Abstract
Objective
On-pump beating heart (OP-BH) coronary artery bypass grafting (CABG) is often undertaken as an alternative between off-pump coronary artery bypass (OPCAB) and conventional on-pump coronary artery bypass grafting (On-pump CABG), especially in India. However, outcome data following OP-BH surgery is sparse. The aim of this study was to compare the outcomes of OP-BH CABG with OPCAB.
Methods
From our institutional database, all patients undergoing OP-BH CABG (n = 531) were identified. A propensity-matched cohort undergoing OPCAB (n = 531) was identified from the database. Nearest neighbor matching technique was used and the groups were matched for variables including age, gender, body mass index, EuroSCORE, history of recent myocardial infarction or unstable angina, hypertension, peripheral vascular disease, chronic obstructive airway disease, diabetes, pre-op renal impairment, pre-op neurological events, and left ventricular function.
Results
The propensity-matched groups were well matched in terms of baseline characteristics. The mean EuroSCORE was 3.17 and 3.20 in the OP-BH and the OPCAB groups. The unadjusted 30-day mortality in the propensity-matched OPCAB group was 2.07% (11/531) while mortality in the on-pump beating heart group was significantly higher at 6.9% (37/531). Multivariate analysis showed that OP-BH CABG was an independent risk factor for 30-day mortality as well as major adverse post-operative outcomes including renal, neurological, and respiratory outcomes and post-operative atrial fibrillation.
Conclusions
OP-BH CABG is associated with worse clinical outcomes compared to patients undergoing OPCAB.
Keywords: On-pump beating heart, OPCAB, CABG
Introduction
On-pump beating heart surgery (OP-BH) has attracted the interest of coronary surgeons in the last couple of decades. Unlike conventional on-pump coronary artery bypass grafting (On-pump CABG) which utilizes both cardiopulmonary bypass (CPB) as well as cardioplegic arrest and off-pump coronary artery bypass (OPCAB) which utilizes neither, OP-BH uses CPB but not cardioplegic arrest. Thus, it is often considered to be an intermediate strategy between OPCAB and On-pump CABG for myocardial revascularization.
The technique is occasionally used in high-risk situations like after a recent myocardial infarction (MI) or acute coronary syndrome (ACS), during emergency surgery or in patients with impaired left ventricular function. It has also been used as a bridge for training of coronary surgeons wishing to make a transition from On-pump CABG to OPCAB as well as by junior trainees.
Despite the technique being in vogue for almost 2 decades, outcome data is sparse with conflicting reports in the literature. While some studies have shown lower in-hospital mortality in the OP-BH group, others have reported no mortality benefit between OP-BH and conventional On-pump CABG [1–5]. Yet others have concluded that while the 30-day mortality was similar, incidence of new irreversible myocardial injury in the OP-BH patients was significantly higher [6].
However, it has to be noted that OP-BH has mostly been compared to conventional on-pump technique and rarely with OPCAB. The outcome data emerging out of these comparisons have also been influenced adversely by the heterogeneity of study population as well as by small sample sizes. There have been only two randomized control trials (RCT) and one propensity-matched comparison on the subject all of which compared OP-BH with conventional On-pump CABG [1, 2, 6]. Until date, there have been no RCT comparing OP-BH and OPCAB. There has been only a single prospective study [7], with the rest of the evidence made available from retrospective studies of varying sizes and research questions [5, 8–15].
In the Indian scenario, where over 60% of myocardial revascularizations are performed using the OPCAB technique, it is more relevant to compare the outcomes of OP-BH surgery with OPCAB. We carried out this propensity-matched comparison between OP-BH and OPCAB to address this important lacuna in literature.
Material and methods
This study is a propensity-matched comparison of patients undergoing OP-BH (n = 531) at our institution. The study period extended from 2011 to 2019. The total number of patients undergoing CABG during this time period was 10,572. Of these, 531 (5.02%) were carried out using the OP-BH technique and 10,041 (94.9%) were operated using the OPCAB technique. The patients undergoing OP-BH (n = 531) were then matched with patients undergoing OPCAB (n = 10,041) during the same period using propensity matching.
The aim of the study was to compare OP-BH with OPCAB in propensity-matched cohorts. The objective of the study was to assess if OP-BH is an independent risk factor for adverse outcome following coronary artery bypass grafting. The primary outcome was 30-day all-cause mortality. Secondary outcome was post-operative morbidity and included atrial fibrillation; respiratory, renal, neurological, and cardiovascular complications; sternal dehiscence; and deep sternal wound infections (DSWI).
All patients undergoing isolated primary CABG using the OPCAB or OP-BH technique were included in the study. Patients undergoing combined procedures or those below the age of 18 years were excluded from the study.
Anesthetic techniques
A standard anesthetic technique was used throughout the study period, with short-acting, easily reversible agents for induction and volatile agents for maintenance. All patients received sedative premedication.
Surgical techniques
All operations were performed by cardiac surgeons with significant experience in OPCAB surgery. During both OPCAB and OP-BH procedures, the Octopus stabiliser (Octopus Device, Medtronic, Minneapolis, MN) was used for stabilization of the target coronary artery along with Star fish apical stabilization device. In OP-BH, cardiopulmonary bypass was established using standard distal ascending aorta and 2-stage right atrial venous cannulation technique. An intra-coronary shunt was used for all coronary anastomoses. Visualization was enhanced by using a surgical blower-humidifier. The target mean arterial pressure (MAP) was kept between 70 and 80 mmHg to optimize coronary perfusion during coronary grafting.
Definitions
Operative mortality was defined as any death that occurred within 30 days of operation. Additive European System for Cardiac Operative Risk Evaluation (EuroSCORE) I was used to calculate the risk profile as in a significant number of patients in the early part of the study only EuroSCORE I was recorded. Renal failure was defined using the RIFLE (Risk, Injury, Failure, Loss of kidney function, and End-stage kidney disease) criteria and included a rise of creatinine 3 times the baseline or serum creatinine ≥4 mg/dl, urine output <0.3 ml/kg/h for 24 h or anuria for 12 h or need for new-onset renal replacement therapy [16]. Gastro-intestinal (GI) complications included GI bleeds, ischemia, acute abdomen, and paralytic ileus lasting more than 48 h. Adverse neurological events included both type I (fatal or nonfatal stroke; as well as transient ischemic attacks and coma) and type II (confusion and seizures which required treatment) events. Post-operative MI was defined by presence of persistent ST changes anytime during the in-hospital stay accompanied by evidence of new regional wall dysfunction on echocardiography. Troponin I was measured in these patients but no clear cut threshold was in place to define MI in the early part of the study.
Definitions with respect to other pre-morbid conditions and post-operative complications are those used in the Society of Thoracic Surgeons (STS) Adult Cardiac Surgical Database, Version4.20.2 [17]. Major adverse cardiac and cerebral event (MACCE) rates were defined as a composite of 30-day mortality, post-operative MI, and stroke.
Statistical analysis
Categorical data was described as number and percentage. Continuous variables were reported using mean and standard deviation. For propensity matching, nearest neighbor matching technique was used and the groups were matched for variables including age, gender, body mass index, EuroSCORE, history of recent myocardial infarction or unstable angina, hypertension, peripheral vascular disease, chronic obstructive airway disease, diabetes, pre-op renal impairment, pre-op neurological events, and left ventricular function. Multiple logistic regression was carried out on the pooled data of 1062 patients. Mortality was the dichomatous dependent variable. The independent variables included age, body mass index (BMI), additive EuroSCORE, glycosylated hemoglobin (HbA1c), gender, history of recent MI, unstable angina, peripheral vascular disease, hypertension, chronic obstructive airway disease, pre-operative renal impairment, cerebro-vascular accident, left ventricular ejection fraction (LVEF) < 40%, presence of left main coronary artery stenosis, triple vessel disease, usage of left internal thoracic artery, and the OP-BH technique. Odds ratio (OR) and 95% confidence intervals (CI) were used to express risk-adjusted outcomes. All statistical analysis was performed using SPSS v.24.0 (IBM Corp., Armonk, NY, USA).
Results
The total study population consisted of 1062 patients (mean age 58.79 ± 8.41) and consisted of 122 (11.5%) females. Two hundred fourteen (20.2%) presented with a recent history of MI within the last 30 days prior to the procedure. The cohort included two groups each including 531 patients. The first group consisted of patients who had undergone OP-BH surgery. Another cohort of 531 propensity-matched patients was identified from the patients who underwent OPCAB surgery during the same time period.
The two groups were compared for baseline characteristics and were found to be closely matched (Table 1). There were no differences between the groups with regard to age (p = 0.9), gender distribution (p = 0.3), or risk profile as assessed by EuroSCORE (p = 0.45). No differences were observed in terms of presence of left main stem disease (p = 0.36), triple vessel disease (p = 0.93), presence of carotid stenosis (p = 0.69), or other pre-morbid conditions like hypertension (p = 0.49) and neurological dysfunction (p = 0.45). The mean ejection fraction between the OP-BH and the OPCAB groups was 50.43 ± 0.53 and 49.66 ± .55 respectively (p value = 0.32).
Table 1.
Baseline comparison of propensity-matched groups
| OPCAB (n = 531) | OP-BH n = 531) | ||
|---|---|---|---|
| no(%) | no(%) | p-value | |
| Age* | 58.9 ± 8.4 | 58.66 ± 8.4 | 0.955 |
| Female | 56 (10.55%) | 66 (12.43%) | 0.387 |
| Body mass index* | 23.9 ± 3.5 | 24 ± 3.9 | 0.855 |
| EuroSCORE* | 3.42 ± 2.32 | 3.36 ± 2.37 | 0.45 |
| Left main disease | 64 (12.05%) | 75 (14.12%) | 0.363 |
| Triple vessel disease | 439 (82.67%) | 437 (82.30%) | 0.936 |
| Double vessel disease | 75 (14.12%) | 77 (14.5%) | 0.93 |
| Single vessel disease | 13 (2.45%) | 10 (1.88%) | 0.67 |
| LVEF<40% | 171 (32.2%) | 161 (30.32%) | 0.551 |
| Carotid artery stenosis | 58 (10.92%) | 63 (11.86%) | 0.69 |
| Pre-op CVA | 6 (1.13%) | 10 (1.88%) | 0.451 |
| Pre-op renal impairment | 31 (5.84%) | 40 (7.53%) | 0.326 |
| Hypothyroid | 23 (4.33%) | 31 (5.84%) | 0.328 |
| COPD | 47 (8.85%) | 48 (9.04%) | 1 |
| Smoker | 124 (23.35%) | 141 (26.55%) | 0.257 |
| Hypertension | 357 (67.23%) | 381 (71.75%) | 0.125 |
| PVD | 22 (4.14%) | 32 (6.03%) | 0.208 |
| Recent MI | 112 (21.09%) | 102 (19.21%) | 0.491 |
* expressed as mean ± sd. CVA cerebro-vascular accident, COPD chronic obstructive pulmonary disease, PVD peripheral vascular disease, MI myocardial infarction, LVEF left ventricular ejection fraction
The mean number of grafts in the OP-BH and the OPCAB was 3.3 and 3.5 respectively. Usage of one or more arterial grafts in addition to the left internal thoracic artery (LITA) was 31 (5.8%) in the OPCAB group and 34 (6.4%) in the OP-BH group (p = 0.7).
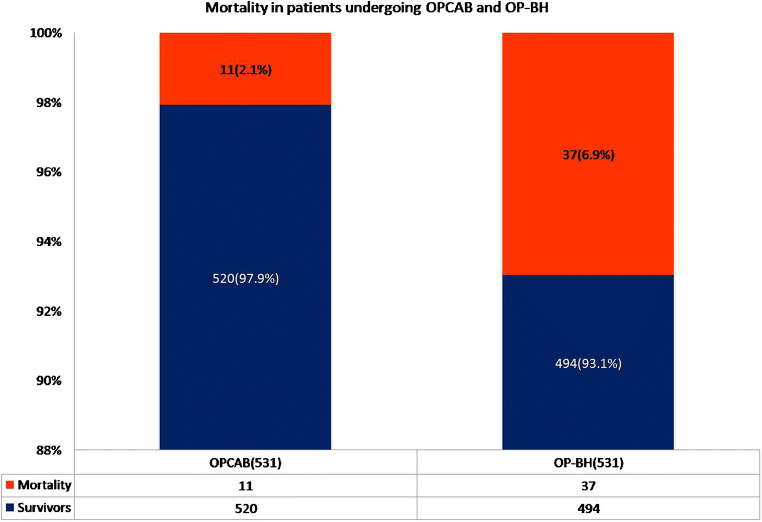
In the OP-BH group, univariate comparison revealed a significantly higher incidence of atrial fibrillation (p = 0.002) as well as life-threatening arrhythmias like ventricular tachycardia and ventricular fibrillation (p = 0.01). Respiratory complications (p = 0.001), renal failure (p < 0.001), GI (p = 0.005), and neurological complications (p = 0.01) were all significantly more common in the OP-BH group despite the groups being closely matched (Table 2). The MI rate in the OPCAB group was 5 (0.9%) as compared to 30 (5.6%) in the OP-BH group and the stroke rate was 1 (0.18%) and 4 (0.75%) respectively (p = 0.17). There were 48 (4.5%) deaths in total. Of these, 11 (2.1%) occurred in the OPCAB group and 37 (6.9%) in the OP-BH group (p < 0.001) (Fig. 1). The overall MACCE rates were 17 (3.2%) in the OPCAB group and 71 (13.3%) in the OP-BH group, p < 0.001.
Table 2.
Univariate post-operative comparison in propensity-matched groups
| OPCAB (531) | On-pump beating heart (531) | ||
|---|---|---|---|
| Atrial fibrillation | 70 (13.8%) | 106 (19.96%) | 0.002 |
| Episodes of VT/VF needing defibrillation | 4 (0.75%) | 15 (2.82%) | 0.01 |
| Respiratory* complications | 103 (19.4%) | 152 (28.63%) | 0.001 |
| CPAP | 6 (1.13%) | 13 (2.45%) | 0.163 |
| Atelectasis | 40 (7.53%) | 56 (10.55%) | 0.108 |
| Effusion (including mild) | 78 (14.69%) | 112 (21.09%) | 0.008 |
| Pneumothorax | 1 (0.19%) | 3 (0.56%) | 0.624 |
| Trachesostomy | 7 (1.32%) | 20 (3.77%) | 0.011 |
| Re-intubation | 23 (4.3%) | 48 (9%) | .001 |
| Post-op renal failure | 16 (3.01%) | 49 (9.23%) | <.001 |
| GI complications | 6 (1.13%) | 20 (3.77%) | .005 |
| Re-explorations | 15 (2.8%) | 41 (7.7%) | <0.001 |
| IABP | 38 (7.1%) | 87 (16.3%) | <0.001 |
| High inotropic support | 17 (3.2%) | 69 (12.9%) | <0.001 |
| MI | 5 (0.9%) | 30 (5.6%) | <0.001 |
| Adverse neurological outcomes | 12 (2.26%) | 28 (5.27%) | .010 |
| Sternal dehiscence | 7 (1.32%) | 11 (2.07%) | 0.34 |
| Deep sternal wound infection | 10 (1.88%) | 12 (2.26%) | 0.667 |
| Leg wound infection | 3 (0.56%) | 8 (1.51%) | 0.224 |
| Transfusion of blood or blood products | 242 (45.57%) | 396 (74.58%) | <0.001 |
*Some patients had more than one respiratory complications. VT ventricular tachycardia, VF venticular fibrillation, GI gastro-intestinal, CPAP continuous positive airway pressure, MACCE major adverse cardiac and cerebral events, IABP intra-aortic balloon pump. High inotropic support—adrenaline requirement of greater than 0.5 mcg/kg/min or use of vasopressin in addition to adrenaline
Fig. 1.
30-day mortality comparison between OP-BH and OPCAB in propensity-matched cohort
Multiple logistic regression was carried out to assess if OP-BH was an independent risk factor for 30-day mortality (Table 3). Apart from OP-BH (OR 5.658, 95% CI 2.8–11.4), only other risk factor which influenced 30-day mortality independently was the EuroSCORE (OR 1.38, 95% CI 1.14–1.66).
Table 3.
Risk factors as identified following multiple logistic regression analysis for 30-day mortality
| OR | 95% CI | p value | |
|---|---|---|---|
| Age | 1.004 | 0.96–1.04 | 0.839 |
| BMI | 0.973 | 0.89–1.05 | 0.494 |
| EuroSCORE | 1.383 | 1.14–1.66 | <0.001 |
| Gender | 1.629 | 0.78–3.39 | 0.192 |
| Recent MI | 0.708 | 0.33–1.49 | 0.364 |
| Pre-op renal impairment | 1.605 | 0.69–3.72 | 0.270 |
| Pre-op CVA | 0.773 | 0.09–6.4 | 0.811 |
| LVEF <40% | 1.318 | 0.71–2.41 | 0.373 |
| Left main disease | 0.805 | 0.36–1.79 | 0.597 |
| OP-BH | 5.658 | 2.8–11.4 | <0.001 |
Risk-adjusted outcome analysis showed that atrial fibrillation (OR 1.66, 95% CI 1.82–2.34) respiratory (OR 1.64, 95% CI 1.22–2.21), renal (OR 6.25, 95% CI 1.76–22.13), cardiovascular (OR 5.51, 95% CI 3.1–9.8), and neurological (OR 2.27, 95% CI 1.11–4.63) complications were all significantly more common in the OP-BH. After adjustment, the risk of sternal dehiscence (OR 1.56, 95% CI 0.58–4.17) and DSWI (OR 1.24, 95% CI 0.52–2.97) was similar across both groups.
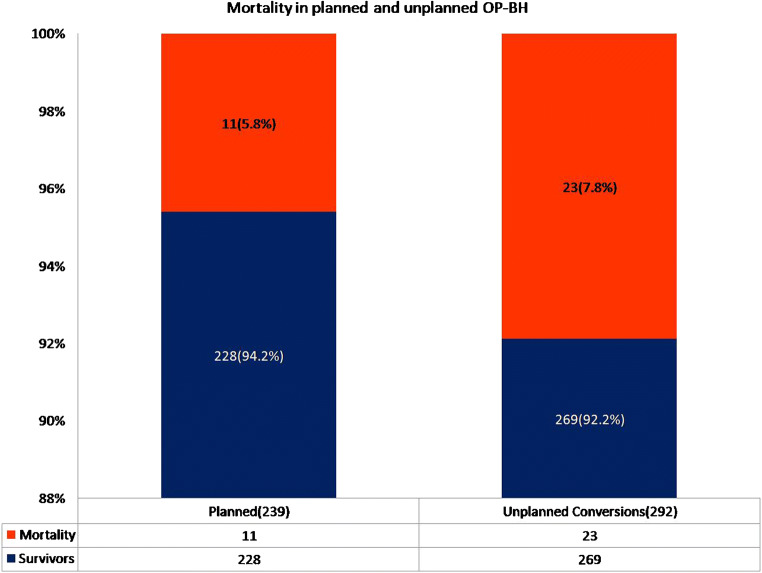
Of the 531 patients, OP-BH was decided upon in 239 patients at the outset. Of the remaining 10,333 patients where OPCAB was the initial technique, 292 (2.8%) were converted to OP-BH intra-operatively. Thus, 292 of OP-BH cases resulted due to conversions from planned OPCAB cases. A sub-group analysis of mortality in these patients showed that there were 23 (7.8%) deaths in patients who were converted from OPCAB to OP-BH. The cohort where OP-BH was planned before the start of the operation, the mortality was 14 (5.8%) out of 239 patients. The difference in 30-day mortality between those where OP-BH was carried out as a result of conversion was thus higher (7.8%) but not statistically significant (p = 0.3) compared to those where the OP-BH was planned at the outset (5.8%) (Fig. 2).
Fig. 2.
Mortality comparison between patients undergoing OP-BH as an emergency conversion and as planned procedure
Discussion
The main finding of our study was that OP-BH compared with OPCAB is associated with worse outcomes. OP-BH was an independent risk factor for 30-day mortality as well as major adverse post-operative outcomes including renal, neurological, and respiratory outcomes and post-operative atrial fibrillation. Irrespective of whether OP-BH was undertaken as conversion from OPCAB or planned at the outset, the outcomes remained worse when compared to OPCAB.
OP-BH was first reported more than 25 years back and used in high-risk patients for whom OPCAB surgery was considered technically too challenging while conventional CABG surgery was considered too risky [18, 19]. Even though avoidance of cardioplegic arrest was thought to be beneficial in high-risk patients both CPB and cardioplegic arrest have the potential to determine inflammatory activation and myocardial, cerebral, and renal dysfunction [20–22]. Cardioplegic arrest is associated with myocardial injury, low cardiac output, renal impairment, and release of free oxygen radicals and interleukins after reperfusion of the ischaemic myocardium [23–25] but despite avoiding cardioplegic arrest, OP-BH still requires CPB support. It is well known that CPB-related factors like lower systemic pressures, non-pulsatile blood flow, and exposure of blood to artificial surfaces can lead to sub-system organ injury and activation of inflammatory humoral and cellular responses [26, 27].
A randomized controlled study comparing conventional CABG with OP-BH confirmed that the increased inflammatory activation and myocardial injury are similar and are due mostly to CPB which is used both in conventional CABG as well as OP-BH [2]. In OPCAB, the deleterious effects of both cardiopulmonary bypass and cardioplegic arrest can be avoided, and thus, the superiority of OPCAB over conventional on-pump CABG as well as OP-BH is therefore scientifically intuitive.
However, the available evidence is quite conflicting. Compared to conventional CABG, adoption of OP-BH has been reported to be associated with improved mortality [1, 3, 28, 29]. This has however been contested by other studies which have shown either no difference or beneficial outcome for conventional CABG [2, 4–7, 12, 13]. The comparison between OP-BH and OPCAB has been mainly carried out in retrospective studies [5, 8–15]. These studies have also reported contradictory findings; however, predominantly most of the studies showed similar outcomes between OPCAB and OP-BH [5, 9, 10, 12, 14, 15].
In one of the studies, OPCAB was compared with OP-BH in patients with LVEF <40%. The study showed equivalent mortality rates between the two techniques [14]. Similar findings were seen in another study that compared OP-BH with OPCAB in patients with LVEF<35% [15]. In the OP-BH group, there was an increase in post-operative morbidity in terms of respiratory complications and neurological outcomes but these differences did not reach statistical significance. This lack of difference in mortality or morbidity could be due to a small sample size that ranged from only 44 to 88 patients in the OP-BH arm in these studies [5, 9, 10, 14, 15].
The indications of using OP-BH in our study varied depending on the timing of the decision. Intra-operatively, the main indications for conversions included presence of significant hemodynamic instability, ventricular arrhythmias or widespread ischemic changes. The decision for OP-BH made prior to the start of the operation was influenced by presence of diffuse coronary artery disease where endarterectomy was contemplated; as well as very poor ejection fraction with severe hemodynamic instability that required pre-operative intubation, inotropic support and intra-aortic balloon pump (IABP). Heparin and other anti-platelet agents may have been continued in these patients until the time of surgery. Since, data on duration of pre-operative cessation of anti-platelet agents was not available in all cases this could not be used for propensity matching. Endarterectomies along with continuation of anti-platelet agents may have contributed to the significantly higher re-exploration rates seen in the OP-BH group.
Increased incidence of myocardial infractions and inotropic requirements seen in our study can be partially explained by the left ventricle being susceptible to subendocardial ischemia during OP-BH. This has been established by another study that provided Magnetic resonance imaging (MRI) evidence of irreversible myocardial injury in more than one-third of the patient undergoing OP-BH [6]. An increase in mortality has also been reported by two other studies with the OP-BH technique compared to OPCAB [7, 8].
The underlying mechanism is due to the subendocardium of the left ventricle being especially prone to myocardial ischemia, as perfusion to this area occurs exclusively during diastole [30]. Subendocardial ischemia results due to an imbalance between energy supply and demand. The energy supply is dependent on the oxygen delivery which in turn is primarily dependent on the coronary perfusion. With a decrease in coronary perfusion pressure, there is a progressive redistribution of blood flow away from the subendocardium [31]. In OPCAB surgery, subendocardial ischemia to a large extent is prevented by auto-regulation [32]. In OP-BH surgery, the cardiac workload is reduced in an empty beating heart; however, the bypassed beating heart is completely dependent on the perfusion pressure and a drop in perfusion pressure below 50 mm of Hg leads to significant subendocardial ischemia [33, 34].
Another important explanation for higher mortality seen in the OP-BH group could be due to the conversions (planned or unplanned). These conversions could have been either an outcome of hemodynamic instability requiring emergency conversions (unplanned) or could have been chosen electively at the start of the operation in anticipation of hemodynamic instability or technical problems (planned). High-volume centers have reported a mortality rate as high as 6% where the conversion occurred electively but was 32% in emergency conversions [35]. However, in our study, the mortality in the patients who were converted from OPCAB was higher (7.8%) but not significantly so compared to those where OP-BH was used as an elective strategy (5.8%). It is also possible that some of the OP-BH strategy deemed elective were done so because of concerns over using the preferred strategy of OPCAB. In fact, this important issue was discussed in a best evidence paper comparing OP-BH with OPCAB, which highlighted that most of the available data on OP-BH arises from specialist off-pump surgeons or centers where OP-BH is invariably carried out in the higher risk patients [36]. OP-BH has been used primarily in high-risk situation and it is difficult to ascertain whether the poor outcome seen with OP-BH is due to the technique or is merely a reflection of a more severe underlying disease process and patient-related factors. In view of available evidence, a randomized study may be ethically challenging and outcome data from well-designed prospective observational studies in low-risk patients can provide some evidence about the technique itself. In view of poor outcomes seen with this technique, utilization of the conventional on-pump technique should be contemplated in these situations.
Limitations
The most important limitation of our study is a selection bias. All surgeons at the institution were predominantly OPCAB surgeons. Therefore, every time a patient was chosen for OP-BH, there must have been compelling reasons for doing so. While the risk stratification takes cognizance of well-defined parameters, there are undefined factors, determined by the surgical experience to anticipate problems, with a particular technique. Severe diffuse lesions, poor targets, and anticipation of needing endarterectomies are not assessed by risk stratification scores but may have influenced surgeons’ decision to embark on OP-BH. We have attempted to adjust for this selection bias by carrying out a robust propensity matching where the groups were closely matched for all measured parameters. However, certain unmeasured factors may remain which could have influenced our outcomes. We also used EuroSCORE I and not the more recent EuroSCORE II or the STS score because in a significant number of patients, in the early part of the study, only EuroSCORE I was recorded. However, we feel that since the same risk stratification method was used in both arms it should not unfairly influence the interpretation of our findings. Retrospective studies are also limited by adequacy and accuracy of data capturing. In our study, capturing of type II neurological defects as well as MI is liable to be deficient in this respect.
Conclusion
OP-BH in our study was associated with poor outcomes. Propensity matching allowed a balance comparison between OPCAB and OP-BH; however, unquantified factors may have influenced the outcomes too. Irrespective of the cause, it is apparent that utilization of OP-BH either by design or by compulsion is associated with worse outcomes. Thus, OP-BH in a predominantly OPCAB center may be considered to be an indirect marker of poor outcome. Further, prospective randomized studies would be required to answer the question with certainty but its feasibility remains questionable.
Funding
None.
Declarations
Ethics committee approval
Was obtained from the institutional ethics committee (NHRTIICSEC/AP/2021/002) on the 4th of January 2021.
Human rights statement
The research was conducted in accordance with the 1964 Helsinki Declaration.
Informed consent
As the study was a retrospective analysis of data, the need for individual patient consent was waived off.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mizutani S, Matsuura A, Miyahara K, et al. On-pump beating-heart coronary artery bypass: a propensity matched analysis. Ann Thorac Surg. 2007;83:1368–1373. doi: 10.1016/j.athoracsur.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 2.Narayan P, Rogers CA, Bayliss KM, et al. On-pump coronary surgery with and without cardioplegic arrest: comparison of inflammation, myocardial, cerebral and renal injury and early and late health outcome in a single-centre randomised controlled trial. Eur J Cardiothorac Surg. 2011;39:675–683. doi: 10.1016/j.ejcts.2010.08.032. [DOI] [PubMed] [Google Scholar]
- 3.Prifti E, Bonacchi M, Giunti G, et al. Does on-pump/beating-heart coronary artery bypass grafting offer better outcome in end-stage coronary artery disease patients? J Card Surg. 2000;15:403–410. doi: 10.1111/j.1540-8191.2000.tb01300.x. [DOI] [PubMed] [Google Scholar]
- 4.Sabban MA, Jalal A, Bakir BM, et al. Comparison of neurological outcomes in patients undergoing conventional coronary artery bypass grafting, on-pump beating heart coronary bypass, and off-pump coronary bypass. Neurosciences (Riyadh). 2007;12:35–41. [PubMed] [Google Scholar]
- 5.Tsai Y-T, Lin F-Y, Lai C-H, Lin Y-C, Lin C-Y, Tsai C-S. On-pump beating-heart coronary artery bypass provides efficacious short- and long-term outcomes in hemodialysis patients. Nephrol Dial Transplant. 2012;27:2059–2065. doi: 10.1093/ndt/gfr536. [DOI] [PubMed] [Google Scholar]
- 6.Pegg TJ, Selvanayagam JB, Francis JM, et al. A randomized trial of on-pump beating heart and conventional cardioplegic arrest in coronary artery bypass surgery patients with impaired left ventricular function using cardiac magnetic resonance imaging and biochemical markers. Circulation. 2008;118:2130–2138. doi: 10.1161/CIRCULATIONAHA.108.785105. [DOI] [PubMed] [Google Scholar]
- 7.Edgerton JR, Dewey TM, Magee MJ, et al. Conversion in off-pump coronary artery bypass grafting: an analysis of predictors and outcomes. Ann Thorac Surg. 2003;76:1138–1142. doi: 10.1016/S0003-4975(03)00747-1. [DOI] [PubMed] [Google Scholar]
- 8.Darwazah AK, Bader V, Isleem I, Helwa K. Myocardial revascularization using on-pump beating heart among patients with left ventricular dysfunction. J Cardiothorac Surg. 2010;5:109. 10.1186/1749-8090-5-109. [DOI] [PMC free article] [PubMed]
- 9.Letsou GV, Wu YX, Grunkemeier G, Rampurwala MM, Kaiser L, Salaskar AL. Off-pump coronary artery bypass and avoidance of hypothermic cardiac arrest improves early left ventricular function in patients with systolic dysfunction. Eur J Cardiothorac Surg. 2011;40:227–232. doi: 10.1016/j.ejcts.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Munos E, Calderon J, Pillois X, et al. Beating-heart coronary artery bypass surgery with the help of mini extracorporeal circulation for very high-risk patients. Perfusion. 2011;26:123–131. doi: 10.1177/0267659110395650. [DOI] [PubMed] [Google Scholar]
- 11.Reber D, Brouwer R, Buchwald D, et al. Beating-heart coronary artery bypass grafting with miniaturized cardiopulmonary bypass results in a more complete revascularization when compared to off-pump grafting. Artif Organs. 2010;34:179–184. doi: 10.1111/j.1525-1594.2009.00836.x. [DOI] [PubMed] [Google Scholar]
- 12.Tarakji KG, Sabik JF, 3rd, Bhudia SK, Batizy LH, Blackstone EH. Temporal onset, risk factors, and outcomes associated with stroke after coronary artery bypass grafting. JAMA. 2011;305:381–390. doi: 10.1001/jama.2011.37. [DOI] [PubMed] [Google Scholar]
- 13.Uva MS, Rodrigues V, Monteiro N, et al. Coronary surgery: which method to use? Rev Port Cardiol. 2004;23:517–530. [PubMed] [Google Scholar]
- 14.Wang W, Wang Y, Piao H, et al. Early and medium outcomes of on-pump beating-heart versus off-pump CABG in patients with moderate left ventricular dysfunction. Braz J Cardiovasc Surg. 2019;34:62–69. doi: 10.21470/1678-9741-2018-0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xia LM, Ji Q, Song K, et al. Early clinical outcomes of on-pump beating-heart versus off-pump technique for surgical revascularization in patients with severe left ventricular dysfunction: The experience of a single center. J Cardiothorac Surg. 2017;12:11. 10.1186/s13019-017-0572-x. [DOI] [PMC free article] [PubMed]
- 16.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–R212. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adult Cardiac Surgery Database Data Collection | STS. https://www.sts.org/registries-research-center/sts-national-database/adultcardiac-surgery-database/data-collection. Accessed 30 Dec 2020.
- 18.Sweeney MS, Frazier OH. Device-supported myocardial revascularization: safe help for sick hearts. Ann Thorac Surg. 1992;54:1065–1070. doi: 10.1016/0003-4975(92)90071-b. [DOI] [PubMed] [Google Scholar]
- 19.Perrault LP, Menasché P, Peynet J, et al. On-pump, beating-heart coronary artery operations in high-risk patients: an acceptable trade-off? Ann Thorac Surg. 1997;64:1368–1373. doi: 10.1016/S0003-4975(97)00842-4. [DOI] [PubMed] [Google Scholar]
- 20.Flack JE, 3rd, Cook JR, May SJ, et al. Does cardioplegia type affect outcome and survival in patients with advanced left ventricular dysfunction? Results from the CABG Patch Trial. Circulation. 2000;102:III84–III89. doi: 10.1161/01.cir.102.suppl_3.iii-84. [DOI] [PubMed] [Google Scholar]
- 21.Chowdhury UK, Malik V, Yadav R, et al. Myocardial injury in coronary artery bypass grafting: on-pump versus off-pump comparison by measuring high-sensitivity C-reactive protein, cardiac troponin I, heart-type fatty acid-binding protein, creatine kinase-MB, and myoglobin release. J Thorac Cardiovasc Surg. 2008;135:1110-9,1119.e1-10. 10.1016/j.jtcvs.2007.12.029. [DOI] [PubMed]
- 22.Nicolini F, Beghi C, Muscari C, et al. Myocardial protection in adult cardiac surgery: current options and future challenges. Eur J Cardiothorac Surg. 2003;24:986–993. doi: 10.1016/S1010-7940(03)00475-5. [DOI] [PubMed] [Google Scholar]
- 23.Ascione R, Lloyd CT, Gomes WJ, Caputo M, Bryan AJ, Angelini GD. Beating versus arrested heart revascularization: evaluation of myocardial function in a prospective randomized study. Eur J Cardiothorac Surg. 1999;15:685–690. doi: 10.1016/s1010-7940(99)00072-x. [DOI] [PubMed] [Google Scholar]
- 24.Ascione R, Lloyd CT, Underwood MJ, Gomes WJ, Angelini GD. On-pump versus off-pump coronary revascularization: evaluation of renal function. Ann Thorac Surg. 1999;68:493–498. doi: 10.1016/s0003-4975(99)00566-4. [DOI] [PubMed] [Google Scholar]
- 25.Ivey CL, Williams FM, Collins PD, Jose PJ, Williams TJ. Neutrophil chemoattractants generated in two phases during reperfusion of ischemic myocardium in the rabbit. Evidence for a role for C5a and interleukin-8. J Clin Invest. 1995;95:2720–2728. doi: 10.1172/JCI117974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Butler J, Parker D, Pillai R, Westaby S, Shale DJ, Rocker GM. Effect of cardiopulmonary bypass on systemic release of neutrophil elastase and tumor necrosis factor. J Thorac Cardiovasc Surg. 1993;105:25–30. [PubMed]
- 27.Cremer J, Martin M, Redl H, et al. Systemic inflammatory response syndrome after cardiac operations. Ann Thorac Surg. 1996;61:1714–1720. doi: 10.1016/0003-4975(96)00055-0. [DOI] [PubMed] [Google Scholar]
- 28.Izumi Y, Magishi K, Ishikawa N, Kimura F. On-pump beating-heart coronary artery bypass grafting for acute myocardial infarction. Ann Thorac Surg. 2006;81:573–576. doi: 10.1016/j.athoracsur.2005.08.036. [DOI] [PubMed] [Google Scholar]
- 29.Erkut B, Dag O, Kaygin MA, et al. On-pump beating-heart versus conventional coronary artery bypass grafting for revascularization in patients with severe left ventricular dysfunction: Early outcomes. Can J Surg. 2013;56:398–404. doi: 10.1503/cjs.018412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Algranati D, Kassab GS, Lanir Y. Why is the subendocardium more vulnerable to ischemia? A new paradigm. Am J Physiol Heart Circ Physiol. 2011;300:H1090–H1100. doi: 10.1152/ajpheart.00473.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vijayan S, Barmby DS, Pearson IR, Davies AG, Wheatcroft SB, Sivananthan M. Assessing coronary blood flow physiology in the cardiac catheterisation laboratory. Curr Cardiol Rev. 2017;13:232–243. doi: 10.2174/1573403X13666170525102618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nakajima H, Iguchi A, Tabata M, et al. Preserved autoregulation of coronary flow after off-pump coronary artery bypass grafting: retrospective assessment of intraoperative transit time flowmetry with and without intra-aortic balloon counterpulsation. J Cardiothorac Surg. 2016;11:156. doi: 10.1186/s13019-016-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mo A, Lin H, Wen Z, Lu W, Long X, Zhou Y. Efficacy and safety of on-pump beating heart surgery. Ann Thorac Surg. 2008;86:1914–1918. doi: 10.1016/j.athoracsur.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 34.Buckberg GD. Left ventricular subendocardial necrosis. Ann Thorac Surg. 1977;24:379–393. doi: 10.1016/s0003-4975(10)63418-2. [DOI] [PubMed] [Google Scholar]
- 35.Mack MJ, Pfister A, Bachand D, et al. Comparison of coronary bypass surgery with and without cardiopulmonary bypass in patients with multivessel disease. J Thorac Cardiovasc Surg. 2004;127:167–173. doi: 10.1016/j.jtcvs.2003.08.032. [DOI] [PubMed] [Google Scholar]
- 36.Sepehripour AH, Chaudhry UAR, Harling L, Athanasiou T. Off-pump or on-pump beating heart: which technique offers better outcomes following coronary revascularization? Interact Cardiovasc Thorac Surg. 2015;20:546–549. doi: 10.1093/icvts/ivu451. [DOI] [PubMed] [Google Scholar]