Abstract
Background
Early identification of poor adherence to CPAP treatment is of major clinical importance to optimize treatment outcomes in patients with OSA.
Research Question
How do socioeconomic factors influence CPAP adherence?
Study Design and Methods
Nationwide, population-based cohort study of patients with OSA receiving CPAP treatment reported to the Swedish quality registry Swedevox between 2010 and 2018 was cross-linked with individual socioeconomic data from Statistics Sweden. Socioeconomic factors associated with CPAP adherence were identified using a multivariate linear regression model, adjusted for age and sex.
Results
In total, 20,521 patients were included: 70.7% men; mean age ± SD, 57.8 ± 12.2 years; BMI, 32.0 ± 6.1 kg/m2; apnea-hypopnea index, 36.9 ± 22.1; Epworth Sleepiness Scale, 10.4 ± 5.0; and median nocturnal CPAP use, 355 min (interquartile range, 240-420 min). Adherence after 1.3 ± 0.8 years of CPAP use was significantly (all P < .001) associated with civil status (married vs unmarried: +20.5 min/night), education level (high, ≥ 13 years vs low, ≤ 9 years: +13.2 min/night), total household income (highest/third/second vs lowest quartile: +15.9 min/night, +10.4 min/night, and +6.1 min/night, respectively), and country of birth (born in Sweden with one native parent/born in Sweden with two native parents vs being born abroad: +29.0 min/night and +29.3 min/night, respectively).
Interpretation
Civil status, educational level, household income, and foreign background predict CPAP adherence in a clinically significant manner and should be considered when treating OSA with CPAP.
Key Words: adherence, CPAP, OSA, socioeconomic factors
Abbreviations: AHI, apnea-hypopnea index; ESS, Epworth Sleepiness Scale
OSA with excessive daytime sleepiness is common, affecting at least 6% of men and 4% of women,1 and is associated with increased risk of cardiovascular mortality and morbidity.2,3 CPAP treatment improves daytime sleepiness and daily functioning,4 mitigates an elevated risk of motor vehicle accidents,5 and reduces BP.6 In observational studies, CPAP has been shown to improve cardiovascular outcomes.7,8 However, this association was not shown in intention-to-treat analyses of randomized controlled trials,9, 10, 11, 12 but rather in the subgroup of patients with high adherence to CPAP.10, 11, 12 Four hours of mean nightly CPAP use have been identified as the cutoff point for the above-mentioned beneficial CPAP effects.
Adherence to CPAP treatment often is insufficient and a major clinical problem. As many as 29% to 83% of patients with OSA who are receiving CPAP treatment have a nocturnal CPAP use of less than 4 h.13 Excessive daytime sleepiness and a high apnea-hypopnea index (AHI), indicating more severe OSA, are associated with better adherence to CPAP therapy.14 Only a handful of studies, many of those small and with short follow-up duration, have evaluated the association between socioeconomic factors and adherence. Income,15,16 educational level,17 socioeconomic status in neighborhood,16, 17, 18 number of household members, and civil status18,19 have been associated with adherence in ,some but not all, studies.20, 21, 22, 23 The aim of this large population-based study with extended follow-up was to evaluate the association between socioeconomic factors and long-term adherence to CPAP in patients with OSA.
Methods
Study Design and Population
The study was an analysis of the CPAP subcohort in the prospective, longitudinal cohort study Course of Disease in Patients Reported to the Swedish CPAP Oxygen and Ventilator Registry. A detailed description of the study protocol was published previously.24 Patients with OSA treated with CPAP reported to the Swedevox registry between July 1, 2010, and March 12, 2018, were included, and data were cross-linked with several other quality and governmental registries. In this study, socioeconomic data from Statistics Sweden were used.
The total cohort comprised 66,265 patients, and those with complete data regarding CPAP adherence at the scheduled 1-year follow-up visit were analyzed further (n = 20,521) (Fig 1). Patients lacking reported data on nocturnal CPAP use or who claimed no further need of CPAP at the follow-up visit were excluded from subsequent analysis. Potential explanation for ceased need for CPAP can be significant weight loss with decreased symptoms of OSA or other successful sleep hygienic intervention.
Figure 1.
Study flowchart.
The procedure for reporting to the Swedevox registry has been detailed elsewhere.25 In brief, CPAP-related data were reported manually to a web-based case report format by 39 sleep centers. The geographical coverage is estimated to be 90% (www.ucr.uu.se/swedevox/rapporter/arsrapporter) (e-Fig 1). Since 2015, up to 17 centers reported data via automated data transfer from the Swedish Sleep Apnea Registry (www.sesar.se). Information about sex, age, height, weight, AHI, oxygen desaturation index, excessive daytime sleepiness using the Epworth Sleepiness Scale (ESS) score,26 and the presence of hypertension as well as information about the use of a humidifier were reported to the registry when CPAP therapy was initiated. At follow-up, data regarding nocturnal CPAP use time (hours per total number of nights) from the CPAP’s data log were reported.
Socioeconomic Data From Statistics Sweden
Individual data on civil status and country of birth were based on data from the nationwide Swedish Civil Registry supplied to Statistics Sweden, a government-based agency that brings official statistics to the public (www.scb.se/en). Civil status was categorized as: married or in a civil partnership, unmarried, divorced, and widow or widower. National origin was categorized as: born in Sweden with two native parents, born in Sweden with one native and one foreign parent, born in Sweden with two foreign parents, and born abroad.
Total household income at year of inclusion in the Swedevox registry or control group was obtained from the Swedish Tax Agency and was index-linked and categorized into quantiles.27,28 The Swedish Longitudinal Integrated Database for Health Insurance and Labour Market Studies provided data on length of education.29 Education was categorized into three levels: low (≤ 9 years), medium (10-12 years), and high (≥ 13 years), corresponding to compulsory school, secondary school, and postsecondary school (college and university), respectively.
Ethics
The study was approved by the Ethical Board of Lund University (Identifier: Log No. 2018/51). Reporting to a National Quality Registry in Sweden requires careful information and verbal consent, but does not require written informed consent.
Statistical Analyses
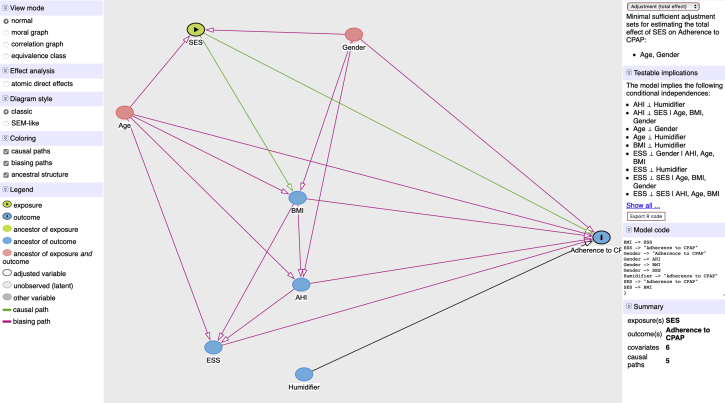
Normal distributed continuous data were expressed as mean ± SD, and skewed distributed continuous data were expressed as median with interquartile range. Categorical data were presented as frequencies and percentages. The t test was used for comparisons of continuous variables, and the χ 2 test was used for comparisons of categorical variables. The associations between adherence to CPAP therapy as a dependent variable and covariates were evaluated in multivariate linear and logistic regression models. Direct acyclic graphs were created using the browser-based environment DAGitty (www.dagitty.net)30 and identified age and sex as the main confounding factors (Fig 2). In the fully adjusted linear regression model all covariates (socioeconomic factors, age, sex, BMI, AHI, ESS score, and use of humidifier) were included to make effect sizes comparable and interpretable in a clinical context. To make a comparison of effect size between classic variables associated with CPAP adherence and socioeconomic variables possible and interpretable in a clinical context, the continuous variables age, BMI, AHI, and ESS score were transformed to categorical variables using widely accepted clinical severity thresholds. Age was stratified into young (< 40 years), middle-aged (40-< 60 years), and elderly (≥ 60 years) and total household income was stratified into quartiles to make the variable understandable for international readers. A sensitivity analysis was conducted comparing counties with reported follow-up data on more than 50% of patients with counties reporting lower follow-up rates. A P value of < .05 was considered statistically significant. Statistical analyses were conducted using Stata version 16.0 software (StataCorp LP).
Figure 2.
Direct acyclic graph identifying main confounders among the covariates. Dependent variable is nocturnal CPAP use time. AHI = apnea-hypopnea index; ESS = Epworth Sleepiness Scale; SES = socioeconomic status.
Results
In total, 20,521 patients were included in the analysis after a mean of 1.3 ± 0.8 years of CPAP use; 70.7% were men with a mean age of 57.8 ± 12.2 years, BMI of 32.0 ± 6.1 kg/m2, AHI of 36.9 ± 22.1 events/h, and ESS score of 10.4 ± 5.0. Nocturnal CPAP use of ≥ 4 h was reported in 15,511 patients (76%), whereas lower adherence was reported in 5,010 patients (Table 1, Fig 1). The median nocturnal CPAP use time was 355 min (interquartile range, 240-420 min). CPAP-adherent patients were slightly older, showed higher AHI levels at baseline, and showed a slightly lower BMI. Patients nonadherent to CPAP were less frequently married, had lower levels of education, and more frequently had a foreign background.
Table 1.
Baseline Characteristics
| Characteristic | All | Fully Adherent to CPAP (≥ 4 h/night) | Nocturnal CPAP Use < 4 h/night |
|---|---|---|---|
| No. of patients | 20,521 | 15,511 | 5,010 |
| Men | 14,501 (70.7) | 11,029 (71.1) | 3,472 (69.3) |
| Nocturnal CPAP use, min | 355 (240-420) | 386 (328-432) | 69 (0-180) |
| Age, y | 57.8 ± 12.2 | 58.2 ± 11.9 | 56.6 ± 12.7 |
| <40 | 1,632 (8.0) | 1,137 (7.3) | 495 (9.9) |
| 40-60 | 8,938 (43.6) | 6,604 (42.6) | 2,334 (46.6) |
| ≥60 | 9,951 (48.5) | 7,770 (50.1) | 2,181 (53.5) |
| BMI, kg/m2 | 32.0 ± 6.1 | 32.0 ± 6.0 | 32.3 ± 6.6 |
| < 25 | 1,667 (8.4 | 1,227 (8.2) | 440 (9.2) |
| 25-< 30 | 6,565 (33.2) | 5,031 (33.6) | 1,534 (32.0) |
| 30-< 35 | 6,305 (31.9) | 4,850 (32.4) | 1,455 (30.3) |
| ≥ 35 | 5,241 (26.5) | 3,874 (25.9) | 1,367 (28.5) |
| AHI, events/h | 36.9 ± 22.1 | 38.3 ± 22.2 | 32.6 ± 21.3 |
| < 5 | 202 (1.0) | 118 (0.8) | 84 (1.7) |
| 5-< 15 | 2,491 (12.3) | 1,579 (10.3) | 912 (18.5) |
| 15-< 30 | 6,287 (31.1) | 4,652 (30.4) | 1,635 (33.1) |
| ≥ 30 | 11,252 (55.6) | 8,944 (58.5) | 2,308 (46.7) |
| ESS | 10.4 ± 5.0 | 10.5 ± 4.9 | 9.9 ± 5.0 |
| < 7 | 4,557 (24,3) | 3,309 (23.2) | 1,248 (27.8) |
| 7-10 | 5,118 (27.3) | 3,859 (27.1) | 1,259 (28.0) |
| 11-15 | 5,982 (31.9) | 4,669 (32.8) | 1,313 (29.2) |
| > 16 | 3,072 (16.4) | 2,396 (16.8) | 676 (15.0) |
| Use of humidifier | 10,028 (49.3) | 7,686 (49.9) | 2,342 (47.4) |
| Civil status | |||
| Unmarried | 4,736 (23.1) | 3,366 (21.7) | 1,370 (27.4) |
| Married | 11,509 (56.1) | 9,046 (58.4) | 2,462 (49.3) |
| Divorced | 3,319 (16.29 | 2,396 (15.5) | 923 (18.5) |
| Widower or widow | 935 (4.6) | 696 (4.5) | 239 (4.8) |
| Educational level | |||
| Low, ≤ 9 y | 4,392 (22.2) | 3,256 (21.7) | 1,140 (23.9) |
| Medium, 10-12 y | 10,222 (51.7) | 7,669 (51.1) | 2,550 (53.5) |
| High, > 12 y | 5,168 (26.1) | 4,088 (27.2) | 1,082 (22.6) |
| Households total income, index-linked gross pay, € | 32,270 ± 18,921 | 32,861 ± 19,056 | 30,437 ± 18,540 |
| 1st quartile (lowest) | 5,129 (25.0) | 3,674 (23.7) | 1,455 (29.1) |
| 2nd quartile | 5,128 (25.0) | 3,853 (24.8) | 1,275 (25.5) |
| 3rd quartile | 5,130 (25.0) | 3,905 (25.2) | 1,225 (24.5) |
| 4th quartile (highest) | 5,128 (25.0) | 4,078 (26.3) | 1,050 (21.0) |
| Birth country | |||
| Born abroad | 2,335 (11.4) | 1,617 (10.4) | 718 (14.3) |
| Born in Sweden, two foreign parents | 427 (2.1) | 298 (1.9) | 129 (2.6) |
| Born in Sweden, one native parent | 1,149 (5.6) | 864 (5.6) | 285 (5.7) |
| Born in Sweden, two native parents | 16,610 (80.9) | 12,732 (82.1) | 3,878 (77.4) |
Data are presented as No. (%), mean ± SD, or median (interquartile range). AHI = apnea-hypopnea index; ESS = Epworth Sleepiness Scale.
In multivariate linear regression analysis (Table 2), independent predictors of higher nocturnal CPAP use were female sex, age of ≥ 60 years, BMI of 25 to 35 kg/m2, AHI of ≥ 15 events/h, ESS of > 10, and use of a humidifier. Among the socioeconomic factors, being married, having a high educational level exceeding 13 years, having a total household income exceeding the lowest quartile, and being born in Sweden with one or two native parents all were associated independently with longer nocturnal CPAP use (Table 2, Fig 3).
Table 2.
Multiple Linear Regression Models With Minutes of Nightly CPAP Use as Dependent Variable
| Variable | Model 2A: β-Coefficient for Minutes of Nightly CPAP Use (95% CI)a | P Value | Model 2B: β-Coefficient for Minutes of Nightly CPAP Use (95% CI)b | P Value | Model 2C: β-Coefficient for Minutes of Nightly CPAP Use (95% CI)c | P Value |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male | 1 | ... | 1 | ... | 1 | ... |
| Female | –1.7 (–6.2 to 2.8) | .460 | 3.1 (–1.7 to 7.9) | .208 | 7.3 (2.3-12.4) | .005 |
| Age, y | ||||||
| < 40 | 1 | ... | 1 | ... | 1 | ... |
| 40-60 | 13.6 (5.7-21.4) | .001 | 7.5 (–0.8 to 15.7) | .076 | 7.6 (–0.9 to 16.2) | .079 |
| ≥ 60 | 33.8 (26.0-41.6) | < .001 | 26.3 (17.6-34.9) | < .001 | 27.0 (18.0-36.0) | < .001 |
| BMI, kg/m2 | ||||||
| < 25 | ... | ... | ... | ... | 1 | ... |
| 25-< 30 | ... | ... | ... | ... | 10.0 (1.7-18.4) | .018 |
| 30-< 35 | ... | ... | ... | ... | 10.8 (2.3-19.2) | .012 |
| ≥ 35 | ... | ... | ... | ... | 6.5 (–2.3 to 15.2) | .146 |
| AHI, events/h | ||||||
| < 5 | ... | ... | ... | ... | 1 | ... |
| 5-< 15 | ... | ... | ... | ... | 25.8 (3.2-48.4) | .025 |
| 15-< 30 | ... | ... | ... | ... | 62.9 (40.8-85.0) | < .001 |
| ≥ 30 | ... | ... | ... | ... | 84.4 (62.4-106.4) | < .001 |
| ESS score | ... | ... | ... | ... | ... | ... |
| < 7 | ... | ... | ... | ... | 1 | ... |
| 7-10 | ... | ... | ... | ... | 6.5 (0.5-12.5) | .032 |
| 11-15 | ... | ... | ... | ... | 13.7 (7.9-19.5) | < .001 |
| > 16 | ... | ... | ... | ... | 17.2 (10.3-24.1) | < .001 |
| Use of humidifier | ... | ... | ... | ... | 8.4 (4.1-12.7) | < .001 |
| Civil status | ||||||
| Unmarried | ... | ... | 1 | ... | 1 | ... |
| Married | ... | ... | 20.5 (14.8-25.6) | < .001 | 20.6 (14.9-26.3) | < .001 |
| Divorced | ... | ... | –6.8 (–13.7 to 0.2) | .056 | –5.2 (–12.4 to 2.0) | .415 |
| Widower or widow | ... | ... | 3.9 (–7.2 to 15.1) | .489 | 0.1 (–11.6 to 11.8) | .984 |
| Educational level | ||||||
| Low (≤ 9 y) | ... | ... | 1 | ... | 1 | ... |
| Medium (10-12 y) | ... | ... | 3.1 (–2.2 to 8.4) | .256 | 2.3 (–3.2 to 7.9) | .415 |
| High (≥ 13 y) | ... | ... | 13.2 (7.0-19.4) | < .001 | 12.8 (6.3-19.2) | < .001 |
| Household total income (index-linked) | ||||||
| Quartile 1 (lowest income) | ... | ... | 1 | ... | 1 | ... |
| Quartile 2 | ... | ... | 6.1 (0.2-12.0) | .043 | 8.5 (2.3-14.6) | .007 |
| Quartile 3 | ... | ... | 10.4 (4.3-16.5) | .001 | 12.1 (5.8-18.5) | < .001 |
| Quartile 4 (highest income) | ... | ... | 15.9 (9.5-22.3) | < .001 | 17.0 (10.3-23.7) | < .001 |
| Birth country | ||||||
| Born abroad | ... | ... | 1 | ... | 1 | ... |
| Born in Sweden, two foreign parents | ... | ... | 10.7 (–4.9 to 26.3) | .179 | 3.2 (–12.9 to 19.3) | .698 |
| Born in Sweden, one native parent | ... | ... | 29.0 (18.3-39.8) | < .001 | 25.5 (14.4-36.6) | < .001 |
| Born in Sweden, two native parents | ... | ... | 29.3 (22.7-36.0) | < .001 | 27.2 (20.2-34.2) | < .001 |
AHI = apnea-hypopnea index; ESS = Epworth Sleepiness Scale.
Adjusted for sex and age.
Adjusted for sex, age, and socioeconomic factors.
Adjusted for all variables in the table.
Figure 3.
Forest plot showing the contribution of independent variables on total nocturnal CPAP use (min/night). AHI = apnea-hypopnea index; ESS = Epworth Sleepiness Scale.
In a sensitivity analysis addressing a potential reporting bias, all socioeconomic factors remained significant as independent predictors of CPAP adherence in counties with more than 50% of patients with reported follow-up data (8 counties; 13,138 patients). In counties with less than 50% of patients with a reported follow-up visit (11 counties; 7,383 patients), all factors except education level and total household income for counties with < 50% follow-up remained significant (e-Table 1). The impact of socioeconomic factors on adherence to CPAP treatment was confirmed in a multivariate logistic regression analysis adjusting for the same covariates (Table 3). Patients lost to follow-up (n = 39,949) showed a slightly lower AHI at baseline compared with the analysis population (34.6 ± 22.7 vs 36.9 ± 22.1 events/h; P < .001); otherwise, no clinically significant differences at baseline were identified (e-Table 2).
Table 3.
OR for Having Nocturnal CPAP Use of ≥ 4 h
| Variable | OR (95% CI) | P Value |
|---|---|---|
| Civil status | ||
| Unmarried | 1 | ... |
| Married | 1.36 (1.25-1.48) | < .001 |
| Divorced | 0.96 (0.87-1.07) | .498 |
| Widower or widow | 1.06 (0.88-1.27) | .547 |
| Education | ||
| Low (≤ 9 y) | 1 | ... |
| Medium (10-12 y) | 1.08 (0.99-1.17) | .079 |
| High (≥13 y) | 1.26 (1.14-1.39) | < .001 |
| Household total income | ||
| Quartile 1 (lowest income) | 1 | ... |
| Quartile 2 | 1.15 (1.05-1.26) | .004 |
| Quartile 3 | 1.26 (1.14-1.38) | < .001 |
| Quartile 4 (highest income) | 1.43 (1.29-1.59) | < .001 |
| Birth country | ||
| Born abroad | 1 | ... |
| Born in Sweden, two foreign parents | 1.09 (0.86-1.38) | .476 |
| Born in Sweden, one native parent | 1.38 (1.17-1.63) | < .001 |
| Born in Sweden, two native parents | 1.37 (1.24-1.52) | < .001 |
Adjusted for sex, age, and all variables in the table. AHI = apnea-hypopnea index; ESS = Epworth Sleepiness Scale.
Discussion
The main finding of this longitudinal population-based study is that civil status, educational level, household income, and foreign background can be established as strong predictors for CPAP adherence in OSA. As illustrated in the regression analysis, the effect sizes of socioeconomic factors are equivalent to those often used for the indication of CPAP therapy like the degree of daytime sleepiness or OSA severity.
To the best of our knowledge, the impact of socioeconomic factors on adherence to CPAP therapy have not been analyzed in a large population-based cohort. Previous studies are based on small clinical cohorts consisting of 70 to 330 patients,15, 16, 17, 18, 19, 20, 21, 22 and follow-up times generally were short.20 Because of the small sample size in previous studies, multivariate analysis is statistically challenging, rendering the results inconsistent. To estimate the impact of socioeconomic status despite small sample sizes, different compound socioeconomic variables were created. Such compound variables were able to show associations with CPAP adherence in some studies,17 whereas others studies failed to do so.20,21 Indeed, neighborhood social status has been used as a proxy for socioeconomic factors, and some studies have found associations with CPAP adherence,16, 17, 18 whereas others have not.23
In the present study, being married was associated with longer time undergoing CPAP therapy. In a retrospective cohort study with 330 OSA patients, being married was associated with higher nocturnal CPAP use of ≥ 4 h after 1 week.18 In another study with 80 patients and a follow-up time of 1 month, patients living with a partner evinced higher CPAP use.19 Other studies have failed to show associations between civil status and CPAP adherence.21,22 Studies analyzing associations between educational level and CPAP adherence are sparse and the results are conflicting.17,21 Two studies from Israel and one from Iran have found associations with low income levels and impaired adherence15,16,31 and have pointed to patients’ inability to afford a CPAP device as a partial explanation. In Sweden, the health care system largely is tax funded, making patients mainly independent of private economy or private health care insurance to obtain access to CPAP treatment. In the present study, those with the lowest household total income showed lower CPAP use, a finding that accords with small studies from New Zealand and the United States, where low incomes were associated with less time using CPAP.17,32 In several studies from the United States and New Zealand, being Black or of non-European origin, respectively, were associated with worse adherence to CPAP therapy, but after adjusting for socioeconomic factors, the associations weakened or disappeared.17,18,22,32 In the present study, being born abroad or being born in Sweden with two foreign parents was associated independently with lower CPAP use. This may be explained by linguistic difficulties or cultural differences.
Mean AHI at initiation of CPAP therapy was 37, and adherence rate was 355 min of nocturnal CPAP use, both high rates compared with those reported from in other countries.33 In accordance with Swedish national guidelines, mild to moderate OSA often is treated with a mandibular advancement device, whereas severe OSA is treated preferably with CPAP. Presence of severe OSA is associated positively with adherence,25 and these factors together can explain, at least in part, the elevated baseline AHI and the proportionally high amount of CPAP adherence reported in our study when compared with data published elsewhere.13,33 Age and degree of sleep apnea at baseline did not differ substantially between reporting centers. In contrast, partial copayment for CPAP therapy by the patients may vary substantially between administrative regions in Sweden (€0-€200 per year). However, mean CPAP adherence differs only to a small extent between different regions in Sweden (e-Fig 2).34
As expected, we identified significant intercorrelations between socioeconomic factors (eg, education level and income) as well as between socioeconomic factors and anthropometric factors (eg, education level and BMI). However, the influence of socioeconomic factors on compliance remained unchanged in the final statistical model (data not shown).
The current study has a number of strengths, including the generalizability of our findings. First, this large patient cohort has a nationwide coverage of more than 90% of all patients with OSA treated with CPAP in Sweden. In addition, reported Swedevox registry data have a high degree of internal and external validity, as evidenced by an actual validation study that demonstrated > 98% agreement of register data and source data in the medical records.35 Cross-linkage of our patient data with high-quality socioeconomic data from the nationwide Swedish Civil Registry and Tax Authorities creates a world-unique database in size and data quality.
A number of limitations need to be discussed, including a high proportion of patients lost to follow-up (more than 60%), which may have created an important bias in our analysis. Despite development and spread of remote monitoring of CPAP treatment, data still are reported to the Swedevox registry manually via a web questionnaire. Plenty of technological and juridical issues must be solved first, but automated follow-up reporting definitely would increase data capture and would strengthen overall data quality from the registry. Plausible explanations of low reported follow-up rates are that reporting to the registry is down-prioritized at some centers or that patients do not show up when called for control. In the current study, 76% of the patients showed nocturnal CPAP use exceeding 4 h at the 1-year follow-up visit, a proportion slightly higher compared with what was found in previous studies,13 supporting the assumption that patients not attending follow-up assessments may have worse adherence rates. We performed a number of additional analyses. First, we identified no clinically significant differences in baseline characteristics between included and not included patients, which reduces the risk of bias. In addition, our final study cohort was slightly biased toward a lower proportion of unmarried patients and those born abroad, two factors associated with lower compliance. Therefore, our analysis may rather underestimate the impact of these socioeconomic factors on CPAP adherence. Finally, a high rate of completed follow-up visits is a quality marker for generalizability of data, so we performed a sensitivity analysis including centers with high (> 50%) and low (< 50%) follow-up rates. In centers with lower follow-up frequency, educational level and total household income were no longer associated with adherence. Thus, this sensitivity analysis confirmed the strong influence of socioeconomic factors on CPAP adherence because the association between socioeconomic factors and adherence was even stronger in this subpopulation characterized by less selection bias.
Our results show that socioeconomic factors such as economic, educational, and cultural background affect CPAP treatment adherence. Low socioeconomic status is associated with poorer health and shorter life expectancy.36 Identifying modifiable factors like treatment adherence that could be part of the explanation for these differences—and acting on these findings—could contribute to better health. When treating patients with CPAP, a greater awareness of the impact of different socioeconomic factors on adherence and, when necessary, individually tailored follow-up may improve treatment adherence and may contribute to health equity.
Interpretation
Civil status, educational level, household income, and foreign background are important factors associated with adherence to CPAP therapy in patients with OSA. To promote adherence, socioeconomic factors should be considered. Education and follow-up programs should be tailored better to people with low socioeconomic status.
Take-home Points.
Study Question: How do socioeconomic factors influence CPAP adherence?
Results: Civil status, educational level, household income, and foreign background predict CPAP adherence in a clinically significant manner.
Interpretation: Education and follow-up programs should be tailored better to people with low socioeconomic status.
Acknowledgments
Author contributions: A. P. had full access to all data from the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. A. P. and L. G. were responsible for data analysis. A. P., L. G., J. T.-H., M. L., J. S., B. M., and M. E. made substantial contributions to study conception and design, acquisition of data, or analysis and interpretation of data. A. P. drafted the article and L. G., J. T.-H., M. L., J. S., B. M., and M. E. revised the article critically for important intellectual content. All authors had final approval of the version to be published.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following: L. G. reports grants from Bayer, Resmed, Respironics/Philips, Desitin, and the European Respiratory Society and nonfinancial support from Itamar Medical and Resmed; serves on the speakers bureau for Resmed, Philips, AstraZeneca, Fisher, and Paykel; and holds a patent on sleep apnea therapy issued. None declared (A. P., J. T.-H., M. L., J. S., B. M., M. E.).
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Other contributions: The authors thank Krister Ågren, MSc, for statistical support, all centers in Sweden reporting data to the Swedevox registry, all patients who allowed themselves be included in the registry, and the Swedish Heart and Lung Association for their commitment to the Swedevox registry’s steering committee.
Additional information: The e-Figures and e-Tables can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: This work was supported by the Swedish Society for Sleep Research and Sleep Medicine, Uppsala-Örebro Regional Research Council [Grant Log Nos RFR-931234]; the Centre for Research and Development, Uppsala University/Region Gävleborg [Grant Log Nos CFUG-925881]; Bror Hjerpstedt’s Foundation, and the Fagerström Foundation. L. G. was supported by the Swedish Heart and Lung Foundation and the agreement concerning research and education of doctors [Grant ALFGBG-725601]. M. E. was supported by unrestricted grants from the Swedish Society for Medical Research and the Swedish Research Council [Grant: Log No. 2019-02081].
Supplementary Data
References
- 1.Franklin K.A., Lindberg E. Obstructive sleep apnea is a common disorder in the population: a review on the epidemiology of sleep apnea. J Thorac Dis. 2015;7(8):1311–1322. doi: 10.3978/j.issn.2072-1439.2015.06.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Young T., Finn L., Peppard P.E. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31(8):1071–1078. [PMC free article] [PubMed] [Google Scholar]
- 3.Punjabi N.M., Caffo B.S., Goodwin J.L. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6(8) doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weaver T.E., Maislin G., Dinges D.F. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007;30(6):711–719. doi: 10.1093/sleep/30.6.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karimi M., Hedner J., Habel H., Nerman O., Grote L. Sleep apnea-related risk of motor vehicle accidents is reduced by continuous positive airway pressure: Swedish Traffic Accident Registry data. Sleep. 2015;38(3):341–349. doi: 10.5665/sleep.4486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bratton D.J., Stradling J.R., Barbe F., Kohler M. Effect of CPAP on blood pressure in patients with minimally symptomatic obstructive sleep apnoea: a meta-analysis using individual patient data from four randomised controlled trials. Thorax. 2014;69(12):1128–1135. doi: 10.1136/thoraxjnl-2013-204993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marin J.M., Carrizo S.J., Vicente E., Agusti A.G. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–1053. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 8.Campos-Rodriguez F., Martinez-Garcia M.A., de la Cruz-Moron I., Almeida-Gonzalez C., Catalan-Serra P., Montserrat J.M. Cardiovascular mortality in women with obstructive sleep apnea with or without continuous positive airway pressure treatment: a cohort study. Ann Intern Med. 2012;156(2):115–122. doi: 10.7326/0003-4819-156-2-201201170-00006. [DOI] [PubMed] [Google Scholar]
- 9.Barbe F., Duran-Cantolla J., Sanchez-de-la-Torre M. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;307(20):2161–2168. doi: 10.1001/jama.2012.4366. [DOI] [PubMed] [Google Scholar]
- 10.McEvoy R.D., Antic N.A., Heeley E. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med. 2016;375(10):919–931. doi: 10.1056/NEJMoa1606599. [DOI] [PubMed] [Google Scholar]
- 11.Peker Y., Glantz H., Eulenburg C., Wegscheider K., Herlitz J., Thunstrom E. Effect of positive airway pressure on cardiovascular outcomes in coronary artery disease patients with nonsleepy obstructive sleep apnea. The RICCADSA randomized controlled trial. Am J Respir Crit Care Med. 2016;194(5):613–620. doi: 10.1164/rccm.201601-0088OC. [DOI] [PubMed] [Google Scholar]
- 12.Sanchez-de-la-Torre M., Sanchez-de-la-Torre A., Bertran S. Effect of obstructive sleep apnoea and its treatment with continuous positive airway pressure on the prevalence of cardiovascular events in patients with acute coronary syndrome (ISAACC study): a randomised controlled trial. Lancet Respir Med. 2020;8(4):359–367. doi: 10.1016/S2213-2600(19)30271-1. [DOI] [PubMed] [Google Scholar]
- 13.Weaver T.E., Grunstein R.R. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173–178. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sin D.D., Mayers I., Man G.C., Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430–435. doi: 10.1378/chest.121.2.430. [DOI] [PubMed] [Google Scholar]
- 15.Simon-Tuval T., Reuveni H., Greenberg-Dotan S., Oksenberg A., Tal A., Tarasiuk A. Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep. 2009;32(4):545–552. doi: 10.1093/sleep/32.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brin Y.S., Reuveni H., Greenberg S., Tal A., Tarasiuk A. Determinants affecting initiation of continuous positive airway pressure treatment. Isr Med Assoc J. 2005;7(1):13–18. [PubMed] [Google Scholar]
- 17.Bakker J.P., O’Keeffe K.M., Neill A.M., Campbell A.J. Ethnic disparities in CPAP adherence in New Zealand: effects of socioeconomic status, health literacy and self-efficacy. Sleep. 2011;34(11):1595–1603. doi: 10.5665/sleep.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Platt A.B., Field S.H., Asch D.A. Neighborhood of residence is associated with daily adherence to CPAP therapy. Sleep. 2009;32(6):799–806. doi: 10.1093/sleep/32.6.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewis K.E., Seale L., Bartle I.E., Watkins A.J., Ebden P. Early predictors of CPAP use for the treatment of obstructive sleep apnea. Sleep. 2004;27(1):134–138. doi: 10.1093/sleep/27.1.134. [DOI] [PubMed] [Google Scholar]
- 20.Gulati A., Ali M., Davies M., Quinnell T., Smith I. A prospective observational study to evaluate the effect of social and personality factors on continuous positive airway pressure (CPAP) compliance in obstructive sleep apnoea syndrome. BMC Pulm Med. 2017;17(1):56. doi: 10.1186/s12890-017-0393-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Billings M.E., Auckley D., Benca R. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34(12):1653–1658. doi: 10.5665/sleep.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ye L., Pack A.I., Maislin G. Predictors of continuous positive airway pressure use during the first week of treatment. J Sleep Res. 2012;21(4):419–426. doi: 10.1111/j.1365-2869.2011.00969.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Campbell A., Neill A., Lory R. Ethnicity and socioeconomic status predict initial continuous positive airway pressure compliance in New Zealand adults with obstructive sleep apnoea. Intern Med J. 2012;42(6):e95–e101. doi: 10.1111/j.1445-5994.2010.02360.x. [DOI] [PubMed] [Google Scholar]
- 24.Palm A., Ågren K., Grote L. Course of DISease In patients reported to the Swedish CPAP Oxygen and VEntilator RegistrY (DISCOVERY) with population-based controls. BMJ Open. 2020;10(11) doi: 10.1136/bmjopen-2020-040396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palm A., Midgren B., Theorell-Haglow J. Factors influencing adherence to continuous positive airway pressure treatment in obstructive sleep apnea and mortality associated with treatment failure—a national registry-based cohort study. Sleep Med. 2018;51:85–91. doi: 10.1016/j.sleep.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 26.Johns M.W. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 27.Ekonomifakta Real löneutveckling. July 20, 2020. Ekonomifakta website. https://www.ekonomifakta.se/Fakta/Arbetsmarknad/Loner/Loneutveckling-och-inflation/?graph=/20419/1/all/
- 28.Statistics Sweden Income and tax registry. Statistics Sweden website. https://www.scb.se/vara-tjanster/bestalla-mikrodata/vilka-mikrodata-finns/individregister/inkomst-och-taxeringsregistret-iot/
- 29.Ludvigsson J.F., Svedberg P., Olen O., Bruze G., Neovius M. The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur J Epidemiol. 2019;34(4):423–437. doi: 10.1007/s10654-019-00511-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lederer D.J., Bell S.C., Branson R.D. Control of confounding and reporting of results in causal inference studies. Guidance for authors from editors of respiratory, sleep, and critical care journals. Ann Am Thorac Soc. 2019;16(1):22–28. doi: 10.1513/AnnalsATS.201808-564PS. [DOI] [PubMed] [Google Scholar]
- 31.Rezaie L., Phillips D., Khazaie H. Barriers to acceptance and adherence to continuous positive airway pressure therapy in patients with obstructive sleep apnea: a report from Kermanshah province, western Iran. Patient Prefer Adherence. 2018;12:1299–1304. doi: 10.2147/PPA.S165905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scharf S.M., Seiden L., DeMore J., Carter-Pokras O. Racial differences in clinical presentation of patients with sleep-disordered breathing. Sleep Breath. 2004;8(4):173–183. doi: 10.1007/s11325-004-0173-5. [DOI] [PubMed] [Google Scholar]
- 33.Bakker J.P., Weaver T.E., Parthasarathy S., Aloia M.S. Adherence to CPAP: what should we be aiming for, and how can we get there? Chest. 2019;155(6):1272–1287. doi: 10.1016/j.chest.2019.01.012. [DOI] [PubMed] [Google Scholar]
- 34.The Swedevox Registry Annual report 2019. Uppsala Clinical Research Center website. https://www.ucr.uu.se/swedevox/rapporter/arsrapporter/arsrapport-2019-2/viewdocument/548
- 35.Ekström M., Albrecht D., Andersson S. Validation of the Swedevox registry of continuous positive airway pressure, long-term mechanical ventilator and long-term oxygen therapy. ERJ Open Res. 2021;7(1) doi: 10.1183/23120541.00340-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Makenzius M., Skoog-Garås E., Lindqvist N., Forslund M., Tegnell A. Health disparities based on neighbourhood and social conditions: Open Comparisons—an indicator-based comparative study in Sweden. Public Health. 2019;174:97–101. doi: 10.1016/j.puhe.2019.06.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.