Abstract
Background
Black men and women suffer from disparities in morbidity and mortality from hypertension, cardiovascular disease, and currently, COVID-19. These conditions are associated with social determinants of health and psychosocial stress. While previous trials demonstrated that stress reduction with meditation lowered BP in the grade I range in Black adults, there is a paucity of evidence for high normal and normal BP.
Objective
This randomized controlled trial was conducted to evaluate the effect of stress reduction with the Transcendental Meditation (TM) technique in Black adults with high normal BP and normal BP using international classifications.
Methods
A total of 304 Black men and women with high normal (130–139/85–89 mm Hg) and normal BP (120–129/80–84 mm Hg) were randomized to either TM or health education (HE) groups. BP was recorded at 3, 6, 9, 12, 24, 30 and 36 months after baseline. Linear mixed model analysis was conducted to compare the BP change between TM and HE participants in the high-normal BP and normal-BP groups. Survival analysis for hypertensive events was conducted.
Results
After an average of 19.9 ± 11.1 months follow-up, TM participants in the high-normal BP group showed significantly lower posttest SBP (-3.33 mm Hg, p = 0.045). There was no difference in DBP (-0.785 mm Hg, p = 0.367) compared to HE participants. In the normal BP group, the SBP and DBP were not different between the TM and HE participants. The hazard ratio for hypertensive events was 0.52 (p = 0.15) in the high normal BP group (7 TM vs 13 HE) with no difference in the normal BP group
Conclusion
This RCT found that meditation lowered systolic BP in Black men and women with high normal BP but not in normal BP participants. These results may be relevant to reducing health disparities in CVD and related co-morbidities.
Keywords: Blood pressure, High normal BP, Stress reduction, Lifestyle modification, Meditation, Health education
1. Introduction
Black adults in the United States suffer from disproportionately high mortality compared to whites [1,2]. The largest contributor to this disparity is cardiovascular disease (CVD) [3]. Despite overall decline in CVD mortality in the general population in recent decades, Black adults continue to have the highest total burden of CVD from coronary heart disease (CHD), cerebrovascular disease, and heart failure compared to other racial/ethnic groups [1,3]. While Black men and women have higher rates of several CVD risk factors, hypertension arguably confers the greatest risk [3,4]. The prevalence of high blood pressure (≥130/80 mm Hg) in Black adults is 56% and the incidence is 75% by age 55. These rates are 30% and 60% higher respectively than in white adults and is amongst the highest in the world [4,5]. Estimates are that hypertension accounts for 50% of the disparities in mortality between Black and white adults [6,7]. These racial disparities begin in youth and track into adulthood [8].
In 2020, coronavirus disease 2019 (COVID-19) was the leading cause of death in the United States [9,10]. Death rates from COVID-19 were 200–300% higher in Black Americans than white Americans [11]. Co-morbid hypertension and CVD increase the risk for COVID-19 mortality [12,13]. Therefore, the Black-white racial disparity in COVID-19 morbidity and mortality may be due, at least in part, to the disproportionate rates of high blood pressure in Black Americans [11,[14], [15], [16]].
Two recent American Heart Association (AHA) scientific statements conclude that social determinants of health (SDOH) and associated psychosocial stress contribute to these racial disparities in hypertension and CVD [3,17]. This conclusion is echoed by the American Psychological Association (APA) report on health disparities [18]. The 2020 International Society of Hypertension (ISH) Global Hypertension Practice Guidelines acknowledge the association of stress with hypertension and potential role of stress reduction for hypertension [19]. The AHA, APA, and ISH statements all recommend stress management interventions, such as meditation to reduce health disparities in high risk groups, such as Black adults [3,17,18]. While there have been trials on meditation for treatment of grade I hypertension in Black Americans conducted by our collaborative team and others [20], [21], [22], [23], to our knowledge, there have been no published clinical trials on stress reduction for high normal or normal BP in Black adults. This is particularly relevant to clinical practice because lower levels of high blood pressure are recommended for intervention, especially nonpharmacologic intervention in the latest American, European and international clinical practice guidelines [19,[24], [25], [26]]
In response to the renewed recognitions of: 1. racial disparities in health, 2. associations of racial disparities in CVD health to social determinants of health and 3. the clinical importance of high normal and normal BP, we analyzed results from an earlier clinical trial on effects of stress reduction in Black men and women with high normal and normal BP [11,14,19,27,28]. This research was conceived, conducted and reported in consideration of best practices for research in racial and ethnic health disparities [29].
2. Methods
2.1. Overall design
This was a randomized, controlled, single-blind clinical trial that compared the efficacy of stress reduction with the Transcendental Meditation (TM) technique to a health education (HE) control in two groups of Black adults without known CVD. The first group had high normal BP (130–139 SBP and/or 85–89 DBP mm Hg). The second group had normal BP (120–129 mm Hg SBP and/or 80–84 mm Hg DBP). The BP classifications for this study were originally based on the classification system of the Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 6) [30,31]. This classification is consistent with the BP strata used in the global hypertension practice guidelines of the International Society of Hypertension [19], and the guidelines of the European Society of Cardiology/European Society of Hypertension [24] and are similar to the 2017 American College of Cardiology/American Heart Association definitions of stage I hypertension and elevated BP [32,33].
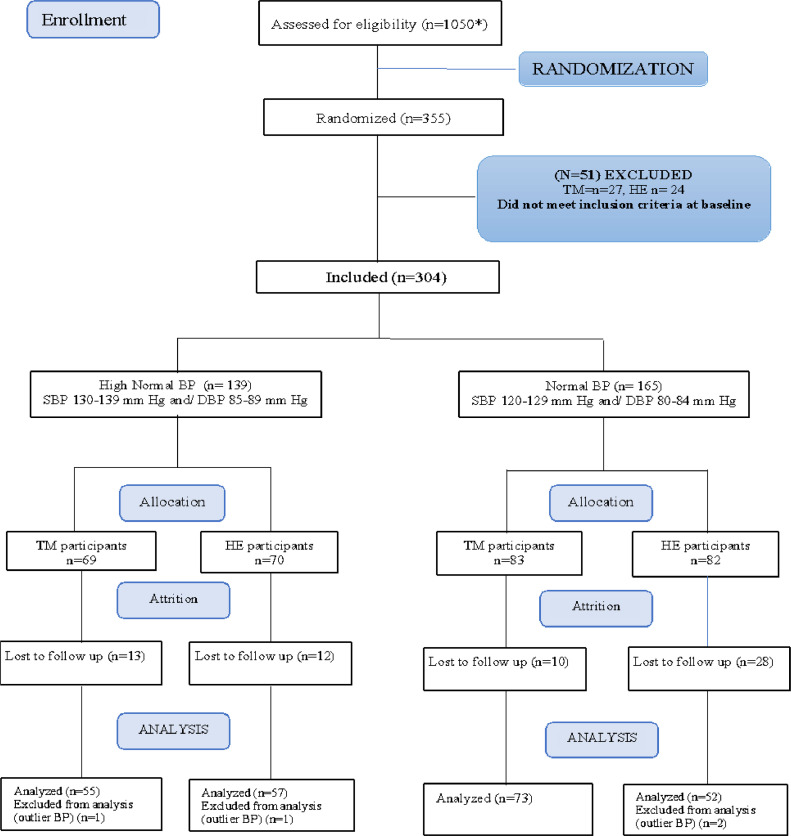
The protocol was modified in the first year of the study. That is, the original protocol called for the inclusion of participants with high normal BP. However, in the first year of the trial, the executive committee approved addition of participants with normal BP. This modification allowed the subsequent analysis of high normal BP and normal BP groups in parallel (see Fig. 1, Participant Flow Chart).
Fig. 1.
Participant Flow Chart.
This randomized controlled trial was conducted between January 1999 and April 2005. The clinical center for the trial was the Department of Medicine, Medical College of Wisconsin (MCW), Milwaukee, Wisconsin. The administrative and data coordinating center was the Institute for Natural Medicine and Prevention, Fairfield, Iowa. Written informed consent was provided by all participants. The trial was approved by the institutional review boards of both institutions.
2.2. Subjects
The sample included self-identified Black women and men, aged 21–75 years with either high normal BP (130–139 mm Hg and/or DBP 85–89 mm Hg) or normal BP (SBP 120–129 mm Hg and/DBP 80–84 mm Hg) without antihypertensive medications. Participants were excluded if they had a history of cardiovascular disease: myocardial infarction, angina, peripheral artery disease, heart failure, stroke, renal failure, diabetes mellitus, major psychiatric disorder or substance abuse disorder or other life-threatening disease. In addition, potential participants who were planning to move out of the study area, unwilling to accept randomization or unwilling to give informed consent were excluded.
2.3. Study protocol
Participants were assessed during the baseline period that comprised three BP and behavioral assessment visits on three separate days. Stratified block randomization (with stratification for gender, age, and baseline levels of SBP and DBP) was used to assign participants in a 1:1 ratio to either meditation or health education groups. The random allocation sequence was based on computer-generated random numbers. Allocation concealment was maintained by the study biostatistician, who allocated each participant to treatment intervention and informed the study coordinator of treatment assignments, who then notified the participants.
Investigators, staff assessing outcomes, and data management staff were blinded to treatment group assignment. Participants were posttested for at 3, 6, 12, 18, 24, 30, and 36 months after baseline for blood pressure and at 12, 24 and 36 months for behavioral and psychological factors.
2.4. Outcomes
The primary outcome was office blood pressure, measured with a mercury sphygmomanometer using standard clinical trial technique [34,35]. A trained research technician measured BP in the supported right arm after the participant remained seated and resting for 5 min. Participants were told not to practice any stress reduction technique immediately before or during BP recording. Three successive readings were taken at one-minute intervals. To control for possible whitecoat BP variability, the first reading was discarded and the average of the last two readings was used in the data analysis. All BP observers were trained and certified using the Shared Care Research and Education BP Quality assurance program [36] and were re-certified every 6 months by direct observation of performance using AHA measurement guidelines [37] and by double stethoscope and video testing of the ability to record and interpret Korotkoff sounds.
Secondary outcomes were hypertensive events, heart rate, BMI, physical activity, anger expression and adherence. Hypertensive events were defined as SBP ≥140 and/or DBP ≥90 mm Hg on two successive occasions or first prescribed use of antihypertensive medications. Heart rate was measured manually by the research technician in the right radial artery. Anger expression was assessed by anger-in, anger-out and anger-total scores with the \ State-Trait Anger Scale [38]. In previous studies, anger expression was consistently associated with high BP [39,40]. Physical activity was assessed by standardized questionnaire derived from the Minnesota Physical Activity Questionnaire [41].
Intervention adherence was measured using a blinded self-report form at each clinic visit. Meeting attendance was recorded at each visit session by the instructors for both the TM and HE groups.
2.5. Interventions
The two study interventions were matched for attention, duration, expectancy, and other nonspecific factors. Both the meditation and health education interventions had previously demonstrated acceptability and feasibility in Black adults with hypertension [20], [21], [22]. All participants continued their usual medical care during the trial.
The Transcendental Meditation (TM) technique was a standardized and validated meditation technique that is used for stress reduction that is practiced twice a day for 20 min while sitting comfortably with eyes closed. [42]. Instruction in the TM technique involved a seven-step course over five sessions of 1.5 h each as previously described [22]. This included an introduction and brief personal interview (session 1), personal instruction (session 2), and three follow-up meetings in small groups (sessions 3,4, and 5). The last four sessions were conducted over four consecutive days. Participants were advised to practice the technique for 20 min twice daily at home for the duration of the study. Follow-up refresher meetings were conducted 1 week later, every 2 weeks for 2 months, and once a month for the duration of the study. There were no instructions to modify lifestyle in the meditation course. A trained and certified instructor of Transcendental Meditation taught the course.
The health education (HE) intervention comprised a series of classes and group discussions on lifestyle modification for high blood pressure and CVD prevention that matched the meditation course in time and attention. The curriculum was based on methods of the Trials of Hypertension Prevention [43,44]. This group received written materials, structured presentations, didactic instructions and group support for modifying the major cardiovascular risk factors including salt restriction, weight reduction, aerobic exercise, alcohol, and smoking cessation. The topic of stress and BP was described, but participants did not learn a specific stress reduction technique. The HE group participants attended a 90-minute meeting once a week for the first 5 weeks, followed by bi-weekly sessions for two months, and then once a month for the duration of the study. The HE intervention was taught by a qualified health educator.
2.6. Data analysis
Analyses were conducted for the high-normal BP and normal BP groups in parallel (Fig. 1). All participants, regardless of their adherence to the intervention protocols, who completed at least one posttest were analyzed according to the modified intention-to-treat (ITT) principle [45]. Baseline characteristics of the TM and HE participants were compared with t-tests and chi-square tests. The changes in primary and secondary outcomes between TM and HE participants were calculated by linear mixed model analysis. The effects of attrition on the composition of the groups was evaluated by t-test of the baseline variables with treatment and attrition versus non-attrition as grouping variables. Data was checked for extreme outliers using the method of Hoaglin and Iglewicz in SPSS [46].
Changes in systolic and diastolic BP between TM and HE interventions in the high normal and normal BP groups were analyzed as the adjusted difference in posttest BP between TM and HE using linear mixed model analysis. Adjustment factors were significant predictors for SBP (baseline SBP, age, heart rate, education, and income). For DBP, baseline DBP, age, heart rate, income, and education were covariates. For heart rate, the anger-in, anger-out, and anger-total, the baseline value of the respective variables were used as covariates.
For analysis of hypertensive events, we constructed Kaplan–Meier curves according to intervention (TM and HE) group using time-to-first event. Hazard ratios (HRs) and 95% confidence intervals (CIs) were estimated using the Cox proportional hazard model. All data analyses were conducted using SPSS software (IBM SPSS Statistics, v25).
3. Results
The participant flow diagram is presented in Fig. 1. Of the 304 eligible and randomized participants, 139 participants were in the high normal BP group (69 TM, 70 HE). Of these, 114 or 82% completed follow-up testing. Two participants’ baseline BP were extreme outliers and were removed from the analysis set, resulting in 112 participants in the final analysis of high normals. There were 165 participants in the normal BP group (83 TM, 82 HE). Of these, 127 or 77% completed follow-up testing. Two participants' baseline BP were in the extreme outlier range and were excluded, resulting in 125 participants in the final analysis of normals.
3.1. Baseline characteristics
Baseline characteristics of the high normal BP group and the normal BP group participants are presented in Tables 1 and 2.
Table 1.
Baseline Characteristics of High-Normal BP Group.
| Variable | Intervention | N | Mean | SD | p-value |
|---|---|---|---|---|---|
| Age (years) | TM | 55 | 43.4 | 9.3 | 0.545 |
| HE | 57 | 44.5 | 10.9 | ||
| Females | TM | 29 (52.7%) | 0.717 | ||
| HE | 32 (56.1%) | ||||
| BMI kg/m2 | TM | 55 | 30 | 7 | 0.076 |
| HE | 52 | 32.6 | 8.2 | ||
| Exercise (hours/day) | TM | 54 | 7.3 | 4.3 | 0.801 |
| HE | 54 | 7.5 | 4.1 | ||
| Education (years) | TM | 53 | 12.1 | 3.3 | 0.501 |
| HE | 53 | 12.8 | 3.2 | 0.402 | |
| Income (annual) | TM | 55 | $18,650 | ||
| HE | 55 | $22,400 | |||
| SBP mm Hg | TM | 55 | 128.7 | 6.5 | 0.298 |
| HE | 57 | 130 | 3.9 | ||
| DBP mm Hg | TM | 55 | 84.2 | 4.8 | 0.059 |
| HE | 57 | 82.7 | 7.3 | ||
| HR bpm | TM | 55 | 73.7 | 7 | 0.813 |
| HE | 53 | 73.4 | 0.9 | ||
| Anger | TM | 55 | 2.7 | 0.9 | 0.669 |
| In score | HE | 55 | 2.8 | 0.7 | |
| Anger | TM | 55 | 2.5 | 0.7 | 0.308 |
| Out score | HE | 55 | 2.6 | 14.2 | |
| Anger | TM | 55 | 29.4 | 12.5 | 0.985 |
| Total score | HE | 55 | 29.5 |
As seen in Table 1, the mean SBP for the high-normal group was 129.3 ± 6.8 mm Hg and DBP were 83.4 ± 4.3 mm Hg; the participants were aged (43.9 ± 10.0 years), and there were 54.5% (n = 61) females.
Table 2.
Baseline Characteristics of Normal BP Group.
| Variable | Intervention | N | Mean | SD | P-value |
|---|---|---|---|---|---|
| Age (years) | TM | 73 | 41.38 | 9 | 0.878 |
| HE | 52 | 41.63 | 9 | ||
| Females | TM | 44 (60.3%) | 0.772 | ||
| HE | 30 (57.7%) | ||||
| BMI Kg/m2 | TM | 70 | 30.99 | 8.3 | 0.435 |
| HE | 48 | 32.14 | 7.5 | ||
| Exercise (hours/day) | TM | 68 | 7.65 | 4.8 | 0.872 |
| HE | 50 | 7.52 | 3.7 | ||
| SBP mm Hg | TM | 73 | 122.59 | 4.7 | 0.673 |
| HE | 52 | 122 | 5.4 | ||
| DBP mm Hg | TM | 73 | 77.92 | 5.3 | 0.811 |
| HE | 52 | 78.15 | 5.2 | ||
| HR bpm | TM | 71 | 72.58 | 8.2 | 0.257 |
| HE | 48 | 74.35 | 8.4 | ||
| Anger In score | TM | 71 | 2.59 | 0.9 | 0.234 |
| HE | 49 | 2.78 | 0.8 | ||
| Anger Out score | TM | 71 | 2.59 | 0.8 | 0.619 |
| HE | 49 | 2.66 | 0.6 | ||
| Anger Total score | TM | 71 | 27.73 | 12.5 | 0.383 |
| HE | 49 | 29.75 | 12.4 | ||
| Income (annual) | TM | 72 | $23,490 | ||
| HE | 51 | $20,833 | |||
| Education (years) | TM | 56 | 12.1 | ||
| HE | 55 | 12.8 |
As seen in Table 2 for the normal BP group, the mean SBP was 122.3 ± 5.0 mm Hg and DBP were 78.0 ± 5.2 mm Hg; the participants were aged (41.5 ± 8.8 years), and there were 59.2% (n = 74) females.
For the comparison of completers and attritors in high-normal BP group, there was no significant difference between participants who completed posttesting (n = 114) and those who did not (n = 25) on the primary or secondary outcome variables at baseline. For the comparison of completers and attritors in normal BP group, there was no significant difference between subjects who completed post-testing and those who did not on the primary or secondary outcome variables at baseline.
3.2. Outcomes in high normal BP group
Changes in the primary and secondary outcomes for the high normal group are presented in Table 3.
Table 3.
Outcomes in High Normal BP Group.
| Variable | TM Posttest Adjusted Mean (SEM) | HE Posttest Adjusted Mean (SEM) | Adjusted Mean Difference (SEM) | 95% Confidence Interval | p value | |
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||
| N (Sample size) | 55 | 57 | ||||
| Follow-up (months) | 20.1 ± 9.9 | 19.7 ± 12.2 | 0.4 ± 2.1 | −3.8 | 4.6 | .850 |
| SBP (mmHg) | 126.7 ± 1.1 | 130 ± 1.2 | −3.2 ± 1.6 | −6.4 | −0.7 | .045* |
| DBP (mm Hg) | 81.2 ± 1.0 | 82.9 ± 1.1 | −0.92 ± 1.5 | −3.8 | 2.0 | .533 |
| HR (bpm) | 71.8 ± 0.7 | 72.3 ±.6 | −0.50 ±.9 | −2.2 | 1.2 | .151 |
| Anger In | 2.5 ±.10 | 2.7 ±.1 | −0.19 ±.1 | −0.5 | 0.1 | .559 |
| Anger Out | 2.7 ± 0.1 | 2.7 ±.1 | −0.06 ±.1 | −0 0.3 | .19 | .173 |
| Anger Total | 28.9 ± 1.6 | 30.3 ± 1.7 | −1.3 ± 2.2 | −5.8 | 3.1 | .649 |
| Body Mass Index (BMI, kg/m2) | 29.9 ± 7 | 32.5 ± 8.1 | −2.6 ± 1.5 | −5.5 | 0.3 | .545 |
| Physical activity (active hours/day) | 7.3 ± 4.4 | 7.5 ± 4.0 | −0.2±.8 | −1.8 | 1.4 | .076 |
| Hypertensive events (N and hazard ratio) | 7 | 13 | 0.52 | 0.21 | 1.13 | .15 |
| Adherence- Home practice (at least once/day) | 84% | 90% | .371 | |||
| Adherence - Meeting attendance (% total) | 48% | 42% | .203 | |||
p < 0.05 level of significance.
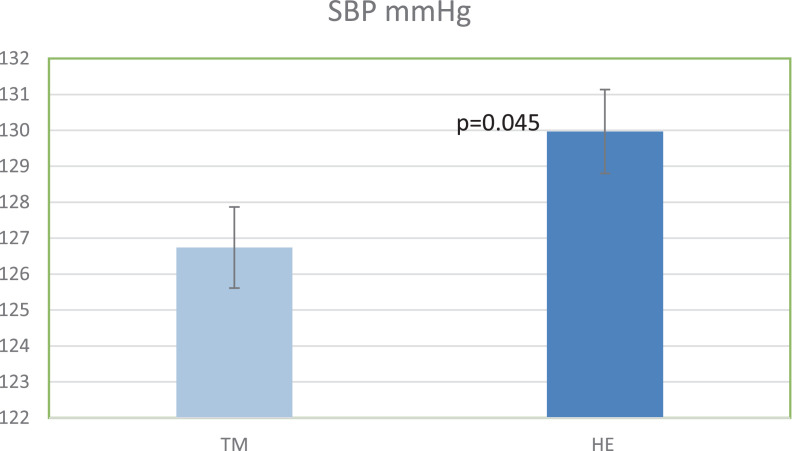
In the high normal BP group, the average follow-up period was 19.9 ± 11.1 months (range = 3–36 months). There was a significantly greater SBP reduction in the TM compared to HE group of −3.2 ± 1.6 mm Hg, p = 0.045) (Fig. 2). The adjusted DBP difference of (−0.9 mm Hg, p = 0.53) was not significant between TM or HE participants (Table 3).
Fig. 2.
Comparison of Posttest SBP between TM and HE Participants in the High-Normal BP group.
There were 7 hypertensive events in the group assigned to a TM intervention (12.7%) and 13 in the group assigned to HE (22.8%). The hazard ratio was 0.523 (95% confidence interval [CI], 0.208 to 1.1313, p = 0.15) for the high normal BP group. Anger in, anger out and anger total change scores were not different between the TM and HE participants (Table 3)
Regarding treatment adherence in the high normal BP group, 84% of the TM participants reported practicing meditation at home at least once a day for the duration of the study while 90% of the HE participants reported adherence with at least one recommended healthful activity at home at least once a day. For meeting attendance in the high normal BP groups, the TM participants attended 48% of all possible meetings compared to 42% for the HE group.
3.3. Outcomes in the normal BP group
The follow-up period averaged 13.84±10.13, SD months (range = 3–36 months). The linear mixed model analysis showed no difference in changes in SBP (0.84±1.55 mm Hg, P = 0.589), DBP (−0.23±1.14 mm Hg, P = 0.841), heart rate (1.16±.94 beats/ minute, p = 0.220), anger-in (−0.27±.14, p = 0.071), anger-out (−0.08±.12, p = 0.517), or anger total (−1.58±1.66, p = 0.342), or between the TM and the HE participants. There were 7 hypertensive events in the participants assigned to a TM intervention (9.5%) and 3 in the participants assigned to HE (5.7%) intervention in the Normal BP group. The hazard ratio was 1.768 (95% confidence interval [CI], 0.456 to 6.852, p = 0.40) for the normal BP group. (See table 4.)
Table 4.
Outcomes in the Normal BP Group.
| Variable | TM Posttest Adjusted mean (SEM) | HE Posttest Adjusted mean (SEM) | Adjusted Mean difference (SEM) | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | P value | ||||
| N (Sample size) | 73 | 52 | ||||
| Follow-up (months) | 19.8 ± 11.1 | 21.1 ± 10.6 | −1.3 ± 2 | −5.3 | 2.6 | .496 |
| SBP (mmHg) | 123.9 ± 1.1 | 123.1 ± 1.2 | −0.8 ± 1.5 | −2.2 | 3.9 | .589 |
| DBP (mm Hg) | 78.9 ±.8 | 79.1 ±.9 | −0.2 ± 1.1 | −2.5 | 2.0 | .841 |
| Hypertensive events (N and hazard ratio) | 7 | 3 | 1.77 | .46 | 6.85 | .402 |
| HR (bpm) | 72.6 ±.6 | 71.4 ±.7 | 1.2 ±.9 | −0.7 | 3.0 | .220 |
| Anger In | 2.5 ±.1 | 2.7 ±.1 | −0.3 ±.1 | −0.5 | .02 | .071 |
| Anger out | 2.7 ±.1 | 2.8 ±.1 | −0.1 ±.1 | −0.3 | .16 | .517 |
| Anger Total | 28.8 ± 1.1 | 30.4 ± 1.4 | −1.6 ± 1.7 | −4.9 | 1.7 | .342 |
| Body Mass Index (BMI, kg/m2) | 31±8.3 | 32.1 ± 7.5 | −1.1 ± 1.5 | −4.1 | 1.8 | .444 |
| Physical activity (hours/day) | 7.6 ± 4.8 | 7.5 ± 3.7 | .1±.8 | −1.5 | 1.7 | .872 |
| Adherence-home practice (at least once/day) | 67% | 100% | .423 | |||
| Adherence -meeting attendance (% total) | 47% | 40% | .008 | |||
For treatment adherence in those in the normal BP group, 67% of the TM participants reported regular home practice while the 100% of the HE group reported home practice of their healthy activity at least once a day. Regarding meeting attendance, 47% of the TM participants attended meetings compared to 40% of the HE group.
4. Discussion
In consideration of the substantial and persistent disparities in hypertension, CVD and related co-morbidities, such as COVID-19 in Black adults which are associated with social determinants of health and psychosocial stress, this randomized controlled trial compared the long-term effects of stress reduction with meditation to health education control in Black men and women with high normal and normal blood pressure. The results showed a significant reduction in systolic BP (−3.2 mm Hg) in the high normal group assigned to the meditation condition over an average of 20 months. The relative risk reduction of 48% for hypertensive events in the high normal BP meditation group did not reach statistical significance (HR = 0.52 (95% CI 0.20 to 1.13, p = 0.15). In the normal BP group, there were no significant changes in systolic or diastolic BP or hypertensive events. These findings suggest that the practice of Transcendental Meditation may lower BP over an average of 20 months in Black men and women with high normal BP and perhaps contribute to the prevention of hypertension, CVD and related health disparities.
The major international and national clinical practice guidelines recognize that systolic BP in the 130–139 mm Hg range confers excess risk for CVD mortality and morbidity[19, 24, 33]. Current International Society on Hypertension (ISH) and European Society of Cardiology/European Society of Hypertension (ESC/ESH) guidelines classifies this range as high normal BP while the American College of Cardiology/American Heart Association (ACC/AHA) guidelines classify it as stage I hypertension [19,24]. In the Prospective Studies Collaboration meta-analysis from one million adults, BP is “strongly and directly related to vascular and overall mortality to at least 115/75 mm Hg.” [47]. Recently, Whelton et al. confirmed that every 10 mm Hg increase in systolic BP above 90 mm Hg is associated with a 50% increase in risk for atherosclerotic CVD events [48]. Notably, the majority of CVD events occur in individuals with BP < 140/90 mm Hg. Amongst Black adults, the proportion of CVD events in individual with BP < 140/90 is nearly 60% [49].
There is a dearth of clinical trials of nonpharmacologic interventions in individuals with high normal BP. The Blood Pressure Lowering Treatment Trialists’ Collaboration (BPLTT) reported a meta-analysis of 48 trials of pharmacologic interventions with 350,000 participants with a wide range of baseline blood pressures [50,51][52]. In patients with systolic BP in the high normal range and with no prior CVD, as was the case for participants in this trial, a standardized reduction of 5 mm Hg SBP was associated a 10% reduction in major adverse cardiovascular events with [50,52,53]. For these reasons, the International, European and American guidelines all recommend lifestyle modification for individuals with high normal BP (or stage I equivalent), especially for those without concomitant CVD as was the case for participants in this trial. [19,24,54].
It has been reported that 40% of individuals with high normal BP develop hypertension in two years and 63% become hypertensive over four years [55]. The risk is especially high in Black men and women compared to other racial groups [56,57]. In our study, there was a 48% lower rate of hypertensive events over 20 months in the high normal TM group compared to controls, although this did not reach statistical significance (p = 0.15). However, the present study was not adequately powered to assess hypertensive event incidence due to limitations of both sample size and duration of follow-up. It is possible that this estimate of risk reduction may be used to gauge the effect size for future definitive trials. Previous studies with adequate statistical power reported significantly lower risk for major adverse cardiovascular events (MACE) in the TM groups compared to controls with high BP [22,58].
There have been few RCTs of lifestyle interventions for individuals with high normal BP and even fewer trials in Black populations. The Trials of Hypertension Prevention (TOHP II) evaluated effects of lifestyle modification with weight loss and sodium restriction in overweight people with high normal BP. The average net BP reductions in the lifestyle group were −2.0/−1.3 mm Hg after 18 months. The follow up period and BP severity in TOHP were similar to the current trial. The PREMIER trial employed lifestyle modification with the DASH diet in participants with high normal BP [59]. After six months of intervention, the net changes were −3.1/−1.8 mm Hg in the active intervention groups compared to controls. Therefore, in the present trial, the net reduction of −3.2 mm Hg systolic BP in the high normal group practicing meditation was similar to or greater than changes in somewhat similar trials of lifestyle modification in general population samples [59,60]. It may be possible that meditation is additive or synergistic with other lifestyle modifications for lowering BP. This may tested in future pragmatic clinical trials.
There have been several previous trials of lifestyle modification with Transcendental Meditation in Black adults with high BP [23,[61], [62], [63], [64]]. However, these were conducted in patient populations with BP > 140/90 mm Hg [20,21] or in patients with documented coronary heart disease [22] and thus substantially differ from the current trial of participants with either normal BP or high normal BP without known CVD.
In the meta-analyses of randomized controlled trials of Transcendental Meditation and blood pressure, the average reduction in SBP was – 4 to 5 mm Hg and in DBP – 2 to 3 mm Hg for all BP groups. At the same time, these meta-analyses found that changes were inversely associated with baseline BP [63]. That is, the higher the baseline BP, the greater BP reduction over time. Larger effects with higher baseline BPs may be related to the mechanisms of high BP and meditation. Excess sympathetic nervous system tone is a pathophysiologic mechanism for high BP [65], [66], [67], [68], [69]. Excess cardiovascular reactivity to stress is one possible mechanism for high BP [70]. Furthermore, one of the proposed etiologies for sympathetic overactivation in high BP is psychosocial stress [71], [72], [73]. The role of social determinants of health and psychosocial stress in contributing to high BP in Black men and women is well described [3,17].
Previous studies reported that Transcendental Meditation practice reduces sympathetic activation [74], [75], [76]. Therefore, it is plausible that meditation practice lowered SNS tone in the high normal BP group in the current trial. It is also possible that the normal BP group had insufficient SNS tone to be modified by a stress reducing practice.
There are several limitations to the present study. This trial included Black participants exclusively and the results may not generalize to other racial groups. However, other trials have reported lower BP with Transcendental Meditation practice in general population samples [77,78]. The blood pressure outcomes employed office BP readings with standardized clinical trial technique. Technological limitations did not allow the use of ambulatory BP monitoring. For the high normal BP group, subjects were recruited with systolic BP of 130–139 and/or diastolic BP of 85–89. However, the average baseline BP in this group was 129.3 ± 6.8 mm Hg and DBP were 83.4 ± 4.3 mm Hg. Although the group average is 1–2 mm less than the SBP or DBP entry criteria, we estimate that this is due to the distribution of subjects meeting either SBP and/or DBP criteria at entry. Adherence to the interventions were relatively high with approximately 80% of participants reporting daily practice of at least once per day. However, instructional meeting attendance was lower at approximately 50%. While there may be bias in self-reported adherence, we are unable to determine if meeting attendance or self-report is a more accurate indicator of adherence in this trial. Nevertheless, a strength of this study is that all subjects were included in the data analysis regardless of their level of adherence to the treatments and all BP recordings were masked to treatment assignment. The planned follow-up period was 36 months, yet the average follow-up was 20 months. Thus, there was attrition from long-term BP measurement visits. In the data analysis, subjects with a minimum of one follow-up visit regardless of treatment assignment or adherence were included in the modified intent-to-treat analysis which reduces bias [45]. The approximately 1 mm Hg reduction in DBP in the high normal group did not reach statistical significance. This differs from meta-analyses of TM and BP that did find significant differences in DBP [62,63]. This null finding may relate to insufficient power to detect a small difference in DBP. The possibility of confirmation bias cannot be ruled out in participants who volunteered for a randomized controlled trial of lifestyle interventions; however, the randomization process mitigated this effect [79]. At baseline, participants reported an average of seven hours of physical activity per day. It is possible that this level of physical activity was be related to occupations of the participants that required this level of physical activity since the average education was 12 years and average income was approximately $20,000 per year.
This study did not find a significant difference in anger between TM and HE participants. This null finding may be because of variability in the perception of anger. Studies have reported that TM decreases the physiological correlates of psychosocial stress factors including anger, such as sympathetic activity [80,81], plasma catecholamines [82], cortisol [83], and cardiovascular reactivity [76]. It is possible that while the perception of anger was not significantly changed, TM practice may have reduced the physiological correlates of psychosocial stress and BP. Future studies might examine neurophysiological and neuroendocrine mechanisms simultaneously with BP and psychosocial stress. Future studies might also address the combination of stress reduction with conventional health education compared to no treatment or behavioral controls.
5. Conclusion
This was the first randomized controlled trial of meditation as a lifestyle intervention in Black men and women with high normal BP and normal BP without known CVD. The results of this trial suggest that the efficacy of the TM technique in reducing systolic BP in patients with high normal BP,for whom pharmacotherapy may not be indicated, but who nevertheless are at elevated risk for CVD. Meditation may be a clinically useful lifestyle modification for reducing high blood pressure, CVD and associated co-morbidities in high-risk Black populations.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Funding
This study was supported by a grant from the National Institutes of Health - National Heart, Lung and Blood Institute, #R01HL060703. The study sponsor did not have a role in study design; the collection, analysis, and interpretation of data; in writing the report; nor in the decision to submit the article for publication.
Trial Registration
clinicaltrials.gov NCT# 0482150
Data Sharing Plan
Research data that documents, supports, and validates research findings will be made available upon request.
Contributor Information
Robert H. SCHNEIDER, Email: rschneider@prevention-research.org.
John W. SALERNO, Email: jsalerno@miu.edu.
References
- 1.Cunningham TJ, Croft JB, Liu Y, Lu H, Eke PI, Giles WH, Signs Vital. Vol. 66. 2017. Racial Disparities in Age-Specific Mortality Among Blacks or African Americans - United States, 1999-2015; pp. 444–456. (MMWR. Morbidity and mortality weekly report). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kochanek KD, Murphy SL, Xu J, Arias E. Deaths: Final Data for 2017. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2019;68(9):1–77. [PubMed] [Google Scholar]
- 3.Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG. Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. Circulation. 2017;136(21):e393–e423. doi: 10.1161/CIR.0000000000000534. [DOI] [PubMed] [Google Scholar]
- 4.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141(9):e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 5.Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation. 2016;134(6):441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Musemwa N, Gadegbeku CA. Hypertension in African Americans. Current Cardiology Reports. 2017;19(12):129. doi: 10.1007/s11886-017-0933-z. [DOI] [PubMed] [Google Scholar]
- 7.Maraboto C, Ferdinand KC. Update on hypertension in African-Americans. Progress in cardiovascular diseases. 2020;63(1):33–39. doi: 10.1016/j.pcad.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Bao W, Threefoot SA, Srinivasan SR, Berenson GS. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa Heart Study. Am J Hypertens. 1995;8(7):657–665. doi: 10.1016/0895-7061(95)00116-7. [DOI] [PubMed] [Google Scholar]
- 9.Top causes of death in the United States: Heart disease, cancer and COVID19. 2020 https://usafacts.org/articles/top-causes-death-united-states-heart-disease-cancer-and-covid-19/ Available from: [Google Scholar]
- 10.Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill L. Excess Deaths From COVID-19 and Other Causes, March-April 2020. JAMA. 2020;324(5):510–513. doi: 10.1001/jama.2020.11787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yancy CW, COVID-19. African Americans JAMA. 2020;323(19):1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 12.Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G. Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic. Journal of the American College of Cardiology. 2020;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. International journal of infectious diseases: IJID: official publication of the International Society for Infectious Diseases. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yancy CW, Academic Medicine. Black Lives Matter Time for Deep Listening. JAMA. 2020;324(5):435–436. doi: 10.1001/jama.2020.12532. [DOI] [PubMed] [Google Scholar]
- 15.Millett GA, Jones AT, Benkeser D, Baral S, Mercer L, Beyrer C. Assessing differential impacts of COVID-19 on black communities. Annals of epidemiology. 2020;47:37–44. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferdinand K, Batieste T, Fleurestil M. Contemporary and Future Concepts on Hypertension in African Americans: COVID-19 and Beyond. Journal of the National Medical Association. 2020;112(3):315–323. doi: 10.1016/j.jnma.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132(9):873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 18.American Psychological Association Working Group on Stress and Health Disparities. Stress and health disparities: Contexts, mechanisms, and interventions among racial/ethnic minority and low-socioeconomic status populations. 2017 [Google Scholar]
- 19.Unger T, Borghi C, Charchar F, Khan N, Poulter N, Prabhakaran D. 2020 International Society of Hypertension global hypertension practice guidelines. Journal of Hypertension. 2020;39:982–1004. doi: 10.1097/HJH.0000000000002453. [DOI] [PubMed] [Google Scholar]
- 20.Schneider RH, Staggers F, Alexander C, Sheppard W, Rainforth M, Kondwani K. A randomized controlled trial of stress reduction for hypertension in older African Americans. Hypertension. 1995;26:820–827. doi: 10.1161/01.hyp.26.5.820. [DOI] [PubMed] [Google Scholar]
- 21.Schneider R, Alexander C, Staggers F, Orme-Johnson D, Rainforth M, Salerno J. A randomized controlled trial of stress reduction in the treatment of hypertension in African Americans during one year. American Journal of Hypertension. 2005;18(1):88–98. doi: 10.1016/j.amjhyper.2004.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schneider R, Grim C, Rainforth M, Kotchen T, Nidich S, Gaylord-King C. Stress reduction in the secondary prevention of cardiovascular disease: randomized controlled trial of Transcendental Meditation and health education in Blacks. Circulation: Cardiovascular Quality and Outcomes. 2012;5:750–758. doi: 10.1161/CIRCOUTCOMES.112.967406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schneider R, Salerno J, Brook R. 2020 International Society of Hypertension global hypertension practice guidelines - lifestyle modification (editorial) Journal of Hypertension. 2020;38(11):2340. doi: 10.1097/HJH.0000000000002625. [DOI] [PubMed] [Google Scholar]
- 24.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. Journal of Hypertension. 2018;36(10):1953–2041. doi: 10.1097/HJH.0000000000001940. [DOI] [PubMed] [Google Scholar]
- 25.Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2018;71(19):2199–2269. doi: 10.1016/j.jacc.2017.11.005. Jr. [DOI] [PubMed] [Google Scholar]
- 26.Gijon-Conde T, Sanchez-Martinez M, Graciani A, Cruz JJ, Lopez-Garcia E, Ortola R. Impact of the European and American guidelines on hypertension prevalence, treatment, and cardiometabolic goals. Journal of Hypertension. 2019;37(7):1393–1400. doi: 10.1097/HJH.0000000000002065. [DOI] [PubMed] [Google Scholar]
- 27.Brook RD, Appel LJ, Rubenfire M, Ogedegbe G, Bisognano JD, Elliott WJ. Beyond Medications and Diet: Alternative Approaches to Lowering Blood Pressure: A Scientific Statement From the American Heart Association. Hypertension. 2013;61:1360–1383. doi: 10.1161/HYP.0b013e318293645f. HYP.0b013e318293645f [pii] [DOI] [PubMed] [Google Scholar]
- 28.Levine GN, Lange RA, Bairey-Merz CN, Davidson RJ, Jamerson K, Mehta PK. Meditation and Cardiovascular Risk Reduction: A Scientific Statement From the American Heart Association. Journal of the American Heart Association. 2017;6(10) doi: 10.1161/JAHA.117.002218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Breathett K, Spatz ES, Kramer DB, Essien UR, Wadhera RK, Peterson PN. The Groundwater of Racial and Ethnic Disparities Research: A Statement From Circulation: Cardiovascular Quality and Outcomes. Circulation. Cardiovascular quality and outcomes. 2021;14(2) doi: 10.1161/CIRCOUTCOMES.121.007868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Committee Joint National. The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure (JNC VI) Archives of Internal Medicine. 1997;157(21):2413–2440. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 31.Stress Reduction and Hypertension Prevention in African Americans NCT#04821505. 2021 www.clinicaltrials.gov www.clinicaltrials.gov. Available from: [Google Scholar]
- 32.Whelton PK, Carey RM. The 2017 Clinical Practice Guideline for High Blood Pressure. JAMA. 2017 doi: 10.1001/jama.2017.18209. [pii] [DOI] [PubMed] [Google Scholar]
- 33.Qi Y, Han X, Zhao D, Wang W, Wang M, Sun J. Long-Term Cardiovascular Risk Associated With Stage 1 Hypertension Defined by the 2017 ACC/AHA Hypertension Guideline. Journal of the American College of Cardiology. 2018;72(11):1201–1210. doi: 10.1016/j.jacc.2018.06.056. [DOI] [PubMed] [Google Scholar]
- 34.Whelton PK, Kumanyika SK, Cook NR, Culter JA, Borhani N, Hennekens C. Efficacy of nonpharmacologic intervention in adults with high-normal blood pressure: Results of Phase I of the Trials of Hypertension Prevention. American Journal of Clinical Nutrition. 1997;50(5):652S–660S. doi: 10.1093/ajcn/65.2.652S. [DOI] [PubMed] [Google Scholar]
- 35.Kronmal RA, Rutan GH, Manolio TA, Borhani NO. Properties of the random zero sphygmomanometer. Hypertension. 1993;21(5):632–637. doi: 10.1161/01.hyp.21.5.632. [DOI] [PubMed] [Google Scholar]
- 36.Osrchega Y, Prineas R, Paulose-Ram R, Grim C, Willard G, Collins D. National Health and Examination Survey 1999-2000: Effect of observer training and protocol for standardization on reducing blood pressure measurement error. Journal of Clinical Epidemiology. 2003;56:768–774. doi: 10.1016/s0895-4356(03)00085-4. [DOI] [PubMed] [Google Scholar]
- 37.Frolich E, Grim C, Labarthe D, Maxwell M, Perloff D, Weidman W. Recommendations for Human Blood Pressure Determination by Sphygmomanometers: Report of a Special Task Force Appointed by the Steering Committee, American Heart Association, 1987. Hypertension. 1988;11(2):209A–222A. [Google Scholar]
- 38.Spielberger CD, Jacobs G, Russell S, Crane R. In: Advances in personality assessment. Butcher JN, Spileberger CD, editors. Erlbaum; Hillsdale: 1983. Assessmentof Anger: The State Trait Anger Scale; pp. 159–187. [Google Scholar]
- 39.Rutledge T, Hogan B. A quantitative review of prospective evidence linking psychological factors with hypertension development. Psychosomatic Medicine. 2002;64:758–766. doi: 10.1097/01.psy.0000031578.42041.1c. [DOI] [PubMed] [Google Scholar]
- 40.Schum JL, Jorgensen RS, Verhaeghen P, Sauro M, Thibodeau R, anger Trait. anger expression, and ambulatory blood pressure: a meta-analytic review. Journal of Behavioral Medicine. 2003;26(5):395–415. doi: 10.1023/a:1025767900757. [DOI] [PubMed] [Google Scholar]
- 41.Taylor T, Jacobs D, Schucker B, Knudsen J, Leon A, Debacker G. A questionaire for the assessment of leisure time physical activities. Journal of Chronic Diseases. 1978;31(12):741–755. doi: 10.1016/0021-9681(78)90058-9. [DOI] [PubMed] [Google Scholar]
- 42.Roth R. Simon and Schuster; New York: 2018. Strength in Stillness: The Power of Transcendental Meditation. [Google Scholar]
- 43.Trials of Hypertension Prevention Collaborative Research Group The effects of nonpharmacological interventions on blood pressure of persons with high normal levels—results of the trials of hypertension prevention, Phase I. JAMA. 1992;267(9):1213–1220. doi: 10.1001/jama.1992.03480090061028. [DOI] [PubMed] [Google Scholar]
- 44.The Trials of Hypertension Prevention Collaborative Research Group Effects of Weight Loss and Sodium Reduction Intervention on Blood Pressure and Hypertension Incidence in Overweight People With High-Normal Blood Pressure: The Trials of Hypertension Prevention, Phase II. Archives of Internal Medicine. 1997;157:657–667. [PubMed] [Google Scholar]
- 45.Dossing A, Tarp S, Furst DE, Gluud C, Wells GA, Beyene J. Modified intention-to-treat analysis did not bias trial results. Journal of Clinical Epidemiology. 2016;72:66–74. doi: 10.1016/j.jclinepi.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 46.Hoaglin D, Iglewicz B. Fine-tuning some resistant rules for outlier labeling. Journal of the American Statistical Association. 1987;82(400):1147–1149. [Google Scholar]
- 47.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Collaboration Prospective Studies. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903. doi: 10.1016/s0140-6736(02)11911-8. -13S0140673602119118 [pii] [DOI] [PubMed] [Google Scholar]
- 48.Whelton SP, McEvoy JW, Shaw L, Psaty BM, Lima JAC, Budoff M. Association of Normal Systolic Blood Pressure Level With Cardiovascular Disease in the Absence of Risk Factors. JAMA cardiology. 2020 doi: 10.1001/jamacardio.2020.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tajeu GS, Booth JN, 3rd, Colantonio LD, Gottesman RF, Howard G, Lackland DT. Incident Cardiovascular Disease Among Adults With Blood Pressure <140/90 mm Hg. Circulation. 2017;136(9):798–812. doi: 10.1161/CIRCULATIONAHA.117.027362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rahimi K, Canoy D, Nazarzadeh M, Salimi-Khorshidi G, Woodward M, Teo K. Investigating the stratified efficacy and safety of pharmacological blood pressure-lowering: an overall protocol for individual patient-level data meta-analyses of over 300 000 randomised participants in the new phase of the Blood Pressure Lowering Treatment Trialists' Collaboration (BPLTTC) BMJ Open. 2019;9(5) doi: 10.1136/bmjopen-2018-028698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rahimi K. Blood Pressure Lowering Treatment Trialists’ Collaboration (BPLTTC): Blood Pressure Lowering for Prevention of Cardiovascular Events across Different Levels of Blood Pressure in ESC Congress 2020. August 31, 2020 [Google Scholar]
- 52.Collaboration TBPLTT, Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet. 2021;397:1625–1636. doi: 10.1016/S0140-6736(21)00590-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rahimi K. ESC Congress 2020 – The Digital Experience. European Society of Cardiology; Sophia Antipolis, France: Aug 31, 2020. Pharmacological blood pressure-lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant meta-analysis of 48 randomized clinical trials and 348,854 participants. [Google Scholar]
- 54.Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017:2017HYP. doi: 10.1161/HYP.0000000000000065. 0000000000000065 [pii] [DOI] [PubMed] [Google Scholar]
- 55.Julius S, Nesbitt SD, Egan BM, Weber MA, Michelson EL, Kaciroti N. Feasibility of treating prehypertension with an angiotensin-receptor blocker. The New England Journal of Medicine. 2006;354(16):1685–1697. doi: 10.1056/NEJMoa060838. [DOI] [PubMed] [Google Scholar]
- 56.Kshirsagar AV, Carpenter M, Bang H, Wyatt SB, Colindres RE. Blood pressure usually considered normal is associated with an elevated risk of cardiovascular disease. The American Journal of Medicine. 2006;119(2):133–141. doi: 10.1016/j.amjmed.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 57.Carson AP, Howard G, Burke GL, Shea S, Levitan EB, Muntner P. Ethnic differences in hypertension incidence among middle-aged and older adults: the multi-ethnic study of atherosclerosis. Hypertension. 2011;57(6):1101–1107. doi: 10.1161/HYPERTENSIONAHA.110.168005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Schneider RH, Alexander CN, Staggers F, Rainforth M, Salerno JW, Hartz A. Long-term effects of stress reduction on mortality in persons >55 years of age with systemic hypertension. American Journal of Cardiology. 2005;95(9):1060–1064. doi: 10.1016/j.amjcard.2004.12.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Svetkey LP, Erlinger TP, Vollmer WM, Feldstein A, Cooper LS, Appel LJ. Effect of lifestyle modifications on blood pressure by race, sex, hypertension status, and age. Journal of Human Hypertension. 2005;19(1):21–31. doi: 10.1038/sj.jhh.1001770. [DOI] [PubMed] [Google Scholar]
- 60.Trials of Hypertension Collaborative Research Group Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidents in over weight people with high normal blood pressure: The Trials of Hypertension, Phase II. Archives of Internal Medicine. 1997;157:657–667. [PubMed] [Google Scholar]
- 61.Rainforth M, Schneider R, Nidich S, King C, Salerno J, Anderson J. Stress Reduction Programs in Patients with Elevated Blood Pressure: A Systematic Review and Meta-analysis. Current Hypertension Reports. 2007;9(6):520–528. doi: 10.1007/s11906-007-0094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Anderson J, Liu C, Kryscio R. Blood Pressure Response to Transcendental Meditation: a meta-analysis. American Journal of Hypertension. 2008;21(3):310–316. doi: 10.1038/ajh.2007.65. [DOI] [PubMed] [Google Scholar]
- 63.Bai Z, Chang J, Chen C, Li P, Yang K, Chi I. Investigating the effect of transcendental meditation on blood pressure: a systematic review and meta-analysis. Journal of Human Hypertension. 2015 doi: 10.1038/jhh.2015.6. jhh20156 [pii] [DOI] [PubMed] [Google Scholar]
- 64.Ooi SL, Giovino M, Pak SC. Transcendental meditation for lowering blood pressure: An overview of systematic reviews and meta-analyses. Complementary Therapies in Medicine. 2017;34:26–34. doi: 10.1016/j.ctim.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 65.Grassi G. Assessment of sympathetic cardiovascular drive in human hypertension: achievements and perspectives. Hypertension. 2009;54(4):690–697. doi: 10.1161/HYPERTENSIONAHA.108.119883. [DOI] [PubMed] [Google Scholar]
- 66.Smith PA, Graham LN, Mackintosh AF, Stoker JB, Mary DA. Relationship between central sympathetic activity and stages of human hypertension. American Journal of Hypertension. 2004;17(3):217–222. doi: 10.1016/j.amjhyper.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 67.Hering D, Kara T, Kucharska W, Somers VK, Narkiewicz K. Vol. 22. Blood Pressure; 2013. pp. 183–187. (High-normal blood pressure is associated with increased resting sympathetic activity but normal responses to stress tests). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Palatini P, Julius S. The role of cardiac autonomic function in hypertension and cardiovascular disease. Current Hypertension Reports. 2009;11(3):199–205. doi: 10.1007/s11906-009-0035-4. [DOI] [PubMed] [Google Scholar]
- 69.Mancia G, Bousquet P, Elghozi JL, Esler M, Grassi G, Julius S. The sympathetic nervous system and the metabolic syndrome. Journal of Hypertension. 2007;25(5):909–920. doi: 10.1097/HJH.0b013e328048d004. [DOI] [PubMed] [Google Scholar]
- 70.Abramson J, Berger A, Krumholz HM, Vaccarino V. Depression and risk of heart failure among older persons with isolated systolic hypertension. Archives in Internal Medicine. 2001;161(14):1725–1730. doi: 10.1001/archinte.161.14.1725. ioi00718 [pii] [DOI] [PubMed] [Google Scholar]
- 71.Liu MY, Li N, Li WA, Khan H. Association between psychosocial stress and hypertension: a systematic review and meta-analysis. Neurological research. 2017;39(6):573–580. doi: 10.1080/01616412.2017.1317904. [DOI] [PubMed] [Google Scholar]
- 72.Valenzuela PL, Carrera-Bastos P, Galvez BG, Ruiz-Hurtado G, Ordovas JM, Ruilope LM. Lifestyle interventions for the prevention and treatment of hypertension. Nature reviews. Cardiology. 2020 doi: 10.1038/s41569-020-00437-9. [DOI] [PubMed] [Google Scholar]
- 73.Schneider RH, Egan B, Johnson E, Drobny H, Julius S. Anger and anxiety in borderline hypertension. Psychosomatic Medicine. 1986;48:242–248. doi: 10.1097/00006842-198603000-00009. [DOI] [PubMed] [Google Scholar]
- 74.Orme-Johnson D, stability Autonomic, Meditation Transcendental. Autonomic stability and Transcendental Meditation. Psychosomatic Medicine. 1973;35:341–349. doi: 10.1097/00006842-197307000-00008. [DOI] [PubMed] [Google Scholar]
- 75.Dillbeck MC, Orme-Johnson DW. Physiological differences between Transcendental Meditation and rest. American Psychologist. 1987;42:879–881. [Google Scholar]
- 76.Barnes VA, Treiber FA, Davis H. Impact of Transcendental Meditation on cardiovascular function at rest and during acute stress in adolescents with high normal blood pressure. Journal of Psychosomatic Research. 2001;51(4):597–605. doi: 10.1016/s0022-3999(01)00261-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Paul-Labrador M, Polk D, Dwyer J, Velasquez I, Nidich S, Rainforth M. Effects of a randomized controlled trial of Transcendental Meditation on components of the metabolic syndrome in subjects with coronary heart disease. Archives in Internal Medicine. 2006;166:1218–1224. doi: 10.1001/archinte.166.11.1218. [DOI] [PubMed] [Google Scholar]
- 78.Wallace RK, Silver J, Mills PJ, Dillbeck MC, Wagoner DE. Systolic blood pressure and long-term practice of the Transcendental Meditation and TM-Sidhi programs: Effects of TM on systolic blood pressure. Psychosomatic Medicine. 1983;45(1):41–46. doi: 10.1097/00006842-198303000-00006. [DOI] [PubMed] [Google Scholar]
- 79.Mansournia MA, Higgins JP, Sterne JA, Hernan MA. Biases in Randomized Trials: A Conversation Between Trialists and Epidemiologists. Epidemiology. 2017;28(1):54–59. doi: 10.1097/EDE.0000000000000564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Alexander CN, Swanson GC, Rainforth MV, Carlisle TW, Todd CC, Oates RM. Effects of the Transcendental Meditation program on stress reduction, health, and employee development: A prospective study in two occupational settings. Anxiety, Stress and Coping: An International Journal. 1993;6:245–262. [Google Scholar]
- 81.Gaylord-King C, Orme-Johnson D, Travis F. The effects of the Transcendental Meditation technique and progressive muscle relaxation on EEG coherence, stress reactivity, and mental health in black adults. International Journal of Neuroscience. 1989;46(1-2):77–86. doi: 10.3109/00207458908991618. [DOI] [PubMed] [Google Scholar]
- 82.Infante JR, Torres-Avisbal M, Pinel P, Vallejo JA, Peran F, Gonzalez F. Catecholamine levels in practitioners of the transcendental meditation technique. Physiology and Behavior. 2001;72(1–2):141–146. doi: 10.1016/s0031-9384(00)00386-3. [DOI] [PubMed] [Google Scholar]
- 83.Jevning R, Wilson AF, Smith WR. Adrenocortical activity during meditation. Hormones and Behavior. 1978;10(1):54–60. doi: 10.1016/0018-506x(78)90024-7. [DOI] [PubMed] [Google Scholar]