Abstract
Aims
The mental health of slum residents is under-researched globally, and depression is a significant source of worldwide morbidity. Brazil's large slum-dwelling population is often considered part of a general urban-poor demographic. This study aims to identify the prevalence and distribution of depression in Brazil and compare mental health inequalities between slum and non-slum populations.
Methods
Data were obtained from Brazil's 2019 National Health Survey. Slum residence was defined based on the UN-Habitat definition for slums and estimated from survey responses. Doctor-diagnosed depression, Patient Health Questionnaire (PHQ-9)-screened depression and presence of undiagnosed depression (PHQ-9-screened depression in the absence of a doctor's diagnosis) were analysed as primary outcomes, alongside depressive symptom severity as a secondary outcome. Prevalence estimates for all outcomes were calculated. Multivariable logistic regression models were used to investigate the association of socioeconomic characteristics, including slum residence, with primary outcomes. Depressive symptom severity was analysed using generalised ordinal logistic regression.
Results
Nationally, the prevalence of doctor diagnosed, PHQ-9 screened and undiagnosed depression were 9.9% (95% confidence interval (CI): 9.5–10.3), 10.8% (95% CI: 10.4–11.2) and 6.9% (95% CI: 6.6–7.2), respectively. Slum residents exhibited lower levels of doctor-diagnosed depression than non-slum urban residents (8.6%; 95% CI: 7.9–9.3 v. 10.7%; 95% CI: 10.2–11.2), while reporting similar levels of PHQ-9-screened depression (11.3%; 95% CI: 10.4–12.1 v. 11.3%; 95% CI: 10.8–11.8). In adjusted regression models, slum residence was associated with a lower likelihood of doctor diagnosed (adjusted odds ratio (adjusted OR): 0.87; 95% CI: 0.77–0.97) and PHQ-9-screened depression (adjusted OR: 0.87; 95% CI: 0.78–0.97). Slum residents showed a greater likelihood of reporting less severe depressive symptoms. There were significant ethnic/racial disparities in the likelihood of reporting doctor-diagnosed depression. Black individuals were less likely to report doctor-diagnosed depression (adjusted OR: 0.66; 95% CI: 0.57–0.75) than white individuals. A similar pattern was observed in Mixed Black (adjusted OR: 0.72; 95% CI: 0.66–0.79) and other (adjusted OR: 0.63; 95% CI: 0.45–0.88) ethnic/racial groups. Slum residents self-reporting a diagnosis of one or more chronic non-communicable diseases had greater odds of exhibiting all three primary depression outcomes.
Conclusions
Substantial inequalities characterise the distribution of depression in Brazil including in slum settings. People living in slums may have lower diagnosed rates of depression than non-slum urban residents. Understanding the mechanisms behind the discrepancy in depression diagnosis between slum and non-slum populations is important to inform health policy in Brazil, including in addressing potential gaps in access to mental healthcare.
Key words: Depression, Brazil, slums, inequalities, PHQ-9, LMIC, urban health
Introduction
Mental health morbidities, including major depressive disorder (depression), account for an ever-increasing proportion of the global disease burden (Liu et al., 2020). Depression is estimated to affect nearly 280 million people globally (Global Burden of Disease Collaborative Network, 2020). This burden is predominantly focused in low- and middle-income countries (LMICs) as over 80% of global depression-related disability comes from these settings (Global Burden of Disease Collaborative Network, 2020). Recognition of depression's role as a cause of disability and its association with deteriorating physical health (Patten et al., 2008) has been accompanied by action to raise the profile of mental health conditions at an international level. Target 3.4 of the United Nations (UN) Sustainable Development Goals (SDGs), aiming for a one-third reduction in premature mortality from non-communicable diseases (NCDs) by 2030 (United Nations Development Programme, 2021), includes tackling mental health challenges alongside those posed by other NCDs. Moreover, in 2019 the World Health Organization (WHO) launched a ‘Special Initiative for Mental Health’ (World Health Organization, 2019) aimed at expanding health coverage for common mental disorders, including depression, as a necessity for achieving Universal Health Coverage.
Brazil has a considerable and growing country-level burden of depression, increasing from 7.9% in 2013 to 10.8% in 2019 (Souza Lopes et al., 2021). Brazil's Unified Health System (Sistema Único de Saúde; SUS) has a strong focus on primary care and health promotional activities at the local level (Macinko and Harris, 2015). Teams of community health workers, nurses and physicians – under the national Family Health Strategy (FHS) – provide basic mental health services, frequently supported by mental health specialists (Soares and de Oliveira, 2016). Expansion of the FHS has been shown to reduce urban inequalities in health outcomes (Bastos et al., 2017; Pinto and Giovanella, 2018; Hone et al., 2020). Despite this research, the mental health of Brazil's slum populations remains infrequently studied.
This lack of research into the mental health of the more than 1 billion people estimated to live in slums (UN-Habitat, 2015) is a global issue. The health of slum residents is not only of importance due to the size of this population but also because of the impacts that slums, as diverse spatial entities and concentrations of deprivation (Rice and Rice, 2009; Nolan et al., 2018), have on mental health outcomes. Although no universally accepted definition of a slum has been formulated, they are broadly characterised as deprived urban areas with a lack of access to basic public services (Ezeh et al., 2017). Many slums exhibit common traits including violence, little open space for relaxation and poor sanitation (Lilford et al., 2017). Qualitative and cross-sectional quantitative research in India has found a considerable burden of common mental disorders, including anxiety and depression, in slum areas (Subbaraman et al., 2014). The impacts of lived environments on health are known as ‘neighbourhood effects’ and have been suggested to play a role in negatively mediating health outcomes in slum areas (Lilford et al., 2019). Studies conducted with people living in slums in Ghana found that community-level influences such as poor sanitation and crime can contribute to poor mental health outcomes (Greif and Nii-Amoo Dodoo, 2015), whereas studies from Hong Kong and other areas have shown that household-level deprivation (Cheung and Chou, 2019; Chung et al., 2020) and individual poor socioeconomic status (Lorant et al., 2007) are associated with increased rates of depressive symptoms.
Over 16% of Brazil's urban population are estimated to live in slums (The World Bank, 2018). Those living in slums are usually the largest and poorest urban population groups in Brazil and their mental health has been infrequently studied. Despite the distinction of slum areas in national statistics, Brazilian research on depression often examines only urban (Ferrari et al., 2013) and rural (Corrêa et al., 2020) differences, whereas the prevalence of depression within urban populations, including within slum populations have not been explored.
The lack of analysis of depression between different sociodemographic groups in Brazilian urban and slum environments provides an opportunity for further exploration. This study aimed to investigate how doctor diagnosed, screened and undiagnosed prevalence measures of depression vary between slum and non-slum populations and the Brazilian population at large. We also explored the socioeconomic patterns associated with the prevalence of these depression outcomes and establish whether they vary between slum and non-slum populations. Finally, we investigated how the severity of depressive symptoms varies in these same populations.
Methods
Study design
This observational, cross-sectional study made use of data collected during the 2019 Brazilian National Health Survey (Pesquisa Nacional de Saúde – PNS).
Data source
The PNS is a nationwide household survey conducted by the Brazilian Institute of Geography and Statistics (IBGE) and the Brazilian Ministry of Health (Stopa et al., 2020). First carried out in 2013, it aims to ‘evaluate health conditions {and} health service access’ as well as perform ‘surveillance of non-communicable diseases and their social determinants’ (Stopa et al., 2020). The PNS targets individuals aged 15 and over, living in ‘permanent private dwellings’ (Stopa et al., 2020). In the PNS 2019, a total of 279 382 households and 94 114 respondents to the individual questionnaire were included. Individual respondents were randomly selected from all household members aged 15 and above. Data were collected between August 2019 and March 2020 (Stopa et al., 2020). The survey collected individual socio-demographic information (e.g. age, sex, ethnicity/race and education) and contained modules addressing such themes as: general health status, lifestyle, communicable and NCDs and health service usage, among others. Weighting of responses adjusted for likelihood of selection and rate of non-response by sex and age category.
Ethical considerations
No ethical approval was required for this analysis as it uses secondary data. The individual anonymised dataset is publicly available from IBGE (https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?=&t=downloads).
Measures
Primary outcomes
This study considers three primary outcomes: PHQ-9 screened, doctor diagnosed and undiagnosed depression. The PNS used two metrics to gauge depression prevalence. It used the Patient Health Questionnaire-9 (PHQ-9) for depression screening alongside asking about previous depression diagnosis. PHQ-9-screened depression was determined by asking participants to respond to all nine questions from the PHQ-9 depression screening questionnaire. Doctor-diagnosed depression was established by asking respondents whether they had previously been given a diagnosis of depression by a psychiatrist or psychologist. Finally, we considered undiagnosed depression in individuals who met the PHQ-9 definition of depression but did not report previous diagnosis by a health professional.
Each of the PHQ-9 questionnaire's nine questions gathers information about one depressive symptom from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V) (Kroenke et al., 2001). This study classified respondents as exhibiting symptoms indicative of significant major depressive disorder if their aggregate PHQ-9 score was ⩾10. Validation of the questionnaire in Brazil and elsewhere has found that this cut-off point confers considerable diagnostic validity (Spitzer et al., 1999; Kroenke et al., 2001; Manea et al., 2012; Santos et al., 2013) and maximises both sensitivity and specificity (Levis et al., 2019). Portuguese translations of PHQ-9 questions can be found in online Supplementary Table 1. Portuguese adaptations of the questionnaire have been performed by Brazilian psychiatrists in previously published research (Fraguas et al., 2006) which was used in Santos and colleagues' 2013 validation of the tool.
One further primary outcome, undiagnosed depression, was derived. A respondent was coded positively for undiagnosed depression if they met the PHQ-9 definition of depression but did not report previous diagnosis by a health professional.
Secondary outcomes
This study examined five categories of depressive symptom severity, defined by respondents' aggregate PHQ-9 score. Scores of 5–9, 10–14, 15–19 and ⩾20 were coded as mild, moderate, moderately-severe and severe depressive symptoms, respectively (Kroenke et al., 2001). Mild depressive symptoms (PHQ-9 score ⩽9) were not considered indicative of major depressive disorder for this analysis, as indicated above. However, even mild symptoms have been shown to negatively impact day-to-day mental wellbeing and quality of life (Coyne et al., 1994; Brenes, 2007) and thus were considered for analysis as a secondary outcome. A new categorical, ordinal variable, depression severity, was derived based off aggregate PHQ-9 score.
Exposures of interest
The main exposure variable of interest was slum residence. A designation based on the operational definition of a slum of the UN Human Settlements Programme (UN-Habitat) (UN-Habitat, 2015) was used to classify respondents as slum or non-slum urban residents according to their responses to PNS questions: access – or lack thereof – to improved sanitation, water and household construction and the presence of overcrowded living conditions (⩾3 residents per room) (UN-Habitat, 2015). As no section of the PNS addressed security of respondents' residential tenure, that component of the UN-Habitat definition was not incorporated.
Urban-dwelling respondents who met one or more of these conditions were classified as slum residents. Available data were mapped onto the concepts contained in the UN-Habitat definition. Table 1 demonstrates the five characteristics, and the variables used to discern them, that were employed to categorise respondents as slum residents.
Table 1.
Attributes used to define variable of interest (slum or non-slum)
| Component of the UN-Habitat definition | Questions from PNS used identify presence/absence of component | Responses to questions indicative of component of slum definition |
|---|---|---|
| Urban setting (Ezeh et al., 2017) |
|
|
| Overcrowding (UN-Habitat, 2015) |
|
|
| Lack of access to improved drinking water (UN-Habitat, 2015) |
|
|
| Lack of access to improved sanitation (UN-Habitat, 2015) |
|
|
| Lack of durable housing (UN-Habitat, 2015) |
|
|
Note: Slum residents were defined as those who reported residing in an urban area and who met one or more of the other components of the modified UN-Habitat slum definition derived from PNS responses.
A range of other sociodemographic characteristics were included in the analyses. Selected variables were included either because of their previously determined association with depression in Brazil and other settings (e.g. age, sex, smoking status, alcohol consumption, comorbidity and physical activity) (Ford and Erlinger, 2004; Ströhle, 2009; Zivin et al., 2010; Stopa et al., 2015; Souza Lopes et al., 2016; Barros et al., 2017; Lever-van Milligen et al., 2017; Tampubolon and Maharani, 2017) or their potential to behave as confounders in the multivariable analysis of slum residence and depression prevalence (e.g. socioeconomic status, income and health service access) (Szwarcwald et al., 2011; Jankowska et al., 2012; Araya et al., 2018).
The specific sociodemographic attributes of respondents included were: sex (male or female); age (categorised into 15–24 years, 25–34, 35–44, 45–54, 55–64, 65–75, 75 and over); level of education (no formal education, incomplete elementary, complete elementary, incomplete secondary, complete secondary, incomplete tertiary, complete tertiary education); self-reported ethnicity/race (White, Black, Mixed Black, or other (Asian, Indigenous or not reported)); dwelling (urban slum, urban non-slum, rural); presence of comorbidities (categorised as having 1, 2 or 3 or more chronic conditions); registration with the Family Health Strategy (yes, no, unknown); physical activity history (some or no engagement in physical activity in the last 3 months); current smoking status (yes or no); alcohol consumption (currently drinking or not); enrolment in a private medical insurance scheme (PMI) (yes or no) and household income (reported as: less than ¼ minimum wage, ¼–½ min. wage, ½–1× min. wage, 1–2× min. wage, 2–3× min. wage, 3–5× min. wage, ⩾5× min. wage). The Brazilian annual minimum wage was USD 5198.40 in 2020 when adjusted for purchasing power (Organisation for Economic Co-operation and Development, 2021).
Respondents identifying as part of the Asian or Indigenous groups were combined with those who ignored the question and categorised as one subpopulation (other) for analysis due to their relatively small size compared to other categories. FHS registration status was included as a covariate due to the role it has been reported to play in reducing inequities in healthcare access in Brazil in the last 15 years (Paim et al., 2011; Hone et al., 2020).
Statistical analyses
The prevalence of the outcomes was descriptively analysed. Frequencies were weighted to account for survey design and adjust for the composition of Brazil's adult population.
Multivariable binary logistic regression was performed to explore the association between dwelling (urban slum, urban non-slum, rural) and other socioeconomic factors on depression prevalence. This allowed for associations with individual covariates, including slum residence, to be examined after controlling for other explanatory variables. Covariates were tested for collinearity. All exhibited variance inflation factors of less than 2 (James et al., 2013) and were thus not excluded from the model. Adjusted odds ratios (adjusted OR) with 95% confidence intervals (95% CIs) and p-values were estimated. Statistical significance was defined as p < 0.05.
In subsequent analyses, dwelling was interacted with selected socio-demographic covariates to identify inequalities between slums and non-slum areas in the associations between depression outcomes and socioeconomic factors. This tested whether socioeconomic inequalities differed between slum and non-slum areas. Covariates selected for interaction analysis were: number of comorbidities, sex, age, education and ethnicity/race given their previously documented relationship to depression and healthcare access in Brazil (Stopa et al., 2015; Souza Lopes et al., 2016).
For secondary outcomes, generalised ordinal logistic (GOL) regression analysis was carried out to investigate the sociodemographic patterning of depressive symptom severity in Brazil. All covariates from the multivariable analysis were included. Brant testing of a normal ordinal logistic regression model revealed that the regression coefficients for each individual covariate differed significantly between each level of symptom severity. As such, the proportional odds and parallel line assumptions were violated, and a GOL model was selected (Williams, 2006).
All analyses were completed using Stata v16.1® (Stata Corp., College Station, TX, USA).
Results
Descriptive analysis
A total of 90 846 individuals aged 15 years or over, who answered the individual questionnaire, were included in the analysis (Table 2). The proportion of individuals identifying as female was 53.0% (95% CI: 52.4–53.6). Most individuals were under age 45, with 18.6% (95% CI: 18.0–19.2) younger than 25. The proportion of individuals living in slums was 14.3% (95% CI: 13.7–15.0). The prevalence of doctor-diagnosed depression was 9.9% (95% CI: 9.5–10.3). The prevalence of PHQ-9-screened depression was higher at 10.8% (95% CI: 10.4–11.2). The proportion of undiagnosed depression was estimated at 6.9% (95% CI: 6.6–7.2).
Table 2.
Description of the PNS sample that answered the individual health questionnaire (n = 90 846)
| Prevalence | |||||
|---|---|---|---|---|---|
| Respondents | Proportion of Brazilian population | Doctor-diagnosed depression | PHQ-9-screened depression (⩾10) | Undiagnosed depression | |
| Total | 90 846 | 100.0% | 9.9% (9.5–10.3) | 10.8% (10.4–11.2) | 6.9% (6.6–7.2) |
| Sex | |||||
| Female | 48 047 | 53.0% (52.4–53.6) | 14.3% (13.7–14.9) | 15.1% (14.4–15.7) | 9.3% (8.8–9.8) |
| Male | 42 799 | 47.1% (46.5–47.7) | 4.9% (4.6–5.3) | 6.0% (5.6–6.4) | 4.2% (3.9–4.6) |
| Age category | |||||
| 15–24 | 10 460 | 18.6% (18.0–19.2) | 5.3% (4.6–6.2) | 10.8% (9.7–11.9) | 8.1% (7.2–9.1) |
| 25–34 | 15 970 | 17.1% (16.6–17.6) | 7.1% (6.4–7.8) | 9.6% (8.8–10.5) | 6.6% (5.9–7.3) |
| 35–44 | 18 033 | 19.1% (18.7–19.6) | 10.8% (9.9–11.7) | 10.6% (9.8–11.3) | 6.5% (6.0–7.2) |
| 45–54 | 15 885 | 16.9% (16.4–17.3) | 12.7% (11.8–13.7) | 11.8% (10.9–12.7) | 6.8% (6.1–7.5) |
| 55–64 | 14 572 | 14.2% (13.8–14.6) | 13.4% (12.3–14.5) | 11.4% (10.5–12.4) | 6.3% (5.6–7.0) |
| 65–74 | 9965 | 8.9% (8.5–9.2) | 11.8% (10.7–13.0) | 10.0% (9.0–11.2) | 6.2% (5.5–7.1) |
| 75+ | 5961 | 5.2% (5.0–5.5) | 10.2% (8.9–11.6) | 12.0% (10.7–13.5) | 8.6% (7.5–9.8) |
| Education level | |||||
| Without education | 7658 | 5.8% (5.6–6.1) | 8.0% (7.0–9.2) | 12.8% (11.6–14.2) | 9.1% (8.0–10.3) |
| Incomplete elementary or equivalent | 28 618 | 28.5% (27.9–29.1) | 11.0% (10.4–11.7) | 12.1% (11.4–12.8) | 7.7% (7.2–8.3) |
| Complete elementary or equivalent | 7167 | 8.8% (8.5–9.1) | 8.9% (7.8–10.2) | 11.1% (9.9–12.5) | 7.5% (6.5–8.7) |
| Incomplete secondary or equivalent | 6353 | 8.6% (8.3–9.0) | 7.7% (6.5–9.1) | 11.3% (9.8–13.0) | 7.3% (6.2–8.4) |
| Complete secondary or equivalent | 23 471 | 28.4% (27.9–29.0) | 8.6% (8.0–9.3) | 9.4% (8.7–10.1) | 6.2% (5.6–6.8) |
| Incomplete 3° or equivalent | 3962 | 4.8% (4.6–5.1) | 11.2% (9.3–13.4) | 13.0% (10.9–15.3) | 7.9% (6.4–9.8) |
| Graduated from 3° | 13 617 | 15.0% (14.4–15.6) | 12.2% (11.3–13.2) | 9.0% (8.1–10.0) | 5.0% (4.3–5.8) |
| Ethnicity/race | |||||
| White | 33 133 | 42.9% (42.2–43.7) | 12.1% (11.5–12.8) | 10.6% (10.0–11.2) | 6.3% (5.8–6.8) |
| Black | 10 345 | 11.4% (11.0–11.8) | 7.9% (7.1–8.8) | 11.7% (10.7–12.8) | 8.2% (7.4–9.1) |
| Mixed Black | 45 994 | 44.2% (43.5–44.8) | 8.3% (7.8–8.8) | 10.7% (10.2–11.3) | 7.2% (6.7–7.6) |
| Other | 1374 | 1.5% (1.3–1.7) | 7.7% (5.6–10.5) | 10.0% (7.0–14.3) | 7.6% (4.8–11.8) |
| Dwelling | |||||
| Urban slum | 20 741 | 14.3% (13.7–15.0) | 8.6% (7.9–9.3) | 11.3% (10.4–12.1) | 7.7% (7.0–8.4) |
| Urban non-slum | 49 132 | 71.6% (70.8–72.4) | 10.7% (10.2–11.2) | 11.3% (10.8–11.8) | 7.1% (6.8–7.5) |
| Rural | 20 973 | 14.1% (13.7–14.5) | 7.2% (6.6–7.8) | 7.6% (6.9–8.2) | 5.0% (4.5–5.5) |
| Number of comorbidities | |||||
| 0 | 46 427 | 53.1% (52.5–53.8) | 5.3% (5.0–5.7) | 6.8% (6.3–7.2) | 5.0% (4.6–5.4) |
| 1 | 25 087 | 26.7% (26.2–27.2) | 10.7% (10.0–11.4) | 11.3% (10.6–12.1) | 7.4% (6.8–8.0) |
| 2 | 11 621 | 12.0% (11.6–12.3) | 16.3% (15.1–17.6) | 16.0% (14.9–17.3) | 10.0% (9.1–11.0) |
| 3+ | 7711 | 8.2% (7.9–8.6) | 27.3% (25.3–29.3) | 27.2% (25.6–29.0) | 13.1% (11.9–14.4) |
| Registered with the FHS | |||||
| Registered | 57 500 | 61.8% (60.7–62.9) | 9.9% (9.4–10.3) | 11.1% (10.6–11.7) | 7.1% (6.8–7.5) |
| Not registered | 22 512 | 26.9% (25.9–27.9) | 10.0% (9.3–10.7) | 10.5% (9.7–11.4) | 6.8% (6.2–7.4) |
| Unknown | 10 834 | 11.3% (10.8–11.9) | 9.9% (8.8–11.0) | 9.5% (8.5–10.6) | 6.0% (5.2–6.9) |
| Physically active in last 3 months | |||||
| Yes | 36 398 | 43.4% (42.7–44.1) | 9.3% (8.6–9.9) | 8.3% (7.8–8.9) | 5.2% (4.8–5.6) |
| No | 54 448 | 56.6% (55.9–57.3) | 10.4% (9.9–10.9) | 12.7% (12.1–13.2) | 8.2% (7.8–8.7) |
| Smoking status | |||||
| Non-smoker | 79 460 | 87.8% (87.5–88.2) | 9.7% (9.3–10.1) | 10.2% (9.8–10.7) | 6.6% (6.3–6.9) |
| Smoker | 11 386 | 12.2% (11.8–12.5) | 11.4% (10.4–12.4) | 14.7% (13.5–16.0) | 9.3% (8.3–10.4) |
| Drinks alcohol | |||||
| No | 55 430 | 58.9% (58.3–59.6) | 11.1% (10.6–11.6) | 11.9% (11.4–12.4) | 7.4% (7.0–7.8) |
| Yes | 35 416 | 41.1% (40.4–41.7) | 8.2% (7.7–8.7) | 9.2% (8.7–9.8) | 6.2% (5.8–6.7) |
| Enrolled in private health plan | |||||
| Yes | 20 568 | 26.6% (25.8–27.3) | 12.4% (11.6–13.2) | 9.3% (8.6–10.1) | 5.3% (4.8–5.9) |
| No | 70 278 | 73.4% (72.7–74.2) | 9.0% (8.6–9.4) | 11.3% (10.9–11.8) | 7.5% (7.1–7.9) |
| Household income | |||||
| <0.25× MW | 9550 | 8.2% (7.9–8.6) | 8.1% (7.1–9.1) | 12.7% (11.5–14.0) | 9.0% (8.0–10.1) |
| 0.25–0.5× MW | 14 147 | 14.9% (14.4–15.3) | 8.2% (7.4–9.0) | 12.4% (11.4–13.4) | 8.4% (7.6–9.3) |
| 0.5–1.0× MW | 26 406 | 29.2% (28.6–29.8) | 9.3% (8.6–10.0) | 11.5% (10.8–12.2) | 7.6% (7.0–8.1) |
| 1–2× MW | 22 466 | 27.5% (27.0–28.1) | 10.1% (9.4–10.9) | 10.3% (9.5–11.1) | 6.5% (5.9–7.2) |
| 2–3× MW | 7612 | 8.9% (8.6–9.3) | 12.1% (10.6–13.7) | 9.3% (8.1–10.7) | 4.9% (4.2–5.7) |
| 3–5× MW | 5554 | 6.2% (5.9–6.5) | 11.9% (10.6–13.4) | 7.8% (6.6–9.2) | 4.5% (3.7–5.4) |
| 5+× MW | 5089 | 5.0% (4.6–5.4) | 13.7% (12.2–15.4) | 7.9% (6.7–9.3) | 4.0% (3.2–5.0) |
FHS, family health strategy; MW, minimum wage.
Note: Prevalence of self-reported depression diagnosis, PHQ-9-screened depression and undiagnosed depression displayed (95% CI). PHQ-9 information was not available for 3268 of the 94 114 individual respondents.
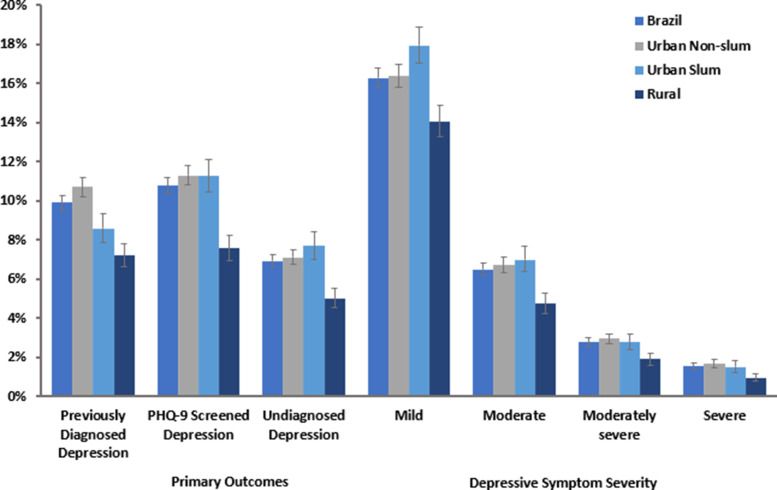
The prevalence of doctor-diagnosed depression was lower in urban slum-dwelling populations (8.6%; 95% CI: 7.9–9.3) than in urban non-slum populations (10.7%; 95% CI: 10.2–11.2) (Fig. 1). PHQ-9-diagnosed depression estimates were similar between the two groups, with slum and non-slum urban populations both reporting a prevalence of 11.3% with 95% CIs of 10.5–12.3 and 10.8–11.8, respectively. The prevalence of undiagnosed depression was similar in urban slum (7.7%; 95% CI: 7.0–8.4) and urban non-slum (7.1%; 95% CI: 6.8–7.5) subgroups but was lower in rural areas (5.0%; 95% CI: 4.5–5.5). Rural populations had a lower prevalence of all depression outcomes than urban populations. Aside from the higher prevalence of mild depression in urban-slum populations (17.9%; 95% CI: 17.0–19.0), there was no substantial difference in the distribution of symptom severity between the different urban sub-groups.
Fig. 1.
Estimated prevalence of depression outcomes (non-age-adjusted) in the Brazilian population by location of residence.
Note: Error bars represent 95% confidence interval. Disease severity based on aggregate PHQ-9 score.
Females were more likely to report higher levels of all depression outcomes than males with the largest differences in doctor diagnosed (14.3%; 95% CI: 13.7–14.9 v. 4.9%; 95% CI: 4.6–5.3) and PHQ-9-screened depression (15.1%; 95% CI: 14.4–15.7 v. 6.0%; 95% CI: 5.6–6.4). The prevalence of doctor-diagnosed depression was found to increase with age from 5.3% (95% CI: 4.6–6.2) in 15–24-year-olds to a peak of 13.4% (95% CI: 12.3–14.5) among 55–64-year-olds. Such a steep gradient was not visible in PHQ-9-screened depression, with 10.8% (95% CI: 9.7–11.9) of 15–24-year-olds classified as depressed compared to 11.4% (95% CI: 10.5–12.4) of 55–64-year-olds.
Rates of doctor-diagnosed depression were lower in Black (7.9%; 95% CI: 7.1–8.8), and Mixed Black (8.3%; 95% CI: 7.8–8.8) ethnic/racial groups compared to those self-classifying as White (12.1%; 95% CI: 11.5–12.8). Rates of PHQ-9-diagnosed depression, however, were similar across racial/ethnic groups. Higher income groups reported greater rates of doctor-diagnosed depression (13.7%; 95% CI: 12.2–15.4 v. 8.1%; 95% CI: 7.1–9.1, highest v. lowest income category) and a lower prevalence of PHQ-9-screened depression (7.9%; 95% CI: 6.7–9.3 v. 12.7%: 95% CI: 11.5–14.0).
Socioeconomic patterning of depression outcomes
In the multivariable logistic regression analysis we found that, after adjusting for all socioeconomic variables, individuals living in slums had a lower likelihood of reporting doctor diagnosed (adjusted OR: 0.87; 95% CI: 0.77–0.97) and PHQ-9-screened depression (adjusted OR: 0.87; 95% CI: 0.78–0.97) when compared to urban non-slum populations (Table 3).
Table 3.
Results from multivariable logistic regression analysis
| Doctor-diagnosed depression | PHQ-9-screened depression | Undiagnosed depression | ||||
|---|---|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Sex | ||||||
| Male | 1 (ref) | – | – | – | – | – |
| Female | 2.77*** | (2.52–3.05) | 2.43*** | (2.22–2.67) | 2.12*** | (1.90–2.37) |
| Age category | ||||||
| 15–24 | 1 (ref) | – | – | – | – | – |
| 25–34 | 1.21 | (0.99–1.47) | 0.78** | (0.67–0.92) | 0.73*** | (0.61–0.87) |
| 35–44 | 1.58*** | (1.30–1.92) | 0.70*** | (0.60–0.82) | 0.61*** | (0.52–0.72) |
| 45–54 | 1.47*** | (1.20–1.79) | 0.61*** | (0.52–0.72) | 0.52*** | (0.44–0.63) |
| 55–64 | 1.17 | (0.95–1.43) | 0.43*** | (0.36–0.51) | 0.39*** | (0.32–0.48) |
| 65–74 | 0.82 | (0.65–1.02) | 0.31*** | (0.25–0.38) | 0.35*** | (0.28–0.43) |
| 75+ | 0.63*** | (0.49–0.81) | 0.34*** | (0.27–0.42) | 0.44*** | (0.35–0.56) |
| Education level | ||||||
| Without education | 1 (ref) | – | – | – | – | – |
| Incomplete elementary or equivalent | 1.34*** | (1.13–1.60) | 0.87* | (0.75–1.00) | 0.80** | (0.69–0.94) |
| Complete elementary or equivalent | 1.23 | (0.99–1.54) | 0.85 | (0.70–1.03) | 0.80* | (0.65–0.99) |
| Incomplete high school or equivalent | 1.37* | (1.06–1.78) | 0.88 | (0.70–1.10) | 0.71** | (0.56–0.90) |
| Complete high school or equivalent | 1.20 | (0.99–1.45) | 0.74*** | (0.63–0.87) | 0.68*** | (0.57–0.81) |
| Incomplete 3° or equivalent | 1.78*** | (1.32–2.40) | 1.18 | (0.91–1.53) | 0.94 | (0.71–1.26) |
| Graduated from 3° | 1.37** | (1.11–1.71) | 0.87 | (0.70–1.07) | 0.73* | (0.56–0.96) |
| Ethnicity/race | ||||||
| White | 1 (ref) | – | – | – | – | – |
| Black | 0.66*** | (0.57–0.75) | 1.00 | (0.88–1.14) | 1.15 | (0.99–1.34) |
| Mixed Black | 0.72*** | (0.66–0.79) | 0.94 | (0.86–1.03) | 1.03 | (0.92–1.15) |
| Other | 0.63** | (0.45–0.88) | 0.87 | (0.55–1.37) | 1.10 | (0.64–1.91) |
| Dwelling | ||||||
| Urban non-slum | 1 (ref) | – | – | – | – | – |
| Urban slum | 0.87* | (0.77–0.97) | 0.87* | (0.78–0.97) | 0.92 | (0.82–1.03) |
| Rural | 0.81*** | (0.73–0.91) | 0.58*** | (0.51–0.65) | 0.57*** | (0.50–0.65) |
| Number of comorbidities | ||||||
| 0 | 1 (ref) | – | – | – | – | – |
| 1 | 2.08*** | (1.87–2.32) | 2.04*** | (1.83–2.27) | 1.76*** | (1.55–1.99) |
| 2 | 3.35*** | (2.95–3.82) | 3.41*** | (3.02–3.85) | 2.68*** | (2.31–3.10) |
| 3+ | 6.62*** | (5.68–7.71) | 7.14*** | (6.28–8.13) | 3.66*** | (3.11–4.30) |
| Registered with the FHS | ||||||
| Registered | 1 (ref) | – | – | – | – | – |
| Not registered | 0.89* | (0.80–0.99) | 1.00 | (0.90–1.12) | 1.05 | (0.93–1.19) |
| Unknown | 1.00 | (0.87–1.15) | 0.94 | (0.82–1.07) | 0.94 | (0.80–1.10) |
| Physically active in last 3 months | ||||||
| Yes | 1 (ref) | – | – | – | – | – |
| No | 1.00 | (0.91–1.11) | 1.36*** | (1.25–1.49) | 1.40*** | (1.26–1.56) |
| Smoking status | ||||||
| Non-smoker | 1 (ref) | – | – | – | – | – |
| Smoker | 1.44*** | (1.28–1.62) | 1.66*** | (1.48–1.86) | 1.50*** | (1.30–1.72) |
| Drinks alcohol | ||||||
| No | 1 (ref) | – | – | – | – | – |
| Yes | 0.82*** | (0.75–0.90) | 0.93 | (0.84–1.02) | 1.03 | (0.92–1.15) |
| Enrolled in private health plan | ||||||
| No | 1 (ref) | – | – | – | – | – |
| Yes | 1.14* | (1.02–1.27) | 0.87* | (0.77–0.99) | 0.84* | (0.72–0.98) |
| Household income | ||||||
| <0.25× MW | 1 (ref) | – | – | – | – | – |
| 0.25–0.5× MW | 1.00 | (0.84–1.20) | 0.97 | (0.83–1.12) | 0.93 | (0.78–1.10) |
| 0.5–1.0× MW | 1.03 | (0.88–1.20) | 0.87 | (0.76–1.00) | 0.84* | (0.71–0.98) |
| 1–2× MW | 1.08 | (0.92–1.27) | 0.82* | (0.70–0.96) | 0.78* | (0.65–0.94) |
| 2–3× MW | 1.23 | (0.98–1.56) | 0.77* | (0.61–0.97) | 0.63*** | (0.50–0.80) |
| 3–5× MW | 1.23 | (0.99–1.54) | 0.68** | (0.53–0.88) | 0.62*** | (0.47–0.82) |
| 5+× MW | 1.41** | (1.09–1.82) | 0.73* | (0.56–0.96) | 0.60** | (0.43–0.84) |
AOR, adjusted odds ratio (fully adjusted model); 95% CI, 95% confidence intervals; FHS, family health strategy; MW, minimum wage.
*p < 0.05, **p < 0.01, ***p < 0.001.
Other socioeconomic inequalities persisted in adjusted regression models. When looking at doctor-diagnosed depression, there was a greater likelihood of depression in females (adjusted OR: 2.77; 95% CI: 2.52–3.05); those aged 35–44 (adjusted OR: 1.58; 95% CI: 1.30–1.92) and 45–54 (adjusted OR: 1.47; 95% CI: 1.20–1.79); and those with one (adjusted OR: 2.08; 95% CI: 1.87–2.32), two (adjusted OR: 3.36; 95% CI: 2.95–3.82) and three or more (adjusted OR: 6.62; 95% CI: 5.69–7.71) comorbidities. PMI enrolment (adjusted OR: 1.14; 95% CI: 1.02–1.27) and a household income of 5+ times the minimum wage (adjusted OR: 1.41; 95% CI: 1.09–1.82) were also associated with an increased likelihood of reporting doctor-diagnosed depression. A lower likelihood of reporting this outcome was observed in those who were of Black (adjusted OR: 0.66; 95% CI: 0.57–0.75), Mixed Black (adjusted OR: 0.72; 95% CI: 0.66–0.79) or other (adjusted OR: 0.63; 95% CI: 0.45–0.88) ethnic/racial groups.
When looking at PHQ-9-screened depression, we observed a higher likelihood of depression in females (adjusted OR: 2.43; 95% CI: 2.22–2.67), those who had not engaged in physical activity in the 3 months preceding the survey (adjusted OR: 1.36; 95% CI: 1.25–1.49) and in smokers (adjusted OR: 1.66; 95% CI: 1.48–1.86). Lower odds of PHQ-9-screened depression was observed in older age categories, for example an adjusted OR of 0.43 (95% CI: 0.36–0.51) in 55–64-year-olds and an adjusted OR of 0.34 (95% CI: 0.27–0.42) in those aged 75 and older. Lower odds of PHQ-9-screened depression were also observed in those in possession of PMI (adjusted OR: 0.87; 95% CI: 0.77–0.99), urban-slum residents (adjusted OR: 0.87; 95% CI: 0.78–0.97) and members of higher household income categories, for example those in receipt of 1–2 times (adjusted OR: 0.82; 95% CI: 0.70–0.96) and 2–3 times (adjusted OR: 0.77; 95% CI: 0.61–0.97) the minimum wage.
The presence of undiagnosed depression was positively associated with female sex (adjusted OR: 2.12; 95% CI: 1.90–2.37), lack of physical activity (adjusted OR: 1.40; 95% CI: 1.26–1.56) and being a smoker (adjusted OR: 1.50; 95% CI: 1.30–1.72). A similar relationship was observed in people reporting one (adjusted OR: 1.76; 95% CI: 1.55–1.99), two (adjusted OR: 2.68; 95% CI: 2.31–3.10) and three or more (adjusted OR: 3.66; 95% CI: 3.11–4.30) comorbidities. Increased age, income and education levels as well as PMI enrolment were also associated with a lower likelihood of undiagnosed depression.
Slum impact on depression severity
Depressive symptom severity was defined using aggregate PHQ-9 score. Slum residents were significantly less likely (adjusted OR: 0.86; 95% CI: 0.78–0.96) than non-slum urban residents to be classified as exhibiting moderate, moderately-severe or severe depressive symptoms v. no or mild symptoms (Table 4; online Supplementary Table 2). Slum residents were also less likely (adjusted OR: 0.77; 95% CI: 0.66–0.89) than non-slum urban populations to exhibit moderately-severe or severe symptoms v. no, mild or moderate symptoms of depression.
Table 4.
Results of generalised ordinal logistic regression analysis of depression by symptom severity (PHQ-9 score)
| 0 v. 1, 2, 3, 4 | 0 and 1 v. 2, 3, 4 | 0, 1, 2 v. 3 and 4 | 0, 1, 2, 3 v. 4 | |||||
|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Urban non-slum | 1 (ref) | – | – | – | – | – | – | – |
| Urban slum | 0.99 | (0.92–1.07) | 0.86** | (0.78–0.96) | 0.77*** | (0.66–0.89) | 0.75* | (0.58–0.96) |
| Rural | 0.67*** | (0.62–0.73) | 0.57*** | (0.51–0.64) | 0.52*** | (0.44–0.61) | 0.46*** | (0.36–0.60) |
AOR, adjusted odds ratio (fully adjusted model); 95% CI, 95% confidence intervals; FHS, family health strategy.
Note: 0 = no depression; 1 = mild symptoms, 2 = moderate symptoms; 3 = moderately-severe symptoms, 4 = severe symptoms.
*p < 0.05, **p < 0.01, ***p < 0.001.
Variation in primary outcomes by socioeconomic characteristics in slum populations
Table 5 shows the interaction between dwelling (urban slum, urban non-slum and rural) with the number of reported comorbidities in the multivariable model (the only significant interaction identified). Slum residents with one and three or more comorbidities had 1.34 (95% CI: 1.02–1.76) and 1.59 (95% CI: 1.16–2.19) greater adjusted odds, respectively, of reporting doctor-diagnosed depression than non-slum urban residents (online Supplementary Table 3). Slum residents with two comorbidities were also more likely to exhibit PHQ-9 screened (adjusted OR: 1.48; 95% CI: 1.12–1.96) and undiagnosed depression (adjusted OR: 1.51; 95% CI: 1.09–2.09). Nearly all other interactions tested were non-significant (online Supplementary Tables 4–7).
Table 5.
Results from interactions between slum residency and number of comorbidities
| Doctor-diagnosed depression | PHQ-9-screened depression | Undiagnosed depression | ||||
|---|---|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Dwelling | ||||||
| Urban non-slum | 1 (ref) | – | – | – | – | – |
| Urban slum | 0.69*** | (0.57–0.84) | 0.76** | (0.64–0.91) | 0.82 | (0.67–1.00) |
| Rural | 0.84 | (0.69–1.03) | 0.49*** | (0.40–0.60) | 0.45*** | (0.36–0.57) |
| Number of comorbidities | ||||||
| 0 | 1 (ref) | – | – | – | – | – |
| 1 | 2.04*** | (1.79–2.33) | 1.99*** | (1.74–2.26) | 1.70*** | (1.45–1.99) |
| 2 | 3.34*** | (2.87–3.90) | 3.08*** | (2.66–3.56) | 2.34*** | (1.96–2.80) |
| 3+ | 6.08*** | (5.07–7.30) | 6.75*** | (5.81–7.84) | 3.44*** | (2.85–4.16) |
| Interaction | ||||||
| Urban slum-dwelling × Number of comorbidities | ||||||
| 0 | 1 (ref) | – | – | – | – | – |
| 1 | 1.34* | (1.02–1.76) | 1.15 | (0.89–1.48) | 1.07 | (0.80–1.42) |
| 2 | 1.25 | (0.93–1.67) | 1.48** | (1.12–1.96) | 1.51* | (1.09–2.09) |
| 3 | 1.59** | (1.16–2.19) | 1.13 | (0.85–1.51) | 1.20 | (0.85–1.69) |
AOR, adjusted odds ratio (fully adjusted model); 95% CI, 95% confidence intervals; FHS, family health strategy; MW, minimum wage.
*p < 0.05, **p < 0.01, ***p < 0.001.
Discussion
Inequalities in the distribution of major depressive disorder in Brazil are stark, including among the country's substantial slum-dwelling population. Although this study found that over one in ten Brazilian individuals exhibited depression, those who were older, female and of White ethnic/racial group reported higher rates of diagnosed depression. Younger people and those with lower levels of education and household income were more likely to have undiagnosed depression. Slum residents had lower levels of doctor-diagnosed depression, a similar level of PHQ-9-screened depression and reported less severe depressive symptoms than non-slum urban residents. However, people who live in slums with comorbidities were at an increased risk of depression than non-slum urban comorbid individuals.
These findings indicate a higher prevalence of PHQ-9-screened depression (10.8%) than studies from 2013 (7.9%) (Souza Lopes et al., 2016), suggesting increases in recent years. Our estimate is also considerably higher than the WHO's own estimates for Brazil (5.8%) and Peru (6.4%) (Hernández-Vásquez et al., 2020). Depression prevalence in urban populations (11.3%) was also greater than in 2013 (8.1%) and other studies from Sao Paulo in 2008 (9.4%) (Andrade et al., 2012).
There was a notable burden of undiagnosed depression (6.9%), suggesting barriers to healthcare seeking behaviours and gaps in access to mental health services. This is lower than found by researchers in Canada and Japan, determining the rates of undiagnosed depression to be 10.9% (Farid et al., 2020) and 8.5% (Yamabe et al., 2019), respectively. However, it is greater than 5.0% found by Lotfaliany and colleagues' analysis of the WHO SAGE Wave 1 study of adults in six LMICs (China, Ghana, India, Mexico, Russia and South Africa) (Lotfaliany et al., 2018).
Inequalities in the distribution of doctor diagnosed and screened depression are stark. The findings echo those of earlier research in Brazil and internationally, which shows female sex, increased age, comorbidities, and smoking are associated with increased odds of depression (Wittayanukorn et al., 2014; Stopa et al., 2015; Souza Lopes et al., 2016; Abdi et al., 2021). Although research has not determined a definitive cause for higher rates of depression in women, previous analysis has suggested that higher Gross National Income (GNI) and shifting gender roles can influence the ratio of depression between males and females (Rai et al., 2013). This study was unable to infer the relationship between smoking status and comorbidity and the depression outcomes studied.
The finding that non-White ethnic/racial groups reported a lower likelihood of doctor-diagnosed depression is also concordant with 2013 data from Brazil (Stopa et al., 2015). This could be an indicative of a gap in access to mental health diagnostic services among Black and Mixed Black ethnic/racial groups. Such a gap has been observed in access to depression treatment (Souza Lopes et al., 2016) as well as prenatal and maternal health services (Matijasevich et al., 2008), breast cancer screening (Oliveira et al., 2011) and overall healthcare utilisation (Boccolini and de Souza Junior, 2016).
Depression results across slum and non-slum populations were mixed. In descriptive prevalence estimates, slum residents had lower levels of doctor-diagnosed depression than non-slum urban residents but had similar levels of PHQ-9-screened depression. However, in adjusted regression models, slum populations had lower odds of doctor-diagnosed and PHQ-9-screened depression compared to non-slum urban populations. These findings suggest that slum residence was associated with a lower likelihood for depression even after adjusting for socioeconomic and health service factors. This is notable as it refutes the a priori expectation that slum residence could negatively impact mental health outcomes independently of socioeconomic factors (Lilford et al., 2017; Lilford et al., 2019).
One possible explanation for the lower likelihood of depression in adjusted models for slum dwellers could be specific social and community aspects of slum-dwelling which are protective against depression. Social capital, including community engagement, social networks and trust, has been related to improved mental health outcomes (Berkman et al., 2000) and has been found to mitigate poor mental health in slum settings (Rabbani et al., 2018). Alternatively, there may be explanations from factors not controlled for in this analysis. Intergenerational co-habitation is one-example, with evidence from Europe and Asia showing it is negatively associated with depressive symptoms (Silverstein et al., 2006; Courtin and Avendano, 2016). Multigenerational dwelling may be inadvertently captured by overcrowding measures used in determining slum residence. Furthermore, high levels of depression have been reported in homeless populations (Perry and Craig, 2015), who would have been excluded from the PNS in slums and as such may have impacted our findings.
The findings from this study also showed that national-level inequalities in the prevalence of depression persist in slums. There were non-significant interactions between slum-residence and socioeconomic variables except for quantity of comorbidities. These results support the idea that slums are not homogenous populations, and efforts to tackle inequalities within slum populations are important. Comorbidities increase both greater medical costs and functional impairment (Moussavi et al., 2007; Kang et al., 2015), contributing to depression. Slum inhabitants with comorbidities may be at a greater risk of depression as they may incur greater healthcare costs (Buigut et al., 2015), need to continue working despite functional impairment (Niessen et al., 2018) or might forgo healthcare. The built environment of slums may further exacerbate poor quality of life for those with comorbidities by increasing barriers to healthcare access.
There are several limitations to the study. First, accurately identifying slum-dwelling populations is challenging. This was not easy using survey data, meaning that this study relied on a household-level definition of slum residence. Therefore, we were unable to account for the contiguous nature of slums (Snyder et al., 2014) that distinguish them from standalone deprived housing. Furthermore, the PNS sample only included respondents living in ‘permanent private dwellings’ (Stopa et al., 2020) and may have excluded those slum residents with more precarious living situations (e.g. people experiencing homelessness). Second, our study's cross-sectional nature precludes causal inference and there may be other unmeasured variables that explain the associations found. Self-reporting bias (Althubaiti, 2016) on the part of survey respondents may also underestimate the true burden of depression in Brazilian slums as well as the country at large.
Future research may benefit from adopting a geospatial approach to slum definition when examining depression outcomes in Brazil. Identifying favela or slum census tracts from the PNS 2019 survey would improve accuracy. City-level analyses using this approach have taken place in Rio de Janeiro (Szwarcwald et al., 2011; Snyder et al., 2014). Additionally, the UN-Habitat definition of slums does not disaggregate which and how many of its five components a slum resident is experiencing (Hacker et al., 2013). Subsequent studies, making use of satellite data with high-resolution remote-sensing capabilities and land-cover data, could monitor evolutions in slum size between decennial censuses (Mahabir et al., 2018).
There are important policy-relevant implications from this study. Notably, that socioeconomic inequalities in depression persist both within and outside slums. There is a need to recognise and tackle the wider socioeconomic determinants of poor health and depression. Although underdiagnosis (Rathod et al., 2017) and undertreatment (Lund et al., 2012) of common mental disorders remain prevalent globally, strengthening community-based mental healthcare operations and the use of lay-workers has proved effective at improving mental health outcomes in LMICs (Patel et al., 2008). Further efforts by the Brazilian government to tackle the causes of NCDs alongside mental health should focus on bolstering the capacity of local health teams to identify common mental disorders such as depression.
Conclusion
Major depressive disorder unequally impacts a large share of the Brazilian population including slum residents. There are persisting socioeconomic inequalities in depression in Brazil, and undiagnosed depression remains a challenge. Slum populations may have lower diagnosed rates of depression than non-slum populations, potentially attributable to a lack of healthcare access, but understanding the mechanisms behind this are important for tackling the determinants of poor mental health, providing appropriate high-quality healthcare services, and making progress towards the SDGs for health and inequalities.
Acknowledgements
CFMP would like to thank Dr Liza Jachens, Dr Marianne Murphy Francke, Ms Katherine Jachens, as well as Max T. Fontaine, Lily M. Rietbergen, David J. Pitcairn and Gayle E. Pitcairn for their support and input on various aspects of this study.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.
Ethical standards
No ethical approval was required for this analysis. The dataset is publicly available.
Availability of data and materials
The PNS 2019 dataset can be obtained from the following web address: https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?=&t=downloads.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S204579602100055X.
click here to view supplementary material
References
- Abdi F, Rahnemaei FA, Shojaei P, Afsahi F and Mahmoodi Z (2021) Social determinants of mental health of women living in slum: a systematic review. Obstetrics & Gynecology Science 64, 143–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Althubaiti A (2016) Information bias in health research: definition, pitfalls, and adjustment methods. Journal of Multidisciplinary Healthcare 9, 211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade LH, Wang Y, Andreoni S, Silveira CM, Alexandrino-Silva C, Siu ER, Nishimura R, Anthony JC, Gattaz WF, Kessler RC and Viana MC (2012) Mental disorders in megacities: findings from the São Paulo megacity mental health survey, Brazil. PLoS One 7, e31879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araya R, Zitko P, Markkula N, Rai D and Jones K (2018) Determinants of access to health care for depression in 49 countries: a multilevel analysis. Journal of Affective Disorders 234, 80–88. [DOI] [PubMed] [Google Scholar]
- Barros MBDA, Lima MG, Azevedo RCSD, Medina LBDP, Lopes CDS, Menezes PR and Malta DC (2017) Depression and health behaviors in Brazilian adults – PNS 2013. Revista de Saúde Pública 51(suppl 1), 8s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastos ML, Menzies D, Hone T, Dehghani K and Trajman A (2017) The impact of the Brazilian family health strategy on selected primary care sensitive conditions: a systematic review. PLoS One 12, e0182336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I and Seeman TE (2000) From social integration to health: Durkheim in the new millennium. Social Science & Medicine 51, 843–857. [DOI] [PubMed] [Google Scholar]
- Boccolini CS and de Souza Junior PR (2016) Inequities in healthcare utilization: results of the Brazilian National Health Survey, 2013. International Journal for Equity in Health 15, 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenes GA (2007) Anxiety, depression, and quality of life in primary care patients. Primary Care Companion to the Journal of Clinical Psychiatry 9, 437–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buigut S, Ettarh R and Amendah DD (2015) Catastrophic health expenditure and its determinants in Kenya slum communities. International Journal for Equity in Health 14, 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung KCK and Chou K (2019) Poverty, deprivation, and depressive symptoms among older adults in Hong Kong. Aging & Mental Health 23, 22–29. [DOI] [PubMed] [Google Scholar]
- Chung RY, Marmot M, Mak JK, Gordon D, Chan D, Chung GK, Wong H and Wong SYS (2020) Deprivation is associated with anxiety and stress. A population-based longitudinal household survey among Chinese adults in Hong Kong. Journal of Epidemiology and Community Health 75, 335–342. [DOI] [PubMed] [Google Scholar]
- Corrêa ML, Carpena MX, Meucci RD and Neiva-Silva L (2020) Depression in the elderly of a rural region in southern Brazil. Ciencia & Saude Coletiva 25, 2083–2092. [DOI] [PubMed] [Google Scholar]
- Courtin E and Avendano M (2016) Under one roof: the effect of co-residing with adult children on depression in later life. Social Science & Medicine (1982) 168, 140–149. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Fechner-Bates S and Schwenk TL (1994) Prevalence, nature, and comorbidity of depressive disorders in primary care. General Hospital Psychiatry 16, 267–276. [DOI] [PubMed] [Google Scholar]
- Ezeh A, Oyebode O, Satterthwaite D, Chen Y, Ndugwa R, Sartori J, Mberu B, Melendez-Torres GJ, Haregu T, Watson SI, Caiaffa W, Capon A and Lilford RJ (2017) The history, geography, and sociology of slums and the health problems of people who live in slums. Lancet (London, England) 389, 547–558. [DOI] [PubMed] [Google Scholar]
- Farid D, Li P, Da Costa D, Afif W, Szabo J, Dasgupta K and Rahme E (2020) Undiagnosed depression, persistent depressive symptoms and seeking mental health care: analysis of immigrant and non-immigrant participants of the Canadian longitudinal study of aging. Epidemiology and Psychiatric Sciences 29, e158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari AJ, Somerville AJ, Baxter AJ, Norman R, Patten SB, Vos T and Whiteford HA (2013) Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psychological Medicine 43, 471–481. [DOI] [PubMed] [Google Scholar]
- Ford DE and Erlinger TP (2004) Depression and C-reactive protein in US adults: data from the third national health and nutrition examination survey. Archives of Internal Medicine 164, 1010–1014. [DOI] [PubMed] [Google Scholar]
- Fraguas R, Henriques SG, De Lucia MS, Iosifescu DV, Schwartz FH, Rossi Menezes P, Farid Gattaz W and Arruda Martins M (2006) The detection of depression in medical setting: a study with PRIME-MD. Journal of Affective Disorders 91, 11–17. [DOI] [PubMed] [Google Scholar]
- Global Burden of Disease Collaborative Network (2020) GBD Results Tool – Global Burden of Disease Study 2019 (GBD 2019) Results. Available at http://ghdx.healthdata.org/gbd-results-tool (Accessed 7 February 2021).
- Greif MJ and Nii-Amoo Dodoo F (2015) How community physical, structural, and social stressors relate to mental health in the urban slums of Accra, Ghana. Health & Place 33, 57–66. Available at https://www.sciencedirect.com/science/article/pii/S1353829215000167. [DOI] [PubMed] [Google Scholar]
- Hacker KP, Seto KC, Costa F, Corburn J, Reis MG, Ko AI and Diuk-Wasser MA (2013) Urban slum structure: integrating socioeconomic and land cover data to model slum evolution in Salvador, Brazil. International Journal of Health Geographics 12, 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández-Vásquez A, Vargas-Fernández R, Bendezu-Quispe G and Grendas LN (2020) Depression in the Peruvian population and its associated factors: analysis of a national health survey. Journal of Affective Disorders 273, 291–297. [DOI] [PubMed] [Google Scholar]
- Hone T, Saraceni V, Medina Coeli C, Trajman A, Rasella D, Millett C and Durovni B (2020) Primary healthcare expansion and mortality in Brazil's urban poor: a cohort analysis of 1.2 million adults. PLoS Medicine 17, e1003357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James G, Witten D, Hastie T and Tibshirani R (2013) Linear regression. In Anonymous (ed.), An Introduction to Statistical Learning. (e-book). New York, NY: Springer, pp. 59–126. Available at https://link.springer.com/chapter/10.1007/978-1-4614-7138-7_3 (Accessed 1 April 2021). [Google Scholar]
- Jankowska MM, Weeks JR and Engstrom R (2012) Do the most vulnerable people live in the worst slums? A spatial analysis of Accra, Ghana. Annals of GIS 17, 221–235. [PMC free article] [PubMed] [Google Scholar]
- Kang H, Kim S, Bae K, Kim S, Shin I, Yoon J and Kim J (2015) Comorbidity of depression with physical disorders: research and clinical implications. Chonnam Medical Journal 51, 8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL and Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lever-van Milligen BA, Lamers F, Smit JH and Penninx BWJH (2017) Six-year trajectory of objective physical function in persons with depressive and anxiety disorders. Depression and Anxiety 34, 188–197. [DOI] [PubMed] [Google Scholar]
- Levis B, Benedetti A and Thombs BD (2019) Accuracy of patient health questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ (Clinical Research Ed.) 365, l1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilford RJ, Oyebode O, Satterthwaite D, Melendez-Torres GJ, Chen Y, Mberu B, Watson SI, Sartori J, Ndugwa R, Caiaffa W, Haregu T, Capon A, Saith R and Ezeh A (2017) Improving the health and welfare of people who live in slums. Lancet (London, England) 389, 559–570. [DOI] [PubMed] [Google Scholar]
- Lilford R, Kyobutungi C, Ndugwa R, Sartori J, Watson SI, Sliuzas R, Kuffer M, Hofer T, Albuquerque JPD and Ezeh A (2019) Because space matters: conceptual framework to help distinguish slum from non-slum urban areas. BMJ Global Health 4, e001267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q, He H, Yang J, Feng X, Zhao F and Lyu J (2020) Changes in the global burden of depression from 1990 to 2017: findings from the global burden of disease study. Journal of Psychiatric Research 126, 134–140. [DOI] [PubMed] [Google Scholar]
- Lorant V, Croux C, Weich S, Deliège D, Mackenbach J and Ansseau M (2007) Depression and socio-economic risk factors: 7-year longitudinal population study. The British Journal of Psychiatry: The Journal of Mental Science 190, 293–298. [DOI] [PubMed] [Google Scholar]
- Lotfaliany M, Bowe SJ, Kowal P, Orellana L, Berk M and Mohebbi M (2018) Depression and chronic diseases: co-occurrence and communality of risk factors. Journal of Affective Disorders 241, 461–468. [DOI] [PubMed] [Google Scholar]
- Lund C, Tomlinson M, De Silva M, Fekadu A, Shidhaye R, Jordans M, Petersen I, Bhana A, Kigozi F, Prince M, Thornicroft G, Hanlon C, Kakuma R, McDaid D, Saxena S, Chisholm D, Raja S, Kippen-Wood S, Honikman S, Fairall L and Patel V (2012) PRIME: a programme to reduce the treatment gap for mental disorders in five low- and middle-income countries. PLoS Medicine 9, e1001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macinko J and Harris MJ (2015) Brazil's family health strategy – delivering community-based primary care in a universal health system. The New England Journal of Medicine 372, 2177–2181. [DOI] [PubMed] [Google Scholar]
- Mahabir R, Croitoru A, Crooks A, Agouris P and Stefanidis A (2018) A critical review of high and very high-resolution remote sensing approaches for detecting and mapping slums: trends, challenges and emerging opportunities. Urban Science 2, 8. [Google Scholar]
- Manea L, Gilbody S and McMillan D (2012) Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): a meta-analysis. CMAJ: Canadian Medical Association Journal = Journal De L'Association Medicale Canadienne 184, 191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matijasevich A, Victora CG, Barros AJD, Santos IS, Marco PL, Albernaz EP and Barros FC (2008) Widening ethnic disparities in infant mortality in southern Brazil: comparison of 3 birth cohorts. American Journal of Public Health 98, 692–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V and Ustun B (2007) Depression, chronic diseases, and decrements in health: results from the world health surveys. Lancet (London, England) 370, 851–858. [DOI] [PubMed] [Google Scholar]
- Niessen LW, Mohan D, Akuoku JK, Mirelman AJ, Ahmed S, Koehlmoos TP, Trujillo A, Khan J and Peters DH (2018) Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the sustainable development agenda. Lancet (London, England) 391, 2036–2046. [DOI] [PubMed] [Google Scholar]
- Nolan LB, Bloom DE and Subbaraman R (2018) Legal status and deprivation in urban slums over two decades. Economic and Political Weekly 53, 47–55. Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6003417/ (Accessed 4 May 2021). [PMC free article] [PubMed] [Google Scholar]
- Oliveira EXGD, Pinheiro RS, Melo ECP and Carvalho MS (2011) Socioeconomic and geographic constraints to access mammography in Brasil, 2003–2008. Ciência & Saúde Coletiva 16, 3649–3664. [DOI] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development (2021) Real Minimum Wages. Available at https://stats.oecd.org/index.aspx?DataSetCode=RMW (Accessed 3 August 2021).
- Paim J, Travassos C, Almeida C, Bahia L and Macinko J (2011) The Brazilian health system: history, advances, and challenges. Lancet (London, England) 377, 1778–1797. [DOI] [PubMed] [Google Scholar]
- Patel V, Garrison P, de Jesus Mari J, Minas H, Prince M and Saxena S (2008) The Lancet's series on global mental health: 1 year on. Lancet (London, England) 372, 1354–1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patten SB, Williams JVA, Lavorato DH, Modgill G, Jetté N and Eliasziw M (2008) Major depression as a risk factor for chronic disease incidence: longitudinal analyses in a general population cohort. General Hospital Psychiatry 30, 407–413. [DOI] [PubMed] [Google Scholar]
- Perry J and Craig TKJ (2015) Homelessness and mental health. Trends in Urology & Men's Health 6, 19–21. [Google Scholar]
- Pinto LF and Giovanella L (2018) The family health strategy: expanding access and reducing hospitalizations due to ambulatory care sensitive conditions (ACSC). Ciencia & Saude Coletiva 23, 1903–1914. [DOI] [PubMed] [Google Scholar]
- Rabbani A, Biju NR, Rizwan A and Sarker M (2018) Social network analysis of psychological morbidity in an urban slum of Bangladesh: a cross-sectional study based on a community census. BMJ Open 8, e020180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rai D, Zitko P, Jones K, Lynch J and Araya R (2013) Country- and individual-level socioeconomic determinants of depression: multilevel cross-national comparison. The British Journal of Psychiatry: The Journal of Mental Science 202, 195–203. [DOI] [PubMed] [Google Scholar]
- Rathod S, Pinninti N, Irfan M, Gorczynski P, Rathod P, Gega L and Naeem F (2017) Mental health service provision in low- and middle-income countries. Health Services Insights 10, 1178632917694350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice J and Rice JS (2009) The concentration of disadvantage and the rise of an urban penalty: urban slum prevalence and the social production of health inequalities in the developing countries. International Journal of Health Services: Planning, Administration, Evaluation 39, 749–770. [DOI] [PubMed] [Google Scholar]
- Santos IS, Tavares BF, Munhoz TN, Almeida, LSPD, Silva NTBD, Tams BD, Patella AM and Matijasevich A (2013) Sensibilidade e especificidade do Patient Health Questionnaire-9 (PHQ-9) entre adultos da população geral. Cadernos de Saúde Pública. 29, 1533–1543. [DOI] [PubMed] [Google Scholar]
- Silverstein M, Cong Z and Li S (2006) Intergenerational transfers and living arrangements of older people in rural China: consequences for psychological well-being. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 61, 256. [DOI] [PubMed] [Google Scholar]
- Snyder RE, Jaimes G, Riley LW, Faerstein E and Corburn J (2014) A comparison of social and spatial determinants of health between formal and informal settlements in a large metropolitan setting in Brazil. Journal of Urban Health: Bulletin of the New York Academy of Medicine 91, 432–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soares S and de Oliveira WF (2016) The matrix approach to mental health care: Experiences in Florianopolis, Brazil. Journal of Health Psychology 21, 336–345. [DOI] [PubMed] [Google Scholar]
- Souza Lopes C, Hellwig N, Silva E, de Azevedo G and Menezes PR (2016) Inequities in access to depression treatment: results of the Brazilian national health survey – PNS. International Journal for Equity in Health 15, 154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza Lopes C, Lopes Gomes N, Leite Junger W and Rossi Menezes P (2021) Trend in the prevalence of depression and correlates in Brazil: results from the national health surveys 2013 and 2019. SciELO Preprints. Available at https://preprints.scielo.org/index.php/scielo/preprint/view/2388/4070. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K and Williams JB (1999) Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient Health Questionnaire. JAMA 282, 1737–1744. [DOI] [PubMed] [Google Scholar]
- Stopa SR, Malta DC, de Oliveira MM, Lopes CDS, Menezes PR and Kinoshita RT (2015) Prevalence of self-reported depression in Brazil: 2013 national health survey results. Revista Brasileira de Epidemiologia = Brazilian Journal of Epidemiology 18(Suppl 2), 170–180. [DOI] [PubMed] [Google Scholar]
- Stopa SR, Szwarcwald CL, Oliveira MMD, Gouvea EDCDP, Vieira MLFP, Freitas MPSD, Sardinha LMV and Macário EM (2020) National health survey 2019: history, methods and perspectives. Epidemiologia e Servicos de Saude: Revista do Sistema Unico de Saude do Brasil 29, e2020315. [DOI] [PubMed] [Google Scholar]
- Ströhle A (2009) Physical activity, exercise, depression and anxiety disorders. Journal of Neural Transmission (Vienna, Austria: 1996) 116, 777–784. [DOI] [PubMed] [Google Scholar]
- Subbaraman R, Sood K, Nolan L, Shitole T, Sawant K, Shitole S, Nanarkar M, Ghannam J, Betancourt TS, Bloom DE and Patil-Deshmukh A (2014) The psychological toll of slum living in Mumbai, India: a mixed methods study. Social Science & Medicine 119, 155–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szwarcwald CL, da Mota JC, Damacena GN and Pereira TGS (2011) Health inequalities in Rio de Janeiro, Brazil: lower healthy life expectancy in socioeconomically disadvantaged areas. American Journal of Public Health 101, 517–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tampubolon G and Maharani A (2017) When did old age stop being depressing? Depression trajectories of older Americans and Britons 2002–2012. The American Journal of Geriatric Psychiatry 25, 1187–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank (2018) Population living in slums (% of urban population) – Brazil. Available at https://data.worldbank.org/indicator/EN.POP.SLUM.UR.ZS?locations=BR (Accessed 9 February 2021).
- UN-Habitat (2015) Slum Almanac 2015/2016: Tracking Improvement in the Lives of Slum Dwellers. Nairobi, Kenya: UN-Habitat. Available at https://unhabitat.org/slum-almanac-2015-2016-0. [Google Scholar]
- United Nations Development Programme (2021) Sustainable Development Goals. Available at https://www.undp.org/sustainable-development-goals (Accessed 9 August 2021).
- Williams R (2006) Generalized ordered logit/partial proportional odds models for ordinal dependent variables. Stata Journal 6, 58–82. Available at https://www.stata-journal.com/article.html?article=st0097. [Google Scholar]
- Wittayanukorn S, Qian J and Hansen RA (2014) Prevalence of depressive symptoms and predictors of treatment among U.S. adults from 2005 to 2010. General Hospital Psychiatry 36, 330–336. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2019) The WHO Special Initiative for Mental Health (2019–2023): Universal Health Coverage for Mental Health. Geneva, Switzerland: World Health Organization. Available at https://apps.who.int/iris/handle/10665/310981. [Google Scholar]
- Yamabe K, Liebert R, Flores N and Pashos CL (2019) Health-related quality of life outcomes, economic burden, and associated costs among diagnosed and undiagnosed depression patients in Japan. ClinicoEconomics and Outcomes Research: CEOR 11, 233–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zivin K, Llewellyn DJ, Lang IA, Vijan S, Kabeto MU, Miller EM and Langa KM (2010) Depression Among older adults in the United States and England. The American Journal of Geriatric Psychiatry 18, 1036–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S204579602100055X.
click here to view supplementary material
Data Availability Statement
The PNS 2019 dataset can be obtained from the following web address: https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?=&t=downloads.