Abstract
Objectives:
In this study, we examine associations between objectively measured weekend night versus school night sleep patterns, weight status, and weight-related behaviors among adolescents.
Design:
Cross-sectional study.
Setting:
Five Minnesota high schools that started early (7:30 or 7:45 am) in Spring 2016.
Participants:
Ninth grade students, ages 14.5 to 16 years (n=284).
Measurements:
Students completed surveys, had body measurements taken, and wore sleep (wrist) actigraphs for one week (n=284). We examined weekend night-school night differences in sleep duration and sleep timing. We then assessed whether these factors were related to weight status and weight-related behaviors (eating behaviors, food consumption, physical activity, beverage consumption) using generalized linear mixed models.
Results:
On average, students slept 1.5 hours (95% CI: 1.3–1.7) more and had a sleep midpoint 1.9 hours (1.8–2.1) later on weekend nights compared to school nights. Female students had larger increases in sleep duration on weekend nights than males but similar timing differences. Sleep duration differences were uncorrelated with sleep timing differences (r = −0.01). Neither duration or timing differences were associated with overweight, obesity, or any of the eating behaviors we examined. However, sleeping longer on weekend nights than on school nights was associated with lower probability of being active 6–7 days per week (p=0.02).
Conclusions:
Adolescents have substantial sleep duration and sleep timing differences on weekend nights versus school nights. While these differences may not be associated with weight status or weight-related behaviors, they reflect the reality that most adolescents have schedules that restrict their sleep.
Keywords: adolescents, sleep timing, sleep duration, school, weight, weight behaviors
INTRODUCTION
Early high school start times are a major contributor to inadequate sleep among adolescents in the United States (US).1 Although the American Academy of Sleep Medicine recommends that adolescents aged 13 to 18 get 8–10 hours of sleep per night,2 a majority of US high school students (68.9%) report getting under 8 hours of sleep.3 Developmental changes in sleep regulatory mechanisms as children transition to adolescents, including delays in the release of nocturnal melatonin, reset young people’s sleep-wake cycles such that they are approximately two hours later than their pre-pubescent sleep timing.4 Additionally, “sleep drive”, which is the opposing force to wakefulness that accumulates throughout the day, begins to build up more slowly in adolescence.5 These changes make it difficult for most adolescents to fall asleep before 11 pm or wake earlier than 8 am.6 Because high schools often start very early, they are at odds with adolescent circadian biology.4,6
A growing body of research suggests insufficient sleep is associated with increased risk of obesity in adolescents.7–9 Although longitudinal results have been mixed, two meta-analyses concluded that adolescents with shorter sleep duration have increased risk of overweight and obesity.10,11 Insufficient sleep may cause an energy imbalance that increases risk of obesity through multiple pathways. First, inadequate sleep may alter appetite as people choose more energy-dense and higher quantities of food when they are short on sleep.12,13 Second, insufficient sleep could increase sedentary behavior14 if a fatigued person’s activities are different from what they would be if they were well-rested. Third, lack of sleep may alter base metabolic rates.15 Among adults, adequate sleep duration is associated with maintenance of a healthy Mediterranean diet,16 and decreases in sleep duration are adversely associated with changes in diet and physical activity.17 Cross-sectionally, insufficient sleep among adolescents is associated with a variety of poor dietary outcomes including increased sugar-sweetened beverage consumption,9 decreased vegetable consumption,9 decreased breakfast eating,9 and lower dietary quality.18 Additionally, short sleep duration is associated with lower levels of physical activity.9
In addition to sleep duration, sleep timing has also been linked to weight status and weight-related behaviors. Adolescents with an evening preference have higher BMI,19 waist circumferences,20 and fat mass indices20 and report consuming more energy-dense, poor nutrition foods,19,21 eating fewer fruits and vegetables,19,22 drinking more soda,22 drinking more caffeinated beverages,21 and being less physically active.22 Additionally, children and adolescents with later school night bedtimes consume junk food more frequently than those who go to sleep before 9 pm,23 and students with later sleep midpoints on weekend nights have higher BMI z-scores and greater waist-to-height ratios.24
The association between suboptimal sleep and weight-related behaviors in adolescence may be explained by circadian disruptions caused by differences in school night and weekend night sleep. First, teens who endure sleep deprivation during the school week may catch-up by sleeping longer hours on the weekend.1,25 Catch-up sleep may offset some of the school week deficits but does not compensate for chronic sleep curtailment.26 Second, due to early high school start times, many teens must wake early on school days but are often more able to sleep according to their circadian timing and their sleep debt on weekends. In this situation, which is sometimes referred to as “social jet lag”, there will be a differential between the weekend night and school night sleep midpoint times. These weekend night-school night duration and timing differences could further contribute to circadian disruption of both sleep and eating behaviors, which can in turn contribute to excess body mass.27
Evidence on weekend night-school night sleep differences and weight among children and adolescents has been inconclusive.28 Some studies have found that sleeping longer on weekend nights than school nights is associated with increased risk of overweight/obesity,29 while others report a protective effect for longer weekend sleep30,31 or null findings.32 Some evidence suggests that later sleep timing on weekend nights is associated with increased BMI, higher fat mass index, and higher waist circumference in children and adolescents,20,24 but not all studies report an association between sleep timing differences and obesity.33 In addition to reporting conflicting findings, existing studies are subject to several limitations. First, only one study on weekend night-school night sleep differences has used objectively estimated sleep timing and duration.22 Second, few studies have examined weekend night-school night sleep duration differences and timing differences within the same sample. Third, while studies examining weight status are becoming more common, the association between weekend night-school night sleep differences and weight-related behaviors among adolescents remains limited.
In this study, we investigated the association of objectively measured weekend night-school night differences in sleep duration and sleep timing with adolescent weight status and weight-related behaviors. We hypothesize adolescents with large weekend night-school night sleep discrepancies are more likely to be overweight/obese and report less healthy weight-related behaviors.
PARTICIPANTS AND METHODS
The START study (n=2,134) followed a cohort of students (class of 2019) from five Minnesota high schools to evaluate impacts of modifying school start times.34 Prior to policy change (Baseline), when the cohort was in 9th grade, all five high schools started early, at either 7:30 or 7:45 am. Data for this cross-sectional analysis comes from a subsample of students at Baseline who were randomly selected to have their sleep measured by wrist actigraphy (n=284).
Study Population and Recruitment
All study procedures were reviewed and approved by the University of Minnesota Institutional Review Board (IRB) and the school districts’ research review panels. Letters describing the study, including its voluntary nature and instructions on opting out, were sent to the parents or guardians of all ninth-grade students at the five schools. Students who had not been opted out by their parents or guardians were provided information about the study and given the opportunity to assent to participating. In total, 90% of eligible students (2,134 students from the 2,362 students enumerated in school-provided lists), completed an in-school, self-administered Baseline survey that focused on sleep and weight-related behaviors.
Students were randomly selected, proportional to school size, to be invited to participate in a substudy where additional data were to be collected. For this substudy, parent/guardian consent was required, and students with parent/guardian consent then could assent to participate. A monetary incentive of $85 was offered each year to substudy participants who completed all additional procedures, including sleep actigraphy. The Baseline substudy had 284 participants (28% response proportion of those invited).34
Objective Sleep Data Collection and Processing
Substudy participants were instructed to wear an actigraph on their non-dominant wrist for at least 7 days. The actigraph devices (wGT3X-BT Monitor, ActiGraph, Pensacola, FL, USA) are small wristwatch-like accelerometers designed to capture data on movement, light, time spent sleeping versus awake, and sleeping patterns. In previous validation studies, data from wrist actigraphs correlated with data from polysomnography,35 the gold standard of objective sleep measurement. Substudy participants were also instructed to concurrently complete a sleep log which was used to cross-check the scoring of actigraphs.
After the completion of data collection, each student’s actigraph data and sleep log were sent to the Brigham Sleep Reading Center (SRC) in Boston, Massachusetts for processing. Actigraph data were scored using ActiLife version 6.13 analysis software (ActiGraph Corp, Pensacola, FL) using a validated algorithm.36 An analyst who was masked to student identity and all other study data then annotated the start and end of the main sleep period using the sleep logs combined with activity counts and light data from the actigraphs.
Sleep periods were categorized as occurring on weekend nights or school nights (nights that preceded a school day). Sleep periods that preceded days involving weather-related school cancelations or holidays were excluded from the sample. At one school, instruction began 30 minutes later on Wednesdays. To maintain consistency across schools, we excluded all sleep periods preceding Wednesdays.. Students had to have at least five days of actigraphy to be included in this analysis.
Sleep Measures
We characterized the average duration and timing of the main sleep period on both school nights and weekend nights. School night sleep duration was defined as the minutes between the average objectively recorded main sleep onset and offset on nights preceding a school day. Similarly, weekend night sleep duration was defined as the time between objectively measured average main sleep onset and offset on nights preceding a weekend day. Weekend night-school night sleep duration difference was defined as average weekend night sleep duration minus average school night sleep duration, so that a positive difference corresponds to longer sleep on weekend nights. To facilitate interpretation and allow for non-linear associations with our weight-related behavior outcomes, duration difference was then categorized into < −0.5 hours, ≥ −0.5 to < 0.5 hours, ≥ 0.5 to < 1.5 hours, ≥ 1.5 to < 2.5 hours, and ≥ 2.5 hours. The cutoffs for these categories were determined by the distribution of the data.
Sleep midpoint, which is defined as the clock time midway between objectively measured sleep onset and sleep offset, was used as an indicator of average sleep timing on school nights and weekend nights. Weekend night-school night timing difference was defined as average weekend night sleep midpoint minus average school night sleep midpoint. Classic social jet lag formulas take the absolute value of differences in sleep midpoint,37 but we decided not to include absolute value in order to differentiate between adolescents whose sleep timing was later on school nights and those whose timing was later on weekends. Though both groups are misaligned, these could be very distinct situations; since a week has five school nights and two weekend nights, students who have delayed sleep during the school week may have a greater proportion of the week where their sleep is misaligned. For our timing difference variable, positive values correspond to students whose average midpoint was later on weekend nights. Timing difference was then categorized into < 1 hours,≥ 1 to < 2 hours, ≥ 2 to < 3 hours, and ≥ 3 hours. As with the sleep duration difference measure, these cutoffs were determined based on the distribution of the data. Very few students had a negative difference, so we were unable to create a category specifically for earlier sleep timing on weekend nights.
Outcome Measures: Weight Status & Weight-Related Behaviors
Baseline survey questions were used to assess 10 outcomes corresponding to weight status, eating behaviors, food consumption, physical activity, and beverage consumption. We included two measures of weight status: BMI z-score at or above the 85th percentile (overweight) and BMI z-score at or above the 95th percentile (obese). Height and weight were used to calculate BMI z-scores, which were categorized according to CDC/NCHS growth curve data.38 Participant height and weight were measured twice by trained data collectors during the school day using a protocol adapted from Project EAT (Eating and Activity among Teens).34,39 Students received $2 for participating. Objectively measured average height and weight were used to calculate BMI when available. Subjective height and weight from the survey were used only in cases where the student was missing objective measurements (n=17).
Measures of eating behavior, which were adapted from Project EAT,40 included frequency of eating breakfast during a normal school week (5 days vs less often) and frequency of eating supper with family (5–7 days per week vs less often). Measures of food consumption, which were adapted from Project EAT and the Diet History Questionnaire (DHQ),41 included consuming fruit or vegetables other than potatoes (daily vs less often) and consuming fast food (weekly vs less often). Physical activity measures, which were adapted from Godin and Shepard,42 included days of physical activity (6–7 days per week vs less often) and hours of moderate or strenuous physical activity per week (≥ 7 hours or less). Measure of beverage consumption, also adapted from DHQ items,43 included mean times per day drinking sugar-sweetened beverages and mean times per day drinking caffeinated beverages.
Demographic Measures
Students were asked to report demographic items including age, sex (male, female), and racial/ethnic categorization (check all that apply: American Indian or Alaskan Native; Asian; Black, African, or African American; Hispanic or Latino/a; Native Hawaiian or other Pacific Islander; White or Caucasian; Something else). For this analysis, racial/ethnic categorization was collapsed into non-Hispanic white alone versus non-white and/or Hispanic due to the small proportion who identified as non-white (6%). Students were also asked to report the highest level of each parent’s or guardian’s education which was collapsed into at least one parent or guardian finished college versus no parent or guardian finished college. Finally, participants were asked whether they qualified for free or reduced-price lunch at school (yes, no, don’t know).
Statistical Analysis
We first calculated descriptive statistics for the sample, including school night sleep duration, weekend night sleep duration, weekend night-school night sleep duration difference, school night sleep midpoint, weekend night sleep midpoint, and weekend night-school night sleep timing difference. We also calculated the average sleep duration difference and average sleep timing difference by population subgroup (male vs female; non-Hispanic white vs Hispanic or nonwhite; free or reduced-price lunch eligible vs not eligible vs unknown).
We computed a set of regression models examining the association between weekend night-school night sleep duration difference and each outcome measure. We used generalized linear mixed models for categorical outcomes (eating behaviors, food consumption, physical activity, weight status) and estimated predicted probabilities of each outcome among students in each level of the sleep duration difference exposure. We used general linear mixed models for continuous outcomes (beverage consumption) and then estimated marginal means across levels of exposure. All models were adjusted for student age, sex, racial/ethnic categorization, and free/reduced lunch eligibility and included school as a random effect to account for nesting of students within schools. All categorical predictor variables were dummy coded in our regression models. Additionally, models examining BMI z-score as an outcome included an adjustment variable indicating whether objective or subjective measures were used. To verify that using subjective BMI for the small number of students (n=17) that did not have objective measures did not affect our results, we conducted a sensitivity analysis including only the subsample of students (n=267) with objective measures. The results of this sensitivity analysis (not shown) were comparable to the results of our primary analyses.
We then computed a second set of regression models with weekend night-school night sleep timing difference as the exposure. In an additional analysis, we ran a series of regression models that included both categorical duration difference and categorical timing difference.
We previously determined that missing data on objective sleep measures and covariates followed a missing-at-random pattern.44 Based on this determination, we used maximum likelihood estimation in our mixed-effects models. Maximum likelihood provides unbiased and asymptotically efficient estimates when data are missing at random. Cases were excluded on a variable-by-variable basis for each part of the analysis, resulting in a sample size of 224–233 for each model. Analyses were conducted using SAS version 9.4 (SAS/STAT, Inc., Cary, NC).
RESULTS
Our sample (n=284) was 15.2 years on average, 54.4% female, and 93.4% white (Table 1). More than 80% of students had a parent/guardian who had completed college, and 6.7% of the sample qualified for free or reduced lunch.
Table 1.
Demographics and sleep variables (n=284)
| Missing, na | na (%) or mean (sd) | |
|---|---|---|
| Age (in years) | 24 | 15.2 (0.3) |
| Sex | 23 | |
| Male | 119 (45.6%) | |
| Female | 142 (54.4%) | |
| Racial/ethnic categorization (check all that apply) | ||
| American Indian or Alaskan Native | 24 | 8 (3.1%) |
| Asian | 24 | 11 (4.2%) |
| Black, African, or African American | 24 | 10 (3.9%) |
| Hispanic or Latino/a | 19 | 8 (3.0%) |
| Native Hawaiian or other Pacific Islander | 24 | 2 (0.8%) |
| White or Caucasian | 24 | 244 (93.4%) |
| Something else | 24 | 2 (0.8%) |
| Parent education | 41 | |
| Finished college | 204 (84.0%) | |
| High school or some college | 39 (16.1%) | |
| Qualify for free or reduced-price lunch | 31 | |
| Yes | 17 (6.7%) | |
| No | 186 (73.5%) | |
| I don’t know | 50 (19.8%) | |
| School night sleep onset | 0 | 10:29 PM (52.7 min) |
| Weekend night sleep onset | 9 | 11:40 PM (80.6 min) |
| School night sleep offset | 0 | 6:15 AM (39.2 min) |
| Weekend night sleep offset | 9 | 8:53 AM (80.4 min) |
| School night sleep duration (hours) | 0 | 7.8 (1.0) |
| Weekend night sleep duration (hours) | 9 | 9.2 (1.3) |
| Weekend night-school night sleep duration differenceb, continuous (hours) | 9 | 1.5 (1.5) |
| Weekend night-school night sleep duration differenceb, categorical | 9 | |
| > 0.5 hours shorter on weekend nights | 19 (6.9%) | |
| 0.5 hours shorter to 0.5 hours longer on weekend nights | 48 (17.5%) | |
| 0.5–1.5 hours longer on weekend nights | 76 (27.6%) | |
| 1.5–2.5 hours longer on weekend nights | 67 (24.4%) | |
| >2.5 hours longer on weekend nights | 65 (23.6%) | |
| School night sleep midpoint | 0 | 2:22 AM (35.9 min) |
| Weekend night sleep midpoint | 9 | 4:17 AM (70.6 min) |
| Weekend night-school night sleep timing differencec, continuous (hours) | 9 | 1.9 (1.0) |
| Weekend night-school night sleep timing differencec, categorical | 9 | |
| < 1 hour later on weekend nights | 57 (20.7%) | |
| 1–2 hours later on weekend nights | 92 (33.5%) | |
| 2–3 hours later on weekend nights | 83 (30.2%) | |
| >3 hours later on weekend nights | 43 (15.6%) |
Min = minutes
Number of participants with missing values for that variable only.
Weekend night-school night sleep duration difference refers to the difference in weekend night and school night sleep duration (weekend night duration – school night duration), so that a positive difference corresponds to longer duration on weekend nights compared to school nights and a negative difference corresponds to a shorter duration on weekend nights.
Weekend night-school night sleep timing difference refers to the difference in weekend night and school night sleep timing (weekend night midpoint – school night midpoint), so that a positive difference corresponds to later midpoint on weekend nights than school nights and a negative difference corresponds to an earlier midpoint on weekend nights.
In this Baseline study, all students attended schools that started early, at either 7:30 or 7:45 am. On school nights, students fell asleep at approximately 10:29 pm and woke up at 6:15 am, getting an average of 7.8 hours of sleep. On weekend nights, students fell asleep at approximately 11:40 pm and work up at 8:53 am, getting an average of 9.2 hours of sleep. Most students slept longer on weekend nights than on school nights. However, 6.9% of students slept at least 30 minutes longer on school nights. Female students had larger weekend night-school night sleep duration differences on average compared to male students (Figure 1A).
Figure 1.
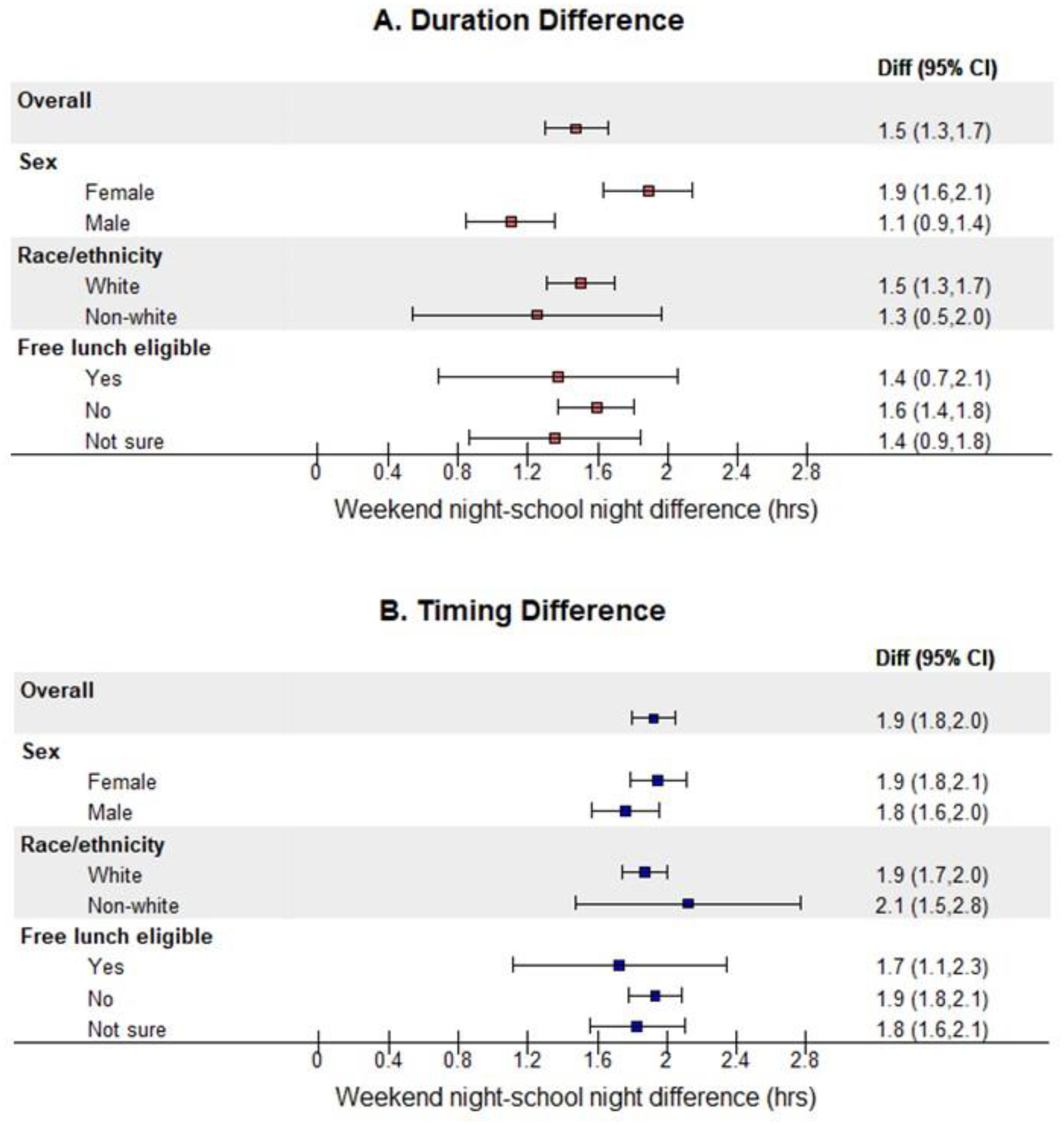
Weekend night-school night sleep (A) duration difference and (B) timing difference by subgroup
In Figure 1A, duration difference refers to the difference in weekend night and school night sleep duration (weekend night duration – school night duration), so that a positive difference corresponds to longer duration on the weekend. In Figure 1B, timing difference refers to the difference in weekend night and school night sleep timing (weekend night midpoint – school night midpoint), so that a positive difference corresponds to later midpoint on the weekend.
On average, students’ sleep midpoint occurred at 2:22 am on school nights (sd= 35.9 minutes) and 4:17 am on weekend nights (sd=70.6 minutes). There were no differences in timing difference by demographic sub-groups (Figure 1B) though our sample was predominately white and may be underpowered to detect differences. Most students had a weekend night sleep midpoint that was at least one hour later than on school nights (Table 1). Despite both measures assessing differences in weekend night-school night sleep patterns, sleep duration difference and sleep timing difference were not correlated (r=0.01).
Neither weekend night-school night duration difference nor timing difference was associated with weight status (Table 2–3). Students with larger increases in weekend night sleep duration compared with school night sleep duration were less likely to report being physically active 6–7 days per week; 28.9% of students who had a duration difference larger than 2.5 hours were physically active 6–7 days per week compared with 48.8% to 61.2% of students with a duration difference of < 2.5 hours (p=0.02). However, there were no other associations between sleep duration or timing differences and the weight-related behavioral outcomes that we examined. Regression models including both weekend night-school night sleep duration difference and sleep timing difference simultaneously had broadly similar results (Table 4).
Table 2.
Predicted probabilities of weight status and weight-related behaviors by weekend night-school night sleep duration difference
| Weekend Night-School Night Sleep Duration Differenceb | |||||||
|---|---|---|---|---|---|---|---|
| n | <−0.5 hours | ≥−0.5 to <0.5 hours | ≥0.5 to <1.5 hours | ≥1.5 to <2.5 hours | ≥2.5 hours | pa (df=4) | |
| Weight status | |||||||
| BMI z-score ≥85th percentilec | 224 | 15.3% | 15.5% | 11.6% | 11.8% | 18.3% | 0.73 |
| BMI z-score ≥95th percentilec | 224 | 9.7% | 12.5% | 6.4% | 4.3% | 16.1% | 0.20 |
| Eating behaviors | |||||||
| Eat breakfast 5 days/week | 225 | 43.5% | 51.2% | 29.4% | 79.7% | 73.7% | 0.32 |
| Eat supper with family 5–7 days a week | 228 | 57.8% | 52.9% | 51.6% | 54.6% | 54.9% | 0.99 |
| Food consumption | |||||||
| Fruit or vegetables daily | 228 | 72.4% | 69.7% | 62.2% | 72.2% | 70.2% | 0.78 |
| Fast food weekly | 227 | 69.7% | 71.5% | 65.4% | 72.7% | 63.5% | 0.82 |
| Physical activity | |||||||
| Active 6–7 days/week | 227 | 59.3% | 48.8% | 51.2% | 61.2% | 28.9% | 0.02 |
| Moderate-strenuous activity ≥7 hours/week | 227 | 75.4% | 41.1% | 43.5% | 45.8% | 30.7% | 0.09 |
| Beverage consumption (mean times/day) | |||||||
| Sugar-sweetened beverages | 228 | 1.5 | 1.3 | 1.1 | 1.4 | 1.2 | 0.81 |
| Caffeinated beverages | 228 | 0.5 | 0.3 | 0.5 | 0.8 | 0.6 | 0.36 |
BMI = body mass index; df = degrees of freedom
Bold text indicates p ≤0.05
Regression models adjusted for age, sex, free or reduced-price lunch eligibility, and racial/ethnic categorization (non-Hispanic white vs Hispanic or not white); school ID included as a random effect due to students nested within schools.
Weekend night-school night sleep duration difference refers to the difference in weekend night and school night sleep duration (weekend night duration – school night duration), so that a positive difference corresponds to longer duration on weekend nights compared to school nights and a negative difference corresponds to a shorter duration on weekend nights.
Objective height/weight data used when available.
Table 3.
Predicted probabilities of weight status and weight-related behaviors by weekend night-school night sleep timing difference
| Weekend Night-School Night Sleep Timing Differenceb | ||||||
|---|---|---|---|---|---|---|
| n | <1 hours | ≥1 to <2 hours | ≥2 to <3 hours | ≥3 hours | pa (df=3) | |
| Weight status | ||||||
| BMI z-score ≥85th percentilec | 224 | 15.6% | 18.0% | 10.7% | 18.2% | 0.49 |
| BMI z-score ≥95th percentilec,d | 233 | 10.0% | 9.1% | 4.8% | 15.2% | 0.26 |
| Eating behaviors | ||||||
| Eat breakfast 5 days/week | 225 | 63.8% | 53.3% | 58.8% | 57.4% | 0.72 |
| Eat supper with family 5–7 days a week | 228 | 59.0% | 54.6% | 58.3% | 39.4% | 0.32 |
| Food consumption | ||||||
| Fruit or vegetables daily | 228 | 72.5% | 66.2% | 72.2% | 66.3% | 0.78 |
| Fast food weekly | 227 | 61.9% | 67.6% | 72.3% | 71.1% | 0.67 |
| Physical activity | ||||||
| Active 6–7 days/week | 227 | 51.9% | 41.9% | 49.9% | 59.6% | 0.41 |
| Moderate-strenuous activity ≥7 hours/week | 227 | 49.1% | 34.6% | 45.4% | 55.2% | 0.18 |
| Beverage consumption (mean times/day) | ||||||
| Sugar-sweetened beverages | 228 | 1.4 | 1.2 | 1.2 | 1.4 | 0.93 |
| Caffeinated beverages | 228 | 0.4 | 0.6 | 0.4 | 0.7 | 0.53 |
BMI = body mass index; df = degrees of freedom
Bold text indicates p ≤0.05
Regression models adjusted for age, sex, free or reduced-price lunch eligibility, and racial/ethnic categorization (non-Hispanic white vs Hispanic or not white); school ID included as a random effect due to students nested within schools.
Weekend night-school night sleep timing difference refers to the difference in weekend night and school night sleep timing (weekend night midpoint – school night midpoint), so that a positive difference corresponds to later midpoint on weekend nights than school nights and a negative difference corresponds to an earlier midpoint on weekend nights.
Objective height/weight data used when available.
Model with 95th percentile BMI outcome not adjusted for free/reduced lunch eligibility due to convergence issues.
Table 4.
Predicted probabilities of weight status and weight-related behaviors, incorporating both weekend night-school night sleep duration difference and sleep timing difference into the same model
| Weekend Night-School Night Sleep Duration Differenceb | |||||||
|---|---|---|---|---|---|---|---|
| n | <−0.5 hours | ≥−0.5 to <0.5 hours | ≥0.5 to <1.5 hours | ≥1.5 to <2.5 hours | ≥2.5 hours | pa (df=4) | |
| Weight status | |||||||
| BMI z-score ≥85th percentiled | 224 | 15.8% | 16.2% | 11.9% | 12.1% | 19.1% | 0.72 |
| BMI z-score ≥95th percentiled,e | 233 | 6.9% | 11.1% | 6.2% | 3.6% | 15.7% | 0.13 |
| Eating behaviors | |||||||
| Eat breakfast 5 days/week | 225 | 37.2% | 59.1% | 64.3% | 56.1% | 48.1% | 0.31 |
| Eat supper with family 5–7 days a week | 228 | 61.9% | 53.2% | 49.8% | 52.6% | 55.0% | 0.96 |
| Food consumption | |||||||
| Fruit or vegetables daily | 228 | 73.1% | 70.1% | 62.5% | 72.7% | 70.9% | 0.76 |
| Fast food weekly | 227 | 68.7% | 71.5% | 65.5% | 72.3% | 62.3% | 0.80 |
| Physical activity | |||||||
| Active 6–7 days/week | 227 | 58.5% | 51.4% | 56.3% | 66.5% | 31.1% | 0.02 |
| Moderate-strenuous activity ≥7 hours/week | 227 | 74.8% | 44.2% | 47.4% | 50.9% | 33.2% | 0.11 |
| Beverage consumption (mean times/day) | |||||||
| Sugar-sweetened beverages | 228 | 1.5 | 1.4 | 1.2 | 1.5 | 1.2 | 0.81 |
| Caffeinated beverages | 228 | 0.5 | 0.3 | 0.5 | 0.8 | 0.6 | 0.34 |
| Weekend Night-School Night Sleep Timing Differenceb | |||||||
| n | <1 hours | ≥1 to <2 hours | ≥2 to <3 hours | ≥3 hours | pa (df=3) | ||
| Weight status | |||||||
| BMI z-score ≥85th percentiled | 224 | 15.4% | 17.8% | 10.3% | 16.8% | 0.48 | |
| BMI z-score ≥95th percentiled,e | 233 | 9.2% | 8.3% | 3.9% | 12.1% | 0.28 | |
| Eating behaviors | |||||||
| Eat breakfast 5 days/week | 225 | 57.2% | 46.7% | 53.1% | 55.0% | 0.72 | |
| Eat supper with family 5–7 days a week | 228 | 61.1% | 56.9% | 60.0% | 39.8% | 0.27 | |
| Food consumption | |||||||
| Fruit or vegetables daily | 228 | 73.5% | 66.9% | 72.8% | 66.4% | 0.75 | |
| Fast food weekly | 227 | 61.4% | 67.2% | 72.3% | 71.3% | 0.64 | |
| Physical activity | |||||||
| Active 6–7 days/week | 227 | 52.8% | 41.6% | 51.9% | 64.2% | 0.25 | |
| Moderate-strenuous activity ≥7 hours/week | 227 | 52.9% | 39.1% | 50.5% | 59.3% | 0.24 | |
| Beverage consumption (mean times/day) | |||||||
| Sugar-sweetened beverages | 228 | 1.4 | 1.3 | 1.3 | 1.4 | 0.84 | |
| Caffeinated beverages | 228 | 0.5 | 0.6 | 0.4 | 0.8 | 0.49 | |
BMI = body mass index; df = degrees of freedom
Bold text indicates p ≤0.05
Regression models include both the sleep duration and sleep timing predictor variables. Regression models adjusted for age, sex, free or reduced-price lunch eligibility, and racial/ethnic categorization (non-Hispanic white vs Hispanic or not white); school ID included as a random effect due to students nested within schools.
Weekend night-school night sleep duration difference refers to the difference in weekend night and school night sleep duration (weekend night duration – school night duration), so that a positive difference corresponds to longer duration on weekend nights compared to school nights and a negative difference corresponds to a shorter duration on weekend nights.
Weekend night-school night sleep timing difference refers to the difference in weekend night and school night sleep timing (weekend night midpoint – school night midpoint), so that a positive difference corresponds to later midpoint on weekend nights than school nights and a negative difference corresponds to an earlier midpoint on weekend nights
Objective height/weight data used when available.
Model with 95th percentile BMI outcome not adjusted for free/reduced lunch eligibility due to convergence issues.
Our primary analyses include our sleep difference measures as categorical predictors and our weight status and weight-related behaviors as dichotomous outcomes. Our analyses were robust to alternate model specifications including treating the sleep difference predictors as continuous (Table S1) and modeling the weight status, eating behavior, food consumption, and physical activity measures as ordinal or continuous (Table S2). These alternate models yielded results that were similar to the results presented in our primary tables (Tables 2–3). However, categorical sleep duration difference was significantly associated with days of physical activity when modeled as a dichotomous outcome (6–7 days/week vs less often) or as an ordinal outcome but not when modeled as a continuous outcome.
DISCUSSION
Adolescents in our sample, who all attended high schools with early start times (prior to 7:45 am), exhibited different patterns of objectively measured sleep on weekend nights compared with school nights. On average, students obtained nearly 1.5 hours more sleep on weekend nights than on school nights, while shifting the timing of their sleep nearly 2 hours later. Contrary to our hypotheses, weekend night-school night sleep duration and timing differences were not associated with various measures of weight status, eating behaviors, food consumption, or beverage consumption. However, sleeping longer on weekend nights was associated with reduced likelihood of being active 6–7 days per week.
Consistent with prior analyses,45,46 we found substantial differences between the sleep patterns of adolescents during school nights and weekend nights. Compared to male students, female students had larger increases in sleep duration on weekend nights but similar differences in sleep timing. Previous analyses of this sample suggest that female students have shorter sleep duration during the school week than male students.9 Therefore, female students may need to sleep longer on weekends than male students to catch up from their school week sleep deficit.
Weekend night-school night differences in sleep duration have previously been associated with poor academic performance28,47 and more depressive symptoms.28 Further, large weekend night-school night differences in sleep timing are associated with poor academic performance28,47 and higher levels of risk-taking behaviors.47 These prior findings suggest that large differences in weekend night-school night sleep patterns are concerning for adolescents even in the absence of an association with weight status or weight-related behaviors. These sleep differentials are likely driven by a variety of factors including short sleep duration on school nights that stems from early start times, over-commitment to extracurricular activities, homework, and jobs. Additionally, social pressures and screen use (social media, videos, gaming) also curtail adolescents’ sleep. As an example, in our sample, a very high proportion, 60% of participants, reported using screens before bed at least five nights a week and this likely has influence on sleep timing and duration. Further, interventions that promote sleep adequacy throughout the week and consistency could be important for equity if there are sub-group disparities in any of the negative outcomes that have been linked to weekend night-school night sleep differences.
We found that adolescents who slept at least 2.5 hours longer on the weekends were less likely to engage in physical activity 6–7 days per week. However, as this is a cross-sectional analysis, the directionality of the observed relationship is unclear. Students with large sleep duration differences could be too tired to participate in daily, or almost daily, physical activity. Alternatively, students who participate in organized weekend sports may not have sufficient time to sleep substantially longer on the weekends regardless of their level of sleep deficiency.
Weekend night-school night differences in sleep duration and timing did not appear to be associated with weight status or other weight related outcomes. Contrary to our null findings, a 2019 systematic review concluded that larger increases in sleep duration on weekend nights were correlated with decreased risk of overweight/obesity among children and adolescents.28
However, our study used objective sleep measures whereas all but one study included in the systematic review relied on subjective report of sleep patterns.28 Additionally, the protective effect of larger sleep duration differences was only observed in individual studies among children in Korea, Hong Kong, and China. Given that our study took place in the US and among older adolescents, our results on the association between sleep duration difference and BMI are more in line with studies on non-Asian youth, all but one of which also reported null results.
There are several potential explanations for our null findings. First, it is possible that weekend night-school night differences in sleep duration and sleep timing truly have no impact on weight status and weight-related behaviors or the impact is too small to be detected given our sample size. Perhaps longer-term sleep patterns play a larger role in weight-related behaviors than those characterized by metric of within-week sleep variability. A second possibility lies with the study’s design. Our cross-sectional observational study did not experimentally modify weekend night-school night sleep patterns, and therefore we do not know if reducing these differences could modify weight behaviors over time. Third, there may be heterogeneity among the types of adolescents that have either little or substantial weekend night-school night sleep differentials. For example, the group of students that have no or small differences in sleep duration could be composed of those who get sufficient sleep to meet metabolic and cognitive needs and do no need catch-up sleep on weekends. That group may also include adolescents who experienced short sleep during the week but do not have opportunity to catch up on weekends.
Our study was subject to several limitations. First, although we use objectively measured sleep, our weight-related behavioral outcomes are subjective. Second, our results may be subject to residual confounding by school-level factors and other measures. For instance, it is possible that a real association was masked by a quality that school populations share related both to sleep habits and weight-related behaviors. Third, the START sample was predominantly white and relatively affluent, limiting the generalizability of study findings. Additionally, the response proportion for the actigraphy substudy was low (28%), and students who participated in the substudy were more white and had higher SES than the full sample.
CONCLUSIONS
Adolescents who attend early starting schools have large increases in sleep duration and delays in sleep timing on weekend nights compared to school nights. Although we found little evidence of an association between weekend night-school night sleep differences and weight-related behaviors, large sleep differentials may still be cause for concern for the health and development of adolescents given prior data linking large weekend night-school night differences to poor academic performance, high risk-taking behavior, and increased depression.28,47 Policies that delay school start times, which match more closely with adolescent circadian rhythms have been shown to increase average sleep duration among adolescents44,45 and decrease weekend night-school night duration differences by reducing the need for catch-up sleep.44,48 The American Academy of Pediatrics recommends high schools start after 8:30 am,1 and many school districts are enacting delayed start policies. However, less than 15% of US high schools currently meet those guidelines, and 42% high schools start before 8:00 am.49 Implementing delayed start schedules that are more friendly to teen well-being should be a healthy youth development priority.
Supplementary Material
ACKNOWLEDGEMENTS
The Authors would like to thank the adolescents participating in the START study, the districts that welcomed us to do research in their schools, the START data collectors, and Bill Baker for his work to manage the data. Thank you to Kate Bauer for sharing your great ideas.
This study is supported by funding from the National Institutes of Health’s (NIH) Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) (R01 HD088176). Additionally, the authors gratefully acknowledge support from the Minnesota Population Center (MPC) and the MPC’s Population Health Training Program, which receive core funding (P2C HD041023 and T32 HD095134, respectively) from the Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD).
DECLARATION OF CONFLICTS OF INTEREST
Ms. Berry and Dr. Widome report grants from the Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD) during the conduct of the study. Dr. Redline reports consulting fees from Eisai Inc and Apnimed med and grant funding from Jazz Pharma-unrelated to this paper. The remaining authors have nothing to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing Interests: The authors declare no competing financial interests.
REFERENCES
- 1.Adolescent Sleep Working Group, Committe on Adolescence, Council on School Health. School Start Times for Adolescents. Pediatrics. 2014;134(3):642–649. doi: 10.1542/peds.2014-1697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paruthi S, Brooks LJ, D’Ambrosio C, et al. Consensus Statement of the American Academy of Sleep Medicine on the Recommended Amount of Sleep for Healthy Children: Methodology and Discussion. J Clin Sleep Med. 2016;12(11):1549–1561. doi: 10.5664/jcsm.6288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eaton DK, McKnight-Eily LR, Lowry R, Perry GS, Presley-Cantrell L, Croft JB. Prevalence of Insufficient, Borderline, and Optimal Hours of Sleep Among High School Students – United States, 2007. J Adolesc Heal. 2010;46(4):399–401. doi: 10.1016/j.jadohealth.2009.10.011 [DOI] [PubMed] [Google Scholar]
- 4.Frey S, Balu S, Greusing S, Rothen N, Cajochen C. Consequences of the Timing of Menarche on Female Adolescent Sleep Phase Preference. PLoS One. 2009;4(4):1–7. doi: 10.1371/journal.pone.0005217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taylor DJ, Jenni OG, Acebo C, Carskadon MA. Sleep tendency during extended wakefulness: Insights into adolescent sleep regulation and behavior. J Sleep Res. 2005;14(3):239–244. doi: 10.1111/j.1365-2869.2005.00467.x [DOI] [PubMed] [Google Scholar]
- 6.Carskadon M, Acebo C, Jenni OG. Regulation of Adolescent Sleep: Implications for Behavior. Ann N Y Acad Sci. 2004;1021(1):276–291. doi: 10.1196/annals.1308.032 [DOI] [PubMed] [Google Scholar]
- 7.Chen X, Beydoun MA, Wang Y. Is Sleep Duration Associated With Childhood Obesity? A Systematic Review and Meta-analysis. Obesity. 2008;16(2):265–274. doi: 10.1038/oby.2007.63 [DOI] [PubMed] [Google Scholar]
- 8.Garaulet M, Ortega FB, Ruiz JR, et al. Short sleep duration is associated with increased obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. Int J Obes. 2011;35(10):1308–1317. doi: 10.1038/ijo.2011.149 [DOI] [PubMed] [Google Scholar]
- 9.Widome R, Lenk KM, Laska MN, et al. Sleep Duration and Weight-Related Behaviors among Adolescents. Child Obes. 2019;15(7):434–442. doi: 10.1089/chi.2018.0362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fatima Y, Doi SAR, Mamun AA. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev. 2015;16(2):137–149. doi: 10.1111/obr.12245 [DOI] [PubMed] [Google Scholar]
- 11.Ruan H, Xun P, Cai W, He K, Tang Q. Habitual Sleep Duration and Risk of Childhood Obesity: Systematic Review and Dose-response Meta-analysis of Prospective Cohort Studies. Sci Rep. 2015;5(1):16160. doi: 10.1038/srep16160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beebe DW, Simon S, Summer S, Hemmer S, Strotman D, Dolan LM. Dietary Intake Following Experimentally Restricted Sleep in Adolescents. Sleep. 2013;36(6):827–834. doi: 10.5665/sleep.2704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simon SL, Field J, Miller LE, DiFrancesco M, Beebe DW. Sweet/Dessert Foods Are More Appealing to Adolescents after Sleep Restriction. Mistlberger RE, ed. PLoS One. 2015;10(2):e0115434. doi: 10.1371/journal.pone.0115434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Dyk TR, Krietsch KN, Saelens BE, Whitacre C, McAlister S, Beebe DW. Inducing more sleep on school nights reduces sedentary behavior without affecting physical activity in short-sleeping adolescents. Sleep Med. 2018;47:7–10. doi: 10.1016/j.sleep.2018.03.007 [DOI] [PubMed] [Google Scholar]
- 15.Adamantidis A, de Lecea L. Sleep and metabolism: shared circuits, new connections. Trends Endocrinol Metab. 2008;19(10):362–370. doi: 10.1016/j.tem.2008.08.007 [DOI] [PubMed] [Google Scholar]
- 16.Castro-Diehl C, Wood AC, Redline S, et al. Mediterranean diet pattern and sleep duration and insomnia symptoms in the Multi-Ethnic Study of Atherosclerosis. Sleep. 2018;41(11):1–10. doi: 10.1093/sleep/zsy158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cespedes EM, Bhupathiraju SN, Li Y, Rosner B, Redline S, Hu FB. Long-term changes in sleep duration, energy balance and risk of type 2 diabetes. Diabetologia. 2016;59(1):101–109. doi: 10.1007/s00125-015-3775-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bel S, Michels N, De Vriendt T, et al. Association between self-reported sleep duration and dietary quality in European adolescents. Br J Nutr. 2013;110(5):949–959. doi: 10.1017/S0007114512006046 [DOI] [PubMed] [Google Scholar]
- 19.Golley RK, Maher CA, Matricciani L, Olds TS. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes. 2013;37(4):546–551. doi: 10.1038/ijo.2012.212 [DOI] [PubMed] [Google Scholar]
- 20.Cespedes Feliciano EM, Rifas-Shiman SL, Quante M, Redline S, Oken E, Taveras EM. Chronotype, Social Jet Lag, and Cardiometabolic Risk Factors in Early Adolescence. JAMA Pediatr. 2019;173(11):1049–1057. doi: 10.1001/jamapediatrics.2019.3089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fleig D, Randler C. Association between chronotype and diet in adolescents based on food logs. Eat Behav. 2009;10(2):115–118. doi: 10.1016/j.eatbeh.2009.03.002 [DOI] [PubMed] [Google Scholar]
- 22.Malone SK, Zemel B, Compher C, et al. Characteristics Associated With Sleep Duration, Chronotype, and Social Jet Lag in Adolescents. J Sch Nurs. 2016;32(2):120–131. doi: 10.1177/1059840515603454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agostini A, Lushington K, Kohler M, Dorrian J. Associations between self-reported sleep measures and dietary behaviours in a large sample of Australian school students (n = 28,010). J Sleep Res. 2018;27(5). doi: 10.1111/jsr.12682 [DOI] [PubMed] [Google Scholar]
- 24.Malone SK, Zemel B, Compher C, et al. Social jet lag, chronotype and body mass index in 14–17-year-old adolescents. Chronobiol Int. 2016;33(9):1255–1266. doi: 10.1080/07420528.2016.1196697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wahlstrom KL, Dretzke BJ, Gordon MF, Peterson K, Edwards K, Gdula J. Examining the Impact of Later High School Start Times on the Health and Academic Performance of High School Students: A Multi-Site Study. 2014:72. https://conservancy.umn.edu/bitstream/handle/11299/162769/Impact of Later Start Time Final Report.pdf?sequence=1%0Ahttp://www.ccsdschools.com/Community/documents/ImpactofLaterStartTime.pdf. [Google Scholar]
- 26.Depner CM, Melanson EL, Eckel RH, et al. Ad libitum Weekend Recovery Sleep Fails to Prevent Metabolic Dysregulation during a Repeating Pattern of Insufficient Sleep and Weekend Recovery Sleep. Curr Biol. 2019;29(6):957–967.e4. doi: 10.1016/j.cub.2019.01.069 [DOI] [PubMed] [Google Scholar]
- 27.Roenneberg T, Allebrandt KV, Merrow M, Vetter C Social jetlag and obesity. Curr Biol. 2012;22(10):939–943. doi: 10.1016/j.cub.2012.03.038 [DOI] [PubMed] [Google Scholar]
- 28.Sun W, Ling J, Zhu X, Lee TMC, Li SX. Associations of weekday-to-weekend sleep differences with academic performance and health-related outcomes in school-age children and youths. Sleep Med Rev. 2019;46:27–53. doi: 10.1016/j.smrv.2019.04.003 [DOI] [PubMed] [Google Scholar]
- 29.Paiva T, Gaspar T, Matos MG. Sleep deprivation in adolescents: correlations with health complaints and health-related quality of life. Sleep Med. 2015;16(4):521–527. doi: 10.1016/j.sleep.2014.10.010 [DOI] [PubMed] [Google Scholar]
- 30.Lee BH, Kang S-G, Choi J-W, Lee YJ. The Association between Self-reported Sleep Duration and Body Mass Index among Korean Adolescents. J Korean Med Sci. 2016;31(12):1996. doi: 10.3346/jkms.2016.31.12.1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chung K-F, Kan KK-K, Yeung W-F. Sleep duration, sleep–wake schedule regularity, and body weight in Hong Kong Chinese adolescents. Biol Rhythm Res. 2013;44(2):169–179. doi: 10.1080/09291016.2012.656247 [DOI] [Google Scholar]
- 32.Quan S, Combs D, Parthasarathy S. Impact of sleep duration and weekend oversleep on body weight and blood pressure in adolescents. Southwest J Pulm Crit Care. 2018;16(1):31–41. doi: 10.13175/swjpcc150-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schneider AC, Zhang D, Xiao Q. Adolescent sleep characteristics and body-mass index in the Family Life, Activity, Sun, Health, and Eating (FLASHE) Study. Sci Rep. 2020;10(1):1–10. doi: 10.1038/s41598-020-70193-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Widome R, Wahlstrom KL, Laska MN, et al. The START study: An evaluation to study the impact of a natural experiment in high school start times on adolescent weight and related behaviors. Obs Stud. 2020;6:66–86. [PMC free article] [PubMed] [Google Scholar]
- 35.Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The Role of Actigraphy in the Study of Sleep and Circadian Rhythms. Sleep. 2003;26(3):342–392. doi: 10.1093/sleep/26.3.342 [DOI] [PubMed] [Google Scholar]
- 36.Cole RJ, Kripke DF, Gruen W, Mullaney DJ, Gillin JC. Automatic Sleep/Wake Identification From Wrist Activity. Sleep. 1992;15(5):461–469. doi: 10.1093/sleep/15.5.461 [DOI] [PubMed] [Google Scholar]
- 37.Roenneberg T, Kuehnle T, Pramstaller PP, et al. A marker for the end of adolescence. Curr Biol. 2004;14(24):1038–1039. doi: 10.1016/j.cub.2004.11.039 [DOI] [PubMed] [Google Scholar]
- 38.CDC Growth Charts. Centers for Disease Control and Prevention. https://www.cdc.gov/growthcharts/cdc_charts.htm. Accessed June 26, 2020.
- 39.Neumark-Sztainer D, Story M, Hannan PJ, Croll J. Overweight status and eating patterns among adolescents: Where do youths stand in comparison with the Healthy People 2010 objectives? Am J Public Health. 2002;92(5):844–851. doi: 10.2105/AJPH.92.5.844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Neumark-Sztainer D, Wall M, Perry C, Story M. Correlates of fruit and vegetable intake among adolescents: Findings from Project EAT. Prev Med (Baltim). 2003;37(3):198–208. doi: 10.1016/S0091-7435(03)00114-2 [DOI] [PubMed] [Google Scholar]
- 41.French SA, Story M, Neumark-Sztainer D, Fulkerson JA, Hannan P. Fast food restaurant use among adolescents: Associations with nutrient intake, food choices and behavioral and psychosocial variables. Int J Obes. 2001;25(12):1823–1833. doi: 10.1038/sj.ijo.0801820 [DOI] [PubMed] [Google Scholar]
- 42.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10(3):141–146. http://www.ncbi.nlm.nih.gov/pubmed/4053261. [PubMed] [Google Scholar]
- 43.NIH. Diet History Questionnaire II.; 2018. https://epi.grants.cancer.gov/dhq2/forms/dhq2_pastyear.pdf.
- 44.Widome R, Berger AT, Iber C, et al. Association of Delaying School Start Time With Sleep Duration, Timing, and Quality Among Adolescents. JAMA Pediatr. 2020;55454. doi: 10.1001/jamapediatrics.2020.0344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Boergers J, Gable CJ, Owens JA. Later school start time is associated with improved sleep and daytime functioning in adolescents. J Dev Behav Pediatr. 2014;35(1):11–17. doi: 10.1097/DBP.0000000000000018 [DOI] [PubMed] [Google Scholar]
- 46.Paksarian D, Rudolph KE, He JP, Merikangas KR. School start time and adolescent sleep patterns: Results from the US National Comorbidity Survey-adolescent supplement. Am J Public Health. 2015;105(7):1351–1357. doi: 10.2105/AJPH.2015.302619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.O’Brien EM, Mindell JA. Sleep and Risk-Taking Behavior in Adolescents. Behav Sleep Med. 2005;3(3):113–133. doi: 10.1207/s15402010bsm0303_1 [DOI] [PubMed] [Google Scholar]
- 48.Owens JA, Dearth-Wesley T, Herman AN, Oakes JM, Whitaker RC. A quasi-experimental study of the impact of school start time changes on adolescent sleep. Sleep Heal. 2017;3(6):437–443. doi: 10.1016/j.sleh.2017.09.001 [DOI] [PubMed] [Google Scholar]
- 49.Wheaton AG, Ferro GA, Croft JB. School Start Times for Middle School and High School Students — United States, 2011–12 School Year. MMWR Morb Mortal Wkly Rep. 2015;64(30):809–813. doi: 10.15585/mmwr.mm6430a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


