Abstract
Background
All types of diabetes can damage the heart, blood vessels, eyes, kidneys, nerves and increase the overall risk of disability and premature death. Diabetes mellitus requires a range of self-care practices, scientifically recommended to control the glycemic level and maintain the patient’s health. However, perceived barriers that hinder patients from fully implementing these diabetes self-care practices and obstacles have not been thoroughly explored. Therefore, this study aimed to explore the barriers to diabetes patients’ self-care practices from the perspective of health care providers in two public hospitals in Harar City, Eastern Ethiopia.
Methods
Researchers conducted an exploratory qualitative study among 26 health care providers working in two public hospitals from March to June 2021. The study participants were recruited from different disciplines working on diabetes care. Interviews were conducted in the Amharic language until the saturation point was reached. The interviews were tape-recorded, transcribed, and translated to English. Each transcript was read, re-read, and then exported to ATLAS.ti 7 software for coding. Field notes were used to supplement verbatim transcriptions. Initial codes were generated. The consistency between the two coders and their alignment with research questions were checked and applied to all subsequent transcripts after reached on consensus. The thematic analysis was employed in line with the primary set research question.
Results
Researchers identified barriers to diabetes patients’ self-care practices such as system, health care providers, and patient-level. These barriers were categorized under three main themes: lack of organized diabetes care services, limited collaborative care practices, and perceived lack of knowledge on self-care practices. In addition, the lack of multidisciplinary team care, lack of training for health care providers on diabetes self-care practices, and availability of laboratory tests and diabetes medication were prominent barriers.
Conclusion
Multi-level barriers to diabetes patients’ self-care practices such as system, health care providers, and patients were identified. Therefore, interventions targeting proper service integration, building providers’ and patients’ capacity on diabetes self-care practices, and ensuring the sustainability of laboratory tests and medication supplies are essential. These interventions need to be accomplished through multi-level stakeholders’ engagement and one-to-one or group interventions covering the multi-level challenges.
Keywords: diabetes, self-care, barriers, health care providers, holistic care, Eastern Ethiopia
Introduction
Diabetes mellitus (DM) is a metabolic disorder characterized by the presence of hyperglycemia1 that occurs when the body cannot produce enough insulin or ineffective response to insulin.2,3 There are two significant categories of diabetes mellitus: Type 1 diabetes, which usually occurs in childhood, and Type 2 diabetes, which often occurs in adults, but gradually affects children and adolescents. Both types of diabetes can damage the heart, blood vessels, eyes, kidneys, nerves, increasing the overall risk of disability and premature death.3 Evidence suggests that Type 2 accounts for about 90% to 95% of all DM cases. In addition, the changes in population age, social, economic, cultural aspects, and degree of urbanization contribute to a more inactive lifestyle, and consuming an unhealthy diet leads to obesity.4
Globally in 2019, 9.3% (463 million) of people aged 20 to 79 had diabetes, with the number of people with diabetes predicted to rise 10.2% (578 million) by 2030, and more than three quarters (79.4%) live in low- and middle-income countries.4 Additionally, data indicate that around four million deaths were attributed to diabetes annually.1
In Ethiopia, diabetes increases5 while most people remain undiagnosed until serious complications become evident.6 In 2017, the projected national diabetes prevalence among people aged 20–79 was 5.2%, and there were 2.6 million diabetic cases in the country.2 Likewise, a recent systematic review indicated that the magnitude of diabetes ranged from 2.0% to 6.5%.7 As a result, the Federal Ministry of Health (FMoH) conducted a national survey to determine the prevalence and common risk factors to inform public health policy. At the same time, the ministry endorsed further investigation of determinant factors and pocket-sized studies to generate evidence locally for the implementation of NCD prevention and control activities.8 Moreover, an analysis of policy was made, and strategy gaps were suggested to develop targeted strategies to reduce behavioral risk factors in Ethiopia.9
Patients with diabetes have an increased risk of morbidity and mortality.10 In addition, they have the risk of developing other chronic non-communicable or infectious diseases.1 Therefore, continuous and regular quality care with multiple risk-reduction strategies is adequately initiated and practiced.1,11 Diabetes self-management education, medical nutrition therapy, psychosocial care, and self-care have paramount importance in reducing their risks.12 Diabetes self-care behaviors include healthy eating, regular physical exercise, proper medication follow-up, blood glucose self-monitoring, problem-solving skills, coping with the illness, monitoring disease progression, and eye care.13–15 Commitment to these activities can reduce the risk of complications and improve quality of life.16–18 However, despite these facts, diabetes self-care has been poorly practiced,19 contributing to suboptimal glycemic control20 and resulting in an increased risk of overall diabetes complications.21–23
Therefore, active engagement of the patients and health care providers (HCPs) is crucial for high-quality healthcare services. Active participation helps to establish a partnership, have shared decisions, and encourage the patients to own their lifestyle goals and action plans.24,25 Thus, improving self-care behaviors is the basis for improving the health status of patients with diabetes.26,27 However, there is limited evidence indicating the barriers to diabetes patients' self-care practices that requires further exploration from various perspectives. Therefore, this qualitative study aimed to explore these barriers from the perspective of the health care professionals in two public hospitals found in Harar City, Eastern Ethiopia.
Furthermore, this study has significant implications for nurses, which comprise the majority of the health care providers in the country.28 The increase in diabetes patients may require nurses who educate the patients to manage their disease. Along with this, providing standard, evidence-based, and cost-effective care can improve the health care quality and the patient’s health condition.29
Methods
The methods are based on the consolidated criteria for reporting qualitative research (COREQ) framework, consisting of 32-items mainly grouped into three domains: research team and reflexivity, study design, and data analysis and reporting. The checklist helps report essential aspects of the research team, study methods, context of the study, findings, analysis, and interpretations.30
Research Team and Reflexivity
Two researchers with experience in qualitative research methods and an understanding of the subject matter were used to collect data. They are also proficient in both the Amharic and English languages. One of the researchers’ team has a master’s degree in nursing specializing in chronic diseases, while the others had a Ph.D. degree in Public Health and Nursing with the academic rank of assistant to associate professors. There were no prior interactions between the researchers and participants before the commencement of the study. Therefore, the potential influence of unbalanced power between researchers and participants was minimized. The modifications we made included the appropriate use of medical jargon, vocabularies, tone of voice, and interview mode since the participants were from different professions, levels of education, and gender.
Study Design and Period
The research team conducted an exploratory qualitative study utilizing health professionals working in diabetes care in two hospitals through in-depth interviews. The study was conducted from March to June 2021.
Study and Data Collection Settings
Harari Region is found in eastern Ethiopia, and the capital City is Harar, located 526 kilometers away from Addis Ababa, the capital city of Ethiopia. There are two public hospitals in the city, Hiwot Fana Specialized Comprehensive Hospital and Jugal Hospital, where the study was undertaken. Both hospitals provide services for the entire community of eastern Ethiopia. The hospitals have several departments that deliver services. These include Medical, surgical, pediatric, obstetrics, gynecology wards, Intensive Care Units (ICUs), outpatient departments (OPDs), radiology, pathology, laboratory, and pharmacy departments. In addition, the hospitals also serve as teaching centers for health and medical sciences students. More than 2707 people with DM are followed in the outpatient clinics of the hospitals. Thirty nurses, 12 residents, 13 internists, and 13 general practitioners are involved in DM care in the OPDs and medical wards. The interviews were conducted in separate rooms of the hospitals for the suitability, confidentiality, and assuring privacy.
Participants
Participants were the health care providers (HCPs) who directly engaged in providing diabetes care at the OPDs, medical ward, and medical ICU in the last three months. The nurses usually facilitate documentation and follow-up while ward nurses participate in medication administration and patient education. General practitioners (GPs) and internal medicine resident students evaluate the patients at OPDs and in the wards assisted by consulting internists. Among physically communicated HCPs, two physicians were dropped out due to their busy schedules.
Sample Size and Sampling Strategy
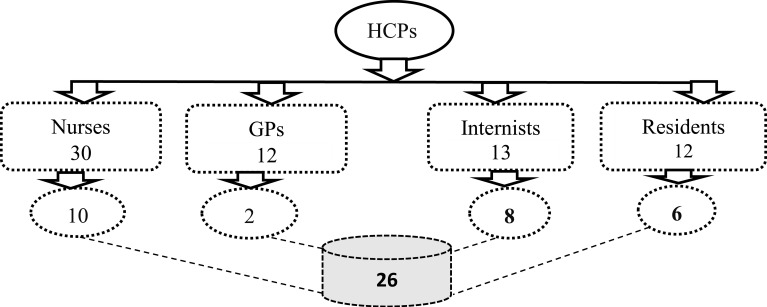
The study participants were recruited from nurses, general practitioners, internal medicine resident students, and general internists using the purposive sampling technique. The inclusion criteria were having experiences and direct involvement in diabetes care as primary caregivers. There were 13 internists, 12 resident students, 14 general practitioners, and 30 nurses working in outpatient departments, medical wards, and medical ICU of both hospitals. The participants were primarily approached by phone, and then the face-to-face discussions were made. Finally, they were invited by the research team for interviews at a jointly arranged time (Figure 1).
Figure 1.
Schematic presentation of sampling strategy of the health care professionals working in Hiwot Fana Specialized Comprehensive Hospital and Jugal Hospital, Harar, Eastern Ethiopia.
Abbreviations: HCPs, health care providers; GPs, general practitioner.
Data Collection Procedure
Written informed consent was obtained from all the interviewees on the interview day before initiating the interview. The interviews were carried out using pre-tested semi-structured guides. The interview guides were prepared in English and translated into the Amharic language by a bilingual translator. This interview guide contains demographic information of participants and a series of open-ended questions, mainly concentrating on the barriers to diabetes self-care practices. These were sample questions: “Please would you tell me about diabetes self-care?”; “How are you assisting your diabetes patients in achieving optimal self-care practices?”; “What are the existing barriers to diabetes patients’ self-care practice?”, and “How do these barriers independently hinder patients’ self-care practices?” All these questions were used for initiating in-depth interviews. In addition, the participants were encouraged to describe the detail of the challenges through probing where it was necessary. Two voice recorders were used to record interviews simultaneously for backup in case of recording problems. In addition, field notes were taken to supplement the verbatim transcription. Each interview took approximately 30 to 60 minutes. Accordingly, the interviews were continued until the saturation point was attained.
Data Management
The in-depth interviews were recorded, transcribed daily by the interviewer and note-taker, and translated into English by two bilingual research team members. The data were analyzed following the thematic analysis approach.31 First, the transcripts were read and re-read to be familiarized with the data’s depth, breadth, and contents, then exported into ATLAS.ti 7 software for coding. Initial codes were generated to identify the data features in line with the research questions, and the consistency of codes between the two coders was checked. After reached on a consensus about coding and the codes were applied to all subsequent transcripts. The preliminary generated codes with similar ideas were grouped into thematic headings. Those potentially identified themes were reviewed, refined, split up, or combined based on their relevance to the research questions. Then themes were defined and named. Finally, the researchers produced the report by linking memos with the quotations and finalized the write-up.32 The quality of this study was assured through several ways: first, the interview guide questions were developed from existing literature, gaps identified during quantitative survey we did and evaluated by the teams who have sufficient experience in diabetes care and qualitative research. Secondly, the respondents validated the summarized information at the end of each interview. Thirdly, the same interview guide/questions were used to maintain the consistency of the data across all the interviewees. Lastly, after completing the analysis, the key findings were presented to all participants for further validation and feedback.
Ethical Clearance
This study explored the views of health care providers towards the barriers of diabetes patients’ self-care practices through an in-depth interview. Several actions were put in place to assure the study participants’ privacy, comfort, and dignity. Each interviewee was conducted in a separate private office. Recording interviews took place after written informed consent was obtained from an individual interviewee that included publication of anonymized responses. They were assured that data or information obtained from them were kept confidential except for authorized researchers. Personal identifiers were not used. Ethical approval was obtained from the Institutional Health Research Ethics Review Committee of the College of Health and Medical Sciences, Haramaya University (IHRERC). We also checked that this study complies with the Declaration of Helsinki.33
Results
Sociodemographic Characteristics of Study Participants
A total of 26 in-depth interviews were conducted with nurses, general practitioners, internal medicine resident students, and internists who have engagement in diabetes care in the two public hospitals. The mean age of the participants was 30.4 ±5.9 years, and most of the participants 21(80.8%) were males (Table 1).
Table 1.
Demographic Characteristics of the Study Participants
| Variable | Category | Number | % |
|---|---|---|---|
| Age, year | Mean(±SD) | 30.4±5.9 | – |
| ≤30 | 15 | 57.7 | |
| >30 | 11 | 42.3 | |
| Sex | Male | 21 | 80.8 |
| Female | 05 | 19.2 | |
| Professional Category | Nursing | 10 | 38.5 |
| Medicine | 16 | 61.5 | |
| Level of Education/Specialty | Nurses (Diploma to MSc) | 12 | 46.2 |
| Internal Medicine Resident students | 06 | 23.1 | |
| Internists | 08 | 30.7 | |
| Working Experience, year | Mean(±SD) | 6.4±4.7 | – |
| ≤5 | 15 | 57.9 | |
| >5 | 11 | 42.3 |
Barriers to Diabetes Patients’ Self-Care Practices from Health Care Providers Perspective
The analysis of barriers to diabetes patients’ self-care practices from perspectives of HCPs in nursing and medicine disciplines was conducted following the typical thematic analysis approach. Though there was a complex interrelationship between themes and sub-themes, the findings were systematically presented. Initially, 28 subthemes emerged in the early stage of analysis, and later, these were condensed to 14 sub-themes. Among all sub-themes, six were categorized under the central theme named lack of organized diabetes care services, which corresponds to the health care system, whereas four were categorized under the theme of limited collaborative practices, which corresponds to health care providers related barriers. The last three sub-themes belonged to lack of knowledge about diabetes and its care which corresponds to diabetes patient-level barriers. Each sub-theme was presented in the table with its description. Moreover, the theme and sub-themes were adequately explained in the text (Table 2).
Table 2.
Summary of Barriers to Diabetes Patients’ Self-Care Practices from Health Care Providers’ Perspectives in Hiwot Fana Specialized Comprehensive Hospital and Jugal Hospital, Harar, 2021, Eastern Ethiopia
| Category | Main Themes | Sub-Themes | Descriptions |
|---|---|---|---|
| Health Care System | Lack of organized diabetes care services | Lack of well-integrated services for diabetes care Unavailability of experts (Endocrinologists) Lack of in-service training of health workers Lack of trained diabetes nurse educators Inconsistent availability of laboratory tests and drugs Poor response to Covid-19 pandemic |
Arrangement of services entry points into one corner for easy access Sub-specialists who make the correct diagnosis and treatment On-job training for health workers about diabetes care Trained nurses who educate and assist patients in self-care practices HbA1c, lipid panel, electrolytes, and organ function tests Lack of home care, glucose monitoring, and telephone consultation |
| Health Care Providers | Limited Collaborative Practices | Lack of multidisciplinary team DM care Unavailability of holistic care provision Inadequate patient-centered diabetes care Limited and contradictory information provision |
Services delivered by interprofessional teams of HCPs Package of cares that addresses the whole aspects of patients Care considers patient’s interests, values, and decision Unstructured and incomplete diabetes care information |
| Patients with Diabetes | Lack of knowledge about diabetes and its care | Misperception about diabetes and its care Lack of self-motivation to practices self-care Incapable of changing dietary habits Low health literacy level |
Misunderstanding about DM and its life-long self-care practices Lacks self-courage and inspiration to engage into self-care Eat their usual diet or any diet they get due to food insecurity Unable to read, write, and understand health information |
Theme One: Lack of Organized Diabetes Care Services
Lack of Well-Integrated Services for Diabetes Care
The informants stated that the diabetes care-related services are not well-integrated. The service areas are not well aligned; the patients move from one building to another to get laboratory and pharmacy services. Electronic communication means that serve for easy exchange of patients’ information among the units are not established. The patients must often wait for long periods at each service entry. On top of this, the lack of proper handling and documentation of the patients’ medical records affects clinical decision-making. There are also delay in the referral and consultation system between specialty clinics. Periodical evaluation for eyes, teeth, kidneys, and heart are not adopted. The services are poorly organized, not easily accessed, not centered on the patients’ multiple needs, and do not acknowledge their role in their health issues. As a result of these, the patients interrupted the regular follow-up. The support and services obtained from health care providers were ceased, then they were discouraged from practicing self-care. In support of this, one of the participants stated:
“The services which are given in the record room, pharmacy and laboratory facility for diabetes patients are not synchronized to one corner or around the endocrinology unit.” (Participant 10, Internist)
“I know a patient who was admitted to the medical ward for treatment but developed gangrene over his lower leg. He has spent 15 days without any treatment due to an ineffective referral system between medical and surgical wards.” (Participant 8, BSc nurse)
Unavailability of Experts (Endocrinologists)
Some participants reported that the unavailability of experts affects overall diabetes care in some way. For example, the lack of endocrinologists significantly weakens collaborative efforts among departments. It also contributes to frequent interruption of laboratory services related to diabetes and an unsustainable supply of essential diabetes medications that affect the continuity of diabetes self-care practices. Moreover, they expressed that this lack worsens integrating the diabetic services under the Endocrinology unit, which might be a base for comprehensive diabetes care.
“The existing DM care-related problems will decrease at least by 50% if an Endocrinologist is available so that the correct diagnosis and treatment can be made. All services rendered for patients with diabetes can be organized, and the continuity of the services can also be guaranteed” (Participant 12, Resident)
Lack of Diabetes Nurse Educators
Some interviewees reflected that diabetes nurse educators are a neglected component of the current ongoing service in the two hospitals. As a result, there were no qualified nurse educators. Timely identifying the patient’s health care needs and working collaboratively with the patient and healthcare provider team to develop the most appropriate treatment plan and nutrition education might require diabetes nurse educators. In addition, a qualified nurse educator works to increase the patients’ understanding of diabetes self-care practices. Furthermore, they promote self-care, identify barriers, and supporting patients with diabetes in acquiring skills that enable them to carry out their diabetes self-care.
“The lack of a dedicated nurse who is specifically trained for diabetes management is significant as they can contribute a lot.” (Participant13, Internist)
“Diabetes nurse educators are required to assist the patients in carrying out diabetes self-care practices.” (Participant 14, BSc Nurse)
Lack of In-Service Training of Health Care Providers
The participants described that most health professionals directly engaged in diabetes care had no additional training on diabetes management though there is integrated national guideline for non-communicable diseases. As a result, nurses, residents, and internists reported a lack of the most updated information on diabetes. The nurses expressed that they lack adequate knowledge about diabetes, and self-care dimensions. In addition, they explained the lack of basic communication skills, counseling skills, and knowledge about recommended diabetes diets specific to the patients’ socio-cultural context. The communication skills may help to establish an excellent rapport with the patients. The health care providers who lack of these knowledge and skills cannot adequately teach and counsel the patients to motivate them to perform their self-care.
“I have no additional and adequate training on diabetes management. I only try to apply directly the sciences that are in the textbook. The communication skill is also an important skill by itself, and this directly benefits the patients.” (Participant 3, General Practitioner)
“I have not been trained to educate, counsel or provide diabetes self-care other than the training I received during my baccalaureate study.” (Participant 6, BSc Nurse)
Inconsistent Availability of Laboratory Tests and Essential Drugs
Many participants expressed that HbA1c, lipid panel, and electrolyte tests are not consistently available despite HbA1c being the most reliable and good indicator of glycemic control. In addition, a lipid panel is helpful to assess the risk of cardiovascular problems. They explained that diabetes ketoacidosis (DKA) is managed without appropriate blood glucose monitoring, urinalysis, and electrolyte tests. In addition, there is a lack of glucometers and urine dipsticks for bedside monitoring. These tests are available but costly in private hospitals. This irregularity adversely affects the success of diabetes self-care.
“Recently, HbA1c test was started in our hospital, I am requesting now, but I am not requesting a lipid panel although it is indicated for patients with diabetes due to its unavailability.” (Participant 12, Resident)
Almost all the participants reported a shortage of essential medications, such as insulin. Patients who live in remote areas cannot obtain sufficient prescriptions to reduce unnecessary visits and expenses. In addition, regular insulin for DKA management is not consistently available. Participants reported that patients with diabetes do not have access to newer and safer medications. The patients who have no health insurance certificate could not get free Lente insulin. They are obligated to purchase their insulin from the private pharmacy where they do not receive comprehensive diabetes care, resulting in poor glycemic control.
“But now, the patients will get only two vials of insulin per month. Even if I prescribe for three months, no one supplies them.” (Participant 5, Resident)
“There is no supply of other safer medications other than metformin and Glibenclamide” (Participant 11, Internist)
“Medication supply is a big challenge. Soon we started to manage DKA with regular insulin; we heard the news that the stock ran out. Besides, those who do not have health insurance cannot get Lente insulin and are forced to use only regular insulin or buy from a private pharmacy”. (Participant 21, BSc Nurse)
Poor Response to Covid-19 Pandemic
Many of the participants witnessed a significant disruption of the routine care of diabetes during the Covid-19 pandemic. Diabetic patients discontinued their regular follow-up and blood glucose checking at the health facility, and most patients do not have a glucometer at their home; they were buying and taking their medication from the private pharmacy without knowledge of their glycemic control. In addition, as the pandemic progresses, there has been an increase in admissions due to acute diabetes complications. One coping strategy during the pandemic was to give several months’ worth of prescriptions; however, there was a shortage of medications in the hospital. Furthermore, no remote electronic consultation (media, telephone, or other means) revealed the lack of resources and readiness, resulting in a poor response to DM self-care. Hence, the patients were not able to carry out their diabetes self-care at home.
“Many patients discontinued their follow-up, medications, and glucose monitoring, and no alternative home-based service delivery was arranged.” (Participant 6, BSc Nurse)
Theme Two: Limited Collaborative Practices
Lack of Multi-Disciplinary Team Care
Almost all respondents reflected that currently, the patients are not receiving the multi-disciplinary team care approach. As a result, this practice has been neglected among different disciplines and within the same discipline. For example, some participants stated that patient care and decision-making rely on one discipline that does not constitute the provision of comprehensive diabetes self-care services. On the other hand, some mentioned that a multidisciplinary team remains unattainable when one does not appreciate the contribution of others in the team.
“Diabetes care is continued with none of the nurses, nutritionist, psychologist’s involvement.” (Participant 9, Internist)
“Nurse can contribute a lot in diabetes self-care practices. But our misperception is that we as physicians can address all things”. (Participant 13, Internist)
Unavailability of Holistic Care Provision
Most of the participants expressed that diabetes patients visit the health facility to get a package of services. The patients might have concomitant social, psychological, or emotional problems which necessitate holistic interventions. The diabetes care currently provided is not comprehensive. It is targeted to achieve glycemic control, making patients lose confidence in the services. While the patients’ multiple needs are left unaddressed, they are dissatisfied and demotivated to have diabetes self-care practices.
“No doubt, holistic care benefits the patients, but our primary target is controlling blood glucose so that the patients received incomplete services and failed to stick to suitable self-care practices.” (Participant 5, Residents)
“Holistic care requires a multidisciplinary approach. This inclusive approach is required to address multi-sided problems via diabetes self-care practices.” (Participant 6, BSc Nurse)
Inadequate Patient-Centered Diabetes Care
Most participants stated that much of the diabetes care responsibilities go to the patients themselves—this demands active involvement in their care. However, the implementation has limitations. They believed that the current care provision is provider-centered, limiting the patients’ interests and shared decision-making roles. The participants also reported perceived reasons for non-patient-centered care, such as high patient load and inability to establish a patient partnership. In addition, some participants reported that it would be challenging to implement patient-centered care when patients have insufficient knowledge about care options. However, most participants appreciated that diabetes self-care practices are necessary and best achieved through the consistent implementation of patient-centered care.
“I do not fully involve all patients in their care issues. It depends on the patient’s ability to understand my instructions.” (Participant 4, General Practitioner)
“If I consider patients’ preference and allow them to decide on their care, almost all of them prefer to take the pill rather than insulin injection.” (Participant 9, Internist)
Limited and Contradictory Information Provision
Almost all participants reported that they provide limited, inconsistent, and insufficient information. This limitation does not prepare the patients to be fully aware of diabetes and engage in self-care practices. They outlined that the failure to convey adequate diabetes education information to their patients is attributed to health care providers’ lack of adequate knowledge and language barriers. This study setting was a teaching hospital, where the students of different disciplines with varying knowledge levels about diabetes self-care practices were engaged in service provisions. Furthermore, there is a lack of educational resources, such as TV programs and leaflets, to facilitate learning about self-care practices.
“There is insufficient information provision about proper care and available treatment options.” (Participant 1, Resident)
“Some of the nurses have a language barrier while others lack adequate knowledge to guide and support the patients in self-care practices.” (Participant 7, Diploma Nurse)
Theme Three: Lack of Knowledge About Diabetes and Its Care
Misperception Towards Diabetes and Its Care
The interviewees involved in this study felt that most diabetes patients under their care have misperceptions about the nature of DM and its lifelong self-care practices. The patients perceived diabetes as if diabetes is a curable disease. As a result, they discontinued their medication once their health condition improved. Moreover, they prefer to take herbal medicines rather than modern medicines. Therefore, they experienced poor glycemic control and recurrent diabetes emergencies. This misperception resulted from a lack of appropriate information from untrained nurses and busy physicians.
“Some of the diabetes patients believe that DM is shortly curable. Then, they discontinue their follow-up after getting treated for months.” (Participant1, Resident)
“Some of the diabetes patients have the misunderstanding about the disease course and its treatments so that they discontinued their medication, and search for the herbalists.” (Participant 26, BSc Nurse)
Lack of Self-Motivation to Practices Self-Care
Many interviewees expressed that most diabetes patients are not interested in integrating diabetes self-care practices into their daily lives. The healthcare providers associated the lack of self-motivation with a lower literacy level and awareness about diabetes self-care practices. Additionally, it was also noted that the patients have never received structured and adequate information to potentially increase their motivation and confidence to make an informed decision. The chronic nature of diabetes causing them to lose focus and motivation to integrate self-care practices into their daily life.
“Patients with diabetes have lower awareness about the disease and lack motivation for diabetes self-care practices”. (Participant 1, Resident)
Incapable to Change Dietary Habits
Most patients with diabetes consistently consume the same type of diet as expressed by many of the subjects. While some patients are resistant to modify their usual diets, others are more compliant to change their diets. In addition, some patients have a shortage of food; as a result, they eat any food they can access without choices. Such non-adherence to dietary self-care recommendations leads to uncontrolled blood glucose and increases the risk of diabetes complications. The following interview transcript can ascertain this.
“Most of the patients do not know diabetes diet. Some are resistant to change their habits. E.g., if it is ‘injera, they always eat ‘injera.’ If it is bread, they usually eat the bread. They have no experience of eating varieties of diet.” (Participant 3, BSc Nurse)
“Socioeconomic condition of the patients is another serious challenge that put them difficult to eat healthy diets that do not increase blood sugar.” (Participant 8, BSc Nurse)
Low Level of Patients’ Health Literacy
The participants expressed that most diabetes patients were uneducated; they lacked functional, interactive, and numeracy skills. Diabetes patients are unable to read, write, and understand essential information about their health. Hence, they cannot follow the health care provider’s instructions, including the dose of medications. Additionally, as it was expressed, there is inadequate health information provided by health care providers. They also felt inadequate to provide relevant and up-to-date information for diabetes patients to maintain self-care practices.
“The majority of patients who came from rural areas are not educated. They are not able to understand medication instructions. They do not know numbers to take the right dose of insulin even after they are demonstrated.”. (Participant 3, BSc Nurse)
Discussion
This exploratory qualitative study was conducted on barriers to diabetes patients’ self-care practices. The findings suggested that lack of well-integrated services, unavailability of Endocrinologists, lack of in-service training for health care providers, lack of trained diabetes nurse educators, inconsistent availability of laboratory tests and DM medications, and poor response to Covid-19 pandemic were health care system barriers. Moreover, lack of a multi-disciplinary team, unavailability of holistic care, inadequate patient-centered care, and limited and contradictory information provision were barriers related to health care providers. Lastly, the patients’ related barriers included lack of self-motivation, misperception about the disease and its treatment, low literacy level, and inability to modify dietary habits, which were barriers to the diabetes patients’ self-care practices.
The lack of well-integrated services for diabetes care was found a significant barrier. The services rendered from each department, such as the Endocrinology unit, record room, laboratory, and pharmacy, were fragmented. There was also a poor referral system for getting specialty care such as neurology, ophthalmic and dental care, hindering the patients’ self-care practices. Previous evidence showed that integrating services improves the quality of care, patient satisfaction, quality of life, and system efficiency. The fragmented and poorly integrated services lead to poor diabetes care outcomes.34,35 The provision of comprehensive care necessitates integrated health care services.36 This finding is essential for hospital administrators to integrate diabetes care services to facilitate easy access and enhance the diabetes patients’ service-seeking behavior and satisfaction.
The unavailability of Endocrinologists who provide specialized services was a barrier to diabetes self-care practices. This finding was in line with a study conducted in Ghana that identified the lack of Endocrinologists affected the quality of care11 when there were complex diabetes cases.37,38 Furthermore, several studies showed that Endocrinologist-based care, both as a consultant or DM care team, significantly reduces the length of hospital stay.39,40 However, the management of chronic diseases might not draw the attention of stakeholders like infectious diseases. Consequently, there are few specialists in the country. Moreover, telehealth could be an alternative solution to increase patients’ access to expert care if feasible, and scaling up an enrollment for the endocrine sub-specialty is essential.
We identified that a lack of adequate in-service training of health care providers was an existing barrier to diabetes self-care. Evidence from sub-Saharan African showed that health care providers had inadequate training on diabetes care.41 For example, a recent study in Nigeria revealed that physicians treated diabetes patients without in-service training after they graduated from medical school, significantly hindering the patients’ self-care practices.42 Similarly, another review indicated a limited knowledge of nurses in diabetes care associated with a lack of additional in-service training on diabetes29 which adversely influences the provision of quality diabetes care.43 However, this finding contradicted the national action plans that endorsed the training of health professionals to provide quality diabetes care.44 In our context, most in-service training has been highly donor-based so that it is not sustainable. Moreover, the stakeholders might not incorporate in-service training into the national health care system plan.
The lack of diabetes nurse educators was one main barrier voiced by the interviewees. Diabetes patients’ education is the foundation of diabetes care. In most settings, nurses are trained to assist diabetic patients in establishing healthy lifestyles.45 Therefore, those nurses trained for diabetes care could better educate and support the diabetes patients to accomplish their diabetes care.29,46 These in turn improves clinical outcomes, quality of life,47,48 and satisfaction of people with diabetes.49 The nurse population in the study setting was the majority with ample clinical experience, but they were the less utilized healthcare professionals. Therefore, extending the nurse’s role with adequate training is cost-effective, and it is critically important to facilitate patients’ access to diabetes education to enrich their knowledge of diabetes self-care practices.50
Inconsistent availability of laboratory services and essential medications were potential barriers to diabetes self-care practices. This finding was in line with another similar study conducted in Cambodia, where laboratory tests and supplies of essential medications scarce.51 Several other studies also reported how laboratory and medications unavailability likely deter diabetes self-care practices.11,43,52 Although the national guideline recommends a periodical screening of HbA1c, lipid panel, and urine analysis,53 blood glucose and other patients’ conditions were not consistently monitored. In addition, the patients could not purchase the medications from the private pharmacies to aid self-care practices. Consequently, the glycemic goal remains unattainable for the patients, which significantly increases the risk of long-term diabetes complications. This problem was made worse by the recent Covid-19 global pandemic, which shared many of the same resources and impeded the constant supply of laboratory tests and essential diabetes medications.
The poor response of the Covid-19 pandemic was found to be a barrier to ensure continuity of diabetes self-care practices, manifested through discontinuation of follow-up and monitoring blood glucose levels.54 This finding was consistent with a study in Wuhan, China, and a brief report of Covid-19, which indicated several clinical follow-ups were postponed. The patients had been under stress, but not have support through digital health services, and physical activity was poorly performed.55,56 However, it is well known that even if numerous related studies were conducted, its effects were wide-ranging and continuing, and the related knowledge continues. Hence, further exploration will be required to distinguish its impact on diabetes self-care practices.
The lack of multidisciplinary team-based DM care was another barrier to diabetes self-care practices. This finding was congruent with a study from Ghana that reported that the lack of multi-disciplinary teams negatively affects the diabetes patients’ self-care practices.11 Many findings from the developed countries indicated the availability of multi-disciplinary team-based diabetes care,57–60 which hastened the glycemic target and shortened the length of stay in hospitalized patients.61 Moreover, the multi-disciplinary team approach significantly improves the psychosocial and clinical outcomes in diabetes patients.62,63 On the other hand, ineffective multi-disciplinary care can negatively affect the patients’ safety and resources through fragmented care.64 Though integrating several disciplines for complex diabetes care received wide recognition, there was a delay in launching the multi-disciplinary team care in the study setting. This discrepancy might be that many developing countries were suffering from infectious diseases which might not equally deserve integrated multi-disciplinary care as chronic non-communicable diseases with various complications and co-morbidities. This means that a few years ago, chronic non-communicable diseases may not be perceived as a priority health problem of the country.
The unavailability of holistic care provision was a significant barrier identified which agreed with a study done in Mauritius that holistic care lacked much attention and focused on the drugs-based model.65 The holistic care approach benefits the patients by giving equal weight to their physical, psychological, social, and spiritual well-being.66 A study in Iran showed a higher level of satisfaction of patients with holistic care.67 In this study, the concept of holistic care is well known by health care providers but it was not applied to practice. First, most medical and nursing education focused on the physical needs than the biopsychosocial needs of the patients. Therefore, they only dealt with treating the physical problems in their practical attachments. Secondly, the nurses spend much of their time on other routine care, such as monitoring vital signs, bed making, and assisting physicians than assessing and addressing the patients’ needs through the nurses’ care plans.
Inadequate patient-centered care (PCC) was a barrier to diabetes self-care practices against the existing guidelines and international recommendations.63,68 Our findings agreed with the growing evidence from Sub-Saharan African countries where patient-centered care remains poorly implemented.69,70 However, the role of patient-centered care is a well-recognized dimension of quality health care.68 The ADA and European Association for the Study of Diabetes (EASD) consensus report highlights the PCC’s role in enhancing the patients’ engagement in diabetes self-care practices.25 The most recent study in the Netherlands reported that PCC increased patients’ activation level, diabetes perceptions, and improved clinical outcomes.71 American Diabetes Association highlights that patient-centered care is one of the priority areas to achieve optimal diabetes management.72 The present findings imply the need for the health care reform to change from provider-center to a patient-centered care model that warrants patients’ autonomy and guides the decision-making about their health care. Furthermore, it also proposes advocating patient-centered care and its successful execution and transformation into practice.
There was limited and contradictory diabetes self-care information for the patients due to language barrier, lack of diabetes self-care knowledge, lack of in-service training of health care providers, and lack of educational resources (guideline, leaflets and posters). The current finding was consistent with previous evidence that the language barrier,73 lack of training, having limited knowledge, and lack of confidence to care for patients with diabetes complications51 though they expected to have better diabetes self-care knowledge to treat and teach the patients.74 This might be due to non-adherence to the national guideline so that the health care providers transmit incorrect information, which interferes with patients’ self-care practices. Another reason might be that the study settings are training centers for health and medical sciences students with different years of study and diverse knowledge levels that could expose the patients to inconsistent and contradictory information.
The patients’ misperceptions about the treatment and self-care practices of diabetes mellitus were prominently revealed. Some felt cured and discontinued their medication after months of treatment, whereas others used herbal medicine. This is in line with a recent review done in Sub-Saharan Africa revealed that many patients had a misperception about diabetes treatment, and used herbal medicines are good treatment and opted as one alternative therapy,75 whereas a study in southern India indicated that nearly half of them perceived that diabetes is a curable disease.76 A study conducted in Taiwan identified misperceptions that insulin affects the kidneys and eating vegetables can regulate blood glucose.77 The reason might be that there was no context-based education program, no diabetes nurse educators who assessed educational needs, planned, and provided counseling for diabetes patients to address these misconceptions. A holistic patient assessment would be warranted to identify more profound patients’ misperceptions about diabetes and the required standard care and lifestyle change.
We found that providers feel that patients are not self-motivated to integrate self-care practices into their daily lives, which was a significant barrier. This finding was consistent with the studies done in Ghana, which disclosed that lack of motivation hampered self-care practices and physical exercises.78 Furthermore, lack of low or lack of motivation is associated with a lack of knowledge about the risks of diabetes complications resulting from poor self-care management.79 In addition, evidence showed that depression is a co-morbidity affecting people’s motivation to adopt effective diabetes self-care practices and increased risk of diabetes complications.80,81 This might be that there were no structured, need-based diabetes education and counseling services that potentially motivate or empower the patients to practice self-care and absence of depressive symptoms screening. Another reason might be that the study area is where khat is predominantly used, which might influence patients’ motivation.
The incapable of changing dietary habits was identified as a barrier in this study. The finding was in line with a study in Cambodia and Ghana that reported dietary modification was the most challenging self-care. The patients could not modify their favorite diets they have eaten for an extended period.51,78 In addition, a study in China identified dietary-related barriers in patients with poorly controlled type 2 diabetes. The feeling of deprivation, eating away from home, lower levels of diet knowledge and empowerment, and more negative appraisal indicated the difficulty of dietary change.82 Another review reported that barriers to lifestyle modification include established food habits, lack of self-efficacy, motivation, social support, inadequate knowledge, low socioeconomic status, food culture, and poor time management.83 Dietary non-adherence behavior might be due to the lack of trained nurses or dietitians in the study setting who assess patients’ barriers and provide ongoing dietary counseling and support behavioral modification that leads to safer and healthy dietary practices.
Low health literacy level was a barrier to diabetes self-care. This finding was consistent with a study conducted in Iran where low health literacy was associated with poor diabetes self-care practices,84 and the patients with lower health literacy did not adequately understand instructions to perform diabetes self-care.85,86 This lower literacy might be that no best strategy was implemented to enhance patients’ health literacy levels. In addition, there was no well-designed diabetes patients’ education that considers literacy, culture, languages to enhance their literacy levels through multiple strategies, including video-assisted education, which might enhance self-care practices.
Strengths and Limitations
The study allowed us to thoroughly explore and understand diverse barriers of diabetes patients’ self-care from multiple perspectives, such as nurses, general practitioners, internal medicine residents, and internists. As a result, we believed that this study generated important shreds of evidence that might be used by various stakeholders, including policymakers, regional health officers, hospital administrators, health care providers, and researchers, to design multi-pronged strategies to improve the self-care practices of patients with diabetes. However, the study did not include views of other health care providers and experiences of patients with diabetes and their families regarding self-care practices.
Besides, face-to-face interview techniques of data collection might introduce social desirability bias. Hence, future qualitative research needs to incorporate and triangulate the perspectives of health care providers with experiences of patients with diabetes and their families deemed necessary along with the quantitative study to determine the magnitude of these barriers.
Implications for Nursing Practices
This study identified several barriers affecting diabetes patients’ self-care practices and the way forward to improve overall diabetes care. In addition, the finding has some implications for nursing practices since they are the majority health care professionals in the health care system, and they are spending 24 hours with the patients and accessible to them and their families. The nurses were aware of knowledge gaps in diabetes care in which they need to improve in delivering diabetes care. They need to fill their knowledge gaps through in-service capacity-building training or continuous professional development programs. The nurses also perceived that patient-centered care and holistic care provision were limited. Therefore, they prepare themselves to implement patient-centered holistic diabetes care that may assist the patients in overcoming various barriers to achieve desired goals. The finding also suggested empowering nurses with more independent roles such as diabetes nurse educators as a possible initiative to improve the patients’ health outcomes.
Conclusions
Multiple barriers that hindered diabetes self-care practices were identified, which included lack of well-integrated services for diabetes care, unavailability of Endocrinologists and diabetes nurse educators, lack of in-service training for health care workers, inconsistent availability of tests and essential drugs, lack of multidisciplinary team, lack of holistic care, inadequate patient-centered care, limited and contradictory information provision, patients’ misperception about the disease and its care, low health literacy level, lack of motivation and difficulty of changing dietary habits were the prominent barriers to diabetes self-care practices. Therefore, we recommend integrated services that can facilitate better patient care, establishing a context-based multidisciplinary team centered around the patients to address the patient’s needs and enhance diabetes self-care practice, achieve target glycemic control, and prevent complications.
Capacity-building training is also recommended for health professionals who provide direct care and support for diabetes patients—for example; training diabetes nurse educators is essential to regularly provide standard diabetes self-management education (DSME) and targeted counseling services that improve patient’s literacy, motivation, and misperceptions to overcome perceived barriers to diabetes self-care practices. In addition, the hospital administrators should ensure the continuous supply of laboratory materials and stock pharmacies with safer and adequate essential diabetes medications for augmenting the effectiveness of diabetes self-care practices.
Acknowledgments
We thank all research participants, and Haramaya University.
Funding Statement
This research was funded by Haramaya University, Ethiopia.
Abbreviations
ADA, American Diabetes Association; BSc, Bachelor of Sciences; DKA, Diabetes Keto Acidosis; DM, Diabetes Mellitus; DSME, Diabetes Self-Management Education; FMoH, Federal Ministry of Health; HbA1c, Glycated Hemoglobin A1c; ICU, Intensive Care Unit; IDI, In-Depth-Interview; GPs, General Practitioners; OPD, Outpatient Department; and WHO, World Health Organization.
Author Contributions
All authors made a significant contribution to the conception, study design, execution, acquisition of data, analysis and interpretation of the data; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.WHO. Classification of Diabetes Mellitus. WHO; 2019. [Google Scholar]
- 2.IDF. IDF Diabetes Atlas. Eighth ed. IDF; 2017. [Google Scholar]
- 3.WHO. Global Report on Diabetes. WHO; 2016. [Google Scholar]
- 4.IDF. IDF Diabetes Atlas. Ninth ed. IDF; 2019. [Google Scholar]
- 5.Shiferaw F, Letebo M, Misganaw A, et al. Non-communicable Diseases in Ethiopia: disease burden, gaps in health care delivery and strategic directions. Ethiop J Health Dev. 2018;32(3). [Google Scholar]
- 6.Zekewos A, Loha E, Egeno T, Wubshet K, Merga Z. Prevalence of diabetes mellitus and associated factors in Southern Ethiopia: a community based study. Ethiop J Health Sci. 2018;28(4):451–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bishua KG, Jenkins C, Yebyod HG, Atsbha M, Wubayehu T, Gebregziabher M. Diabetes in Ethiopia: a systematic review of prevalence, risk factors, complications, and cost. Obes Med. 2019;15:100132. [Google Scholar]
- 8.EPHI, FMoH, WHO. Ethiopia Steps Report on Risk Factors for Non-Communicable Diseaes and Prevalence of Selected NcDs. WHO; 2016. [Google Scholar]
- 9.Shiferaw F, Letebo M, Feleke Y, et al. Non-communicable diseases in Ethiopia: policy and strategy gaps in the reduction of behavioral risk factors. Ethiop J Health Dev. 2019;33(4). [Google Scholar]
- 10.Ogurtsova K, da Rocha Fernandes JD, Huang Y, et al. IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50. doi: 10.1016/j.diabres.2017.03.024 [DOI] [PubMed] [Google Scholar]
- 11.Mogre V, Johnson NA, Tzelepis F, Paul C. Attitudes towards, facilitators and barriers to the provision of diabetes self-care support: a qualitative study among healthcare providers in Ghana. Diabetes Metab Syndr. 2019;13(3):1745–1751. doi: 10.1016/j.dsx.2019.03.041 [DOI] [PubMed] [Google Scholar]
- 12.ADA. American Diabetes Association standards of medical care in diabetes. J Clin Appl Res Educ. 2019;42(Supplement 1):213–219. [Google Scholar]
- 13.Kolb L; Association of Diabetes Care & Education Specialists. An effective model of diabetes care and education: the ADCES7 self-care behaviors™. Sci Diabetes Self Manag Care. 2021;47(1):30–53. doi: 10.1177/0145721720978154 [DOI] [PubMed] [Google Scholar]
- 14.Powers MA, Bardsley JK, Cypress M, et al. Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care. 2020;43(7):1636–1649. [DOI] [PubMed] [Google Scholar]
- 15.Monfared EL, Tehrani H, Teiho Z, Jafari A. The study of eye care behaviors in patients with type 2 diabetes. J Diabetes Metab Disord. 2020;19:257–263. doi: 10.1007/s40200-020-00499-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayele BH, Mengesha MM, Tesfa T. Predictors of self-care activities of outpatient diabetic residents in Harar and Dire Dawa: a hospital-based cross-sectional study. SAGE Open Med. 2019;7:1–10. doi: 10.1177/2050312119865646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Babazadeh T, Dianatinasab M, Daemi A, Nikbakht HA, Moradi F, Ghaffari-Fam S. Association of self-care behaviors and quality of life among patients with type 2 diabetes mellitus: Chaldoran County, Iran. Diabetes Metab J. 2017;41(6):449–456. doi: 10.4093/dmj.2017.41.6.449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.ADA. 6. Glycemic targets: standards of medical care in diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S55–S64. doi: 10.2337/dc18-S006 [DOI] [PubMed] [Google Scholar]
- 19.Ketema DB, Leshargie CT, Kibret GD, et al. Level of self-care practice among diabetic patients in Ethiopia: a systematic review and meta-analysis. BMC Public Health. 2020;20(1):309. doi: 10.1186/s12889-020-8425-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gebreyohannes EA, Netere AK, Belachew SA, Hirst JA. Glycemic control among diabetic patients in Ethiopia: a systematic review and meta-analysis. PLoS One. 2019;14(8):e0221790. doi: 10.1371/journal.pone.0221790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alramadan MJ, Afroz A, Hussain SM, et al. Patient-related determinants of glycaemic control in people with type 2 diabetes in the gulf cooperation council countries: a systematic review. J Diabetes Res. 2018;2018:9389265. doi: 10.1155/2018/9389265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kayar Y, Ilhan A, Kayar NB, et al. Relationship between the poor glycemic control and risk factors, life style and complications. Biomed Res. 2017;28(4):1581–1586. [Google Scholar]
- 23.Fasil A, Biadgo B, Abebe M. Glycemic control and diabetes complications among diabetes mellitus patients attending at University of Gondar Hospital, Northwest Ethiopia. Diabetes Metab Syndr Obes Targets Ther. 2019;12:75–83. doi: 10.2147/DMSO.S185614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rodriguez-Gutierrez R, Gionfriddo MR, Ospina NS, et al. Shared decision making in endocrinology: present and future directions. Lancet Diabetes Endocrinol. 2016;4(8):706–716. doi: 10.1016/S2213-8587(15)00468-4 [DOI] [PubMed] [Google Scholar]
- 25.Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–2701. doi: 10.2337/dci18-0033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Williams JS, Walker RJ, Smalls BL, Hill R, Egede LE. Patient-centered care, glycemic control, diabetes self-care, and quality of life in adults with type 2 diabetes. Diabetes Technol Ther. 2016;18(10):644–649. doi: 10.1089/dia.2016.0079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gluyas H. Patient-centred care: improving healthcare outcomes. Nurs Standard. 2015;30(4):50–57. doi: 10.7748/ns.30.4.50.e10186 [DOI] [PubMed] [Google Scholar]
- 28.WHO. Improving Health System Efficiency in Ethiopia: Human Resources for Health Reforms. WHO; 2015. [Google Scholar]
- 29.Nikitara M, Constantinou CS, Andreou E, Diomidous M. The role of nurses and the facilitators and barriers in diabetes care: a mixed methods systematic literature review. Behav Sci (Basel). 2019;9(6):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 31.Virginia B, Victoria C. Reflecting on reflexive thematic analysis. Qual Res Sport Exer Health. 2019;11(4):589–597. doi: 10.1080/2159676X.2019.1628806 [DOI] [Google Scholar]
- 32.Neuendorf KA. Research Methods for Applied Psychologists: Design, Analysis and Reporting. New York: Routledge; 2019:211–223. [Google Scholar]
- 33.World Medical Association. World Medical Association declaration of Helsinki ethical principles for medical research involving human subjects. JAMA. 2013;310(20):373. [DOI] [PubMed] [Google Scholar]
- 34.WHO. Continuity and Coordination of care:A Practice Brief to Support Implementation of the WHO Framework on Integrated People-Centred Health Services. WHO; 2018. [Google Scholar]
- 35.WHO. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia: Report of a WHO/Idf ConsultatIon. WHO; 2006. [Google Scholar]
- 36.Simão CC, Costa MB, Colugnati FAB, Paula EA, Vanelli CP, Paula RB. Quality of care of patients with diabetes in primary health services in Southeast Brazil. Hindawi. J Environ Public Health. 2017;7. doi: 10.1155/2017/1709807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Drincic AT, Akkireddy P, Knezevich JT. Common models used for inpatient diabetes management. Curr Diab Rep. 2018;18(3):10. doi: 10.1007/s11892-018-0972-x [DOI] [PubMed] [Google Scholar]
- 38.Malkani S, Keitz SA, Harlan DM. Redesigning diabetes care: defining the role of endocrinologists among alternative providers. Curr Diab Rep. 2016;16(12):121. doi: 10.1007/s11892-016-0818-3 [DOI] [PubMed] [Google Scholar]
- 39.Sheahan KH, Atherly A, Dayman C, Schnure J. The impact of diabetology consultations on length of stay in hospitalized patients with diabetes. Endocrinol Diab Metab. 2021;4:e00199. doi: 10.1002/edm2.199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Puig J, Supervia A, Marquez MA, Flores J, Cano JF, Gutierrez J. Diabetes team consultation: impact on length of stay of diabetic patients admitted to a short-stay unit. Diabetes Res Clin Pract. 2007;78(2):211–216. doi: 10.1016/j.diabres.2007.03.010 [DOI] [PubMed] [Google Scholar]
- 41.Beran D. The impact of health systems on diabetes care in low and lower middle income countries. Curr Diab Rep. 2015;15(4):20. doi: 10.1007/s11892-015-0591-8 [DOI] [PubMed] [Google Scholar]
- 42.Ugwu E, Young E, Nkpozi M. Diabetes care knowledge and practice among primary care physicians in Southeast Nigeria: a cross-sectional study. BMC Fam Pract. 2020;21(1):128. doi: 10.1186/s12875-020-01202-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Atun R, Davies JI, Gale EAM, et al. Diabetes in sub-Saharan Africa: from clinical care to health policy. Lancet Diabetes Endocrinol. 2017;5(8):622–667. [DOI] [PubMed] [Google Scholar]
- 44.FMoH. Ethiopian National Guideline on Major NCDs 2016. FMoH; 2016. [Google Scholar]
- 45.Basu S, Sharma N. Diabetes self-care in primary health facilities in India - challenges and the way forward. World J Diabetes. 2019;10(6):341–349. doi: 10.4239/wjd.v10.i6.341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wallymahmed M. Education: the cornerstone of diabetes management. J Diabetes Nurs. 2015;19(2). [Google Scholar]
- 47.Azami G, Soh KL, Sazlina SG, et al. Effect of a nurse-led diabetes self-management education program on glycosylated hemoglobin among adults with type 2 diabetes. J Diabetes Res. 2018;2018:4930157. doi: 10.1155/2018/4930157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hailu FB, Hjortdahl P, Moen A. SNurse-led diabetes self-management education improves clinical parameters in Ethiopia. Front Public Health. 2018;6:362. doi: 10.3389/fpubh.2018.00302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lawler J, Trevatt P, Elliot C, Leary A. Does the Diabetes Specialist Nursing workforce impact the experiences and outcomes of people with diabetes? A hermeneutic review of the evidence. Hum Resour Health. 2019;17(1):65. doi: 10.1186/s12960-019-0401-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alshammari M, Windle R, Bowskill D, Adams G. The role of nurses in diabetes care: a qualitative study. Open J Nurs. 2021;11:682–695. doi: 10.4236/ojn.2021.118058 [DOI] [Google Scholar]
- 51.Nang EEK, Dary C, Hsu LY, Sor S, Saphonn V, Evdokimov K. Patients’ and healthcare providers’ perspectives of diabetes management in Cambodia: a qualitative study. BMJ Open. 2019;9(11):e032578. doi: 10.1136/bmjopen-2019-032578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pastakia SD, Nuche-Berenguer B, Pekny CR, et al. Retrospective assessment of the quality of diabetes care in a rural diabetes clinic in Western Kenya. BMC Endocr Disord. 2018;18(1):97. doi: 10.1186/s12902-018-0324-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.FMoH. Guidelines on Clinical and Programmatic Management of Major Non Communicable Diseases. FMoH; 2016. [Google Scholar]
- 54.FMoH. National Comprehensive COVID 19 Management Handbook for Health Professionals. FMoH; 2020. [Google Scholar]
- 55.Shi C, Zhu H, Liu J, Zhou J, Tang W. Barriers to self-management of type 2 diabetes during COVID-19 medical isolation: a qualitative study. Diabetes Metab Syndr Obes. 2020;13:3713–3725. doi: 10.2147/DMSO.S268481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nouhjah S, Jahanfar S. Challenges of diabetes care management in developing countries with a high incidence of COVID-19: a brief report. Diabetes Metab Syndr. 2020;14(5):731–732. doi: 10.1016/j.dsx.2020.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Berkowitz SA, Eisenstat SA, Barnard LS, Wexler DJ. Multidisciplinary coordinated care for Type 2 diabetes: a qualitative analysis of patient perspectives. Prim Care Diabetes. 2018;12(3):218–223. doi: 10.1016/j.pcd.2018.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gowing A, Dickinson C, Gorman T, Robinson L, Duncan R. Patients’ experiences of a multidisciplinary team-led community case management programme: a qualitative study. BMJ Open. 2016;6(9):e012019. doi: 10.1136/bmjopen-2016-012019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McGill M, Blonde L, Chan JCN, et al. The interdisciplinary team in type 2 diabetes management: challenges and best practice solutions from real-world scenarios. J Clin Transl Endocrinol. 2017;7:21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Abdulrhim S, Sankaralingam S, Ibrahim MIM, et al. Collaborative care model for diabetes in primary care settings in Qatar: a qualitative exploration among healthcare professionals and patients who experienced the service. BMC Health Serv Res. 2021;21(1):192. doi: 10.1186/s12913-021-06183-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Koproski J, Pretto CZ, Poretsky L. Effects of an intervention by a diabetes team in hospitalized patients with diabetes. Diabetes Care. 1997;20(10):1553–1555. doi: 10.2337/diacare.20.10.1553 [DOI] [PubMed] [Google Scholar]
- 62.Linda S. Team care—the preferred approach to diabetes treatment. US Endocrinol. 2015;11(2):75–76. [Google Scholar]
- 63.ADA. Standards of medical care in diabetes. J Clin Appl Res Educ. 2017;40:S11–S61. [Google Scholar]
- 64.Williams J. Effective team working to improve diabetes care in older people. J Diabetes Nurs. 2016;20(4):137–141. [Google Scholar]
- 65.Kassean HK. Nurses’ perceptions of their role in caring for diabetic patients at the primary care level. J Health Manag. 2005;7(2):207–217. doi: 10.1177/097206340500700203 [DOI] [Google Scholar]
- 66.Juanamasta G, Aungsuroch Y, Gunawan J, Suniyadewi NW, Wati NMN. THolistic care management of diabetes mellitus: an integrative review. Int J Prev Med. 2021;12:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rajabpour S, Rayyani M, Mangolian Shahrbabaki P. The relationship between Iranian patients’ perception of holistic care and satisfaction with nursing care. BMC Nurs. 2019;18:48. doi: 10.1186/s12912-019-0374-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.ADA. Foundations of Care and Comprehensive Medical Evaluation. Diabetes Care. 2016;39:S23–35. doi: 10.2337/dc16-S006 [DOI] [PubMed] [Google Scholar]
- 69.Man JD, Mayega RW, Sarkar N, et al. Patient-centered care and people-centered health systems in sub-Saharan Africa: why so little of something so badly needed? Int J Person Center Med. 2016;6(3). doi: 10.5750/ijpcm.v6i3.591 [DOI] [Google Scholar]
- 70.Topp SM, Chipukuma JM. A qualitative study of the role of workplace and interpersonal trust in shaping service quality and responsiveness in Zambian primary health centres. Health Policy Plan. 2016;31(2):192–204. doi: 10.1093/heapol/czv041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rutten G, Van Vugt H, de Koning E. Person-centered diabetes care and patient activation in people with type 2 diabetes. BMJ Open Diabetes Res Care. 2020;8(2):e001926. doi: 10.1136/bmjdrc-2020-001926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.ADA. Standards of medical care in diabetes. Diabetes Care. 2021;44(Suppl 1):S15. [DOI] [PubMed] [Google Scholar]
- 73.Evans DC. Exploring how language and approaches used when supporting diabetes self management can impact upon an individual’s engagement with their condition: a multicase study of patients, support persons and healthcare professionals. Diabetic Med. 2019;36:34–174. [Google Scholar]
- 74.Mukeshimana M, Hakizimana G, Mwali C, Umuhoza C, Uwambajimana J, Asingizwe D. The knowledge and practice of self-care management among patients attending a diabetes clinic in Kigali, Rwanda. Rwanda J Series F. 2015;2(1):24–30. [Google Scholar]
- 75.Stephani V, Beran BD, Beran D. Self-management of diabetes in Sub-Saharan Africa: a systematic review. BMC Public Health. 2018;18:1148. doi: 10.1186/s12889-018-6050-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dinesh PV, Kulkarni AG, Gangadhar NK. Knowledge and self‑care practices regarding diabetes among patients with type 2 diabetes in Rural Sullia, Karnataka: a community‑based, cross‑sectional study. J Fam Med Prim Care. 2016;5:847–852. doi: 10.4103/2249-4863.201176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chen CC, Chen CL, Ko Y. The misconceptions and determinants of diabetes knowledge in patients with diabetes in Taiwan. J Diabetes Res. 2020;2020:2953521. doi: 10.1155/2020/2953521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mogre V, Johnson NA, Tzelepis F, Paul C. Barriers to diabetic self-care: a qualitative study of patients’ and healthcare providers’ perspectives. J Clin Nurs. 2019;28(11–12):2296–2308. doi: 10.1111/jocn.14835 [DOI] [PubMed] [Google Scholar]
- 79.Swanson V, Maltinsky W. Motivational and behaviour change approaches for improving diabetes management. Pract Diabetes. 2019;36(4):121–125. doi: 10.1002/pdi.2229 [DOI] [Google Scholar]
- 80.Teshome HM, Ayalew GD, Shiferaw FW, Leshargie CT, Boneya DJ. The prevalence of depression among diabetic patients in Ethiopia: a systematic review and meta-analysis. Depress Resand Treat. 2018;2018. doi: 10.1155/2018/6135460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mut-Vitcu G, Timar B, Timar R, Oancea C, Citu IC. Depression influences the quality of diabetes-related self-management activities in elderly patients with type 2 diabetes: a cross-sectional study. Clin Interv Aging. 2016;11:471–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cheng L, Leung DY-P, Sit JW-H, et al. Factors associated with diet barriers in patients with poorly controlled type 2 diabetes. Patient Prefer Adherence. 2016;10:37–44. doi: 10.2147/PPA.S94275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shukri Nam NM, Yassin NQ, Sidek S, Azahari N, Azahari N. Barriers and enablers to make lifestyle changes among type 2 diabetes patients: a review. Sains Malaysiana. 2019;48(7):1491–1502. doi: 10.17576/jsm-2019-4807-18 [DOI] [Google Scholar]
- 84.Maleki Chollou K, Gaffari-Fam S, Babazadeh T, Daemi A, Bahadori A, Heidari S. The association of health literacy level with self-care behaviors and glycemic control in a low education population with type 2 diabetes mellitus: a cross-sectional study in Iran. Diabetes Metab Syndr Obes. 2020;13:1685–1693. doi: 10.2147/DMSO.S253607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.RobatSarpooshi D, Mahdizadeh M, Alizadeh Siuki H, Haddadi M, Robatsarpooshi H, Peyman N. The relationship between health literacy level and self-care behaviors in patients with diabetes. Patient Relat Outcome Meas. 2020;11:129–135. doi: 10.2147/PROM.S243678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kim S, Song Y, Park J, Utz S. Patients’ experiences of diabetes self-management education according to health-literacy levels. Clin Nurs Res. 2020;29(5):285–292. doi: 10.1177/1054773819865879 [DOI] [PubMed] [Google Scholar]