Abstract
Aims
During the early months of the U.S. COVID-19 outbreak, women suffered disproportionate burdens of pandemic-related psychological and economic distress. We aimed to describe the experiences of women in substance use disorder (SUD) recovery programs by (1) exploring the pandemic's impact on their lives, sobriety, and recovery capital and (2) tracking COVID-19 perceptions and preventative behaviors.
Methods
We conducted monthly semistructured interviews with women in residential and outpatient SUD recovery programs in Kansas City in April, May, and June 2020. Participants described the pandemic's impact on their life and sobriety and completed survey items on factors related to COVID-19 preventative behaviors. We interpreted qualitative themes longitudinally alongside quantitative data.
Results
In 64 interviews, participants (n = 24) described reduced access to recovery capital, or resources that support sobriety, such as social relationships, housing, employment, and health care. Most experienced negative impacts on their lives and feelings of stability in March and April but maintained sobriety. Four women described relapse, all attributed to pandemic stressors. Participants described relief related to societal re-opening in May and June, and increased engagement with their communities, despite rising infection rates.
Conclusions
For women recovering from SUDs during COVID-19, securing recovery capital often meant assuming greater COVID-19 risk. As substance use appeared to have increased during the pandemic and COVID-19 transmission continues, public health planning must prioritize adequate and safe access to recovery capital and timely distribution of vaccines to people struggling with SUDs.
Keywords: COVID-19, Substance use disorders, Substance use recovery, Sobriety, Women, U.S., Mixed-methods, Phenomenology, Recovery capital
1. Introduction
On the backdrop of societal disruption, economic slowdown, and climbing infection risk, more than 90% of U.S. adults surveyed in May 2020 reported experiencing moderate or severe negative emotional impacts of the COVID-19 pandemic (Palsson, Ballou, & Gray, 2020). The pandemic has disproportionately affected women, who account for 56% of the almost 20 million jobs lost from February to May 2020 (Ewing-Nelson, 2020). Compared to men, women reported higher rates of pandemic-related, negative changes in sleep, productivity, mood, worries about health, and frustrations with not being able to do what they usually enjoy doing (Palsson et al., 2020). Women under age 50 reported more overall emotional impact from COVID-19 than their male counterparts. Studies have also demonstrated that women were more likely to increase alcohol consumption during the early stages of the pandemic, due to their disproportionate psychological stress (Neill et al., 2020; Rodriguez, Litt, & Stewart, 2020).
Women in treatment for substance use disorders (SUDs) face unique direct and indirect challenges from COVID-19 (Volkow, 2020). Because poor respiratory health is a common comorbidity of SUDs, this population may be especially susceptible to poor outcomes from COVID-19 infection. Moreover, recovery from SUDs is most successful with abundant recovery capital, or resources that facilitate and sustain recovery including social support, employment, health care, and an overall sense of meaning and purpose in life (Hennessy, 2017; A.B. Laudet, Becker, & White, 2009; A.B. Laudet & White, 2008). Experts postulate that pandemic-related social isolation, economic and housing instability, and disruption to SUD treatment and support networks could contribute to decreased well-being and increase risks for relapse (Volkow, 2020).
As the pandemic persists in the United States, prolonged population-level psychological distress may increase demand for effective SUD treatment and recovery services. Meeting this demand will require research that offers empirical, in-depth understanding of how the pandemic has shaped the experience of SUD recovery, particularly in vulnerable subgroups such as women. Yet, to date, this research is scarce. In one Dutch study, 15 men and women in SUD treatment or recovery completed a single interview in March–May 2020 (DeJong, Verhagen, Pols, Verbrugge, & Baldacchino, 2020). Participants overwhelmingly reported negative feelings such as guilt, gloom, fear, panic, restlessness, and stress as well as reduced feelings of connectedness to health care and support groups. Those new into recovery expressed concerns about relapsing.
A deeper, longitudinal understanding of the unique experiences of U.S. women navigating SUD recovery during the pandemic is essential to optimizing SUD recovery efforts while ensuring COVID-19 infection control. We sought to understand the experiences of women who faced the early months of COVID-19 after having recently initiated SUD recovery. Specifically, we aimed to longitudinally characterize (1) the pandemic's impact on life, sobriety, and recovery capital among this population; and (2) participants' COVID-19 risk perceptions and self-efficacy for practicing protective behaviors.
2. Methods
We conducted a longitudinal interview study from April to June 2020. Our study was guided by mixed-methods phenomenology (Mayoh & Onwuegbuzie, 2015), which applies qualitative and quantitative methods to generate in-depth understanding of a lived experience (in this case, recovering from SUDs in the early months of the U.S. COVID-19 epidemic).
2.1. Setting and participants
In February and early March 2020, we recruited 31 participants from three recovery centers (two residential and one outpatient program) in Kansas City, Missouri, to participate in an interrupted time series study aimed at increasing access to contraception. Recovery centers provided services for any type of substance or alcohol use disorder, most commonly polysubstance use disorders that included methamphetamines or opioids. The study enrolled participants in the usual care (no intervention) period if they met these eligibility criteria: aged 18–40 years, able to become pregnant, not using hormonal contraception (i.e., subdermal implant, intrauterine device, injectable, pill, patch, or ring).
2.2. Procedure and measures
When stay-at-home orders suspended the original study in mid-March, we invited women to participate in longitudinal COVID-19 interviews. Of the original 31 enrolled participants, we successfully contacted 24 by phone (representing one residential and one outpatient program), who all consented to participate. All participants had completed a computerized baseline questionnaire at original enrollment, which included demographics, history of substance use (Alcohol, Smoking and Substance Use Involvement Screening Test [ASSIST; Ali et al., 2002; Humeniuk et al., 2008]) and measures on reproductive health and contraception use (Centers for Disease Control and Prevention & National Center for Health Statistics, 2014). As all participants were enrolled in the parent study's usual care period, none received any intervention. The parent study remained in suspension for the duration of the COVID-19 interviews (i.e., no additional enrollment nor intervention activities occurred).
Participants completed three semistructured phone interviews at one-month intervals starting in April, approximately one month after Kansas City issued stay-at-home orders. The city lifted stay-at-home orders and instigated a phased re-opening plan in mid-May, coinciding with participants' second interview. By the final interview in mid-June, the city had permitted businesses to open at 50% capacity (City of Kansas City Missouri, 2020). Over this time, both recovery centers had moved to virtual sessions. The residential program followed local stay-at-home orders, permitting women to leave only for work or essential needs.
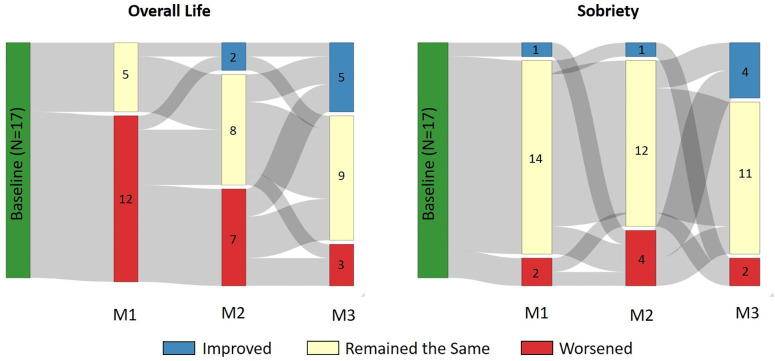
For each 10–20-minute interview, study staff trained in qualitative interviewing asked women a series of questions with the stem, “In the last month, how has COVID-19 affected your…” for topics of overall life, future plans, sobriety, social relationships, job or income, and access to health care. Participants then rated their level of agreement with statements adapted from Timpka and colleagues' study on intentions to perform nonpharmaceutical preventative behaviors during influenza outbreaks (Timpka et al., 2014). Based on protection motivation theory and the health belief model, these measures assessed perceived susceptibility and severity of infection, trust in information, and self-efficacy to perform protective behaviors (e.g. hand-washing, staying home, and avoiding close social contact or public transport; see Fig. 2 for full list of items). Participants responded on a 5-point Likert scale (ranging from “strongly disagree” to “strongly agree”) and study staff invited participants to provide qualitative comments elaborating on their response. In the final interview, participants repeated the ASSIST items, and those who reported any use of substances, not including tobacco, were determined to have relapsed. Participants received $20 for completion of the baseline survey, $15 for the one-month and two-month follow-up and $20 for the three-month follow-up. Study staff transcribed all responses into REDCap© simultaneously or audio-recorded the interviews and transcribed them immediately after the interview. We kept participants' responses separate from their name and contact information and did not share this information with anyone outside the research team. The Institutional Review Board at Children's Mercy Kansas City approved all study methods.
Fig. 2.
COVID-19 attitudes, beliefs, and preventative behaviors among women recovering from SUD (n = 17).
Caption: 1 m interviews = mid-March through mid-April; 2 m interviews = mid-April through mid-May; 3 m interviews = mid-May to mid-June. Analysis conducted on women who completed all three interviews (n = 17).
2.3. Data analysis
We summarized quantitative data descriptively with SAS version 9.4 (SAS Institute Cary, North Carolina, USA). We created data visualizations to examine longitudinal trends among participants who completed all three interviews in R Studio version 1.2.5 with R version 3.6.1. We then performed qualitative analysis in Dedoose version 8.3.35 and began with structural coding to categorize responses by domains explored in the original interview guide (Saldaña, 2015). For domains of overall life and sobriety, we also performed evaluation coding, assigning values to indicate if responses revealed negative change (−1), neutral/no change (0), or positive change (1) from the previous month (Saldaña, 2015). Independent raters double-coded data from one-third of the participants completing all three months and resolved discrepancies through group consensus. We then conducted line-by-line inductive coding, and through periodic debriefing and investigator triangulation, constructed and applied a hierarchical, thematic codebook throughout the dataset. We synthesized data in each domain using Dedoose matrices and coding outputs that allowed examination of thematic data by domain, month, and participant characteristics. We present results as synthesized themes or frequencies of reported experiences, where appropriate (Sandelowski, 2001).
3. Results
3.1. Participant characteristics
We conducted 64 total interviews: 23 in April, 22 in May, and 19 in June 2020. Twenty-four women completed at least one interview, and 17 completed interviews in all three months (see Table 1 ). Women who did not complete a scheduled interviewed are those who did not respond to three attempts at contact. Women were between ages 22 and 38 (median 29), predominately white (79.2%), non-Hispanic (87.5%), and with at least a high school diploma (62.4%). Seventeen (70.8%) had at least one living child, and of these, 12 (70.6%) reported their children living in foster care or with someone else at some point. Three-quarters reported their marital status as single and 16.7% as separated.
Table 1.
Characteristics of female participants from two Midwestern recovery centers (n = 24).
| Participants completing all three interviews (n = 17) | Participants completing one or two interviews (n = 7) | Total (n = 24) |
|
|---|---|---|---|
| Demographics | |||
| Median age in years (IQR) | 30.0 (28.0, 33.0) | 28.0 (26.0, 32.0) | 29.0 (27.0, 32.5) |
| Race | |||
| White | 13 (76.5%) | 6 (85.7%) | 19 (79.2%) |
| American Indian/ Alaska Native | 1 (5.9%) | 1 (14.3%) | 2 (8.3%) |
| Other | 3 (17.6%) | 0 (0.0%) | 3 (12.5%) |
| Ethnicity | |||
| Non-Hispanic | 14 (82.4%) | 7 (100%) | 21 (87.5%) |
| Hispanic/Latina | 3 (17.6%) | 0 (0.0%) | 3 (12.5%) |
| Educational level | |||
| Eighth grade or below | 1 (5.9%) | 0 (0.0%) | 1 (4.2%) |
| Some high school | 6 (35.3%) | 2 (28.6%) | 8 (33.3%) |
| High school graduate or GED | 7 (41.2%) | 4 (57.1%) | 11 (45.8%) |
| Post-high school training/some college | 2 (11.8%) | 0 (0.0%) | 2 (8.3%) |
| Undergraduate degree | 1 (5.9%) | 1 (14.3%) | 2 (8.3%) |
| Marital status | |||
| Single-never married | 12 (70.6%) | 6 (85.7%) | 18 (75.0%) |
| Separated | 4 (23.5%) | 0 (0.0%) | 4 (16.7%) |
| Married/domestic partnership | 1 (5.9%) | 0 (0.0%) | 1 (4.2%) |
| Divorced | 0 (0.0%) | 1 (14.3%) | 1 (4.2%) |
| Number of children | |||
| 0 | 4 (23.5%) | 3 (42.9%) | 7 (29.2%) |
| 1 | 5 (29.4%) | 2 (28.6%) | 7 (29.2%) |
| 2 | 3 (17.6%) | 2 (28.6%) | 5 (20.8%) |
| 3 or more | 5 (29.4%) | 0 (0.0%) | 5 (20.8%) |
| Child has lived in foster care/with someone else because participant was told that child could not stay with her (% among women with children) | 9 (69.2%) | 3 (75.0%) | 12 (70.6%) |
| Living location (prior to entry into recovery) | |||
| Urban | 6 (35.3%) | 3 (42.9%) | 9 (37.5%) |
| Rural | 4 (23.5%) | 2 (28.6%) | 6 (25.0%) |
| Suburban | 4 (23.5%) | 2 (28.6%) | 6 (25.0%) |
| Prefer not to answer | 3 (17.6%) | 0 (0.0%) | 3 (12.5%) |
| Substance use, recovery, and relapse | |||
| Recovery program | |||
| Site 1: Outpatient | 9 (52.9%) | 5 (71.4%) | 14 (58.3%) |
| Site 2: Residential | 8 (47.1%) | 2 (28.6%) | 10 (41.7%) |
| Lifetime experience with substance use | |||
| Amphetamines | 16 (94.1%) | 6 (85.7%) | 22 (91.7%) |
| Tobacco | 15 (88.2%) | 7 (100.0%) | 22 (91.7%) |
| Cannabis | 15 (88.2%) | 6 (85.7%) | 21 (87.5%) |
| Alcohol | 14 (82.4%) | 6 (85.7%) | 20 (83.3%) |
| Opioids | 10 (58.8%) | 5 (71.4%) | 15 (62.5%) |
| Cocaine | 9 (52.9%) | 5 (71.4%) | 14 (58.3%) |
| Hallucinogens | 6 (35.3%) | 5 (71.4%) | 11 (45.8%) |
| Sedatives | 5 (29.4%) | 4 (57.1%) | 9 (37.5%) |
| Inhalants | 3 (17.6%) | 1 (14.3%) | 4 (16.7%) |
| Recency of recovery status (at baseline) | |||
| Any substance use (other than tobacco) in the three months prior to baseline | 6 (35.3%) | 4 (57.14%) | 10 (41.7%) |
| No substance use (other than tobacco) in the three months prior to baseline | 11 (64.7%) | 3 (42.86%) | 14 (58.3%) |
| Relapse during study (April–June 2020) | |||
| Any substance use (other than tobacco) during study | 4 (23.5%) | Unknown | Unknown |
| Health care access (at baseline) | |||
| Health insurance | |||
| Uninsured | 11 (64.7%) | 5 (71.4%) | 16 (66.7%) |
| Public | 3 (17.6%) | 1 (14.3%) | 4 (16.7%) |
| Private | 1 (5.9%) | 1 (14.3%) | 2 (8.3%) |
| Prefer not to answer | 2 (11.8%) | 0 (0.0%) | 2 (8.3%) |
| Participant had time within past 12 months when she thought she should get medical care, but did not | |||
| No | 8 (47.1%) | 3 (42.9%) | 11 (45.8%) |
| Yes | 8 (47.1%) | 4 (57.1%) | 12 (50.0%) |
| Don't remember | 1 (5.9%) | 0 (0.0%) | 1 (4.2%) |
| Sexual health (at baseline) | |||
| Number of current male sexual partners | |||
| 0 | 5 (29.4%) | 1 (14.3%) | 9 (37.5%) |
| 1 | 11 (64.7%) | 4 (57.1%) | 13 (54.2%) |
| 2 or more | 1 (5.9%) | 2 (28.6%) | 2 (8.3%) |
| Condom use during last vaginal or anal sex | |||
| No | 13 (76.5%) | 5 (71.4%) | 18 (75.0%) |
| Yes | 4 (23.5%) | 2 (28.6%) | 6 (25.0%) |
Women were receiving recovery services at either a residential (41.7%) or outpatient (58.3%) facility. Though the study did not explicitly ask women in the outpatient program where they resided, half mentioned living in another transitional facility or halfway house. Women most commonly reported lifetime use of these substances: amphetamines (91.7%), cannabis (87.5%), tobacco (91.7%), alcohol (83.3%), opioids (62.5%), and cocaine (58.3%). At baseline, all 24 participants were in recovery (not currently using any substance other than tobacco), and 14 (58.3%) were three or more months into their recovery. By the end of the three-month study period, 4 of the 17 women who completed all three interviews had reported relapse (three with multiple substances, one with alcohol).
Most women had no health insurance (66.7%) and half said there was a time they thought they should have accessed health care in the last 12 months but did not. Most (62.5%) reported at least one current male sexual partner and three-quarters reported no condom/contraception use at last sexual encounter.
3.2. Impact of life and sobriety
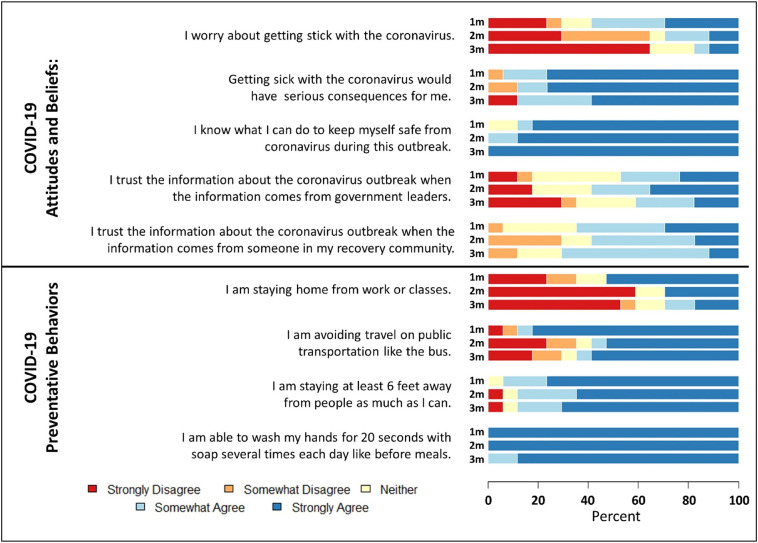
Fig. 1 illustrates month-by-month evaluation coding of responses to “How has COVID-19 affected your overall life in the last month?” and “How has COVID-19 affected your sobriety in the last month?” as indicating improvement, worsening, or remaining constant.
Fig. 1.
Month-by-month impact of COVID-19 on overall life and sobriety among women recovering from SUD (n = 17).
Caption: Qualitative responses to “In the last month, how has COVID-19 affected your life?” and “In the last month, how has COVID-19 affected your sobriety?” were coded as “improved”, “remained the same” or “worsened.” Analysis conducted on women who completed all three interviews (n = 17).
3.2.1. Impact on life
In April, participants overwhelmingly felt their life had worsened due to COVID-19 (Fig. 1). Participants felt like “everything is on standstill” (age 28, April) and the pandemic had interrupted or set them back on progress toward independent, stable living, and caused significant mental health struggles for many.
“I really can't think about my future right now. If I think about all that right now, I will relapse and I just need to take it one day at a time.”
(age 22, April)
“[The pandemic] has affected me pretty heavily. I developed a lot of stress and anxiety. My entire life has been disrupted because of this.”
(age 28, April)
Participants' reports of loss of recovery capital was most profound in April, particularly with reduced access to social networks, delayed plans in housing transitions, and for some, reduction in employment/income. Of the 23 women who we interviewed in April, eight had lost their job or were furloughed, three had their work hours reduced, five remained out of work, and just seven had maintained pre-pandemic employment. Women in residential programs expressed feelings of being shut away, while those in outpatient programs faced increased stress navigating the changed world.
“Everything was getting on track. I had a job that was going to pay me enough and it was rolling just right and then all this happened and it came to a complete stop.”
(age 31, April)
“Well [my job] laid me off from work and [COVID] got us here at [our residential facility]. So we really can't do anything. We don't have meetings anymore so our support went down. […] And we can't go find jobs because we are stuck here and can't leave.”
(age 30, April)
May brought signs of adaptation to pandemic-related adversities. Compared to April, more women in May suggested a neutral or even positive change in response to “Since we last spoke, how has COVID affected your life?” Though many held frustrations with delayed short-term plans or long-term goals, some found hope in the prospect of societal reopening, personal lifestyle adaptations, and new opportunities.
“I hate to say this because I know the virus is bad but it's kinda helped. I'm working so much to get a car and a place, it's helping me save up money.”
(age 30, May)
By June, 15 of the 17 women interviewed reported improvement or consistency in their lives as “things are opening back up” (age 29, June). Women sounded more positive as they spoke of relief (frequently using the expression “finally!”), a renewed hope, and momentum toward future goals.
“I finally got to see my kids for four days last week […] I now get to see my family and it's become easier now with everything else that has opened up. I am not nearly as depressed now that I can see my family and I can travel to go see them and it has been a lot better.”
(age 36, June)
“Hopefully [in the future I will be] done with treatment, with a job. I want to eventually start my own business.”
(age 28, June)
3.2.2. Impact on sobriety
Despite changes and challenges in their lives, 13 of the 17 women completing the study reported remaining sober throughout the three months. Sobriety experiences did not show apparent trends by month. However, as Fig. 1 illustrates, five women reported both improving and worsening experiences with sobriety throughout the study, reflecting the often cyclical nature of recovery. Each of the four women who reported relapse during the study indicated contributions of COVID-related stressors.
"I did relapse. I feel horrible. I blame it on myself and I am just so depressed since they shut treatment down and everything. I can't really do anything [treatment] online because my probation got suspended and I am not supposed to have contact with anyone."
(age 26, April)
Of the women who stayed sober, six described increased difficulty abstaining, citing boredom (“being inside all the time makes you want to use” [age 28, April]), reduced in-person support, or peers who had relapsed. On the other hand, one participant cited COIVD-19 as additional motivation to quit tobacco. In each month, 73–83% of participants reported continuing recovery classes or support groups virtually. While many cited limitations (“it feels less personal” [age 28, June]), they attributed treatment continuity as key to remaining sober.
"There have been some moments where I really wanted to [drink] but I didn't. I am still talking to my case manager and counselor. […] We are starting classes on zoom which I think is great because it will keep us connected and motivated. The internet is a great thing when used appropriately. For me the most important thing is to stay surrounded with positive people and keep reaching out to people. Once I stop keeping in touch, I will start drinking again."
(age 26, April)
Some women in residential programs attributed built-in support as crucial to maintaining sobriety through stay-at-home orders.
"It has been nice living with other girls. We have gotten close. The girls are here for the same reason I am, and we have a good group of people that are focused on what we are here to do and that is to live a better life."
(age 36, April)
3.3. Impact on recovery capital
Participants' lives and experiences with sobriety were shaped by the unique ways in which COVID-19 affected their recovery capital. Table 2 summarizes key themes and trends in negative, positive, and adaptive experiences with social relationships, income/employment, housing, and health care.
Table 2.
Qualitative findings of experiences with recovery capital among women in SUD recovery through COVID-19 (March–June 2020).
| Recovery capital domain | Key themes and trends (+) = positive or adaptive experience (−) = negative experience |
Illustrative quotes (age of participant, month of interview) |
|---|---|---|
| Social Relationships |
|
|
|
|
|
|
|
|
|
|
|
| Income and Employment |
|
|
|
|
|
|
|
|
| Housing |
|
|
|
|
|
| Health care |
|
|
|
|
|
|
|
|
|
|
|
|
|
Participants considered social relationships as key to recovery. Thus, reduced access to friends, partners, and family became the defining challenge of April/May, causing significant, even “devastating” effects on mental health and well-being. Mothers, who often considered their children as their primary motivation for recovery, faced barriers to accessing children not in their custody, including court delays, orders to suspend visits while working front-line jobs, or reduced ability to travel. Women did find social support through coworkers, roommates, and virtual treatment/counseling. As restrictions lifted and comfort with social interaction increased in May/June, more women reported seeing or planning to see loved ones again.
Experiences with income and employment were diverse among participants throughout the study. Starting from various points in re-establishing employment, some women reported pandemic-related job loss, decreased hours and/or difficulty finding new work due to fewer openings and residential facility lockdowns. Three were denied unemployment benefits, having not been working long enough to qualify. A few stated uncertainties about how to access benefits, particularly when social service offices were closed. Those without enough income struggled to pay for rent, food, and things their children needed. Some mentioned accessing government assistance (food stamps, CARES Act) as well as relying on family, friends, and savings. Still, many did maintain or find work, some even reporting increased hours due to demands for “essential” food service, health care, and packing/delivery jobs. Among the fourteen women who were working at baseline and who we interviewed across all three months, six maintained their employment, and five of the eight who lost their job obtained new employment by June. Those with sufficient employment felt “blessed” and “lucky,” benefiting not only from income, but increased access to health care, better prospects for permanent housing, and the accountability and structure to help maintain sobriety (“It just feels really good to be able to go back to work” [age 31, May]).
Overall, women considered independent housing the capstone of recovery. Throughout the study, most saw their living situation as stable yet transitional, at residential programs or temporary stays with friends/relatives. Particularly in April/May, women yearning for more independent living experienced frustration as transition plans became uncertain due to income loss or reduction, delays in housing assistance programs, and lockdowns and delays in transition timelines in residential programs. By June, fewer were living in residential programs (one in the residential recovery center, five in other transitional living facilities), though most participants still considered their current living situation temporary.
While not all participants sought health care during the study, most held a prevailing sense that “doctors have cancelled everything” (age 33, May). Further, transportation to appointments became difficult with reduced bus schedules. Women without insurance spoke of reduced service capacity of free clinics and difficulties trying to apply for Medicaid when they could not do so in person. These barriers amounted to missed opportunities for health care for themselves, parents and/or children. Just three women reported attending an in-person health care visit over the study period and two reported attending a telemedicine appointment outside of SUD treatment. Of the 17 women who, at baseline, reported wanting to start birth control within the next month, only two reported accessing contraception services over this entire study period, with most others citing COVID restrictions and closures as their main barriers. One participant reported an unplanned pregnancy. On the other hand, some women spoke of COVID-related adaptations that facilitated health care access, such as the ability to refill or change medications without an in-person visit.
3.4. COVID-19 perceptions and protective behaviors
Fig. 2 illustrates month-by-month Likert scale responses to questions on COVID-19 attitudes, beliefs, and preventative behaviors.
3.4.1. Perceived susceptibility and severity
In April, 56.5% of participants strongly/somewhat agreed with the statement, “I am worried about getting infected with COVID-19.” Among women completing all three interviews (N = 17), this proportion declined from April (58.8%) to June (17.6%) (Fig. 2). Those who were worried referenced rising cases and personal risks related to employment or pre-existing health conditions. Reasons for less worry included perceptions of being healthy and unlikely to get sick, having taken adequate precautions, or that the government had exaggerated the threat.
The percentage of participants who strongly/somewhat agreed that “Getting sick with COVID-19 would have serious consequences for me” was high in April (82.6%,) and remained high among those completing all three interviews (94.1% in April, 88.2% in June). Many elaborated that “severe consequences” were beyond their own physical health, including threat of isolation from children and family, or of jeopardizing their employment.
3.4.2. Trust in source of information
Consistently throughout the three months, participants were divided in the degree to which they trusted information about the pandemic coming from the government or their recovery site. Participants often mistrusted both sources, believing that recovery sites originally sourced their information from the government.
3.4.3. Self-efficacy for preventative behaviors
Women overwhelmingly felt like they had the resources and knowledge to keep themselves safe from COVID-19 as 100% strongly agreed with both statements by June interviews. However, women who completed all three interviews reported a decline in self-efficacy for all four preventative behaviors, with handwashing remaining high (100% strongly/somewhat agreeing in April, 88.2% in June) but increasing difficulties in ability to avoid public transportation (88.3% strongly/somewhat agreeing in April, 64.7% in June) and stay home from school or work (52.9% in April, 29.4% in June).
4. Discussion
From March through June 2020, women navigated SUD recovery in a society that abruptly shut and slowly reopened atop a persistently circulating novel coronavirus. In the first month, women described abrupt restriction of recovery capital and negative consequences on their life and feelings of stability. As in the general population (Holingue et al., 2020; Jean-Baptiste, Herring, Beeson, Dos Santos, & Banta, 2020), participants shared a common experience of isolation from social networks and some also experienced devastating lack of income or limited access to health care. In the second month, women began regaining access to recovery capital as the local government scaled back restrictions. By the final month, the perception of societal reopening brought women relief and renewed hope in their ability to regain the recovery capital that had been lost or threatened. Throughout the study, those who relapsed or were tempted to use again described COVID-19-related stressors as significant threats to their sobriety, though most participants were ultimately able to remain sober.
For women recovering from SUDs in the early months of the COVID-19 pandemic in the United States, accessing necessary recovery capital often involved placing themselves at increased risk of COVID-19 infection. Throughout the three months of this study, women generally felt like they knew how to protect themselves from COVID-19 and worries about contracting the virus centered less on the threat of direct physical consequences and more on the threat that a positive diagnosis would result in further restriction from recovery capital. Societal adaptations helped women to maintain some sources of recovery capital, notably, the swift transition of SUD treatment and support to virtual platforms. Yet women expressed the most hope about their lives when they had more opportunities to engage in the outside world, like serving in frontline jobs or reuniting with friends and family. Societal reopening toward the end of the study corresponded with lower worry about infection and lower self-efficacy for preventative behaviors. However, one month after the final interviews, Kansas City reported a record number of new infections and a 60% increase in COVID-19 deaths, leaving individuals seeking external recovery capital at an even greater risk of infection.
4.1. Implications
Our study showed how pandemic-related stress disrupted lives and feelings of stability for those already in recovery. However, the need for recovery support is likely growing among the general population. In June 2020, 13% of U.S. adults reported starting or increasing substance use to cope with stress or emotions related to COVID-19 (Czeisler et al., 2020) and data from the Midwest suggest a postpandemic rise in opioid overdoses (Slavova, Rock, Bush, Quesinberry, & Walsh, 2020). Considering our study only examined women in formal treatment, those struggling with SUDs or recovery who are not connected to care are likely to face further difficulties securing the support and recovery capital that they need.
Meeting the needs of people with SUDs will require public health efforts that extend beyond the walls of recovery centers. Experts believe that in general, communities and states are well-positioned to optimize SUD recovery by building recovery-oriented systems of care (ROSC), or systems of macro-level, coordinated services that promote access to recovery capital. As communities and states come together to manage COVID-19, coordinating efforts to maintain strong ROSC should be on the agenda. Strategies that ensure access to and easy navigation of social services, housing, employment, and health care in a rapidly changing world must take into account the unique needs of people with SUDs. Such strategies may include virtual platforms that link recovery communities with ROSC, as well as peer navigator programs, which have a strong evidence base for health promotion in this population (Li, Weeks, Borgatti, Clair, & Dickson-Gomez, 2012; Scott, Grella, Nicholson, & Dennis, 2018). Peers may also be vital conduits of information, given the mixed levels of trust in information coming from government sources among women in our study. COVID-19 prevention messaging tailored to people in recovery should also reaffirm their need for access to recovery capital, but with enhanced safety. Given the higher risk for severe disease as well as increased likelihood for exposure given their congregate living situations and employment in frontline jobs, governments should also prioritize people struggling with SUDs in COVID-19 vaccine distribution.
4.2. Strengths and limitations
While other work has speculated about the impact of COVID-19 on recovery from SUDs (Volkow, 2020), our study is the first to document women's direct, lived experiences using a longitudinal perspective. Our sample is limited, as it is ultimately one of convenience, as we recruited participants from an ongoing study. We also had a high loss to follow-up; most of whom were less than three months in their recovery and potentially at higher risk of relapse. Considering the variability in the pandemic response across states and municipalities, the generalizaibility of our findings to other geographical locations is limited. Finally, our smaller sample size is appropriate for phenomenological studies but does limit our ability to draw population-level inferences from our quantitative data.
5. Conclusion
Our study describes the lived experiences of women recovering from SUDs in the early months of COVID-19. Findings demonstrate how early societal restrictions and the threat of infection severed many from essential sources of recovery capital. Societal re-openings followed, resulting in relief as women reported increased engagement with recovery capital, but risked exposure to a still persistent virus. As social stresses related to COVID-19 continue to disrupt lives, women recovering from SUDs will continue to seek the resources they need to maintain sobriety. Public health planning that prioritizes safe and adequate access to health care, social support, employment, and housing for people in recovery could pay dividends for broader community-level health and lower the burden of both SUDs and COVID-19.
CRediT authorship contribution statement
Emily A. Hurley: Conceptualization, Methodology, Investigation, Formal Analysis, Writing-Original Draft, Supervision, Funding Acquisition. Kimberly Piña: Methodology, Investigation, Formal Analysis, Project Administration, Writing- Review & Editing. Victoria Cegielski: Investigation, Formal Analysis, Writing- Review & Editing. Janelle R. Noel-MacDonnell: Data Curation, Formal Analysis, Data Visualization, Writing- Review & Editing. Melissa K. Miller: Conceptualization, Methodology, Formal Analysis, Writing- Original Draft, Supervision, Funding Acquisition.
Acknowledgments
Acknowledgements
The authors express deep appreciation for the women who so openly shared their experiences with us as participants in this study. We are also grateful to our community partners who helped to facilitate the study, particularly Lori Glenski, Sarah Knopf-Amelung, Jessi Ibarra, Alyssa Ibarra, and Bobbi Jo Reed.
Funding
This study was supported in part by a research grant from Investigator-Initiated Studies Program of Merck Sharp & Dohme Corp. The opinions expressed in this paper are those of the authors and do not necessarily represent those of Merck Sharp & Dohme Corp.
References
- Ali R., Awwad E., Babor T.F., Bradley F., Butau T., Farrell M.…Vendetti J. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction. 2002 doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Health Statistics National Center for Health Statistics. 2014. https://www.cdc.gov/nchs/nsfg/index.htm
- City of Kansas City Missouri COVID-19 in KCMO. 2020. https://www.kcmo.gov/city-hall/departments/health/coronavirus
- Czeisler, M. É., Lane, R. I., Petrosky, E., Wiley, J. F., Christensen, A., Njai, R., Weaver, M. D., Robbins, R., Facer-Childs, E. R., Barger, L. K., Czeisler, C. A., Howard, M. E., & Rajaratnam, S. M. W. (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR. Morbidity and Mortality Weekly Report. doi:10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed]
- DeJong, C. A. J., Verhagen, J. G. D., Pols, R., Verbrugge, C. A. G., & Baldacchino, A. (2020). Psychological impact of the acute COVID-19 period on patients with substance use disorders: we are all in this together. Basic and Clinical Neuroscience. doi:10.32598/bcn.11.covid19.2543.1. [DOI] [PMC free article] [PubMed]
- Ewing-Nelson C. Despite Slight Gains in May, Women Have Still Been Hit Hardest by Pandemic-related Job Losses. 2020. https://nwlc.org/wp-content/uploads/2020/06/May-Jobs-FS.pdf
- Hennessy E.A. Recovery capital: A systematic review of the literature. Addiction Research and Theory. 2017;25(5):349–360. doi: 10.1080/16066359.2017.1297990. [DOI] [Google Scholar]
- Holingue C., Kalb L.G., Riehm K.E., Bennett D., Kapteyn A., Veldhuis C.B.…Thrul J. Mental distress in the United States at the beginning of the COVID-19 pandemic. American Journal of Public Health. 2020 doi: 10.2105/ajph.2020.305857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humeniuk R., Ali R., Babor T.F., Farrell M., Formigoni M.L., Jittiwutikarn J.…Simon S. Validation of the alcohol, smoking and substance involvement screening test (ASSIST) Addiction. 2008 doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- Jean-Baptiste C.O., Herring R.P., Beeson W.L., Dos Santos H., Banta J.E. Stressful life events and social capital during the early phase of COVID-19 in the U.S. Social Sciences & Humanities Open. 2020 doi: 10.1016/j.ssaho.2020.100057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet A.B., Becker J.B., White W.L. Don’t wanna go through that madness no more: Quality of life satisfaction as predictor of sustained remission from illicit drug misuse. Substance Use & Misuse. 2009 doi: 10.1080/10826080802714462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet A.B., White W.L. Recovery capital as prospective predictor of sustained recovery, life satisfaction, and stress among former poly-substance users. Substance Use & Misuse. 2008 doi: 10.1080/10826080701681473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Weeks M.R., Borgatti S.P., Clair S., Dickson-Gomez J. A social network approach to demonstrate the diffusion and change process of intervention from peer health advocates to the drug using community. Substance Use and Misuse. 2012;47(5):474–490. doi: 10.3109/10826084.2012.644097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayoh J., Onwuegbuzie A.J. Toward a conceptualization of mixed methods phenomenological research. Journal of Mixed Methods Research. 2015;9(1):91–107. doi: 10.1177/1558689813505358. [DOI] [Google Scholar]
- Neill E., Meyer D., Toh W.L., van Rheenen T.E., Phillipou A., Tan E.J., Rossell S.L. Alcohol use in Australia during the early days of the COVID-19 pandemic: initial results from the COLLATE project. Psychiatry and Clinical Neurosciences. 2020 doi: 10.1111/pcn.13099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palsson O.S., Ballou S., Gray S. The U.S. National Pandemic Emotional Impact Report. 2020. http://pandemicimpactreport.com [DOI] [PMC free article] [PubMed]
- Rodriguez L.M., Litt D.M., Stewart S.H. Drinking to cope with the pandemic: The unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addictive Behaviors. 2020 doi: 10.1016/j.addbeh.2020.106532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saldaña J. 3rd ed. Sage; 2015. The coding manual for qualitative researchers. [Google Scholar]
- Sandelowski, M. (2001). Real qualitative researchers do not count: the use of numbers in qualitative research. In Research in Nursing and Health (Vol. 24, Issue 3, pp. 230–240). doi: 10.1002/nur.1025. [DOI] [PubMed]
- Scott C.K., Grella C.E., Nicholson L., Dennis M.L. Opioid recovery initiation: pilot test of a peer outreach and modified recovery management checkup intervention for out-of-treatment opioid users. Journal of Substance Abuse Treatment. 2018;86:30–35. doi: 10.1016/j.jsat.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S., Rock P., Bush H.M., Quesinberry D., Walsh S.L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug and Alcohol Dependence. 2020 doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timpka T., Spreco A., Gursky E., Eriksson O., Dahlström Ö., Strömgren M.…Holm E. Intentions to perform non-pharmaceutical protective behaviors during influenza outbreaks in Sweden: a cross-sectional study following a mass vaccination campaign. PLoS One. 2014 doi: 10.1371/journal.pone.0091060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N.D. Annals of Internal Medicine. 2020. Collision of the COVID-19 and addiction epidemics. [DOI] [PMC free article] [PubMed] [Google Scholar]