 2017;61:1–12. doi: 10.1128/AAC.02464-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Williams PCM, Berkley JA. Guidelines for the treatment of severe acute malnutrition: a systematic review of the evidence for antimicrobial therapy. Paediatr Int Child Health. 2018;38:S32–49. doi: 10.1080/20469047.2017.1409453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dayal R, Singh Y, Agarwal D, Kumar M, Swaminathan S, Ramachandran G, et al. Pharmacokinetic study of isoniazid and pyrazinamide in children: Impact of age and nutritional status. Arch Dis Child. 2018;103:1150–1154. doi: 10.1136/archdischild-2017-313910. [DOI] [PubMed] [Google Scholar]
- 87.Thee S, Garcia-Prats AJ, Draper HR, McIlleron HM, Wiesner L, Castel S, et al. Pharmacokinetics and safety of moxifloxacin in children with multidrug-resistant tuberculosis. Clin Infect Dis. 2015;60:549–556. doi: 10.1093/cid/ciu868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Graham SM, Bell DJ, Nyirongo S, Hartkoorn R, Ward SA, Molyneux EM. Low levels of pyrazinamide and ethambutol in children with tuberculosis and impact of age, nutritional status, and human immunodeficiency virus infection. Antimicrob Agents Chemother. 2006;50:407–413. doi: 10.1128/AAC.50.2.407-413.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Garcia-Prats AJ, Draper HR, Thee S, Dooley KE, McIlleron HM, Seddon JA, et al. Pharmacokinetics and safety of ofloxacin in children with drug-resistant tuberculosis. Antimicrob Agents Chemother. 2015;59:6073–6079. doi: 10.1128/AAC.01404-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mukherjee A, Velpandian T, Singla M, Kanhiya K, Kabra SK, Lodha R. Pharmacokinetics of isoniazid, rifampicin, pyrazinamide and ethambutol in Indian children. BMC Infect Dis. 2015;15:1–11. doi: 10.1186/s12879-015-0862-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kumar AKH, Kumar A, Kannan T, Bhatia R, Agarwal D, Kumar S, et al. Pharmacokinetics of second-line antituberculosis drugs in children with multidrug-resistant tuberculosis in India. Antimicrob Agents Chemother. 2018;62:1–9. doi: 10.1128/AAC.02410-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pollock L, Else L, Poerksen G, Molyneux E, Moons P, Walker S, et al. Pharmacokinetics of nevirapine in HIV-infected children with and without malnutrition receiving divided adult fixed-dose combination tablets. J Antimicrob Chemother. 2009;64:1251–1259. doi: 10.1093/jac/dkp358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Worldwide Antimalarial Resistance Network (WWARN) Lumefantrine PK/PD Study Group Artemether-lumefantrine treatment of uncomplicated Plasmodium falciparum malaria: a systematic review and meta-analysis of day 7 lumefantrine concentrations and therapeutic response using individual patient data. BMC Med. 2015;13:227. doi: 10.1186/s12916-015-0456-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Palic S, Kip AE, Beijnen JH, Mbui J, Musa A, Solomos A, et al. Characterizing the non-linear pharmacokinetics of miltefosine in paediatric visceral leishmaniasis patients from Eastern Africa. J Antimicrob Chemother. 2020;75:3260–3268. doi: 10.1093/jac/dkaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.