Abstract
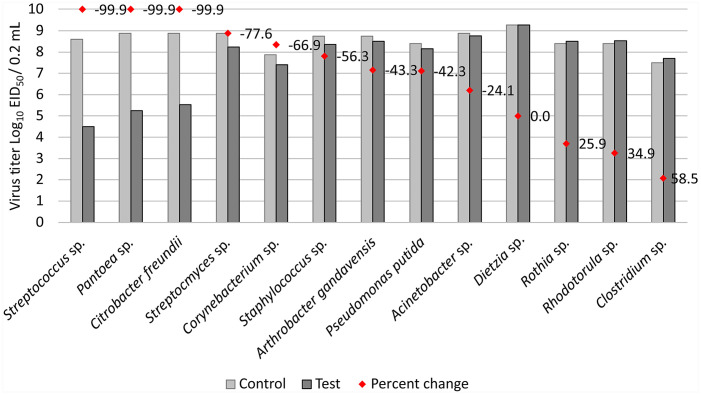
Avian influenza surveillance is a requirement for commercial trade in ostrich products, but influenza A viruses (IAVs) have proven difficult to isolate from ostrich tracheal swabs that test positive using molecular methods. We hypothesized that microbes unique to the ostrich trachea propagate in the transport medium after sampling and affect viral viability. We cultured tracheal swabs from 50 ostriches on 4 farms in South Africa, and recovered and identified 13 bacterial, 1 yeast, and 2 fungal species. Dietzia sp. had not been identified previously in the oropharyngeal tract of a bird, to our knowledge. The bacteria were tested for antimicrobial susceptibility, and most aerobic species, except for Streptococcus sp. and Pseudomonas sp., were sensitive to enrofloxacin; all were susceptible to sulfonamide. Virus inhibition experiments determined that ostrich-source Streptococcus sp., Pantoea sp., and Citrobacter freundii produced extracellular metabolites that caused a substantial reduction in the IAV titers of 99.9%. Streptomyces, Corynebacterium, Staphylococcus, Arthrobacter gandavensis, Pseudomonas putida, and Acinetobacter spp. similarly reduced the viability of IAV from 77.6% to 24.1%. Dietzia appeared to have no effect, but Rothia dentocariosa, Rhodotorula spp., and Clostridium spp. slightly increased the viability of IAV by 25.9, 34.9, and 58.5%, respectively.
Keywords: antimicrobial resistance, antiviral, influenza A virus, ostrich, tracheal swabs
Commercially farmed ostriches (Struthio camelus) are highly versatile production animals valued for their fine leather, feathers, and low-cholesterol lean red meat. Ostriches are native to South Africa and thrive in the semi-desert climate of the areas of the southern Cape Provinces where the farms are concentrated, but the extensive nature of ostrich farming results in the transmission of influenza A viruses (IAVs) from the excretions of wild birds in the environment on a regular basis.1,2 South Africa is the leading exporter of ostrich products globally, with 75% of the market share; the European Union is the main market. 5 To comply with the strict international trade requirement to ensure freedom from avian influenza, all registered export farms are tested monthly, pre-movement, and pre-slaughter. Birds in epidemiologic units that test seropositive are re-sampled within 7 d, and tracheal swabs are collected for virus detection. An epidemiologic unit is defined as any group of ostriches of similar age and/or weight, with a defined epidemiologic relationship that share approximately the same likelihood of exposure to a pathogen, either because of sharing a common environment or because of common management practices. Tracheal swabs are also collected from each epidemiologic unit of all ostrich farms in the country twice a year for compulsory IAV surveillance.
Ostrich tracheal swab fluids are tested for the presence of IAV-specific RNA with reverse-transcription real-time PCR (RT-rtPCR) assays. The swab fluids of positive pools are then treated with antimicrobials and inoculated into embryonated chicken eggs (ECEs) for virus isolation, the international gold standard for virus identification. 19 There is a statistical correlation between the cycle threshold (Ct) value of an RT-rtPCR–positive sample and the ability to isolate the virus in ECEs,5,12 but even with Cts <30, the success rate for isolation of IAVs from ostriches has been consistently low.1-3 For example, in 977 ostrich tracheal swab pools tested by a national veterinary laboratory in 2019 using RT-rtPCR, 109 (11.2%) were IAV positive, but only one virus, an H11N1 strain, was isolated (Olivier A, pers. comm., unpublished diagnostic test reports, 2019). During the 2011 highly pathogenic avian influenza (HPAI) H5N2 subtype outbreaks in ostriches, only 3 viruses were isolated from >1,000 swab pools of 20 commercial ostrich farms. In the 2017 HPAI H5N8 subtype outbreaks, 38 ostrich tracheal swab pools were H5N8 positive on RT-rtPCR, but only 2 viruses were isolated compared with 39 viruses isolated from the oropharyngeal and cloacal swabs or tissue samples of other avian species. 3
The consistently low rate of IAV isolation from ostriches is of concern to national and international regulators, and it is notable that the standard PBS–glycerol transport medium used routinely for ostrich tracheal swabs does not contain any antimicrobials. To investigate why IAVs in ostrich tracheal swab fluids are difficult to isolate in ECEs, we cultured and identified the bacteria present, tested their susceptibility to commonly used antimicrobials, and evaluated their effects on the viability of IAV.
Materials and methods
Sample collection
Ten randomly selected swab pools (n = 50 ostriches; 5 per pool) collected in April 2018 from 4 geographically separated ostrich farms in the Western Cape Province that tested IAV-negative during routine surveillance at the Western Cape Provincial Veterinary Laboratory (WCPVL; Stellenbosch, Western Cape Province, South Africa), and had been stored at 4°C since receipt 48 h after collection, were shipped on ice packs to the University of Pretoria (UP; Onderstepoort, South Africa). Pools consisted of 5 rayon-tipped swabs each in 50% v/v glycerol PBS, pH 7.0–7.4, without antimicrobials.
Microbial culture and identification
Ostrich tracheal swabs were removed aseptically from the transport medium and streaked onto various agar plates for bacterial isolation. For aerobic bacteria, Columbia blood agar with 5% horse blood (Thermo Fisher) and MacConkey agar without crystal violet (Thermo Fisher) were incubated at 37 ± 1°C with or without 5% CO2, respectively, for 24 h. For anaerobic bacteria, Columbia blood agar plates with 5% horse blood were incubated at 37 ± 1°C for 24 h in an anaerobic incubator. Plates were examined every 24 h, for up to 72 h. Where necessary, bacterial colonies were subcultured using a quadrant streaking method to obtain axenic cultures. 7 Potato dextrose agar (Oxoid) and Dermasel agar plates (Oxoid) were used to isolate fungal species, with incubation at 25 ± 1°C for up to 1 mo. Subculturing to obtain axenic fungal cultures was performed where required. Gram staining was applied for the preliminary identification of axenic bacterial cultures, and lactophenol cotton blue stain was used for fungal species identification, using standard procedures for both. 10 Catalase and oxidase tests were performed according to standard methods in the preliminary identification of bacteria, 10 and were supplemented with API 10 S strips (bioMérieux) for the identification of the Enterobacteriaceae and other non-fastidious gram-negative bacteria that were oxidase negative. API 20 NE strips (bioMérieux) were used for the identification of non-fastidious, non-enteric gram-negative rods and gram-negative bacteria that were oxidase positive and grew poorly on the MacConkey agar. Rapid ID 32 A strips (bioMérieux) were used for the identification of anaerobes. Streptococcal species were tested using the Lancefield streptococcal grouping kit (Oxoid). API 20 C Aux (bioMérieux) was used in the identification of isolated yeasts. All tests were performed according to the kit-recommended procedures. Carbohydrate fermentation tests were used to identify Streptococcus spp., Staphylococcus spp., Corynebacterium spp., and Micrococcus spp., as prescribed. 10 Furthermore, suspected Staphylococcus spp. that were gram-positive cocci, oxidase negative, and catalase positive were tested with the DNase + mannitol test and the purple agar with maltose test. An antimicrobial susceptibility test was performed with the novobiocin disk (Oxoid) and the polymyxin B disk (Oxoid) on a Mueller–Hinton agar plate (Thermo Fisher) to confirm Staphylococcus spp. The plates were incubated for 24 h at 37 ± 1°C, after which all reactions were recorded. Differentiation between Staphylococcus and Micrococcus species was also possible by measuring the zone of a bacitracin disk (Oxoid). Samples were not cultured for mycoplasma. Bacterial isolates were inoculated aseptically into cryovials containing 1.5 mL of BHI broth (Oxoid), mixed by vortexing, and frozen; isolates were then stored at −80°C until further tested.
Axenic aerobic cultures streaked onto agar plates were submitted to NOSA Testing (Pretoria, South Africa) for bacterial identification by MALDI-TOF mass spectrometry (Microflex; Bruker). Scores of 2.00–3.00 represented high confidence identification, scores of 1.70–1.99 represented low confidence identification, and no identification was possible when scores were 0.00–1.69.
Antimicrobial susceptibility tests
The standardized Kirby–Bauer disk diffusion method was used to determine the antimicrobial susceptibility of the axenic bacterial isolates. Cultures stored at −80°C were reinoculated into microbiologic media. For the aerobic isolates, antibiograms were conducted against the standard antimicrobials used in the poultry industry, namely ampicillin, colistin sulfate, doxycycline, enrofloxacin, erythromycin, gentamicin–neomycin, sulfonamide–trimethoprim, tetracycline, ceftiofur (all sourced from Oxoid) and fosfomycin (Fosbac). Clinical resistance breakpoints in Suppl. Table 1 were as per Clinical Laboratory Standards Institute guidelines. 4
16S rRNA sequencing
Bacterial cells were pelleted from 5 mL of culture medium by centrifugation at 10,000 × g for 10 min (5804R; Eppendorf). Genomic DNA was extracted from the pellets (Invitrogen PureLink genomic DNA mini kit; Life Technologies, Thermo Fisher) using the protocols for gram-positive or gram-negative bacteria. DNA was eluted in 50 µL of ultrapure water and quantified (NanoDrop spectrophotometer; Inqaba Biotech). DNA samples were supplied to the Ion Torrent PGM sequencing service facility at the University of Pretoria, where 100 ng of each sample was used to build 400-bp barcoded libraries (Ion 16S metagenomics kit; Thermo Fisher), according to the recommended procedure. 16S barcoded libraries were shipped to Stellenbosch University’s Central Analytical Facility (Stellenbosch, South Africa), where massively parallel sequencing was performed (S5-530 chip, Ion Proton system; Thermo Fisher) according to the recommended procedures. Ion Torrent sequencing results were analyzed (CLC Genomics Workbench v.5.1.2; Qiagen). Contigs assembled de novo were identified by BLAST sequence homology (https://blast.ncbi.nlm.nih.gov/Blast.cgi). Sequences generated were deposited in GenBank as MN814254–MN814263.
Virus inhibition
Low pathogenic influenza virus A/ostrich/South Africa/OUD/2012 (H7N1) was propagated in 9- to 11-d-old specific pathogen–free ECEs and titrated using the method of Reed and Muench. 14
A single colony of each bacterium was inoculated into 10 mL of sterile BHI broth and grown overnight with shaking in a 37°C incubator. Cultures were centrifuged at 5,000 × g for 10 min to pellet the cells, and the medium was aspirated and passed through 0.45-µm syringe filters (GVS Life Sciences) into sterile containers. To test whether the filtered overnight cultures were toxic to the chicken embryos, 0.2-mL volumes of each sample were inoculated into 6 ECEs each and incubated at 37°C for 7 d. No embryo deaths were recorded.
Filtered BHI broth (2.25 mL) containing the bacterial metabolites plus a control of sterile BHI broth were incubated with 0.25 mL of egg allantoic fluid containing 109.09 EID50 live A(H7N1) virus for 1 h at 37°C. Each sample was titrated from 10−1 to 10−10 in PBS, and at least 4 titrations of each sample was inoculated into 6 ECEs (Suppl. Table 2). Eggs were incubated for 6 d and inspected daily for deaths. Any deaths occurring prior to day 3 were considered nonspecific. The final virus titer in any eggs that died from day 3 onwards was calculated according to Reed and Muench. 14
Results
Identification of bacteria isolated from ostrich tracheal swabs
Thirteen different bacteria, 1 yeast, and 2 fungal species were isolated and identified by classical techniques from tracheal swabs (Table 1). MALDI-TOF MS confirmed the identification of most bacteria, but there were some discrepancies between the results, for example, B700/18-3 Brevibacterium sp. was identified by MALDI-TOF MS as Arthrobacter gandavensis, therefore 16S rRNA sequencing was used for definitive identification. Two samples, B700/18-10 and B700/18-15, were below the DNA quality cutoff for barcoded DNA library construction and were therefore not sequenced. The species identification was determined by a consensus of at least 2 methods and/or sequence homology >99% on 16S rRNA. Thus, the following microbes were identified—gram-positive bacteria: Clostridium sp., Dietzia sp. (although D. maris was identified by 2 methods; the MALDI-TOF score was only 1.90, and the 16S rRNA sequence homology was 98.6%), A. gandavensis, 2 Streptococcus spp., Pantoea sp., Rothia dentocariosa, 2 Streptomyces spp., and Staphylococcus haemolyticus; gram-negative bacteria: Acinetobacter sp., Pseudomonas putida, and Citrobacter sp.; yeast: Rhodotorula mucilaginosa; fungi: Purpureocillium lilacinum and Alternaria sp. (Table 1).
Table 1.
Identification of microbial species cultured from ostrich tracheal swab pools.
| Isolate | Classical phenotypic methods | MALDI-TOF mass spectrometry | 16S rRNA sequence | |||
|---|---|---|---|---|---|---|
| Identity | Score | Closest match in GenBank | Accession | % identity | ||
| B700/18-0 | Clostridium sp.* | Not tested | Clostridium sp. | KT592379 | 100 | |
| B700/18-1 | Micrococcus sp.* | Dietzia maris | 1.90 | Dietzia maris | MG547917 | 98.6 |
| B700/18-2 | Acinetobacter sp.† | Acinetobacter lwoffii | 2.08 | Acinetobacter sp. | MK548512 | 99.9 |
| B700/18-3 | Brevibacterium sp.* | Arthrobacter gandavensis | 2.43 | Arthrobacter gandavensis | MK646035 | 99.7 |
| B700/18-5 | Streptococcus equinus * | Unidentified | 1.55 | Streptococcus pluranimalium | CP025536 | 98.1 |
| B700/18-8 | Pantoea sp.* | Not tested | Pantoea septica | HM854257 | 98.6 | |
| B700/18-9 | Vibrio parahaemolyticus † | Pseudomonas putida | 1.86 | Pseudomonas putida | CP024086 | 99.8 |
| B700/18-10 | Citrobacter freundii † | Unidentified | 1.91 | Not sequenced¦ | ||
| B700/18-15 | Rothia dentocariosa * | Rothia dentocariosa | 2.30 | Not sequenced¦ | ||
| B700/18-16 | Corynebacterium bovis * | Unidentified | 1.60 | Corynebacterium falsenii | KT824798 | 98.3 |
| B700/18-17 | Streptococcus sp.* | Unidentified | 1.40 | Uncultured bacterium | AB989765 | 99.3 |
| B700/18-18 | Streptomyces sp.* | Streptomyces badius | 1.74 | Curtobacterium sp. | HF566227 | 96.7 |
| B700/18-19 | Staphylococcus sp.* | Staphylococcus haemolyticus | 2.08 | Staphylococcus haemolyticus | CP033814 | 99.8 |
| B700/18-21 | Rhodotorula mucilaginosa ‡ | Not tested | Not sequenced | |||
| B700/18-22 | Purpureocillium lilacinum § | Not tested | Not sequenced | |||
| B700/18-23 | Alternaria spp.§ | Not tested | Not sequenced | |||
Gram-positive bacterium.
Gram-negative bacterium.
Yeast.
Fungi.
DNA was below the quality cutoff for barcoded library preparation.
The aerobic bacteria were tested for susceptibility against different antimicrobial classes commonly used in poultry, namely doxycycline (100 mg/L; class tetracycline), enrofloxacin (100 mg/L; class quinolones), and penicillin–streptomycin (100 mg/L; class penicillin). B700/18-17 (Streptococcus sp.) could not be revived after storage at −80°C and was thus not tested. Of the 3 bacteria for which doxycycline breakpoints are available (Acinetobacter sp., Pantoea sp., Citrobacter sp.), all were susceptible to 30 µg (Table 2). Most aerobic bacterial species were sensitive to 15 µg of enrofloxacin, except for Streptococcus sp. and Pseudomonas sp., which were of intermediate susceptibility. Penicillin–streptomycin was not in the antibiogram panel; however, Dietzia, Acinetobacter, and Streptococcus spp. were susceptible to ampicillin. All aerobic species were susceptible to 300 µg of sulfonamide.
Table 2.
Antimicrobial susceptibility of aerobic bacteria cultured from ostrich tracheal swabs.
| Isolate | Species | Ampicillin (10 µg) | Colistin sulfate (10 µg g) | Doxycycline (30 µg) | Enrofloxacin (15 µg) | Erythromycin (15 µg) | Fosfomycin (200 µg) | Ceftiofur (30 µg) | Neomycin (10 µg) | Kanamycin (30 µg) | Sulfonamides (300 µg) | Trimethoprim (25 µg) | Tetracycline (30 µg) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B700/18-1 | Dietzia sp. | S | R | — | S | S | R | S | — | I | S | R | S |
| B700/18-2 | Acinetobacter sp. | S | S | S | S | — | — | I | S | S | S | S | S |
| B700/18-3 | Arthrobacter gandavensis | — | R | — | S | — | — | S | S | S | S | S | S |
| B700/18-5 | Streptococcus sp. | S | R | — | I | S | — | S | — | R | S | S | I |
| B700/18-8 | Pantoea sp. | R | S | S | S | — | — | S | S | S | S | S | S |
| B700/18-9 | Pseudomonas putida | — | S | — | I | — | — | R | S | S | S | I | S |
| B700/18-10 | Citrobacter sp. | R | S | S | S | — | — | S | S | S | S | S | S |
| B700/18-15 | Rothia dentocariosa | — | R | — | S | S | — | S | — | I | S | S | S |
| B700/18-16 | Corynebacterium sp. | — | R | — | S | S | — | S | — | S | S | S | S |
| B700/18-18 | Streptomyces sp. | — | S | — | S | — | — | R | — | R | S | S | I |
| B700/18-19 | Staphylococcus haemolyticus | S | R | — | S | S | — | S | — | S | S | S | S |
I = intermediate; R = resistant (in bold); S = sensitive; — = susceptibility testing is not recommended; the species is a poor target for therapy with the agent.
Colistin is effective against most gram-negative bacilli, but most gram-positive bacilli are resistant, as are gram-positive aerobic cocci, gram-positive aerobic bacilli, and all anerobes. 7 All 4 gram-negative aerobic bacteria (Acinetobacter sp., Pantoea sp., P. putida, Citrobacter sp.) isolated from ostriches were susceptible to 10 µg of colistin sulfate, as expected. Most of the gram-positive aerobic bacteria identified (Dietzia sp., Arthrobacter sp., Streptococcus sp., R. dentocariosa, Corynebacterium sp., S. haemolyticus) were indeed resistant to colistin, but the gram-positive Streptomyces sp. isolated from ostriches was susceptible.
The single anaerobic isolate (B700/18-0), a Clostridium sp., was tested with a MASTRING-S test (Mast Group). The isolate was sensitive to erythromycin (60 µg), rifampicin (15 µg), penicillin G (2 units), kanamycin (100 µg), and vancomycin (5 µg), but was resistant to colistin sulfate (10 µg).
Effect of bacteria-free growth media on the viability of influenza A virus
Titrations of A(H7N1) virus were incubated with the filtered overnight bacterial cultures, and the treated virus was inoculated into eggs for virus isolation alongside controls incubated in sterile BHI medium (Suppl. Table 2). Three of the bacterial species, namely Streptococcus, Pantoea, and C. freundii, caused a substantial reduction in the viability of the A(H7N1) virus, with 99.9% reductions in the viral titers compared to the controls (Fig. 1). Streptomyces, Corynebacterium, Staphylococcus, A. gandavensis, P. putida, and Acinetobacter spp. similarly reduced the viability of IAV by 77.6% to 24.1% compared to the controls. Dietzia appeared to have no effect, but Rothia, Rhodotorula, and Clostridium spp. slightly increased the viability of the virus by 25.9, 34.9, and 58.5%, respectively.
Figure 1.
Effect of bacteria isolated from ostrich tracheal swabs on the viability of influenza A virus.
Discussion
Five of the 16 microbes cultured from ostrich tracheal swabs were described as colonizing agents of the ostrich oropharynx in a study conducted on 50 healthy breeder ostriches in Brazil. 11 That study identified only 2 gram-positive species, namely Staphylococcus sp. and Streptococcus sp., whereas 12 gram-negative strains were identified. 11 Of the latter, only Citrobacter sp. and Pseudomonas sp. were identified in our study. Rhodotorula was also identified previously, but we isolated neither Candida albicans nor Cryptococcus spp.
Interestingly, we identified a Dietzia sp. by MALDI-TOF MS and confirmed its identity by 16S rRNA sequencing. Dietzia are gram-positive, aerobic, non–spore-forming bacteria taxonomically closely related to actinomycetes, with D. maris originally described as Rhodococcus maris. 13 Dietzia strains inhabit diverse environments, including the oropharyngeal tracts of dogs, 6 but Dietzia has not been cultured from or identified in the oropharyngeal tract of a bird previously, to our knowledge.
Microbes produce and secrete extracellular metabolites into their environment during their growth. These may include primary metabolites such as hydrophilic carbohydrates, volatile alcohols, ketones, amino and non-amino organic acids, hydrophobic lipids, and complex secondary metabolites such as antibiotics, pigments, non-ribosomal peptides, and cofactors. The production and secretion of these primary and secondary metabolites is complex and variable, dependent on factors such as temperature, pH, and the availability and concentration of nutrients. 17 Rhamnolipids, for example, are secondary metabolites produced by Pseudomonas spp. as well as by D. maris. Rhamnolipids are very efficient biosurfactant molecules that are harnessed for industrial applications, for example in the bioremediation of oil spills,9,18 but rhamnolipids have also been demonstrated to have antiviral activity against enveloped viruses. 8 In another example, an 11-kDa protein isolated from the cyanobacterium Nostoc ellipsosporum was demonstrated to have antiviral activity against human immunodeficiency virus and IAV, through binding to viral surface glycoproteins. 15
Ostrich tracheal mucus and saliva on swabs are rich sources of proteins, enzymes, carbohydrates, and electrolytes in the PBS–glycerol transport medium. We found that ostrich tracheal swab fluid supports the growth of at least 16 different microbes, and that most of the bacteria present produce extracellular metabolites that have substantive antiviral effects against IAV. The disruption of the IAV envelope by bacterial proteins would render the virus nonviable, although the viral RNA might still be intact. This could explain why ostrich IAVs are easily detectable by RT-rtPCR but are not isolatable in chicken eggs. A limitation of our study is that we did not determine the prevalence of each of the microbes in the ostrich tracheal swab samples, and the identification of the antiviral compounds was beyond the scope of our investigation.
Some of the bacteria we isolated and identified were resistant to some of the antimicrobial compounds tested, but sulfonamide used at 300 µg appeared to be a suitable broad-spectrum antimicrobial to include in a viral transport medium. Colistin resistance is a worldwide medical concern given that it is a last-line treatment for carbapenemase-producing bacteria. Six of the 7 gram-positive aerobic bacteria that we identified in ostriches, namely Dietzia sp., Arthrobacter sp., Streptococcus sp., R. dentocariosa, Corynebacterium sp., and S. haemolyticus, were resistant to colistin sulfate.
Antimicrobials are not used as growth promotors in ostriches, as is common in traditional poultry production, but are administered to treat specific infections, for example quinolones in chicks for yolk sac infections, and sulfonamide, oxytetracycline, tylosin, and fosfomycin for intestinal infections. Lincomycin–spectinomycin is used for intestinal and respiratory infections, and penicillins are used for intestinal infections. In grower birds (4–12 mo old), oxytetracycline, tylosin, and penicillins are used to treat respiratory and intestinal infections, but colistin has not been used in ostriches in over a decade (Olivier A, pers. comm., 2020).
The World Organisation for Animal Health (OIE) specifically recommends that antibiotics should be added to viral transport media for IAV screening, 19 but this has not been a standard practice in South Africa. Other studies report that PBS should be avoided as a transport medium when virus isolation will be performed because the virus is less stable in PBS, which significantly reduces the sensitivity of isolation compared to a protein-buffered medium. 16 Further studies should investigate the inclusion of broad-spectrum antimicrobials such as sulfonamide and enrofloxacin in a protein-based transport medium for swabs to assess whether virus isolation rates from ostriches can be improved.
Supplemental Material
Supplemental material, sj-pdf-1-vdi-10.1177_10406387211034483 for Identification of bacteria in the tracheal swabs of farmed ostriches and their effect on the viability of influenza A virus by Celia Abolnik, Christine Strydom, Debbie Landman and Reneé Pieterse in Journal of Veterinary Diagnostic Investigation
Acknowledgments
We thank Nicky Olivier, Renate Zipfel, and Dionne Rauff for technical assistance.
Footnotes
Declaration of conflicting interests: The authors declared no conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: Our study was supported by the South African Department of Science and Technology/National Research Foundation’s South African Research Chair Initiative under grant 114612, the Department of Trade and Technology–funded “Healthy Flocks-Quality Leather” grant, and the Western Cape Department of Agriculture. Reneé Pieterse and some of the testing costs were funded from the Belgian Directorate-General for Development Co-operation Framework Agreement (FA4 DGD-ITM 2017-2021) grant FA4-N02000.
ORCID iD: Celia Abolnik  https://orcid.org/0000-0003-3044-465X
https://orcid.org/0000-0003-3044-465X
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Celia Abolnik, Departments of Production Animal Studies, University of Pretoria Faculty of Veterinary Science, Onderstepoort, South Africa.
Christine Strydom, NOSA Testing, Lyttleton, Centurion, South Africa.
Debbie Landman, Veterinary Tropical Diseases, University of Pretoria Faculty of Veterinary Science, Onderstepoort, South Africa.
Reneé Pieterse, Veterinary Tropical Diseases, University of Pretoria Faculty of Veterinary Science, Onderstepoort, South Africa; Provincial Veterinary Laboratory, Western Cape Department of Agriculture, Stellenbosch, South Africa.
References
- 1. Abolnik C, et al. Molecular analysis of the 2011 HPAI H5N2 outbreak in ostriches, South Africa. Avian Dis 2012;56:865–879. [DOI] [PubMed] [Google Scholar]
- 2. Abolnik C, et al. Susceptibility and status of avian influenza in ostriches. Avian Dis 2016;60(Suppl 1):286–295. [DOI] [PubMed] [Google Scholar]
- 3. Abolnik C, et al. The incursion and spread of highly pathogenic avian influenza H5N8 clade 2.3.4.4 within South Africa. Avian Dis 2019;63(Suppl 1):149–156. [DOI] [PubMed] [Google Scholar]
- 4. Clinical Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing. 28th ed. CLSI, 2018. [Google Scholar]
- 5. Department of Agriculture, Forestry and Fisheries, Republic of South Africa. A profile of the South African ostrich market value chain, 2017. https://www.nda.agric.za/doaDev/sideMenu/Marketing/Annual%20Publications/Commodity%20Profiles/Ostrich%20Market%20Value%20Chain%20Profile%202017.pdf
- 6. Elliott DR, et al. Cultivable oral microbiota of domestic dogs. J Clin Microbiol 2005;43:5470–5476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Falagas ME, Kasiakou SK. Colistin: the revival of polymyxins for the management of multidrug-resistant gram-negative bacterial infections. Clin Infect Dis 2005;40:1333–1341. [DOI] [PubMed] [Google Scholar]
- 8. Fracchia L, et al. Potential therapeutic applications of microbial surface-active compounds. AIMS Bioeng 2015;2:144–162. [Google Scholar]
- 9. Irfan-Maqsood M, Seddiq-Shams M. Rhamnolipinds: well-characterized glycolipids with potential broad applicability as biosurfactants. Industrial Biotechnol 2014;10:285–291. [Google Scholar]
- 10. Markey B, et al. Clinical Veterinary Microbiology. 2nd ed. Mosby Elsevier, 2013. [Google Scholar]
- 11. Melville PA, et al. Determinação da microbiota presente na cloaca e orofaringe de avestruzes (Struthio camelus) clinicamente sadios [Determination of the microbiota present in cloaca and oropharynx of clinically normal ostriches (Struthio camelus)]. Cienc Rural 2004;34:1871–1876. Portuguese. [Google Scholar]
- 12. Munster VJ, et al. Practical considerations for high-throughput influenza A virus surveillance studies of wild birds by use of molecular diagnostic tests. J Clin Microbiol 2009;47:666–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rainey FA, et al. Dietzia, a new genus including Dietzia maris comb. nov., formerly Rhodococcus maris. Int J Syst Bacteriol 1995;45:32–36. [DOI] [PubMed] [Google Scholar]
- 14. Reed LJ, Muench H. A simple method for estimating fifty per cent endpoints. Am J Epidemiol 1938;27:493–497. [Google Scholar]
- 15. Shi Z, Gewirtz AT. Together forever: bacterial–viral interactions in infection and immunity. Viruses 2018;10:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Spackman E, et al. Optimal specimen collection and transport methods for the detection of avian influenza virus and Newcastle disease virus. BMC Vet Res 2013;9:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tang J. Microbial metabolomics. Curr Genomics 2011;12:391–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang W, et al. Oil degradation and biosurfactant production by the deep sea bacterium Dietzia maris As-13-3. Front Microbiol 2014;5:711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. World Organisation for Animal Health (OIE). Chapter 3.3.4. Avian influenza (including infection with high pathogenicity avian influenza viruses). In: OIE Terrestrial Manual. OIE, 2021. http://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/3.03.04_AI.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-vdi-10.1177_10406387211034483 for Identification of bacteria in the tracheal swabs of farmed ostriches and their effect on the viability of influenza A virus by Celia Abolnik, Christine Strydom, Debbie Landman and Reneé Pieterse in Journal of Veterinary Diagnostic Investigation