Abstract
Introduction
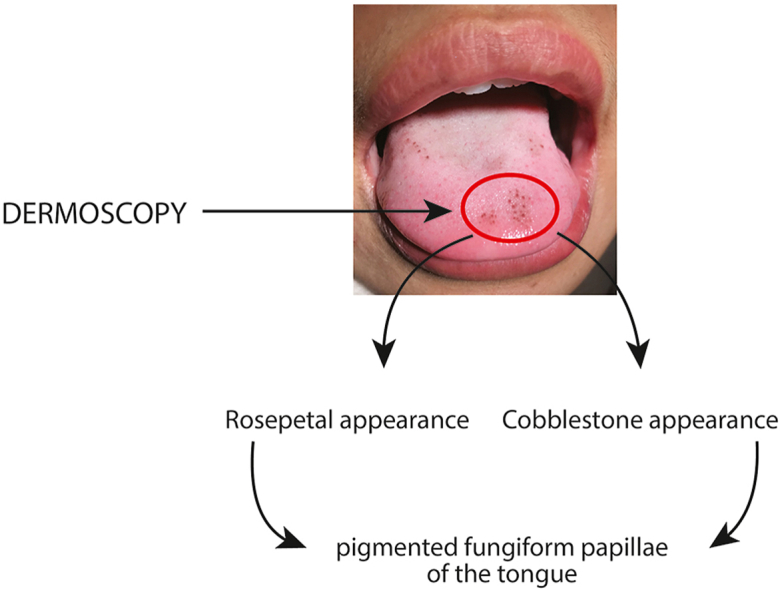
The practice of dermoscopy in dental and oral examination is low due to less popularity and not well established of the diagnostic tool in dental practice. The dermoscopy examination provides a specific dermoscopes details for pigmented papillary fungiform of tongue (PPFT) as cobblestone appearance and rose-petal appearance. With this dermoscopes details serves as a non-invasive diagnostic tool and prevents biopsy procedure.
Objective
We performed a systematic review to evaluate the published papers related to pigmented papillary fungiform on the tongue, aiming to understand the diagnostic role of dermoscopy examination in pigmented papillary fungiform.
Data synthesis
Initial result was 136 studies. Final exclusion of 27 articles was made based on the following factors: reports with no clinical images, studies that did not confirm the diagnosis of PPFT and studies that did not use the dermoscopes details. Finally, seventeen studies with nineteen cases, reported of pigmented papillary fungiform of the tongue. Six studies (consist six cases) reported the dermoscopy and histopathology diagnosis of pigmented papillary fungiform, eleven studies (consist thirteen cases) reported only the dermoscopy. The dermoscopy examination presented cobblestone appearance is 47.37% and rose petal appearance is 52.63%. The comparation study by histopathology diagnosis was done, revealed no specific appearances.
Conclusions
The clinical appearance and dermoscopy is the key for diagnosis of the papillary fungiform on the tongue. Further research is needed for determining the etiology and predisposing factor in papillary fungiform so that the possibility of developing this condition can be predicted and proper treatment could be performed.
Keywords: Dermoscopy, Diagnosis, Human health, Microscopy, Pigmented papillary fungiform, Tongue
Graphical abstract
1. Introduction
The color of oral mucosa is predominantly pink colored and occasionally intermixed with pigmentation. Pigmentation may be observed due to physiological or pathological changes. Oral mucosal pigmentation may be a resultant of exogenous or endogenous causes. Predominant pigmentation change of oral mucosa occurs due to melanin, melanoid, oxyhemoglobin, hemosiderin, bilirubin, iron or carotene.1
Pigmented papillary fungiform of the tongue (PPFT) is a normal anatomical variant that is observed as localized, darkly pigmented papillae over dorsum of tongue. PPFT was first reported by Leonard in 1905 as blackish brown pigmented lesion observed in tongue at the location of fungiform papillae.2 PPFT is commonly observed in dark skinned individuals with a prevalence of 33% among African American individuals and general population prevalence as 1–3%. A study mentioned that PPFT is observed in 30% Black females and 25% Black males.3 Published evidence on PPFT mentioned about occurrence in childhood to young adulthood.4
Research evidence on PPFT is minimal and often identified as a pathological lesion that causes a diagnostic dilemma.5 Evaluation of pigmentation should be done to rule out pathological conditions specifically malignancy.6 The evaluation of medical, drug, dental history and extra- and intra-oral examination should be done.7 The history of the examination should collect the information such as: onset, duration of the pigmented lesion, the presence and absence of associated skin hyper-/hypo-pigmentation, ulceration or other symptoms. The examination details such as color, number, location, distribution, appearance and associated features are important in formulating differential diagnosis.8, 9, 10 Majority of oral mucosal pigmentations are diagnosed through clinical presentation and symptoms. This includes amalgam tattoo, localized argyria, smoker's palate, drug induced pigmentation are confirmed by clinical details.11 Amalgam tattoo is usually blue, black or bluish grey colored macular change observed on the gingival or oral mucosal surface.12,13
Microscopic examination is an important tool for achieving final diagnosis. Biopsy is mandatory for focal pigmentation of oral mucosa with no local factors. Cases of disfigurement of anatomical disturbances were reported due to unnecessary biopsy procedures.14 Non-invasive or minimally invasive chair side diagnostic procedures can prevent such biopsy or diagnostic surgery related complications. Dermoscopy or dermoscopes is a non-invasive, surface microscopic device that is used in dermatology practice to evaluate and differentiate suspicious melanocytic lesions from dysplastic lesions and melanomas, squamous cell carcinoma or basal cell carcinoma.14,15 The use of dermoscopy in the examination of oral mucosa or oral lesions is not well established.16
The microscopic examination of PPFT tissue shows deposition of melanin with hyperpigmentation of basal keratinocytes and the presence of melanophages. The connective tissue stroma showing chronic inflammatory cells infiltrate chiefly lymphocytes. Diagnosis of PPFT is required to exclude the suspicion of malignant melanoma.5 Hence, a non-invasive diagnostic tool is necessary in identifying PPFT.
The diagnostic use of dermoscopy is also applicable in oral tissue examination specifically pigmented changes of oral tissues. Thus, aim of our study was to perform a systematic review of the literature to investigate the diagnostic utility and accuracy of dermoscopy in identifying PPFT without performing biopsy or microscopic examination.
2. Review of literature
2.1. Study design
The design of this systematic review followed the guidance stated by the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-analyses). This review aimed to analyze the following question: Is dermoscopy examination assist a clinician in identifying pigmented papillary fungiform of tongue?
2.2. Search method
The search strategy used in this systematic review was based on the MeSH terms (Medical Subject Heading) and common keywords related to clinical, histology of tongue. The search terms used are: “pigmented papillary fungiform of tongue”, “pigmented fungiform papilla of tongue”, “dark spots on the tongue” and “dermoscopy”. The purpose of using search term “dermoscopy” was to get broad search results of tongue papilla related studies. This systematic review reports on the findings from the oral research studies and case reports on pigmented fungiform papilla of the tongue. According to the specific requirements in PubMed, Google scholar and Embase databases were searched for the studies and case reports published during the period 1974–2020.
2.3. Selection criteria
The inclusion criteria for selection of papers in this review were as follows: original research studies conducted on pigmented papillary fungiform of the tongue (PPFT); diagnosis of PPFT using clinical and/or histopathological investigations; studies/reports that utilized dermoscopy for examination of tongue; and published in English language. Review articles related to PPFT and articles that do not have full text access were excluded.
2.4. Data collection
Initially two reviewers independently screened papers based on titles, abstract of the articles from the databases matching the selection criteria of the study to identify potentially eligible papers. Two reviewers eliminated duplicate reports and discussed about the articles that were selected. Disagreement between the reviewers were itemized and third reviewer was invited to participate in the consensus. The key information of each selected article was recorded, included in the study design and required findings were tabulated. The data collected focused on age, gender, geographic location/race, anatomical location or distribution of PPFT, clinical and dermoscopy appearance of PPFT, histopathological and final diagnosis. The data obtained were recorded in Microsoft Excel 2019 document. The extracted data were tabulated and presented as mean ± standard deviation, range, numbers and percentages.
2.5. Data extraction
The dataset was created and analyzed using Microsoft® Excel 2019 for Mac. Details of the data extraction were tabulated and data presented as mean ± standard deviation, range, numbers, and percentages.
3. Result
3.1. Study selection
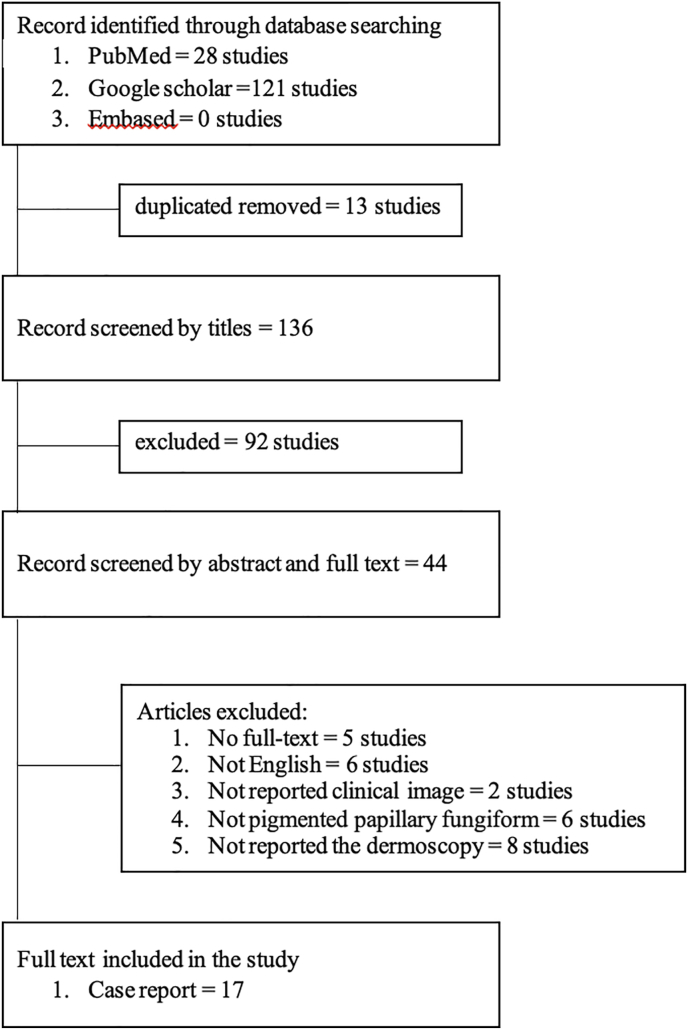
The database search showed a total of one hundred forty-nine studies related to study search terms. The studies with duplicating titles were excluded, which resulted in 136 studies. Further exclusion was made for full text availability and abstract search which resulted in 44 studies. Final exclusion of 27 articles was made based on the following factors: the studies that were not written in English, reports with no clinical images, studies that did not confirm the diagnosis of PPFT and studies that did not use the dermoscopes details. Finally, seventeen studies were selected as suitable and eligible for performing this systematic review analysis (Fig. 1).
Fig. 1.
Schematic research.
3.2. Study result
We identified the seventeen studies (case report), reported of PFTT. Two studies reported two cases in the different individual. The total cases we identified is nineteen cases. Six studies (consist six cases) reported the dermoscopy and histopathology diagnosis of pigmented papillary fungiform, eleven studies (consist thirteen cases) reported only the dermoscopy.
In the most of case report, the patient was female 14 (73.68%). The distribution of the PFTT found around 21.50 ± 10.38 years old, with the youngest at 8 years old and the oldest 44 years old (1 cases not reported the age). The cases of PFTT are closely related with dark skin races, but in the report found, the most cases are Asian (31.58%), European (10.53%), American and African (31.58%) and not reported (26.32%). Most of cases found a PFTT in anterior and or lateral and or dorsum papillary of the tongue (52.63%), anterior papillary only (36.48%), lateral papillary (5.26%) and dorsum papillary (5.26%) (Table 1).
Table 1.
Characteristic of subject.
| Ages (years) |
20.66 ± 11.24 Range 8–44 |
|---|---|
| Gender | |
| Male | 5 (26.32%) |
| Female | 14 (73.68%) |
| Races | |
| Asian | 6 (31.58%) |
| Europe | 2 (10.53%) |
| American and African | 6 (31.58%) |
| Not reported | 5 (26.32%) |
| Location of affected papillary in the tongue | |
| Anterior | 7 (36.84%) |
| Lateral | 1 (5.26%) |
| Dorsum | 1 (5.26%) |
| > 1 location | 10 (52.63%) |
3.3. The dermoscopy examination of pigmented papillary fungiform
The clinical appearance of PPFT is multiple macules, with blue-grey or dark brown papillary, diffuse with symmetrical pattern. Nineteen cases reported the dermoscopy of pigmented papillary fungiform. The dermoscopy appearance presented cobblestone appearance (47.37%) and rose petal appearance (52.63%) (Table 2).
Table 2.
The diagnosis of pigmented papillary fungiform with dermoscopy examination.
| No | Gender | Ages | Races | Location of affected papillary | Clinical appearance | Dermoscopy | Histopathology finding | Ref |
|---|---|---|---|---|---|---|---|---|
| 1 | Male | 28 | NR | Anterior of the tongue | Multiple dark-brown macules and dome shaped papules | Cobblestone pattern |
|
20 |
| 2 | Female | 27 | Italian | Anterior and lateral of the tongue | Multiple blue-grey pigmentation, diffuse and symmetrical pattern | Rose petal pattern |
|
22 |
| 3 | Female | 20 | NR | Anterolateral and dorsum of the tongue | Multiple brown macule | Rose petal pattern | melanophages in the lamina propria | 23 |
| 4 | Male | 26 | Taiwan | Antero-lateral of the tongue | Multiple, tiny, brown macule | Cobblestone pattern | melanophages on the upper lamina propria | 24 |
| 5 | Male | 28 | Hispanic | Lateral distal of the tongue | Multiple dark-brown | Rose petal pattern | melanophages within the lamina propria | 25 |
| 6 | Female | 12 | Asian | Anterior of the tongue | Tiny pigmented macules | Cobblestone pattern | increased number of submucosal melanophages | 26 |
| 7 | Female | 40 | Black | Anterior of the tongue | Multiple hyperpigmented papillary | Rose petal pattern | NP | 5 |
| Female | 44 | Black | Anterior of the tongue | Multiple hyperpigmented papillary | Rose petal pattern | NP | 5 | |
| 8 | Female | 30 | Black | Anterior of the tongue | Multiple hyperpigmented papillary | Rose petal pattern | NP | 17 |
| 9 | Female | 12 | Moroccan | Anterior of the tongue | Multiple hyperpigmented papillary, present in a diffuse and symmetrical pattern | Rose petal pattern | NP | 40 |
| 10 | Female | 12 | African | Anterior, lateral and dorsum of the tongue | Multiple hyperpigmented papillary, presented as dark patches | Rose petal pattern | NP | 48 |
| 11 | Female | 23 | NR | Anterior and lateral of the tongue | Multiple hyperpigmented papillary, present in a diffuse pattern | Rose petal pattern | NP | 54 |
| 12 | Female | 13 | South Asian | Anterior of the tongue | Light to dark brown pigmentation, round or polygonal in shape, circumscribed to the papillary and resembling a cobblestone appearance | Cobblestone pattern | NP | 42 |
| 13 | Female | 12 | NR | Anterior and dorsum of the tongue | multiple discrete tan-brown pinhead papules | Rose petal pattern | NP | 41 |
| 14 | Male | 22 | Javanese | Dorsum of the tongue | multiple asymptomatic macula, which were brownish-black and shared clear border | Cobblestone pattern | NP | 55 |
| Female | 21 | Javanese | Anterior and dorsum of the tongue | multiple brownish-black, diffuse, and asymptomatic macula | Cobblestone pattern | NP | ||
| 15 | Female | 9 | Japanese | pigmented fungiform papillae on the anterior aspect of the dorsum of the tongue | Macroscopic ex- amination revealed approximately 30 fungiform papillae with pigmentation within the lesion | Cobblestone pattern | NP | 53 |
| 16 | Female | NR | NR | dorsal and lateral aspects of her tongue | multiple hyperpigmented papillae and patches | Cobblestone pattern | NP | 56 |
| 17 | Male | 8 | Latin America | Dorsum and tip of the tongue | Multiple asmptomatic and sharply demarcated hyperpigmented pinhead papules | Cobblestone pattern | NP | 57 |
NR = not reported.
NP = not performed.
3.4. The histopathology features of pigmented papillary fungiform
Six cases reported the histopathology diagnosis of pigmented papillary fungiform. The histopathology diagnosis revealed the present of melanophages in the lamina propria or sub-epithelial (six cases), hyperpigmentation of basilar keratinocytes (one cases), and lymphocytes infiltration in the superficial chorion (one cases) (Table 2).
4. Discussion
The mucosa of oral cavity is not uniformly pink colored. The variation in the color of oral mucosa is influenced by physiological and pathological conditions. The color of oral mucosa occurs due to deposition of pigments predominantly melanin. The melanocytes are in the basal layer of oral epithelium. The proliferation of melanocytes in oral epithelium results in hyper pigmentation.9
Pigmented papillary fungiform of the tongue (PPFT) is a physiological pigmented condition of tongue due to accumulation of melanin which often mimics as malignant pigmented lesions.5,17 The microscopic examination of PPFT is characterized by proliferation of melanocytes in basal layer of epithelium.18, 19, 20 Few studies also mentioned about the presence of chromatophores in PPFT biopsied tissues.21 Studies also mentioned about the appearance of melanophages in PPFT tissues.22, 23, 24, 25, 26, 27, 28, 29, 30, 31 Lymphocyte infiltration also observed in microscopic specimens of PPFT.22 Melanophages are the macrophages that contains phagocytized melanin, these are large, bright plump cells with ill-defined cytoplasmic borders.32 Melanophages are usually identified in papillary dermis and found near blood capillaries. Melanophages appeared as large bright plump cells with ill-defined cytoplasmic borders, usually located around or near vessels of the superficial dermis. Role of melanophages in pigmented papillary fungiform of tongue is not fully understood.33
The clinical details are helpful in recognizing PPFT. Holzwanger et al. in 1974 classified PPFT into three types: Type 1, 2 and 3.21 Type 1 is characterized by well-defined hyperpigmented areas on anterior and antero-later aspects of tongue. Type 2 is characterized by few numbers of PPFT over dorsal surface. Usually, the number ranges between 3 and 7. Type 3 is characterized by scattered appearance of PPFT on the dorsum surface.34,35 Visual examination using dermoscopy is helpful in recognizing clinical types and chair side confirmation of PPFT.
The dermoscopy used in the oral cavity in some of reference called as mucoscopy.36 The use of dermoscopy on the oral mucosa is still limited. Several studies defined the dermoscopes on healthy labial mucosa. Dermoscopes obtained was superficial vascular network, deep vascular network, yellow background areas, targetoid brown round areas, clear reticular arrangement, mixed reticular arrangement, grouped hairpin vessels, chain-shaped hairpin vessels, match stick hairpin vessels, dotted vessels, glomerular vessels, purple areas, haemorrhagic dot, white dots, yellowish-white streaks, honeycomb appearance, hyperkeratosis, microaneurysm and microulceration. This dermoscopes results will serve as the basis for normal mucosa and identified the abnormal mucosa on the effect of systemic diseases on oral labial mucosa and studies on localized mucosal diseases.37
The dermoscopy helps the dentist to give a significant and clear of the lesion because it provide 10–20 magnification and good lighting so that the surrounding area can also be observed.38 The dermoscopes of normal fungiform papillae showed as whitish papillae and red background.15 The dermoscopes of PFTT is unique, it appears as cobblestone appearance,39 and rose petal appearance.40 Rose petal appearance showed as pigmented borders, ovoid hyperpigmented projections with dichotomized vessels originating at its base,41 and cobblestone appearance showed as light to dark brown pigmentation on papillae, round or polygonal in shape and circumscribed resembling a cobblestone.20,42 Due to the pigment that is restricted to the borders, they have a much better-defined contour than the usual non-pigmented fungiform papillae.36 Cobblestone and rose-petal appearances are helpful in distinguishing PPFT from other pigmented conditions of tongue. Hence, dermoscopes serves as a reliable clinical diagnostic tool in differentiating from suspicious pigmented lesions. In addition, dermoscopy serves as a non-invasive diagnostic tool and prevents biopsy procedure.16 Few authors mentioned that histopathological examination is not required in examination of pigmented tongue lesion with no underlying systemic conditions or other oral pigmentations.35,40
The PFTT is localized in the tongue, the other condition of pigmented and affected on papillae must consider as differential diagnosis. This condition refers to black hairy tongue,43 median rhomboid glossitis,36 benign migratory glossitis,36 macula melanotic,44 physiological hyperpigmentation,36 lingual varicosity,45,46 and leukoplakia.47 each condition has different dermoscopes as present in Table 3. Leukoplakia has clinical appearance of white plaque, commonly found on the buccal mucosa, lateral of the tongue and gingiva. The case reported by Sonthalia et al., 2018, showed that clinical appearance of leukoplakia on the dorsum of tongue as dark grey discoloration, blunted papillae in the centre with few tiny bright red erosions and interspersed white reticular lesions.47 This cases is able consider as differential diagnosis of PFTT.
Table 3.
The tongue lesion and dermoscopes.
| Oral lesions | Dermoscopes | Reference |
|---|---|---|
| Black hairy tongue |
|
43 |
| Macula melanotic | parallel lines or reticular pattern with greyish granules, globules or dots | 44 |
| Physiological hyperpigmentation | parallel and homogenous structureless pattern | 36 |
| Median rhomboid glossitis | atrophic filiform papillae in the affected area, in comparison to peripherally distributed papillae of normal size | 36 |
| Benign migratory glossitis | loss of filiform papillae in clinically reddish areas on the dorsal surface and whitish lines demarcating affected from unchanged regions | 36 |
| Lingual varicosity |
|
45,46 |
| Leukoplakia |
|
47 |
The systemic conditions that are evidently correlated with PPFT are: childhood obesity, menstruation related problems,48 and secondary oral manifestations of iron deficiency anemia.29 These systemic conditions have classic recognizable dermoscopy examination of tongue pigmentations thus helping in differentiating from PPFT.49
The frequency of pigmentation and PPFT are higher among African descendant and increased synthesis of melanosomes are influenced by specific races predominantly blacks.50 PPFT is also reported as oral manifestation of Laugier-Hunziker syndrome which is a rare muco-cutaneous pigmentation condition that occurs on lips, oral, cutaneous, genital mucosa and nail.3,51 Biopsy is necessary on the patients who show PPFT and other mucosal involvement such as cutaneous or genital mucosa are identified.51
Dermoscopy examination is a reliable clinical diagnostic tool in dermatological examinations, however the use of dermoscopy in oral mucosal examination is minimal. The operational complexity of oral mucosa are related to moistness, flexibility of tissues and higher vascularity.52 The clinical use of dermoscopy is well appreciated in dermatological conditions due to distinct dermoscopes and microscopic examination features. In other words, dermoscopes reduced the need for number of biopsy examination in dermatological practice.16
The visual examination of clinical details and dermoscopes appearance are the key in recognizing PPFT. Biopsy procedures can be minimized using dermoscopy examination of tongue. However, histopathological examination must be considered for suspicious or malignant nature of lesion through appropriate oral surgery service.
5. Final comments
The application of dermoscopy examination in oral cavity is high, however the practice of dermoscopy in dental and oral examination is low due to less popularity of the diagnostic tool in dental practice. The dental educational institutions and oral disease educators should explore and investigate the usefulness of dermoscopy in dental examination which will amplify the diagnostic utility and provide a room for creating flexible and custom designed dermoscopy for oral cavity examination.14 Alternatively, cross sectional studies are required to examine pigmented oral mucosal lesions using dermoscopy for understanding the clinical appearance using this tool. The results of such will allow us to incorporate dermoscopy in routine dental practice. However, dentist must be cautioned and refer the patients to oral surgery care when suspicious pigmented lesions are observed, and biopsies must be mandated for confirming diagnosis of malignant oral pigmentations.16
This systematic review addressed the importance of dermoscopy examination in PPFT and its ability to characterize the condition with specific features. Biopsy is not mandated in PPFT due to absence of pain, discomfort or anatomical disfigurement. The limitations of this paper may be directed towards to the papers selected for systematic review are case reports, lack of explanations on genesis and treatment of PPFT, the data was searched for the published articles written in English. There are no published Randomized Control Trial (RCT) studies on PPFT available in the database. This paper highlighted the importance of non-invasive dermoscopy examination tool in oral and dental examination. The study emphasizes that scope of this tool is highly useful among the patients who are aesthetically concerned about their pigmentations or those patients who are suspected for malignant oral pigmentations.
Declaration of competing interest
All author declares no conflict of interest for this research.
References
- 1.Chandra S., Keluskar V., Bagewadi A., Sah K. Extensive physiologic melanin pigmentation on the tongue: an unusual clinical presentation. Contemp Clin Dent. 2010;1 doi: 10.4103/0976-237X.73205. http://www.contempclindent.org/text.asp?2010/1/3/204/73205 204–6. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El Anzi O. Pigmented fungiform papillae of the tongue: Moroccan case. Our Dermatol Online. 2019;10:215–216. [Google Scholar]
- 3.Marcoval-Caus J. Response to: «pigmented fungiform papillae of the tongue in Laugier disease (or Laugier-Hunziker syndrome)». Actas Dermo-Sifiliográficas (English Ed. 2013;104:174. doi: 10.1016/j.ad.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Smogorzewski J.M., Armstrong P., Young L. Pigmented fungiform papillae of the tongue in an Indian male. Cutis. 2019;103:E16–E17. [PubMed] [Google Scholar]
- 5.Mukamal L.V., Ormiga P., Ramos-e-silva M. Dermoscopy of the pigmented fungiform papillae of the tongue. J Dermatol. 2012;39:397–399. doi: 10.1111/j.1346-8138.2011.01328.x. [DOI] [PubMed] [Google Scholar]
- 6.della Vella F, Lauritano D, Lajolo C, Lucchese A, Di Stasio D, Contaldo M. The Pseudolesions of the Oral Mucosa: Differential Diagnosis and Related Systemic Conditions. Appl Sci. 2019;9:2412. https://www.mdpi.com/2076-3417/9/12/2412 Available from: [Google Scholar]
- 7.Mallikarjuna K., Gupta S., Shukla S., Chaurasia S. Unusual extensive physiologic melanin pigmentation of the oral cavity: a clinical presentation. J Indian Soc Pedod Prev Dent. 2013;31:121–125. doi: 10.4103/0970-4388.115718. [DOI] [PubMed] [Google Scholar]
- 8.O'Hana D., Barthélémy I., Baudet-Pommel M., Pham-Dang N., Devoize L. Differential diagnosis of an oral mucosal pigmented lesion: a case of essential melanosis. Med Buccale Chir Buccale. 2017;23:156–159. [Google Scholar]
- 9.Roy R. Classification of oral pigmented lesions: a review. Int J Appl Dent Sci. 2019;5:397–402. www.oraljournal.com Available from: [Google Scholar]
- 10.Alawi F. Pigmented lesions of the oral cavity. Dent Clin North Am. 2013;57:699–710. doi: 10.1016/j.cden.2013.07.006. https://linkinghub.elsevier.com/retrieve/pii/S0011853213000578 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lundin K., Schmidt G., Bonde C. Amalgam tattoo mimicking mucosal melanoma: a diagnostic dilemma revisited. Case Rep Dent. 2013;2013:1–3. doi: 10.1155/2013/787294. http://www.hindawi.com/journals/crid/2013/787294/ Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thumbigere-math V., Johnson D.K. Treatment of amalgam tattoo with a subepithelial connective tissue graft and acellular dermal matrix. J Int Acad Periodontol. 2014;16:50–54. [PubMed] [Google Scholar]
- 13.Patil S., Raj T., Rao R., Warnakulasuriya S. Journal of pigmentary disorders pigmentary disorders of oral mucosa. Pigment Disord. 2015;2:1–9. [Google Scholar]
- 14.Olszewska M., Banka A., Gorska R., Warszawik O. Dermoscopy of pigmented oral lesions. J Dermatol Case Rep. 2008;2:43–48. doi: 10.3315/jdcr.2008.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okamoto T., Tanaka M., Kaibuchi N., Kuwazawa T., Ando T. Correlation between dermoscopic and histopathological findings of leucoplakia of the tongue: a case report. Br J Oral Maxillofac Surg. 2018;56:758–760. doi: 10.1016/j.bjoms.2018.08.007. Available from: [DOI] [PubMed] [Google Scholar]
- 16.Mordoh A., Casas G., Horacio C. Dermoscopic evaluation improves clinical diagnosis of oral melanotic macules: a study in 50 patients with oral pigmented lesions. Am J Oral Med. 2018;4:1–9. [Google Scholar]
- 17.Pinos-León V. Dermoscopic features of pigmented fungiform papillae of the tongue. Case Res Lett. 2015;106:593–594. doi: 10.1016/j.ad.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 18.Adibi S., Bouquot J.E. Papillary tip melanosis (pigmented fungiform lingual papillae) Tex Dent J. 2011;128:573–574. [PubMed] [Google Scholar]
- 19.Werchniak A.E., Storm C.A., Dinulos J.G.H. Hyperkeratotic plaques on the palms and soles A red-Brown plaque on the nape hyperpigmented patches on the tongue of a young girl. Arch Dermatol. 2009;140 doi: 10.1001/archderm.140.10.1275-g. [DOI] [PubMed] [Google Scholar]
- 20.Chamseddin B., Vandergriff T. Pigmented fungiform papillae of the tongue: a clinical and histologic description. Dermatol Online J. 2019;25:1–3. [PubMed] [Google Scholar]
- 21.Holzwanger J.M., Rudolph R.I., Heaton C.L. Pigmented fungiform papillae of the tongue: a common variant of oral pigmentation. Int J Dermatol. 1974;13:403–408. doi: 10.1111/j.1365-4362.1974.tb05073.x. [DOI] [PubMed] [Google Scholar]
- 22.Ghigliotti G., Chinazzo C., Parodi A., Rongioletti F. Pigmented fungiform papillae of the tongue: the first case in an Italian woman. Clin Exp Dermatol. 2017;42:206–208. doi: 10.1111/ced.13006. [DOI] [PubMed] [Google Scholar]
- 23.Robles-Mendez J.-C., Ayala-Cortes A.S., Villarreal-Martinez A., Ocampo-Candiani J. Dermoscopy of the pigmented fungiform papillae of the tongue. J Dermatol. 2017;76:s40–s42. doi: 10.1016/j.jaad.2016.06.022. [DOI] [PubMed] [Google Scholar]
- 24.Hsiao Y.-H., Ko J.-H., Lu C.-F., Chen M.-J. Dermoscopic findings in pigmented fungiform papillae of the tongue. Eur J Dermatol. 2011;21:819–820. doi: 10.1684/ejd.2011.1490. [DOI] [PubMed] [Google Scholar]
- 25.Maxim E., Dtefano D de. Pigmented fungiform papillae of the tongue: an incidental finding in a patient with mycosis fungoides. J Am Acad Dermatol. 2018;79 https://linkinghub.elsevier.com/retrieve/pii/S0190962218316840 AB221. Available from: [Google Scholar]
- 26.Lin Y.T., Chou C.L. Pigmented macule on the tongue of a 12-year-old girl. J Am Acad Dermatol. 2013;69 doi: 10.1016/j.jaad.2013.05.026. e229–30. Available from: [DOI] [PubMed] [Google Scholar]
- 27.Choi S.J., Rho nark K., Yang J.M., Lee E.S. Two cases of pigmented fungiform papillae of the tongue. Ann Dermatol. 2002;14:216–219. [Google Scholar]
- 28.McCarthy C., Holt D., Triantafyllou A. Solitary pigmentation of the tongue: lentigo simplex or pigmented fungiform papilla? Oral Surg. 2016;11:50–54. [Google Scholar]
- 29.Sharma S.S., Sharma S.S. Pigmentation of the fungiform papillae of the tongue in a child secondary to iron deficiency anaemia: an uncommon occurrence and association. Int J Oral Health Dent. 2016;2:39–42. http://www.indianjournals.com/ijor.aspx?target=ijor:ijohd&volume=2&issue=1&article=007 Available from: [Google Scholar]
- 30.Oh C.K., Kim M.B., Jang H.S., Kwon K.S. A case of pigmented fungiform papillae of the tongue in an Asian male. J Dermatol. 2000;27:350–351. doi: 10.1111/j.1346-8138.2000.tb02181.x. [DOI] [PubMed] [Google Scholar]
- 31.Isogai Z., Kanzaki T. Pigmented fungiform papillae of the tongue. J Am Acad Dermatol. 1993;29:489–490. doi: 10.1016/S0190-9622(08)82004-X. Available from: [DOI] [PubMed] [Google Scholar]
- 32.Pehoushek J.F., Norton S.A. Black taste buds. Arch Fam Med. 2000;9:219–220. [Google Scholar]
- 33.Busam K.J., Charles C., Lee G., Halpern A.C. Morphologic features of melanocytes, pigmented keratinocytes, and melanophages by in vivo confocal scanning laser microscopy. Mod Pathol. 2001;14:862–868. doi: 10.1038/modpathol.3880402. [DOI] [PubMed] [Google Scholar]
- 34.Alzahrani N., Alharithy R. Pigmented fungiform papillae of the tongue in a Saudi woman. J Dermatology Dermatologic Surg. 2018;22:39. [Google Scholar]
- 35.Romiti R., Medeiros LM De. Pigmented fungiform papillae of the tongue. Pediatr Dermatol. 2010;27:398–399. doi: 10.1111/j.1525-1470.2010.01183.x. [DOI] [PubMed] [Google Scholar]
- 36.Jha A., Vinay K., Sławińska M. Application of mucous membrane dermoscopy (mucoscopy) in diagnostics of benign oral lesions ‐ literature review and preliminary observations from International Dermoscopy Society study. Dermatol Ther. 2021:34. doi: 10.1111/dth.14478. https://onlinelibrary.wiley.com/doi/10.1111/dth.14478 Available from: [DOI] [PubMed] [Google Scholar]
- 37.Ayhan E., Öztürk M., An I., Araç E. Dermoscopy of oral labial mucosa according to age and sex in healthy adults: first observational dermoscopic study. Turk Dermatoloji Derg. 2019;13:135–139. [Google Scholar]
- 38.Kaliyadan F. The scope of the dermoscope. Indian Dermatol Online J. 2016;7:359–363. doi: 10.4103/2229-5178.190496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chessa M.A., Patrizi A., Sechi A., Virdi A., Leuzzo M., Neri I. Pigmented fungiform lingual papillae: dermoscopic and clinical features. J Eur Acad Dermatol Venereol. 2018;32:935–939. doi: 10.1111/jdv.14809. [DOI] [PubMed] [Google Scholar]
- 40.Aqil N., Bennani M., Nassiri A., Meziane M., Gallouj S., Mernissi F.Z. Pigmented fungiform papillae of the tongue: clinical and dermoscopic features. Our Dermatol Online. 2019;10:213–214. [Google Scholar]
- 41.Sil A., Panigrahi A., Bhanja D.B. Tongue discoloration in a young girl. J Pediatr. 2020;219:276–277. doi: 10.1016/j.jpeds.2019.12.032. Available from: [DOI] [PubMed] [Google Scholar]
- 42.Collgros H., Iglesias-Sancho M., Galvany L. Dermoscopy of pigmented fungiform papillae of the tongue in an Indian girl. Australas J Dermatol. 2015;56:e81–e82. doi: 10.1111/ajd.12229. [DOI] [PubMed] [Google Scholar]
- 43.Kobayashi K., Takei Y., Sawada M., Ishizaki S., Ito H., Tanaka M. Dermoscopic features of a black hairy tongue in 2 Japanese patients. Dermatol Res Pract. 2010;2010:2–4. doi: 10.1155/2010/145878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gómez-Martín I., Collgros H., Ferguson P.M. Diagnostic accuracy of pigmented labial macules by in vivo reflectance confocal microscopy and correlation among techniques. J Am Acad Dermatol. 2020:1–10. doi: 10.1016/j.jaad.2020.02.067. https://linkinghub.elsevier.com/retrieve/pii/S0190962220303133 Available from: [DOI] [PubMed] [Google Scholar]
- 45.Sonthalia S. Interpreting mucoscopy in lingual varicosities and beyond. Dermatol Pract Concept. 2019;9:146–147. doi: 10.5826/dpc.0902a11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jha A., Zeeshan M.D. Mucoscopy in lingual varicosities. Dermatol Pract Concept. 2018;8:54–55. doi: 10.5826/dpc.0801a12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sonthalia S., Varma S., Jha A.K., Jakhar D., Kaliyadan F. Case Report: dermoscopic features of oral lichen planus - the evolution of mucoscopy. F1000Res. 2018;7:1–10. doi: 10.12688/f1000research.14134.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Docx M.K.F., Vandenberghe P., Govaert P. Pigmented fungiform papillae of the tongue (PFPT) Acta Clin Belg. 2016;71:117–118. doi: 10.1179/2295333715Y.0000000067. [DOI] [PubMed] [Google Scholar]
- 49.Lake P.L. Dark spots on the tongue. J Dermatol Nurses’ Assoc. 2017;9:146–147. [Google Scholar]
- 50.Urbina F., Sudy E. Pigmented fungiform papillae of the tongue in Laugier disease (or Laugier-Hunziker syndrome) Actas Dermo-Sifiliográficas (English Ed. 2013;104:173–174. doi: 10.1016/j.ad.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 51.Verma B., Bahra A., Ajmal A.K.M., Sen S. Laugier–hunziker syndrome in a young female. Indian Dermatol Online J. 2017;8:148–150. doi: 10.4103/2229-5178.202282. http://www.idoj.in/text.asp?2017/8/2/147/202269 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jha A.K., Pathak J. Using a chalazion clamp to enhance dermoscopy of oral mucosal lesions. J Am Acad Dermatol. 2017;76:e91–e92. doi: 10.1016/j.jaad.2016.10.025. [DOI] [PubMed] [Google Scholar]
- 53.Sugiyama Y., Hayashi K., Takayama T. Pigmented fungiform papillae of the tongue in a Japanese child. Clin Case Rep. 2020;8:1104–1106. doi: 10.1002/ccr3.2830. https://onlinelibrary.wiley.com/doi/abs/10.1002/ccr3.2830 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gopinath H., Upadya G.M. Pigmented fungiform papillae in mother and daughter. Indian J Dermatol Venereol Leprol. 2017;85:510–511. doi: 10.4103/ijdvl.IJDVL_826_16. http://www.ijdvl.com/text.asp?2017/83/4/510/204731 Available from: [DOI] [PubMed] [Google Scholar]
- 55.Surboyo M.D.C., Ernawati D.S., Parmadiati A.E., Marsetyo R.I. Pigmented fungiform papillae of the tongue and lingual fimbriae as single presentation in adult: a case report and literature review. Eur J Dent. 2020;14:702–706. doi: 10.1055/s-0040-1714041. http://www.thieme-connect.de/DOI/DOI?10.1055/s-0040-1714041 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ross C.L., Ring C., Yang S. Pigmented Fungiform Papillae of the Tongue. JAMA Dermatol. 2020 doi: 10.1111/jdv.14809. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 57.Piquero-Casals J., Morgado-Carrasco D. Pigmented fungiform lingual papillae. J Pediatr. 2020;224:177–178. doi: 10.1016/j.jpeds.2020.06.001. Available from: [DOI] [PubMed] [Google Scholar]