Abstract
BACKGROUND
Electroconvulsive therapy (ECT) is used to treat major depressive disorder (MDD). Relapse is often observed even after successful ECT, followed by adequate pharmaceutical treatment for MDD.
AIM
To investigate the diagnostic factors and treatment strategies associated with depression relapse.
METHODS
We analyzed the relationships between relapse, the diagnostic change from MDD to bipolar disorder (BP), and treatment after the initial ECT. We performed a 3-year retrospective study of the prognoses of 85 patients of the Shiga University of Medical Science Hospital. The relative risk of relapse of depressive symptoms was calculated based on the diagnostic change from MDD to BP. A receiver operating characteristic (ROC) curve was generated to evaluate the predictive accuracy of diagnostic changes from MDD to BP based on the duration between the first course of ECT and the relapse of depressive symptoms.
RESULTS
Eighty-five patients initially diagnosed with MDD and successfully treated with ECT were enrolled in the study. Compared with the MDD participants, more BP patients experienced relapses and required continuation and/or maintenance ECT to maintain remission (65.6% vs 15.1%, P < 0.001; relative risk = 4.35, 95%CI: 2.19-8.63, P < 0.001). Twenty-nine patients experienced relapses during the three-year follow-up. In 21 (72.4%, 21/29) patients with relapse, the diagnosis was changed from MDD to BP. The duration from the first course of ECT to relapse was shorter for the BP patients than for the MDD patients (9.63 ± 10.4 mo vs 3.38 ± 3.77 mo, P = 0.022); for most patients, the interval was less than one month. The relative risk of depressive symptoms based on diagnostic changes was 4.35 (95% confidence interval: 2.19–8.63, P < 0.001), and the area under the ROC curve for detecting diagnostic changes based on relapse duration was 0.756 (95%CI: 0.562-0.895, P = 0.007).
CONCLUSION
It may be beneficial to suspect BP and change the treatment strategy from MDD to BP for patients experiencing an early relapse.
Keywords: Electroconvulsive therapy, Major depressive disorder, Bipolar disorder, Antidepressant, Prognosis, Relapse
Core Tip: Patients who are diagnosed with major depressive disorder (MDD) but repeatedly relapse after electroconvulsive therapy (ECT) and require continuation and/or maintenance electroconvulsive therapy (C/M-ECT) may be in the depressive phase of bipolar disorder (BP). Rather than repeating C/M-ECT alone, even without obvious manic symptoms, the treatment for MDD may have to be revised to that for BP for patients who relapse within one month.
INTRODUCTION
Treatment options for major depressive disorder (MDD) resistant to pharmaceutical therapy are extremely limited[1]. Currently, electroconvulsive therapy (ECT) is the most promising therapeutic modality for MDD, including drug-resistant depression[2,3]. The efficacy of ECT is reportedly 50%–60% for drug-resistant depression, irrespective of the presence of psychotic features[4]. However, most ECT-treated patients who continue pharmacotherapy experience relapse within 6 mo after receiving adequate ECT[5,6].
Thus, some maintenance therapies after adequate ECT are usually utilized to prevent relapse if the initial therapy results in the complete remission of depression. It has been reported that maintenance therapy with a combination of lithium and an antidepressant is more effective than antidepressants alone[7,8]. Moreover, cumulative evidence suggests that continuation and/or maintenance ECT (C/M-ECT) combined with pharmacotherapy maintains a significantly higher remission rate several months after the initial ECT[9,10]. Recent reviews and meta-analyses have recommended C/M-ECT combined with pharmacotherapy for MDD[11,12].
However, it remains unclear whether the recommended therapeutic strategy obscures the potential risk of a future manic episode since both ECT and mood stabilizers, such as lithium, are effective for both depressive and manic symptoms. A considerable proportion of patients with bipolar disorder (BP) are misdiagnosed with MDD at their first visit[13-15] because their episodes emerge as depression more often than mania.
Several studies have reported a diagnostic change from MDD to BP during the treatment of MDD[14-18]. However, the prognosis of antidepressant-resistant depressive patients after remission using ECT has not been systematically investigated. Therefore, we hypothesized that remission of depression after ECT followed by a relapse, even after receiving an antidepressant-based maintenance therapy without any mood stabilizers, is indicative of BP. To test our hypothesis, we conducted a retrospective cohort study involving a 3-year follow-up of patients who experienced remission of depression after undergoing ECT at our hospital.
MATERIALS AND METHODS
Participants
We recruited patients who were admitted to the Department of Psychiatry at the Shiga University of Medical Science Hospital and had their first ECT between January 2009 and December 2011.
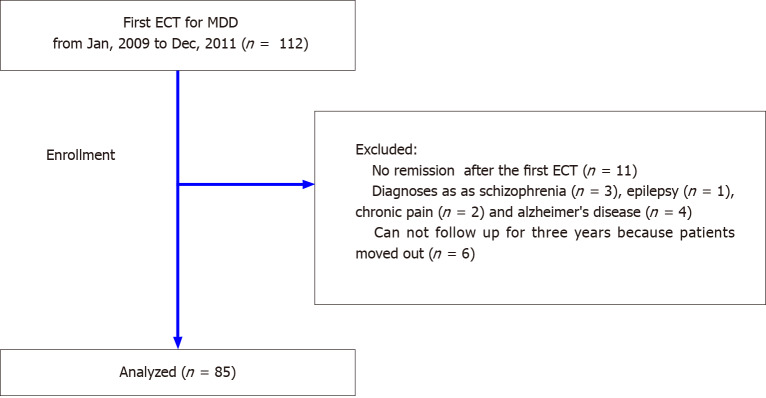
Diagnoses of inpatients in the psychiatry department, based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)[19], were routinely made by the consensus of multiple psychiatrists who are members of the Japanese Board of Psychiatry at weekly conferences. Decisions to change the diagnosis of manic/hypomanic episodes from MDD to BP were also made during the conferences. We included patients who were initially diagnosed with MDD (n = 112) without any other mental or neurological disorders (Figure 1). Patients who were initially diagnosed as BP or with BP mixed episodes were not included in this study.
Figure 1.
Flow diagram of the participants. ECT: Electroconvulsive therapy; MDD: Major depressive disorder.
Definitions of remission and relapse
We defined successful remission after ECT as follows: (1) The patient no longer conformed to the diagnostic criteria for MDD; (2) the Hamilton Depression Scale 21-Item (HAMD-21)[20] score improved by ≥ 60% since admission; and (3) the patient was discharged and resumed normal activity at home.
Relapse was defined as the reappearance of five or more symptoms of the diagnostic criteria for MDD.
Criterion for changing diagnosis
When there was a manic/hypomanic episode meeting the DSM-IV-Text Revision (DSM-IV-TR)[19] criteria during the follow-up, the diagnosis was changed to BP. BP I and II were diagnosed when the patients had manic and hypomanic episodes, respectively. Diagnostic changes and changes in treatment strategy from MDD to BP among inpatients were made within one week after the first manic/hypomanic episodes were observed. Manic/hypomanic episodes of outpatients were determined when manic/hypomanic symptoms persisted for at least more than a couple of days. Moreover, when other psychotic and epileptic symptoms were dominant and met the DSM-IV-TR[19] diagnostic criteria, the diagnosis was changed to schizophrenia and epilepsy, respectively.
The patients were typically treated with antidepressants according to the American Psychiatric Association (APA) guidelines[4]. ECT was carefully applied according to the APA Practice Guideline[4] and the National Institute for Health and Care Excellence (NICE) guidelines in the United Kingdom[21]. At least one of the following criteria was met for the administration of ECT to patients with MDD: (1) The patients did not experience remission despite receiving a sufficient dose of two or more antidepressants (drug resistance); (2) The patients had serious suicidal thoughts; and (3) It was difficult to administer pharmacotherapy, such as when patients were unable to take food and oral medications due to psychomotor retardation or hypobulia.
We excluded patients who failed to achieve remission after the first ECT (n = 11) and those who were diagnosed with schizophrenia (n = 3), epilepsy (n = 1), chronic pain (n = 2), or Alzheimer's disease (n = 4) during the follow-up. We could not follow up 6 patients for the duration after the first ECT, as they moved out (Figure 1).
Eighty-five participants, with a significant improvement in depressive symptoms and remission after the first successful course of ECT, were naturally observed. Depression severity and psychosocial dysfunction were assessed using the HAMD-21[20] and the Global Assessment of Functioning scale (GAF) of the DSM-IV-TR[19]. The duration of the follow-up observation was set to 36 mo after remission was achieved with the first course of ECT. Anxiety symptoms were not included in this study, which were not included in the diagnostic criteria for MDD in the DSM-IV-TR.
The study was conducted according to the guidelines of the Declaration of Helsinki. Written informed consent was not obtained because of the retrospective nature of the study. We displayed the study protocol on the hospital’s website and outpatient units of the hospital. The participants were offered the opportunity to opt out of the study. The study protocol was approved by the Shiga University of Medical Science Ethics Committee (27-178) and registered in the UMIN-CTR (UMIN000030458).
We obtained patient data from the medical records: Age, sex, number, and date of ECT, HAMD-21, GAF, diagnosis, onset of disease, medication, psychotic features, and depressive symptoms. These were all essential medical data for ECT and were cross-checked with the doctors in charge. No missing data were included in the study.
Group classification
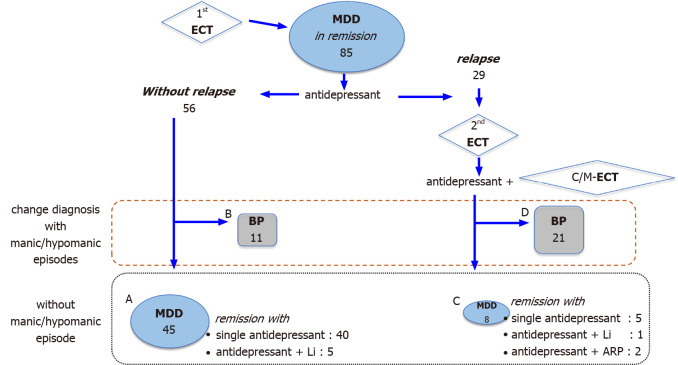
The participants were retrospectively classified into four groups based on their clinical course (Figure 1). Four groups were included and analyzed in this study.
Groups A and B
Fifty-six participants who did not experience a relapse of depressive symptoms after the first course of ECT were classified as A and B. The patients were treated with pharmacotherapy based on their respective diagnoses.
Group A included 45 participants with MDD; 40 remained in remission with treatment with a continuous single antidepressant, and five remained in remission with the concomitant use of lithium and some antidepressants.
Group B included eleven participants with BP, whose diagnoses changed from MDD to BP based on the manic/hypomanic symptoms during their first course of ECT or during subsequent maintenance therapy with antidepressants. Six and five of them were diagnosed with BP I and BP II, respectively. The maintenance therapy was continued after ECT, and the antidepressant treatments were discontinued. All patients in group B were maintained in remission with mood stabilizers.
Groups C and D
Twenty-nine participants who experienced relapses of depressive symptoms after the first course of ECT were classified as C and D. All patients achieved remission after the second course of ECT and were switched to C/M-ECT with antidepressants.
Group C included eight participants with MDD: five experienced a repeated relapse of depressive symptoms and were maintained in remission with SSRIs or SNRIs; two experienced relapse and were maintained in remission on a tricyclic antidepressant and aripiprazole; and one experienced relapse but was maintained in remission on an antidepressant with lithium after C/M-ECT was discontinued.
Group D included twenty-one participants with BP whose diagnoses changed from MDD to BP because they had manic/hypomanic symptoms during C/M-ECT with antidepressants, which persisted after treatment was discontinued. Two and nineteen of them were diagnosed with BP I and BP II, respectively. Patients in this group were maintained in remission with mood stabilizers without C/M-ECT.
ECT procedures
ECT was performed using a THYMATRON SYSTEM IV ECT instrument (Somatics LLC, Lake Bluff, IL, USA). Procedures for anesthesia and the determination of seizure adequacy followed a standardized clinical protocol that was consistent with the current standards of care[3]. Anesthesia for the procedure included intravenous thiamylal (1.0 -1.5 mg/kg) and succinylcholine (1 mg/kg). The participants were pre-oxygenated and manually ventilated using a valve mask and 100% oxygen after they showed adequate muscle relaxation. The electrodes were placed bilaterally on the forehead. The electrical dose for the short-term course of ECT was estimated using the ‘‘half age method.” The median number of ECT sessions was 8.47 ± 3.72. The same energy required for short-term treatment was used for the second course of ECT and C/M-ECT. For the short-term course, the participants received two or three weekly sessions until remission.
Follow-up regimens
Pharmaceutical maintenance therapy was administered to all participants following the first course of ECT. Tricyclic antidepressants (TCAs) were preferentially selected for the maintenance treatment of all participants with MDD if they were tolerable. Sackeim et al[22] reported that nortriptyline increases remission compared to venlafaxine when concomitantly administered with ECT in patients with MDD. Venlafaxine was not available in Japan during the study period. Fifty-two participants primarily received TCAs, and 41 received selective serotonin or norepinephrine reuptake inhibitors (SSRI/SNRIs). All antidepressants were prescribed in doses equivalent to 150 mg of imipramine, which satisfied the maximum allowable dose.
When 29 of the participants experienced a relapse, a second course of ECT was administered, and remission was achieved. Subsequently, the treatment was changed to C/M-ECT with antidepressants. If no relapse was observed, the intervals for the C/M-ECTs gradually increased from one to six months.
We terminated C/M-ECT when remission was maintained for more than 6 mo or new-onset psychiatric symptoms (e.g., mood-incongruent delusions) were dominant.
Statistical analyses
The clinical characteristics are presented as mean ± SD. We performed a chi-square test or t-test to investigate any intergroup differences in the following items as needed: (1) Demographic data (sex, age at onset, and disease duration until the first ECT session); (2) Admission data (HAMD-21 score during admission, GAF score, the presence of psychotic features, and the number of ECT performed during the first course); (3) Discharge data (HAMD-21 score during discharge, GAF score, and type of antidepressants for maintenance therapy); and (4) Post-discharge data (the period of relapse to C/M-ECT and the diagnosis 36 mo after the final ECT).
The relative risk (RR) and 95%CIs of the relapses of depressive symptoms were calculated according to the diagnostic changes from MDD to BP during the three-year follow-up. Receiver operating characteristic (ROC) curves were generated to evaluate the diagnostic accuracy of predicting diagnostic changes from MDD to BP from the duration between the first course of ECT and relapse of depressive symptoms. We used the MedCalc Software Ver. 19.7.2 (Ostend, Belgium) for statistical analyses. Statistical significance was set at P < 0.05. For the sensitivity analysis, we performed a non-parametric analysis (Mann-Whitney test).
Sample and power analyses were performed using G*Power 3.1.9.7 (University of Kiel, Germany). Kellner et al[23] reported that the average duration of relapse was 9.1 ± 7 wk after ECT. We determined to use the same sample size and SDs for the MDD and BP groups, and hypothesized that the mean difference in the relapse durations of 9 wk may be clinically significant. We used α = 0.05, power = 0.80, mean difference = 9, and SD = 7 for the sample size estimation. In this study, we estimated the need for a sample size of 22.
The statistical methods used in this study were reviewed by Prof. Hiromu Kutsumi and Mr. Shoji Momokawa from the Center for Clinical Research and Advanced Medicine, Shiga University of Medical Science.
RESULTS
Characteristics of the participants
This study included 85 participants aged 56.0 ± 17.0 years; 31.8% of them were males (n = 27) (Table 1, Figure 1). The average initial depressive episode started at the age of 51.7 ± 17.4 years, and the first ECT was administered after 53.1 ± 83.2 mo. All participants were followed up for 36 mo. Depression was recovered by the first ECT with scores of HAMD-21 (from 22.3 ± 13.8 to 7.13 ± 5.03, P < 0.001) and GAF (from 32.9 ± 15.5 to 66.6 ± 7.70, P < 0.001).
Table 1.
Characteristics of the participants
|
Variables
|
Total
|
MDD patients
|
BP patients
|
P
values
|
MDD with remission
|
BP with remission
|
P
values
|
| n | 85 | 53 | 32 | 8 | 21 | ||
| Male, n (%) | 27 (31.8) | 16 (30.2) | 11 (34.4) | 0.690 | 2 (25.0) | 7 (33.3) | 0.670 |
| Age, yr | 56.0 ± 17.0 | 56.6 ± 17.6 | 55.0 ± 16.1 | 0.676 | 55.0 ± 21.3 | 51.9 ± 14.9 | 0.656 |
| Onset age, yr | 51.7 ± 17.4 | 53.7 ± 18.3 | 48.5 ± 15.3 | 0.179 | 51.4 ± 23.3 | 47.0 ± 13.2 | 0.527 |
| Duration from onset to first ECT, mo | 53.1 ± 83.2 | 33.5 ± 48.1 | 85.8 ± 115 | 0.009 | 36.9 ± 37.9 | 67.1 ± 86.1 | 0.385 |
| Psychotic features, n (%) | 30 (35.3) | 23 (43.4) | 7 (21.9) | 0.046 | 3 (37.5) | 5 (23.8) | 0.469 |
| HAMD-21 on admission | 22.3 ± 13.8 | 24.4 ± 15.1 | 18.9 ± 10.9 | 0.079 | 26.4 ± 11.0 | 19.1 ± 10.2 | 0.103 |
| HAMD-21 on discharge | 7.13 ± 5.03 | 6.77 ± 4.14 | 7.72 ± 6.26 | 0.008 | 8.75 ± 4.59 | 6.90 ± 5.43 | 0.403 |
| GAF on admission | 32.9 ± 15.5 | 31.0 ± 16.0 | 36.0 ± 14.5 | 0.150 | 37.9 ± 9.88 | 39.0 ± 16.0 | 0.861 |
| GAF on discharge | 66.6 ± 7.70 | 66.4 ± 7.52 | 67.0 ± 8.08 | 0.720 | 66.5 ± 9.07 | 69.2 ± 5.97 | 0.348 |
| Duration from first ECT to relapse, mo | 9.63 ± 10.4 | 3.38 ± 3.77 | 0.022 |
Results showed as mean ± SD. MDD: Major depressive disorder; BP: Bipolar disorder; ECT: Electroconvulsive therapy; HAMD-21: Hamilton Depression Scale; GAF: Global Assessment of Functioning Scale.
The MDD participants included patients whose diagnosis was not changed during the three-year follow-up for the initial ECT (groups A and C in Figure 2).
Figure 2.
Changes in the treatment and diagnosis based on the relapse and manic/hypomanic episodes after remission after the first electroconvulsive therapy. Relapses were characterized by five or more of the diagnostic criteria for major depressive disorder. Patients in groups A and B did not experience relapse after the first course of electroconvulsive therapy (ECT). Patients in groups C and D experienced a relapse after the first course of ECT. When there was a manic/hypomanic episode during the follow-up, the diagnosis was changed from major depressive disorder to bipolar disorder. ECT: Electroconvulsive therapy; MDD: Major depressive disorder; BP: Bipolar disorder; Li: Lithium; ARP: Aripiprazole.
The BP participants included patients whose diagnosis was changed from MDD to BP during the three-year follow-up for initial ECT (groups B and D in Figure 2).
MDD with remission participants included patients who experienced relapses of depressive episodes after the first course of ECT, who maintained remission with MDD treatment (groups C).
BP with remission participants included patients whose diagnoses were changed from MDD to BP because of manic/hypomanic symptoms during C/M-ECT with antidepressants (group D). Subjects in this group experienced relapses of depressive symptoms after the first course of ECT with antidepressants, but they maintained remission with BP treatment.
Three subjects without relapse were excluded from this study. The diagnoses of two subjects (one male and one female) were changed to schizophrenia due to psychotic episodes. The diagnosis of another man was changed to epileptic psychosis because of his past convulsive seizure episodes with psychotic features.
Seven subjects with relapse were also excluded from the study. Four subjects (two women and two men) had their diagnoses changed to concomitant MDD and Alzheimer's dementia due to their consistent mnemonic impairments; two males had their diagnoses changed to concomitant MDD and chronic pain, and another male had his diagnosis changed to schizophrenia.
Diagnostic group-specific characteristics (MDD vs BP)
We compared the demographic data of the participants whose MDD diagnosis did not change during the three-year follow-up (Groups A and C) and those whose diagnosis was changed to BP (Groups B and D). There were no significant differences between the two groups related to sex, age, age of onset, and HAMD-21/GAF scores during admission or discharge (Table 1). However, the duration from the onset of depression to the first ECT was significantly shorter in the MDD participants (Groups A and C) than in the BP participants (Groups B and D) (33.5 ± 48.1 vs 85.8 ± 114.9%, P = 0.009), while psychotic features were more prominent in the MDD participants (43.4% vs 21.9%, P = 0.046).
The MDD and BP participants with remission (Group C vs D) had similar demographic data, except for the duration from the first course of ECT to relapse (Table 1).
Diagnostic change due to manic/hypomanic episodes
Of the 85 participants, 32 (37.6%) had their diagnosis changed to BP because of manic/hypomanic episodes experienced after remission after the first ECT or during the C/M-ECT period (Groups B and D; Figure 2).
Higher risk of relapse among patients with diagnostic changes than those without
We observed a significantly higher risk of relapse in the diagnostic change groups (Groups B and D) than in the unchanged groups (Groups A and C) (RR = 4.35, 95%CI: 2.19-8.63, P <0.001). A higher percentage of relapses was found in participants whose diagnosis was changed from MDD to BP (65.6%: Group D/Groups B + D) than in those whose diagnosis was MDD (15.1%: Group C/Groups A + C) (P <0.001) (Figure 2). In addition, the types of antidepressants (SSRI/SNRI or TCA) for maintenance therapy were similar among the groups (Groups A, B, C, and D) (chi-square test, P = 0.77).
Period until relapse
We investigated the duration from the first course of ECT to the relapse of depressive symptoms in the patients with MDD and BP (groups C and D). The relapse was significantly earlier in the group with a change in the diagnosis to BP (Group D) than in the group without any diagnostic changes (Group C). (t-test, P = 0.022; Figure 3). As a sensitivity analysis, we performed a non-parametric analysis (Mann-Whitney test) on duration from the first course of ECT to relapse between patients with MDD and BP (groups C and D), and we had a similar finding with a P value of 0.034.
Figure 3.
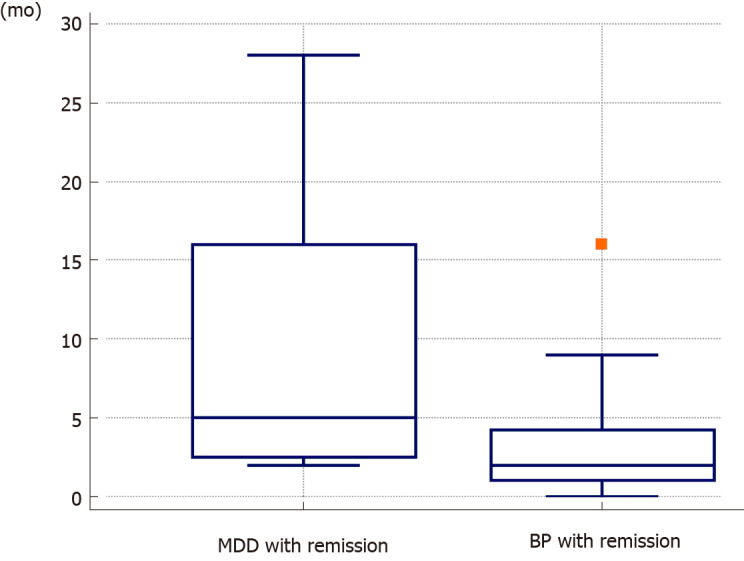
Period to relapse in the continuation and/or maintenance electroconvulsive therapy group. The box-and-whisker plot displays the statistical summary of the variables. The central box shows values from the lower to the upper quartiles. The middle line represents median values. The horizontal line extends from the minimum to the maximum value, excluding the outliers, which are displayed as separate points. The BP participants in group D experienced relapse significantly earlier than the major depressive disorder participants in group C.
To determine the predictive value of the duration until relapse for BP, we performed an ROC analysis (Figure 4). Of the patients who experienced a relapse of depressive symptoms within 3 mo, 75% had BP, whereas 61.9% of those who remained relapse-free for at least 3 mo had MDD.
Figure 4.
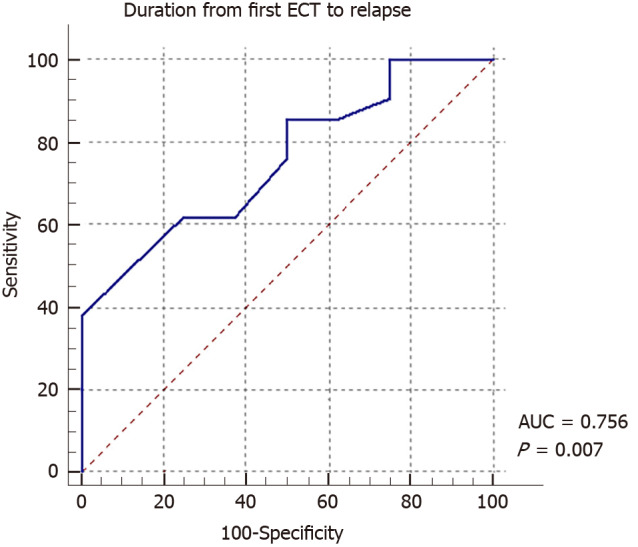
Receiver operating characteristic analysis for determining the accuracy of the diagnosis based on the duration of the period until relapse. Receiver operating characteristic (ROC) curves were generated to evaluate the diagnostic accuracy of predicting diagnostic changes from major depressive disorder to Bipolar disorder from the duration between the first course of electroconvulsive therapy and relapse of depressive symptoms. The area under the ROC curve to for detecting diagnostic changes by based on relapse duration was 0.756 (95%CI: 0.562-0.895, P = 0.007).
A period of less than 1 mo to relapse demonstrated a sensitivity of 38.1% (95%CI: 18.1%-61.6%), specificity of 100% (95%CI: 63.1%-100%), and the area under the ROC curve of 0.756 (95%CI: 0.562-0.895) (P = 0.007), which indicated a moderately predictive of the diagnostic change from MDD to BP.
DISCUSSION
Patients with BP are more likely to experience relapses after ECT
We investigated the prognosis of 85 participants who were initially diagnosed with MDD, underwent ECT, and experienced remission over 3 years to identify the effect of subsequent maintenance pharmacotherapy on patients with MDD. Our results indicate that 29 participants experienced a relapse despite maintenance therapy with antidepressants after their first course of ECT and subsequently required C/M-ECT. Twenty-one participants (group D) had their diagnosis changed to BP. Therefore, BP was overlooked when potential BP patients who had depressive episodes were diagnosed with MDD, underwent ECT, and were treated with antidepressants. Patients with BP are more likely to experience a relapse during maintenance therapy with antidepressants[24,25]. This may be a major reason for drug resistance and necessitates repeated C/M-ECT.
There are no established guidelines for the management of ECT–induced mania, and there is little evidence to guide clinicians beyond case reports and clinical experience[26]. A case report by Lee et al[27] described ECT-induced mania treated by aborting ECT and adding a mood stabilizer. Another case report by Thomas et al[26] described ECT-induced mania treated with repeated ECT alone. In this study, we aborted ECT and used mood stabilizers to treat ECT–induced mania.
Generally, a large proportion of patients with BP-associated depression may be misdiagnosed with MDD and initially treated with antidepressants alone. Regardless of treatment resistance, their diagnoses changed from MDD to BP during treatment [14-18]. In agreement with this, we found that the proportion of participants whose diagnosis was changed from MDD to BP during the maintenance treatment was similar to or higher than those reported in previous studies, although those studies involved smaller samples or reported shorter follow-ups than the current study[14-18]. To our knowledge, this is the first report to date that focuses on the possibility that patients with MDD, for which ECT is repeatedly indicated, may experience the depressive phase of BP. When patients have never experienced manic/hypomanic episodes, they cannot be diagnosed with BP; therefore, they remain diagnosed with MDD and are treated with maintenance antidepressant therapy until a first manic/hypomanic episode occurs.
Predictors of conversion to BP include the prevalence of psychotic depression[28]. Psychotic features were not prevalent among patients diagnosed with BP in this study, which may be related to the relatively old age of the patient group in this study (51.7 ± 17.4 years).
Requirements of augmentation pharmacotherapy as a potential predictor for future BP diagnosis
Of the 53 participants (groups A and C) who were ultimately diagnosed with MDD, 45 (84.9%) remained in remission with a single antidepressant, irrespective of the type of antidepressant (TCA or SSRI/SNRI). Although antidepressant-antipsychotic cotreatment is known to be effective in treating psychotic depression[29], there are no established guidelines for the management of MDD manifesting with psychotic symptoms after ECT.
In groups A and C, only five participants in group A and three participants in group C required lithium or aripiprazole augmentation to maintain remission (15.1%: (5 + 3)/(45 + 8)), whereas 45 participants maintained remission using a single antidepressant without requiring the use of lithium [84.9%: (40 + 5)/(45 + 8)]. Sackeim et al[7] (2001) indicated that the concomitant use of lithium was more effective than the use of nortriptyline alone in maintaining remission after ECT in patients with MDD. Likewise, aripiprazole has also been reported as a popular augmentation agent for the treatment of depression[30]. Although we considered the possibility that lithium augmentation could obscure the actual diagnosis, the results indicated that BP was more common in the relapse group.
A recent observational study reported no significant difference in the relapse ratio between MDD and BP after receiving ECT during a one-year follow-up[31]. However, valproate maintenance pharmacotherapy for MDD was associated with a lower risk of relapse than valproate treatment (multivariate analysis, hazard ratio: 0.091; P = 0.022).
In the current study, a large proportion (84.9%, 45/53) of patients with MDD remained in remission for three years with only a single antidepressant. Thus, an adequate dose of antidepressant monotherapy can maintain remission with good tolerability if the diagnosis of MDD is accurate.
These results indicate the importance of the initial diagnosis of MDD. Moreover, relapse that occurs during antidepressant maintenance therapy seems to be a major predictor of later changes in BP diagnosis.
Average time to relapse after administration of initial ECT
Relapse occurred significantly earlier in patients with BP than in those with MDD after the first course of ECT, indicating that BP depression is difficult to prevent through the pharmacological action of antidepressants. Paradoxically, a large proportion of MDD patients could maintain remission with a single antidepressant for at least 3 years if remission was achieved by ECT. A time threshold of one month until relapse may be a good predictor of BP diagnosis.
Although a large proportion of BP patients requires treatment with mood stabilizers to maintain remission, all patients who recovered from depression after ECT were treated with antidepressants. This may explain the earlier relapse in BP patients in the current study. The time-to-relapse may be a good indicator for predicting the prospective occurrence of manic/hypomanic episodes. Early and repetitive relapses of depressive symptoms may be an adequate milestone for predicting BP and for changing treatment strategies for maintaining remission[32].
Limitations
A major limitation of this study is that it was a naturalistic and retrospective cohort study based in a clinical setting. Diagnosis was based on the consensus of multiple psychiatrists, and the Structured Clinical Interview for DSM Disorders[33] was not performed in this study. Scales for BP, such as the Mood Disorder Questionnaire[34] and Bipolar Spectrum Diagnostic Scale [35], were not used. Although a family history of BP is one of the predictors of conversion to BP[28], a family history of BP was not analyzed.
Furthermore, the number of patients was relatively small from a single perspective, which could be a generalization bias. Retrospective clinical investigations could not perfectly exclude the ambiguity of diagnosis, because clinical diversity and flexibility are often required for the optimal treatment of patients. Comprehensive judgments are required for past clinical history and current agonizing symptoms for diagnosis such as mixed states, among others, for a diagnostic change. However, this study strictly adheres to a therapeutic strategy for maintaining remission using a single antidepressant. Thus, the current results ensure novelty in detecting the margin of antidepressant maintenance therapy for drug-resistant depressive patients achieving remission by ECT. With such limitations, our study suggests that C/M-ECT is commonly required for patients initially diagnosed with MDD, and the diagnosis was subsequently changed to BP. Patients diagnosed with MDD who are unable to continue using antidepressants after remission with ECT and relapse and require C/M-ECT may have BP. C/M-ECT with an antidepressant plus lithium prevents both BP and MDD relapses; however, it may have several side effects and lead to a lost opportunity for validating the diagnosis for remission.
CONCLUSION
Appropriate withdrawal from C/M-ECT and multiple dosing regimens contribute to improvements in the quality of life of patients and the suppression of medical and social welfare costs. It may be reasonable that changes from the treatment of MDD to BP can be considered for patients who experience a relapse within one month after the course of ECT, even if they do not have a manic/hypomanic episode. The development of a method to predict manic/hypomanic episodes can prevent the exacerbation of MDD and overtreatment to maintain the remission of MDD after the initial ECT.
ARTICLE HIGHLIGHTS
Research background
Certain proportions of depressed patients relapse after electroconvulsive therapy (ECT), and it is important to explore ways to maintain remission.
Research motivation
Since 2001, when Sackeim reported on the addition of lithium to antidepressants for maintenance treatment after ECT, only symptomatic measures, such as continuation of continuation and/or maintenance ECT (C/M-ECT) have been proposed, and there have been no new findings leading to a fundamental solution for more than 20 years.
Research objectives
The objective of our study was to investigate the diagnostic factors and treatment strategies associated with the relapse of depression.
Research methods
We analyzed the relationships between relapse, the diagnostic change from major depressive disorder (MDD) to bipolar disorder (BP), and treatment strategies after the initial administration of ECT. We performed a 3-year retrospective cohort study on the prognosis of 85 patients at the Shiga University of Medical Science Hospital. The relative risk of relapse of depressive symptoms was calculated based on the diagnostic changes from MDD to BP. A receiver operating characteristic (ROC) curve was generated to evaluate the accuracy of predicting diagnostic changes from MDD to BP based on the duration between the first course of ECT and the relapse of depressive symptoms.
Research results
Compared with the MDD participants, a greater proportion of BP participants experienced relapse and required continuation and/or maintenance ECT for maintaining remission. The duration from the first course of ECT to relapse was shorter for the BP than the MDD patients.
Research conclusions
Instead of repeating treatment for MDD, such as C/M-ECT with antidepressants without definitive evidence of resolution, patients who relapse after ECT and maintenance with antidepressants may benefit from changing the maintenance treatment after remission with C/M-ECT to the treatment for BP depression, which includes mood stabilizers without antidepressants.
Research perspectives
It is also necessary to develop a method for predicting the occurrence of manic episodes to prevent the exacerbation of MDD, as well as overtreatment for maintaining the remission of severe MDD after initial ECT.
ACKNOWLEDGEMENTS
We thank the staff at the Department of Psychiatry, Shiga University of Medical Science, for their assistance. We thank Prof. Kutsumi and Mr. Momokawa from the Center for Clinical Research and Advanced Medicine, Shiga University of Medical Science, for their technical and statistical support.
Footnotes
Institutional review board statement: The study protocol was approved by the Shiga University of Medical Science Ethics Committee (27-178) and registered in the UMIN-CTR (UMIN000030458).
Informed consent statement: All patients provided informed consent through an opt-out methodology.
Conflict-of-interest statement: NK reports honoraria for lectures from Otsuka Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., and Janssen Pharmaceutical K.K. TI reports honoraria for lectures from Otsuka Pharmaceutical Co., Ltd., Yoshitomiyakuhin Corporation, Lundbeck Japan K.K., and Janssen Pharmaceutical K.K.; honoraria for manuscript writing from Kitaohji Syobo, Maruzen Publishing Co., Ltd., and SEIKAISHA Ltd. KK reports grants from Otsuka Pharmaceutical Co., Ltd., Meiji Seika Pharma Co., Ltd., MSD K.K., Eisai Co., Ltd., Takeda Pharmaceutical Co., Ltd., Pfizer Jaoan Inc., Shionogi Pharma Co., Ltd., Mitsubishi-Tanabe Pharma Corporation, Tsumura and Co., and Kao Corporation, and honoraria for lectures from Meiji Seika Pharma Co., Ltd., Eli Lilly Japan K.K., Eisai Co., Ltd., MSD K.K., Yoshitomiyakuhin Corporation, Tsumura and Co., and Takeda Pharmaceutical Co., Ltd. H.K. is associated with a laboratory that is supported by donations from Fukuda Lifetech Co., Ltd., Fukuda Life Tech Keiji Co., Ltd., Tanaka Sleep Clinic, Akita Sleep Clinic, and AiAi Care Co., Ltd., Shiga University of Medical Science. H.K. received grants from Eisai Co., Ltd., and Merck Sharp and Dohme Corp/MSD K.K. (Investigator-Initiated Studies Program). HK reports honoraria for lectures from Eisai Co., Ltd., Nobelpharma Co., Ltd. Shiga prefecture, honoraria for manuscript writing from Nipponrinsyosya Co., Ltd., Life Science, and Asakura Publishing Co., Ltd., and consulting fees from Takeda Pharmaceutical Co., Ltd. Grants and personal fees from companies are not directly related to this study. The opinions expressed in this paper are those of the authors and do not necessarily represent those of companies including Merck Sharp and Dohme Corp/MSD K.K. The other authors declare no conflicts of interest.
STROBE statement: The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: The Japanese Society of Psychiatry and Neurology, 21270.
Peer-review started: March 28, 2021
First decision: July 15, 2021
Article in press: August 30, 2021
Specialty type: Psychiatry
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chakrabarti S S-Editor: Wang LL L-Editor: A P-Editor: Guo X
Contributor Information
Naoki Kurimoto, Department of Psychiatry, Shiga University of Medical Science, Otsu 520-2192, Shiga, Japan; Department of Psychiatry, Shigasato Hospital, Otsu 520-0006, Shiga, Japan.
Takahiko Inagaki, Department of Psychiatry, Shiga University of Medical Science, Otsu 520-2192, Shiga, Japan; Department of Psychiatry, Biwako Hospital, Otsu 520-0113, Shiga, Japan.
Takashi Aoki, Department of Psychiatry, Shiga University of Medical Science, Otsu 520-2192, Shiga, Japan; Department of Psychiatry, Shiga Hachiman Hospital, Omihachiman 523-8503, Shiga, Japan.
Hiroshi Kadotani, Department of Psychiatry, Shiga University of Medical Science, Otsu 520-2192, Shiga, Japan. kadotanisleep@gmail.com; Department of Sleep and Behavioral Sciences, Shiga University of Medical Science, Otsu 520-2192, Shiga, Japan.
Fujiki Kurimoto, Department of Psychiatry, Shigasato Hospital, Otsu 520-0006, Shiga, Japan.
Kenichi Kuriyama, Department of Psychiatry, Shiga University of Medical Science, Otsu 520-2192, Shiga, Japan; Department of Sleep-Wake Disorders, National Institute of Mental Health, National Center of Neurology and Psychiatry, Kodaira 187-8502, Tokyo, Japan.
Naoto Yamada, Department of Psychiatry, Shiga University of Medical Science, Otsu 520-2192, Shiga, Japan.
Yuji Ozeki, Department of Psychiatry, Shiga University of Medical Science, Otsu 520-2192, Shiga, Japan.
Data sharing statement
The datasets analyzed in the current study are available from the corresponding author upon reasonable request at kadotanisleep@gmail.com.
References
- 1.Luan D, Zhao MG, Shi YC, Li L, Cao YJ, Feng HX, Zhang ZJ. Mechanisms of repetitive transcranial magnetic stimulation for anti-depression: Evidence from preclinical studies. World J Psychiatry. 2020;10:223–233. doi: 10.5498/wjp.v10.i10.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landry M, Lafrenière S, Patry S, Potvin S, Lemasson M. The clinical relevance of dose titration in electroconvulsive therapy: A systematic review of the literature. Psychiatry Res. 2020;294:113497. doi: 10.1016/j.psychres.2020.113497. [DOI] [PubMed] [Google Scholar]
- 3.Guideline committee for affective disorders in the Japanese Society of Mood Disorders. Treatment guideline for major depressive disorders by the Japanese Society of Mood Disorders. Tokyo: Japanese Society of Mood Disorders, 2016. [cited 28 February 2021]. Available from: https://www.secretariat.ne.jp/jsmd/iinkai/katsudou/data/20190724-02.pdf .
- 4.American Psychiatric Association. American Psychiatric Association Practice Guidelines for the Treatment of Psychiatric Disorders: Compendium 2006. Arlington: American Psychiatric Publishing, Inc., 2006. [Google Scholar]
- 5.Khalid N, Atkins M, Tredget J, Giles M, Champney-Smith K, Kirov G. The effectiveness of electroconvulsive therapy in treatment-resistant depression: a naturalistic study. J ECT. 2008;24:141–145. doi: 10.1097/YCT.0b013e318157ac58. [DOI] [PubMed] [Google Scholar]
- 6.UK ECT Review Group. Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet. 2003;361:799–808. doi: 10.1016/S0140-6736(03)12705-5. [DOI] [PubMed] [Google Scholar]
- 7.Sackeim HA, Haskett RF, Mulsant BH, Thase ME, Mann JJ, Pettinati HM, Greenberg RM, Crowe RR, Cooper TB, Prudic J. Continuation pharmacotherapy in the prevention of relapse following electroconvulsive therapy: a randomized controlled trial. JAMA. 2001;285:1299–1307. doi: 10.1001/jama.285.10.1299. [DOI] [PubMed] [Google Scholar]
- 8.Prudic J, Haskett RF, McCall WV, Isenberg K, Cooper T, Rosenquist PB, Mulsant BH, Sackeim HA. Pharmacological strategies in the prevention of relapse after electroconvulsive therapy. J ECT. 2013;29:3–12. doi: 10.1097/YCT.0b013e31826ea8c4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Serra M, Gastó C, Navarro V, Torres X, Blanch J, Masana G. [Maintenance electroconvulsive therapy in elderly psychotic unipolar depression] Med Clin (Barc) 2006;126:491–492. doi: 10.1157/13086850. [DOI] [PubMed] [Google Scholar]
- 10.Petrides G, Tobias KG, Kellner CH, Rudorfer MV. Continuation and maintenance electroconvulsive therapy for mood disorders: review of the literature. Neuropsychobiology. 2011;64:129–140. doi: 10.1159/000328943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown ED, Lee H, Scott D, Cummings GG. Efficacy of continuation/maintenance electroconvulsive therapy for the prevention of recurrence of a major depressive episode in adults with unipolar depression: a systematic review. J ECT. 2014;30:195–202. doi: 10.1097/YCT.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 12.Elias A, Phutane VH, Clarke S, Prudic J. Electroconvulsive therapy in the continuation and maintenance treatment of depression: Systematic review and meta-analyses. Aust N Z J Psychiatry. 2018;52:415–424. doi: 10.1177/0004867417743343. [DOI] [PubMed] [Google Scholar]
- 13.Ratheesh A, Davey C, Hetrick S, Alvarez-Jimenez M, Voutier C, Bechdolf A, McGorry PD, Scott J, Berk M, Cotton SM. A systematic review and meta-analysis of prospective transition from major depression to bipolar disorder. Acta Psychiatr Scand. 2017;135:273–284. doi: 10.1111/acps.12686. [DOI] [PubMed] [Google Scholar]
- 14.Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, Keller M, Warshaw M, Clayton P, Goodwin F. Switching from 'unipolar' to bipolar II. An 11-year prospective study of clinical and temperamental predictors in 559 patients. Arch Gen Psychiatry. 1995;52:114–123. doi: 10.1001/archpsyc.1995.03950140032004. [DOI] [PubMed] [Google Scholar]
- 15.Xiang YT, Zhang L, Wang G, Hu C, Ungvari GS, Dickerson FB, Kilbourne AM, Si TM, Fang YR, Lu Z, Yang HC, Lai KY, Lee EH, Hu J, Chen ZY, Huang Y, Sun J, Wang XP, Li HC, Zhang JB, Chiu HF. Sociodemographic and clinical features of bipolar disorder patients misdiagnosed with major depressive disorder in China. Bipolar Disord. 2013;15:199–205. doi: 10.1111/bdi.12052. [DOI] [PubMed] [Google Scholar]
- 16.Angst J, Azorin JM, Bowden CL, Perugi G, Vieta E, Gamma A, Young AH BRIDGE Study Group. Prevalence and characteristics of undiagnosed bipolar disorders in patients with a major depressive episode: the BRIDGE study. Arch Gen Psychiatry. 2011;68:791–798. doi: 10.1001/archgenpsychiatry.2011.87. [DOI] [PubMed] [Google Scholar]
- 17.Sharma V, Khan M, Smith A. A closer look at treatment resistant depression: is it due to a bipolar diathesis? J Affect Disord. 2005;84:251–257. doi: 10.1016/j.jad.2004.01.015. [DOI] [PubMed] [Google Scholar]
- 18.Inoue T, Nakagawa S, Kitaichi Y, Izumi T, Tanaka T, Masui T, Kusumi I, Denda K, Koyama T. Long-term outcome of antidepressant-refractory depression: the relevance of unrecognized bipolarity. J Affect Disord. 2006;95:61–67. doi: 10.1016/j.jad.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 19.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association, 1994. [Google Scholar]
- 20.HAMILTON M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Institute for Clinical Excellence. Guidance on the Use of Electroconvulsive Therapy. Technology Appraisal Guidance 59. [cited 28 February 2021]. Available from: https://www.nice.org.uk/guidance/ta59 . 2003.
- 22.Sackeim HA, Dillingham EM, Prudic J, Cooper T, McCall WV, Rosenquist P, Isenberg K, Garcia K, Mulsant BH, Haskett RF. Effect of concomitant pharmacotherapy on electroconvulsive therapy outcomes: short-term efficacy and adverse effects. Arch Gen Psychiatry. 2009;66:729–737. doi: 10.1001/archgenpsychiatry.2009.75. [DOI] [PubMed] [Google Scholar]
- 23.Kellner CH, Knapp RG, Petrides G, Rummans TA, Husain MM, Rasmussen K, Mueller M, Bernstein HJ, O'Connor K, Smith G, Biggs M, Bailine SH, Malur C, Yim E, McClintock S, Sampson S, Fink M. Continuation electroconvulsive therapy vs pharmacotherapy for relapse prevention in major depression: a multisite study from the Consortium for Research in Electroconvulsive Therapy (CORE) Arch Gen Psychiatry. 2006;63:1337–1344. doi: 10.1001/archpsyc.63.12.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McInerney SJ, Kennedy SH. Review of evidence for use of antidepressants in bipolar depression. Prim Care Companion CNS Disord. 2014;16 doi: 10.4088/PCC.14r01653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bowden CL, Perlis RH, Thase ME, Ketter TA, Ostacher MM, Calabrese JR, Reilly-Harrington NA, Gonzalez JM, Singh V, Nierenberg AA, Sachs GS. Aims and results of the NIMH systematic treatment enhancement program for bipolar disorder (STEP-BD) CNS Neurosci Ther. 2012;18:243–249. doi: 10.1111/j.1755-5949.2011.00257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomas RK, White PJ, Dursun S. Treating electroconvulsive therapy-induced mania with more electroconvulsive therapy: Evidence for electroconvulsive therapy as the ultra-mood stabilizer. SAGE Open Med Case Rep. 2018;6:2050313X18799236. doi: 10.1177/2050313X18799236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee J, Arcand L, Narang P, Lippmann S. ECT-induced Mania. Innov Clin Neurosci. 2014;11:27–29. [PMC free article] [PubMed] [Google Scholar]
- 28.Kessing LV, Willer I, Andersen PK, Bukh JD. Rate and predictors of conversion from unipolar to bipolar disorder: A systematic review and meta-analysis. Bipolar Disord. 2017;19:324–335. doi: 10.1111/bdi.12513. [DOI] [PubMed] [Google Scholar]
- 29.Farahani A, Correll CU. Are antipsychotics or antidepressants needed for psychotic depression? J Clin Psychiatry. 2012;73:486–496. doi: 10.4088/JCP.11r07324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arandjelovic K, Eyre HA, Lavretsky H. Clinicians' Views on Treatment-Resistant Depression: 2016 Survey Reports. Am J Geriatr Psychiatry. 2016;24:913–917. doi: 10.1016/j.jagp.2016.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Itagaki K, Takebayashi M, Shibasaki C, Kajitani N, Abe H, Okada-Tsuchioka M, Yamawaki S. Factors associated with relapse after a response to electroconvulsive therapy in unipolar vs bipolar depression. J Affect Disord. 2017;208:113–119. doi: 10.1016/j.jad.2016.08.047. [DOI] [PubMed] [Google Scholar]
- 32.Sugawara H, Sakamoto K, Harada T, Ishigooka J. Predictors of efficacy in lithium augmentation for treatment-resistant depression. J Affect Disord. 2010;125:165–168. doi: 10.1016/j.jad.2009.12.025. [DOI] [PubMed] [Google Scholar]
- 33.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders SCID-I: Clinician Version, Administration Booklet. American Psychiatric Publishing, Inc., 1997. [Google Scholar]
- 34.Hirschfeld RM, Williams JB, Spitzer RL, Calabrese JR, Flynn L, Keck PE Jr, Lewis L, McElroy SL, Post RM, Rapport DJ, Russell JM, Sachs GS, Zajecka J. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000;157:1873–1875. doi: 10.1176/appi.ajp.157.11.1873. [DOI] [PubMed] [Google Scholar]
- 35.Nassir Ghaemi S, Miller CJ, Berv DA, Klugman J, Rosenquist KJ, Pies RW. Sensitivity and specificity of a new bipolar spectrum diagnostic scale. J Affect Disord. 2005;84:273–277. doi: 10.1016/S0165-0327(03)00196-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed in the current study are available from the corresponding author upon reasonable request at kadotanisleep@gmail.com.