Abstract
PURPOSE:
Patients with chronic sixth nerve palsy (CSNP) comprise a heterogeneous population, and the optimal surgical solution remains uncertain. Here, we present the success rate and factors associated with the success of strabismus surgeries for CSNP.
METHODS:
This was a retrospective cohort study of patients with strabismus due to CSNP operated on between 2015 and 2019 in a tertiary eye hospital in central Saudi Arabia. Surgical success was defined as a horizontal deviation of ≤10 prism diopters (PDs) assessed at least 12 months after surgery. Differences between groups with respect to the primary outcome were assessed.
RESULTS:
Fifty-five patients were analyzed with a median follow-up of 24 (range 12–48) months. Superior rectus and inferior rectus transposition (34.5%) and medial rectus recession with lateral rectus resection (32.7%) were the main surgeries performed. The overall success rate was 67.3% (95% confidence interval 54.9–79.7). Bilateral CSNP (P = 0.05), a higher preoperative angle of deviation (P = 0.002), or a greater degree of preoperative limitation of abduction (P = 0.012), but not the type of surgery (P = 0.09), were more likely to result in an under-corrected outcome of >10 PD. The preoperative deviation angle showed a trend toward being associated with a poor outcome after surgery (P = 0.06). Six patients with high-angle deviation before surgery required second surgery.
CONCLUSION:
While the surgical procedure does not impact outcomes, the severity of preoperative horizontal deviation might impact surgical success and the need for reoperation. Patients with severe CSNP should be counseled appropriately about the chances of surgical success and the potential need for further interventions.
Keywords: Abducens nerve palsy, botulinum toxin, muscle transposition, strabismus surgery
Introduction
Sixth (abducens) nerve palsy is the most common isolated cranial nerve neuropathy, occurring in 11/100,000 of the population.[1] Common causes include neoplasm, trauma, microvascular disease, and idiopathic causes.[1,2] Its injury results in unilateral impairment of abduction, esotropia, and binocular horizontal diplopia. If the esotropia does not improve with conservative management and treatment of the underlying etiology, surgery may be indicated. If abducens nerve palsy does not improve spontaneously within 6 months of development, it is termed chronic sixth nerve palsy (CSNP).
The choice of surgery in patients with CSNP depends on whether the lateral rectus (LR) muscle has residual function and the size of the deviation. In patients with LR muscles with residual function or small horizontal deviations, the primary surgical choice is medial rectus (MR) recession with or without resection of the ipsilateral LR. With larger deviations or in the absence of residual LR function, vertical rectus muscle transposition (VRT) to the LR is often performed, which can either be a single superior or inferior rectus (IR) or double-muscle (i. e., both superior and inferior recti) procedure. Other ancillary surgical procedures for strabismus include ipsilateral MR recession when the MR is contracted, posterior augmentation (Foster) sutures, or botulinum toxin injection.
With the variety of underlying etiologies and variable disease severity, the choice of strabismus surgery for CSNP is debated. Furthermore, with the high and increasing prevalence of diabetes in Saudi Arabia[3] likely to contribute to an increased prevalence of CSNP, optimizing the management of the condition is a clinical imperative. There have been no prospective randomized controlled trials (RCTs) comparing different surgical procedures in carefully selected patient groups to guide the management of these heterogeneous patients. Indeed, a recent meta-analysis of 27 studies examining the correction achieved by 12 individual transposition procedures revealed that a comparison of these studies was hampered by a lack of RCTs, the variable severity of preoperative esotropia, and the different postoperative outcome measures reported.[4] Only a few studies have directly compared other procedures. For example, superior rectus transposition with MR recession was said to be equivalent to double-muscle VRT in terms of deviation correction. Still, the former was reported to result in fewer additional surgical procedures.[5] Superior rectus transposition with MR recession is both equivalent[6] and superior[7] to superior MR recession alone in head-to-head comparisons. It has favorable outcomes in single cohort studies.[8,9]
The long-term success from strabismus surgery for CSNP is reported to be between 46% and 90%.[4,10] However, to our best knowledge, there no reports of the surgical outcomes of patients with CSNP in Saudi Arabia, although studies of surgical outcomes for patients with esotropia of any cause have reported success rates of 70%–80%.[11,12] Furthermore, while there have been attempts to identify risk factors for poor outcomes from CSNP in other populations,[9,13,14] there have been no such studies in Saudi Arabia.
Given this lack of data from Saudi Arabia, heterogeneity in the clinical features of the treated population, and the wide variety of surgical options available, we examined preoperative clinical and surgical predictors of postoperative outcomes from a variety of surgical procedures performed for abducens nerve palsy. Identifying prognostic factors could help allocate patients to the most appropriate surgical procedure in an attempt to improve outcomes and reduce the need for secondary operations.
Methods
Ethical approval
The Institutional Review Board of our institute approved the study protocol. Since this was a retrospective cohort study, the written consent of participants was waived. The study was performed adhering to the tenets of the Declaration of Helsinki.
Patients and data collection
This was a one-armed retrospective cohort study. Patients undergoing strabismus surgery at (redacted), Saudi Arabia, due to CSNP between January 2015 and December 2019. The clinical records were reviewed to extract demographic, clinical, surgical, and outcome data. The information included age and gender; the underlying etiology of the sixth nerve palsy; laterality, where the more severely affected eye was used for analysis as previously;[10,15] pre and postoperative primary deviation using cover/uncover testing and prisms at 6 m where possible, otherwise using Krimsky light reflex testing; pre and postoperative degree of limitation of abduction as per the scale described by Scott and Kraft[16](duction of 0 = normal, −1 = rotate from the midline to 75% of a full rotation, −2 = rotate from the midline to 50% of maximum rotation, −3 = rotate from the midline to 25% of a full rotation, −4 = rotate to midline but not into a given field, and − 5= unable to rotate from opposite field to midline), where abduction deficits of −4 or −5 were classified as complete and abduction deficits of −1, −2, or −3 were classified as incomplete;[10,15] pre and postoperative head turn; pre and postoperative presence or absence of diplopia; and the type of surgical procedure.
Standardized preoperative and postoperative graded force duction test (0–5) is a valuable tool to evaluate the contraction of MR muscle, at onset and the end of surgery. It is a good complement with the clinical abduction limitation. We excluded this variable from the study. This data was not clearly specified in all patients.
Outcomes
The primary outcome was treatment success defined as a postoperative horizontal deviation of ≤10 prism diopter (PD), as previously.[9,14] Changes in the degree of limitation of abduction, head turn, and diplopia were also considered secondary outcomes.
Statistical analysis
Microsoft Access® and SPSS v25 (IBM Statistics, Armonk, NY, USA) were used for data collection and statistical analysis. Differences in outcome variables before and after surgery were assessed using Wilcoxon's rank-sum test for continuous variables and McNemar's test for categorical variables. Differences between groups for the primary outcome were assessed using the Mann–Whitney U-test or the Chi-squared test for continuous and categorical variables, respectively. Parameters with P < 0.25 in univariable analysis were used to design the most appropriate binary logistic regression model for the primary outcome variable. Lower P value thresholds, such as 0.05, can fail to identify variables known to be important.[17,18] There were no strong intercorrelations between variables. Odds ratios (ORs) were calculated with 95% of confidence intervals (CIs). A P < 0.05 was considered statistically significant.
Results
The clinical and surgical characteristics of the 55 patients meeting the inclusion criteria are shown in Table 1. Forty-four patients were male (80%), and 20 were female (20%), with a median age of 26 years (interquartile range [IQR] 19–37 years). 85.5% of patients had unilateral esotropia, caused by sixth nerve trauma (76.4%) followed by neoplasm (9.1%) and idiopathic causes (7.3%). The minimum length of follow-up was 12 months with a median duration of follow-up of 24 months (IQR 18–14 months).
Table 1.
The clinical and surgical characteristics of the patients undergoing surgery for esotropia due to sixth nerve palsy
| Variable | n (%)/median (IQR) | |
|---|---|---|
| Age | 26.0 (19.0-37.0) | |
| Gender | ||
| Male | 44 (80.0) | |
| Female | 11 (20.0) | |
| Affected eye(s) | ||
| Unilateral | 47 (85.5) | |
| Bilateral | 8 (14.5) | |
| Etiology | ||
| Neoplasm | 5 (9.1) | |
| Trauma | 42 (76.4) | |
| Viral | 1 (1.8) | |
| Idiopathic | 4 (7.3) | |
| Vasculopathy | 3 (5.5) | |
| Management | ||
| Surgery with botulinum toxin | 22 (40.0) | |
| Surgery without botulinum toxin | 33 (60.0) | |
| Type of surgery | ||
| Vertical SR + IR transposition | 19 (34.5) | |
| Vertical SR + IR transposition and MR recession | 6 (10.9) | |
| MR recession and LR resection | 18 (32.7) | |
| SR transposition + MR recession | 5 (9.1) | |
| MR recession | 2 (3.6) | |
| BMR recession | 5 (9.1) | |
| Type of vertical transposition | ||
| Hummelsheim | 9 (16.4) | |
| Full tendon | 21 (38.2) | |
| Foster suture | ||
| Yes | 15 (27.2) | |
| No | 40 (72.8) | |
| Second surgery indicated | ||
| Yes | 6 (10.9) | |
| No | 49 (89.1) |
IQR: Interquartile range, SR: Superior rectus, IR: Inferior rectus, MR: Medial rectus, LR: Lateral rectus, BMR: Bilateral medial rectus
Various surgeries were performed: Patients received superior vertical rectus (SR) and IR transposition (34.5%) or MR recession with LR resection (32.7%), while approximately 10% of patients each received SR and IR transposition with MR recession, SR transposition with MR recession, or bilateral MR (BMR) recession, respectively. Two patients received the MR recession alone. A majority of patients did not receive botulinum toxin injections (60%). About 15/55 (27.2%) patients had vertical muscle transposition augmented with a Foster suture which was used in cases with severe limitation of abduction (−4, −5). In the 30 patients undergoing vertical transposition, nine (30%) experienced an augmented Hummelsheim procedure, while 21 (70%) had a full tendon procedure. The overall success rate was 67.3% (95% CI 54.9–79.7).
There were improvements in all primary and secondary outcomes after surgery [Table 2; all P < 0.0001]. The median esodeviation in primary position improved from 45 PD (IQR 30.0–60.0)–4.0 PD (0–12.0); after surgery, 37/55 (67.3%) patients had an angle of deviation ≤10 PD compared to none before surgery. In terms of secondary outcomes, only 11/55 (20%) patients had complete limitation of abduction after surgery compared to 40/55 (72.7%) before surgery; 45/55 (81.8%) patients were free from diplopia after surgery compared to 9/55 (16.4%) before surgery, and only 10/55 (18.2%) of patients had anomalous head turn after surgery compared to 32 (58.2%) before surgery.
Table 2.
Changes in primary and secondary outcomes before and after strabismus surgery in eye with 6th nerve palsy
| Outcome variable | Before surgery, n (%) | After surgery, n (%) | P |
|---|---|---|---|
| Angle of deviation | |||
| Median | 45.0 (30.0-60.0) | 4.0 (0-12.0) | <0.0001 |
| ≤10 PD | 0 | 37 (67.3) | <0.0001 |
| >10 PD | 55 (100) | 18 (32.7) | |
| Degree of limitation of abduction | |||
| Incomplete | 15 (24.3) | 44 (80.0) | <0.0001 |
| Complete | 40 (72.7) | 11 (20.0) | |
| Presence of diplopia | |||
| Yes | 46 (83.6) | 10 (18.2) | <0.0001 |
| No | 9 (16.4) | 45 (81.8) | |
| Head turn | |||
| Yes | 32 (58.2) | 10 (18.2) | <0.0001 |
| No | 23 (41.8) | 45 (81.8) |
PD: Prism diopters
Traumatic sixth nerve palsy, most of the patients had −4 –5 limitation of abduction, with higher preoperative deviation. The preoperative angle of deviation was 36.68 PD and postoperative angle of deviation was 6.19 PD on average [Chart 1].
Chart 1.
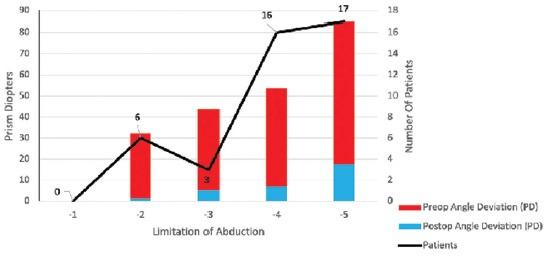
Sixth nerve palsy after TRAUMA. Preoperative and postoperative angle of deviation
In univariable analysis, patients with bilateral CSNP (P = 0.05), a higher preoperative angle of deviation (P = 0.002), or a greater degree of preoperative limitation of abduction (P = 0.012) were more likely to have an under-corrected outcome of >10 PD [Table 3].
Table 3.
Univariate associations between clinical and surgical variables and the primary outcome of residual esotropia ≤10 prism diopters in persons with strabismus following chronic 6th nerve palsy
| Variable | ≤10 PD (n=37), n (%) | >10 PD (n=18), n (%) | P |
|---|---|---|---|
| Age | 27.0 (17) | 22.0 (20) | 0.38 |
| Gender | |||
| Male | 29 (65.9) | 15 (34.1) | 0.67 |
| Female | 8 (72.7) | 3 (27.3) | |
| Affected eye(s) | |||
| Unilateral | 34 (72.3) | 13 (27.7) | 0.05 |
| Bilateral | 3 (37.5) | 5 (62.5) | |
| Etiology | |||
| Neoplasm | 4 (80.0) | 1 (20.0) | 0.25 |
| Trauma | 25 (59.5) | 17 (40.5) | |
| Viral | 1 (100) | 0 | |
| Idiopathic | 4 (100) | 0 | |
| Vasculopathy | 3 (100) | 0 | |
| Preoperative angle of deviation | |||
| Median | 40.0 (23) | 60 (39) | 0.002 |
| Preoperative degree of limitation of abduction | |||
| Incomplete | 14 (37.8) | 1 (5.6) | 0.012 |
| Complete | 23 (62.2) | 17 (94.4) | 0.41 |
| Preoperative presence of diplopia | |||
| Yes | 5 (13.5) | 4 (22.2) | 0.78 |
| No | 32 (86.5) | 14 (77.8) | |
| Preoperative head turn | |||
| Yes | 15 (40.5) | 8 (44.4) | |
| No | 22 (59.5) | 10 (55.6) | |
| Management | |||
| Surgery with botulinum toxin | 14 (63.6) | 8 (36.4) | 0.64 |
| Surgery without botulinum toxin | 23 (69.7) | 10 (30.3) | |
| Type of surgery | |||
| SR + IR transposition | 9 (47.4) | 10 (52.6) | 0.09 |
| SR + IR transposition and MR recession | 3 (50.0) | 3 (50.0) | |
| MR recession and LR resection | 16 (88.9) | 2 (11.1) | |
| SR transposition + MR recession | 4 (80.0) | 1 (20.0) | |
| MR recession | 2 (100) | 0 | |
| BMR | 3 (60.0) | 2 (40.0) |
SR: Superior rectus, IR: Inferior rectus, MR: Medial rectus, LR: Lateral rectus, BMR: Bilateral medial rectus, PD: Prism diopters
When all variables with P > 0.25 were included in a bivariate logistic regression model including laterality, etiology, preoperative angle of deviation, preoperative limitation of abduction, and type of surgery as independent variables, there was a trend toward preoperative deviation being significantly associated with an increased odds of a poor outcome after surgery (OR 1.05, 95% CI 0.997–1.11; P = 0.06; P values for all other independent variables >0.19).
Six patients (10.9%) required reoperation due to combined postoperative horizontal deviation >20 PD, limitation of abduction ≥−3, persistent diplopia, and abnormal head turn. Although these six patients were not significantly different from patients not requiring secondary surgery in terms of most demographic, clinical, or surgical parameters, they did have considerably greater preoperative angles of deviation (75[30] PD vs. 40[30] PD; Mann–Whitney U-test P = 0.004), consistent with the results of the regression analysis. These second surgeries were successful (one SR transposition, two vertical SR + IR transpositions, one MR recession, and two BMR recessions, respectively, with three fully corrected horizontal deviations and three with 10, 12, and 15 PD, respectively.
Discussion
In this study, one of the largest of its kind with extended follow-up and the first to investigate risk factors for poor outcomes from CSNP surgery in Saudi Arabia,[4] we assessed preoperative clinical and surgical factors associated with postoperative outcomes from strabismus surgery for chronic abducens nerve palsy. Overall, our success rate of 67% for the primary endpoint of horizontal deviation ≤10 PD was excellent and consistent with other reports of long-term outcomes from strabismus surgery for CSNP of between 46% and 90%.[4,10] Our median esodeviation correction from all 41 PD surgeries is consistent with previously reported weighted corrections of between 27.0 and 58.3 PD across 12 equivalent surgical procedures in 27 studies.[4] Furthermore, our surgical success rate is similar to that reported for patients with esotropia of any cause (70%–80%).[11,12]
While no single preoperative parameter was highly predictive of surgical outcome, preoperative deviation showed a trend toward being significantly associated with a slightly increased odds of a poor outcome after surgery (OR 1.05, 95% CI 0.997–1.11; P = 0.06), consistent with a similar small study of 13 patients in whom the degree of preoperative abduction deficit was the sole prognostic factor for augmented superior rectus transposition for CSNP in multivariable analysis.[13] Similarly, in their study of 13 patients undergoing superior rectus transposition with MR recession for sixth nerve palsy, Patil-Chhablani et al.[9] found that the two surgical failures had large preoperative deviations of 110 and 50 PD. There have also been attempts to identify factors predictive of surgical outcome in third nerve palsy, and similar to these results, the preoperative deviation was predictive of more poor postoperative results.[19]
In another attempt to identify predictors of poor outcomes from sixth nerve palsy, Peragallo et al.[14] examined combined motor and functional outcomes (absence of diplopia, vertical deviation ≤2 PD, and horizontal deviation ≤10 PD) after various strabismus surgeries for sixth nerve palsy and despite the more stringent criteria for success, reported a success rate of 58% (compared to 67% here). Similar to our findings, success rates were similar across etiologies, although they found that reoperation frequency was higher in patients with neoplastic or traumatic etiologies.[14] While we detected no such association between etiology and reoperation, our study was limited by the small number of patients with etiologies other than trauma. Because most of patients with vascular causes improve spontaneously, no surgery was needed so they were excluded. The fact that such a large proportion (76.5%) of our patients had a traumatic etiology might seem surprising since most of these cases resolve spontaneously;[20] however, the majority of sixth nerve palsies that do not settle are traumatic in etiology, explaining this finding.
To our best knowledge, this is the first study to examine whether intraoperative botulinum toxin influences strabismus surgery outcomes. In our study, the decision of botulinum toxin or recession was based on the surgeon's preferences. Scott proposed intraoperative botulinum toxin in 1981 as an approach to weaken the antagonist MR in transposition procedures, postulating that it reduces MR contracture to allow complete recovery of LR function.[16,21] However, esotropia can recur 4–6 months later using this approach when the MR function recovers. Our data found no difference in outcomes between patients who did and did not receive intraoperative botulinum injections. While Lee and Lambert[5] did not specifically examine their subgroup of five of eight VRT patients receiving MR botulinum injections, the similar outcomes between this group and those receiving superior rectus transpositions and MR recession are consistent with the current results.
In our study, vertical transposition was performed in most cases with the limitation of abduction −4 –5 alone or combined with BMR. Furthermore, mention that in four patients with-4–5 limitation was performed R and R as primary procedure and three of them required second procedure [Chart 2]. Our results also suggest that patients with more severe esodeviation are not only more likely to have unsatisfactory correction but are also more likely to require a second operation, as previously reported.[13] Patients who required further surgical procedures had a POSITIVE intraoperative force duction traction test. Although reoperation outcomes were good using a mixture of approaches, it remains to be determined which procedure is the best choice for reoperation in these patients. However, IR transposition has been suggested in one study.[13]
Chart 2.
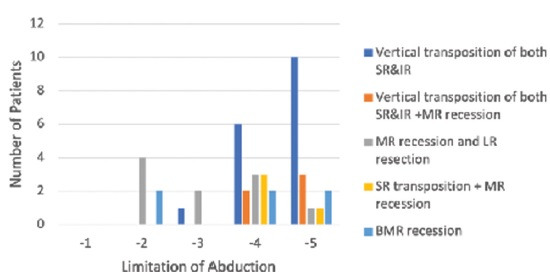
Sixth nerve palsy after TRAUMA. Procedure performed and preoperative limitation of abduction
Surgical complications were not reported, only five patients after vertical transposition have vertical deviation but were minimal and asymptomatic.
Overall, our data add to a growing body of evidence that, in the absence of prospective RCTs directly comparing different procedures, the choice of operation for sixth nerve palsy has less impact on the clinical outcome than the severity of the esodeviation. It has essential implications for preoperative patient counseling since patients with large deviations should have their expectations managed concerning the possibility of suboptimal surgical outcomes and a greater possibility of a need for reoperation.
Our study has some limitations. Although this was one of the largest cohorts of sixth nerve palsy patients analyzed to date and had a relatively long follow-up period, it remains a relatively small retrospective study from a single institution, reducing the power to detect significant differences between subgroups. Secondly, patients were operated on by several different surgeons, and several other clinicians performed pre and postoperative examinations. Third, pre and postoperative primary deviation were measured using various techniques. Quantifying the degree of diplopia using an accepted test such as the cervical range of motion method or the Goldmann perimeter would have been useful for formally assessing secondary outcomes.[22]
Conclusion
While the choice of procedure does not appear to significantly impact outcomes from strabismus surgery for sixth nerve palsy, our data support the severity of preoperative horizontal deviation affecting the surgical success and the need for reoperation. While prospective RCTs comparing different surgical approaches remain a high clinical priority, patients with severe esotropia should be counseled appropriately about the chances of surgical success and the potential need for further interventions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Patel SV, Mutyala S, Leske DA, Hodge DO, Holmes JM. Incidence, associations, and evaluation of sixth nerve palsy using a population-based method. Ophthalmology. 2004;111:369–75. doi: 10.1016/j.ophtha.2003.05.024. [DOI] [PubMed] [Google Scholar]
- 2.Elder C, Hainline C, Galetta SL, Balcer LJ, Rucker JC. Isolated abducens nerve palsy: Update on evaluation and diagnosis. Curr Neurol Neurosci Rep. 2016;16:69. doi: 10.1007/s11910-016-0671-4. [DOI] [PubMed] [Google Scholar]
- 3.Meo SA. Prevalence and future prediction of type 2 diabetes mellitus in the Kingdom of Saudi Arabia: A systematic review of published studies. J Pak Med Assoc. 2016;66:722–5. [PubMed] [Google Scholar]
- 4.Sen S, Dhiman R, Saxena R, Phuljhele S, Sharma P. Vertical rectus transposition procedures for lateral rectus palsy: A systematic review. Indian J Ophthalmol. 2019;67:1793–9. doi: 10.4103/ijo.IJO_1841_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee YH, Lambert SR. Outcomes after superior rectus transposition and medial rectus recession versus vertical recti transposition for sixth nerve palsy. Am J Ophthalmol. 2017;177:100–5. doi: 10.1016/j.ajo.2017.02.019. [DOI] [PubMed] [Google Scholar]
- 6.Abdallah ME, Eltoukhi EM, Awadein AR, Zedan RH. Superior rectus transposition with medial rectus recession versus medial rectus recession in esotropic Duane retraction syndrome. J Pediatr Ophthalmol Strabismus. 2020;57:309–18. doi: 10.3928/01913913-20200506-02. [DOI] [PubMed] [Google Scholar]
- 7.Yang S, MacKinnon S, Dagi LR, Hunter DG. Superior rectus transposition vs medial rectus recession for treatment of esotropic Duane syndrome. JAMA Ophthalmol. 2014;132:669–75. doi: 10.1001/jamaophthalmol.2014.358. [DOI] [PubMed] [Google Scholar]
- 8.Mehendale RA, Dagi LR, Wu C, Ledoux D, Johnston S, Hunter DG. Superior rectus transposition and medial rectus recession for Duane syndrome and sixth nerve palsy. Arch Ophthalmol. 2012;130:195–201. doi: 10.1001/archophthalmol.2011.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patil-Chhablani P, Kothamasu K, Kekunnaya R, Sachdeva V, Warkad V. Augmented superior rectus transposition with medial rectus recession in patients with abducens nerve palsy. J AAPOS. 2016;20:496–500. doi: 10.1016/j.jaapos.2016.07.227. [DOI] [PubMed] [Google Scholar]
- 10.Holmes JM, Leske DA. Long-term outcomes after surgical management of chronic sixth nerve palsy. J AAPOS. 2002;6:283–8. doi: 10.1067/mpa.2002.127917. [DOI] [PubMed] [Google Scholar]
- 11.Al-Wadaani FA. Outcome of strabismus surgery by nonadjustable suture among adults attending a University Hospital of Saudi Arabia. Niger J Clin Pract. 2017;20:335–40. doi: 10.4103/1119-3077.196086. [DOI] [PubMed] [Google Scholar]
- 12.Sulayem LM, Bin-Khathlan AA. Outcomes of esotropia surgery in Saudi Arabia: An audit from a single center. Saudi J Ophthalmol. 2018;32:280–5. doi: 10.1016/j.sjopt.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu Y, Wen W, Zou L, Wu S, Wang S, Liu R, et al. Application of SRT plus MR recession in supra-maximal esotropia from chronic sixth nerve palsy. Graefes Arch Clin Exp Ophthalmol. 2019;257:199–205. doi: 10.1007/s00417-018-4102-x. [DOI] [PubMed] [Google Scholar]
- 14.Peragallo JH, Bruce BB, Hutchinson AK, Lenhart PD, Biousse V, Newman NJ, et al. Functional and motor outcomes of strabismus surgery for chronic isolated adult sixth nerve palsy. Neuroophthalmology. 2014;38:320–5. doi: 10.3109/01658107.2014.957780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holmes JM, Leske DA, Christiansen SP. Initial treatment outcomes in chronic sixth nerve palsy. J AAPOS. 2001;5:370–6. doi: 10.1067/mpa.2001.120176. [DOI] [PubMed] [Google Scholar]
- 16.Scott AB, Kraft SP. Botulinum toxin injection in the management of lateral rectus paresis. Ophthalmology. 1985;92:676–83. doi: 10.1016/s0161-6420(85)33982-9. [DOI] [PubMed] [Google Scholar]
- 17.Bendel RB, Afifi AA. Comparison of stopping rules in forward “stepwise” regression. J Am Stat Assoc. 1977;72:46–53. [Google Scholar]
- 18.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989;129:125–37. doi: 10.1093/oxfordjournals.aje.a115101. [DOI] [PubMed] [Google Scholar]
- 19.Cabrejas L, Hurtado-Ceña FJ, Tejedor J. Predictive factors of surgical outcome in oculomotor nerve palsy. J AAPOS. 2009;13:481–4. doi: 10.1016/j.jaapos.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 20.Holmes JM, Droste PJ, Beck RW. The natural history of acute traumatic sixth nerve palsy or paresis. J AAPOS. 1998;2:265–8. doi: 10.1016/s1091-8531(98)90081-7. [DOI] [PubMed] [Google Scholar]
- 21.Scott AB. Botulinum toxin injection of eye muscles to correct strabismus. Trans Am Ophthalmol Soc. 1981;79:734–70. [PMC free article] [PubMed] [Google Scholar]
- 22.Hatt SR, Leske DA, Holmes JM. Comparing methods of quantifying diplopia. Ophthalmology. 2007;114:2316–22. doi: 10.1016/j.ophtha.2007.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]


