Abstract
Purpose.
Pediatric hospice is a comprehensive model of care for medically complex children at end of life. The Affordable Care Act changed regulatory requirements for pediatric Medicaid enrollees to allow for enrollment into hospice services while still receiving life-prolonging therapy. There are gaps in understanding factors associated with pediatric concurrent hospice care use. The objectives were to examine the prevalence of concurrent hospice care overtime and investigated the relationship between medical complexity and concurrent hospice care among Medicaid children.
Design and Methods.
We used national Medicaid data and included children < 21years with an admission to hospice care. Medical complexity was defined with 4 criteria (i.e., chronic conditions, functional limitations, high health care use and substantial needs). Using multivariate logistic regression, we evaluated the influence of medical complexity on concurrent hospice care use, while controlling for demographic, hospice, and community characteristics.
Results.
Thirty-four percent of the study sample used concurrent hospice care. Medical complexity was unrelated to concurrent hospice care. However, the 4 individual criteria were associated. A complex chronic condition was negatively related to concurrent hospice care, whereas technology dependence, multiple complex chronic conditions, and mental/behavioral disorders were positively associated to concurrent care use.
Practice Implications.
These findings suggest that concurrent hospice care may be important for a subset of medically complex children with functional limitations, high health utilization, and substantial needs at end of life.
Keywords: pediatric, concurrent hospice care, end-of-life care, hospice care, Medicaid
Introduction
Nearly one-quarter of the 40,000 childhood deaths in the United States involve medically complex children, and their care needs at the end of life are significant(Murphy, Mathews, Martin, Minkovitz, & Strobino, 2017). By definition, medically complex children experience multi-organ system problems, chronic childhood conditions, limitations in functional status, and ongoing use of medical technology, along with extremely high health care resource use and substantial needs(Cohen et al., 2011). They have the highest risk of all children for adverse medical, developmental, psychosocial, and family outcomes (Kuo, Houtrow, & Council on Children with Disabilities, 2016; Lindley, 2019; Mooney-Doyle & Lindley, 2020). Due to the degree of their medical complexity and overall healthcare utilization, medically complex children have been at the forefront of state-and-federal policy initiatives focused on high quality, comprehensive, and coordinated care provision across a variety of settings.
Pediatric hospice is an important care model for medically complex children as they approach end of life (Institute of Medicine, 2015; Institute of Medicine (US) Committee on Palliative and End-of-Life Care for Children and Their Families, 2003). Yet, pediatric hospice remains underutilized with roughly 80% of children and their families seeking high-intensity, life-prolonging care up until death(Lindley, 2017; Mack et al., 2015, 2013). Standard pediatric hospice care provides pain and symptom management for medically complex children and psychosocial support for the family during illness and after the death of the child(Lindley & Lyon, 2013). Due to regulatory requirement, standard hospice requires medically complex children to discontinue all life-prolonging care. Families must choose between hospice and life-prolonging care. However, the passage of the 2010 Patient Protection and Affordable Care Act (ACA, section 2302) now allows Medicaid and Children’s Health Insurance Plan (CHIP) children with a 6-months-to-live prognosis to simultaneously utilize hospice and life-prolonging services12.
Although there is emerging literature on pediatric concurrent hospice care, the effects of medical complexity on its use among children at end of life has not received sufficient attention(Lindley, Keim-Malpass, et al., 2020). Concurrent hospice care enables children to continue care for their medically complex condition, such as receiving chemotherapy or radiation for a cancer diagnosis, while also receiving pain and symptom management from hospice(Miller, Laragione, Kang, & Feudtner, 2012). Under concurrent care, hospice becomes an additional layer of support for medically complex children and their families(Keim-Malpass, Hart, & Miller, 2013; Lindley, 2011; Mooney-Doyle, Keim-Malpass, & Lindley, 2019). Because children with medical complexity have a known association with high health care utilization, costs, transitions in care, and unmet needs, understanding the relationship between medical complexity and concurrent care use is critical to improving end-of-life outcomes for these children(Berry et al., 2014; Coller et al., 2016; Kuo, Berry, et al., 2016; Kuo et al., 2014). Knowledge of concurrent care use and medical complexity may facilitate advances in clinical care and care coordination between hospices and providers of life-prolonging care for these children.
Given the limited literature on pediatric concurrent hospice care and the association between medical complexity and pediatric concurrent hospice care, the current investigation had two aims. The first aim was to examine the prevalence concurrent hospice care. The present study included an analysis of concurrent care from 2011 to 2013 to determine the impact of early ACA federal policy implementation. The second aim of the study was to examine the relationship between medical complexity and concurrent versus standard hospice care for children at end of life. We used a large, national Medicaid database to investigate this relationship and tested our analysis by conducting sensitivity analyses.
Methods
Study Design and Data
This study was a retrospective cohort design using national Medicaid claim files22. We used the Medicaid Analytical Extract (MAX) files, which are an administrative database of a health care claims for Medicaid enrollees in all 50 US states and the District of Columbia (DC)23. Our files included claims between January 1, 2011 and December 31, 2013. We manually linked the Medicaid files with data from 2010 US Census, Centers for Medicare & Medicaid Services (CMS) Hospice Provider of Services, and CMS Hospice Utilization and Payment. Because this study involved the use of protected health information(Lindley, Svynarenko, & Profant, 2020), the study was reviewed and approved by the University of Tennessee, Knoxville Institutional Review Board.
Sample
The study population was children age < 21years with an admission to hospice care during the study period. Hospice care was identified using the procedure and revenue codes for hospice within the Medicaid files. The age for the study was informed by the ACA, section 2302 which indicates concurrent hospice care for Medicaid and CHIP enrolled children is not available to youth after age 20. Children with no Medicaid hospice service claims, 21 years or older, or missing data (i.e., dates of birth) were excluded.
Measures
Dependent Variable.
The main outcome measure was concurrent hospice care versus standard hospice care use. The definition of concurrent care - children may receive medical services for their terminal illness during hospice care - guided the creation of this measure. First, we created a hospice episode from the Medicaid claims data, which was the consecutive days of hospice admission.(Mor et al., 2016, 2019) Second, we used the episode dates to evaluate whether a child received medical services during a hospice episode. Because all hospice services are included in the Medicaid per-diem reimbursement, any medical services received on the same day as hospice care claim would constitute concurrent care. We coded an episode that included medical services as concurrent care, and episodes without medical services were deemed standard hospice care.
Independent Variables.
Following Kuo and colleagues, we defined medical complexity for children in the cohort as meeting all four criteria of medical complexity: chronic condition (complex chronic condition), functional limitations (technology dependence), high health care use (multiple complex chronic conditions), and substantial needs (mental/behavioral disorders). Study participants were classified as medically complex or not. We also created individual measures for the 4 medical complexity criteria. Using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), diagnosis codes contained in Feudtner’s definition of complex chronic conditions were used to create the measure24. We defined functional limitations as children, who are technology dependent and require complex medical technology or devices(Feudtner, Feinstein, Zhong, Hall, & Dai, 2014). Children with multiple complex chronic conditions defined as 2 or more complex chronic conditions generally have high health care use(Lindley, 2017). Because children with mental and/or behavioral disorders have unique service needs at end of life that may or may not be covered during standard or concurrent hospice care, we created a variable using ICD-9-CM mental and behavioral health diagnosis codes(Garfield et al., 2015).
Covariates.
We assessed patient demographic, hospice, and community characteristics that might correlate with our outcome for children in the cohort. Demographic characteristics included age, sex, race (Caucasian or non-Caucasian), and ethnicity (Hispanic or non-Hispanic). To assess the hospice characteristics, we created measures of size (< 50 employees or >=50 employees), ownership (for-profit or nonprofit/government), organizational age (number of years licensed) and pediatric program (specialized pediatric hospice services). Community characteristics includes community household income (less than $50,000 annually or more than &50,000 annually), region (Northeast, Midwest, south, west), and urban/rural.
Data Analysis
Our analysis began by examining the descriptive statistics for all study variables in order to examine the data and test statistical assumptions. Percentages and means with standard deviations were used to describe the children in the cohort. We used a logistic regression model to explore the relationship between medical complexity and our outcome, while controlling for demographic and hospice characteristics. We accounted for the clustering of children within the hospice episodes. The years of the study were included to control for temporal changes during the study period. Robust standard errors were included in all analyses. The findings were reported as odds ratios and their 95% confidence intervals.
We also investigated the robustness of the findings by performing two sensitivity analyses on our outcome. First, we repeated the logistic regression analysis including only children who received any Medicaid waiver services (e.g., 1115, 1915). Second, we also repeated the analysis with only children who resided in states which were early-adopter of concurrent hospice care(Keim-Malpass & Lindley, 2017). These included 22 states: Alabama, Arizona, California, Delaware, Hawaii, Iowa, Maryland, Massachusetts, Michigan, Mississippi, Missouri, Nebraska, New Jersey, New York, North Carolina, Ohio, Oklahoma, Oregon, Texas, Virginia, Washington, and Wisconsin. All analyses were performed using Stata statistical software, version 15.0 (StataCorp LP, College Station, TX).
Results
Table 1 displays our sample characteristics. The final cohort in the study included 18,145 pediatric decedents from 2011 to 2013. Approximately 13% met the Kuo and colleague definition of medical complexity. Less than 50% had a complex chronic condition, 23% were technology dependent. Almost a third of the children had multiple complex chronic conditions (28%), while more than a third had a mental and/or behavioral disorder. The average age of children in the sample was 7.5 years. Sex and race were equivalent and 22% of children were Hispanic. The hospices used by the children frequently employed less than 50 employees (64%) and were for-profit (61%). They operated on average for over 18 years, and a third had a specialized pediatric program (34%). Most children resided in a communist with an average household income was greater than $50,000 (64%) and in the northeast (57%). A third of children lived in rural communities (33%).
Table 1.
Characteristics of Study Participants (N=18,145)
| Variables | n | % or Mean /SD |
|---|---|---|
| Medical Complexity | 2357 | 12.98 |
| Complex Chronic Condition | 8784 | 48.39 |
| Technology Dependence | 4160 | 22.92 |
| Multiple Complex Chronic Conditions | 5088 | 28.03 |
| Mental/Behavioral Disorders | 6195 | 34.13 |
| Covariates | ||
| Age | 18145 | 7.45 (6.33) |
| Sex | ||
| Male | 9290 | 51.22 |
| Female | 8855 | 48.78 |
| Race | ||
| Caucasian | 9767 | 53.81 |
| Non-Caucasian | 8378 | 46.19 |
| Hispanic | 4001 | 22.04 |
| Hospice Size | ||
| <50 employees | 11691 | 64.44 |
| >50 employees | 6454 | 35.56 |
| Hospice Ownership | ||
| For-Profit | 11113 | 61.26 |
| Nonprofit/Government | 7032 | 38.74 |
| Hospice Age | 18145 | 18.30 (9.82) |
| Hospice Pediatric Program | 6111 | 33.67 |
| Community Household Income | ||
| <$50,000/yr | 6455 | 35.56 |
| >$50,000/yr | 11690 | 64.44 |
| Region | ||
| Northeast | 10431 | 57.46 |
| Midwest | 4404 | 24.26 |
| South | 2132 | 11.75 |
| West | NA | NA |
| Rural | 6068 | 33.43 |
Note: SD, standard deviation; NA, not able to report due to data use agreement restrictions
Figure 1 shows the prevalence of pediatric concurrent hospice care use among study participants from 2011 to 2013. In 2011, 36% received this care, followed by 50% in 2012 and 31% in 2013. The overall trend was 34% of children received concurrent care versus standard hospice care during the study timeframe.
Figure 1.
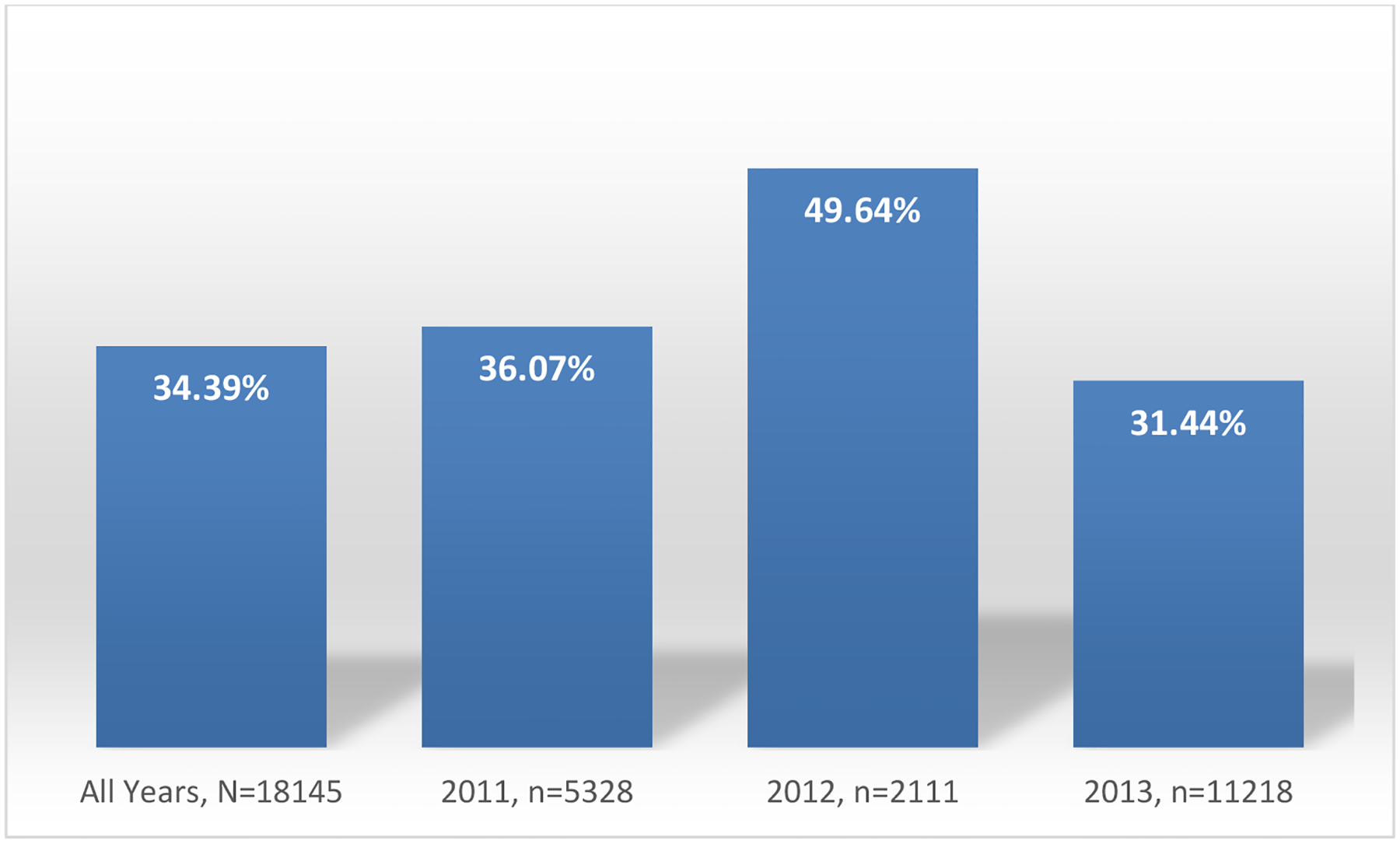
Use of pediatric concurrent hospice care, 2011 to 2013
Table 2 lists the results of the regression analysis estimating the association between medical complexity and concurrent hospice versus standard hospice care use, while holding the other variables constant in the model. Medical complexity was not related to concurrent care use. Children with medical complexity were not more like to use concurrent hospice care than standard hospice care. The four individual criteria of medical complexity, however, were associated to concurrent care use. A complex chronic condition was negatively related to concurrent hospice care (aOR 0.71, P<0.001). In other words, children with a complex chronic condition had greater odd of using standard hospice care versus concurrent care, compared to those without a complex chronic condition. Technology dependence was positively associated with concurrent care use, such that these children had almost twice the odds (aOR=1.20, P<0.05) of using concurrent care versus standard hospice care, compared to their peers. In addition, multiple complex chronic conditions (aOR=1.42, P<0.001) and mental/behavioral disorders (aOR=1.16, P<0.01) were positively related to concurrent hospice care use versus standard hospice, compared to their counterparts.
Table 2.
Regression Analysis of Concurrent versus Standard Hospice Care Use
| Variables | aOR | 95%CI | |
|---|---|---|---|
| Medical Complexity | 1.11 | 0.92–1.34 | |
| Complex Chronic Condition | 0.71 | *** | 0.64–0.79 |
| Technology Dependence | 1.20 | * | 1.22–1.65 |
| Multiple Complex Chronic Conditions | 1.42 | *** | 1.05–1.29 |
| Mental/Behavioral Disorders | 1.16 | ** | 1.03–1.42 |
| Covariates | |||
| Age | 1.11 | *** | 1.01–1.02 |
| Sex | |||
| Male | (ref) | ||
| Female | 0.96 | 0.89–1.04 | |
| Race | |||
| Caucasian | 0.95 | 0.87–1.03 | |
| Non-Caucasian | (ref) | ||
| Hispanic | 1.22 | *** | 1.11–1.39 |
| Hospice Size | |||
| <50 employees | (ref) | ||
| >50 employees | 0.98 | 0.89–1.09 | |
| Hospice Ownership | |||
| For-Profit | (ref) | ||
| Nonprofit/Government | 1.25 | *** | 1.10–1.41 |
| Hospice Age | 0.99 | 0.99–1.01 | |
| Hospice Pediatric Program | 1.19 | ** | 1.06–1.34 |
| Community Household Income | |||
| <$50,000/yr | 1.31 | *** | 1.18–1.46 |
| >$50,000/yr | (ref) | ||
| Region | |||
| Northeast | (ref) | ||
| Midwest | 1.74 | *** | 1.42–2.13 |
| South | 3.91 | *** | 3.24–4.73 |
| West | 2.27 | *** | 1.87–2.76 |
| Rural | 1.26 | *** | 1.14–1.39 |
Note: aOR, adjusted odds ratio
Note: Adjusted for study years
p <0.001
p <0.01
p <0.05
Other notable results were that age (aOR=1.11, P<0.001), Hispanic (aOR=1.22, P<0.001), non-profit/government ownership (aOR=1.25, P<0.001), pediatric program (aOR=1.19, P<0.01), community household income (aOR=1.31, P<0.001), Midwest (aOR=1.74, P<0.001), south (aOR=3.91, P<0.001), west (aOR=2.27, P<0.001), and rural (aOR=1.26, P<0.001) were associated with concurrent care use. No other factors were related to concurrent versus standard hospice care.
Table 3 shows the results of the sensitivity analyses. In the analysis that included only children who received any Medicaid waiver services, we found medical complexity and the 4 criteria performed similarly to the primary analysis with respect to direction and significance of findings. The only exception was technology dependence, which was not significantly related to concurrent care use. These results were the same for children who resided in early adopter states of concurrent hospice care. In general, these sensitivity results suggest that the findings from our primary analysis were robust.
Table 3.
Sensitivity Analyses
| Medicaid Waiver n=13233 | Early Adopter States n=15883 | |||
|---|---|---|---|---|
| Variables | aOR | 95%CI | aOR | 95%CI |
| Medical Complexity | 1.03 | 0.83–1.29 | 1.09 | 0.89–1.32 |
| Complex Chronic Condition | 0.69 | 0.61–0.79 | 0.72 | 0.64–0.80 |
| Technology Dependence | 1.18 | 0.97–1.43 | 1.18 | 0.99–1.39 |
| Multiple Complex Chronic Conditions | 1.33 | 1.11–1.58 | 1.39 | 1.19–1.62 |
| Mental/Behavioral Disorders | 1.34 | 1.0–1.28 | 1.12 | 1.00–1.25 |
Note: aOR, adjusted odds ratio
Note: Adjusted for all covariates and study years
p <0.001
p <0.01
p <0.05
Discussion
The goal of our study was to examine the prevalence of pediatric concurrent hospice care and the relationships between medical complexity and concurrent versus standard hospice care in a national study of Medicaid children at end of life. The project expands on past efforts to explain medical complexity by expanding the focus to those in hospice care. In our national sample, pediatric decedents used concurrent hospice care. Although, the percentages fluctuated between 2011 to 2013, more than a third of children used concurrent hospice care. In addition, the prevalence of medical complexity was relatively low given that the sample were at end of life. The results of our study shed important new evidence on connection between medical complexity and concurrent versus standard hospice care among a very vulnerable and understudied population.
The study results revealed that medical complexity defined as meeting all 4 criteria of medical complexity was unrelated to concurrent hospice care(Kuo, Houtrow, et al., 2016). Although 13% of children had a complex chronic condition, technology dependence, multiple complex chronic conditions, and mental/behavioral disorders, they were no more likely to use concurrent care than standard hospice care. Many of these children have survived extreme prematurity and other congenital problems at birth, and their families have often spent the child’s entire lifetime managing and navigating numerous health care professional, settings, and treatments(Larroque et al., 2008). It is possible that at end of life, these children and their families are primarily interested in hospice care for the benefits of pain and symptom management. They may not necessarily be seeking additional medical treatments under concurrent hospice care anymore. Opportunities to investigate the needs of children with medical complex and their families at end of life are needed, which might include a qualitative examination of medically complex children in hospice care.
Among the individual medical complexity criteria, it was interesting and unexpected that a single complex chronic condition was negatively associated with concurrent care use. Nearly half of patients overall had complex chronic conditions, but children with complex chronic conditions had lower rates of concurrent care than children without CCCs. In order words, children with a complex chronic condition were more likely to use standard hospice care. The pediatric literature is consistent with this finding which has shown a relationship between cancer, cardiovascular disease, and congenital anomalies and standard hospice enrollment(Lindley, 2016; Lindley & Newnam, 2017). One explanation is that the subspecialist who is treating the single complex chronic condition might only be aware of standard hospice care as an option for their patients. Although concurrent hospice care has been available for a decade, many clinicians, hospice providers, and families still do not know about the service. Recent evidence suggests that the wide variation in state-level implementation of concurrent care from 2010 to present might have led to lack of adoption due to silos in clinical knowledge related to the novel model of care(Laird, Mack, Cozad, Keim-Malpass, & Lindley, n.d.). Future research examining implementation of concurrent care at the clinical level is warranted.
The results of the present study suggest that technology dependence, multiple complex chronic conditions, and mental/behavioral disorders are independent predictors of concurrent hospice care among pediatric decedents. We found that children with multiple complex chronic conditions did have higher rates of concurrent care use relative to children with no or fewer conditions. In addition, mental and behavioral health conditions and technology dependence were associated with higher rates of concurrent care use. These findings suggest that concurrent care use occurred among a subset of complex and medically dependent population. The Affordable Care Act’s provision for Concurrent Care for Children was developed in part to help meet the need for high quality end-of-life care for these young children and their families(Keim-Malpass et al., 2013). Children under this provision can receive hospice services while also benefiting from potentially curative care and higher levels of medical support than hospice teams can traditionally provide. Thus, children who require ventilators, for example, need not give up more intensive nursing support in the home that can allow families respite to rest and care for other children. Children with functional limitations, high health care use, and substantial needs might benefit especially from this important care as they near the end of life.
Given its retrospective, non-experimental design, this study has limitations. First, although it controlled for two major causes of confounding through inclusion of demographic and hospice characteristics, it is possible that there may be the presence of unobserved confounding factors that may bias the estimates. Second, given that the cross-sectional variation is greater than the number of time periods, if measurement error exists within the medical complexity variables, then the bias caused by that error may be exacerbated by the inclusion of state-fixed effects. Given the way these variables were constructed, the likelihood of such measurement error is small. In addition, the pooled cross-sectional logistic analysis represents the most robust choice of statistical analysis given the selected data source and is demonstrated by consistent patterns of associations found within the sensitivity analysis. Third, the study sample was Medicaid children and the result cannot be generalized to children covered under other insurances. However, the nationally representative data set of children lends itself to conclusions about the use of concurrent care by terminally ill children within the United States. Finally, this study was based on data between 2011 and 2013. It is possible that family and provider views, along with cultural norms about concurrent hospice care may have shifted since the timeframe of this study. However, the study provides critical information on the initial years of ACA, Section 2302. Future research is clearly warranted that examines children in a current health care environment.
Despite these limitations, the findings from the study have implications for practice. We should note that concurrent care may not be right for every child and family. Some will benefit from the focus on purely palliative interventions provided by hospice; those who have decided to forgo life-prolonging or curative measures may not need concurrent care. Given concurrent care is in its infancy in terms of implementation, we do not yet know what the “right” rate of concurrent care for children may be. However, the rate of concurrent care in this nationally representative sample of children was low even among those with medical complexity. However, children with technology dependence represent an important sub-group for consideration because the practical support they require in the home is beyond standard hospice care and additional support from concurrent care services might be welcomed by many families. Therefore, in order to fully support terminally ill children and their families, those responsible for coordination of care should raise awareness about the potential benefits of concurrent care when appropriate.
Acknowledgements:
Special thanks to Ms. Jamie Butler for her assistance in preparing the manuscript.
Funding Source:
This publication was made possible by Grant Number R01NR017848 from the National Institute of Nursing Research (PI: Lindley). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Nursing Research or National Institutes of Health.
Contributor Information
Jessica Keim-Malpass, School of Nursing, University of Virginia, Charlottesville, Virginia 22908.
Melanie J. Cozad, Department of Health Services Policy and Management, University of South Carolina, Columbia, SC 29201.
Radion Svynarenko, College of Nursing, University of Tennessee, Knoxville, Knoxville, Tennessee 37996.
Jennifer W. Mack, Department of Pediatric Oncology and Division of Population Sciences, Dana-Farber Cancer Institute, Boston Children’s Hospital, Boston, MA 02214.
Lisa C. Lindley, College of Nursing, University of Tennessee, Knoxville, Knoxville, Tennessee 37996.
References
- Berry JG, Hall M, Neff J, Goodman D, Cohen E, Agrawal R, … Feudtner C (2014). Children with medical complexity and Medicaid: spending and cost savings. Health Affairs (Project Hope), 33(12), 2199–2206. 10.1377/hlthaff.2014.0828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen E, Kuo DZ, Agrawal R, Berry JG, Bhagat SKM, Simon TD, & Srivastava R (2011). Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics, 127(3), 529–538. 10.1542/peds.2010-0910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coller RJ, Lerner CF, Eickhoff JC, Klitzner TS, Sklansky DJ, Ehlenbach M, & Chung PJ (2016). Medical Complexity among Children with Special Health Care Needs: A Two-Dimensional View. Health Services Research, 51(4), 1644–1669. 10.1111/1475-6773.12416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feudtner C, Feinstein JA, Zhong W, Hall M, & Dai D (2014). Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatrics, 14, 199. 10.1186/1471-2431-14-199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfield LD, Brown DS, Allaire BT, Ross RE, Nicol GE, & Raghavan R (2015). Psychotropic drug use among preschool children in the Medicaid program from 36 states. American Journal of Public Health, 105(3), 524–529. 10.2105/AJPH.2014.302258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee on Palliative and End-of-Life Care for Children and Their Families. (2003). When Children Die: Improving Palliative and End-of-Life Care for Children and Their Families. (Field MJ & Behrman RE, Eds.). Washington (DC): National Academies Press (US). 10.17226/10390 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Dying in America: improving quality and honoring individual preferences near the end of life. (2015). Washington, D.C.: National Academies Press. 10.17226/18748 [DOI] [PubMed] [Google Scholar]
- Keim-Malpass J, Hart TG, & Miller JR (2013). Coverage of palliative and hospice care for pediatric patients with a life-limiting illness: a policy brief. Journal of Pediatric Health Care : Official Publication of National Association of Pediatric Nurse Associates & Practitioners, 27(6), 511–516. 10.1016/j.pedhc.2013.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keim-Malpass J, & Lindley LC (2017). Repeal of the affordable care act will negatively impact children at end of life. Pediatrics, 140(3). 10.1542/peds.2017-1134 [DOI] [PubMed] [Google Scholar]
- Kuo DZ, Berry JG, Glader L, Morin MJ, Johaningsmeir S, & Gordon J (2016). Health Services and Health Care Needs Fulfilled by Structured Clinical Programs for Children with Medical Complexity. The Journal of Pediatrics, 169, 291–6.e1. 10.1016/j.jpeds.2015.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo DZ, Goudie A, Cohen E, Houtrow A, Agrawal R, Carle AC, & Wells N (2014). Inequities in health care needs for children with medical complexity. Health Affairs (Project Hope), 33(12), 2190–2198. 10.1377/hlthaff.2014.0273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo DZ, Houtrow AJ, & COUNCIL ON CHILDREN WITH DISABILITIES. (2016). Recognition and management of medical complexity. Pediatrics, 138(6). 10.1542/peds.2016-3021 [DOI] [PubMed] [Google Scholar]
- Laird JM, Mack JW, Cozad M, Keim-Malpass J, & Lindley LC (n.d.). Examining variation in state Medicaid implementation of ACA: The case of Concurrent Care for Children. Health Affairs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larroque B, Ancel P-Y, Marret S, Marchand L, André M, Arnaud C, … EPIPAGE Study group. (2008). Neurodevelopmental disabilities and special care of 5-year-old children born before 33 weeks of gestation (the EPIPAGE study): a longitudinal cohort study. The Lancet, 371(9615), 813–820. 10.1016/S0140-6736(08)60380-3 [DOI] [PubMed] [Google Scholar]
- Lindley;, M.-D. K (2019). The Association between Poverty and Family Financial Challenges of Caring for Medically Complex Children. Nursing Economic$. [Google Scholar]
- Lindley LC (2011). Health care reform and concurrent curative care for terminally ill children: A policy analysis. Journal of Hospice and Palliative Nursing : JHPN : The Official Journal of the Hospice and Palliative Nurses Association, 13(2), 81–88. 10.1097/NJH.0b013e318202e308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC (2016). The effect of pediatric palliative care policy on hospice utilization among california medicaid beneficiaries. Journal of Pain and Symptom Management, 52(5), 688–694. 10.1016/j.jpainsymman.2016.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC (2017). Multiple Complex Chronic Conditions and Pediatric Hospice Utilization among California Medicaid Beneficiaries, 2007–2010. Journal of Palliative Medicine, 20(3), 241–246. 10.1089/jpm.2016.0227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC, Keim-Malpass J, Svynarenko R, Cozad MJ, Mack JW, & Hinds PS (2020). Pediatric concurrent hospice care: A scoping review and directions for future nursing research. Journal of Hospice and Palliative Nursing : JHPN : The Official Journal of the Hospice and Palliative Nurses Association, 22(3), 238–245. 10.1097/NJH.0000000000000648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC, & Lyon ME (2013). A profile of children with complex chronic conditions at end of life among Medicaid beneficiaries: implications for health care reform. Journal of Palliative Medicine, 16(11), 1388–1393. 10.1089/jpm.2013.0099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC, & Newnam KM (2017). Hospice Use for Infants With Life-Threatening Health Conditions, 2007 to 2010. Journal of Pediatric Health Care : Official Publication of National Association of Pediatric Nurse Associates & Practitioners, 31(1), 96–103. 10.1016/j.pedhc.2016.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley LC, Svynarenko R, & Profant TL (2020). Data infrastructure for sensitive data: nursing’s role in the development of a secure research enclave. Computers, Informatics, Nursing : CIN, 38(9), 427–430. 10.1097/CIN.0000000000000677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mack JW, Chen K, Boscoe FP, Gesten FC, Roohan PJ, Schymura MJ, & Schrag D (2015). High Intensity of End-of-Life Care Among Adolescent and Young Adult Cancer Patients in the New York State Medicaid Program. Medical Care, 53(12), 1018–1026. 10.1097/MLR.0000000000000437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mack JW, Chen K, Boscoe FP, Gesten FC, Roohan PJ, Weeks JC, … Schrag D (2013). Underuse of hospice care by Medicaid-insured patients with stage IV lung cancer in New York and California. Journal of Clinical Oncology, 31(20), 2569–2579. 10.1200/JCO.2012.45.9271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller EG, Laragione G, Kang TI, & Feudtner C (2012). Concurrent care for the medically complex child: lessons of implementation. Journal of Palliative Medicine, 15(11), 1281–1283. 10.1089/jpm.2011.0346 [DOI] [PubMed] [Google Scholar]
- Mooney-Doyle K, Keim-Malpass J, & Lindley LC (2019). The ethics of concurrent care for children: A social justice perspective. Nursing Ethics, 26(5), 1518–1527. 10.1177/0969733018765308 [DOI] [PubMed] [Google Scholar]
- Mooney-Doyle K, & Lindley LC (2020). Family and child characteristics associated with caregiver challenges for medically complex children. Family & Community Health, 43(1), 74–81. 10.1097/FCH.0000000000000245 [DOI] [PubMed] [Google Scholar]
- Mor V, Joyce NR, Coté DL, Gidwani RA, Ersek M, Levy CR, … Shreve ST (2016). The rise of concurrent care for veterans with advanced cancer at the end of life. Cancer, 122(5), 782–790. 10.1002/cncr.29827 [DOI] [PubMed] [Google Scholar]
- Mor V, Wagner TH, Levy C, Ersek M, Miller SC, Gidwani-Marszowski R, … Shreve S (2019). Association of expanded VA hospice care with aggressive care and cost for veterans with advanced lung cancer. JAMA Oncology, 5(6), 810–816. 10.1001/jamaoncol.2019.0081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy SL, Mathews TJ, Martin JA, Minkovitz CS, & Strobino DM (2017). Annual Summary of Vital Statistics: 2013–2014. Pediatrics, 139(6). 10.1542/peds.2016-3239 [DOI] [PubMed] [Google Scholar]


