Abstract
Background
Accurate blood pressure (BP) measurement is essential for the diagnosis and management of hypertension. In clinical practice, BP is estimated using noninvasive methods with significant variability of application of guidelines in clinical practice, impacting the accuracy and certainty of BP measurements.
Objective
We sought to assess how BP is measured in clinical practice.
Methods
A survey was administered through professional societies that included predominantly cardiologists. Assessment of adherence to guideline recommendations for BP assessment was measured and compared to the level of confidence in clinic BP measurement.
Results
There were 571 surveys completed. The majority of respondents were cardiologists (61.1%), with 47 preventive cardiologists. BP was routinely checked in both arms by 53% at the initial visit, 48% check BP once each visit, and 64% wait 5 min before initial BP assessment. Automated BP assessment is used by 58% respondents. The majority (83%) trust their BP readings, and those who trust their BP readings are more likely to perform the initial BP assessment themselves, compared to those who do not trust the clinic BP readings (30.2% vs. 13.6%, P = 0.009). Accurate BP measurement is performed by 23% of cardiologists, and more likely performed accurately by a preventive cardiologist (38.3%) compared with other cardiologists (20.0%, P = 0.007). Accurate BP measurement is more likely for those who perform the initial BP themselves rather than any other staff (36.8% vs. 17.9%; P<0.001); and for those who repeat BP manually (80% vs. 54%; P<0.001), compared to those who do not measure BP accurately. Despite the inaccuracy of BP measurement, there is a high level of confidence in the BP readings.
Conclusions
Accurate BP assessment continues to remain suboptimal in clinical practice. Reliability of BP assessment requires education, identifying barriers to implementation of recommendations and engagement of the entire team to improve BP assessment.
Keywords: Blood pressure, Hypertension, Blood pressure assessment, Measurement, Skills
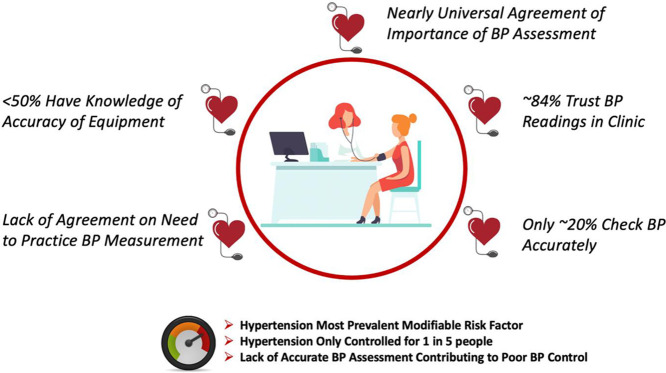
Graphical abstract
Survey of Healthcare Professionals on Blood Pressure Assessment
.
Hypertension remains the leading risk factor globally for deaths and quantitatively is the most important noncommunicable disease given its impact on cardiovascular, neurologic and renal disease. It affects over 1 billion people worldwide and it is estimated that less than 1 in 5 people are adequately controlled, contributing to over 10 million deaths per year [1]. Accurate measurement of blood pressure (BP) is essential to the diagnosis of hypertension and also for its management. BP assessment is the most important and commonly performed measurement in clinical medicine. Inaccuracies in BP measurement in a population, even if small, can have considerable consequences. Overestimation can result in inappropriate treatment, just as underestimation can lead to increased adverse cardiovascular outcomes. Overestimating true BP by 5 mm Hg in the population could result in inappropriate treatment with antihypertensives in approximately 30 million Americans, exposing them unnecessarily to adverse side effects of the medications and unnecessary costs [2]. Underestimations of the same 5 mm Hg can miss over 20 million Americans when extracted on a population level, with a potential 25% increase in fatal strokes and myocardial infarction [3].
Nonetheless, accurate BP measurement in the clinic is highly undervalued and often performed inaccurately. For some clinicians, this results in clinical inertia with the awareness that BP is often inaccurate in their clinical setting, resulting in a hesitation to treat an elevated BP, given the lack of confidence they have in their BP readings. In others, there is simply lack of awareness of how to accurately assess BP, and hence, the clinicians will respond and initiate treatment to inaccurate readings. Current recommendations for BP measurement in the outpatient setting vary amongst different organizations across the world. This has led to ambiguity and a lack of standardization in clinical practice. The 2017 American College of Cardiology (ACC)/American Heart Association (AHA) guidelines recommend two separate BP readings 1–3 min apart taken after the patient has been sitting for at least 5 min [4]. Guidelines published in 2018 by European Society of Cardiology (ESC)/European Society of Hypertension (ESH) describe a similar protocol but at least three BP measurements [5]. Both recommend ambulatory and home BP monitoring to confirm diagnosis outside the clinic setting. In addition, the European guidelines also emphasize unattended automated (AOBP) measurements to reduce or even eliminate white coat hypertension. By automating this process, it inherently creates a standardized process that minimizes interruption and variation between patients. In the BP assessment algorithm published by Hypertension Canada, all initial AOBP measurements are performed unattended [6]. General consensus amongst guidelines favors automated over manual BP readings; however, there is delay in uptake in clinical practice.
To date, there is limited information regarding how cardiologists assess BP clinically, particularly since the 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults were released. We sought to determine how BP is assessed in clinical practice by cardiologists, to determine both the accuracy of BP assessment and trust cardiologists had in their BP measurements.
1. Methods
This study was approved by the internal review board of the University of Arizona. The survey (Appendix 1) was distributed to three professional societies, which were chosen due to their focus on cardiovascular disease prevention and hypertension. It was also shared on twitter which resulted in additional responses. Although the target populations intended was cardiologists, others in healthcare could also respond. Only those who completed the entire survey were included in the analysis
1.1. Study design
The survey was distributed by e-mail by three professional societies that include predominantly cardiologists or clinicians that specialize in hypertension and cardiovascular disease prevention. This included the American Society for Preventive Cardiology, The Society for Cardiovascular Computed Tomography, and the High Blood Pressure Research Council of Australia. The survey was open for 30 days on SurveyMonkey™, and allowed only a single response from respondents. The survey was shared on social media in the last 2 weeks of the data collection but represented only 22% of the total respondents.
1.2. Accurate BP assessment
We defined “Accurate BP Assessment” if the respondents reported the following: routinely checking BP in both arms; checking BP two or more times per visit; and waiting 5 min before checking BP. Although respondents were asked if they used an automated BP monitor versus a manual monitor, this was not included in the definition of accurate BP assessment.
1.3. Statistics
We performed a descriptive analysis of variables of interest, presenting categorical variables as percentages. We performed unadjusted comparisons of the characteristics of those persons checking BP accurately compared to those who do not in our cohort by using χ2 tests. All p values were 2-tailed, and the level of significance was set at alpha = 0.05. Data were analyzed using STATA 16.0 (StataCorp, College Station, TX).
2. Results
There were 612 respondents in the 30 days of sending the request to complete our survey. A total of 571 persons responded to all questions, which was a 93.3% completion rate. The majority of respondents were cardiologists: 349 (61.1%), with 47 of them identified as preventive cardiologists (Table 1). The remaining respondents were: 127 (22.2%) physicians of other types 40 (7.0%), nurse practitioners, 11 (1.9%) nurses, 5 (0.9%) medical assistants, and 39 (6.8%) other healthcare professionals. Those who completed the entire survey are included in this analysis, with most of the respondents (55.5%) from the United States (Table 1).
Table 1.
Respondent characteristics.
| N = 571 (%) | ||
|---|---|---|
| Clinical Role | Preventive Cardiologists | 47 (8.2) |
| CardiologistPhysician (other)Other Healthcare Professional | 302 (52.9)127 (22.3)95 (16.6) | |
| Country of Practice | USA | 317 (55.5) |
| Canada | 38 (6.7) | |
| Mexico | 54 (9.5) | |
| Europe | 63 (11.0) | |
| Australia/New Zealand | 34 (6.0) | |
| South America | 46 (8.0) | |
| Asia | 11 (1.9) | |
| Africa | 8 (1.4) |
2.1. Clinic blood pressure assessment
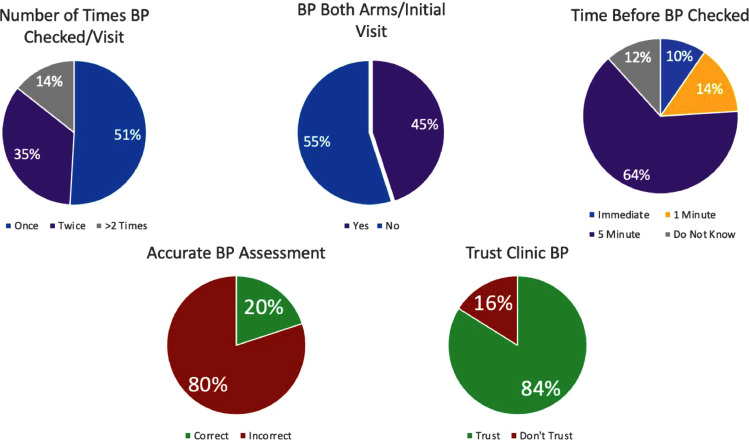
The majority of the people responding to this survey reported that they did not routinely check BP in both arms at the initial clinic visit (55.5%) or check BP more than once at each clinic visit (51.0%). Most reported waiting 5 min before checking BP (64.3%). (Fig. 1) In most cases, from everyone completing the survey only 25.9% assessed the blood pressure themselves. Nonetheless, 57.6% (276) repeated the BP manually, and 61.3% (214) cardiologists performed a manual BP measurement themselves. (Table 2)
Fig. 1.
Accuracy of blood pressure assessment.
Table 2.
Clinical blood pressure assessment.
| N = 571(%) | ||
|---|---|---|
| At the initial visit do you routinely check BP in both arms? | YesNo | 247 (45.0)314 (55.0) |
| How many times in a clinic visit do you check BP? | OnceTwiceMore than 2X | 291 (51.0)198 (34.7)82 (14.3) |
| How many minutes do you wait before the initial BP measurement? | Immediate1 min5 MinDo Not Know | 55 (9.6)82 (14.4)367 (64.3)67 (11.7) |
| Who Checks the Initial BP in Your Clinic? | Medical AssistantPhysician AssistantNurseNurse PractitionerMyselfOther/Missing | 264 (46.2)7 (1.2)130 (22.8)17 (3.0)148(25.9)5 (0.9) |
| Do You Trust Your Clinic BP? | YesNo | 479 (83.9)92 (16.1) |
| Do you check BP using an automated BP monitor? | YesNo | 348 (61.0)233 (39.0) |
| If you use an automated BP monitor, does anyone from your staff remain in the room? | Yes & No instructions About TalkingYes & Instructed to Not Talk to The PatientNo staff remains in the roomI don't use an automated BP monitor | 137 (24.0)165 (28.9)112 (19.6)157 (27.5) |
| When do you order a 24-hour ambulatory BP monitor in your practice? | To diagnose or rule out White Coat HTNTo diagnose or rule out Masked HTNTo confirm a diagnosis of HTN based on clinical assessmentTo diagnose or rule out either White Coat HTN or Masked HTN or confirm a diagnosis of HTNI don't use an ambulatory BP monitor | 71 (12.4)18 (3.2)35 (6.1)298 (52.2)149 (26.1) |
| How often do you recommend Home BP monitoring? | In all patients with HTNIn newly diagnosed HTNWhen blood pressure appears uncontrolled and new medications startedI don't recommend home BP assessmentMost of my patients cannot afford a home BP monitor | 301 (52.7)36 (6.3)184 (32.2)34 (6.0)16 (2.8) |
BP= Blood Pressure, HTN = Hypertension.
Automated BP monitors for BP assessment in clinic were not used in 39% of those surveyed. In those who do use automated BP monitors in their clinics, 24% don't give any instructions to the person taking the BP measurement about talking during the procedure, while 28.9% instruct the person taking the BP to not talk to the patient. Only 19.6% have the person measuring the BP to leave the patient's room while the automated cuff is inflating. (Table 2)
2.2. Use of ambulatory and home blood pressure monitoring
The majority (52.2%) of respondents use ambulatory BP monitoring to assess for white coat hypertension or Masked hypertension or confirm a diagnosis of hypertension, although 26.1% do not use ambulatory BP monitoring (Table 2). The remainder use ambulatory BP monitoring for a single specific reason but not for all indications. From those surveyed, 52.7% recommend the use of home BP monitoring in all patients with HTN, and 32.2% recommend it only when BP appears uncontrolled and new medications started. Interestingly, only 2.3% reported that most of their patients cannot afford a home BP monitor.
2.3. Trust in BP readings
The majority of those surveyed trusted their BP measurement (83.9%), despite most of those surveyed perform it inaccurately, with no difference in those who trusted or did not trust the clinic BP assessment (P = 0.13) (Fig. 1). Those who trusted their clinic BP assessments were more likely to routinely check BP in both arms at initial visit, when compared with those who did not trust their BP (47.4% vs 32.6%; P = 0.009). They were also more likely to perform the initial BP assessment themselves when compared with those who did not trust their BP (28.7% vs 13%; P = 0.002). Performance of a manual repeat BP did not differ between those who trusted or did not trust their clinic BP measures. There was also no difference in terms of the number of times that the BP was checked or use of an automated BP monitor, if that was used. (Table 3)
Table 3.
Confidence in blood pressure assessment.
| ALL PARTICPANTS | Trust BPN = 479 | Do Not Trust BPN = 92 | P-value |
|---|---|---|---|
| Routinely Check BP in Both Arms at Initial Visit | 227 (47.4) | 30 (32.6) | 0.009 |
| Initial BP assessed by:MyselfOther | 136 (28.7)338 (71.3) | 12 (13.0)80 (87.0) | 0.002 |
| Manually repeat BP in clinic | 276 (57.6) | 56 (60.9) | 0.56 |
| How many times in a clinic visit do you check BP?OnceTwiceGreater than Two Times | 240 (50.1)163 (34.0)76 (15.9) | 51 (55.4)35 (38.0)6 (6.5) | 0.065 |
| How many times in a clinic visit do you check BP?OnceTwice or Greater | 240 (50.1)239 (49.9) | 51 (55.4)41 (44.6) | 0.35 |
| Accurate Use of Automated BP Monitor (No Staff in Room)YesNo | 96 (20.0)383 (80.0) | 16 (17.3)76 (82.6) | 0.56 |
| Accuracy of BP AssessmentAccurateInaccurate | 101 (21.1)378 (78.9) | 13 (14.1)79 (85.9) | 0.13 |
| CARDIOLOGISTS ONLY | N = 290 | N = 59 | |
| ParticipantsCardiologistsPreventive Cardiologists | 255 (97.9)35 (12.1) | 47 (79.7)12 (20.3) | 0.090 |
| Initial BP assessed by:MyselfOther | 87 (30.2)201 (69.8) | 8 (13.6)51 (86.4) | 0.009 |
| Do You Manually repeat BP in clinic?YesNo | 175 (60.3)115 (39.7) | 39 (66.1)20 (33.9) | 0.41 |
| How many times in a clinic visit do you check BP?OnceTwiceGreater than twice | 138 (47.6)112 (38.6)40 (13.8) | 30 (50.8)25 (42.4)4 (6.8) | 0.33 |
| Use of Automated BP Monitor/No Staff in RoomYesNo | 58 (20.0)232 (80.0) | 7 (11.9)52 (88.1) | 0.14 |
| Accuracy of BP AssessmentAccurateInaccurate | 69 (23.8)221 (76.2) | 11 (18.9)48 (81.4) | 0.391 |
BP= Blood Pressure.
2.4. Accuracy of bp measurement
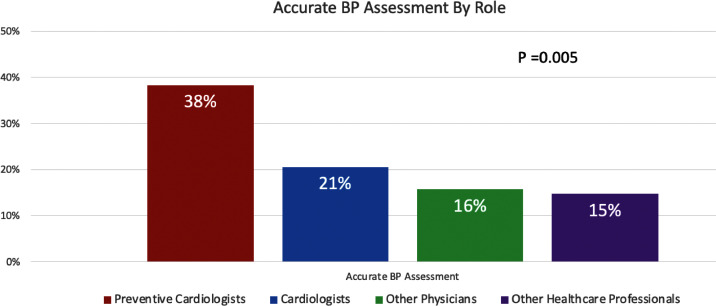
Using the definition of accurate BP in this study, only 114 persons (20.0%) accurately measured BP, yet 479 (83.9%) trusted their BP assessments in their clinics (Fig. 1). Although accurate BP measurement was infrequently performed, it was more likely to be done accurately by preventive cardiology respondents, over other group (38.3% vs 18.3%; P <0.001) (Fig. 2), and this was true even when comparing preventive cardiologists to all cardiologists (38.3% vs. 20.5%; P = 0.007). An accurate BP assessment was more likely when performed by the person being surveyed than any other person in the clinic. In those who performed the BP accurately, 79.8% performed a manual reading in their clinic compared with 52.7% in the group where BP assessment was inaccurate (P<0.001). Regardless of accuracy of BP measurement, there was no difference in the level of trust in their clinic BP readings which was high: 88.6% in those who performed BP accurately vs 82.7% who performed BP inaccurately (P = 0.13). (Table 4)
Fig. 2.
Accurate blood pressure assessment by role.
Table 4.
Accuracy of blood pressure measurement.
| ALL PARTICPANTS | Accurate BP Measurement N = 114 | Inaccurate BP Measurement N = 457 | P-value |
|---|---|---|---|
| ParticipantsPreventive CardiologistsAll Others | 18 (15.8)96 (84.2) | 29 (6.4)428 (93.7) | 0.001 |
| Initial BP assessed by:MA/PA/RN/NPMyself | 67 (58.8)47 (41.2) | 356 (77.9)101 (22.1) | <0.0001 |
| Manually repeat BP in clinic | 91 (79.8%) | 241 (52.7%) | <0.0001 |
| Trust Clinic's BP Measurement | 101 (88.6%) | 378 (82.7%) | 0.13 |
| CARDIOLOGISTS ONLY | N = 80 | N = 269 | |
| ParticipantsCardiologistsPreventive Cardiologists | 62 (20.5)18 (38.3) | 240 (79.5)29 (1.7) | 0.007 |
| Initial BP assessed by:MA/PA/RN/NPMyself | 45 (17.9)35 (36.8) | 207 (82.1)60 (63.2) | <0.0001 |
| Manually repeat BP in clinic | 64 (80.0%) | 150 (55.8%) | <0.0001 |
BP= Blood Pressure.
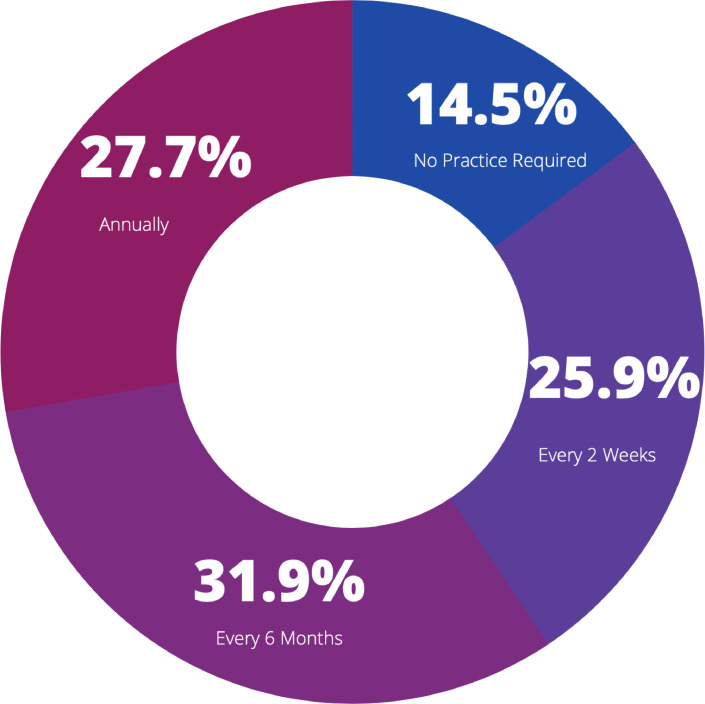
2.5. Importance of blood pressure assessment
There was almost universal agreement that accurate BP assessment was a skill that was essential for medical assistants, nurses and doctors; with >99% who agree or strongly agree on this and consider accurate BP assessment as an important part of the physical exam. In terms of opinions regarding the need and frequency of practice of taking BP, there was wide variability: 14.5% responded that no practice of BP measurement skills were needed, 25.9% selected that skills needed practice every 2 weeks, while 31.9% selected every 6 months and 27.7% responded annual practice of skills was needed. (Fig. 3)
Fig. 3.
Blood pressure skills
How often should blood pressure skills be assessed?.
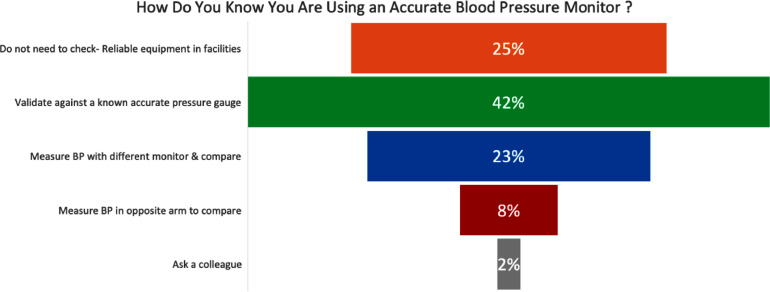
2.6. Knowledge of blood pressure equipment accuracy
The knowledge of those surveyed regarding the reliability of the equipment they use to measure BP was quite variable. Most reported that they know they are using an accurate BP monitor when it was validated against an accurate gage (42.0%), while 25.4% felt that they did not need to check their equipment and their facility provided reliable equipment. Further 22.8% responded they would measure the BP with another monitor and compare, 7.8% would measure the BP in the opposite arm to assess accuracy and 1.8% ask their colleagues to determine the accuracy of their BP monitor (Fig. 4).
Fig. 4.
Knowledge of accuracy of equipment.
3. Discussion
Our study demonstrates that the knowledge of blood pressure measurement skills remains deficient amongst all healthcare professions, with only 1 in 5 persons accurately assessing BP. Despite BP measurement being the most commonly performed procedure in the healthcare setting, there remains significant room for improvement. The assessment of BP provides essential information to aid in the diagnosis and monitoring of hypertension, with a timely response and appropriate treatment. Nonetheless, it is dependent on an accurate measurement and our findings demonstrate lack of awareness of the optimal assessment of BP.
The awareness of the effect of inaccurate BP measurement has been well-described but appears to remain unknown to many in clinical practice, as demonstrated in our survey. The effect of active listening when BP is assessed can increase the systolic BP by up to 10 mm Hg [7]. If a patient needs to urinate, the systolic BP can increase even higher than 10 mm Hg [8]. Crossed legs and lack of any back support can raise BP as well [9, 10]. Taking blood pressure over any clothing can create artifacts in BP assessment although alone does not raise blood pressure [11]. Nonetheless, rolling up sleeves has the potential to create a tourniquet effect that can raise BP up to 50 mm Hg [12]. Using a cuff that is too big or too small can lower or raise BP, respectively [13]. Lack of arm support, [14] or having the arm not at the level of the heart can also raise BP [15]. Additionally there are preferences for the terminal digit to end with zero, estimated to occur in 60–80% of readings which ultimately affects BP accuracy,[16] as well as treatment with antihypertensive medication, especially for women [17]. Reliance on a single read, not measuring BP in both arms at the initial visit, and auscultation rather than automated BP readings can also reduce the accuracy of a clinical BP assessment. Inter-arm differences in systolic blood pressure >5 mmHg are associated with increased cardiovascular mortality for those with elevated cardiovascular disease (CVD) risk[18] as well as people free of pre-existing CVD [19]. Our definition of “accurate BP” was quite liberal and did not include all of these details that are important to accuracy. We assessed if: (1) BP was measured in both arms; (2) time before the initial BP was taken; and (3) the number of times BP was taken. With just these three measures of accuracy, we saw dismally low rates of accurate BP assessment.
While the reliance of BP measurement in the clinic setting continues to guide the diagnosis and management of hypertension, the use of automated BP monitoring is increasingly recommended by guidelines and adopted to reduce these potential sources of errors. Our findings reveal that despite the majority of respondents using automated devices (61%), only one BP measurement was preferred by most (51%) respondents, with a high level of trust in their measurement. In addition, our survey shows that there was great variability in knowledge regarding the reliability of the equipment they use to measure BP, with only 42% reporting the they know they are using an accurate BP monitor when it was validated against and accurate gage. Hence reliable BP measures require not only further training to improve knowledge and compliance with recommended procedures, but also understanding to the barriers for implementation as well as monitoring of assessment procedures [20].
Despite high rates of inaccurate BP assessment, almost all of those surveyed understand the importance of BP assessment and see it as a skill that is essential for medical assistants, nurses and physicians, as well as an essential part of the physical exam. Although only a small proportion of those surveyed felt that BP skills did not need to be practiced, it is clear that most medical professions may not receive proper initial instruction of BP measuring skills and may not receive any additional training or regular reassessment of their BP skills,[21] given the majority of respondents (84%) trusted their BP assessment in the clinic.
3.1. Strengths and limitations
Limitations of this study include use of self-reporting via electronic survey rather than skills assessment, although the findings are supported by previous reports of the known BP measurement challenges. Using electronic survey has many advantages such as being rapid and also allow control of order in which questions are answered to prevent respondents returning to change answers [22]. Our findings provide further support for the awareness-to-adherence model used by Heneghan et al. [23]. in which recommendations or practices may not be adopted despite awareness. Another limitation includes responder bias, since those who voluntarily completed the survey may be interested in hypertension assessment, in contrast with those that did not. This respondent bias would likely underestimate the true inaccuracy in BP assessment. Additionally, we did not collect data on gender of respondents or years in practice, that may influence BP measurement skills. We also did not identify whether respondents accessed the survey via their professional society or via social media. We were also unable to estimate the response rate and have no true denominator. Lastly, our definition of accurate BP assessment does not encompass all the variables that can affect the accuracy of BP measurement, but as noted, was a very liberal assessment of clinical skills. Even with this, it is apparent that BP assessment skills need refinement in clinical practice.
4. Conclusion
The results of this study demonstrate that accurate BP assessment continues to remain suboptimal in clinical practice, including by cardiologists and preventive cardiologists. The potential impact on our patients is difficult to estimate but given the importance of the diagnosis and treatment of hypertension on reducing cardiovascular disease and kidney disease, the importance of these simple skills cannot be overstated. Reliability of BP assessment in clinic requires continued education, identifying the barriers to implementation of recommendations and engagement of the entire team to improve BP assessment, which will lead to improved cardiovascular outcomes for our patients.
CRediT authorship contribution statement
Martha Gulati: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft. Lori-Ann Peterson: Data curation, Project administration, Writing – review & editing. Anastasia Mihailidou: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank the American Society for Preventive Cardiology (ASPC), the Society for Cardiac Computed Tomography (SCCT) and the High Blood Pressure Research Council of Australia (HBPRCA) for helping us distribute this survey to its members. We would also like to thank those cardiologists across the world who took the time to complete our survey.
Footnotes
Conflicts of Interest: None
Funding: None
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajpc.2021.100280.
Appendix. Supplementary materials
References
- 1.Collaborators GBDRF Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones D.W., Appel L.J., Sheps S.G., Roccella E.J., Lenfant C. Measuring blood pressure accurately: new and persistent challenges. JAMA. 2003;289:1027–1030. doi: 10.1001/jama.289.8.1027. [DOI] [PubMed] [Google Scholar]
- 3.Lewington S., Clarke R., Qizilbash N., Peto R., Collins R., Prospective Studies C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 4.Whelton P.K., Carey R.M., Aronow W.S., Casey D.E., Collins K.J., Dennison Himmelfarb C., DePalma S.M., Gidding S., Jamerson K.A., Jones D.W., MacLaughlin E.J., Muntner P., Ovbiagele B., Smith S.C., Spencer C.C., Stafford R.S., Taler S.J., Thomas R.J., Williams K.A., Williamson J.D., Wright J.T. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138:e484–e594. doi: 10.1161/CIR.0000000000000596. [DOI] [PubMed] [Google Scholar]
- 5.Williams B., Mancia G., Spiering W., Agabiti Rosei E., Azizi M., Burnier M., Clement D.L., Coca A., de Simone G., Dominiczak A., Kahan T., Mahfoud F., Redon J., Ruilope L., Zanchetti A., Kerins M., Kjeldsen S.E., Kreutz R., Laurent S., Lip G.Y.H., McManus R., Narkiewicz K., Ruschitzka F., Schmieder R.E., Shlyakhto E., Tsioufis C., Aboyans V., Desormais I., Group ESD 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 6.Nerenberg K.A., Zarnke K.B., Leung A.A., Dasgupta K., Butalia S., McBrien K., Harris K.C., Nakhla M., Cloutier L., Gelfer M., Lamarre-Cliche M., Milot A., Bolli P., Tremblay G., McLean D., Padwal R.S., Tran K.C., Grover S., Rabkin S.W., Moe G.W., Howlett J.G., Lindsay P., Hill M.D., Sharma M., Field T., Wein T.H., Shoamanesh A., Dresser G.K., Hamet P., Herman R.J., Burgess E., Gryn S.E., Grégoire J.C., Lewanczuk R., Poirier L., Campbell T.S., Feldman R.D., Lavoie K.L., Tsuyuki R.T., Honos G., Prebtani A.P.H., Kline G., Schiffrin E.L., Don-Wauchope A., Tobe S.W., Gilbert R.E., Leiter L.A., Jones C., Woo V., Hegele R.A., Selby P., Pipe A., McFarlane P.A., Oh P., Gupta M., Bacon S.L., Kaczorowski J., Trudeau L., Campbell N.R.C., Hiremath S., Roerecke M., Arcand J., Ruzicka M., Prasad G.V.R., Vallée M., Edwards C., Sivapalan P., Penner S.B., Fournier A., Benoit G., Feber J., Dionne J., Magee L.A., Logan A.G., Côté A.M., Rey E., Firoz T., Kuyper L.M., Gabor J.Y., Townsend R.R., Rabi D.M., Daskalopoulou S.S., Canada H. Hypertension Canada's 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol. 2018;34:506–525. doi: 10.1016/j.cjca.2018.02.022. [DOI] [PubMed] [Google Scholar]
- 7.Le Pailleur C., Helft G., Landais P., Montgermont P., Feder J.M., Metzger J.P., Vacheron A. The effects of talking, reading, and silence on the "white coat" phenomenon in hypertensive patients. Am J Hypertens. 1998;11:203–207. doi: 10.1016/s0895-7061(97)00403-2. [DOI] [PubMed] [Google Scholar]
- 8.Fagius J., Karhuvaara S. Sympathetic activity and blood pressure increases with bladder distension in humans. Hypertension. 1989;14:511–517. doi: 10.1161/01.hyp.14.5.511. [DOI] [PubMed] [Google Scholar]
- 9.Cushman W.C., Cooper K.M., Horne R.A., Meydrech E.F. Effect of back support and stethoscope head on seated blood pressure determinations. Am J Hypertens. 1990;3:240–241. doi: 10.1093/ajh/3.3.240. [DOI] [PubMed] [Google Scholar]
- 10.Pinar R., Ataalkin S., Watson R. The effect of crossing legs on blood pressure in hypertensive patients. J Clin Nurs. 2010;19:1284–1288. doi: 10.1111/j.1365-2702.2009.03148.x. [DOI] [PubMed] [Google Scholar]
- 11.Pinar R., Ataalkin S., Watson R. The effect of clothes on sphygmomanometric blood pressure measurement in hypertensive patients. J Clin Nurs. 2010;19:1861–1864. doi: 10.1111/j.1365-2702.2010.03224.x. [DOI] [PubMed] [Google Scholar]
- 12.Whelton P.K., Carey R.M., Aronow W.S., Casey D.E., Jr., Collins K.J., Dennison Himmelfarb C., DePalma S.M., Gidding S., Jamerson K.A., Jones D.W., MacLaughlin E.J., Muntner P., Ovbiagele B., Smith S.C., Jr., Spencer C.C., Stafford R.S., Taler S.J., Thomas R.J., Williams K.A., Sr., Williamson J.D., Wright J.T., Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 13.Tugrul E., Karacam Z. Comparison of blood pressure and pulse readings measured on a bare arm, a clothed arm and on an arm with a rolled-up sleeve. Int J Nurs Stud. 2020;105 doi: 10.1016/j.ijnurstu.2019.103506. [DOI] [PubMed] [Google Scholar]
- 14.Adiyaman A., Verhoeff R., Lenders J.W., Deinum J., Thien T. The position of the arm during blood pressure measurement in sitting position. Blood Press Monit. 2006;11:309–313. doi: 10.1097/01.mbp.0000218007.57957.56. [DOI] [PubMed] [Google Scholar]
- 15.Mariotti G., Alli C., Avanzini F., Canciani C., Di Tullio M., Manzini M., Salmoirago E., Taioli E., Zussino A., Radice M. Arm position as a source of error in blood pressure measurement. Clin Cardiol. 1987;10:591–593. doi: 10.1002/clc.4960101016. [DOI] [PubMed] [Google Scholar]
- 16.Thavarajah S., White W.B., Mansoor G.A. Terminal digit bias in a specialty hypertension faculty practice. J Hum Hypertens. 2003;17:819–822. doi: 10.1038/sj.jhh.1001625. [DOI] [PubMed] [Google Scholar]
- 17.Nietert P.J., Wessell A.M., Feifer C., Ornstein S.M. Effect of terminal digit preference on blood pressure measurement and treatment in primary care. Am J Hypertens. 2006;19:147–152. doi: 10.1016/j.amjhyper.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 18.Iida M., Ishiguro Y., Ueda N., Honjo H. Inter-arm difference of systolic blood pressure measured by automated double-cuff device is associated with arterial stiffness in patients with hypertension. Blood Press Monit. 2020;25:26–33. doi: 10.1097/MBP.0000000000000416. [DOI] [PubMed] [Google Scholar]
- 19.Clark C.E., Taylor R.S., Butcher I., Stewart M.C., Price J., Fowkes F.G., Shore A.C., Campbell J.L. Inter-arm blood pressure difference and mortality: a cohort study in an asymptomatic primary care population at elevated cardiovascular risk. Br J Gen Pract. 2016;66:e297–e308. doi: 10.3399/bjgp16X684949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elias M.F., Goodell A.L. Human errors in automated office blood pressure measurement: still room for improvement. Hypertension. 2021;77:6–15. doi: 10.1161/HYPERTENSIONAHA.120.16164. [DOI] [PubMed] [Google Scholar]
- 21.Hwang K.O., Aigbe A., Ju H.H., VC Jackson, Sedlock E.W. Barriers to accurate blood pressure measurement in the medical office. J Prim Care Community Health. 2018;9 doi: 10.1177/2150132718816929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Braithwaite D., Emery J., De Lusignan S., Sutton S. Using the Internet to conduct surveys of health professionals: a valid alternative? Fam Pract. 2003;20:545–551. doi: 10.1093/fampra/cmg509. [DOI] [PubMed] [Google Scholar]
- 23.Heneghan C., Perera R., Mant D., Glasziou P. Hypertension guideline recommendations in general practice: awareness, agreement, adoption, and adherence. Br J Gen Pract. 2007;57:948–952. doi: 10.3399/096016407782604965. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.