Abstract
Among all contaminants of emerging interest, drugs are the ones that give rise to the greatest concern. Any of the multiple stages of the drug's life cycle (production, consumption and waste management) is a possible entry point to the different environmental matrices. Psychiatric drugs have received special attention because of two reasons. First, their use is increasing. Second, many of them act on phylogenetically highly conserved neuroendocrine systems, so they have the potential to affect many non-target organisms. Currently, wastewater is considered the most important source of drugs to the environment. Furthermore, the currently available wastewater treatment plants are not specifically prepared to remove drugs, so they reach practically all environmental matrices, even tap water. As drugs are designed to produce pharmacological effects at low concentrations, they are capable of producing ecotoxicological effects on microorganisms, flora and fauna, even on human health. It has also been observed that certain antidepressants and antipsychotics can bioaccumulate along the food chain. Drug pollution is a complicated and diffuse problem characterized by scientific uncertainties, a large number of stakeholders with different values and interests, and enormous complexity. Possible solutions consist on acting at source, using medicines more rationally, eco-prescribing or prescribing greener drugs, designing pharmaceuticals that are more readily biodegraded, educating both health professionals and citizens, and improving coordination and collaboration between environmental and healthcare sciences. Besides, end of pipe measures like improving or developing new purification systems (biological, physical, chemical, combination) that eliminate these residues efficiently and at a sustainable cost should be a priority. Here, we describe and discuss the main aspects of drug pollution, highlighting the specific issues of psychiatric drugs.
Keywords: Antipsychotics, Pharmaceuticals in the environment, Drug pollution, Antidepressants, Wastewater, Ecotoxicity
Core Tip: Psychiatric drugs have received special attention as contaminants of emerging interest because of two reasons: First, their use is increasing. Second, many act on phylogenetically conserved neuroendocrine systems, potentially affecting many non-target organisms. Drug pollution is a complicated problem involving many stakeholders with different values and interests. Solutions can be applied at source, using medicines more rationally, prescribing greener drugs or designing pharmaceuticals that are more biodegradable. Besides, end of pipe measures, e.g., developing new purification systems will also be crucial. Finally, educating both health professionals and citizens, and collaboration between environmental and healthcare sciences is going to be essential.
INTRODUCTION
Toxic problems caused by chemicals, such as aromatic compounds, polychlorinated biphenyls, heavy metals, pesticides, etc., are well known. However, concern regarding the so-called “pollutants of emerging interest” is increasing, with pharmaceuticals causing the greatest concern. Pharmaceutical products have two important characteristics that are driving this preoccupation: Firstly, they produce pharmacological effects at low concentrations, such as those found in the environment. Secondly, they are designed with stability in mind, so they are more likely to reach and interact with their target molecules.
THE PROBLEM OF ENVIRONMENTAL POLLUTION WITH PHARMACEUTI-CALS
Publications in scientific journals regarding the presence of pharmaceutical products in the environment has grown exponentially since the end of the 1990s, due to improvements in analytical techniques allowing for the detection of lower concentrations of drugs in different matrices[1]. Currently available information regarding the presence of pharmaceuticals in the environment and their consequences is simply overwhelming.
A recent study estimated that approximately 4000 different pharmacologically active substances are currently being administered globally, including: Prescription drugs for human use, over-the-counter drugs, and veterinary drugs[2]. Global drug use continues to grow, with an estimate of 4.5 trillion doses consumed in 2020[3]. The trend will probably continue for the following reasons[2]: The age and life expectancy of populations has increased; economies are growing, especially emerging economies, so the capacity and expectations to treat aging and chronic diseases increase; intensification of livestock and aquaculture practices to meet demand; the design of new pharmaceutical products; climate change, which will aggravate existing diseases (both communicable and non-communicable).
Psychiatric drugs have received particular attention above other therapeutic classes for two main reasons: Their widespread use and their potential to provoke ecotoxicological damage. Some authors believe the current situation due to the Coronavirus disease 2019 pandemic may lead to an increase use of certain psychiatric drugs, like anxiolytics or antidepressants[4].
Life cycle of drugs
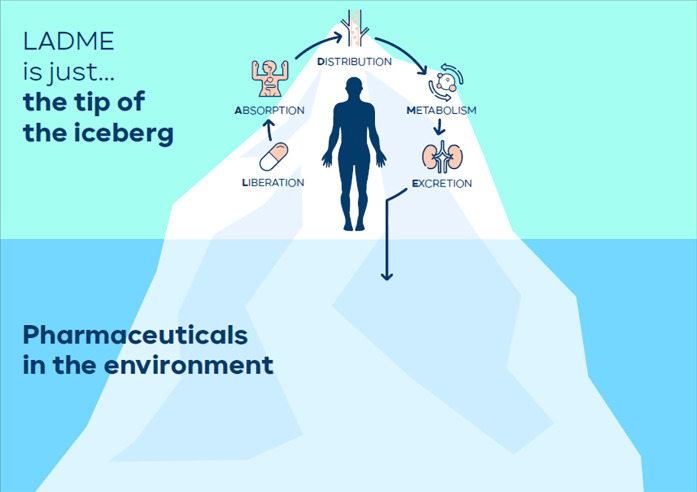
The liberation, absorption, distribution, metabolism, excretion (LADME) scheme showing the curse of drugs in the human organism is still shown in universities across the world. Drugs are first released, then absorbed, distributed, metabolized, and finally excreted outside. But in this anthropocentric scheme, little or no attention is paid to drugs and metabolites once they are excreted outside the organism (Figure 1).
Figure 1.
The liberation, absorption, distribution, metabolism, excretion scheme is just the tip of the iceberg. LADME: Liberation, absorption, distribution, metabolism, excretion.
Of course, drugs and their metabolites do not disappear after flushing the toilet, but rather reach the environment in different amounts depending on the proportion metabolized in the body. It has been estimated that the percentage of unchanged drug excreted in feces and urine is between 30% and 90% on average[5].
Any of the multiple stages that make up the life cycle of the drug: production, consumption and waste management; is a possible entry point to the different environmental matrices.
In any case, currently the most important source is considered to be wastewater, which includes wastewater of domestic, hospital, industrial and of agricultural or livestock origin. Pollution due to industrial waste disposal was not considered a major factor until recently. Contemporary research shows, however, that certain production factories can cause environmental pollution at levels well above what was previously thought[6]. For example, very high venlafaxine concentrations were found in a wastewater treatment plant (WWTP) that received the discharge of a large industrial plant near Jerusalem, in Israel[7].
But pharmaceutical products can reach the aquatic environment by other routes, including, for example: aquaculture, runoff water from the agricultural sector, through the removal of sewage sludge (especially when used as fertilizer in agriculture), or leaching to groundwater after rain. Likewise, the presence of pharmaceuticals has to be considered when re-using wastewater in agriculture, a practice that is expected to increase in the near future[8].
The current purification systems: WWTPs
Currently available WWTPs are not specifically designed to remove drugs. Some of them are eliminated, but others remain unchanged and are discharged with the effluents. As an example, a study carried out in the United Kingdom in 2018 estimated that in 13% of the WWTPs available in that country, the effluent contained potentially dangerous concentrations of drugs such as ethynylestradiol, diclofenac, propranolol, macrolide antibiotics and fluoxetine[9]. Sometimes, paradoxically, the drug concentration in the effluent of the WWTP can be even higher than that in the influent. This is due to the microorganisms in charge of the biological (secondary) treatment of wastewater may be in charge of metabolizing the conjugates with glucuronic acid, so that the drug returns to its original form[5]. This is the case with carbamazepine, amitriptyline, lamotrigine, doxepine, citalopram, among many other pharmaceuticals[10]. Besides, a study estimated that up to 70% of all wastewater does not receive treatment before being discharged, so the situation in developing countries is probably even worse[11,12].
Presence of drugs in environmental matrices
Residues of multiple types of drugs (about 700) have been detected in different environmental compartments mainly in wastewater, surface and groundwater, but also in soil, air and biota, even in the tap water that we drink[13]. In the specific case of psychiatric drugs, there are complete books reviewing their presence in the environment[14]. Carbamazepine has even been considered as a marker for wastewater influenced water bodies due to its omnipresence[15].
For a greater detail of all the drugs detected in any environmental matrix, the free database of the German Environment Agency can be consulted, which maintains an exhaustive registry of all published studies, available from: https://www.umweltbundesamt.de/dokument/database-pharmaceuticals-in-the-environment-excel.
Furthermore, once they have reached the environment, parent drugs (or metabolites) continue to transform and continue to undergo complex metabolic processes by different organisms as well as by different physicochemical mechanisms (photo-degradation, adsorption to solids, etc.), leading to “transformation compounds”. For example, Trawiński et al[16] reviewed the photodegradation process of psychotropic drugs. Some substances can remain unchanged in the environment for decades, i.e., are very persistent. This is the case of oxazepam, which has remained unchanged at the bottom of Swedish lakes for more than 30 years[17].
Ecotoxicological effects of psychiatric drugs
Toxic effects of drugs in the environment can go far beyond growth, mortality or reproduction. For example, psychoactive drugs can affect organism behaviour and fitness, altering population dynamics[18-21]. The therapeutic targets and the physiological systems in which drugs act are not exclusive to human beings. Many of these structures and signaling pathways are highly conserved phylogenetically, and are present in many living organisms[22]. For example, multiple behavioral tests (such as anxiety, fear and stress) for experimental drugs intended for human use are performed on fish[23]. Fish share many of the neurotransmitter and signaling pathways with us. In fact, biogenic monoamines (serotonin, dopamine, norepinephrine, etc.) are found in vertebrates and invertebrates, including amphibians, fish, insects and echinoderms[24,25]. These substances are so ancient from an evolutionary point of view that they are present in organisms outside the animal kingdom. For example, acetylcholine is present in fungi and bacteria[26] and serotonin in plants[27]. Fluoxetine has shown to induce behavioral changes in crickets[28]. Fish also become constipated in the presence of the antipsychotic clozapine[29], plants accumulate benzodiazepines that could act on their GABAergic system[30], or sertraline affects sedimentary nitrification processes by altering the microbial trophic chain[31].
Castillo-Zacarías et al[32] have recently reviewed available literature about the presence and effects of antidepressants on the environment. We have also shown that the role of antipsychotic drugs as environmental pollutants has probably been underrated so far[33].
In short, the psychoactive drugs that we use and excrete into the environment can have pharmacological effects in different non-target organisms. However, the extent of exposure and subsequent effects remains unknown for many taxa and ecosystems[34] (Table 1).
Table 1.
Examples of the presence of certain psychiatric drugs in the environment and ecotoxicological effects on organisms
|
Therapeutic class
|
Drug
|
Non-target organism
|
Ecotoxicological effects
|
Ref.
|
| Antiepileptics | Carbamazepine | Ryegrass (Lolium perenne) | Accumulation in plants tissues | Carter et al[83], 2014 |
| Antidepressants | Various | Platypus (Ornithorhynchus anatinus), Brown Trout (Salmo trutta) | Half of human daily dose, insectivorous diet. Effects? | Richmond et al[41], 2018 |
| Sertraline | River sediment microorganisms | Sedimentary nitrification processes by altering the microbial trophic chain | Li et al[31], 2020 | |
| Fluoxetine | Cricket (Gryllus campestris) | Behaviour disturbance | Abey-Lee et al[28], 2018 | |
| Starling (Sturnus vulgaris) | Reduced female attractiveness | Whitlock et al[84], 2018 | ||
| Benzodiazepines | Various | Beet (Beta vulgaris) | Phitotoxicity | Carter et al[30], 2018 |
| Oxazepam | European perch (Perca fluviatilis) | Behaviour and feeding rate disturbance | Brodin et al[85], 2013 | |
| Antipsychotics | Clozapine | Zebra fish (Danio rerio) | Constipation | de Alvarenga et al[29], 2017 |
| Risperidone | Zebra fish (Danio rerio) | Alteration of antipredatory behavior, transgenerational effect | Kalichak et al[86], 2019 | |
| Various | Chub (Squalius cephalus) | Fish plasma concentrations > Human plasma therapeutic concentrations | Cerveny et al[42], 2020 |
Effects of drug pollution on human health
The effect of drug pollution on human health is still relatively little studied. A WHO report published in 2012 concluded that drug concentrations in tap water should not pose any health problems[35]. These findings were confirmed in a recent study carried out in China[36]. However, the presence of drugs in the environment could be a problem for the most vulnerable groups of patients (e.g., allergic[5]). Although there is no evidence of short-term effects on human health, uncertainties remain, in particular concerning long-term exposure (chronic exposure) to a mixture of pollutants[5]. The possible routes of exposure are, mainly, consumption of drinking water, vegetables and tubers, meat, fish, shellfish and dairy products[5].
Probably the best known example of the deleterious effect of drug pollution on human health is that of the increase in bacteria with resistance to antibiotics, which is currently recognized as the biggest public health problem worldwide. In this sense, we consider that the “One Health” approach or philosophy, which considers that human health is closely interrelated with environmental health, is essential[37]. Nevertheless, we believe that it is necessary to extend this approach to all therapeutic groups including psychiatric drugs, not only antibiotics[38,39].
Some authors have suggested that psychoactive drugs present in the environment may potentially be associated with human neuropsychiatric disorders such as autism, Alzheimer’s disease and schizophrenia, since they are able to cross the maternal barriers affecting the development of the embryonic brain[40].
Bioaccumulation
Recent studies suggest that certain drugs bioaccumulate in non-target organisms through the food web, reaching tissue concentrations much higher than those found in the environment. For example, a study carried out in five Australian rivers found that platypuses and brown trouts bioaccumulate 66 of the 80 drugs studied due to their insectivorous diet. First, the larvae of riparian insect’s bioaccumulated certain drugs present in surface waters, and subsequently, these drugs can pass to the animals that eat them. Surprisingly, the researchers estimated that, in the case of antidepressants, platypus might be exposed to amounts up to half the daily doses used in humans[41]. (Table 1).
A recent work studied the presence of more than 90 drugs pertaining to 23 different drug classes in blood plasma of wild European fish in three different European countries. For some drugs, measured fish plasma concentrations were above human therapeutic plasma concentrations. Indeed, three of the four drugs that showed a moderate or a high risk of inducing toxic effects on fish were antipsychotics: i.e., risperidone, flupentixol and haloperidol[42].
An excellent review of the bioaccumulation of pharmaceuticals (including psychiatric drugs) in aquatic fish and invertebrates was published by Miller et al[43]. Besides, this bioaccumulation process is not exclusively restricted to the aquatic environment. A study carried out in the Doñana National Park, Spain, showed that dung beetles accumulate the antiparasitic ivermectin used in livestock in their tissues. Ivermectin, with recognized insecticidal activity, is toxic to beetles that are in charge of processing manure, in such a way that the properties of the soil are altered[44]. In addition, some studies suggest certain psychiatric drugs like carbamazepine and fluoxetine might bioaccumulate in terrestrial organisms (earthworms) depending on the properties of the soil and the physico-chemical characteristics of the drug[45].
We still understand little about what is happening ... although highly hypothetical, what if insectivorous bats were accumulating drugs in their tissues? What consequences could this have on the appearance of new zoonosis[46]?
Environmental impact risk reports from the European Medicines Agency
Since October 2005, the European Medicines Agency has required the laboratories holding the marketing authorization to assess the environmental impact of medicines[47] (ERA: Environmental risk assessment). Despite this significant progress, this report is not considered during the benefit-risk balance in drug evaluation, even if it shows potential risks for the environment. For example, the ERA of the recently marketed antidepressant vortioxetine[48] recognizes that this drug is “potentially harmful to the environment”. Something similar occurs with the antipsychotic asenapine[49], for which the ERA recognizes that it is a potential endocrine disruptor. Despite this, both drugs have been marketed without any restrictions.
At the moment, and contrary to what happens for certain medicinal products for veterinary use, the environmental impact is not taken into account in the benefit/risk balance of the evaluation of medicinal products for human use, which is based solely on criteria of efficacy and safety. We believe that this may change in the future, as we gain knowledge on the environmental risks of medicines[38]. In addition, another aspect to consider is that all drugs marketed before that date (October 30, 2005) are exempt from submitting this environmental impact report in the renewal of their marketing authorization, so the information available about many of the drugs currently used is scarce or non-existent. For some drugs, such as fluoxetine, an ERA is published many decades after its authorization[50]. Another aspect is that current ecotoxicological tests demanded by the EMA do not include behavioral tests. Some authors propose updating the demanded tests in order to incorporate these kind of ecotoxicological tests[21]. Currently, the regulation of ERAs for medicines for human use is under review. It seems that some changes will occur, specifically in terms of bioaccumulation and fundamentally endocrine disruptors[51]. However, the legislation involved in Europe is varied, abundant, complex and not always easy to understand by non-experts in the field[52]. Another important issue is that legislation differs between countries, or is, directly, non-existent[53]. On the other hand, there are veterinary drugs used in pets, for which the environmental impact assessment is not considered in the benefit/risk balance either. There are authors who consider that this should change, taking into account the toxicity of some of the substances used and the increasing number of pets in our environment[54,55].
POSSIBLE SOLUTIONS
The study of the problem of drug pollution is among the priority lines of research of the main organizations dedicated to the protection of public and environmental health, such as the WHO and the European Commission. In this regard, it is worth highlighting the publication of the “Strategic approach of the European Union in the field of pharmaceutical products in the environment” by the European authorities, probably the front-runners in the field[56].
The contamination of the environment with pharmaceutical products is a complicated and diffuse problem that entails scientific uncertainties, a large number of stakeholders with different values and interests, and great complexity. This is probably why the Dutch government has classified it as a “wicked problem” (a problem that is difficult or impossible to solve given that it presents incomplete, contradictory and changing requirements that are generally difficult to recognize). In their comprehensive strategy to face the problem, they have established that all agents involved in the complex life cycle of the drug should participate in the solution[57].
It is more than likely that in the future, as the detection of drugs and ecotoxicological studies progress, many drugs will end up being a priority in legislative matters, and that maximum concentration of certain drugs in wastewater may be established. We believe that we are on the verge of a revolution in the field of psychopharmacology[38].
At source measures
Before trying to improve the elimination processes of drugs once they reach the WWTP and the environment, it is probably reasonable to act at source. Considering that drugs have offered, and continue to offer, an unquestionable benefit to the health of humanity, great care must be taken not to restrict access to those drugs that are necessary. Here are some ideas that could help improve the problem.
Rational use of the drug, eco-prescription, or "green prescription"
The “Rational use of medicines” is a term coined by WHO experts more than 30 years ago, in 1985[58]. To date, the rational use of medicine has been defined as “patients receive the appropriate medication for their clinical needs, in the doses corresponding to their individual requirements, for an adequate period of time and at the lowest possible cost for them and for the community”. This term has served as a conceptual framework of undoubted value to promote actions and strategies that have improved the health of countless patients, avoiding excesses in the use of medications, polypharmacy, etc. However, we believe that the term requires an update, so that the "One Health´s philosophy, which tries to achieve optimal health for people, animals and our environment taking into account the existing interrelations, is considered[59]. Currently this philosophy is already applied, but fundamentally to antimicrobials. We believe that broadening the approach is necessary. Reducing the inappropriate consumption of drugs will reduce their entry into ecosystems, improving people's health and that of the environment[60].
Christian Daughton, head of the American Environment Agency, now retired, proposed more than 5 years ago the term “eco-prescription”, or “green prescription”. Ultimately, it means that the prescriber should consider the characteristics and environmental behavior of drugs when prescribing them[10]. This is definitely going to be challenging. For example, oxazepam (not available in some countries such as Spain, but a common metabolite of numerous benzodiazepines commonly used in our setting), is considered a good choice for the elderly due to its adequate pharmacokinetic profile, since it is not eliminated by oxidative metabolism and is excreted unchanged in urine. However, it is a known to cause of potential toxic effects in fish, and can accumulate for decades without biodegrading. From an environmental point of view, substances that are metabolized to inactive metabolites prior to elimination may be preferable[10]. We believe that incorporating environmental criteria in the use of medicines is essential, and it may become a true revolution in pharmacotherapeutics[38].
Another interesting classification of drugs is the one proposed by the Swedish Environmental Research Institute. It is one of the few available classifications of drugs according to their environmental characteristics. It is an initiative of the Stockholm City Council, driven by the pharmaceutical industry. Each drug receives three scores, each of which can take a value from 0 to 3: one on its persistence in the environment (P); another on bioaccumulation (B) and another on toxicity (T). The overall score is the sum of the points obtained for each item[61].
Prescribers may incorporate this information when using drugs in individual patients. The “Wise List” (Kloka Listan), is so far, the only multifaceted approach incorporating environmental aspects to recommend drugs in ambulatory care[62]. The chain approach of the Dutch Government also incorporates a “psychotropic task force” in order to reduce psychotropics in water[57]. We believe further research is urgently needed in this crucial area.
The design of more biodegradable and sustainable drug: “Green design”
An attractive idea for the future is to design greener and more biodegradable drugs; i: e: “benign by design” concept[63]. Although there are already some examples of the development of more "environmentally friendly" drugs, such as glufosfamide[64] and green drug delivery systems[65], no psychoactive drugs has been designed to be more biodegradable.
Furthermore, a holistic approach should be considered when evaluating the environmental impact of medicines, and other constituent parts of medicines ought to be taken into account apart from active pharmaceutical ingredients. We believe there is room for improvement in this specific area. For example, inhaled loxapine, a recently marketed antipsychotic for the treatment of agitation, requires a lithium battery for each dose administered. Another example would be Abilify Mycite®, in which an electronic circuit is excreted with each capsule administered[38].
Education
Until now, healthcare professionals who are in charge of prescribing, administering and dispensing drugs have paid little attention to the problem of drug contamination, which has been preferentially addressed by biologists, chemists and other professional profiles such as environmentalists. We firmly believe that this concern cannot be ignored anymore in the schools of Medicine, Pharmacy and Nursing[66]. Recent studies carried out in China have shown that awareness of the problem in both pharmacists[67] and prescribers[72] has a wide room for improvement. As proposed in the European Commission strategy[56], we believe that general education for both health professionals and citizens is a key element in the fight against drug pollution.
Improved waste management, responsible consumption
The incorrect management of pharmaceutical waste is one of the routes of entry of medicines into the environment. Studies indicate that up approximately 33% of patients do not use all the medicines dispensed, which generates a waste of health resources and possible environmental contamination[2]. The generalization of the adoption of refund schemes such as SIGRE, implemented in Spain, will be another key element. This is especially important in countries where waste management is not working well and where inappropriate drug disposal can be expected, such as regions form the Middle East, Asian and African countries[69]. Optimizing package sizes and extending drug expiration dates where possible will allow drugs that are still safe to use from being unnecessarily discarded. The idea of reusing drugs has also been proposed. In this regard, a survey conducted in the United Kingdom found that more than half of those surveyed would welcome the reuse of medicines in the future[70]. Although it is not legally accepted in many countries, it could help reduce the amount of unused medicine accumulation, a fact that can lead to overuse or incorrect use of medicines or also to incorrect disposal. However, obviously, considering security issues is mandatory if such policies are going to be implemented.
From a regulatory perspective, the European Parliament suggests that “eco-labeling” of pharmaceutical products with a high risk for the environment should be explored (Figure 2), as is already done with other products in the market[71].
Figure 2.
Will we see drugs with eco-label?
Legislation
As knowledge about the environmental impact of pharmaceuticals keeps mounting up, ERAs need to update accordingly to improve our capability of correctly assessing the risk posed. It is interesting to highlight that last year, venlafaxine and desvenlafaxine were considered as suitable for inclusion in the next “Watch List” (WL): under the European Union Water Framework Directive[72]. These antidepressants are the first psychoactive drugs ever to be included in such a list[73].
End of pipe measures
Apart from implementing at source measures, it is essential to address the problem of waste already generated. Taking into account the growing consumption of drugs at a global level, the research and development of new purification systems (biological, physico-chemical) that eliminate these residues efficiently and at a sustainable cost should be a priority.
Improvement of WWTPs
The design of purification systems requires prior knowledge of the physical-chemical characteristics of the effluent wastewater and of the concentration of the main eliminated drugs, especially those that represent a greater risk for the environment.
For example, in order to optimize costs, various authors propose eliminating drugs at the hospital wastewater effluent instead of treating the total amount of water reaching WWTPs, since hospitals are the main consumers of certain types of pharmaceuticals (some cytostatics, broad-spectrum antibiotics, iodine contrasts). There are already interesting initiatives such as the one implemented at the Herlev Hospital in Copenhagen, Denmark, where improved treatment of hospital wastewater is performed on-site to effectively remove all drugs before they reach the municipal WWTP[74].
Anther strategy is that carried out by Switzerland, a country in which all treatment plants from a certain size are going to be improved (through tertiary treatment with ozone and activated carbon) to effectively eliminate drugs and other emerging contaminants, at an approximate cost of 1 billion euros[75]. However, this strategy is probably not sustainable or applicable to most countries. On the other hand, ozonation can oxidize drugs producing new transformation products with poor known ecotoxicological effects[76].
New methods that improve the performance of WWTPs in the elimination of drugs continue to be studied and sought. A curious method is the use of xylophagous fungi (white rot fungi) of which the species most used to date is Trametes versicolor. These fungi, in charge of degrading soil organic matter in nature, possess enzymes, called “laccases” with the capacity to oxidize a wide spectrum of organic substances, including drugs[77].
Eco-pharmacovigilance, environmental pharmacovigilance
In the 1960s, the use of thalidomide was used for the treatment of nausea and vomiting in pregnant women. Later, the drug proved to be teratogenic, producing thousands of newborns malformations. This disaster gave rise to the modern pharmacovigilance systems currently in place. Since the ecological disaster produced by diclofenac in the Indian subcontinent, various authors have asked to create a new discipline, i.e., “Eco-pharmacovigilance” or “environmental pharmacovigilance”[78]. This discipline will dedicate to “monitor” the environmental impact of drugs[79]. Will be ever witness a market withdrawal of an antidepressant or an antipsychotic, or any other drug, because of environmental factors in the future? May be.
Phytoremediation
From the point of view of environmental drug contamination, the accumulation of drugs by plants can be harmful (in the case of agriculture) or beneficial, if done on purpose. Phytoremediation is a technology that uses plants and the associated microorganisms of the rhizosphere (zone of interaction between plant roots and soil microorganisms) to eliminate, transform or contain toxic chemicals located in soils, sediments, groundwater and surface waters, among others. Different species of plants have been used for the treatment or removal of a variety of pollutants such as oil, chlorinated solvents, pesticides, metals, radionuclides, explosives and pharmaceuticals[80]. The design of constructed wetlands, a technique than can be employed for the removal of pharmaceuticals from wastewater, has received particular attention[81]. It is interesting to verify that the detoxification mechanisms used by plants, are sometimes surprisingly similar to those of mammals, as in the case of glutathione conjugation of paracetamol in the Brassica juncea plant[82].
CONCLUSION
So far, the problem of drug pollution has been largely ignored by healthcare professionals and academics. However, if the problem is to be dealt with effectively, an interdisciplinary approach will be necessary, allowing integration of the knowledge of the different agents involved[38].
In conclusion, drug pollution with psychiatric drugs is a problem of emerging concern. This complex problem involves many stakeholders with different values and interests. Solutions can be implemented at source, before drugs reach the environment: using medicines more rationally, prescribing greener drugs, or designing pharmaceuticals that are more easily biodegradable. Besides, end of pipe measures, such as the development of new, sustainable purification systems will also be crucial. Finally, educating both health professionals and citizens, and collaboration between environmental and healthcare sciences is going to be essential.
ACKNOWLEDGEMENTS
The authors would like to thank A .Vitoria-Gasteiz and F.Vital for their support.
Footnotes
Conflict-of-interest statement: The authors declare no conflicts of interest.
Manuscript source: Invited manuscript
Peer-review started: February 23, 2021
First decision: June 18, 2021
Article in press: August 31, 2021
Specialty type: Psychiatry
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hosak L, Seeman MV S-Editor: Wu YXJ L-Editor: A P-Editor: Yu HG
Contributor Information
Julene Argaluza, Department of Epidemiology and Public Health, Bioaraba Health Research Institute, Vitoria-Gasteiz 01002, Spain.
Saioa Domingo-Echaburu, Department of Pharmacy, Alto Deba Integrated Health Care Organization, Arrasate 20500, Spain.
Gorka Orive, NanoBioCel Group, Laboratory of Pharmaceutics, School of Pharmacy, University of the Basque Country UPV/EHU, Paseo de la Universidad 7, Vitoria-Gasteiz 01006, Spain; Biomedical Research Networking Centre in Bioengineering, Biomaterials and Nanomedicine (CIBER-BBN), Vitoria-Gasteiz 01006, Spain; Bioaraba, NanoBioCel Research Group, Vitoria-Gasteiz 01006, Spain; Singapore Eye Research Institute, Discovery Tower, Singapore 168751, Singapore.
Juan Medrano, Department of Psychiatry, Biocruces Bizkaia Health Research Institute, Mental Health Network Research Group, Osakidetza, Portugalete 48920, Spain.
Rafael Hernandez, Department of Internal Medicine, Araba Mental Health Network, Vitoria-Gasteiz 01006, Spain.
Unax Lertxundi, Bioaraba Health Research Institute; Osakidetza Basque Health Service, Araba Mental Health Network, Araba Psychiatric Hospital, Pharmacy Service, Vitoria-Gasteiz 01006, Alava, Spain. unax.lertxundietxebarria@osakidetza.net.
References
- 1.Daughton CG. Pharmaceuticals and the Environment (PiE): Evolution and impact of the published literature revealed by bibliometric analysis. Sci Total Environ. 2016;562:391–426. doi: 10.1016/j.scitotenv.2016.03.109. [DOI] [PubMed] [Google Scholar]
- 2.Organisation for Economic Co-operation and Development (OECD) Pharmaceutical Residues in Freshwater Hazards and Policy Responses. [cited 8 October 2020]. Available from: https://www.oecd.org/publications/pharmaceutical-residues-in-freshwater-c936f42d-en.htm .
- 3.IMS institute. Global Medicines in 2020. [cited 8 October 2020]. Available from: https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/global-medicines-use-in-2020 .
- 4.The Guardian. Antidepressant drug use in UK. [cited January 4, 2021]. Available from: https://www.theguardian.com/society/2021/jan/01/covid-antidepressant-use-at-all-time-high-as-access-to-counselling-in-england-plunges .
- 5.BIO Intelligence Service. Study on the environmental risks of medicinal products. Final report prepared for Executive Agency for Health and Consumers. 2013. [cited 7 October 2020]. Available from: https://ec.europa.eu/health/sites/health/files/files/environment/study_environment.pdf .
- 6.Larsson DG. Pollution from drug manufacturing: review and perspectives. Philos Trans R Soc Lond B Biol Sci. 2014;369 doi: 10.1098/rstb.2013.0571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gasser G, Pankratov I, Elhanany S, Werner P, Gun J, Gelman F, Lev O. Field and laboratory studies of the fate and enantiomeric enrichment of venlafaxine and O-desmethylvenlafaxine under aerobic and anaerobic conditions. Chemosphere. 2012;88:98–105. doi: 10.1016/j.chemosphere.2012.02.074. [DOI] [PubMed] [Google Scholar]
- 8.Poustie A, Yang Y, Verburg P, Pagilla K, Hanigan D. Reclaimed wastewater as a viable water source for agricultural irrigation: A review of food crop growth inhibition and promotion in the context of environmental change. Sci Total Environ. 2020;739:139756. doi: 10.1016/j.scitotenv.2020.139756. [DOI] [PubMed] [Google Scholar]
- 9.Comber S, Gardner M, Sörme P, Leverett D, Ellor B. Active pharmaceutical ingredients entering the aquatic environment from wastewater treatment works: A cause for concern? Sci Total Environ. 2018;613-614:538–547. doi: 10.1016/j.scitotenv.2017.09.101. [DOI] [PubMed] [Google Scholar]
- 10.Daughton CG. Eco-directed sustainable prescribing: feasibility for reducing water contamination by drugs. Sci Total Environ. 2014;493:392–404. doi: 10.1016/j.scitotenv.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 11.United Nations. World Water Assessment Programme (UNESCO WWAP). [cited 7 October 2020]. Available from: http://www.unesco.org/new/es/natural-sciences/environment/water/wwap/wwdr/
- 12.Fekadu S, Alemayehu E, Dewil R, Van der Bruggen B. Pharmaceuticals in freshwater aquatic environments: A comparison of the African and European challenge. Sci Total Environ. 2019;654:324–337. doi: 10.1016/j.scitotenv.2018.11.072. [DOI] [PubMed] [Google Scholar]
- 13.Weber F. Pharmaceuticals in the environment - The global perspective: Occurrence, effects, and potential cooperative action under SAICM. 2014. German Federal Environmental Agency. [cited 29 October 2020]. Available from: https://www.umweltbundesamt.de/sites/default/files/medien/378/publikationen/pharmaceuticals_in_the_environment_0.pdf .
- 14.Silva B, Costa F, Neves IC, Tavares T. Psychiatric Pharmaceuticals as Emerging Contaminants in Wastewater. 2015. [Google Scholar]
- 15.Hai FI, Yang S, Asif MB, Sencadas V, Shawkat S, Sanderson-Smith M, Gorman J, Xu ZQ, Yamamoto K. Carbamazepine as a Possible Anthropogenic Marker in Water: Occurrences, Toxicological Effects, Regulations and Removal by Wastewater Treatment Technologies. Water. 2018;10:107. [Google Scholar]
- 16.Trawiński J, Skibiński R. Studies on photodegradation process of psychotropic drugs: a review. Environ Sci Pollut Res Int. 2017;24:1152–1199. doi: 10.1007/s11356-016-7727-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klaminder J, Brodin T, Sundelin A, Anderson NJ, Fahlman J, Jonsson M, Fick J. Long-Term Persistence of an Anxiolytic Drug (Oxazepam) in a Large Freshwater Lake. Environ Sci Technol. 2015;49:10406–10412. doi: 10.1021/acs.est.5b01968. [DOI] [PubMed] [Google Scholar]
- 18.Ford AT. From gender benders to brain benders (and beyond! Aquat Toxicol. 2014;151:1–3. doi: 10.1016/j.aquatox.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Brodin T, Piovano S, Fick J, Klaminder J, Heynen M, Jonsson M. Ecological effects of pharmaceuticals in aquatic systems--impacts through behavioural alterations. Philos Trans R Soc Lond B Biol Sci. 2014;369 doi: 10.1098/rstb.2013.0580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gilbert N. Drug waste harms fish. Nature. 2011;476:265. doi: 10.1038/476265a. [DOI] [PubMed] [Google Scholar]
- 21.Ågerstrand M Arnold K, Balshine S, Brodin T, Brooks BW Maack G, McCallum ES, Pyle G, Saaristo M, Ford AT. Emerging investigator series: use of behavioural endpoints in the regulation of chemicalsEnviron. Environ Sci Processes Impacts . 2020;22:49–65. doi: 10.1039/c9em00463g. [DOI] [PubMed] [Google Scholar]
- 22.Gunnarsson L, Jauhiainen A, Kristiansson E, Nerman O, Larsson DG. Evolutionary conservation of human drug targets in organisms used for environmental risk assessments. Environ Sci Technol. 2008;42:5807–5813. doi: 10.1021/es8005173. [DOI] [PubMed] [Google Scholar]
- 23.Stewart A, Wu N, Cachat J, Hart P, Gaikwad S, Wong K, Utterback E, Gilder T, Kyzar E, Newman A, Carlos D, Chang K, Hook M, Rhymes C, Caffery M, Greenberg M, Zadina J, Kalueff AV. Pharmacological modulation of anxiety-like phenotypes in adult zebrafish behavioral models. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1421–1431. doi: 10.1016/j.pnpbp.2010.11.035. [DOI] [PubMed] [Google Scholar]
- 24.Bauknecht P, Jékely G. Ancient coexistence of norepinephrine, tyramine, and octopamine signaling in bilaterians. BMC Biol. 2017;15:6. doi: 10.1186/s12915-016-0341-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Turlejski K. Evolutionary ancient roles of serotonin: long-lasting regulation of activity and development. Acta Neurobiol Exp (Wars) 1996;56:619–636. doi: 10.55782/ane-1996-1167. [DOI] [PubMed] [Google Scholar]
- 26.Horiuchi Y, Kimura R, Kato N, Fujii T, Seki M, Endo T, Kato T, Kawashima K. Evolutional study on acetylcholine expression. Life Sci. 2003;72:1745–1756. doi: 10.1016/s0024-3205(02)02478-5. [DOI] [PubMed] [Google Scholar]
- 27.Mukherjee S. Novel perspectives on the molecular crosstalk mechanisms of serotonin and melatonin in plants. Plant Physiol Biochem. 2018;132:33–45. doi: 10.1016/j.plaphy.2018.08.031. [DOI] [PubMed] [Google Scholar]
- 28.Abbey-Lee RN, Uhrig EJ, Garnham L, Lundgren K, Child S, Løvlie H. Experimental manipulation of monoamine levels alters personality in crickets. Sci Rep. 2018;8:16211. doi: 10.1038/s41598-018-34519-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Alvarenga KAF, Sacramento EK, Rosa DV, Souza BR, de Rezende VB, Romano-Silva MA. Effects of antipsychotics on intestinal motility in zebrafish larvae. Neurogastroenterol Motil. 2017;29 doi: 10.1111/nmo.13006. [DOI] [PubMed] [Google Scholar]
- 30.Carter LJ, Williams M, Martin S, Kamaludeen SPB, Kookana RS. Sorption, plant uptake and metabolism of benzodiazepines. Sci Total Environ. 2018;628-629:18–25. doi: 10.1016/j.scitotenv.2018.01.337. [DOI] [PubMed] [Google Scholar]
- 31.Li Y, Miao Y, Zhang W, Yang N, Niu L, Zhang H, Wang L. Sertraline inhibits top-down forces (predation) in microbial food web and promotes nitrification in sediment. Environ Pollut. 2020;267:115580. doi: 10.1016/j.envpol.2020.115580. [DOI] [PubMed] [Google Scholar]
- 32.Castillo-Zacarías C, Barocio ME, Hidalgo-Vázquez E, Sosa-Hernández JE, Parra-Arroyo L, López-Pacheco IY, Barceló D, Iqbal HNM, Parra-Saldívar R. Antidepressant drugs as emerging contaminants: Occurrence in urban and non-urban waters and analytical methods for their detection. Sci Total Environ. 2021;757:143722. doi: 10.1016/j.scitotenv.2020.143722. [DOI] [PubMed] [Google Scholar]
- 33.Escudero J, Muñoz JL, Morera-Herreras T, Hernandez R, Medrano J, Domingo-Echaburu S, Barceló D, Orive G, Lertxundi U. Antipsychotics as environmental pollutants: An underrated threat? Sci Total Environ. 2021;769:144634. doi: 10.1016/j.scitotenv.2020.144634. [DOI] [PubMed] [Google Scholar]
- 34.Arnold KE, Brown AR, Ankley GT, Sumpter JP. Medicating the environment: assessing risks of pharmaceuticals to wildlife and ecosystems. Philos Trans R Soc Lond B Biol Sci. 2014;369 doi: 10.1098/rstb.2013.0569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization. Pharmaceuticals in drinking water. [cited 29 October 2020]. Available from: https://www.who.int/water_sanitation_health/publications/2012/pharmaceuticals/en/
- 36.Wang Z, Gao S, Dai Q, Zhao M, Yang F. Occurrence and risk assessment of psychoactive substances in tap water from China. Environ Pollut. 2020;261:114163. doi: 10.1016/j.envpol.2020.114163. [DOI] [PubMed] [Google Scholar]
- 37.Amuasi JH, Lucas T, Horton R, Winkler AS. Reconnecting for our future: The Lancet One Health Commission. Lancet . 2020;395:1469–1471. doi: 10.1016/S0140-6736(20)31027-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lertxundi U, Hernández R, Medrano J, Orive G. Drug pollution and pharmacotherapy in psychiatry: A "platypus" in the room. Eur Psychiatry. 2020;63:e33. doi: 10.1192/j.eurpsy.2020.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Domingo-Echaburu S, Orive G, Lertxundi U. Ivermectin & COVID-19: Let's keep a One Health perspective. Sustain Chem Pharm. 2021;21:100438. doi: 10.1016/j.scp.2021.100438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaushik G, Thomas MA. The potential association of psychoactive pharmaceuticals in the environment with human neurological disorders. Sustain Chem Pharm. 2019;13 doi: 10.1016/j.scp.2019.100148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Richmond EK, Rosi EJ, Walters DM, Fick J, Hamilton SK, Brodin T, Sundelin A, Grace MR. A diverse suite of pharmaceuticals contaminates stream and riparian food webs. Nat Commun. 2018;9:4491. doi: 10.1038/s41467-018-06822-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cerveny D, Grabic R, Grabicová K, Randák T, Larsson DGJ, Johnson AC, Jürgens MD, Tysklind M, Lindberg RH, Fick J. Neuroactive drugs and other pharmaceuticals found in blood plasma of wild European fish. Environ Int. 2020;146:106188. doi: 10.1016/j.envint.2020.106188. [DOI] [PubMed] [Google Scholar]
- 43.Miller TH, Bury NR, Owen SF, MacRae JI, Barron LP. A review of the pharmaceutical exposome in aquatic fauna. Environ Pollut. 2018;239:129–146. doi: 10.1016/j.envpol.2018.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Verdú JR, Cortez V, Ortiz AJ, Lumaret JP, Lobo JM, Sánchez-Piñero F. Biomagnification and body distribution of ivermectin in dung beetles. Sci Rep. 2020;10:9073. doi: 10.1038/s41598-020-66063-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carter LJ, Ryan JJ, Boxall ABA. Effects of soil properties on the uptake of pharmaceuticals into earthworms. Environ Pollut. 2016;213:922–931. doi: 10.1016/j.envpol.2016.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Orive G, Lertxundi U. Virus, bats and drugs. Rev Environ Health. 2020;35:301–302. doi: 10.1515/reveh-2020-0083. [DOI] [PubMed] [Google Scholar]
- 47.European Medicines Agency. Environmental risk assessment of medicinal products for human use. [cited 28 October 2020]. Available from: https://www.ema.europa.eu/en/environmental-risk-assessment-medicinal-products-human-use .
- 48.Brintelix® (vortioxetina) European Public Assesment Report. [cited 8 October 2020]. Available from: https://www.ema.europa.eu/en/documents/assessment-report/brintellix-epar-public-assessment-report_en.pdf .
- 49.Sycrest® (asenapina) European Public Assesment Report. [cited 8 October 2020]. Available from: European Public Assesment Report.
- 50.Oakes KD, Coors A, Escher BI, Fenner K, Garric J, Gust M, Knacker T, Küster A, Kussatz C, Metcalfe CD, Monteiro S, Moon TW, Mennigen JA, Parrott J, Péry AR, Ramil M, Roennefahrt I, Tarazona JV, Sánchez-Argüello P, Ternes TA, Trudeau VL, Boucard T, Van Der Kraak GJ, Servos MR. Environmental risk assessment for the serotonin re-uptake inhibitor fluoxetine: Case study using the European risk assessment framework. Integr Environ Assess Manag. 2010;6 Suppl:524–539. doi: 10.1002/ieam.77. [DOI] [PubMed] [Google Scholar]
- 51.European Medicines Agency. Environmental risk assessment of medicinal products for human use. Review Draft. [cited 7 October 2020]. Available from: https://www.ema.europa.eu/en/environmental-risk-assessment-medicinal-products-human-use .
- 52.Wess RA. Update of EMA's Guideline on the Environmental Risk Assessment (ERA) of Medicinal Products for Human Use. Ther Innov Regul Sci. 2021;55:309–323. doi: 10.1007/s43441-020-00216-1. [DOI] [PubMed] [Google Scholar]
- 53.Jose J, Sandra Pinto J, Kotian B, Mathew Thomas A, Narayana Charyulu R. Comparison of the regulatory outline of ecopharmacovigilance of pharmaceuticals in Europe, USA, Japan and Australia. Sci Total Environ. 2020;709:134815. doi: 10.1016/j.scitotenv.2019.134815. [DOI] [PubMed] [Google Scholar]
- 54.Little CJ, Boxall AB. Environmental pollution from pet parasiticides. Vet Rec . 2020;186:97. doi: 10.1136/vr.m110. [DOI] [PubMed] [Google Scholar]
- 55.Domingo-Echaburu S, Lertxundi U, Boxall ABA, Orive G. Environmental contamination by pet pharmaceuticals: A hidden problem. Sci Total Environ. 2021;788:147827. doi: 10.1016/j.scitotenv.2021.147827. [DOI] [PubMed] [Google Scholar]
- 56.European Commission. European Union Strategic Approach to Pharmaceuticals in the Environment. [cited 22 September 2020]. Available from: https://ec.europa.eu/info/Law/better-regulation/initiatives/ares-2017-2210630_en .
- 57.Government of the Netherlands. Reducing Pharmaceutical Residues in Water: A Chain Approach. [cited 7 March 2020]. Available from: https://www.government.nl/documents/policy-notes/2019/02/12/reducing-pharmaceutical-residues-in-water-achain-approach.
- 58.World Health Organization. Rational Use of Medicines. [cited 29 October 2020]. Available from: http://www.who.int/medicines/areas/rational_use/en/index.html .
- 59.Orive G, Domingo-Echaburu S, Lertxundi U. Redefinig “rational use of medicines”. Sustainable Chemistry and Pharmacy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lertxundi U, Domingo-Echaburu S, Orive G. Rational use of drugs as a source control measure to fight drug pollution. J Hazard Mater. 2021;410:124664. doi: 10.1016/j.jhazmat.2020.124664. [DOI] [PubMed] [Google Scholar]
- 61.Swedish Environmental Research Institute. Environmentally Classified Pharmaceuticals. [cited 9 December 2020]. Available from: https://politiquedesante.fr/wp-content/uploads/2014/05/PBT-2014-2015-copie.pdf .
- 62.Gustafsson LL, Wettermark B, Godman B, Andersén-Karlsson E, Bergman U, Hasselström J, Hensjö LO, Hjemdahl P, Jägre I, Julander M, Ringertz B, Schmidt D, Sjöberg S, Sjöqvist F, Stiller CO, Törnqvist E, Tryselius R, Vitols S, von Bahr C Regional Drug Expert Consortium. The 'wise list'- a comprehensive concept to select, communicate and achieve adherence to recommendations of essential drugs in ambulatory care in Stockholm. Basic Clin Pharmacol Toxicol. 2011;108:224–233. doi: 10.1111/j.1742-7843.2011.00682.x. [DOI] [PubMed] [Google Scholar]
- 63.Leder C. Putting benign by design into practice-novel concepts for green and sustainable pharmacy: Designing green drug derivatives by non-targeted synthesis and screening for biodegradability. Sustainable Chem Pharm. 2015;2:31–36. [Google Scholar]
- 64.Banik BK. In Advances in Green Chemistry, Green Approaches in Medicinal Chemistry for Sustainable Drug Design. Elsevier . 2020 [Google Scholar]
- 65.Dai L, Liu K, Si C, Wang L, Liu J, He J, Lei J. Ginsenoside nanoparticle: a new green drug delivery system. J Mater Chem B. 2016;4:529–538. doi: 10.1039/c5tb02305j. [DOI] [PubMed] [Google Scholar]
- 66.Lertxundi U, Domingo-Echaburu S, Orive G. It’s about time healthcare professionals and academics start thinking about drug pollution. Sustainable Chem Pharm . 2020 [Google Scholar]
- 67.Liu J, Wang J, Hu XM. Knowledge, perceptions, and practice of ecopharmacovigilance among pharmacy professionals in China. Environ Monit Assess. 2017;189:552. doi: 10.1007/s10661-017-6289-4. [DOI] [PubMed] [Google Scholar]
- 68.Wang J, Li S, He B. Chinese physicians' attitudes toward eco-directed sustainable prescribing from the perspective of ecopharmacovigilance: a cross-sectional study. BMJ Open. 2020;10:e035502. doi: 10.1136/bmjopen-2019-035502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Paut Kusturica M, Tomas A, Sabo A. Disposal of Unused Drugs: Knowledge and Behavior Among People Around the World. Rev Environ Contam Toxicol. 2017;240:71–104. doi: 10.1007/398_2016_3. [DOI] [PubMed] [Google Scholar]
- 70.Alhamad H, Patel N & Donyai P. Beliefs and intentions towards reusing medicines in the future: a large‐scale, cross‐sectional study of patients in the UK. Int J Pharm Pract. 2018;26 Suppl 1:12. [Google Scholar]
- 71.European Parliament. [cited 7 October 2020]. Available from: https://www.europarl.europa.eu/doceo/document/TA-9-2020-0226_EN.pdf .
- 72.Gomez Cortes L, Marinov D, Sanseverino I. Selection of substances for the 3rd Watch List under the Water Framework Directive, EUR 30297 EN, Publications Office of the European Union, Luxembourg, 2020. [Google Scholar]
- 73.Lertxundi U, Domingo-Echaburu S, Hernandez R, Medrano J, Orive G. Venlafaxine and desvenlafaxine to be included in the surface water Watch List. Aust N Z J Psychiatry. 2021:4867421998787. doi: 10.1177/0004867421998787. [DOI] [PubMed] [Google Scholar]
- 74.Herlev´s hospital wastewater treatment. [cited 8 October 2020]. Available from: https://nordiclifescience.org/nordic-solutions-for-handling-pharma-waste/
- 75.Swiss Federal Institute of Aquatic Science and Technology (EAWAG) [cited 8 October 2020]. Available from: https://www.eawag.ch/en/
- 76.Bourgin M, Beck B, Boehler M, Borowska E, Fleiner J, Salhi E, Teichler R, von Gunten U, Siegrist H, McArdell CS. Evaluation of a full-scale wastewater treatment plant upgraded with ozonation and biological post-treatments: Abatement of micropollutants, formation of transformation products and oxidation by-products. Water Res. 2018;129:486–498. doi: 10.1016/j.watres.2017.10.036. [DOI] [PubMed] [Google Scholar]
- 77.Cruz Del Álamo A, Pariente MI, Martínez F, Molina R. Trametes versicolor immobilized on rotating biological contactors as alternative biological treatment for the removal of emerging concern micropollutants. Water Res. 2020;170:115313. doi: 10.1016/j.watres.2019.115313. [DOI] [PubMed] [Google Scholar]
- 78.Kühler TC, Andersson M, Carlin G, Johnsson A, Akerblom L. Do biological medicinal products pose a risk to the environment? Drug Saf. 2009;32:995–1000. doi: 10.2165/11316540-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 79.Manuel Gómez-Oliván L. Ecopharmacovigilance: Multidisciplinary Approaches to Environmental Safety of Medicines. The Handbook of Environmental Chemistry. Springer, 2019. [Google Scholar]
- 80.Susarla S, Medina VF, McCutcheon SC (2002) Phytoremediation: an ecological solution to organic chemical contamination. Ecol Eng 2002; 18: 647–658. [Google Scholar]
- 81.Carvalho PN, Basto MC, Almeida CM, Brix H. A review of plant-pharmaceutical interactions: from uptake and effects in crop plants to phytoremediation in constructed wetlands. Environ Sci Pollut Res Int. 2014;21:11729–11763. doi: 10.1007/s11356-014-2550-3. [DOI] [PubMed] [Google Scholar]
- 82.Bartha B, Huber C, Harpaintner R, Schröder P. Effects of acetaminophen in Brassica juncea L. Czern.: investigation of uptake, translocation, detoxification, and the induced defense pathways. Environ Sci Pollut Res Int. 2010;17:1553–1562. doi: 10.1007/s11356-010-0342-y. [DOI] [PubMed] [Google Scholar]
- 83.Carter LJ, Harris E, Williams M, Ryan JJ, Kookana RS, Boxall AB. Fate and uptake of pharmaceuticals in soil-plant systems. J Agric Food Chem. 2014;62:816–825. doi: 10.1021/jf404282y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Whitlock SE, Pereira MG, Shore RF, Lane J, Arnold KE. Environmentally relevant exposure to an antidepressant alters courtship behaviours in a songbird. Chemosphere. 2018;211:17–24. doi: 10.1016/j.chemosphere.2018.07.074. [DOI] [PubMed] [Google Scholar]
- 85.Brodin T, Fick J, Jonsson M, Klaminder J. Dilute concentrations of a psychiatric drug alter behavior of fish from natural populations. Science. 2013;339:814–815. doi: 10.1126/science.1226850. [DOI] [PubMed] [Google Scholar]
- 86.Kalichak F, de Alcantara Barcellos HH, Idalencio R, Koakoski G, Soares SM, Pompermaier A, Rossini M, Barcellos LJG. Persistent and transgenerational effects of risperidone in zebrafish. Environ Sci Pollut Res Int. 2019;26:26293–26303. doi: 10.1007/s11356-019-05890-9. [DOI] [PubMed] [Google Scholar]