Abstract
Introduction and importance
A multi-level non-contiguous spinal fracture (MNSF) caused by a high-energy impact is a type of complex traumatic injury that is been frequently initially missed, and resulting in delayed diagnosis which adversely affects can result in spinal deformity and neurological deficit. This report describes the operative management of a patient with MNSF with spinal cord injury involving the cervical and thoracic vertebrae by cervical orthosis and posterior thoracic decompression and fusion.
Case presentation
An 18-year-old male presented with extensive neck pain and paraplegia (ASIA A), following a motor vehicle accident. Radiographic imaging revealed MNSF: a non-displaced spinous process fracture of C5 (AO Spine subaxial cervical injury classification A0) with spinal cord injury combined with fracture-dislocation of T5 to T9 (AO Spine thoracolumbar injury classification C3). Posterior thoracic decompression and fusion was performed at T3 to T8. After the patient underwent the thoracic spine and cervical orthosis treatment, He received rehabilitation program and training transfer with wheelchair without caregiver. His sitting and balance were significantly improved at the 6 months follow-up. Although the lower extremity functions (ASIA A) may not improve due to the severe spinal cord injury.
Clinical discussion
MNSF with spinal cord injury following a high-velocity accident is an unstable and complex injury. Important of the clinical assessment and according to the injuries the treatment may vary.
Conclusions
Cervical orthosis was alternative treatment to preserve cervical motion treatment and posterior thoracic decompression with fixation is an effective option for patients in this MNSF with spinal cord injury.
Keywords: Multilevel noncontiguous spinal fractures, MNSI, Spinal cord injury
Highlights
-
•
Multilevel noncontiguous spinal fractures (MNSF) with multiple spinal cord injury are serious injuries and complex of spinal injuries at more than one level.
-
•
MNSF of the clinical assessment and according to the injuries the treatment may vary.
-
•
MNSF involving multilevel spinal cord injury following a motor vehicle accident and treated by posterior thoracic decompression and fusion combine with cervical orthosis might be an option in this condition.
1. Introduction and importance
Multilevel noncontiguous spinal fractures (MNSF) are a serious type of injury and may involve special types of spinal injuries at more than one level. MNSF associated with high-velocity trauma may include multilevel spinal cord injuries. Incidence rates of MNSF have been reported, varying from 1.6% to 23.8% and increasing to 23.1% to 83.3% in cases of delayed diagnosis of the second lesion [1], [2]. Surgical decisions regarding early total management are challenging for spine surgeons, e.g., spinal stabilization, spinal protection, urgent adequate decompression and spinal fixation in cases of instability. This report presents a case of MNSF involving a multilevel spinal cord injury following a motor vehicle accident which was treated by posterior thoracic decompression and fusion combined with cervical orthosis. This case has been reported in accordance with SCARE criteria [3].
2. Case presentation
An 18-year-old male presented with extensive neck pain and lower extremity weakness 3 h following a motor vehicle accident. He had undergone the advanced trauma life support (ATLS) protocol. He had right pneumothorax and his hemodynamic status was unstable. At the intensive care unit (ICU), an intercostal drain (ICD) was inserted and he was given resuscitation until his condition stabilized. A secondary survey found he had no history of smoking, drinking alcohol or using recreational drugs. Physical examination after the spinal shock showed initial vital signs and mental status were normal. He had bilateral upper extremity weakness below the triceps level (C7) (motor power gr. III) and lower extremity weakness (gr. 0). Sensation decreased below C6 and was absent below the T4 level. His biceps and triceps reflex were 2+ but lower extremity deep tendon reflexes were absent. Rectal examination found a loss of sphincter tone. The bulbocarvernosus reflex was present, but sacral sparing was absent. Radiographic imaging (CT-scans) showed moderate cervical canal stenosis (Pavlov ratio 0.72 at C5 and 0.69 at C6), a non-displaced fracture of the spinous process of the C5 vertebra (Fig. 1A) and multiple thoracic spine fractures from T3 to T9 with multiple bony fragments in the spinal canal at the T5–T6 level (Fig. 1B–G).
Fig. 1.
Radiographic (CT-scan) in axial and mid-sagittal views of the cervicothoracic spine show a non-displaced fracture of the spinous process of the C5 vertebra (A) and multiple thoracic spine fractures from T4 to T9 (B–G).
Magnetic resonance imaging (MRI) revealed spinal stenosis. The cervical spinal cord at C5/C6 had an increased signal intensity in the T2 weighted image (T2WI) and there was a complex fracture dislocation at T5 to T7 (a posterior element injury including bilateral facet dislocation and disruption of the posterior ligamentous complex) with increased T2 signal intensity of the spinal cord at the T6 level in T2WI (Fig. 2). MRI results suggested a multilevel noncontiguous injury of the spine and a spinal cord injury as well as a diagnosis of MNSF in cervical levels (AO Spine subaxial cervical injury classification A0) and thoracic levels (AO Spine thoracolumbar (TL)) injury classification C3. Based on the examination results, posterior thoracic decompression and fusion was performed at T3 to T8 under general anesthesia and a cervical orthosis was selected. The patient was placed in the prone position for a posterior surgical approach. The patient underwent surgery the thoracic spine by an experienced spine surgeon (SP). Intra-operative findings included severe multiple posterior ligaments complex injury (Fig. 3A), multiple bony fragments (Fig. 3B) and large dural tears (Fig. 3D) at the T5/T6 the level. Pedicle screws were inserted followed by posterior thoracic decompression with direct dural repair. A crosslinking device was attached and then posterolateral fusion with local bone graft was carried out at T3 to T8. (Fig. 3D, E). Postoperative radiographic films showed good alignment compared to the pre-operative radiographic films (Fig. 4).
Fig. 2.
MRI in axial and mid sagittal view of the cervicothoracic spine showed MNSF at the cervical (A–D) and thoracic levels (E–H).
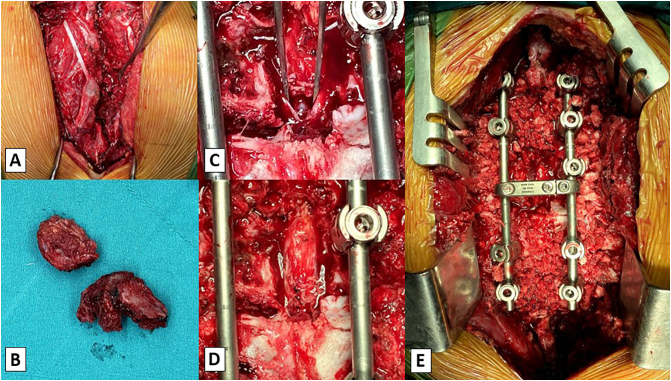
Fig. 3.
Intra-operative findings included severe multiple posterior ligament complex injury (A), multiple bony fragments (B) and large dural tears at the T5/T6 level (C), direct dural repairing (D), posterior inseminations and posterolateral fusion (E).
Fig. 4.
Preoperative radiographic films (A) and post-operative radiographic films (B).
After the operation, a cervical orthosis was applied to treat the non-displaced fracture at C5 and the patient was entered into a rehabilitation program. At the 6 months follow-up visit after the operation, he was able to transfer himself to and from a wheelchair without caregiver assistance and his upper extremity function was significant improved. The patient was highly satisfied, although the lower extremity functions (ASIA A) may not improve due to the severe spinal cord injury from the high-velocity traumatic MNSF at the thoracic level.
3. Clinical discussion
MNSF with multilevel spinal cord injury, a special type of multilevel spinal injury, most frequently occurs in high-velocity traffic accidents or falls from height [1], [2]. Delayed diagnosis of a second fracture has been reported in between 23.1% to 83.3% of cases, with delays ranging from 2.8 to 52.6 days [2], [4]. In traumatic lacerations of the dura or of dura tears, 18–36% were associated with spine injuries. The most common fracture pattern related to dura tears is fracture-dislocation associated with complete spinal cord injuries [5]. The current standard treatment of MNSF with traumatic dura tears includes early detection, ridged internal fixation plus decompression and dura repair, with results showing improvements in outcomes and reduction of deformity [4], [5].
In a recent study investigating MNSF patterns based on whole spine MRI, Kanna RM et al. described five patterns of non-contiguous spinal injuries: Pattern 1: cervical and thoracic fracture, Pattern 2: thoracolumbar and lumbosacral fracture, Pattern 3: thoracic and thoracolumbar fracture, Pattern 4: cervical and thoracolumbar fracture and Pattern 5: lumbosacral facture and associated injuries [6]. The principle of spinal stability includes both mechanical stability and spinal neurologic stability, factors which need to be considered when making decisions regarding total management. Spinal neurologic stability is graded using the American Spinal Injury Association (ASIA) score system. The AO Spine Thoracolumbar (TL) and Subaxial Injury Classification systems are a revision of the Magerl classification which were developed based on morphology and clinical factors relevant to clinical decision making [7]. The MRI classification for this patient was pattern 2 using the Kanna RM et al. system: a spine subaxial cervical injury classification type A0 combined with an AO Spine TL injury classification type C3, i.e., this was the most severe injury. A complete examination and full investigation is important for reducing the risk of a missed diagnosis as well as prevention of secondary damage to neurological structures related to clinical outcomes [4]. In this patient choose conservative treatment on cervical problem despite some neurological deficit because after we classified by AO Spine subaxial cervical injury, it was type A0 (included only lamina or spinous process fracture in cervical spine) and MRI scan showed no spinal cord compression, minimal displaced of C5 spinous process without rupture of posterior ligamentous complex (stable stability). AO Spine type A0 suggested to conservative treatment [7]. Cervical orthosis was alternative treatment to preserve cervical motion when compare with posterior spinal fusion. At the 6 months follow-up visit, this patient was improved cervical motion and bony union. However, thoracic level was AO Spine TL injury classification type C3 that its severe unstable injury. AO Spine TL recommends and requests surgery of adequate reduction, decompression and rigid fixation for due with severe injury [6], [7].
Our hypothesis is that the mechanism of severe injury of the thoracic spine is flexion and rotation of the spine combined with cervical spine failure under extension. The combination of these different mechanisms of spinal injury and different neurological stations in MNSF is uncommon. For that reason, we choose conservative treatment with cervical orthosis at the cervical level and operative management at the thoracic level.
4. Conclusions
For MNSF cases involving a multilevel spinal cord injury following a high-velocity motor vehicle accident, treatment with posterior thoracic decompression and fusion combined with cervical orthosis might be an option. The early detection of MNFS (secondary lesion), surgical treatment and suitable rehabilitation training including wheelchair transfer and sitting balance are important for the prevention of complications and the achievement of the best possible clinical outcomes.
Ethical approval
This case report was approved by the Institutional Review Board, Faculty of Medicine, Chiang Mai University.
Source of funding
Funding for this research was provided by the Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand. The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
CRediT authorship contribution statement
Nantawit Sugandhavesa (NS): resources, data curation, review & editing, supervision.
Wongthawat Liawrungrueang (WL): conceptualization, methodology, visualization, writing -original draft, editing and revision the final version for publication.
Komchat Kaewbuadee (KK): resources, data curation.
Suthipas Pongmanee (SP): resources, data curation, review & editing, supervision.
Guarantor
Nantawit Sugandhavesa (NS) and Suthipas Pongmanee (SP).
Registration of research studies
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and the accompanying images. A copy of the written consent is available for review upon request to the Editor-in Chief of this journal on request.
Declaration of competing interest
None.
Acknowledgments
Acknowledgments
The authors would like to express their sincere thanks to Dr. G. Lamar Robert, Ph.D., and Assoc. Prof. Dr. Chongchit Sripun Robert, Ph.D., for editing the English manuscript. We would also like to express our thanks to the Research Unit, Department of Orthopaedics, Faculty of Medicine, Chiang Mai University for their support.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Gupta A., el Masri W.S. Multilevel spinal injuries. Incidence, distribution and neurological patterns. J. Bone Joint. Surg. Br. 1989;71:692–695. doi: 10.1302/0301-620X.71B4.2768324. [DOI] [PubMed] [Google Scholar]
- 2.Lian X.F., Zhao J., Hou T.S., Yuan J.D., Jin G.Y., Li Z.H. The treatment for multilevel noncontiguous spinal fractures. Int. Orthop. 2007;31:647–652. doi: 10.1007/s00264-006-0241-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 Guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 4.Seçer M., Alagöz F., Uçkun O., Karakoyun O.D., Ulutaş M.Ö., Polat Ö. Multilevel noncontiguous spinal fractures: surgical approach towards clinical characteristics. Asian Spine J. 2015;9:889–894. doi: 10.4184/asj.2015.9.6.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luszczyk M.J., Blaisdell G.Y., Wiater B.P., Bellabarba C., Chapman J.R., Agel J.A. Traumatic dural tears: what do we know and are they a problem? Spine J. 2014;14:49–56. doi: 10.1016/j.spinee.2013.03.049. [DOI] [PubMed] [Google Scholar]
- 6.Kanna R.M., Gaike C.V., Mahesh A., Shetty A.P., Rajasekaran S. Multilevel non-contiguous spinal injuries: incidence and patterns based on whole spine MRI. Eur. Spine J. 2016;25:1163–1169. doi: 10.1007/s00586-015-4209-2. [DOI] [PubMed] [Google Scholar]
- 7.Schnake K.J., Schroeder G.D., Vaccaro A.R., Oner C. AOSpine classification systems (Subaxial, Thoracolumbar) J. Orthop. Trauma. 2017;31(Suppl 4):S14–S23. doi: 10.1097/BOT.0000000000000947. [DOI] [PubMed] [Google Scholar]