Abstract
Background
No report has yet described good prognosis following the induced membrane technique (IMT) for bone defects over 200 mm.
Case presentation
A 46-year-old male developed osteomyelitis over a large portion of the right femoral diaphysis, which had an unknown infection route, and subtrochanteric fracture during the waiting period of the planed IMT. Around 3 days after the pathological fracture, the first stage was performed. Aggressive debridement resulted in large segmental bone defect, which was treated with internal fixation using intramedullary nailing and insertion of an antibiotic-impregnated polymethylmethacrylate (PMMA) spacer. Postoperative radiographs showed a radiographic apparent bone gap of 221 mm. A subsequent culture of the debrided bone test identified Corynebacterium as the causative organism, with blood examination indicating normal C-reactive protein, white blood cell count, and erythrocyte sedimentation rate following 4 weeks of intravenous antibiotic administration. Around 7 weeks after the first stage, the second stage was initiated. After removing the PMMA spacer, grafting was performed by filling the bone defect with a combination of autologous cancellous bone harvested from the posterior iliac crest and β-tricalcium phosphate (β-TCP), which were mixed in approximately equal proportions. Routine postoperative radiographs confirmed a sequential healing process and callus formation in three out of four cortices 3 years after surgery.
Conclusions
In the present case, IMT was able to successfully treat the osteomyelitis-induced large segmental bone defect of the femoral shaft exceeding 200 mm. Had autologous cancellous bone alone been applied during the second stage, the possible amount of bone defect covered by the IMT would have been limited. However, this limitation can be addressed by applying β-TCP. Further expansion of IMT indications may help address challenges in the treatment of extensive bone defects.
Keywords: Induced membrane technique, Osteomyelitis, Autologous cancellous bone, β-Tricalcium phosphate
Introduction
The induced membrane technique (IMT), first introduced by Masquelet et al., has been one of the reconstructive procedures employed for segmental bone defects due to trauma, infection, and tumors [1], [2], [3]. IMT consists of two stages, the first of which includes aggressive resection of necrotic and infected tissue and placement of a temporary polymethylmethacrylate (PMMA) spacer, which subsequently induces the formation of a bioactive membrane. Meanwhile, the second stage involves the removal of the PMMA spacer and autologous cancellous bone grafting after confirming the elimination of infection [1], [2], [3]. Recent clinical evidence has confirmed the effectiveness of the IMT for segmental bone defect reconstruction in long bones; however, no report has yet described good prognosis following the IMT for the bone defects over 200 mm [4], [5], [6].
This case report describes a case involving a middle-aged man with osteomyelitis over a large portion of the right femoral diaphysis. Our experience suggests the potential availability of the IMT method for extensive osteomyelitis of long bones, which has not been applied in all cases.
Case report
Written informed consent for publishing this case report, including the images, was obtained from the patient.
A 46-year-old male was admitted to the gastrointestinal medicine department of our institute due to persistent abdominal pain and fever over 38 °C for 3 weeks. The patient also had severe right thigh pain for 1 week without a history of trauma and could not walk without a crutch. He had been diagnosed with diabetes mellitus (HbA1c: 6.9%), which had been left untreated. Blood examination indicated elevated white blood cell (WBC) count (18,800/μL) and C-reactive protein (CRP) (20.8 mg/dL). Radiological findings revealed a liver abscess, with immediate percutaneous drainage identifying Klebsiella pneumoniae as the causative bacteria. Intravenous administration of the antibacterial meropenem (3 g daily) for 2 weeks improved his abdominal symptoms. However, given that the pain in his right thigh persisted, he was referred to our department for further examination and treatment. The range of motion in the patient's hip and knee joints was restricted, while tenderness and localized heat were observed on his thigh. Radiological examinations, including plain radiographs, computed tomography, and magnetic resonance imaging, indicated osteomyelitis of the right femur (Fig. 1A–C). The patient had no significant medical or family history, and additional detailed examination revealed no potential immunodeficiency. We instructed the patient to maintain strict non-weightbearing with double crutches and planned to perform the IMT. During this waiting period, he fell and sustained a femoral subtrochanteric fracture (Fig. 1D). Around 3 days after the injury, the first stage of the IMT was initiated.
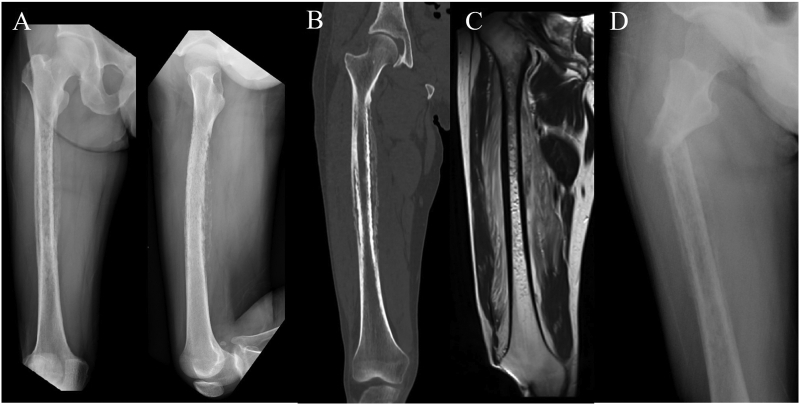
Fig. 1.
Anteroposterior and lateral radiographs showing widespread irregularity of the medullary canal at the shaft accompanied by periosteal reaction (A). Coronal computed tomography showing the same findings as radiography (B). Coronal magnetic resonance imaging showing side spread signal change of the medullary canal at the shaft and surrounding soft tissues (C).
Surgery was performed under general anesthesia with the patient in the left lateral position. The affected bone was exposed through a long longitudinal incision in the lateral portion of the femur, followed by aggressive debridement of abnormal bone and surrounding soft tissue. Guided by confirmation of bleeding from the proximal and distal portions of the remaining femur, debridement resulted in a significant large segmental bone defect with a final size of approximately 20 cm (Fig. 2A). After antegrade intramedullary nailing was conducted to stabilize the proximal and distal fragments, the bone defect was filled with an antibiotic-impregnated polymethylmethacrylate (PMMA) spacer comprising 2 g of vancomycin powder and 40 g of PMMA (Cemex® RX; Tecres Corp., Verona, Italy). A small amount of indigocarmine was applied to color the spacer for ease of differentiation from normal bone and for the preparation of the second stage (Fig. 2B). The radiological examination after the first stage revealed a radiographic apparent bone gap of 221 mm (Fig. 2C). Culture of the debrided bone identified Corynebacterium as the causative organism, for which linezolid (600 mg twice daily for 3 days), followed by daptomycin (8 mg/kg once daily), was administered intravenously. This protocol had continued until 4 weeks after the first stage, with subsequent blood examination indicating normal CRP, WBC count, and erythrocyte sedimentation rate.
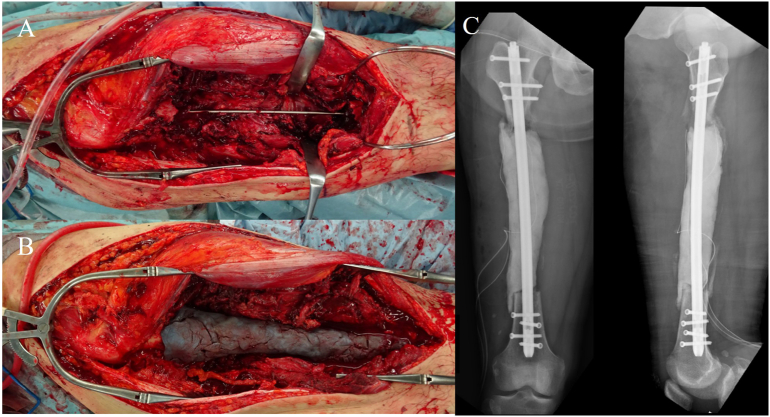
Fig. 2.
Intraoperative images at the first stage showing extensive segmental bone defect with a size of approximately 20 cm of after aggressive debridement (A) and an inserted antibiotic-impregnated polymethylmethacrylate (PMMA) spacer into the large bone defect (B). Postoperative radiographs showing a radiographic apparent bone gap of 221 mm (C).
Around 7 weeks after the first stage, the second stage procedure was conducted under general anesthesia with the patient positioned prone. After harvesting cancellous bone from the bilateral posterior iliac crest, the patient's position was changed to the left semi-lateral position, and the femoral shaft was exposed through the same approach as the first stage procedure. After the colored PMMA spacer was removed, the bone defect was filled with the graft consisting of approximately equal proportions of harvested autologous cancellous bone and β-tricalcium phosphate (TCP) (OSferion, Olympus Terumo Biomaterials Corp, Tokyo, Japan) (Fig. 3).
Fig. 3.
Intraoperative images at the second stage showing induced membrane (A), mixed autograft and β-TCP in approximately equal proportions (B), and grafting (C).
After the surgery, non-weightbearing was continued for 4 weeks, after which 1/3 partial weightbearing was allowed. Around 3 months after the second stage, 2/3 partial weightbearing was allowed, and full weightbearing was achieved at 4 months. The patient was able to initially return to work 6 months after the second stage. Fig. 4 showed a sequential healing process after the second stage. Radiographs 3 years after the surgery revealed callus formation in three out of four cortices (Fig. 5).
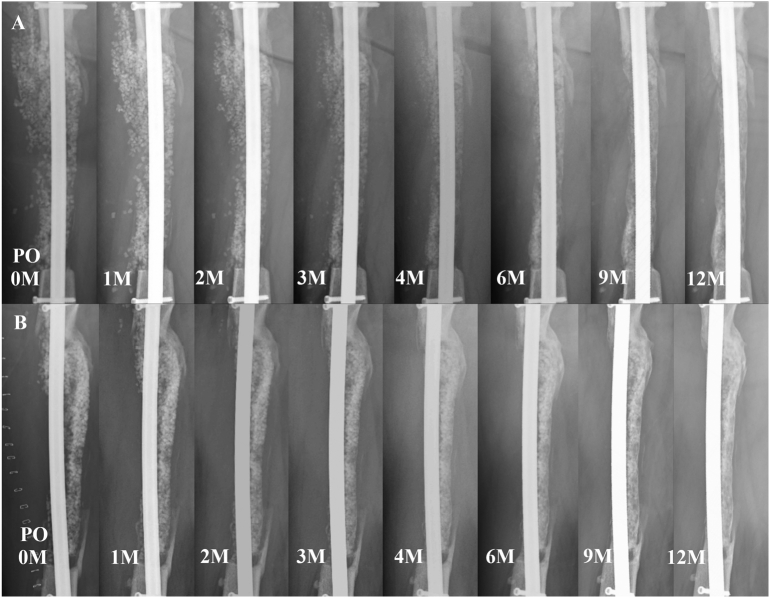
Fig. 4.
Sequential anteroposterior (A) and lateral (B) radiographs showing gradual healing progression after the second stage.
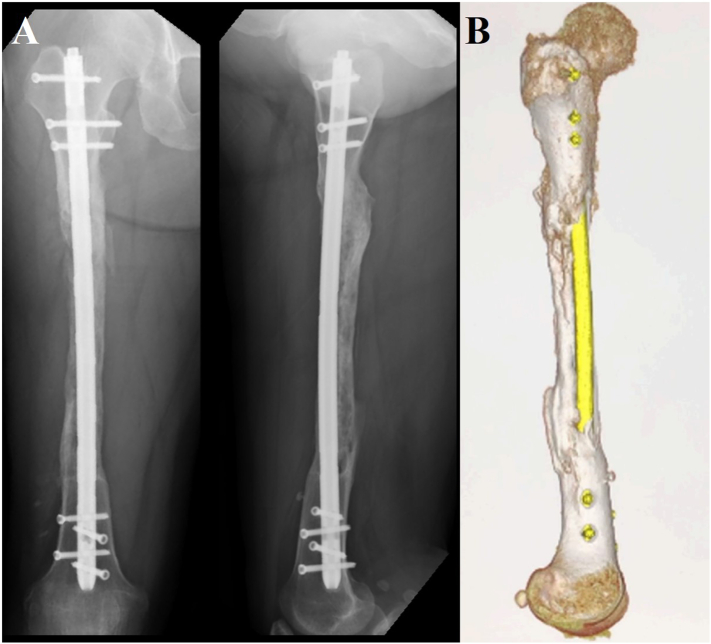
Fig. 5.
Anteroposterior and lateral radiographs (A) and 3D-computed tomography (B) at 3 years after surgery showing callus formation in three out of four cortices.
Discussion
In 1986, Masquelet et al. introduced the IMT as a reconstructive procedure for the segmental bone defect resulting from trauma, infection, and tumors. Following the publication of the original paper, several case series had confirmed the effectiveness of the IMT [1], [4], [5], [6]. However, to the best of our knowledge, no report has described successful reconstruction using the IMT for large segmental bone defects of over 20 cm in the long bones of the lower extremities. The critical concern for applying the IMT for large bone defects has been the limited amount of autograft harvested from the iliac crest, which may be insufficient to fill the defect due to adequate debridement of the infected bone. To address this problem, we introduced the application of β-TCP, which can be used as an extender by mixing it with autograft in approximately equal proportions [7], [8]. In the present case, plain radiographs indicated successfully callus formation in three out of four cortices. Another concern related to the use of the IMT for large bone defects in the femur has been the strength of reconstructive bone. A biomechanical study by Johnson and Tencer reported that intramedullary nail fixation of femoral shaft fractures with locking bolts can be expected to have approximately 75% of the intact femur's rigidity during bending and can support approximately 400% of a normal body weight (70 kg) [9]. Additionally, the patient did not experience re-fracturing despite his physically demanding work. Based on the aforementioned findings, we believe that the reconstructed femoral shaft had sufficient strength.
Further application of the IMT for the reconstruction of large bone defects may aid research on the indications and development of biologics. In the present case, β-TCP was mixed with autograft in approximately equal proportions. Had the proportion of β-TCP been greater, larger-sized bony defects could have been treated. The IMT can be thus be considered for treating large segmental bone defects.
Funding
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board of the authors' institution and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Declaration of competing interest
We have no conflict of interest.
Acknowledgements
No acknowledgement.
References
- 1.Masquelet A.C., Fitoussi F., Begue T., Muller G.P. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann. Chir. Plast. Esthet. 2000;45:346–353. [PubMed] [Google Scholar]
- 2.Giannoudis P.V., Faour O., Goff T., Kanakaris N.K., Dimitriou R. Masquelet technique for the treatment of bone defects: tips-tricks and future directions. Injury. 2011;42:591–598. doi: 10.1016/j.injury.2011.03.036. [DOI] [PubMed] [Google Scholar]
- 3.Masquelet A.C. The evolution of the induced membrane technique: current status and future directions. Tech. Orthop. 2016;31:3–8. [Google Scholar]
- 4.Giannoudisa P.V., Gudipatia S., Harwooda P., Kanakaris N.K. Long bone non-unions treated with the diamond concept: a case series of 64 patients. Injury. 2015;46:S48–S54. doi: 10.1016/S0020-1383(15)30055-3. [DOI] [PubMed] [Google Scholar]
- 5.Giotikas D., Tarazi N., Spalding L., Nabergoj M., Krkovic M. Results of the induced membrane technique in the management of traumatic bone loss in the lower limb: a cohort study. J. Orthop. Trauma. 2019;33:131–136. doi: 10.1097/BOT.0000000000001384. [DOI] [PubMed] [Google Scholar]
- 6.Wang J., Yin Q., Gu S., Wu Y., Rui Y. Induced membrane technique in the treatment of infectious bone defect: a clinical analysis. 2019;105:535–539. doi: 10.1016/j.otsr.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 7.Sasaki G., Watanabe Y., Miyamoto W., Yasui Y., Morimoto S., Kawano H. Induced membrane technique using beta-tricalcium phosphate for reconstruction of femoral and tibial segmental bone loss due to infection: technical tips and preliminary clinical results. Int. Orthop. 2018;42:17–24. doi: 10.1007/s00264-017-3503-5. [DOI] [PubMed] [Google Scholar]
- 8.Sasaki G., Watanabe Y., Yasui Y. Clinical and radiological assessment of the induced membrane technique using beta-tricalcium phosphate in reconstructive surgery for lower extremity long bone defects. Bone Joint J. 2021;103-B:456–461. doi: 10.1302/0301-620X.103B3.BJJ-2020-1542.R1. [DOI] [PubMed] [Google Scholar]
- 9.Johnson K.D., Tencer A. Mechanics of intramedullary nails for femoral fractures. Unfallchirurg. 1990;93:506–511. [PubMed] [Google Scholar]